Abstract
Background and Purpose
Changes to hospital systems were implemented from March 2020 in Australia in response to the coronavirus disease 2019 pandemic, including decreased resources allocated to stroke units. We investigate changes in the quality of acute care for patients with stroke or transient ischemic attack during the pandemic according to patients’ treatment setting (stroke unit or alternate ward).
Methods
We conducted a retrospective cohort study of patients admitted with stroke or transient ischemic attack between January 2019 and June 2020 in the Australian Stroke Clinical Registry (AuSCR). The AuSCR monitors patients’ treatment setting, provision of allied health and nursing interventions, prescription of secondary prevention medications, and discharge destination. Weekly trends in the quality of care before and during the pandemic period were assessed using interrupted time series analyses.
Results
In total, 18,662 patients in 2019 and 8,850 patients in 2020 were included. Overall, 75% were treated in stroke units. Before the pandemic, treatment in a stroke unit was superior to alternate wards for the provision of all evidence-based therapies assessed. During the pandemic period, the proportion of patients receiving a swallow screen or assessment, being discharged to rehabilitation, and being prescribed secondary prevention medications decreased by 0.58% to 1.08% per week in patients treated in other ward settings relative to patients treated in stroke units. This change represented a 9% to 17% increase in the care gap between these treatment settings during the period of the pandemic that was evaluated (16 weeks).
Conclusions
During the first 6 months of the pandemic, widening care disparities between stroke units and alternate wards have occurred.
Keywords: Quality of health care, Stroke, COVID-19
Introduction
Hospital systems have been changed in response to the coronavirus disease 2019 (COVID-19) pandemic in order to ensure the virus does not spread, and that health care workers and visitors are kept safe. A consequence has been the redeployment of hospital staff, changes to emergency department workflows, cancelation of elective surgery, and repurposing of hospital wards to increase capacity [1]. For conditions such as acute stroke or transient ischemic attack, reports on the effect of these disruptions have been mixed, but generally point to delays in presentation and treatment [2]. Particularly of concern in Australia, is the fact that resources in hospitals with specialist services dedicated for stroke—whereby hospital beds are collocated and there is a dedicated and experienced interdisciplinary team that manages the patients in this part of the hospital (also known as a stroke unit ward)—have had the number of beds reduced or specialized staff redeployed [3]. Care in organized, dedicated stroke units by expert, interdisciplinary clinicians ensures best-practice treatments are provided and outcomes are better for patients than if treated in alternate ward settings [4,5]. We have previously reported that, despite few COVID-19 cases in the first wave of the pandemic (first case recorded January 25, 2020 until mid-June 2020, when new cases were under 20 per day), significantly fewer patients had access to stroke units, and the length of stay in the hospital decreased [6].
The downstream effects of these changes in hospital treatment pathways for patients with stroke and transient ischemic attack during the pandemic have not been previously reported by the type of ward setting the patients have been managed within. We aimed to examine the quality of care for patients admitted to the hospital with stroke or transient ischemic attack during the COVID-19 pandemic according to the ward setting they were treated in (stroke units or other wards).
Methods
The data and study materials that support the findings of this study are available from the corresponding author with the permission of the Florey Institute of Neuroscience and Mental Health acting on behalf of the Australian Stroke Clinical Registry (AuSCR) Consortium. Restrictions apply to the availability of these data, which were used under license for this study (Requests to access these datasets should be directed to admin@ auscr.com.au).
The AuSCR is a clinical quality registry that was established in 2009 to monitor and improve the quality of care provided to patients admitted with acute stroke or transient ischemic attack. Public hospitals from six Australian states and territories contribute data to the AuSCR, with funding provided primarily by state governments. Hospitals participating in the AuSCR prospectively collect a standardized minimum dataset that includes information on demographic and clinical characteristics of patients, and evidence-based therapies provided during the admission and at discharge from the hospital [7]. The evidence-based therapies monitored in the AuSCR include treatment in a stroke unit, the provision of reperfusion therapies (intravenous thrombolysis and endovascular clot retrieval), allied health and nursing interventions, the prescription of secondary stroke prevention medications, and provision of discharge care plans.
