Abstract
Sleep in adolescents was significantly impacted by the COVID-19 pandemic. We present a commentary on a range of articles exploring COVID-19’s impact on sleep in teenagers, exploring the variety of effects internationally, interactions with sleep biology and the environment, mental health, online learning and Long COVID. We conclude with vicious and virtuous flowers suggesting ways to mitigate the impacts of COVID-19 on adolescent sleep.
Keywords: Sleep, adolescent, teen, COVID-19, pandemic, paediatric, mental health, circadian, long COVID
Intro
The impacts of the COVID-19 pandemic have been widespread, ranging from the effects the pathogen itself on the body, to the wider social impacts that have been felt worldwide. These impacts have also had individual and collective psychological effects. This article explores what the COVID-19 pandemic has taught us about adolescent sleep. It is not a systematic review, but rather a commentary on the articles that we have found the most interesting over the course of the pandemic. Sleep can be understood via a biopsychosocial and contextual model (Becker et al., 2015). The wide-reaching effects of the pandemic have made the interactions between the areas abundantly clear and shown how vicious cycles can develop. We conclude with suggestions of ways to facilitate virtuous cycles to mitigate the impacts.
Impacts across the globe
In early spring 2020, during the first wave of the pandemic, Socarras et al., 2021 surveyed 498 Canadian adolescents and young adults (aged 12–25 years) about the impact of the pandemic on their self-reported sleep quality, duration and scheduling. The participants were grouped into four age ranges (12–14, 15–17, 18–21 and 22–25), and the study revealed significant differences between these age ranges. No differences were revealed between male and female participants (although the study consisted of more female participants).
Changes in sleep habits and sleep durations were shown to be significantly more pronounced in the teenage years (although present across the ages). Additionally, although longer sleep durations were shown across the board, only the adolescent groups reported an improvement in daytime sleepiness (perhaps indicating the noticeable level of pre-pandemic sleep deprivation in this group, as well as the social confirmatory effect of the daily timetable moving later). The young adult group were likely to have more flexible scheduling pre-pandemic. When coupled with the biological shift to an earlier chronotype which tends to accompany the transition from adolescence to young adulthood, (Roenneberg et al., 2004) this may account for the lack of impact noted on daytime sleepiness. Additionally, the young adult groups reported longer sleep onset latency, more nightmares and early morning wakings (whereas the adolescent groups did not report this). It is important to note that this study observed adolescents in the first wave of the pandemic, where remote teaching and reduced educational expectation was the norm (as well as increased time at home). It may well be that as ‘the new normal’ continues to impose difficulties on families, teachers and children, that the impact of the pandemic is felt at adolescent level also.
Zhou et al., 2020 aimed to examine the influencing factors and prevalence of insomnia in Chinese adolescents and college students. 7736 high school student participants completed their online survey which captured respondents’ experience of the impact of the pandemic, knowledge about coronavirus and attitudes towards forecasts of COVID trends. Additional assessment tools were administered to measure depression and anxiety symptoms, insomnia symptoms and respondents’ social support. This study identified several risk factors for insomnia symptoms, including female sex, living in cities and attending senior high school. Overall, 23.2% of the entire sample reported insomnia symptoms, with junior high students (18%) reporting fewer symptoms than senior high students (25.3%). Compared to both college and junior high school students, a greater proportion of senior high school students were found to have less sleep and more delayed sleep times which had a profound effect on their daytime function.
In a sample of 10,569 junior and senior high school adolescents aged 12–20 years, Zhai et al., (2021) explored factors associated with poor sleep quality during the covid-19 pandemic in China. Poor sleep quality was found to be associated with the presence of a COVID-19 diagnosis in a family member or friend, female gender, senior high school education level, as well as greater use of electronic devices. Improved diet quality and increased daily exercise was strongly related to good sleep quality. This study also provides further support for the link between sleep quality and mental health related factors.
Residence in the Hubei province was inversely related to poor sleep quality. Zhai et al., (2021) suggest this is likely due to the greater availability of medical resources and counselling services available to people living in Hubei. Good sleep quality was also found to be related to longer average time spent monitoring COVID-19 news. The authors speculate that following the news might shatter misconceptions and misinformation about the virus which might be feeding into adolescent anxiety, eventuating in sleep quality deterioration. Whilst in both junior and senior high schoolers anxiety and fear of negative evaluation was related to poor sleep quality, Zhai et al., (2020) suggest that comparatively poorer sleep quality in senior students may be attributable to higher anxiety levels due to a greater number of academic-related stressors. Accordingly, Zhai and colleagues conclude with recommendations to reduce anxiety in adolescents in order to promote healthy sleep habits.
