Key Points
Question
What conditions should be prioritized for research involving hospitalized children?
Findings
In this cross-sectional study of 627 314 inpatient encounters among children at 165 hospitals in Ontario, Canada, 65.0% of encounters and 43.8% of costs occurred at general hospitals. Several newborn and mental health conditions were identified as most prevalent, costly, and with high variation in cost across hospitals.
Meaning
The results of this study can be used to design a research agenda for the care of hospitalized children that includes general hospitals and may inform researchers, health care system leaders, and funders about research areas and quality improvement efforts that could be prioritized.
Abstract
Importance
Identifying conditions that could be prioritized for research based on health care system burden is important for developing a research agenda for the care of hospitalized children. However, existing prioritization studies are decades old or do not include data from both pediatric and general hospitals.
Objective
To assess the prevalence, cost, and variation in cost of pediatric hospitalizations at all general and pediatric hospitals in Ontario, Canada, with the aim of identifying conditions that could be prioritized for future research.
Design, Setting, and Participants
This population-based cross-sectional study used health administrative data from 165 general and pediatric hospitals in Ontario, Canada. Children younger than 18 years with an inpatient hospital encounter between April 1, 2014, and March 31, 2019, were included.
Main Outcomes and Measures
Condition-specific prevalence, cost of pediatric hospitalizations, and condition-specific variation in cost per inpatient encounter across hospitals. Variation in cost was evaluated using (1) intraclass correlation coefficient (ICC) and (2) number of outlier hospitals. Costs were adjusted for inflation to 2018 US dollars.
Results
Overall, 627 314 inpatient hospital encounters (44.8% among children younger than 30 days and 53.0% among boys) at 165 hospitals (157 general and 8 pediatric) costing $3.3 billion were identified. A total of 408 003 hospitalizations (65.0%) and $1.4 billion (43.8%) in total costs occurred at general hospitals. Among the 50 most prevalent and 50 most costly conditions (of 68 total conditions), the top 10 highest-cost conditions accounted for 55.5% of all costs and 48.6% of all encounters. The conditions with highest prevalence and cost included low birth weight (86.2 per 1000 encounters; $676.3 million), preterm newborn (38.0 per 1000 encounters; $137.4 million), major depressive disorder (20.7 per 1000 encounters; $78.3 million), pneumonia (27.3 per 1000 encounters; $71.6 million), other perinatal conditions (68.0 per 1000 encounters; $65.8 million), bronchiolitis (25.4 per 1000 encounters; $54.6 million), and neonatal hyperbilirubinemia (47.9 per 1000 encounters; $46.7 million). The highest variation in cost per encounter among the most costly medical conditions was observed for 2 mental health conditions (other mental health disorders [ICC, 0.28] and anxiety disorders [ICC, 0.19]) and 3 newborn conditions (intrauterine hypoxia and birth asphyxia [ICC, 0.27], other perinatal conditions [ICC, 0.17], and surfactant deficiency disorder [ICC, 0.17]).
Conclusions and Relevance
This population-based cross-sectional study of hospitalized children identified several newborn and mental health conditions as having the highest prevalence, cost, and variation in cost across hospitals. Findings of this study can be used to develop a research agenda for the care of hospitalized children that includes general hospitals and to ultimately build a more substantial evidence base and improve patient outcomes.
This cross-sectional study assesses the prevalence, cost, and variation in cost of pediatric hospitalizations at all general and pediatric hospitals in Ontario, Canada, and identifies conditions that may be prioritized for future research.
Introduction
Hospital care costs account for the largest component of all health care costs.1,2 Among children, hospital expenditures are high, with costs increasing over time.3,4 Despite the large volume and high cost of admissions, hospitalized children may not receive optimal care owing to a lack of high-quality evidence.5,6,7 For example, few randomized clinical trials have been conducted in pediatric hospitals compared with specialty units, such as oncology8 and critical care.9,10 The lack of high-quality research can produce unnecessary variation in clinical practice and outcomes.11,12,13,14
Identifying topics to prioritize for future research is necessary to build a meaningful research agenda for the care of hospitalized children. One factor identified in research prioritization frameworks is the condition-related criterion, which includes assessing the prevalence, cost, and variation in cost of the illness.15,16 Conditions that are common, require costly care, and have high cost variation increase in rank to become high-priority conditions for research.15,16 Existing studies have examined the burden of pediatric hospitalizations in North America,16,17,18,19,20 but study limitations have made it difficult to use their findings for future research. In the US, 3 studies16,17,18 have identified common and costly conditions among hospitalized children. The most recent study18 excluded general hospitals, in which most pediatric hospitalizations occur.17 In Canada, 2 studies19,20 identified the most common reasons for pediatric hospitalization; however, those studies used data that are now more than 2 decades old and did not explore the cost of conditions.
Therefore, the aim of this study was to describe the epidemiologic characteristics of pediatric hospitalizations and identify conditions that could be prioritized for research using population-based data across all general and pediatric hospitals in Ontario, Canada. The specific objectives were to (1) assess the condition-specific prevalence, cumulative cost, and variation in cost of pediatric hospitalizations and (2) rank order the pediatric hospital conditions to identify those with high prevalence, cost, and/or variation in cost as priorities for future research involving hospitalized children.
Methods
Study Design
This population-based cross-sectional study focused on children with hospital encounters in Ontario, the most populous province in Canada with a population of 14.8 million.21 Data were obtained from linked Ontario health administrative databases housed at ICES (formerly known as the Institute for Clinical Evaluative Sciences). The data included all children eligible for provincial health care coverage and all general and pediatric hospitals in Ontario. The study was approved by the Hospital for Sick Children Research Ethics Board with a waiver of informed consent because deidentified data were used. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cross-sectional studies.22
Data Sources
Clinical information and intensity of resources consumed for hospital encounters (inpatient discharges or same-day surgery) were obtained from the Canadian Institute for Health Information Discharge Abstract Database and the Same Day Surgery Database. Demographic information was extracted from the Registered Persons Database,23 and annual population estimates for Ontario were obtained from intercensal population estimates and projections for local health integrated networks.24
Study Population
Children younger than 18 years with an inpatient hospital encounter between April 1, 2014, and March 31, 2019, were included. We excluded encounters among children with missing or invalid birth dates, death dates, or discharge dates; encounters among non-Ontario residents; encounters indicating normal newborn birth based on a most responsible diagnostic code (defined as the condition that contributes the greatest extent to the patient's hospital stay) from the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Canada (ICD-10-CA); and same-day surgery encounters (all exclusions are shown in the eFigure in the Supplement).
