Abstract
Objective: To investigate the improvement effect of evidence-based nursing intervention on treatment compliance, quality of life and self-efficacy of patients with lung carcinoma (LC) undergoing radiotherapy and chemotherapy. Methods: From May 2018 to August 2019, 183 patients with LC who received radiotherapy and chemotherapy in our hospital were selected and divided into two groups in accordance with different nursing methods. Among them, 85 patients who received routine nursing intervention were included in the control group (CG), and 98 patients who received evidence-based nursing intervention were included in the research group (RG). The improvement of pulmonary function indexes [(FVC), forced expiratory volume in one second (FEV1), ratio of forced expiratory volume in one second to forced vital capacity (FEV1/FVC)] was observed before and after nursing. The pain degree was evaluated by the visual analogue scale (VAS). The treatment compliance between groups was compared. The psychological emotions of the patients were evaluated by a self-rating anxiety scale (SAS) and a self-rating depression scale (SDS). The General Self-efficacy Scale (GSES) was applied to assess the self-efficacy and the Quality of Life (SF-36) scale was applied to evaluate the quality of life. The incidence of secondary infection was observed in the two groups. The nursing satisfaction was evaluated by a nursing satisfaction questionnaire made by our hospital. Results: After nursing, the improvement of FEV1, FVC and FEV1/FVC levels in the RG were obviously better than that in the CG; The scores of VAS, SAS and SDS and total incidence of secondary infection in the RG were obviously lower than those in the CG; The treatment compliance, GSES and SF-36 scores, and nursing satisfaction scores of patients in the RG were obviously higher than that in the CG. Conclusion: Evidence-based nursing intervention can improve treatment compliance, lung function, self-efficacy and quality of life for patients with LC undergoing radiotherapy and chemotherapy.
Keywords: Evidence-based nursing, radiotherapy and chemotherapy for lung carcinoma, treatment compliance, quality of life, self-efficacy
Introduction
LC is a common malignant tumor with high morbidity and mortality, which seriously threatens the health of patients [1]. When most patients are diagnosed, their condition has deteriorated, cancer cells have metastasized and spread, and the disease stage is mostly in the middle and late stages [2]. Therefore, patients are given chemotherapy intervention in clinic. Chemotherapy intervention can not only assist surgical treatment, but also reduce the recurrence rate of postoperative diseases [3]. It can also be independently implemented to improve patients’ symptoms and prolong patients’ life to a certain extent [4]. However, most chemotherapy drugs will cause different degrees of stimulation to patients’ bodies [5], so it is necessary to give effective nursing intervention during chemotherapy.
Studies have shown that most patients will have different stress reactions when they receive chemotherapy intervention [6], as well as adverse reactions such as nausea and vomiting and decreased appetite [7]. These adverse reactions will also cause physical and mental unrest to patients, so that some patients’ compliance with the treatment is reduced, or some even give up treatment [8]. Other studies have shown that there is a correlation between the curative effect after chemotherapy and the life quality, and the quality of life will be decreased in most patients after receiving chemotherapy intervention [9]. Research even shows that most patients who receive chemotherapy for LC will have serious adverse reactions, which will reduce the curative effect of chemotherapy and cause adverse prognosis [10]. Therefore, it is particularly important to reduce the adverse reactions caused by chemotherapy and improve the quality of life [11]. However, the routine nursing has many limitations at this stage [12], such as giving intervention measures only to prevent various complications, or focusing on diseases and ignoring the needs of patients themselves, thus patients’ negative emotions cannot be fully and effectively alleviated [13]. Evidence-based nursing is a kind of targeted nursing for individuals, which can help patients grasp their progress, the course of treatment, strengthen patients’ understanding of diseases, and give targeted psychological guidance to patients, so that patients can face treatment with a positive attitude and improve therapeutic effect [14,15]. It can also be designed to provide educational guidance to family members, so that the family members of the patients can correctly understand the nursing intervention methods, and the patients can have higher quality nursing intervention after discharge [16]. For example, studies by XX et al. have shown that effective nursing intervention can lessen the decline of patients’ body function, reduce the unhealthy emotions during chemotherapy and improve the therapeutic effect for patients with neurotoxic chemotherapy [17].
In this study, evidence-based nursing intervention was given to patients with LC who received chemotherapy intervention to explore the improvement effect of this model on treatment compliance, self-efficacy after intervention and quality of life of patients, aiming to provide a feasible nursing plan for patients with LC during chemotherapy.
Materials and methods
Baseline data
From May 2018 to August 2019, 183 patients with LC who received radiotherapy and chemotherapy in Tangshan Central Hospital were selected and divided into two groups in accordance with different nursing methods. Among them, 85 patients who received routine nursing intervention were included in the CG, and 98 patients who received evidence-based nursing intervention were included in the RG.
Inclusion criteria: In both groups, patients were diagnosed with LC by pathological examination [18], and they were treated with radiotherapy and chemotherapy in our hospital. Their general data were complete in the two groups, and the predicted survival time was > 6 months. The patients had clear thinking and could communicate with medical staff normally. The study plan was submitted to the hospital ethical committee for review. The research subjects and their families were informed and signed a completely informed consent form.