Italy was the first country in Europe to enforce lockdowns with home confinement. Bruni et al., 2021 conducted a survey of sleep patterns of 4314 Italian children and teenagers during COVID-19 lockdowns. The surveys were shared via social media between May and June 2020 and invited responses from caregivers in relation to their children, and explored sleep timings and conditions, as well as screening for specific sleep disorders, neurodevelopmental and medical issues, and exploring drivers of sleep changes. The respondents were broken down into four age groupings: 1–3, 4–5, 6–12 and 13–18 years. Delayed sleep schedules were reported in all groups, and this effect was most pronounced in the latter two groups, with a bedtime on weekdays later than 2300 rising from just below 1% to 28.4% in the school-aged group, and from 12.3% to 63.5% in adolescents. All age groups reported wake times after 800 on weekdays and after 900 on weekends in the majority of participants. Participants took longer to fall asleep during lockdowns. Napping reduced in the two youngest age groups, but increased in teenagers. Screen time increased quite dramatically in all age-ranges. Younger children exhibited higher rates of sleep disorders, including nightmares, anxiety and sleep terrors, as well as daytime sleepiness. Adolescents were less affected by sleep disturbances, with difficulties in falling asleep being the only significantly increased phenomenon. This study agrees with studies by DiGeorgio et al., (2020) and Liu et al., (2020) that also found an increased prevalence of paediatric sleep disorders during lockdown in Italy and China, respectively.
Orgiles et al., 2020 examined the impact of the COVID-19 pandemic on the psychological well-being of 1143 Spanish and Italian children aged 3–18 years, who at the time were subjected to Europe’s most restrictive home confinement rules. This study found that overall, in the course of home-confinement, Italian children gained an average of 30 minutes of sleep and Spanish children’s total sleep time did not change. Corroborating the findings of Bruni et al., 2021, both Italian and Spanish parents reported an increase in children’s use of screens and a reduction in daily physical activity. Interestingly, the changes in children’s routines were found to be significantly associated with parental perception of their family’s coexistence, stress and perceived severity of the impact of COVID-19 on their family’s well-being. In Italy, higher ratings of perceived seriousness of current COVID-19 situation were related to longer screen-time, inactivity, and fewer hours of sleep, and in Spain, this pattern was found in children whose parents reported difficulties in family’s coexistence during quarantine. In both Spain and Italy, however, heightened parental stress was significantly related to fewer hours of sleep.
According to Orgiles et al., 2020, a possible explanation for this trend is that parental stress can translate to more inconsistent discipline and enforcement of routines. Intriguingly, quarantine was found to have a greater psychological and behavioural impact on Spanish children. This finding may be accounted for by the difference in living arrangements and the severity of enforced restrictions in the Italian and Spanish cohorts, in which Italian children had greater opportunities to stay physically active: 52% of Italian homes had a garden compared to just 18% in Spain, and Italian children were permitted to take short daily walks outside under parental supervision, whilst in Spain one was only permitted to go outside for a justified reason like work and shopping for essentials. Spanish children had scarcer opportunities to engage in physical exercise and reap its potential mental health benefits. Collectively, these findings demonstrate the importance of social context in assessing the impact of home-confinement on well-being. Wider context including national restrictions, living arrangements and parental stress and perception of COVID-19 were all shown to be important contributors and predictors of young people’s adoption of healthy sleep habits and routines.
A longitudinal study by Gruber et al., (2021) compared the sleep of a cohort of 62 typically developing Canadian adolescents before and during the COVID-19 pandemic. Using home actigraphy and questionnaires, this study was compared sleep duration, quality, behaviours and social/emotional states across these time points. In line with other findings globally, the study shows that during the pandemic teenagers slept longer and later, with ‘social jet lag’ eliminated at Time two. A significant proportion of the participants were gaining the recommended amount of sleep over the pandemic period, the authors suggest that this confirms that sleep duration in teens is a truly modifiable behaviour that can be addressed through social change. The study also found that both the adolescents’ levels of pre-pandemic cognitive arousal at bedtime and their overall sleep quality was associated with high levels of stress during the pandemic. The authors theorise that there may be a link between impaired sleep, the negative impact of this on executive function, and the ability to quickly adapt to changed circumstances. Although further research is needed into this area to explore the mechanism of action, interventions that target cognitive arousal at bedtime are recommended.