Pediatric Clinical Classification System
For each hospital encounter, the most responsible diagnosis was determined using the ICD-10-CA discharge diagnostic code and classified into discrete clinical condition categories using codes from the Pediatric Clinical Classification System. This system classifies 16 992 ICD-10-CA codes into 781 clinically meaningful categories to identify specific pediatric conditions, including treatments (eg, chemotherapy). The Pediatric Clinical Classification System was first developed for the US International Statistical Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) coding system and evaluated using US administrative pediatric hospitalization data.25 This grouping system categorized conditions into medical, surgical, and medical/surgical based on the percentage of encounters for the condition that had a surgical procedure code. If fewer than 30% of encounters for the condition had a surgical procedure code, the condition was classified as medical; if more than 70% of encounters for the condition had a surgical procedure code, the condition was classified as surgical; and if between 30% and 70% of encounters for the condition had a surgical procedure code, the condition was classified as medical/surgical.18
Outcome Measures
We estimated the condition-specific prevalence of hospitalization for each condition, with condition-specific prevalence defined as the proportion of hospital encounters owing to the specific condition over the study period. We also calculated the condition-specific cost of hospitalization for each condition as a proxy for the volume of resources used to manage the condition.16 Costs were estimated using an ICES costing algorithm, which multiplied the resource intensity weight assigned to each inpatient case recorded in the Canadian Institute for Health Information Discharge Abstract Database with the provincial mean unit cost of acute hospitalization (ie, cost per weighted case) for the corresponding fiscal year.26 The resource intensity weight represents the amount of resources used by the inpatient case relative to an average inpatient case.26 Costs were adjusted for inflation to 2018 US dollars (mean exchange rate: $0.77 US dollars = $1.00 Canadian dollar). Details on the case-costing methods are available online.26 We also estimated the condition-specific variation in cost per encounter across hospitals to measure the variation in resources used to manage each condition across hospitals.16
Patient, Encounter, and Hospital Characteristics
Patient characteristics included age at the time of the hospital encounter (<30 days, ≥30 days to <1 year, 1-4 years, 5-12 years, and 13 to <18 years),16 sex, and rural vs urban residence (measured using the Rurality Index for Ontario, with urban defined as a score <40 and rural defined as a score ≥40).27,28 The components used to calculate the Rurality Index for Ontario included community population size and density as well as travel time to the nearest basic and advanced referral centers.27 The number of complex chronic conditions (CCCs) present (0, 1, 2, or ≥3)29,30 for each patient was estimated using the diagnostic and procedural codes adopted by the Canadian Institute for Health Information.31 To identify whether CCCs were present, for each encounter, the patient’s hospital data were examined for the previous 2 years or until birth if the patient was younger than 2 years. To measure the socioeconomic status of the cohort, the Ontario Marginalization Index was used to identify material deprivation32 by quintile (with quintile 1 indicating least deprived and quintile 5 indicating most deprived). The factors used to measure material deprivation were income, quality of housing, educational level, and family structure characteristics.32,33 For hospital encounter characteristics, we identified the condition type (medical, surgical, or medical/surgical) and length of stay in days.
For hospital characteristics, we identified hospital type, which was categorized as general or pediatric (defined as a tertiary care children’s hospital or a hospital with a level 3 neonatal intensive care unit). The hospital region (central east, central south, central west, east, north, southwest, or Toronto, Ontario) and the mean volume of inpatient encounters per year were also identified.
Statistical Analysis
For each hospital condition, we determined the condition-specific prevalence over the study period using the number of hospital encounters associated with the condition as the numerator and the total number of encounters associated with all conditions as the denominator. We calculated the prevalence per 1000 patient encounters. The median and mean cost per encounter and the cumulative cost of encounters for each condition were also calculated. Hospital conditions were ranked from highest to lowest based on the total volume of encounters (called prevalence rank) and based on cumulative cost.
For the 25 medical conditions with the highest cumulative cost, we determined the variation in cost per encounter across hospitals. We focused on the conditions with the highest cumulative cost because they would either be highly prevalent or highly costly per encounter.16 The condition-specific variation in cost across hospitals was adjusted for known factors associated with variation in cost, including age, sex, number of CCCs present, material deprivation, and rural vs urban classification to minimize confounding from other factors that may have biased the extent of variation in cost across hospitals.16,34,35,36
To alleviate skewness, hospital encounter costs were log transformed before conducting the analysis of variation in cost. The variation in cost per encounter was assessed using 2 methods16: intraclass correlation coefficient (ICC) and number of outlier hospitals. To assess variation in cost per encounter using the ICC method, for each condition, the variation in cost (using cost per encounter) across hospitals was divided by the total variation in cost per encounter (which included within-hospital and across-hospital variation in costs). The ICC was calculated using a mixed-effects model with random intercepts for each hospital and patient characteristics as fixed effects.16 To assess variation in cost per encounter using the number of outlier hospitals, for each condition, the number of hospitals with more than 30% of encounters in the highest or lowest quintile of overall cost per encounter was calculated. The ICC was a single measure that quantified the extent of variation in cost across hospitals, whereas the number of outlier hospitals provided granularity regarding the number of hospitals that met the low-cost and/or high-cost outlier hospital criteria for the condition.16 To ensure we had an adequate sample of hospitals and encounters per hospital for the analysis of variation in cost, we restricted this analysis to conditions (from the 25 highest-cost medical conditions) that had data available from at least 10 hospitals with more than 25 encounters per hospital for the corresponding condition.37 Secondary analysis examined the variation in cost per encounter for each condition across general hospitals alone. This analysis was not performed separately across pediatric hospitals because of the small number of pediatric hospitals.
Additional analyses identified the 25 most prevalent and 25 most costly conditions in pediatric vs general hospitals. These analyses were conducted as differences in the volume, cost, and characteristics of pediatric hospitalizations reported between hospital types.17 Analyses were performed using SAS Enterprise Guide software, version 7.1 (SAS Institute Inc).
Results
In total, there were 1 361 712 hospital encounters among children in Ontario between April 1, 2014, and March 31, 2019. After exclusions (437 166 of which were normal newborn births), 627 314 inpatient encounters among children were included from 157 general hospitals and 8 pediatric hospitals (eFigure in the Supplement). The total hospital cost was $3.3 billion, with 408 003 hospitalizations (65.0%) and $1.4 billion (43.8%) in total costs occurring at general hospitals.
Of the included encounters, 281 230 (44.8%) were among children younger than 30 days, 332 494 (53.0%) were among boys, and 571 437 (91.1%) were among children residing in urban areas (Table 1). Children with at least 1 CCC represented 141 653 inpatient encounters (22.6%). A total of 471 440 encounters (75.2%) occurred because of medical conditions, 94 727 encounters (15.1%) occurred because of surgical conditions, and 61 147 encounters (9.7%) occurred because of medical/surgical conditions. The median length of stay was 2 days (IQR, 1-4 days). The median annual hospital volume of inpatient encounters was 73.0 (IQR, 4.6-1003.2).
Table 1. Patient, Encounter, and Hospital Characteristics Among Children With Inpatient Encounters in Ontario, Canada, From 2014 to 2019.
| Characteristic | No. (%) |
|---|---|
| Patients | |
| Total inpatient encounters, No. | 627 314 |
| Age at time of encounter, median (IQR), y | 0 (0-8.0) |
| Age range at time of encounter | |
| <30 d | 281 230 (44.8) |
| ≥30 d to <1 y | 53 827 (8.6) |
| 1 to 4 y | 93 217 (14.9) |
| 5 to 12 y | 92 730 (14.8) |
| 13 to <18 y | 106 310 (16.9) |
| Sex | |
| Female | 294 820 (47.0) |
| Male | 332 494 (53.0) |
| Rurality of residence | |
| Rural | 41 548 (6.6) |
| Urban | 571 437 (91.1) |
| Missing | 14 329 (2.3) |
| No. of complex chronic conditions present | |
| 0 | 485 661 (77.4) |
| 1 | 74 685 (11.9) |
| 2 | 26 537 (4.2) |
| ≥3 | 40 431 (6.4) |
| Material deprivation, quintile | |
| 1 (Least deprived) | 123 336 (19.7) |
| 2 | 119 456 (19.0) |
| 3 | 113 473 (18.1) |
| 4 | 115 571 (18.4) |
| 5 (Most deprived) | 142 832 (22.8) |
| Missing | 12 646 (2.0) |
| Encounters | |
| Type of condition | |
| Medical | 471 440 (75.2) |
| Medical/surgical | 61 147 (9.7) |
| Surgical | 94 727 (15.1) |
| Length of stay, median (IQR), d | 2.0 (1.0-4.0) |
| Hospitals | |
| Total hospitals, No. | 165 |
| Type of hospital | |
| Pediatric | 8 (4.8) |
| General | 157 (95.2) |
| Region | |
| Southwest | 35 (21.2) |
| Central south | 12 (7.3) |
| Central west | 15 (9.1) |
| Central east | 19 (11.5) |
| Toronto | 14 (8.5) |
| East | 27 (16.4) |
| North | 43 (26.1) |
| Annual volume of inpatient encounters, median (IQR) | 73.0 (4.6-1003.2) |
Prevalence and Cost
The 50 most prevalent and 50 most costly conditions (of 68 total conditions) ranked by cumulative cost are shown in Table 2. The top 10 most costly conditions accounted for 55.5% of all costs and 48.6% of all encounters among the 68 conditions. Extreme immaturity of newborn had the highest median cost per encounter ($21 702; IQR, $3698-$40 779). Low birth weight had the highest prevalence (86.2 per 1000 encounters). Several mental health conditions had the highest prevalence and highest cost among children; these conditions included major depressive disorder (20.7 per 1000 encounters; $78.3 million), adjustment disorders (12.1 per 1000 encounters; $40.9 million), anorexia nervosa (2.8 per 1000 encounters; $31.5 million), anxiety disorders (8.0 per 1000 encounters; $30.7 million), other mental health disorders (5.1 per 1000 encounters; $19.3 million), schizophrenia and psychotic disorders (2.4 per 1000 encounters; $17.2 million), and attention-deficit/hyperactivity disorder (3.5 per 1000 encounters; $16.3 million). Diagnoses within the condition category other mental health disorders are shown in eTable 1 in the Supplement.