Exclusion criteria were as follows: Communication barriers; Comorbid with autoimmune diseases or hematological diseases; Contraindications of radiotherapy and chemotherapy drugs; Those who quit the experiment halfway; Those who were not interviewed.
Nursing methods
In the CG, patients received routine nursing: After admission, the patients were given basic health and disease education, and the changes of vital signs were closely observed. According to the doctor’s orders, the medical staff provided various drugs, guided the patients to pay attention to the matters needing attention when taking drugs, and informed them about adverse reactions after radiotherapy and chemotherapy or the corresponding treatment measures of adverse reactions after medication, so as to relieve the patients’ worries. The patients were also told to stay in bed more often.
In the RG, patients received evidence-based nursing: 1. Disease explanation: Before radiotherapy and chemotherapy, patients were informed of the related medication and use methods, so that patients could understand the frequency of medication. While explaining the significance of chemotherapy and radiotherapy to patients, the medical staff listened patiently to their suggestions and feedback, and actively provided patients with effective information about their illness and chemo-radiotherapy, so as to make patients felt respected and cared for psychologically. In addition, the medical staff actively informed patients of adverse reactions that may develop in the process of chemo-radiotherapy, so that patients could be psychologically prepared and knew the importance of persistence, so as to fully cooperate with the work of nursing staff. 2. Psychological guidance: Patients were generally seriously ill, so patients were prone to various unhealthy emotions. Therefore, nursing staff actively adjusted patients’ unhealthy emotions and mobilized their families to provide comfort and support for patients. When the patient was in a low mood, it was necessary to actively communicate with the patient to help the patient eliminate the negative feelings of treatment and enhance their confidence in treatment. 3. Dietary intervention: Radiotherapy and chemotherapy can lead to the decrease of gastrointestinal reaction and appetite of patients, which can result in lower nutrition intake and affect their physical skills and therapeutic effect. According to the patients’ eating habits, the medical staff gave corresponding dietary guidance and told the patients to eat more foods high in protein, with fruit and other healthy foods. 4. Pain intervention: During radiotherapy and chemotherapy, pain can affect treatment compliance and increase negative emotions. According to their personality and hobbies, they were provided with recreational activities to divert their attention and relieve pain. If necessary, they were given appropriate painkillers. 5. Adverse reaction intervention: Medical staff monitored the patient’s condition changes or adverse reaction symptoms in real time, and timely reported them to the doctor, making the corresponding treatment, and doing a good job of appeasement.
Outcome measures
Lung function indicators
Before and after treatment, the forced vital capacity (FVC), forced expiratory volume in one second (FEV1), and the ratio of forced expiratory volume in one second to forced vital capacity (FEV1/FVC) in the two groups were measured with a lung function instrument (Zeao Medical Technology Co., Ltd., Beijing, China, z00502).
VAS score [19]
There were 10 points in the scale: 0 meant painless, 1-3 meant slight pain, 4-6 meant medium pain, and 7-10 meant serious pain.
Compliance
This was divided into three parts: very compliant, compliance and non-compliance. Patients who highly cooperated with nursing staff and finished treatment on time were very compliant; Patients who cooperated with nursing staff were compliant; Patients who did not fully cooperate with nursing staff and evaded treatment were incompliant. Total compliance rate = (partial compliance + full compliance)/total cases ×100%.
Negative emotion [20]
The total score of SAS scale was 100 points. After nursing intervention, patients’ score of 50-70 indicated mild anxiety, patients’ score of 71-90 indicated moderate anxiety, and patients’ score of > 90 indicated severe anxiety. The higher the score, the more severe the anxiety. The total score of SDS scale was 100 points. After nursing intervention, a patients’ score of 50-70 indicated mild depression, a patients’ score of 71-90 indicated moderate depression, and a patients’ score of > 90 indicated severe depression. The higher the score, the more serious the depression.
GSES score [21]
There were 10 items in the scale, and each item scored 1-4 points, with a total score of 40 points. The higher the score, the higher the patient’s self-efficacy.
SF-36 score [22]
There were 8 items in the scale (general health, social function, physical function, emotional function, physiological role, physical pain, mental health, vitality). The percentile scoring system was used. The higher the score, the higher the quality of life.
Incidence of secondary infection
The incidence of secondary infection such as upper respiratory tract infection, lower respiratory tract infection, gastrointestinal tract infection and urinary tract infection was observed. In patients with more than two sites of infection, only the first infection was recorded without repeated counting.
Nursing satisfaction
A self-made Satisfaction Questionnaire was used for scoring, which consisted of five items, namely, service timeliness, management normalization, service attitude, hospitalization environment and comprehensive quality of nursing staff. The higher the score, the higher the patient’s satisfaction with service.