In this study, data on admissions between January 1, 2019 and June 23, 2020 were retrospectively analyzed. Only admissions from hospitals contributing data in both 2019 and 2020 were included in this analysis. Data were excluded from one hospital contributing fewer than 100 cases over the study period. The last 2 weeks of data for the study period were removed due to low case numbers entered into the AuSCR (defined as more than two standard deviations below the average number of admissions per week) because of delays with data collection (Supplementary Figure 1).
This study was approved by the Monash University Human Research Ethics Committee (project 26558). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements. The AuSCR uses opt-out consent and a waiver of consent for deaths in order to minimize selection bias [8].
Data analysis and statistics
Descriptive statistics appropriate to the type and distribution of the data were used. Patient demographics, clinical characteristics, process of care metrics for the provision of evidence-based therapies, and hospital outcomes such as length of stay and discharge destination were compared between treatment groups and time periods using chi-square and Kruskal-Wallis tests. In the case where a specific evidence-based therapy for any individual hospital contained >30% missing data, these hospitals were excluded from the analysis of that specific variable. In all other cases where there was missing data related to the provision of evidence-based therapies, it was assumed the therapy was not provided.
Proportions of patients provided allied health and nursing interventions (antithrombotic medications within 48 hours of arrival, mobilized, and swallow screen or assessment) and discharge processes (prescribed secondary prevention antihypertensive medication, antithrombotic medication and lipid lowering medication; discharged to the community with a care plan; and discharge to rehabilitation) were calculated by week and ward setting (stroke units or other wards). Differences between ward settings were assessed in an interrupted time series analyses [9]. The provision of reperfusion therapies was not investigated in this analysis because provision of reperfusion therapies generally occurs in Emergency Departments and patients who receive reperfusion therapies are subsequently managed in a stroke unit since they require intensive monitoring.
Trends in the proportion of patients provided these evidence-based therapies were compared before and after the week including March 1, 2020 (week 61 in the model spanning February 25, 2020 to March 2, 2020). This interruption date of March 1, 2020 coincided with the first COVID-19-related death in Australia. Nationwide restrictions related to reducing COVID-19 transmission in the community were imposed on March 21, 2020. Seasonality in admissions was considered by using a lag period of 53 weeks for correlations. Estimates were adjusted by the number of episodes per week and the number of patients with different clinical diagnoses (stroke, intracerebral hemorrhage, transient ischemic attack, and undetermined stroke). Analyses related to the provision of antithrombotic medications and lipid lowering medication were conducted with patients with intracerebral hemorrhage excluded.
β Coefficients related to the interrupted time series analyses signify either (1) the difference in the average weekly percentage change over several weeks (trend) between groups; or (2) the difference in a percentage change in a given week between groups. Positive values indicate a greater relative percentage increase in stroke units compared with other ward settings. Negative values indicate a greater relative percentage decrease in stroke units compared with other ward settings. Data were analyzed using STATA/SE 15.0 (StataCorp., College Station, TX, USA).
Results
There were 27,512 admissions from 61 hospitals (from five states and territories) registered in the AuSCR between January 2019 and June 2020 that were included for analysis (Table 1). The proportion of patients treated in a stroke unit decreased from 76% (16,666 of 21,892 admissions) during the pre-pandemic period to 69% (3,870 of 5,620 admissions) during the pandemic period (P<0.001). Distributions of diagnosis, previous history of stroke, arrival by ambulance, and transfer from another hospital were different between the pre-pandemic and pandemic periods. Compared with patients who were treated outside of stroke units, patients treated in stroke units were more often male, more often had an ischemic stroke, less often had an in-hospital stroke, more often arrived by ambulance, more often transferred from another hospital, less often able to walk on admission (proxy for greater stroke severity), and had longer lengths of stay in both the pre-pandemic and pandemic periods.
Table 1.