Table 2. Prevalence and Cost for the 50 Most Costly and 50 Most Prevalent Conditions Among Children With Inpatient Encounters in Ontario, Canada, From 2014 to 2019.
| Conditiona | Type of condition | Rank | Inpatient encounters, No. | Cost, $b | |||
|---|---|---|---|---|---|---|---|
| Based on total cost | Based on No. of encountersc | Totald | Prevalencee | Total | Per encounter, median (IQR) | ||
| Low birth weight | Medical | 1 | 1 | 54 100 | 86.2 | 676 292 381 | 2924 (1236-13 777) |
| Preterm newborn | Medical | 2 | 4 | 23 821 | 38.0 | 137 377 386 | 2468 (1255-6011) |
| Major depressive disorder | Medical | 3 | 9 | 12 975 | 20.7 | 78 303 976 | 5780 (5306-6735) |
| Pneumonia | Medical | 4 | 5 | 17 143 | 27.3 | 71 566 538 | 2929 (2709-4029) |
| Other perinatal conditions | Medical | 5 | 2 | 42 674 | 68.0 | 65 791 674 | 1036 (1026-1236) |
| Bronchiolitis | Medical | 6 | 6 | 15 950 | 25.4 | 54 581 261 | 2602 (2392-2700) |
| Surfactant deficiency disorder | Medical | 7 | 43 | 3015 | 4.8 | 50 023 527 | 6645 (2148-15 952) |
| Neonatal hyperbilirubinemia | Medical | 8 | 3 | 30 048 | 47.9 | 46 670 627 | 1447 (1064-1500) |
| Adjustment disorders | Medical | 9 | 17 | 7621 | 12.1 | 40 888 157 | 5114 (4675-6314) |
| Transient tachypnea of newborn | Medical | 10 | 7 | 14 287 | 22.8 | 40 298 745 | 1653 (1428-3383) |
| Chemotherapy | Medical | 11 | 14 | 7905 | 12.6 | 37 529 210 | 4238 (2634-4490) |
| Drug withdrawal syndrome in newborn | Medical | 12 | 39 | 3291 | 5.2 | 37 016 433 | 9473 (8713-13 274) |
| Anorexia nervosa | Medical | 13 | 66 | 1758 | 2.8 | 31 464 629 | 18 398 (16 329-18 752) |
| Anxiety disorders | Medical | 14 | 26 | 5010 | 8.0 | 30 680 583 | 6448 (5395-7030) |
| Asthma | Medical | 15 | 8 | 13 449 | 21.4 | 28 454 191 | 1723 (1623-2081) |
| Acute appendicitis without peritonitis | Surgical | 16 | 12 | 9978 | 15.9 | 27 902 739 | 2655 (2519-2832) |
| Feeding difficulties | Medical/surgical | 17 | 22 | 6560 | 10.5 | 25 848 677 | 1531 (1036-4105) |
| Urinary tract infections | Medical | 18 | 18 | 7088 | 11.3 | 25 645 046 | 3112 (2831-3466) |
| Other congenital anomalies | Surgical | 19 | 42 | 3077 | 4.9 | 25 600 029 | 2474 (930-4716) |
| Infectious gastroenteritis | Medical | 20 | 10 | 11 373 | 18.1 | 25 591 365 | 1735 (1706-1897) |
| Respiratory distress of newborn | Medical | 21 | 16 | 7738 | 12.3 | 23 641 152 | 1541 (1428-2796) |
| Acute lymphoid leukemia | Medical | 22 | 119 | 894 | 1.4 | 23 453 440 | 17 271 (12 208-29 469) |
| Necrotizing enterocolitis | Medical/surgical | 23 | 174 | 459 | 0.7 | 23 045 352 | 17 821 (9370-47 819) |
| Acute appendicitis with peritonitis | Surgical | 24 | 29 | 4400 | 7.0 | 22 170 824 | 4006 (3852-4755) |
| Complications of surgical procedures or medical care | Medical/surgical | 25 | 30 | 4164 | 6.6 | 21 916 650 | 2393 (1438-4175) |
| Extreme immaturity of newborn | Medical | 26 | 147 | 580 | 0.9 | 20 925 776 | 21 702 (3698-40 779) |
| Scoliosis | Surgical | 27 | 101 | 1053 | 1.7 | 20 547 895 | 18 884 (12 943-19 834) |
| Intrauterine hypoxia and birth asphyxia | Medical | 28 | 57 | 2326 | 3.7 | 20 469 981 | 3385 (1528-10 694) |
| Other mental health disorders | Medical | 29 | 41 | 3168 | 5.1 | 19 272 426 | 2843 (2320-6185) |
| Sepsis of newborn | Medical | 30 | 52 | 2638 | 4.2 | 18 806 085 | 4985 (2961-6845) |
| Neutropenia | Medical | 31 | 44 | 3010 | 4.8 | 18 704 373 | 4240 (3703-6717) |
| Septicemia | Medical | 32 | 61 | 1890 | 3.0 | 18 688 859 | 4630 (4117-8729) |
| Fracture of lower limb | Surgical | 33 | 35 | 3776 | 6.0 | 18 566 246 | 3953 (3328-4926) |
| Respiratory failure | Medical | 34 | 138 | 677 | 1.1 | 18 550 691 | 11 766 (4800-36 001) |
| Newborn respiratory failure | Medical | 35 | 20 | 6642 | 10.6 | 18 328 994 | 1268 (1123-2335) |
| Neonatal hypoglycemia | Medical | 36 | 15 | 7844 | 12.5 | 18 226 564 | 1078 (1030-2400) |
| Tetralogy of Fallot | Medical/surgical | 37 | 147 | 580 | 0.9 | 17 923 567 | 17 303 (4047-28 984) |
| Schizophrenia and psychotic disorders | Medical | 38 | 72 | 1519 | 2.4 | 17 244 815 | 10 768 (9374-11 384) |
| Transposition of great vessels | Medical/surgical | 39 | 173 | 461 | 0.7 | 16 416 666 | 20 067 (3217-44 862) |
| Attention-deficit/hyperactivity disorder | Medical | 40 | 58 | 2199 | 3.5 | 16 337 289 | 7046 (6367-7823) |
| Viral infection | Medical | 41 | 21 | 6632 | 10.6 | 16 158 659 | 1918 (1829-2131) |
| Hypertrophy of tonsils and adenoids | Surgical | 42 | 13 | 8166 | 13.0 | 15 948 718 | 1842 (1828-1907) |
| Intracranial injury | Medical | 43 | 90 | 1156 | 1.8 | 15 775 600 | 3945 (2673-11 482) |
| Gastroschisis and exomphalos | Surgical | 44 | 219 | 319 | 0.5 | 15 639 964 | 21 307 (1113-65 445) |
| Congenital tracheoesophageal disorders | Surgical | 45 | 236 | 277 | 0.4 | 15 518 709 | 10 313 (2035-47 866) |
| Sleep apnea | Surgical | 46 | 23 | 6358 | 10.1 | 15 498 436 | 1842 (1828-1907) |
| Hypoplastic left heart syndrome | Medical/surgical | 47 | 253 | 238 | 0.4 | 15 261 396 | 14 977 (1595-54 180) |
| Screening for suspected conditions | Medical | 48 | 11 | 10 817 | 17.2 | 14 444 254 | 1065 (1030-1236) |
| Cystic fibrosis | Medical | 49 | 120 | 856 | 1.4 | 14 429 112 | 14 179 (12 436-16 173) |
| Seizures with and without intractable epilepsy | Medical | 50 | 33 | 3913 | 6.2 | 14 356 766 | 1903 (1801-2754) |
| Cellulitis | Medical | 51 | 31 | 4114 | 6.6 | 14 298 664 | 3055 (2482-3596) |