Statistical methods
SPSS 22.0 (Beijing Baiao Yijie Technology Co., Ltd., China) was applied for statistical analysis. Graphpad 6 software package was used for data analysis and image illustration. The count data within the group were represented by the number of cases/percentage [n (%)]. Chi-squared test was applied for comparison of counting data between groups. When the theoretical frequency in Chi-square test was less than 5, the continuous correction chi-squared test was used. The quantitative data were expressed by mean number ± standard deviation (mean ± SD). The quantitative data between groups were compared by t test of independent samples. Paired t test was applied for comparison in the group before and after nursing. The difference was statistically significant with P < 0.05.
Results
Baseline data
There was no obvious difference in general clinical baseline data such as gender, average age, body mass index, smoking history, drinking history, exercise history, TNM stage, pathological differentiation degree, pathological type and disease site between the two groups (P > 0.05) (Table 1).
Table 1.
Comparison of baseline data between the two groups [n (%)] (mean ± SD)
| Categories | RG (n=98) | CG (n=85) | t/χ2 value | P value |
|---|---|---|---|---|
| Gender | 0.281 | 0.595 | ||
| Male | 58 (59.18) | 47 (55.29) | ||
| Female | 40 (40.82) | 38 (44.71) | ||
| Average age (years old) | 57.53±5.18 | 57.62±5.21 | 0.116 | 0.907 |
| BMI (kg/m2) | 22.64±2.34 | 22.34±2.37 | 0.859 | 0.391 |
| Smoking history | 0.372 | 0.541 | ||
| Yes | 54 (55.10) | 43 (50.59) | ||
| No | 44 (44.90) | 42 (49.41) | ||
| Drinking history | 0.022 | 0.882 | ||
| Yes | 61 (62.24) | 52 (61.18) | ||
| No | 37 (37.76) | 33 (38.82) | ||
| Exercise history | 0.030 | 0.861 | ||
| Yes | 52 (53.06) | 44 (51.76) | ||
| No | 46 (46.94) | 41 (48.24) | ||
| TNM staging | 0.805 | 0.369 | ||
| Stage I + II | 50 (51.02) | 49 (57.65) | ||
| Stage III | 48 (48.98) | 36 (42.35) | ||
| Degree of pathological differentiation | 0.261 | 0.609 | ||
| Well and middle differentiated | 61 (62.24) | 56 (65.88) | ||
| Poorly differentiated | 37 (37.76) | 29 (34.12) | ||
| Disease types | 1.655 | 0.647 | ||
| Low differentiated squamous cell carcinoma | 22 (22.45) | 18 (21.18) | ||
| Middle and well differentiated squamous cell carcinoma | 19 (19.39) | 20 (23.53) | ||
| Small cell lung cancer | 34 (34.69) | 23 (27.06) | ||
| Low differentiated adenocarcinoma | 23 (23.47) | 24 (28.24) | ||
| Disease site | 0.153 | 0.695 | ||
| Left lung | 56 (57.14) | 51 (60.00) | ||
| Right lung | 42 (42.86) | 34 (40.00) |
Comparison of improvement of lung function indexes between the two groups before and after nursing
There was no obvious difference in lung function indexes (FEV1, FVC and FEV1/FVC levels) between the two groups before nursing (P > 0.05). The improvement of FEV1, FVC and FEV1/FVC levels in the two groups after nursing was obviously better than that before nursing (P < 0.05), and the improvement of FEV1, FVC and FEV1/FVC levels in the RG after nursing was obviously better than that in the CG (P < 0.05) (Table 2).
Table 2.
Comparison of improvement of lung function indexes between the two groups before and after nursing (mean ± SD)
| Grouping | n | FEV1/L | FVC/L | FEV1/FVC/% | |||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| Before nursing | After nursing | Before nursing | After nursing | Before nursing | After nursing | ||
| RG | 98 | 66.43±6.08 | 80.05±7.59 | 52.05±5.18 | 68.26±6.29 | 61.28±6.13 | 73.15±7.06 |
| CG | 85 | 67.94±6.12 | 46.58±4.73 | 52.09±5.14 | 71.95±7.07 | 60.07±6.02 | 67.45±6.28 |
| t | - | 1.670 | 35.160 | 0.052 | 3.736 | 1.343 | 5.732 |
| P | - | 0.096 | < 0.001 | 0.958 | 0.001 | 0.181 | < 0.001 |
Comparison of VAS scores between the two groups before and after nursing
There was no obvious difference in VAS scores between the two groups before nursing (P > 0.05). After nursing, the VAS scores of patients in the two groups were obviously lower than that before nursing (P < 0.05), and the VAS score of patients in the RG after nursing was obviously lower than that in the CG (P < 0.05) (Table 3).
Table 3.
Comparison of VAS scores between the two groups before and after nursing (mean ± SD)
| Grouping | n | VAS score | |
|---|---|---|---|
|
| |||
| Before nursing | After nursing | ||
| RG | 98 | 7.05±0.24 | 2.15±0.11 |
| CG | 85 | 7.01±0.26 | 5.31±0.14 |
| T | - | 1.082 | 170.800 |
| P | - | 0.280 | < 0.001 |
Comparison of treatment compliance between the two groups after nursing
The treatment compliance was compared after nursing in both groups. The total compliance rate of patients in the RG was 96.94%, while that in the CG was 78.82%. The results revealed that the treatment compliance of patients in the RG was obviously higher than that in the CG after nursing (P < 0.05) (Table 4).