Patient characteristics by ward setting and pandemic period
| Characteristic | Pre-pandemic (Jan 1, 2019–Feb 24, 2020) |
Pandemic (Feb 25, 2020–Jun 23, 2020) |
Comparison of periods* |
|||||
|---|---|---|---|---|---|---|---|---|
| Treated in a stroke unit |
Treated in a stroke unit |
|||||||
| No (n=5,226) | Yes (n=16,666) | P | No (n=1,750) | Yes (n=3,870) | P | P | ||
| Age (yr) | 0.083 | 0.062 | 0.643 | |||||
| <65 | 1,342 (26) | 4,198 (26) | 404 (23) | 1,009 (26) | ||||
| 65–74 | 1,236 (24) | 3,935 (24) | 433 (25) | 955 (25) | ||||
| 75–84 | 1,438 (28) | 4,951 (30) | 523 (30) | 1,130 (29) | ||||
| ≥85 | 1,051 (21) | 3,283 (20) | 373 (22) | 741 (19) | ||||
| Male | 2,635 (52) | 9,322 (57) | <0.001 | 924 (53) | 2,162 (56) | 0.034 | 0.636 | |
| Diagnosis | <0.001 | <0.001 | 0.001 | |||||
| Intracerebral hemorrhage | 794 (16) | 1,786 (11) | 214 (15) | 443 (12) | ||||
| Ischemic stroke | 2,387 (48) | 12,781 (77) | 671 (47) | 2,885 (75) | ||||
| Transient ischemic attack | 1,633 (33) | 1,807 (11) | 490 (34) | 455 (12) | ||||
| Undetermined stroke | 194 (4) | 236 (1) | 60 (4) | 50 (1) | ||||
| In-hospital stroke | 353 (7) | 433 (3) | <0.001 | 77 (6) | 92 (2) | <0.001 | 0.367 | |
| Previous history of stroke | 1,029 (21) | 3,636 (22) | 0.150 | 214 (19) | 743 (21) | 0.105 | 0.012 | |
| Arrival by ambulance | 3,346 (73) | 12,478 (78) | <0.001 | 913 (77) | 2,913 (81) | 0.002 | <0.001 | |
| Transferred from another hospital | 547 (11) | 3,139 (19) | <0.001 | 118 (8) | 656 (17) | <0.001 | <0.001 | |
| Ability to walk on admission | 2,181 (48) | 6,432 (41) | <0.001 | 496 (47) | 1,384 (40) | <0.001 | 0.298 | |
| Median length of stay (day) (quartile 1-3) | 2 (1–5) | 4 (2–8) | <0.001 | 2 (1–5) | 4 (2–8) | <0.001 | <0.001 | |
Values are presented as number (%) unless otherwise specified.
Patients within periods were aggregated in this comparison.
Patients treated in stroke units more often received evidence-based care in both the pre-pandemic and pandemic periods compared with those treated in other ward settings (Table 2). Apart from discharge to inpatient rehabilitation, there were differences in the proportion of patients provided evidence-based therapies between the pre-pandemic and pandemic periods. Among those treated outside of stroke units, there was a reduction from the pre-pandemic period to the pandemic period in the proportion of patients receiving mobilization, swallow screen or assessment, and secondary prevention medications at discharge from the hospital. These changes were not observed in patients who were treated in stroke units.
Table 2.
Treatment by ward setting and pandemic period
| Variable | Pre-pandemic (Jan 1, 2019–Feb 24, 2020) |
Pandemic (Feb 25, 2020–Jun 23, 2020) |
Comparison of periods* |
||||
|---|---|---|---|---|---|---|---|
| Treated in a stroke unit |
Treated in a stroke unit |
||||||
| No | Yes | P | No | Yes | P | P | |
| Provided antithrombotic medication within 48 hours of arrival† | 2,092/3,371 (62) | 8,289/11,697 (71) | <0.001 | 543/843 (64) | 1,840/2,484 (74) | <0.001 | 0.002 |
| Mobilised during the admission | 3,113/4,951 (63) | 11,679/14,692 (79) | <0.001 | 719/1,578 (46) | 2,412/3,402 (71) | <0.001 | <0.001 |
| Provided swallow screen or assessment | 2,478/4,631 (54) | 12,697/14,129 (90) | <0.001 | 583/1,385 (42) | 2,709/3,029 (89) | <0.001 | <0.001 |
| Discharged to inpatient rehabilitation | 506/5,012 (10) | 4,234/16,249 (26) | <0.001 | 155/1,330 (12) | 987/3,578 (28) | <0.001 | 0.141 |
| Prescribed antihypertensive medication at discharge | 2,656/4,059 (65) | 11,159/14,607 (76) | <0.001 | 613/1,245 (49) | 2,352/3,260 (72) | <0.001 | <0.001 |
| Prescribed antithrombotic medication at discharge† | 3,157/3,773 (84) | 12,642/13,636 (93) | <0.001 | 724/1,175 (62) | 2,626/3,022 (87) | <0.001 | <0.001 |
| Prescribed lipid lowering medication at discharge† | 2,587/3,769 (69) | 11,039/13,649 (81) | <0.001 | 616/1,177 (52) | 2,268/3,004 (76) | <0.001 | <0.001 |
| Discharged to the community with a care plan | 1,303/2,656 (49) | 5,576/7,499 (74) | <0.001 | 322/624 (52) | 1,284/1,606 (80) | <0.001 | <0.001 |
Values are presented as number/total number (%).