| Acute upper respiratory infection | Medical | 52 | 25 | 5023 | 8.0 | 14 272 166 | 2057 (1967-2181) |
| Other lower respiratory disease | Medical | 53 | 38 | 3533 | 5.6 | 14 126 940 | 2213 (1939-2791) |
| Fever of unknown origin | Medical | 54 | 28 | 4693 | 7.5 | 12 746 513 | 2284 (2167-2529) |
| Infant of diabetic mother | Medical | 55 | 19 | 6707 | 10.7 | 12 569 146 | 1078 (1030-1236) |
| Other aftercare | Medical/surgical | 57 | 27 | 4738 | 7.6 | 11 353 620 | 1275 (1187-1554) |
| Fracture of upper limb | Surgical | 61 | 32 | 3953 | 6.3 | 11 037 979 | 2931 (1984-3034) |
| Supracondylar fracture of humerus | Surgical | 63 | 36 | 3713 | 5.9 | 10 643 826 | 2943 (2856-2974) |
| ABO hemolytic disease | Medical | 81 | 34 | 3814 | 6.1 | 8 375 305 | 1858 (1682-2190) |
| Influenza | Medical | 86 | 50 | 2865 | 4.6 | 8 212 883 | 2072 (1970-2393) |
| Diabetic ketoacidosis | Medical | 87 | 46 | 2988 | 4.8 | 8 126 963 | 2607 (2272-2838) |
| Congenital genitourinary anomalies | Surgical | 90 | 40 | 3171 | 5.1 | 7 717 287 | 930 (891-1629) |
| Neonatal tachycardia | Medical | 93 | 48 | 2929 | 4.7 | 7 258 219 | 1078 (1030-1558) |
| Other convulsions | Medical | 103 | 47 | 2954 | 4.7 | 6 568 239 | 1882 (1796-2198) |
| Respiratory problems after birth, other | Medical | 110 | 49 | 2882 | 4.6 | 5 901 470 | 1526 (1428-1677) |
| Tongue-tied | Surgical | 112 | 24 | 5128 | 8.2 | 5 892 461 | 1036 (1026-1078) |
| Birth trauma | Medical/surgical | 118 | 45 | 3002 | 4.8 | 5 344 774 | 1065 (1026-1236) |
| Croup | Medical | 124 | 37 | 3612 | 5.8 | 5 067 750 | 1148 (1103-1292) |
Abbreviation: ABO, ABO blood group system.
Sixty-eight total conditions.
Costs adjusted for inflation to 2018 US dollars (mean 2018 exchange rate: $0.77 US dollars = $1.00 Canadian dollar).
Also known as prevalence rank in this study.
Total number of encounters for the condition over the study period.
Condition-specific prevalence per 1000 encounters.
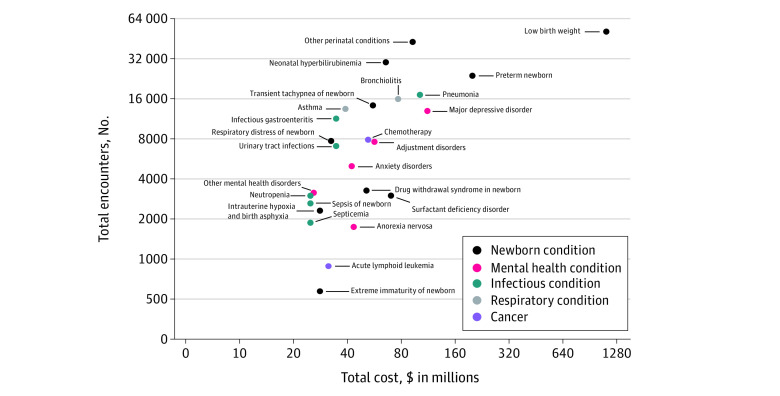
Of the 68 conditions, 7 were highly prevalent and costly: low birth weight (86.2 per 1000 encounters; $676.3 million), preterm newborn (38.0 per 1000 encounters; $137.4 million), major depressive disorder (20.7 per 1000 encounters; $78.3 million), pneumonia (27.3 per 1000 encounters; $71.6 million), other perinatal conditions (68.0 per 1000 encounters; $65.8 million), bronchiolitis (25.4 per 1000 encounters; $54.6 million), and neonatal hyperbilirubinemia (47.9 per 1000 encounters; $46.7 million) (Table 2; data for other perinatal conditions are shown in eTable 1 in the Supplement). The 25 most costly medical conditions were categorized into cancer (2 conditions: acute lymphoid leukemia and chemotherapy), newborn (10 conditions: drug withdrawal syndrome in newborn, extreme immaturity of newborn, intrauterine hypoxia and birth asphyxia, low birth weight, neonatal hyperbilirubinemia, other perinatal conditions, preterm newborn, respiratory distress of newborn, surfactant deficiency disorder, and transient tachypnea of newborn), mental health (5 conditions: adjustment disorders, anorexia nervosa, anxiety disorders, major depressive disorder, and other mental health disorders), infectious (6 conditions: infectious gastroenteritis, neutropenia, pneumonia, sepsis of newborn, septicemia, and urinary tract infections), and respiratory (2 conditions: asthma and bronchiolitis) (Figure 1). Most of the prevalent and costly medical conditions were newborn conditions (low birth weight, preterm newborn, and other perinatal conditions).
Figure 1. Volume and Cost of Encounters for the 25 Highest-Cost Medical Conditions Among Children With Inpatient Encounters in Ontario, Canada, From 2014 to 2019.
Total costs (in millions) are presented in Canadian dollars. To convert Canadian dollars to US dollars (adjusted for inflation to 2018 US dollars), multiply values by 0.77. The x- and y-axes are presented using a log2 scale.
The variation in cost per encounter across hospitals was examined for 23 of the 25 most costly medical conditions that had an adequate number of hospitals and/or encounters (Table 3). Two mental health conditions (other mental health disorders [ICC, 0.28] and anxiety disorders [ICC, 0.19]) and 3 newborn conditions (intrauterine hypoxia and birth asphyxia [ICC, 0.27], other perinatal conditions [ICC, 0.17], and surfactant deficiency disorder [ie, respiratory distress syndrome in newborn; ICC, 0.17]) had the highest variation in cost across hospitals using the ICC method. The outlier hospital method, which was also used to evaluate variation in cost, revealed that more than 50% of the hospitals examined had a high proportion of high- or low-cost hospitalizations for 3 conditions (chemotherapy [25 of 30 hospitals], intrauterine hypoxia and birth asphyxia [14 of 24 hospitals], and other mental health disorders [18 of 30 hospitals]) (Table 3). The variation in cost per encounter across general hospitals was examined for 21 of the 25 most costly medical conditions (eTable 2 in the Supplement). The variation in cost (measured using ICC) for most conditions was similar to the variation found when examined across all hospitals. However, for some conditions, such as intrauterine hypoxia and birth asphyxia (ICC, 0.06) and other perinatal conditions (ICC, 0.06), the ICCs were substantially lower across general hospitals.