Sleep biology and environmental factors
Relatively early on in the COVID-19 pandemic, in May 2020, Becker and Gregory hypothesised about what the existing literature suggested might be the impacts on child and adolescent sleep and mental health. Suggested drivers of detrimental sleep impacts included respiratory effects of the virus itself, reduced activity levels and poorer health behaviours from isolation and shielding leading to weight gain, and heightened stress related to flux and uncertainty in family and living situations. Biologically, they suggested that reduced sunlight exposure might reduce the clarity of zeitgebers available to keep body-clocks set, and moving academic activities home might reduce the purity of the association between bed and sleep. Remote learning could further reduce the presence of zeitgebers relating to social interaction and routines, as well as increasing reliance on technology, which could increase blue light exposure and therefore interfere with dim-light melatonin onset (Gringras et al., 2015).
Rundle et al., (2020) reported on biological impacts that the contextual factor of school closings were likely to have on children primarily in the United States, as lockdowns were anticipated to lead to twice as much time being spent out of school by pupils, increasing the risk of weight gain. They linked this to an increase in food insecurity (psychological and biological impacts) that would be likely to result from children being out of school, as well as families’ stockpiled foods being more likely to be processed and high in calorie content. This, combined with the contextual factors for children living in smaller inner-city dwellings with less access to safe outdoor space was predicted to raise the chance of lower activity levels, and therefore lead to the obesity. Obesity raises the risk of sleep problems, which can lead to a vicious cycle as sleep problems can exacerbate obesity (Fry, 2020). The importance of considering contextual factors was highlighted in a response letter by Joob and Wiwanitkit (2020) who noted that in rural areas of Thailand and potentially other low and middle-income countries, not being at school meant that children were living with parents without means to support them, and thus, school closures could lead to their being underweight. Being underweight is also associated with shorter sleep duration and insomnia, especially in girls (Sivertsen et al., 2014).
Cellini et al., (2021) surveyed 299 mothers of 6 to 10 year old children about their and their children’s sleep and psychological concerns during the Italian COVID-19 lockdown and reflecting back on the same areas before lockdown had been enacted. The results suggest that context is key: connection to the wider world keeps the body clock set. Under lockdown conditions, the children tended towards delayed sleep phase, with later sleep onset and waking times. Daytime routines were also less rigidly adhered to. This was reflected in their mothers’ sleep profiles, with work seemingly having a protective effect on body clock timings. Increasing severity of delayed sleep timings and reduced sleep quality correlated with psychological impacts, with children exhibiting mood and behavioural issues, and mothers reporting more severe emotional difficulties, as well as perceiving time passing more slowly.
The impact on mental health
From a mental health perspective, Becker and Gregory (2020) suggested that sleep disturbances might be catalysed by mental health concerns that young people already experienced. They cite anxiety and depression especially, as well as suggesting that young people on the autistic spectrum might be particularly affected by upheavals in routines and environments. Contextually, at this stage there was no vaccine available for COVID-19, lockdowns were in place worldwide and an air of unsafe uncertainty (Mason, 2015) pervaded the information that was being shared about COVID-19. Adolescents might be particularly vulnerable to sleep issues affected by declining mental health, suggested Becker and Gregory, since adolescence is often a time for shifting from the family unit into peer relationships, and opportunities for independent activities would likely be stifled by COVID-19. A more hopeful note for some was struck towards the end, when it was suggested that young people with night owl chronotypes might benefit, and that all might benefit from reduced travelling times.
Kuhlman et al., (2021) explored the impact of the pandemic on sleep disturbance as part of a wider study into predictors of adolescent resilience during COVID-19. The study found that teenagers who had high levels of both affiliative and self-effacing humour (using the Humour Styles questionnaire) had a moderated impact of the pandemic on their sleep. Additionally, adolescents with the ability to cognitively reappraise or reframe also showed a moderated relationship between the impact of the pandemic and sleep disturbance. Interestingly, the level of social support given over the pandemic period did not have a relationship to sleep. In a similar way to Gruber et al., (2021), the authors recommend a focus on interventions to encourage cognitive reappraisal and humour in order to aid resilience, which may positively impact on sleep. It should be noted that this study was not carried out using adolescent sleep measures, which is a potential future direction for study.
In the previously described study by Zhou et al., 2020, insomnia symptoms were reported more frequently by participants with more pessimistic COVID-19 projections, less knowledge about the virus and those facing greater disruption to studies and life. Interestingly, this study revealed that subjective and/or objective social support has a protective effect against insomnia symptoms in adolescents. An adequate social support network might indirectly reduce the risk of insomnia by alleviating depression and anxiety symptoms that, in line with previous literature, were found to be strong predictors of sleep disturbances. For instance, 44.8% of students with depression symptoms and 34.4% of students with anxiety symptoms reported insomnia symptoms. Based on these findings Zhou et al., 2020 suggest that in order to minimise the risk of adolescents developing insomnia during the pandemic, particular attention should be paid to obtaining more information about COVID-19 to encourage a more optimistic attitude towards the pandemic, and devoting resources to provide adolescents and young people with social support and counselling.