Table 4.
Comparison of treatment compliance between the two groups after nursing [n (%)]
| Grouping | Number of cases | Very compliance | Compliance | Non compliance | Compliance rate (%) |
|---|---|---|---|---|---|
| RG | 98 | 75 (76.53) | 22 (22.45) | 3 (3.06) | 95 (96.94) |
| CG | 85 | 29 (34.12) | 38 (44.71) | 18 (21.18) | 67 (78.82) |
| χ2 | - | - | - | - | 14.701 |
| P | - | - | - | - | < 0.001 |
Comparison of psychological emotions between the two groups before and after nursing
There was no obvious difference in scores of SAS and SDS in both groups before nursing (P > 0.05). After nursing, the scores of SAS and SDS in both groups were obviously lower than those before nursing (P < 0.05). After nursing, the scores of SAS and SDS in the RG were obviously lower than those in the CG (P < 0.05) (Figure 1).
Figure 1.
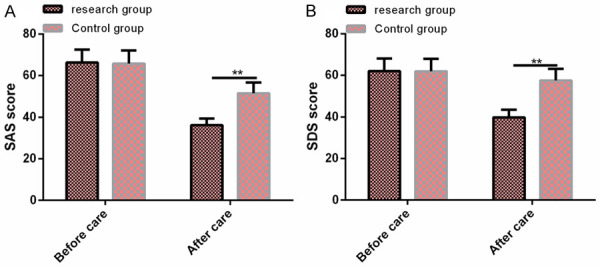
Comparison of psychological emotion between the two groups before and after nursing. A: There was no significant difference in SAS between the two groups before nursing. After nursing, the SAS scores in the RG were significantly lower than those in the CG. B: There was no significant difference in SDS between the two groups before nursing. After nursing, the SDS scores in the RG were significantly lower than those in the CG. Note: Compared with before treatment, * < 0.05; Compared with the two groups after treatment, ** < 0.01.
Comparison of GSES scores between the two groups before and after nursing
There was no obvious difference in GSES scores in both groups before nursing (P > 0.05). After nursing, GSES scores of patients in both groups were significantly higher than those before nursing (P < 0.05). After nursing, the GSES scores in the RG were obviously higher than those in the CG (P < 0.05) (Figure 2).
Figure 2.
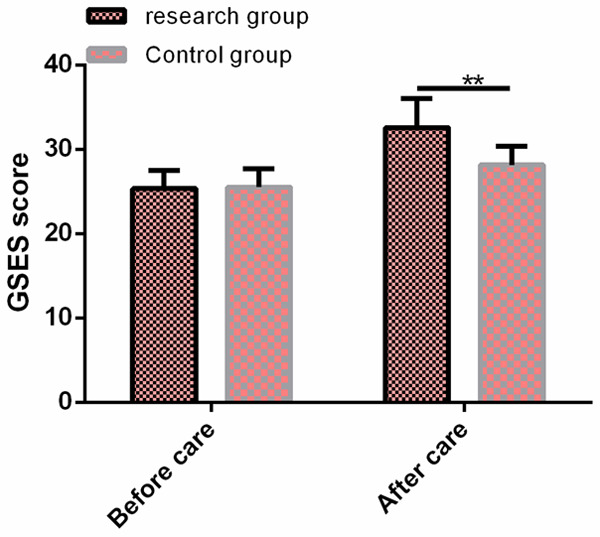
Comparison of GSES scores between the two groups before and after nursing. There was no significant difference in GSES between the two groups before nursing. After nursing, the GSES scores in the RG were significantly higher than those in the CG. Note: Compared with before treatment, * < 0.05; Compared with the two groups after treatment, ** < 0.01.
Comparison of SF-36 scores between the two groups after nursing
After nursing, the SF-36 scores (overall health, social function, physical function, emotional function, physiological role, physical pain, mental health and vitality) in the RG were significantly higher than those in the CG (P < 0.05) (Table 5).
Table 5.
Comparison of SF-36 scores between the two groups after nursing (mean ± SD)
| Grouping | Number of cases | Overall health | Social function | Physical function | Emotional function | Physiological role | Physical pain | Mental health | Vitality score |
|---|---|---|---|---|---|---|---|---|---|
| RG | 98 | 89.41±8.15 | 84.24±8.06 | 88.46±8.14 | 82.46±8.15 | 84.19±8.13 | 85.46±8.25 | 90.34±9.01 | 91.58±9.05 |
| CG | 85 | 74.19±7.29 | 66.11±6.41 | 71.57±7.22 | 73.14±7.17 | 62.78±6.28 | 77.51±7.31 | 66.49±6.73 | 72.49±7.34 |
| t | - | 13.230 | 16.660 | 14.750 | 8.155 | 19.710 | 6.852 | 20.030 | 15.520 |
| P | - | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
Comparison of incidence of secondary infection between the two groups after nursing
After nursing, the total incidence of secondary infection was 6.12% in the RG and 25.88% in the CG, and the results revealed that the total incidence of secondary infection in the RG was obviously lower than that in the CG (P < 0.05) (Table 6).
