Abstract
A 13-year-old boy, with a history of intermittent headache and transient diplopia, was found to have non-hemorrhagic cerebral arteriovenous malformation in the midbrain tegmental region associated with hydrocephalus. Gamma knife radiosurgery was performed at 16 Gy with 75% marginal dose. Posttreatment course was uneventful. Follow-up MR imaging at one year after the treatment revealed complete disappearance of the abnormal vascular flow voids. The size of each ventricle at the treatment and at one year after treatment were as follows; 60.2 cc and 20.9 cc in the lateral ventricles, 3.7 cc and 2.7 cc in the third ventricle. The hydrocephalus might be caused by obstructive mechanism but mostly by high venous pressure due to the shunt blood flow. The goal of treatment for hydrocephalus should be nidus obstruction and normalizing the vascular flow.
Keywords: Cerebral arteriovenous malformation, Hydrocephalus, Radiosurgery, Non- hemorrhage
Introduction
Hydrocephalus is commonly associated with cerebral arteriovenous malformation after the onset of subarachnoid hemorrhage, but it is rarely occurred in non- hemorrhagic case [1]. The mechanism of hydrocephalus is that dilated nidus or draining veins physically obstruct the circulation path of cerebrospinal fluid [2], and/or that an increase in venous perfusion pressure due to shunt blood flow causes cerebrospinal fluid absorption disorders [3]. Case reports such as ventricular peritoneal shunting [4,5] and third ventriculostomy [6], [7], [8] have been found to be effective. We report a case of cerebral arteriovenous malformation with hydrocephalus found only with a slight headache, in which gamma knife treatment for the nidus improved the ventricular enlargement.
Case presentation
A 13-year-old boy, who was naturally healthy, was found to be difficult to see both sides of his visual field during exercise for about 10 minutes. After that, he felt a mild intermittent headache, so when he visited a nearby doctor on the same day and MR images demonstrated a vascular malformation. He was admitted to a core hospital for scrutiny and had the following imaging findings. In MR imaging, a 15 mm-seized nidus was found on the dorsal side of left midbrain, and dilated draining veins were flowing from the Galen vein to the straight sinus (Fig. 1). No evidence of bleeding was found in the brain parenchyma. Angiographically, the feeding arteries were coming from the left posterior cerebral artery, the left upper cerebral artery, and the transmesencephalic artery, and the outflow vein was via the internal cerebral vein (Fig. 2). He was introduced to our hospital for the purpose of treating by gamma knife radiosurgery. After hearing a second opinion regarding the possibility of endovascular treatment and other radiotherapy, he finally requested treatment with gamma knife treatment alone. The marginal dose was prescribed at 15 Gy (75%), considering that the nidus was diffused type and located in the brain stem. A few days after the treatment, he complained to be difficult to focus, but no obvious diplopia was noted. He had MRI studies every three months after the treatment. The flow void of draining vein tended to shrink in six months. The nidus and the draining vein flow void disappeared in 15 months after the treatment (Fig. 3). In FLAIR images, slightly high signal area around the nidus was found but it was asymptomatic.
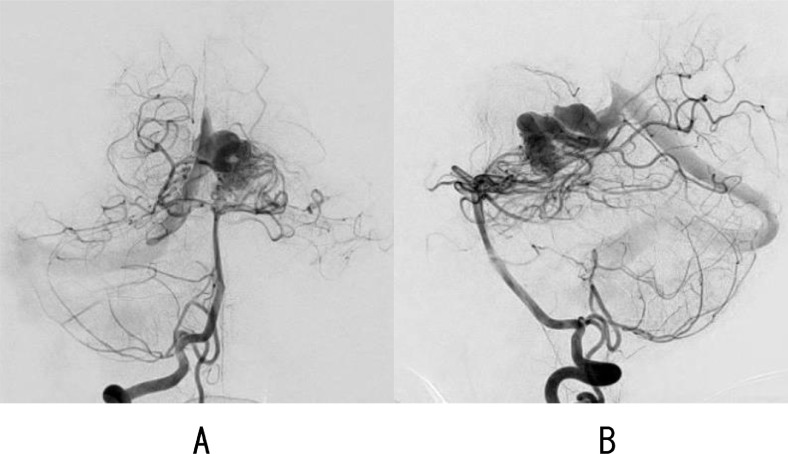
Fig. 1.