Sleep and online learning
In the first year of the pandemic, Meltzer et al., (2021) recruited 5245 adolescents in a study that looked at teaching approaches and the impact on sleep over the pandemic. The participants were a geographically and racially diverse sample from across the United States, and the study looked at three methods of teaching (in person, live online with teacher interaction, online with no live or interactive element). School start times were also considered. The study explored the relationships between these approaches and sleep, opportunity, timing and behaviours. The study reports that more scheduled approaches (in person/live online) have a significant impact on sleep scheduling, with earlier bed times and wake times. Even when given the same start times, the live online approach still gave more sleep opportunity (presumably due to school commute times). The study indicates that sufficient sleep opportunity reaches 50% only when online classes begin between 0800 and 0830 at the earliest, with this moving to a post 0900 start for in person working. The study showed that children with a hybrid of in person and online (not live) working showed the greatest variability in sleep, with ‘social jetlag’ appearing at multiple points over the week. The authors indicate that sleep variability is related with negative social and emotional outcomes for adolescents, and as such does not recommend a hybrid approach. It may be that where a hybrid approach is considered, start times on in person days are shifted later to allow for the same sleep/wake times as online days. Additionally, hybrid approaches should include a live online element to minimise sleep disruption. Notably, sleep opportunity is not the same as sleep duration, as it simply indicates the times in which sleep is available to the adolescent. This study did not objectively measure sleep with actigraphy, which could be useful in a repeated study.
Stone et al., (2021) explored the impact of online school on the circadian rhythms of 59 Australian first year students at secondary school. Using actigraphy, sleep diaries, mood measures and salivary dim-light melatonin onset, the study was able to explore the adolescents sleep schedules in relation to their own circadian rhythm. In line with other studies, the results showed that sleep moved later and lasted longer during remote teaching days than in person days. Additionally, the melatonin results showed that teenagers woke at a later circadian phase during remote learning that is more in line with their endogenous sleeping rhythm. The authors report that waking at an earlier circadian phase (closer to the circadian nadir) has a negative association with alertness and cognitive performance. This is an important addition to the ongoing debate around later school times; as previous studies have indicated that longer sleep duration is achievable with later start times, this study adds the element of optimal cognitive performance and its relationship to circadian rhythm to the argument.
Weingert et al., (2021) explored the impact of COVID-19 school closures on the sleep of 6–12 graders in the USA. They found that when schools were closed and students were being taught remotely, a larger proportion were able to sleep for recommended amounts of time, as they tended to wake later having slept for longer. This effect was more pronounced in high schoolers than middle-schoolers. Weingert and colleagues conclude that this supports recommendations that school starts later than 0830 for middle and high schoolers.
Long covid
As the pandemic progressed, the issue of ‘Post-COVID-19 Syndrome’ or ‘Long COVID’ became apparent. Whilst there is no consensus on the definition of Long COVID, the National Institute for Health and Care Excellence (NICE). (2020) defines Post-COVID-19 Syndrome as:
‘signs and symptoms that develop during or after an infection consistent with COVID-19, continue for more than 12 weeks and are not explained by an alternative diagnosis’
Sleep disturbance is listed as a common symptom of Long COVID in the NICE guideline, as well other symptoms that can be linked to sleep disturbance, including cough, pain, depression, anxiety and tinnitus.
Zimmermann et al., (2021) reviewed 14 studies looking at long COVID symptoms in a total of 19,426 children aged 3 to 17. The second most commonly reported symptom was sleep disturbance (2–63%). Most of the studies did not use a control group, which meant symptoms reported could not be directly attributed to COVID-19 infection, as they could have been connected to other psychosocial impacts of the pandemic. Five of the studies had control groups of children and adolescents who were not showing signs of COVID-19 infection, of which three studies found heightened levels of long-term symptoms in the COVID-19 group. Hearteningly, the majority of the studies show that symptoms tend to no longer be present by 12 weeks. Teenagers left with persistent symptom of sleep disturbance might benefit from a course of CBT for insomnia adapted for the pandemic (Altena et al., 2020).
In a cross-sectional study of Italian children, Buonsenso et al., (2021) found that 27.1% of children assessed more than 120 days after COVID diagnosis had at least one persisting symptom. Insomnia was most frequently reported (18.6%), followed by respiratory symptoms (10.8%). Notably, however, these enduring symptoms, including sleep disturbance, did not solely develop in symptomatic children, but also those with asymptomatic and paucisymptomatic presentations of COVID-19.