Table 6.
Comparison of incidence of secondary infection between the two groups after nursing [n (%)]
| Categories | RG (n=98) | CG (n=85) | χ2 value | P value |
|---|---|---|---|---|
| Upper respiratory tract infection | 3 (3.06) | 8 (9.41) | 3.249 | 0.071 |
| Lower respiratory tract infection | 2 (2.04) | 5 (5.88) | 1.826 | 0.176 |
| Gastrointestinal infection | 0 (0.00) | 3 (3.53) | 3.516 | 0.060 |
| Urinary system infection | 1 (1.02) | 6 (7.06) | 4.512 | 0.033 |
| Overall incidence | 6 (6.12) | 22 (25.88) | 13.711 | 0.001 |
Comparison of nursing satisfaction between the two groups after nursing
The scores of nursing satisfaction (nursing quality, nursing effect, nursing procedure and nursing service) in the RG were significantly higher than that in the CG (P < 0.05) (Table 7).
Table 7.
Comparison of nursing satisfaction between the two groups after nursing (mean ± SD)
| Grouping | n | Service timeliness | Management normalization | Service attitude | Hospitalization environment | Comprehensive quality of nursing staff |
|---|---|---|---|---|---|---|
| RG | 98 | 25.81±2.19 | 24.51±2.41 | 13.98±1.16 | 14.64±1.05 | 11.08±1.02 |
| CG | 85 | 20.25±2.08 | 19.25±2.07 | 10.14±1.03 | 11.27±1.01 | 7.56±0.57 |
| t | - | 17.530 | 15.710 | 23.520 | 22.040 | 28.220 |
| P | - | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
Discussion
LC is a common malignant tumor of the respiratory system that is seen in the clinic. Because of its nonspecific clinical manifestations, most patients are in the middle and late stages at the time of diagnosis [23]. The clinical symptoms of these patients are often accompanied by chest pain, low fever, cough and other symptoms, and the mortality rate is high [24]. Surgical treatment, radioactive therapy, chemotherapy and other interventions are often used in clinic [25]. Although chemotherapy can alleviate the clinical symptoms of patients to a certain extent, the side effects of chemotherapy are relatively serious [26]. Due to the disease progression, most patients will have tremendous psychological pressure, thus affecting the prognosis of patients [27]. Therefore, it is particularly important to provide effective nursing services in clinic during chemotherapy and improve the prognosis and recovery of patients.
In this study, evidence-based nursing was used to intervene in treatment compliance, self-efficacy improvement, adverse reaction of chemotherapy and life quality of patients with LC undergoing chemotherapy. It was found that the patients’ health was significantly improved after nursing intervention. For example, research has revealed that nursing intervention can effectively ameliorate the dyspnea for LC patients with dyspnea, thus improving the blood gas exchange in the lungs and arteries [28]. The findings of this research showed that the improvement of FEV1, FVC and FEV1/FVC levels in the RG after nursing was significantly better than that in the CG, which indicated that the intervention of evidence-based nursing could promote the curative treatment effect more effectively, thus improving the pulmonary function of patients. Studies have shown that cancer patients often suffer from uncontrolled pain, which has a negative impact on patients’ life and treatment, and leads to negative physical and mental conditions. Due to the lack of conventional nursing intervention methods, the prognosis of patients is aggravated [29]. However, this study revealed that the VAS scores in the RG after evidence-based nursing intervention were significantly lower than those in the CG. This is because evidence-based nursing is designed to use visual and auditory dispersion during chemotherapy to help patients relieve chemotherapy pain. This is similar to studies by XX. Effective nursing intervention can reduce pain and anxiety for patients receiving chemotherapy in chemotherapy center [30]. Studies have shown that most patients receiving chemotherapy are affected to different degrees in terms of treatment compliance due to various adverse conditions or the emergence of adverse emotions [31]. For example, research by xx have shown that the different intervention strategies will affect the dialysis compliance of dialysis patients with end-stage renal disease, and the nursing intervention can effectively improve their dialysis compliance [32]. This is similar to the findings of this research, which shows that effective nursing guidance can ameliorate patients’ treatment compliance. The findings of this research revealed that the treatment compliance of patients in the RG after nursing was obviously higher than that in the CG. This is also because evidence-based nursing is designed to provide professional help to patients in various aspects through health guidance, thus improving patients’ confidence in chemotherapy treatment and treatment compliance.