Anteroposterior (A) and lateral (B) angiograms showing nidus locating perimesencephalic region with tortious internal cerebral vein which is finally draining to the vein of Galen.
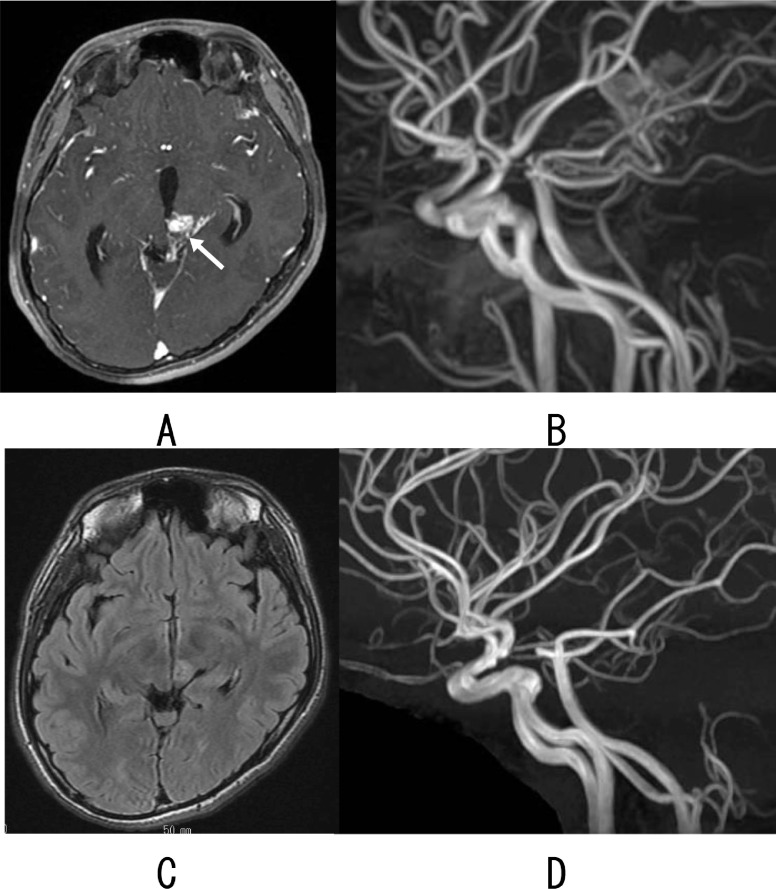
Fig. 2.
Axial fast spoiled gradient echo image with gadolinium showing nidus on the dorsal side of left midbrain (arrow) (A) and MR angiogram showing the nidus (B). One year after the treatment, FLAIR image showing slightly high signal area but no flow void (C) and MR angiogram showing disappearance of the nidus (D).
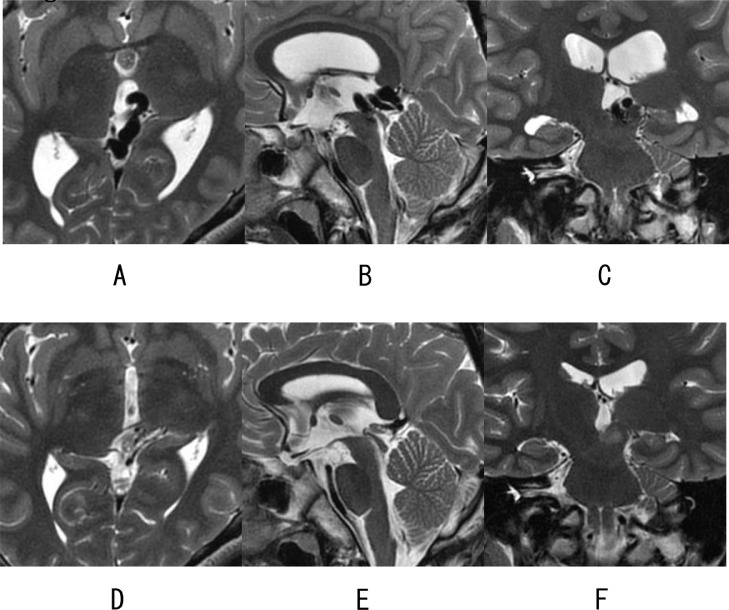
Fig. 3.