Osmanov et al., 2021 conducted a cohort study of 518 children aged 0–18 years, who were admitted to a hospital in Moscow with a confirmed COVID diagnosis. With the aim of investigating Long COVID in children post-hospital discharge, parents were invited for a telephone follow-up interview assessing symptom prevalence over time. At follow-up (median 268 days since discharge), 24.7% of children were found to experience at least one persistent symptom. Fatigue was reported by 10.6% of parents, and insomnia was reported by 5.19%. Whilst researchers observed a tendency towards steady decline in symptom prevalence, some symptoms, including sleep-related symptoms, declined more slowly, and 6–7 months after discharge, the number of children with sleep disturbance had fallen from 7.5% to 5.8%. Interestingly, several changes were attributed directly to the COVID-19 infection and not the associated psychosocial impact of the pandemic generally. Specifically, according to 3.5% of parents, less sleep in children was attributed to COVID-19, whilst 2% of parents attributed more sleep to the illness. Osmanov and colleagues also found that children aged six and above and those with allergic diseases had exhibited greater prevalence of such persistent symptoms.
Asadi-Pooya and colleagues (2021) investigated Long COVID in 58 Iranian children aged 6–17, following COVID-19 related hospital admissions. Of the 26 children that reported persisting symptoms, three were found to have sleep-related difficulties. While most children and adolescents rated Long COVID symptoms as mild and tolerable, sleep disturbance was among the minority of symptoms, along with difficulties with exercise and walking, were classed as severe and disabling complications. Partially in agreement with (Osmanov et al., 2021), older age, muscle pain on admission and ICU admission were significant risk factors for development of Long COVID.
Ludvigson (2020) reported on five children aged from 9 to 15 who reported persistent symptoms 6 to 8 months after initial COVID-19 infection. They came to the attention of the researchers as their parents had contacted them voluntarily in the knowledge that they were interested in COVID-19 and wanted to share information about potential long-term effects. None of the children had yet returned to full-time education, and two of them were described as having disordered sleep.
Initial phases of the pandemic tended to involve more stringent lockdowns and disruptions to education and other activities. As time passes and schedules and opportunities have gradually moved towards pre-pandemic configurations, the longer-term impacts of COVID-19 may become more apparent. The CLoCK study (Stephenson et al., 2021) will explore prevalence of symptoms including sleep problems via questionnaires, in at least 3000 children 3, 6, 12 and 24 months post COVID diagnosis, and compare them to age-matched children with negative test results who have been through similar environmental changes.
Conclusion
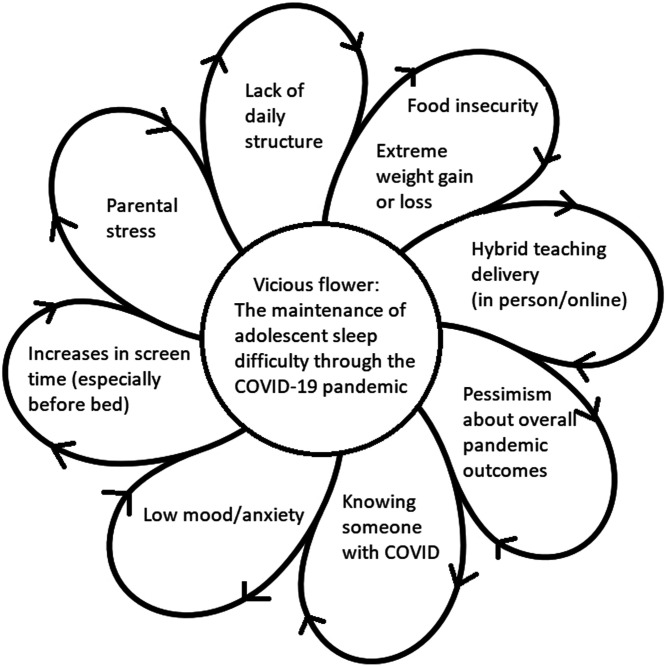
The COVID-19 pandemic has created a unique set of circumstances that has allowed us to explore factors that affect the sleep of children and the research covered here suggests a range of contributors to the vicious cycle that can be detrimental to sleep in young people, and also potential levers to facilitate a more virtuous cycle, supporting sleep.