Table 3. Variation in Cost per Encounter Across Hospitals for the 25 Medical Conditions With the Highest Cumulative Cost Among Children in Ontario From 2014 to 2019.
| Condition | Hospitals included, No.a | ICCb | Outlier hospitals, No.b | ||
|---|---|---|---|---|---|
| Low cost | High cost | Totalc | |||
| Newborn | |||||
| Intrauterine hypoxia and birth asphyxia | 24 | 0.27 | 11 | 3 | 14 |
| Other perinatal conditions | 81 | 0.17 | 4 | 15 | 19 |
| Surfactant deficiency disorder | 39 | 0.17 | 13 | 4 | 17 |
| Low birth weight | 70 | 0.14 | 26 | 5 | 31 |
| Preterm newborn | 67 | 0.11 | 16 | 6 | 22 |
| Transient tachypnea of newborn | 65 | 0.11 | 17 | 6 | 23 |
| Respiratory distress of newborn | 58 | 0.11 | 10 | 9 | 19 |
| Drug withdrawal syndrome in newborn | 35 | 0.07 | 5 | 5 | 9 |
| Neonatal hyperbilirubinemia | 76 | 0.03 | 7 | 4 | 11 |
| Extreme immaturity of newbornd | NA | NA | NA | NA | NA |
| Mental health | |||||
| Other mental health disorders | 30 | 0.28 | 9 | 9 | 18 |
| Anxiety disorders | 29 | 0.19 | 6 | 2 | 8 |
| Major depressive disorder | 34 | 0.05 | 3 | 2 | 5 |
| Adjustment disorders | 28 | 0.05 | 2 | 3 | 5 |
| Anorexia nervosa | 11 | 0.03 | 2 | 0 | 2 |
| Infectious | |||||
| Septicemia | 22 | 0.10 | 5 | 3 | 8 |
| Sepsis of newborn | 33 | 0.07 | 3 | 6 | 9 |
| Neutropenia | 14 | 0.07 | 2 | 1 | 3 |
| Pneumonia | 52 | 0.06 | 8 | 4 | 12 |
| Infectious gastroenteritis | 46 | 0.03 | 5 | 2 | 5 |
| Urinary tract infections | 45 | 0.01 | 0 | 1 | 1 |
| Respiratory | |||||
| Bronchiolitis | 48 | 0.03 | 6 | 3 | 9 |
| Asthma | 46 | 0.02 | 0 | 1 | 1 |
| Cancer | |||||
| Chemotherapy | 30 | 0.12 | 22 | 11 | 25 |
| Acute lymphoid leukemiad | NA | NA | NA | NA | NA |
Abbreviations: ICC, intraclass correlation coefficient; NA, not applicable.
Number of hospitals in Ontario with >25 encounters for each corresponding condition during the study. Analysis of variation in cost was performed using encounter data from these hospitals only.
The ICCs and number of outlier hospitals were calculated using costs that were adjusted for patient age, sex, number of complex chronic conditions present, material deprivation, and rural vs urban classification.
Total number of distinct outlier hospitals for each condition. For some conditions, the total number does not equal the sum of low- and high-cost outlier hospitals because some of these hospitals were reported as both low- and high-cost outlier hospitals.
Analysis of variation in cost was not performed for extreme immaturity of newborn and acute lymphoid leukemia because there were <10 hospitals with >25 encounters for each of the conditions.
Prevalence and Cost by Hospital Type
At general hospitals, the median annual volume of encounters was 53.6 (IQR, 4.0-757.2), whereas in pediatric hospitals, the median annual volume was 4117.1 (IQR, 1924.9-7704.4). The volume and cost of inpatient encounters among children in pediatric and general hospitals are shown in eTable 3 in the Supplement.
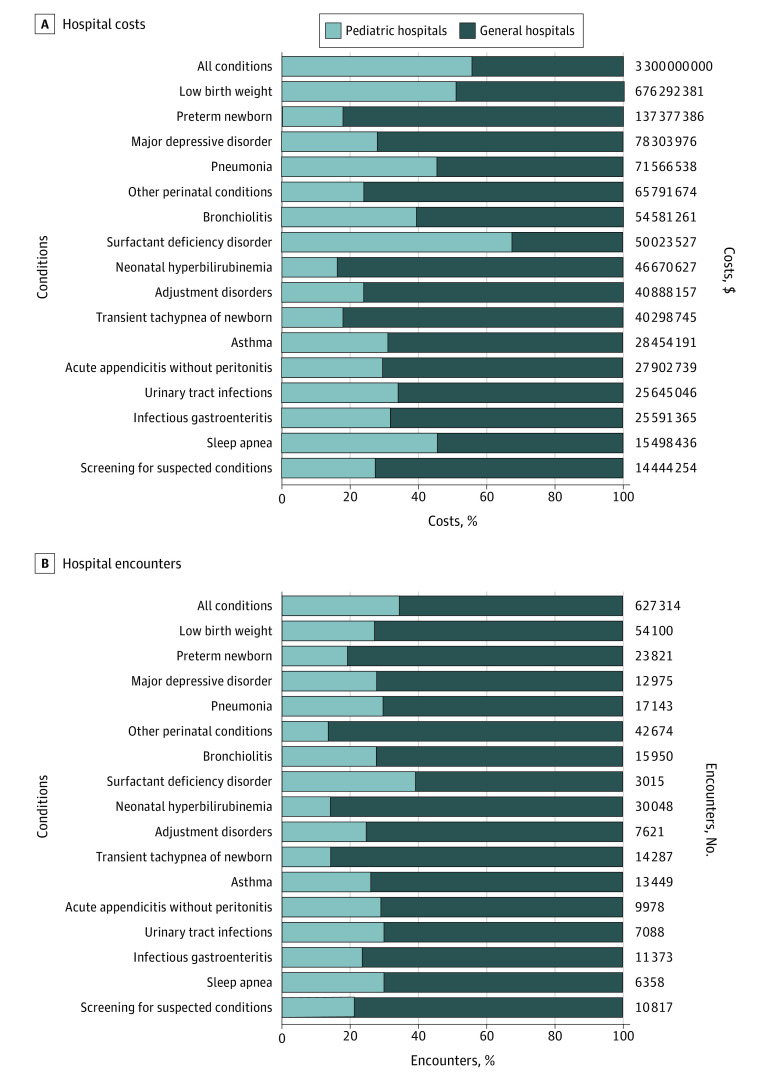
The rank order of the 25 most prevalent and 25 most costly conditions differed slightly between pediatric and general hospitals (eTable 4 and eTable 5 in the Supplement). In pediatric hospitals, the conditions with the highest prevalence and cost were low birth weight (68.2 per 1000 encounters; $348.1 million) and chemotherapy (28.4 per 1000 encounters; $34.2 million). In general hospitals, the most prevalent and costly conditions were low birth weight (95.9 per 1000 encounters) and other perinatal conditions (89.7 per 1000 encounters), and the most costly were low birth weight ($328.1 million) and preterm newborn ($112.3 million). The percentages of hospital costs and encounters that occurred in pediatric vs general hospitals for all conditions in total and for the most costly and/or most prevalent conditions identified in both hospital types are shown in Figure 2. Overall, inpatient encounters at general hospitals represented 65.0% of all hospital encounters and 43.8% of all hospital costs among children. With regard to the most costly and/or prevalent conditions in both hospital types, most of the hospital costs (59.2%) and encounters (77.0%) occurred in general hospitals.
Figure 2. Costs and Encounters of the Most Costly and Prevalent Conditions in Pediatric and General Hospitals in Ontario, Canada, From 2014 to 2019.