Patients within periods were aggregated in this comparison;
Excluding patients with intracerebral hemorrhage.
Trends in the provision of nursing and allied health interventions
In the pre-pandemic period, there were small differences observed in the trends of provision of some nursing and allied health interventions between patients treated in stroke units and those treated outside of stroke units (Figure 1, Supplementary Table 1). There was a 0.09% per week increase in the provision of antithrombotic medications within 48 hours of arrival in patients treated in stroke units relative to those treated outside of a stroke unit (β=0.09; 95% confidence interval [CI], 0.04 to 0.14), and a 0.15% per week decrease in mobilization during the admission in patients treated in stroke units relative to those treated outside of a stroke unit (β=–0.15; 95% CI, –0.23 to –0.07). No such differences in trends were detected within and between groups for the provision of swallow screen or assessment and discharge to rehabilitation during the pre-pandemic period.
Figure 1.
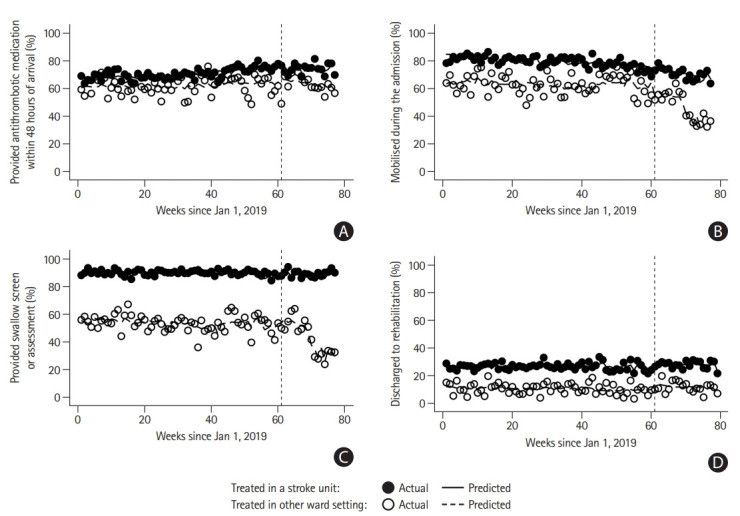
Proportion of patients (A) provided antithrombotic medication within 48 hours of arrival (excluding patients with intracerebral hemorrhage), (B) mobilized during the admission, (C) provided swallow screen or assessment, and (D) discharged to rehabilitation. The vertical line (week 61) indicates the week of the interruption used in this study (1/3/2020, the first coronavirus disease 2019 [COVID-19] related death in Australia). Significant difference in weekly trend between groups prior to interruption (β and 95% confidence intervals [CIs] presented): provided antithrombotic medication within 48 hours of arrival 0.09 (95% CI, 0.04 to 0.14); mobilized during the admission –0.15 (95% CI, –0.23 to –0.07). Significant difference during week of interruption between groups (week 61): provided antithrombotic medication within 48 hours of arrival –5.35 (95% CI, –9.08 to –1.61); provided swallow screen or assessment –5.81 (95% CI, –8.62 to –2.99); discharged to rehabilitation –2.2 (95% CI, –3.72 to –0.68). Significant difference in weekly trend between groups in post-interruption period: provided swallow screen or assessment 0.86 (95% CI, 0.48 to 1.24); discharged to rehabilitation 0.6 (95% CI, 0.37 to 0.83). β in a period signifies the difference in the average weekly percentage change over several weeks (trend) between groups. β during the week of the interruption signifies the difference in a percentage change during that week between groups. Positive values indicate a greater relative percentage increase in the provision of evidence-based care in stroke units compared with other ward settings. Negative values indicate a greater relative percentage decrease in the provision of evidence-based care in stroke units compared with other ward settings. Other point estimates relevant to the figure are provided in the Supplementary Table 1.