A lack of daily structure during lockdowns especially contributed to the development of sleep difficulties. Younger children tended to exhibit higher levels of a wide range of sleep problems during lockdowns, whereas teenagers tended to mainly report difficulties with extended sleep onset latency. This lack of structure can be in the form of a less well-defined daily routine and teaching delivery switching between in-person and online. Changes in the delivery of education also had implications for perceived actual food security for children who might rely on school for the provision of food during term times pre-pandemic. In more affluent countries, this could contribute to children eating less nutritious foods, and gaining weight, and in poorer areas, meals might be missed leading to children becoming underweight. Both weight extremes are associated with poorer sleep. As sleep worsens, healthy weight maintenance also becomes more difficult.
Lockdowns were associated with large increases in screen time, which tends not to be conducive to sleep, especially if screens are being used immediately before or in bed. Parental stress was also linked to shorter sleep durations in children, and this was thought to relate to increased difficulties with keeping a consistent routine. Children with less optimistic beliefs about how the pandemic was likely to pan out tended to have worse sleep. Knowing someone with COVID-19 tended to reduce sleep quality. This linked with the finding that researching, reading and knowing less about COVID-19 correlated with worse sleep. Perhaps there is a sweet-spot in terms of information gathering, where access to reliable information about the pandemic, and screen use at appropriate times might be more conducive to better sleep.
Various studies reported correlations between mental health concerns and sleep difficulties. Low mood and anxiety linked closely with sleep difficulties such as insomnia. Exam-related anxieties were also thought to play a role in the sleep difficulties manifesting in older teens. As sleep onset became later, and sleep quality diminished, there was a correlation with impacts on mental health. Figure 1–Vicious flower (Moorey, 2010).
Figure 1.
Vicious flower formulation of factors contributing to poor adolescent sleep during COVID-19.
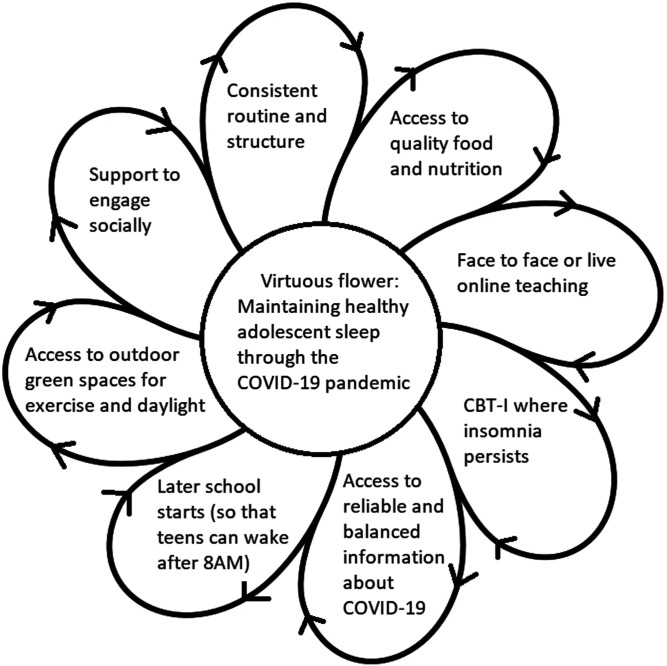
Possibilities for promoting sleep-promoting virtuous cycles include maximising the consistency of daily routines, and making teaching face to face, or live if it is conducted remotely. A key factor is the shifting of school start times later than 0830, as this will benefit the mood and learning ability for a significant proportion of teenagers who have later chronotypes. Policy changes are necessary to facilitate this, as well as support from individual schools. Providing access to quality food for children in need of support, as well as the provision of green spaces for outdoor exercise which has multiple potential benefits including daylight exposure for circadian rhythm entrainment and positive mood impacts. Facilitating access to reliable sources of information about the virus and its impacts could also help people to be less anxious and to sleep better. Support to engage socially, both face to face where safe and via other methods tends to help with wake-sleep cycles happening at appropriate timings, and social support seems to have a protective effect against insomnia. In cases where sleep has been adversely affected to the extent that insomnia develops, provision of support in the form of CBT for insomnia and counselling could be of benefit. Figure 2–Virtuous flower (Moorey, 2010).
Figure 2.
Virtuous flower formulation of strategies to optimise adolescent sleep during COVID-19.
Author biographies
Charlie Tyack is a clinical psychologist who currently works in paediatric sleep and adolescent to adult auditory implants. His research interests include sleep, acceptance and commitment therapy, functional neurological conditions , dementia and auditory implants.
Shreena Unadkat is a clinical psychologist in paediatrics across Evelina London Children's Hospital and Royal Hospital for Children, Glasgow. She is also an associate fellow on the Salomons Doctorate in Clinical Psychology. Her current research interests are in sleep medicine, LGBTQ teen health, and radicalisation/the PREVENT strategy.