Percentage of hospital costs and encounters for all conditions and for the most costly and/or prevalent conditions (based on the top 25 most prevalent conditions and the top 25 most costly conditions identified for each hospital type in eTable 4 and eTable 5 in the Supplement). Costs were adjusted for inflation to 2018 US dollars (mean 2018 exchange rate: $0.77 US dollars = $1.00 Canadian dollar).
Discussion
This population-based cross-sectional study of health administrative data from Canada’s most populous province identified pediatric hospital conditions with high prevalence, cost, and/or variation in cost from 2014 to 2019. The study included 627 314 hospitalizations among children at all general and pediatric hospitals, finding that 65.0% of encounters and 43.8% of costs occurred at general hospitals. Several mental health and newborn conditions (low birth weight, preterm newborn, major depressive disorder, other perinatal conditions, and neonatal hyperbilirubinemia) had the highest prevalence, cost, and variation in cost across hospitals. Findings from this study can be combined with research priorities identified by patients, caregivers, and clinicians38 to develop a research agenda for investigators and funders conducting research involving hospitalized children. Furthermore, the findings may be used to prioritize hospital quality improvement efforts.
A separate study recently examined the prevalence and cost of conditions in US pediatric hospitals.18 Although it is difficult to compare the current study with the previous US study18 because of differences in health care systems,39 coding systems used (ICD-10-CA vs ICD-10-CM), and hospital types included, we observed several differences in the rank order of conditions. Newborn conditions such as low birth weight, which were ranked higher in cumulative cost in the current study, were ranked lower in cumulative cost in US pediatric hospitals,18 which likely reflects the large role of nonpediatric hospitals in neonatal care as well as potential ICD-10 coding differences. The US study18 also identified fewer mental health conditions as prevalent and costly (2 mental health conditions within the top 50 list compared with 7 mental health conditions in the present study). In 1 study conducted in Ontario between 1991 to 1992 and 1997 to 1998,20 respiratory conditions, such as bronchiolitis and asthma, were the primary reasons for medical hospitalization among children younger than 15 years. In the current study, bronchiolitis was ranked sixth and asthma ranked eighth in the list of most prevalent conditions.
Several mental health conditions were identified among the 50 most prevalent and costly conditions, consistent with recent reports40,41 identifying mental disorders as one of the most common reasons for pediatric hospitalization. A recent study41 reported a 60% increase in hospitalizations for mental disorders among children and youths in Canada from 2008 to 2009 and 2018 to 2019. Beyond the health care system burden, 2 mental health conditions (anxiety disorders and other mental health disorders) also had high variation in cost across hospitals, with the broad category of other mental health disorders having the highest ICC (0.28) of all costly medical conditions (specific mental health diagnoses are available in eTable 1 in the Supplement). The high cost and prevalence of mental health conditions in pediatric hospitalization may be owing to a lack of effective interventions and the presence of barriers to accessing mental health services, including long waiting times for counseling and therapy, lack of available mental health professionals, and challenges regarding access to community-based mental health services.42,43,44,45 In Ontario, rates of outpatient visits have modestly increased, whereas emergency department visits and hospitalizations for mental health among children have substantially increased between 2009 and 2017.46 This difference suggests the presence of barriers to outpatient mental health care and an increase in the prevalence43 and burden of mental illnesses that are severe enough to require hospitalization.46 Our study findings highlight the need to improve care standardization across hospitals and evaluate new mental health interventions for children to identify those that are most cost-effective.
Newborn conditions, such as low birth weight and preterm newborn, were also the most prevalent and costly conditions among hospitalized children. We found that almost one-half (44.8%) of the inpatient encounters occurred among children younger than 30 days. Similar findings were observed in previous Canadian studies.20,40,47 Over the last few decades, research in the field of neonatology has produced advancements in neonatal care, which has been associated with improvements in survival and outcomes among infants.48,49 The high cost and prevalence of newborn conditions observed in our study suggests the need for research to identify cost-effective interventions for this population. In addition to high cost and prevalence, several newborn conditions (eg, intrauterine hypoxia and birth asphyxia) had high variation in cost across hospitals. These conditions represent areas in which better understanding of clinical practice variation is needed to identify whether future research or quality improvement initiatives are required to address them.
Most pediatric hospitalizations in Ontario (65.0%) occurred in general hospitals, which is similar to the 70% previously reported in the US.17 The high prevalence and cost of encounters observed in general hospitals suggest the need for future research to focus on ways to better manage these conditions among children admitted to general hospitals and to prioritize quality improvement efforts toward these areas. Most published studies on hospital use or ways to improve hospital care among children have only included pediatric hospitals.18,30,50,51,52 The lack of inclusion of general hospitals (including community hospitals) in research leaves important clinical care questions in these hospitals unanswered.53 Furthermore, because of differences in hospital characteristics (eg, practice settings), quality improvement initiatives based on research conducted in pediatric hospitals may not be applicable to general hospitals.53 It is important that general hospitals be included in research involving hospitalized children to ensure findings are generalizable and reflect the hospital setting in which most children receive care.53
Limitations
This study has several limitations. First, errors may have occurred when coding the discharge diagnosis, which may have resulted in misclassification of conditions. Second, hospitalization costs were estimated using provincial mean unit costs, and the amount of resources consumed was estimated using the patient’s resource intensity weight. Therefore, the costs do not reflect the actual costs of the resources used and may underestimate the extent of the cost variation.26,54 Third, unmeasured factors (eg, disease severity) may have accounted for a portion of the variation in cost across hospitals. Fourth, a few nonspecific conditions, such as other mental health disorders, had high prevalence, cost, and/or variation in cost across hospitals. Future condition-specific research could focus on examining the specific diagnostic codes underlying these nonspecific conditions. Fifth, our system-level analysis did not examine the condition-specific sources of cost or variation in cost (eg, length of stay). Future condition-specific studies could examine these sources. Sixth, the data used in this study were reported before the COVID-19 pandemic.
Conclusions
This population-based cross-sectional study used health administrative data from Ontario, Canada, to identify conditions with high prevalence, cost, and/or variation in cost as priorities for future research. Several newborn and mental health conditions (low birth weight, preterm newborn, major depressive disorder, other perinatal conditions, and neonatal hyperbilirubinemia) were identified as having the highest prevalence, cost, and variation in cost across hospitals. Findings from this study can be used by investigators and funders to develop a research agenda that includes general hospitals, with the goal of improving the evidence base and outcomes for hospitalized children. Furthermore, the findings may help prioritize hospital quality improvement initiatives to ensure high-quality hospital care is provided to children.