Patients suffering from LC must receive surgery, radiotherapy and chemotherapy, targeted therapy or other treatments, which may lead to deformity, physical dysfunction and a series of side effects, resulting in a series of psychological barriers such as anxiety and depression [33]. The findings of this study revealed that the scores of SAS and SDS in the RG were significantly lower than those in the CG after nursing, which was similar to the study by xx. The study showed that the psychological nursing intervention could effectively reduce the symptoms of anxiety and depression for cancer patients undergoing chemotherapy, thus improving their sleep quality [34]. This is also because evidence-based nursing has targeted psychological intervention for each patient in this study, thus eliminating their negative emotions, helping patients face treatment with positive attitude and improving recovery. Studies have revealed that the self-efficacy of most patients is generally low during chemotherapy, and patients with low self-efficacy will also have a negative regulatory effect on cognitive behavior [35]. Effective nursing intervention can significantly ameliorate the self-efficacy of patients [36]. This is similar to the results of this study: the GSES scores of patients in the RG were obviously higher than those in the CG after nursing, suggesting that evidence-based nursing could effectively improve self-efficacy, so that patients could cooperate with nursing intervention and accelerate the recovery of disease. Studies have shown that most patients with LC develop various adverse reactions, depression and other symptoms, which can also have a certain impact on the quality of life of patients. Therefore, effective nursing intervention can effectively ameliorate the quality of life and unhealthy emotions of patients with LC after diagnosis [37]. This is similar to the results of this study: the total incidence of secondary infection in the RG was obviously lower than that in the CG, indicating that evidence-based nursing intervention could effectively reduce the secondary infection rate of patients with LC caused by radiotherapy. The SF-36 score of quality of life in the RG was obviously higher than that in the CG after nursing, indicating that evidence-based nursing could effectively raise the curative effect, thus improving their quality of life of patients. We further compared the satisfaction of patients in the two groups after nursing, and the results revealed that the satisfaction of patients in the RG after nursing was obviously higher than that in the CG, suggesting that evidence-based nursing could help patients and it was highly recognized by patients, so this also provided a powerful reference for subsequent clinical application.
Although this study has revealed that evidence-based nursing intervention can bring better benefits to patients with LC undergoing radiotherapy and chemotherapy, there is still room for improvement in this study. For example, we can analyze the risk factors affecting the poor prognosis of patients undergoing radiotherapy and chemotherapy, which will help nurses to identify which risk factors need additional attention. In the future, we will gradually carry out supplementary research from the above perspectives.
To sum up, evidence-based nursing intervention can improve treatment compliance, lung function, self-efficacy and quality of life for patients with LC undergoing radiotherapy and chemotherapy.
Disclosure of conflict of interest
None.
References
- 1.Xin M, Qiao Z, Li J, Liu J, Song S, Zhao X, Miao P, Tang T, Wang L, Liu W, Yang X, Dai K, Huang G. miR-22 inhibits tumor growth and metastasis by targeting ATP citrate lyase: evidence in osteosarcoma, prostate cancer, cervical cancer and lung cancer. Oncotarget. 2016;7:44252–44265. doi: 10.18632/oncotarget.10020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xu W, Sun D, Wang Y, Zheng X, Li Y, Xia Y, Teng Y. Inhibitory effect of microRNA-608 on lung cancer cell proliferation, migration, and invasion by targeting BRD4 through the JAK2/STAT3 pathway. Bosn J Basic Med Sci. 2020;20:347–356. doi: 10.17305/bjbms.2019.4216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salazar MC, Rosen JE, Wang Z, Arnold BN, Thomas DC, Herbst RS, Kim AW, Detterbeck FC, Blasberg JD, Boffa DJ. Association of delayed adjuvant chemotherapy with survival after lung cancer surgery. JAMA Oncol. 2017;3:610–619. doi: 10.1001/jamaoncol.2016.5829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang YL, Peng HH, Su SY, Lin CT. Combined immunotherapy (OK-432, IL-2) with chemotherapy decrease the recurrence rate in advanced ovarian cancer. Reprod Sci. 2019;26:244–249. doi: 10.1177/1933719118768684. [DOI] [PubMed] [Google Scholar]