During the first week of the pandemic period, there was a relative decrease in the proportion of patients provided nursing and allied health interventions among patients treated in stroke units compared with those treated outside of stroke units. The relative decrease was greatest for the provision of swallow screen or assessment (β=–5.81; 95% CI, –8.62 to –2.99), followed by the provision of antithrombotic medications within 48 hours of arrival (β=–5.35; 95% CI, –9.08 to –1.61) and discharge to inpatient rehabilitation (β=–2.44; 95% CI, –3.75 to –1.12). There was no relative increase or decrease between groups observed in the proportion of patients mobilized during the admission.
Following the first week, the proportion provided a swallow screen or assessment increased for patients treated in stroke units and decreased for patients treated outside of stroke units during the pandemic period. Trends in the proportion of patients discharged to inpatient rehabilitation were unaffected in patients treated outside of stroke units, but there appeared to be an increase in patients discharged to inpatient rehabilitation in those treated in stroke units. This corresponded to a 0.86% per week decrease in the proportion provided a swallow screen or assessment observed in patients treated in alternate ward settings relative to those treated in a stroke unit (β=0.86; 95% CI, 0.48 to 1.24). There were similar findings for the proportion of patients discharged to inpatient rehabilitation, with a 0.52% per week decrease observed in patients treated in alternate ward settings relative to those treated in a stroke unit (β=0.52; 95% CI, 0.09 to 0.95).
Trends in the provision of secondary prevention medications and care plans
In the pre-pandemic period, there was a small difference observed in the trends of provision of care plans at discharge be- tween patients treated in stroke units and those treated outside of stroke units (Figure 2, Supplementary Table 2). There was a 0.09% per week decrease in the provision of care plans among those discharged to the community in patients treated in stroke units relative to those treated outside of a stroke unit (β=–0.09; 95% CI, –0.17 to –0.01). No such differences in trends between groups were seen in the pre-pandemic period for the provision of secondary prevention medications at discharge.
Figure 2.
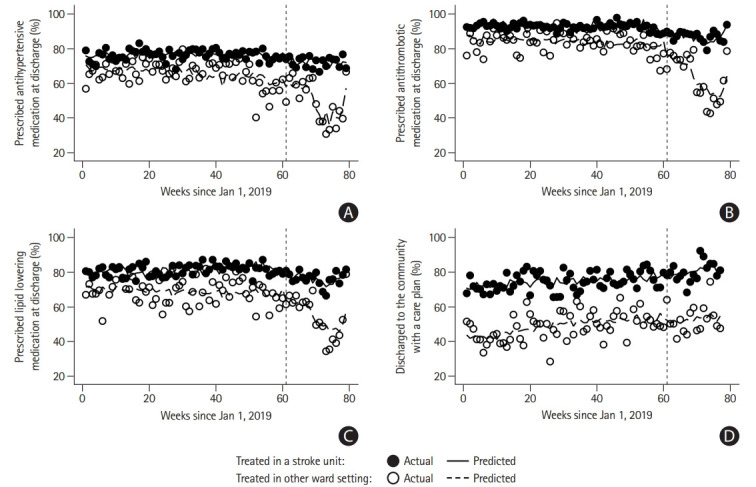
Proportion of patients prescribed secondary prevention medications (A: antihypertensive medication; B: antithrombotic medication; C: lipid lowering medication) at discharge and (D) discharged to the community with a care plan. The vertical line (week 61) indicates the week of the interruption used in this study (1/3/2020, the first coronavirus disease 2019 [COVID-19] related death in Australia). Significant difference in weekly trend between groups prior to interruption (β and 95% confidence intervals [CIs] presented): discharged to the community with a care plan –0.09 (95% CI, –0.17 to –0.01). Significant difference during week of interruption between groups (week 61): discharged to the community with a care plan 3.61 (95% CI, 0.28 to 6.94). Significant difference in weekly trend between groups in post-interruption period: provided antihypertensive medication at discharge 0.58 (95% CI, 0.08 to 1.07); provided antithrombotic medication at discharge 1.08 (95% CI, 0.78 to 1.38); provided lipid lowering medication at discharge 0.69 (95% CI, 0.28 to 1.09). β in a period signifies the the difference in the average weekly percentage change over several weeks (trend) between groups. β during the week of the interruption signifies the difference in a percentage change during that week between groups. Positive values indicate a greater relative percentage increase in the provision of evidence-based care in stroke units compared with other ward settings. Negative values indicate a greater relative percentage decrease in the provision of evidence-based care in stroke units compared with other ward settings. Other point estimates relevant to the figure are provided in the Supplementary Table 2.