eFigure. Flow Diagram of Cohort Construction
eTable 1. Top 10 ICD-10-CA Most Responsible Diagnosis Codes That Led to Hospital Encounters for Each Nonspecific Pediatric Condition Identified in Children With Inpatient Encounters (From Table 2) in Ontario, 2014-2019
eTable 2. Variation in Cost per Encounter Across General Hospitals for the 25 Conditions With the Highest Cumulative Cost Among Children in Ontario, 2014-2019
eTable 3. Volume and Cost of Inpatient Encounters in Pediatric Hospitals and General Hospitals, 2014-2019
eTable 4. Prevalence and Cost of the 25 Most Costly and 25 Most Prevalent Conditions Among Children With Inpatient Encounters in Pediatric Hospitals in Ontario, 2014-2019
eTable 5. Prevalence and Cost for the 25 Most Costly and 25 Most Prevalent Conditions Among Children With Inpatient Encounters in General Hospitals in Ontario, 2014-2019
References
- 1.Centers for Medicare & Medicaid Services . National health expenditures 2018 highlights. Centers for Medicare & Medicaid Services; 2019. Accessed September 23, 2020. https://www.openminds.com/wp-content/uploads/120519nhe2018highlights.pdf
- 2.Canadian Institute for Health Information . National health expenditure trends, 2020. Canadian Institute for Health Information; 2021. Accessed March 2, 2021. https://www.cihi.ca/sites/default/files/document/nhex-trends-2020-narrative-report-en.pdf
- 3.Canadian Institute for Health Information . National health expenditure trends: data tables–series E2. Canadian Institute for Health Information; 2019. Accessed March 2, 2021. https://www.cihi.ca/sites/default/files/document/nhex-trends-narrative-report-2018-en.pdf
- 4.Lassman D, Hartman M, Washington B, Andrews K, Catlin A. US health spending trends by age and gender: selected years 2002-10. Health Aff (Millwood). 2014;33(5):815-822. doi: 10.1377/hlthaff.2013.1224 [DOI] [PubMed] [Google Scholar]
- 5.Cohen E, Goldman RD, Ragone A, et al. Child vs adult randomized controlled trials in specialist journals: a citation analysis of trends, 1985-2005. Arch Pediatr Adolesc Med. 2010;164(3):283-288. doi: 10.1001/archpediatrics.2009.291 [DOI] [PubMed] [Google Scholar]
- 6.Cohen E, Uleryk E, Jasuja M, Parkin PC. An absence of pediatric randomized controlled trials in general medical journals, 1985-2004. J Clin Epidemiol. 2007;60(2):118-123. doi: 10.1016/j.jclinepi.2006.03.015 [DOI] [PubMed] [Google Scholar]
- 7.Groff ML, Offringa M, Emdin A, Mahood Q, Parkin PC, Cohen E. Publication trends of pediatric and adult randomized controlled trials in general medical journals, 2005–2018: a citation analysis. Children (Basel). 2020;7(12):293. doi: 10.3390/children7120293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alexander S, Fisher BT, Gaur AH, et al. ; Children’s Oncology Group . Effect of levofloxacin prophylaxis on bacteremia in children with acute leukemia or undergoing hematopoietic stem cell transplantation: a randomized clinical trial. JAMA. 2018;320(10):995-1004. doi: 10.1001/jama.2018.12512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hartley C, Moultrie F, Hoskin A, et al. Analgesic efficacy and safety of morphine in the Procedural Pain in Premature Infants (Poppi) study: randomised placebo-controlled trial. Lancet. 2018;392(10164):2595-2605. doi: 10.1016/S0140-6736(18)31813-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parker MJ, Thabane L, Fox-Robichaud A, Liaw P, Choong K; Canadian Critical Care Trials Group and the Canadian Critical Care Translational Biology Group . A trial to determine whether septic shock–reversal is quicker in pediatric patients randomized to an early goal-directed fluid-sparing strategy versus usual care (SQUEEZE): study protocol for a pilot randomized controlled trial. Trials. 2016;17(1):556. doi: 10.1186/s13063-016-1689-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klassen TP, Hartling L, Craig JC, Offringa M. Children are not just small adults: the urgent need for high-quality trial evidence in children. PLoS Med. 2008;5(8):e172. doi: 10.1371/journal.pmed.0050172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cramer K, Wiebe N, Moyer V, et al. Children in reviews: methodological issues in child-relevant evidence syntheses. BMC Pediatr. 2005;5:38. doi: 10.1186/1471-2431-5-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Field MJ, Behrman RE, eds; Institute of Medicine (US) Committee on Clinical Research Involving Children . Summary. In: Ethical Conduct of Clinical Research Involving Children. National Academies Press; 2004:1-24. [PubMed] [Google Scholar]
- 14.Li PTS, Goodman DC, Guttmann A. Medical practice variations in pediatric care. In: Johnson A, Stukel T, eds. Medical Practice Variations. Springer; 2016:123-140. Sobolev B, ed. Health Services Research. doi: 10.1007/978-1-4899-7603-1_75 [DOI] [Google Scholar]
- 15.Dubois RW, Graff JS. Setting priorities for comparative effectiveness research: from assessing public health benefits to being open with the public. Health Aff (Millwood). 2011;30(12):2235-2242. doi: 10.1377/hlthaff.2011.0136 [DOI] [PubMed] [Google Scholar]
- 16.Keren R, Luan X, Localio R, et al. ; Pediatric Research in Inpatient Settings (PRIS) Network . Prioritization of comparative effectiveness research topics in hospital pediatrics. Arch Pediatr Adolesc Med. 2012;166(12):1155-1164. doi: 10.1001/archpediatrics.2012.1266 [DOI] [PubMed] [Google Scholar]
- 17.Leyenaar JK, Ralston SL, Shieh MS, Pekow PS, Mangione-Smith R, Lindenauer PK. Epidemiology of pediatric hospitalizations at general hospitals and freestanding children’s hospitals in the United States. J Hosp Med. 2016;11(11):743-749. doi: 10.1002/jhm.2624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gill PJ, Anwar MR, Thavam T, et al. ; Pediatric Research in Inpatient Setting (PRIS) Network . Identifying conditions with high prevalence, cost, and variation in cost in US children’s hospitals. JAMA Netw Open. 2021;4(7):e2117816. doi: 10.1001/jamanetworkopen.2021.17816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Connors C, Millar WJ. Changes in children’s hospital use. Health Rep. 1999;11(2):9-19. [PubMed] [Google Scholar]
- 20.To T, Guttmann A, Dick P. Inpatient and day surgery use by children in Ontario. Institute for Clinical Evaluative Sciences; 2001. Accessed March 2, 2021. https://www.ices.on.ca/flip-publication/inpatient-day-surgery-use-by-children/files/assets/basic-html/index.html#1
- 21.Statistics Canada . Population estimates, quarterly. table 17-10-0009-01. Statistics Canada; 2021. Accessed July 2, 2021. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000901
- 22.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453-1457. doi: 10.1016/S0140-6736(07)61602-X [DOI] [PubMed] [Google Scholar]
- 23.Gershon AS, Mecredy G, Ratnasingham S. Chronic obstructive pulmonary disease in Ontario, 1996/97. to 2014/15. ICES; October 2017. Accessed March 1, 2021. https://www.ices.on.ca/Publications/Atlases-and-Reports/2017/COPD
- 24.Ministry of Finance . Population estimates, 2011-2013, and projections, 2014-2041, for local health integration networks. Ministry of Finance; 2015. Accessed February 21, 2021. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710008801
- 25.Gill PJ, Anwar MR, Thavam T, Hall M, Rodean J, Mahant S. Pediatric clinical classification system for use in inpatient settings. JAMA Pediatr. 2021;175(5):525-527. doi: 10.1001/jamapediatrics.2020.6007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wodchis WP, Bushmeneva K, Nikitovic M, McKillop I. Guidelines on person-level cost using administrative databases in Ontario. Health System Performance Research Network; May 2013. Accessed February 1, 2021. https://tspace.library.utoronto.ca/bitstream/1807/87373/1/Wodchis%20et%20al_2013_Guidelines%20on%20Person-Level%20Costing.pdf
- 27.Kralj B. Measuring Rurality—RIO 2008_BASIC: Methodology and Results. Ontario Medical Association Economics Department; 2009. Accessed March 3, 2021. https://www.worldcat.org/title/measuring-rurality-rio-2008basic-methodology-and-results/oclc/852804297