T2 weighted MR images at the treatment (A)(B)(C) and one year after the treatment (D)(E)(F) demonstrating disappearance of the flow void of draining vein and significant reduction in size of both lateral ventricles and the third ventricle.
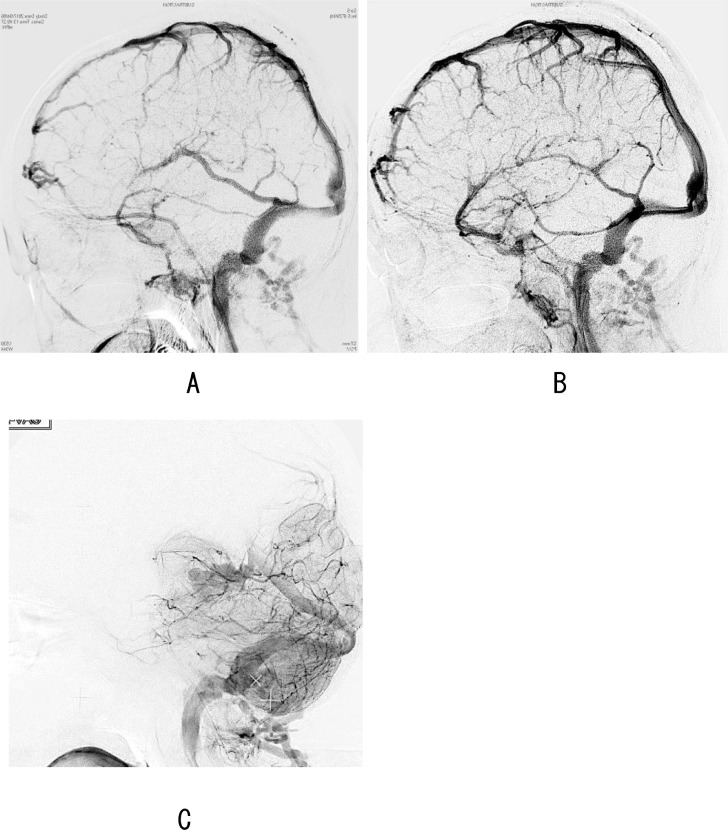
Ventricular size change was as follows: the volume of the lateral ventricle at the time of treatment was 60.2 cc, but the volume decreased over time to 20.9 cc one year after the treatment. The third ventricle also decreased from 3.7 cc to 2.7 cc, but the fourth ventricle did not decrease from 0.7 cc to 1.1 cc. Retrospectively, the blood flow from both internal carotid artery before the treatment perfused only the cortical veins, flowing into the superior sagittal sinus. The venous flow into the internal cerebral vein and the straight sinus was not observed (Fig. 4). This angiographical observation likely indicated abnormally high venous pressure in the deep venous systems.
Fig. 4.
The venous phase of the right internal carotid artery imaging (A), and the left internal carotid artery imaging (B) demonstrating perfusion of the cerebral surface veins flowing through the superior sagittal sinus to the jugular vein. In both images, the venous flow from the internal cerebral vein to the straight sinus was not observed. The venous phase of the right vertebral artery imaging (C) demonstrated that the nidus-mediated shunt flow observed in Fig. 1 flows directly from the internal cerebral vein to the straight sinus.