In the first week of the pandemic period, the proportion of patients treated in stroke units that were discharged with a care plan increased relative to those treated outside of stroke units (β=3.61; 95% CI, 0.28 to 6.94). No such differences between groups were observed for the provision of secondary prevention medications at discharge.
During the pandemic period, trends in the provision of secondary prevention medications were unaffected for patients treated in stroke units, but the proportions of patients treated in alternate ward settings who were provided secondary prevention medications decreased. There was a 0.58% per week decrease in the provision of antihypertensive medications at discharge observed in patients treated in alternate ward settings relative to those treated in a stroke unit (β=0.58; 95% CI, 0.08 to 1.07). There were similar findings for the provision of antithrombotic medications (β=1.08; 95% CI, 0.78 to 1.38) and lipid lowering medications (β=0.69; 95% CI, 0.28 to 1.09). These differences in trends between groups were not seen for the provision of care plans in the pandemic period.
Discussion
To our knowledge, an in-depth assessment of the effect of reduced access to specialized stroke wards and clinicians as an unintended consequence of the COVID-19 pandemic has not been reported. Globally, there have been concerns about the effects of staff redeployment and the reorganization of stroke services, in addition to people with stroke symptoms delaying their presentation to the hospital [10]. Reports from other countries on the overall changes to the quality of care for patients with stroke have been mixed and mainly focused on use of thrombolysis or endovascular clot retrieval for those with stroke [11-14]. The changes in the resources available for stroke in Australian hospitals has meant fewer patients getting access to stroke units during the pandemic [6]. However, what we have learned in this investigation of care in stroke units compared with other ward settings is that the quality of care provided to patients treated in stroke units was largely unaffected. In contrast, with more patients being managed in alternate wards since the pandemic began, our findings of poorer quality of care in these settings when compared with before the pandemic is concerning. The findings reinforce the importance of ensuring the availability of doctors, nurses, and allied health staff with expertise and experience in managing patients with stroke are treating people with stroke. Care in stroke units by staff with expertise must be preferentially offered during a pandemic to ensure standards of care are upheld.
In this study, we examined evidence-based care that was undertaken in the wards following care in emergency departments. We found evidence that the quality of care may have been negatively affected by changes to hospital systems made in response to the COVID-19 pandemic. Using the same cohort, we had previously reported that access to intravenous thrombolysis and endovascular clot retrieval were similar; however, door-to-needle times were longer during the peak national pandemic period (March to April 2020) [6].
In addition, the overall proportion of patients with stroke or transient ischemic attack that received evidence-based therapies during their hospital admission had declined during the pandemic period [6]. However, we did not understand the main driver for these findings until the analysis conducted for this current study. Consistent with prior research, we found evidence that stroke units were superior to alternate wards in providing evidence-based care [5,15]. We also found novel evidence that the disparity in the provision of evidence-based therapies between patients treated in stroke units compared with those treated in other ward settings increased during the pandemic period, when compared with pre-pandemic standards. We surmise that competing priorities or lack of experience in how to manage different aspects of stroke in alternate wards has led to these findings.
The strengths of this study include the large standardized dataset of patients admitted with stroke and transient ischemic attack in major public hospitals treating stroke in five states and territories of Australia. In Australia, over a quarter of hospitals treating patients with stroke do not have a stroke unit. 16 All hospitals included in this analysis had a stroke unit. Another strength is that interrupted time series methods were used, with seasonality considered and time-varying confounders included. Interrupted time series methods are being increasingly used and are considered a robust tool for assessing changes resulting from health interventions [17,18].