- 5.Seckl MJ, Ottensmeier CH, Cullen M, Schmid P, Ngai Y, Muthukumar D, Thompson J, Harden S, Middleton G, Fife KM, Crosse B, Taylor P, Nash S, Hackshaw A. Multicenter, phase III, randomized, double-blind, placebo-controlled trial of pravastatin added to first-line standard chemotherapy in small-cell lung cancer (LUNGSTAR) J. Clin. Oncol. 2017;35:1506–1514. doi: 10.1200/JCO.2016.69.7391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hsu HY, Lin TY, Hu CH, Shu DTF, Lu MK. Fucoidan upregulates TLR4/CHOP-mediated caspase-3 and PARP activation to enhance cisplatin-induced cytotoxicity in human lung cancer cells. Cancer Lett. 2018;432:112–120. doi: 10.1016/j.canlet.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 7.Wang Y, Zhang R, Shen Y, Su L, Dong B, Hao Q. Prediction of chemotherapy adverse reactions and mortality in older patients with primary lung cancer through frailty index based on routine laboratory data. Clin Interv Aging. 2019;14:1187–1197. doi: 10.2147/CIA.S201873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coolbrandt A, Wildiers H, Aertgeerts B, Dierckx de Casterle B, van Achterberg T, Milisen K. Systematic development of CHEMO-SUPPORT, a nursing intervention to support adult patients with cancer in dealing with chemotherapy-related symptoms at home. BMC Nurs. 2018;17:28. doi: 10.1186/s12912-018-0297-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Batran SE, Goetze TO, Mueller DW, Vogel A, Winkler M, Lorenzen S, Novotny A, Pauligk C, Homann N, Jungbluth T, Reissfelder C, Caca K, Retter S, Horndasch E, Gumpp J, Bolling C, Fuchs KH, Blau W, Padberg W, Pohl M, Wunsch A, Michl P, Mannes F, Schwarzbach M, Schmalenberg H, Hohaus M, Scholz C, Benckert C, Knorrenschild JR, Kanngiesser V, Zander T, Alakus H, Hofheinz RD, Roedel C, Shah MA, Sasako M, Lorenz D, Izbicki J, Bechstein WO, Lang H, Moenig SP. The RENAISSANCE (AIO-FLOT5) trial: effect of chemotherapy alone vs. chemotherapy followed by surgical resection on survival and quality of life in patients with limited-metastatic adenocarcinoma of the stomach or esophagogastric junction - a phase III trial of the German AIO/CAO-V/CAOGI. BMC Cancer. 2017;17:893. doi: 10.1186/s12885-017-3918-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.West H, McCleod M, Hussein M, Morabito A, Rittmeyer A, Conter HJ, Kopp HG, Daniel D, McCune S, Mekhail T, Zer A, Reinmuth N, Sadiq A, Sandler A, Lin W, Ochi Lohmann T, Archer V, Wang L, Kowanetz M, Cappuzzo F. Atezolizumab in combination with carboplatin plus nab-paclitaxel chemotherapy compared with chemotherapy alone as first-line treatment for metastatic non-squamous non-small-cell lung cancer (IMpower130): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20:924–937. doi: 10.1016/S1470-2045(19)30167-6. [DOI] [PubMed] [Google Scholar]
- 11.Jiang X, Hidru TH, Zhang Z, Bai Y, Kong L, Li X. Evidence of elemene injection combined radiotherapy in lung cancer treatment among patients with brain metastases: a systematic review and meta-analysis. Medicine (Baltimore) 2017;96:e6963. doi: 10.1097/MD.0000000000006963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fralick M, Gagne JJ, Patorno E, Levin R, Kesselheim AS. Using data from routine care to estimate the effectiveness and potential limitations of outcomes-based contracts for diabetes medications. Value Health. 2020;23:434–440. doi: 10.1016/j.jval.2019.11.004. [DOI] [PubMed] [Google Scholar]
- 13.Wong E, Heuschkel R, Lindsay C, Benson S, Zilbauer M. The growing gap between demand and availability of clinical psychology in paediatric gastroenterology: a retrospective analysis of clinical routine care. Eur J Pediatr. 2020;180:1307–1312. doi: 10.1007/s00431-020-03825-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.36th International Symposium on Intensive Care and Emergency Medicine: Brussels, Belgium. 15-18 March 2016. Crit Care. 2016;20:94. doi: 10.1186/s13054-016-1208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hennessy S, Cocoman AM. What is the impact of targeted health education for mental health nurses in the provision of physical health care? An integrated literature review. Issues Ment Health Nurs. 2018;39:700–706. doi: 10.1080/01612840.2018.1429509. [DOI] [PubMed] [Google Scholar]
- 16.Li L, Dai JX, Xu L, Huang ZX, Pan Q, Zhang X, Jiang MY, Chen ZH. The effect of a rehabilitation nursing intervention model on improving the comprehensive health status of patients with hand burns. Burns. 2017;43:877–885. doi: 10.1016/j.burns.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 17.Knoerl R, Weller E, Halpenny B, Berry D. Exploring the efficacy of an electronic symptom assessment and self-care intervention to preserve physical function in individuals receiving neurotoxic chemotherapy. BMC Cancer. 2018;18:1203. doi: 10.1186/s12885-018-5093-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roy-Chowdhuri S, Aisner DL, Allen TC, Beasley MB, Borczuk A, Cagle PT, Capelozzi V, Dacic S, da Cunha Santos G, Hariri LP, Kerr KM, Lantuejoul S, Mino-Kenudson M, Moreira A, Raparia K, Rekhtman N, Sholl L, Thunnissen E, Tsao MS, Vivero M, Yatabe Y. Biomarker testing in lung carcinoma cytology specimens: a perspective from members of the pulmonary pathology society. Arch Pathol Lab Med. 2016;140:1267–1272. doi: 10.5858/arpa.2016-0091-SA. [DOI] [PubMed] [Google Scholar]