Discussion
Nidus location
It is rare for non-hemorrhagic cerebral arteriovenous malformation to be associated with hydrocephalus. Most of the reports in the literature are single or a few case reports. The only study regarding the frequency, 8 (1.8%) of 440 non-hemorrhagic cerebral arteriovenous malformations in a single institution have been found to be associated with hydrocephalus [1]. In 2007, Mindea et al. [2] reported a case of obstructive hydrocephalus with a 3 cm-sized non-hemorrhagic nidus in the parietooccipital lobe, in which a dilated draining vein located in the quadrigeminal cistern mechanically obstructed the cerebral aqueduct. There have been reports of hydrocephalus due to the obstruction of the cerebrospinal fluid circulation by a similar dilated draining vein. The nidus site is mostly in the posterior fossa or tegmentum area and there are few pediatric cases [1,5]. The fact that there are many adult onsets despite its congenital etiology suggests it takes time to become symptomatic. Our case was found at age 13 before the symptoms of hydrocephalus became apparent and may become symptomatic in the future if treatment for cerebral arteriovenous malformation was not given.
Treatment choice for hydrocephalus
Ventricle-peritoneal shunt or third ventriculostomy is often selected for the treatment of hydrocephalus. There have been reports that ventricular size and clinical symptoms improved soon after placement of the ventricular peritoneal shunt [4,5], but in the case reported by Mineda et al. [2] the enlarged ventricle shrank even after two weeks of external drainage. In that case, the ventricular peritoneal shunt was finally placed and hydrocephalus improved after three weeks. Furthermore, cases have been reported in which shunt dysfunction was repeated after placement and finally third ventriculostomy was performed [9]. In recent years, the third ventriculostomy seems to be preferred [[6], [7], [8],10]. Regarding this point, Geibprasert et al. [1] revealed that 5 out of 6 cases treated with shunt had troubles such as no improvement of symptoms or shunt dysfunction. They pointed out that the cause was that nidus was not obstructed and the high venous pressure due to draining vein has not been normalized and concluded that hydrocephalus cannot be cured only by improving the cerebrospinal fluid circulation with a shunt [1]. In their series, embolization only or embolization followed by gamma knife treatment ultimately improved hydrocephalus. In our case, ventricular enlargement was observed but it was not symptomatic, so shunt surgery was not indicated. This is the first report that hydrocephalus has improved only with gamma knife treatment.
Mechanisms of ventricle enlargement
Many case reports attribute the pathogenesis of hydrocephalus to obstruction of the cerebrospinal fluid circulation [2,[4], [5], [6],9]. On the other hand, Ebinu et al. [3] have reported a case of hydrocephalus in which the cerebral aqueduct was patency and periventricular vein and transmedullary vein were dilated on MRI. Embolization rapidly improved the symptoms and imaging findings of hydrocephalus. Embolization of the nidus was thought to normalize the venous pressure around the ventricles including intraventricular capillaries and intraparenchymal capillaries.
In recent years, regarding the intracranial cerebrospinal fluid circulation, not only the absorption pathway from the classical arachnoid granules but also the absorption pathway from the brain parenchyma has been studied. The mechanism of ventricular enlargement by cerebral arteriovenous malformation is not necessary always an obstructive mechanism [11]. The cerebrospinal fluid absorption system into the blood vessels may be necessary to be improved in some cases. In other vascular disorders, basilar artery aneurysms and venous malformations have been reported to have obstructive hydrocephalus [1,12,13], but in case of cerebral arteriovenous malformation, a more complex mechanism of both physical occlusion and absorption disorder is possibly involved. When managing non-hemorrhagic cerebral arteriovenous malformation, observation is also considered in consideration of the risk of treatment complications, but for cerebral arteriovenous malformation near the cerebral aqueduct, it is important to observe also the progress of the increase in ventricular size. If the ventricles expand progressively, it is recommended to actively consider treatment for cerebral arteriovenous malformation, even if it is non-hemorrhagic.
Conclusion
Hydrocephalus was cured by obstructing nidus with gamma knife treatment alone for non-hemorrhagic cerebral arteriovenous malformation. Mechanism of hydrocephalus is thought to be mainly increased venous pressure. The treatment goal for hydrocephalus should be normalizing the blood flow by nidus obstruction.
Patient consent
Consent was obtained by all participants in this study.