Owing to the COVID-19 pandemic, clinicians working in hospitals that participate in the AuSCR have reported that one in 10 had their bed numbers reduced in the stroke unit, one in four their stroke unit moved, and one in three stroke units had their staff redeployed to other duties [6]. This may explain why fewer patients accessed stroke units during the pandemic periods examined. However, one limitation is that we do not know whether patients with stroke had COVID-19 and may have required management in a COVID-19 ward. Notably, approximately 1.5% of people with COVID-19 have been found to experience stroke [19].
Another limitation of our study is that we did not have data available on treatment and outcomes after discharge from the hospital. Therefore, we were unable to investigate if care usually provided during the hospital admission or at discharge was substituted with other health services. Whether the poorer quality of care provided during the admission was observed during the pandemic period has resulted in poorer quality of life and greater mortality will be investigated in future research.
Conclusions
Stroke is a leading cause of death [20] and disability [21], and it is essential that patients continue to be treated in stroke units, as treatment in a stroke unit reduces the number of people with poor outcomes [4,5]. Our findings underscore the importance of why we need to treat all patients with stroke in specialized wards in line with national guideline recommendations, regardless of whether we are in the midst of a pandemic.
Acknowledgments
We acknowledge Prof. Helen Dewey, Prof. Mark Parsons, Ms. Jot Ghuliani, and other members of the AuSCR office team, governance committees, and data contributors to the AuSCR (see Supplementary acknowledgments).
The Australian Stroke Clinical Registry was funded from various grants obtained from Stroke Foundation, Queensland Health, Victorian government, Tasmania Government, South Australian government. The following authors received Research Fellowship support from the National Health and Medical Research Council: Dominique A. Cadilhac (1154273); and the National Heart Foundation of Australia: Natasha A. Lannin (102055).
Footnotes
Disclosure
The authors have no financial conflicts of interest.
Supplementary materials
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2021.02530.
Number of admissions per week. Mean number of admissions per week: 348.2532 (standard deviation: 45.08808).
Differences in the trends of provision of nursing and allied health interventions between stroke units and other ward settings
Differences in the trends of provision of secondary prevention medications and care plans at discharge between stroke units and other ward settings
References
- 1.McCabe R, Schmit N, Christen P, D’Aeth JC, Løchen A, Rizmie D. Adapting hospital capacity to meet changing demands during the COVID-19 pandemic. BMC Med. 2020;18:329. doi: 10.1186/s12916-020-01781-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brainin M. Stroke care and the COVID19 pandemic: words from our president. World Stroke Organization; https://www.world-stroke.org/news-and-blog/news/stroke-care-and-the-covid19-pandemic. 2020. Accessed September 22, 2021. [Google Scholar]
- 3.Coote S, Cadilhac DA, O'Brien E, Middleton S, Acute Stroke Nurses Education Network (ASNEN) Steering Committee Letter to the editor regarding: critical considerations for stroke management during COVID-19 pandemic in response to Inglis et al., Heart Lung Circ. 2020;29(9):1263-1267. Heart Lung Circ. 2020;29:1895–1896. doi: 10.1016/j.hlc.2020.09.925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stroke Unit Trialists’ Collaboration Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev. 2013;2013:CD000197. doi: 10.1002/14651858.CD000197.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cadilhac DA, Andrew NE, Lannin NA, Middleton S, Levi CR, Dewey HM, et al. Quality of acute care and long-term quality of life and survival: the Australian Stroke Clinical Registry. Stroke. 2017;48:1026–1032. doi: 10.1161/STROKEAHA.116.015714. [DOI] [PubMed] [Google Scholar]