Justyna Voisnyte, an undergraduate psychology student at Queen Mary University of London, currently undergoing a psychology placement in the Paediatric Sleep Department at Evelina London Children’s Hospital at Guy’s and St Thomas’ Trust. At present, conducting a systematic review concerned with the cognitive profile of children with narcolepsy.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Charlie Tyack https://orcid.org/0000-0002-1094-9565
Justyna Voisnyte https//orcid.org/0000-0002-2491-6887
References
- Altena E., Baglioni C., Espie C. A., Ellis J., Gavriloff D., Holzinger B., Schlarb A., Frase L., Jernelov S., Riemann D. (2020). Dealing with sleep problems during home confinement due to the COVID‐19 outbreak: Practical recommendations from a task force of the European CBT‐I Academy. Journal of Sleep Research, 29(4), e13052. 10.1111/jsr.13052 [DOI] [PubMed] [Google Scholar]
- Becker S. P., Gregory A. M. (2020). Editorial perspective: Perils and promise for child and adolescent sleep and associated psychopathology during the COVID-19 pandemic. Journal of Child Psychology & Psychiatry, 61(7), 757–759. 10.1111/jcpp.13278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker S. P., Langberg J. M., Byars K. C. (2015). Advancing a biopsychosocial and contextual model of sleep in adolescence: A review and introduction to the special issue. Journal of Youth and Adolescence, 44(2), 239–270. 10.1007/s10964-014-0248-y [DOI] [PubMed] [Google Scholar]
- Bruni O., Malorgio E., Doria M., Finotti E., Spruyt K., Melegari M. G., Villa M.P, Ferri R. (2021). Changes in sleep patterns and disturbances in children and adolescents in Italy during the Covid-19 outbreak. Sleep Medicine. 10.1016/j.sleep.2021.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buonsenso D., Munblit D., De Rose C., Sinatti D., Ricchiuto A., Carfi A., Valentini P. (2021). Preliminary evidence on long COVID in children. Acta Paediatrica, 110(7), 2208–2211. 10.1111/apa.15870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cellini N., Di Giorgio E., Mioni G., Di Riso D. (2021). Sleep and psychological difficulties in italian school-age children during COVID-19 lockdown. Journal of Pediatric Psychology, 46(2), 153–167. 10.1093/jpepsy/jsab003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Giorgio E., Di Riso D., Mioni G., Cellini N. (2021). The interplay between mothers’ and children behavioral and psychological factors during COVID-19: An Italian study. European Child & Adolescent Psychiatry, 30(9), 1401–1412. 10.1007/s00787-020-01631-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fry A. (2020, November 29). Obesity and Sleephttps://www.sleepfoundation.org/physical-health/obesity-and-sleep.
- Gringras P., Middleton B., Skene D. J., Revell V. L. (2015). Bigger, brighter, bluer-better? Current light-emitting devices-adverse sleep properties and preventative strategies. Frontiers in Public Health, 3, 233. 10.3389/fpubh.2015.00233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber R., Gauthier-Gagne G., Voutou D., Somerville G., Saha S., Boursier J. (2021). Pre-pandemic sleep behavior and adolescents’ stress during Covid-19: a prospective longitudinal study. Child and Adolescent Psychiatry and Mental Health, 15(1), 1–13. 10.1186/s13034-021-00399-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joob B., Wiwanitkit V. (2020). COVID-19, school closings, and weight gain. Obesity (Silver Spring), 28(6), 1006. 10.1002/oby.22825 [DOI] [PubMed] [Google Scholar]
- Kuhlman K. R., Straka K., Mousavi Z., Tran M. L., Rodgers E. (2021). Predictors of adolescent resilience during the COVID-19 pandemic: Cognitive reappraisal and humor. Journal of Adolescent Health, 69(5), 729–736. 10.1016/j.jadohealth.2021.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z., Tang H., Jin Q., Wang G., Yang Z., Chen H., Yan H., Rao W., Owens J. (2021). Sleep of preschoolers during the coronavirus disease 2019 (COVID‐19) outbreak. Journal of Sleep Research, 30(1), e13142. 10.1111/jsr.13142 [DOI] [PubMed] [Google Scholar]
- Ludvigsson J. (2020). Case report and systematic review suggest that children may experience similar long‐term effects to adults after clinical COVID‐19. Acta Paediatrica, 110(3), 914–921. 10.1111/apa.15673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason B. (2015). Towards positions of safe uncertainty. InterAction-The Journal of Solution Focus in Organisations, 7(1), 28-43. [Google Scholar]