References
- 1.Geibprasert S, Pereira V, Krings T, Jiarakongmun P, Lasjaunias P, Pongpech S. Hydrocephalus in unruptured brain arteriovenous malformations: pathomechanical considerations, therapeutic implications, and clinical course. J Neurosurg. 2009;110:500–507. doi: 10.3171/2008.7.JNS0815. [DOI] [PubMed] [Google Scholar]
- 2.Mindea SA, Yang BP, Batjer HH. Unruptured arteriovenous malformation in a patient presenting with obstructive hydrocephalus. Case report and review of the literature. Neurosurg Focus. 2007;22:E11. doi: 10.3171/foc.2007.22.4.13. [DOI] [PubMed] [Google Scholar]
- 3.Ebinu JO, Matouk CC, Wallace MC, Terbrugge KG, Krings T. Hydrocephalus secondary to hydrodynamic disequilibrium in an adult patient with a choroidal-type arteriovenous malformation. Interv Neuroradiol. 2011;17:212–216. doi: 10.1177/159101991101700212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bayri Y, Sakar M, Ozen A, Ziyal MI. Drainage vein induced hydrocephalus caused by an unruptured arteriovenous malformation in an adult presenting with visual loss. Turk Neurosurg. 2017;27:151–154. doi: 10.5137/1019-5149.JTN.12015-14.1. [DOI] [PubMed] [Google Scholar]
- 5.Diren F, Sencer S, Hakan T. Case report of an obstructive hydrocephalus caused by an unruptured mesencephalic arteriovenous malformation in a boy and a review of literature. Open Neuroimag J. 2018;12:10–15. doi: 10.2174/1874440001812010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ono K, Oishi H, Suga Y, Yamamoto M, Nonaka S, Nakajima M, et al. Case report of cerebellar vermis arteriovenous malformation presenting with hydrocephalus due to aqueductal stenosis. No Shinkei Geka. 2015;43:843–848. doi: 10.11477/mf.1436203131. [DOI] [PubMed] [Google Scholar]
- 7.Rodríguez Rodríguez R, Molet Teixido J. Letter to the editor of acta neurochirurgica: obstructive hydrocephalus caused by unruptured arteriovenous malformation treated with endoscopic third ventriculostomy. Acta Neurochir (Wien) 2013;155:901–902. doi: 10.1007/s00701-013-1673-5. [DOI] [PubMed] [Google Scholar]
- 8.Tucker A, Tamura Y, Hanabusa K, Miyake H, Tsuji M, Ukita T, et al. Endoscopic third ventriculostomy for hydrocephalus due to unruptured pineal AVM: case report and review of the literature. J Neurol Surg A Cent Eur Neurosurg. 2013;74(Suppl 1):e45–e49. doi: 10.1055/s-0032-1330120. [DOI] [PubMed] [Google Scholar]
- 9.Champeaux C, Botella C, Lefevre E, Devaux B. Obstructive hydrocephalus caused by an unruptured arteriovenous malformation successfully treated by endoscopic third ventriculostomy after shunt dysfunction. Turk Neurosurg. 2018;28:500. doi: 10.5137/1019-5149.JTN.19435-16.2. [DOI] [PubMed] [Google Scholar]
- 10.Rezaee O, Sharifi G, Samadian M, Haddadian K, Ali-Asgari A, Yazdani M. Endoscopic third ventriculostomy for treatment of obstructive hydrocephalus. Arch Iran Med. 2007;10:498–503. [PubMed] [Google Scholar]
- 11.Rossitti S. Pathophysiology of increased cerebrospinal fluid pressure associated to brain arteriovenous malformations: the hydraulic hypothesis. Surg Neurol Int. 2013;4:42. doi: 10.4103/2152-7806.109657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arantes M, Romão H, Resende M, Costa M, Garcia R, Resende-Pereira J. Hydrocephalus caused by a venous varix. Rev Neurol (Paris) 2010;166:104–107. doi: 10.1016/j.neurol.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 13.Sato S, Sonoda Y, Kuroki R, Kayama T. A rare case of aqueductal stenosis due to venous angioma. No To Shinkei. 2004;56:1042–1046. [PubMed] [Google Scholar]