- 6.Cadilhac DA, Kim J, Tod EK, Morrison JL, Breen SJ, Jaques K, et al. COVID-19 pandemic impact on care for stroke in Australia: emerging evidence from the Australian Stroke Clinical Registry. Front Neurol. 2021;12:621495. doi: 10.3389/fneur.2021.621495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cadilhac DA, Lannin NA, Anderson CS, Levi CR, Faux S, Price C, et al. Protocol and pilot data for establishing the Australian Stroke Clinical Registry. Int J Stroke. 2010;5:217–226. doi: 10.1111/j.1747-4949.2010.00430.x. [DOI] [PubMed] [Google Scholar]
- 8.Tu JV, Willison DJ, Silver FL, Fang J, Richards JA, Laupacis A, et al. Impracticability of informed consent in the Registry of the Canadian Stroke Network. N Engl J Med. 2004;350:1414–1421. doi: 10.1056/NEJMsa031697. [DOI] [PubMed] [Google Scholar]
- 9.Linden A, Arbor A. Conducting interrupted time-series analysis for single- and multiple-group comparisons. Stata J. 2015;15:480–500. [Google Scholar]
- 10.Markus HS, Brainin M. COVID-19 and stroke: a global World Stroke Organization perspective. Int J Stroke. 2020;15:361–364. doi: 10.1177/1747493020923472. [DOI] [PubMed] [Google Scholar]
- 11.Chen CH, Liu CH, Chi NF, Sung PS, Hsieh CY, Lee M, et al. Maintenance of stroke care quality amid the coronavirus disease 2019 outbreak in Taiwan. J Stroke. 2020;22:407–411. doi: 10.5853/jos.2020.02292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Desai SM, Guyette FX, Martin-Gill C, Jadhav AP. Collateral damage: impact of a pandemic on stroke emergency services. J Stroke Cerebrovasc Dis. 2020;29:104988. doi: 10.1016/j.jstrokecerebrovasdis.2020.104988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoyer C, Ebert A, Huttner HB, Puetz V, Kallmünzer B, Barlinn K, et al. Acute stroke in times of the COVID-19 pandemic: a multicenter study. Stroke. 2020;51:2224–2227. doi: 10.1161/STROKEAHA.120.030395. [DOI] [PubMed] [Google Scholar]
- 14.Rudilosso S, Laredo C, Vera V, Vargas M, Renú A, Llull L, et al. Acute stroke care is at risk in the era of COVID-19: experience at a comprehensive stroke center in Barcelona. Stroke. 2020;51:1991–1995. doi: 10.1161/STROKEAHA.120.030329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cadilhac DA, Ibrahim J, Pearce DC, Ogden KJ, McNeill J, Davis SM, et al. Multicenter comparison of processes of care between stroke units and conventional care wards in Australia. Stroke. 2004;35:1035–1040. doi: 10.1161/01.STR.0000125709.17337.5d. [DOI] [PubMed] [Google Scholar]
- 16.Stroke Foundation . National Stroke Audit Acute Services Report 2019. Melbourne: Stroke Foundation; 2019. [Google Scholar]
- 17.Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46:348–355. doi: 10.1093/ije/dyw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schaffer AL, Dobbins TA, Pearson SA. Interrupted time series analysis using autoregressive integrated moving average (ARIMA) models: a guide for evaluating large-scale health interventions. BMC Med Res Methodol. 2021;21:58. doi: 10.1186/s12874-021-01235-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Merkler AE, Parikh NS, Mir S, Gupta A, Kamel H, Lin E, et al. Risk of ischemic stroke in patients with coronavirus disease 2019 (COVID-19) vs patients with influenza. JAMA Neurol. 2020;77:1–7. doi: 10.1001/jamaneurol.2020.2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stroke Foundation . Clinical Guidelines for Stroke Management. Stroke Foundation; 2017. https://informme.org.au/en/Guidelines/Clinical-Guidelines-for-Stroke-Management. Assessed October 12, 2021. [Google Scholar]
- 21.Krishnamurthi RV, Ikeda T, Feigin VL. Global, regional and country-specific burden of ischaemic stroke, intracerebral haemorrhage and subarachnoid haemorrhage: a systematic analysis of the global burden of disease study 2017. Neuroepidemiology. 2020;54:171–179. doi: 10.1159/000506396. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Number of admissions per week. Mean number of admissions per week: 348.2532 (standard deviation: 45.08808).
Differences in the trends of provision of nursing and allied health interventions between stroke units and other ward settings
Differences in the trends of provision of secondary prevention medications and care plans at discharge between stroke units and other ward settings