- 19.Krishnan S, Hendriks HF, Hartvigsen ML, de Graaf AA. Feed-forward neural network model for hunger and satiety related VAS score prediction. Theor Biol Med Model. 2016;13:17. doi: 10.1186/s12976-016-0043-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liang Y, Chen M, Zheng X, Liu J. Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. J Psychosom Res. 2020;133:110102. doi: 10.1016/j.jpsychores.2020.110102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gu ZH, Qiu T, Tian FQ, Yang SH, Wu H. Perceived organizational support associated with depressive symptoms among petroleum workers in China: a cross-sectional study. Psychol Res Behav Manag. 2020;13:97–104. doi: 10.2147/PRBM.S232635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: scoping review. SAGE Open Med. 2016;4:2050312116671725. doi: 10.1177/2050312116671725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Romaszko A, Swietlik E, Doboszynska A, Szpruch P, Luks J. Lung cancer and multiple neoplasms: a retrospective analysis. Adv Exp Med Biol. 2016;911:53–58. doi: 10.1007/5584_2016_224. [DOI] [PubMed] [Google Scholar]
- 24.Chen L, Yu L, Wu Y, Ming WK, Huang Z, Liu S. A 52-year-old man with an 11-month history of fever, cough, chest pain, pleural effusion, and left lung atelectasis. Chest. 2020;158:e153–e157. doi: 10.1016/j.chest.2020.05.546. [DOI] [PubMed] [Google Scholar]
- 25.Dong B, Wang J, Zhu X, Chen Y, Xu Y, Shao K, Zheng L, Ying H, Chen M, Cao J. Comparison of the outcomes of stereotactic body radiotherapy versus surgical treatment for elderly (≥70) patients with early-stage non-small cell lung cancer after propensity score matching. Radiat Oncol. 2019;14:195. doi: 10.1186/s13014-019-1399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pearce A, Haas M, Viney R, Pearson SA, Haywood P, Brown C, Ward R. Incidence and severity of self-reported chemotherapy side effects in routine care: a prospective cohort study. PLoS One. 2017;12:e0184360. doi: 10.1371/journal.pone.0184360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jomar RT, Gomes RAF, Leite DC, Gomes HF, Peres EM, Junior EFP. Nursing diagnoses in adult/elderly patients undergoing outpatient antineoplastic chemotherapy: a review. Ecancermedicalscience. 2017;11:736. doi: 10.3332/ecancer.2017.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Choratas A, Papastavrou E, Charalambous A, Kouta C. Developing and assessing the effectiveness of a nurse-led home-based educational programme for managing breathlessness in lung cancer patients. A feasibility study. Front Oncol. 2020;10:1366. doi: 10.3389/fonc.2020.01366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Erol O, Unsar S, Yacan L, Pelin M, Kurt S, Erdogan B. Pain experiences of patients with advanced cancer: a qualitative descriptive study. Eur J Oncol Nurs. 2018;33:28–34. doi: 10.1016/j.ejon.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 30.Gensic ME, Smith BR, LaBarbera DM. The effects of effleurage hand massage on anxiety and pain in patients undergoing chemotherapy. JAAPA. 2017;30:36–38. doi: 10.1097/01.JAA.0000510988.21909.2e. [DOI] [PubMed] [Google Scholar]
- 31.Di Bona D, Magistà S, Masciopinto L, Lovecchio A, Loiodice R, Bilancia M, Albanesi M, Caiaffa MF, Nettis E, Macchia L AIT Study Group. Safety and treatment compliance of subcutaneous immunotherapy: a 30-year retrospective study. Respir Med. 2020;161:105843. doi: 10.1016/j.rmed.2019.105843. [DOI] [PubMed] [Google Scholar]
- 32.Wang J, Yue P, Huang J, Xie X, Ling Y, Jia L, Xiong Y, Sun F. Nursing intervention on the compliance of hemodialysis patients with end-stage renal disease: a meta-analysis. Blood Purif. 2018;45:102–109. doi: 10.1159/000484924. [DOI] [PubMed] [Google Scholar]
- 33.Yan X, Chen X, Li M, Zhang P. Prevalence and risk factors of anxiety and depression in Chinese patients with lung cancera cross-sectional study. Cancer Manag Res. 2019;11:4347–4356. doi: 10.2147/CMAR.S202119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nguyen LT, Alexander K, Yates P. Psychoeducational intervention for symptom management of fatigue, pain, and sleep disturbance cluster among cancer patients: a pilot quasi-experimental study. J Pain Symptom Manage. 2018;55:1459–1472. doi: 10.1016/j.jpainsymman.2018.02.019. [DOI] [PubMed] [Google Scholar]
- 35.Banik A, Luszczynska A, Pawlowska I, Cieslak R, Knoll N, Scholz U. Enabling, not cultivating: received social support and self-efficacy explain quality of life after lung cancer surgery. Ann Behav Med. 2017;51:1–12. doi: 10.1007/s12160-016-9821-9. [DOI] [PubMed] [Google Scholar]
- 36.Hoffman AJ, Brintnall RA, Given BA, von Eye A, Jones LW, Brown JK. Using perceived self-efficacy to improve fatigue and fatigability in postsurgical lung cancer patients: a pilot randomized controlled trial. Cancer Nurs. 2017;40:1–12. doi: 10.1097/NCC.0000000000000378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Morrison EJ, Novotny PJ, Sloan JA, Yang P, Patten CA, Ruddy KJ, Clark MM. Emotional problems, quality of life, and symptom burden in patients with lung cancer. Clin Lung Cancer. 2017;18:497–503. doi: 10.1016/j.cllc.2017.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]