- Meltzer L. J., Saletin J. M., Honaker S. M., Owens J. A., Seixas A., Wahlstrom K. L., Wolfson A. R., Wong P., Carskadon M. A. (2021). COVID-19 instructional approaches (in-person, online, hybrid), school start times, and sleep in over 5,000 US adolescents. Sleep. in-person online. https://doi.org/10.1093%2Fsleep%2Fzsab180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moorey S. (2010). The six cycles maintenance model: Growing a “vicious flower” for depression. Behavioural and Cognitive Psychotherapy, 38(2), 173–184. 10.1017/s1352465809990580 [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (2020). COVID-19 rapid guideline: Managing the long-term effects of COVID-19. [NICE Guideline No. 188]. https://www.nice.org.uk/guidance/ng188 [PubMed] [Google Scholar]
- Orgiles M., Morales A., DelVeccio E., Mazzeschi C., Espada J. P. (2020). Immediate psychological effects of COVID-19 quarantine in youth from Italy and Spain. SSRN Electronic Journal, 11, 579038. 10.2139/ssrn.3588552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osmanov I., Spiridonova E., Bobkova P., Gamirova A., Shikhaleva A., Andreeva M., Blyuss O., Andreeva M., El-Taravi Y., DunnGalvin A., Comberiati P., Peroni D. G., Apfelbacher C., Genuneit J., Mazankova L., Miroshina A., Chistyakova E., Samitova E., Borzakova S., Munblit D. (2021). Risk factors for long COVID in previously hospitalised children using the ISARIC Global follow-up protocol: A prospective cohort study. European Respiratory Journal, 58(6), 2101341. 10.1183/13993003.01341-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roenneberg T., Kuehnle T., Pramstaller P. P., Ricken J., Havel M., Guth A., Merrow M. (2004). A marker for the end of adolescence. Current Biology, 14(24), R1038–R1039. 10.1016/j.cub.2004.11.039 [DOI] [PubMed] [Google Scholar]
- Rundle A. G., Park Y., Herbstman J. B., Kinsey E. W., Wang Y. C. (2020). COVID-19 related school closings and risk of weight gain among children. Obesity (Silver Spring), 28(6), 1008–1009. https://doi.org/10.1002%2Foby.22813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sivertsen B., Pallesen S., Sand L., Hysing M. (2014). Sleep and body mass index in adolescence: results from a large population-based study of Norwegian adolescents aged 16 to 19 years. BMC Pediatrics, 14(1), 204. 10.1186/1471-2431-14-204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Socarras L. R., Potvin J., Forest G. (2021). COVID-19 and sleep patterns in adolescents and young adults. Sleep Medicine, 83, 26-33. 10.1016/j.sleep.2021.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson T., Shafran R., De Stavola B., Rojas N., Aiano F., Amin-Chowdhury Z., Mcowat K., Simmons R., Zavala M., CLoCk Consortium. Ladhani S. N. (2021). Long COVID and the mental and physical health of children and young people: national matched cohort study protocol (the CLoCK study). BMJ Open, 11(8), e052838. 10.1136/bmjopen-2021-052838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone J. E., Phillips A. J., Chachos E., Hand A. J., Lu S., Carskadon M. A., Klerman E. B., Lockley S. W., Wiley J. F., Bei B., Rajaratnam S. M. W., CLASS Study Team . (2021). In‐person vs home schooling during the COVID‐19 pandemic: Differences in sleep, circadian timing, and mood in early adolescence. Journal of Pineal Research, 71(2), e12757. 10.1111/jpi.12757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weingart R., Bryan C., Olson D., Gazmararian J., Rosati B., Hale L., Van Gilder M. (2021). Adolescent sleep duration and timing during early COVID-19 school closures. Sleep Health, 7(5), 543–547. 10.1016/j.sleh.2021.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai X., Zeng J., Eshak E., Zhang Y., Yang M., Di L., Xiang B., Cao J. (2021). The influencing factors of sleep quality among Chinese junior and senior high school adolescents during the COVID-19 pandemic. Journal of Tropical Pediatrics, 67(4), fmab069. 10.1093/tropej/fmab069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou S., Wang L., Yang R., Yang X., Zhang L., Guo Z., Chen J., Wang J., Chen J. (2020). Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Medicine, 74, 39-47. 10.1016/j.sleep.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmermann P., Pittet L. F., Curtis N. (2021). How common is long COVID in children and adolescents? The Pediatric Infectious Disease Journal, 40(12), e482–e487. 10.1097/INF.0000000000003328 [DOI] [PMC free article] [PubMed] [Google Scholar]