- 28.Glazier RH, Zagorski BM, Rayner J. Comparison of primary care models in Ontario by demographics, case mix and emergency department use, 2008/09. to 2009/10. ICES investigative report. Institute for Clinical Evaluative Sciences; March 2012. Accessed March 7, 2021. https://www.ices.on.ca/flip-publication/comparison-of-primary-care-models-in-ontario-by-demographics/files/assets/basic-html/index.html#2
- 29.Peltz A, Hall M, Rubin DM, et al. Hospital utilization among children with the highest annual inpatient cost. Pediatrics. 2016;137(2):e20151829. doi: 10.1542/peds.2015-1829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Berry JG, Hall DE, Kuo DZ, et al. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children’s hospitals. JAMA. 2011;305(7):682-690. doi: 10.1001/jama.2011.122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Canadian Institute for Health Information . Children and youth with medical complexity in Canada—methodology notes. Canadian Institute for Health Information; 2020. Accessed March 9, 2021. https://www.cihi.ca/sites/default/files/document/children-youth-with-medical-complexity-report-en.pdf
- 32.Matheson FI, Moloney G, van Ingen T. 2016 Ontario marginalization index: user guide. St Michael’s Hospital and Public Health Ontario; October 2018. Accessed March 5, 2021. https://www.publichealthontario.ca/-/media/documents/O/2017/on-marg-userguide.pdf
- 33.Matheson FI, Dunn JR, Smith KLW, Moineddin R, Glazier RH. Development of the Canadian marginalization index: a new tool for the study of inequality. Can J Public Health. 2012;103(8)(suppl 2):S12-S16. doi: 10.1007/BF03403823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tieder JS, McLeod L, Keren R, et al. ; Pediatric Research in Inpatient Settings Network . Variation in resource use and readmission for diabetic ketoacidosis in children’s hospitals. Pediatrics. 2013;132(2):229-236. doi: 10.1542/peds.2013-0359 [DOI] [PubMed] [Google Scholar]
- 35.Cameron DB, Graham DA, Milliren CE, et al. Quantifying the burden of interhospital cost variation in pediatric surgery: implications for the prioritization of comparative effectiveness research. JAMA Pediatr. 2017;171(2):e163926. doi: 10.1001/jamapediatrics.2016.3926 [DOI] [PubMed] [Google Scholar]
- 36.Jonas JA, Shah SS, Zaniletti I, et al. Regional variation in standardized costs of care at children’s hospitals. J Hosp Med. 2017;12(10):818-825. doi: 10.12788/jhm.2829 [DOI] [PubMed] [Google Scholar]
- 37.Bujang MA, Baharum N. A simplified guide to determination of sample size requirements for estimating the value of intraclass correlation coefficient: a review. Arch Orofac Sci. 2017;12(1):1-11. [Google Scholar]
- 38.James Lind Alliance . Paediatric hospital care (Canada). James Lind Alliance; 2021. Accessed May 6, 2021. https://www.jla.nihr.ac.uk/priority-setting-partnerships/paediatric-hospital-care-canada/
- 39.Ridic G, Gleason S, Ridic O. Comparisons of health care systems in the United States, Germany and Canada. Mater Sociomed. 2012;24(2):112-120. doi: 10.5455/msm.2012.24.112-120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Canadian Institute for Health Information . Inpatient hospitalization, surgery and newborn statistics, 2019–2020. Canadian Institute for Health Information. April 29, 2021. Accessed March 3, 2021. https://secure.cihi.ca/estore/productFamily.htm?pf=PFC4562&lang=en&media=0
- 41.Canadian Institute for Health Information . Child and youth mental health in Canada—infographic. Canadian Institute for Health Information; 2020. Accessed July 15, 2021. https://www.cihi.ca/en/child-and-youth-mental-health-in-canada-infographic
- 42.Moroz N, Moroz I, D’Angelo MS. Mental health services in Canada: barriers and cost-effective solutions to increase access. Healthc Manage Forum. 2020;33(6):282-287. doi: 10.1177/0840470420933911 [DOI] [PubMed] [Google Scholar]
- 43.Cairney J, Gandhi S, Guttmann A, et al. ; MHASEF Research Team. The mental health of children and youth in Ontario: a baseline scorecard. Institute for Clinical Evaluative Sciences; March 2015. Accessed September 21, 2021. https://www.ices.on.ca/flip-publication/MHASEF_Report_2015/files/assets/basic-html/index.html#1
- 44.Children’s Mental Health Ontario . Kids can’t wait: 2020 report on wait lists and wait times for child and youth mental health care in Ontario. Children’s Mental Health Ontario; 2020. Accessed July 2021. https://cmho.org/wp-content/uploads/CMHO-Report-WaitTimes-2020.pdf
- 45.Canadian Mental Health Association . Mental health in the balance: ending the health care disparity in Canada. Canadian Mental Health Association; September 2018. Accessed July 15, 2021. https://cmha.ca/wp-content/uploads/2021/07/CMHA-Parity-Paper-Full-Report-EN.pdf
- 46.Mental Health and Addictions Program Framework Research Team . Mental health and addictions system performance in Ontario: 2021 scorecard: chart pack. ICES; 2021. Accessed September 21, 2021. https://www.ices.on.ca/Publications/Atlases-and-Reports/2021/Mental-Health-and-Addictions-System-Performance-in-Ontario-2021-Scorecard
- 47.Canadian Institute for Health Information . Too early, too small: a profile of small babies across Canada. Canadian Institute for Health Information; 2009. Accessed June 21, 2021. https://secure.cihi.ca/free_products/too_early_too_small_en.pdf
- 48.Battin MR, Knight DB, Kuschel CA, Howie RN. Improvement in mortality of very low birthweight infants and the changing pattern of neonatal mortality: the 50-year experience of one perinatal centre. J Paediatr Child Health. 2012;48(7):596-599. doi: 10.1111/j.1440-1754.2012.02425.x [DOI] [PubMed] [Google Scholar]
- 49.Rennie JM, Bokhari SA. Recent advances in neonatology. Arch Dis Child Fetal Neonatal Ed. 1999;81(1):F1-F4. doi: 10.1136/fn.81.1.F1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cohen E, Friedman JN, Mahant S, Adams S, Jovcevska V, Rosenbaum P. The impact of a complex care clinic in a children’s hospital. Child Care Health Dev. 2010;36(4):574-582. doi: 10.1111/j.1365-2214.2009.01069.x [DOI] [PubMed] [Google Scholar]
- 51.Skarsgard ED. Recommendations for surgical safety checklist use in Canadian children’s hospitals. Can J Surg. 2016;59(3):161-166. doi: 10.1503/cjs.016715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Principi T, Fraser DD, Morrison GC, et al. Complications of mechanical ventilation in the pediatric population. Pediatr Pulmonol. 2011;46(5):452-457. doi: 10.1002/ppul.21389 [DOI] [PubMed] [Google Scholar]
- 53.McDaniel CE, Jennings R, Schroeder AR, Paciorkowski N, Hofmann M, Leyenaar J. Aligning inpatient pediatric research with settings of care: a call to action. Pediatrics. 2019;143(5):20182648. doi: 10.1542/peds.2018-2648 [DOI] [PubMed] [Google Scholar]
- 54.Canadian Institute for Health Information . Patient cost estimator: methodological notes and glossary. Canadian Institute for Health Information; 2020. Accessed September 21, 2021. https://www.cihi.ca/sites/default/files/document/pce-methodology-notes-2020-en-web.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. Flow Diagram of Cohort Construction
eTable 1. Top 10 ICD-10-CA Most Responsible Diagnosis Codes That Led to Hospital Encounters for Each Nonspecific Pediatric Condition Identified in Children With Inpatient Encounters (From Table 2) in Ontario, 2014-2019
eTable 2. Variation in Cost per Encounter Across General Hospitals for the 25 Conditions With the Highest Cumulative Cost Among Children in Ontario, 2014-2019
eTable 3. Volume and Cost of Inpatient Encounters in Pediatric Hospitals and General Hospitals, 2014-2019
eTable 4. Prevalence and Cost of the 25 Most Costly and 25 Most Prevalent Conditions Among Children With Inpatient Encounters in Pediatric Hospitals in Ontario, 2014-2019
eTable 5. Prevalence and Cost for the 25 Most Costly and 25 Most Prevalent Conditions Among Children With Inpatient Encounters in General Hospitals in Ontario, 2014-2019