Abstract
Objective
To evaluate whether the initiation of JOTTIE, a one day simulation training course focussed on the management of common obstetric emergencies, was associated with a reduction in the morbidity and mortality associated with postpartum haemorrhage (PPH) at the University Hospital of the West Indies (UHWI).
Study Design
We conducted a retrospective comparative study that evaluated the incidence of multiple outcomes related to maternal morbidity secondary to PPH, during the two year period immediately prior to the introduction of JOTTIE (pre course arm, N = 88) or the two year period, one year post introduction (post course arm, N = 103) for all women who had vaginal deliveries complicated by PPH at UHWI. A relationship was said to be statistically significant if p < 0.05. Additionally, the study examined risk factors in relation to severity of haemorrhage.
Results
Genital tract trauma represented the highest recorded cause of PPH (approximately 71%). The data revealed that patients in the pre training arm were similarly likely to have no adverse outcome in comparison to patients in the post training arm (p = 0.962). There was also no statistically significant relationship between the time period of patient exposure in relation to the JOTTIE course and severity of PPH (p > 0.05). Uterine fibroids and Crohn’s disease were the only co-morbidities found to increase the likelihood of severe PPH, at 5.154 times (p = 0.019,OR = 5.154, CI = 1.314-20.212) and 17.848 times (p = 0.085,OR = 17.848,CI = 0.672-474.365), respectively.
Conclusions
This study suggests that prior to the introduction of the JOTTIE the rate of maternal morbidity associated with PPH was relatively low at UHWI and there was no significant effect on its management or a significant reduction in maternal morbidity since introduction of the course. Future research on the morbidity related to the other obstetric emergencies addressed at JOTTIE is needed in order to assess the effect of the course as a whole.
Introduction
Background
Jamaica core Obstetric Teaching and Training in Emergencies (JOTTIE) is a one-day simulation training course held biannually at The University of the West Indies (UWI), with an aim of reducing maternal and perinatal morbidity and improving the overall standard of obstetric care at UHWI and ultimately the country of Jamaica. JOTTIE was adapted from the Scottish Core Obstetric Teaching and Training in Emergencies (SCOTTIE) course, which is a skills-based course developed and delivered by the Scottish Multi-professional Maternity Development Programme (SMMD). It was developed to enhance the knowledge and skills of labour ward staff in their management of common obstetric emergencies, using simulation training and drills. Since its inception in March 2016, the course has run biannually, with a total of 6 cycles to date and 122 multi-professionals trained thus far. The course curriculum encompasses management of PPH, sepsis, preeclampsia, shoulder dystocia, breech delivery, neonatal resuscitation, recognition of the sick woman and basic life support specific to the pregnant patient. The participant doctors, nurses and midwives; hail from 4 disciplines, including: obstetrics and gynaecology, paediatrics, emergency medicine and anaesthesia.
Perinatal statistics are global health indicators and are considered to be representative of the health status of a nation 1 . “The Millennium Development Goals 4 and 5 called for the reduction of under-five mortality rates (which include neonatal deaths) and maternal mortality ratios by three-quarters by the year 2015.” 5 Jamaica’s maternal mortality rate stood at 94 per 100,000 live births as at 2018, and therefore was unsuccessful in accomplishing the target of 27.5/100,000 2 . In 2014 PPH was estimated as the cause of 18% of maternal deaths in Jamaica 22 . The JOTTIE course was introduced with the aim of improving Jamaica’s maternal and perinatal statistics and the overall standard of obstetric care at UHWI, and by extension the medical region and ultimately the country of Jamaica.
A substantial amount of literature exists surrounding simulation training for obstetrics, from both the developed and developing world .Simulation training has been shown in multiple studies to be effective in increasing knowledge and skills11,13,18,24,25, teamwork performance 15,16,18, and is acceptable to most health care professionals 11,13,18. Nevertheless, data on patient outcomes after clinical training programs are limited, especially in low resource settings, 6,7,9,12,16–18 and this study adds to the limited body of evidence related to PPH outcomes post simulation training; none of which were based in the English-speaking Caribbean. Table 1.
Table 1.
Demographic characteristics of patients.
| CHARACTERISTIC | FREQUENCY | PERCENT |
|---|---|---|
| Marital Status Single |
90 | 47.6 |
| Married/Common Law | 99 | 52.4 |
| Total | 189 | 100.0 |
| Employment Status | ||
| Employed | 142 | 74.3 |
| Unemployed | 37 | 19.7 |
| Self-Employed | 9 | 4.8 |
| Total | 188 | 100.0 |
| Educational level | ||
| Primary | 3 | 1.9 |
| Secondary | 61 | 39.1 |
| Tertiary | 90 | 59 |
| Total | 156 | 100 |
| Age Group (years) Ages 15 to 19 |
5 | 2.6 |
| Ages 20 to 25 | 54 | 29.3 |
| Ages 26 to 34 | 96 | 50.3 |
| Ages 35 and over | 36 | 18.8 |
| Total | 191 | 100.0 |
| Parity Nulliparous |
111 | 58.1 |
| Para 1 | 57 | 29.8 |
| Para 2 or more | 23 | 12.1 |
| Grand-multiparous | 0 | 0 |
| Total | 191 | 100.0 |
Purpose and Significance
The purpose of this study was to assess the impact of this simulation training course on the maternal morbidity associated with PPH for patients who delivered at UHWI during the pre-training period of 2014 to 2015 compared to deliveries in 2017 to 2018, the period immediately one year post training. PPH was the outcome variable selected because of its significant contribution to maternal morbidity and mortality in Jamaica, and relatively high incidence which allowed for securing a feasible sample size to allow for an analysis with sufficient power. The information gleaned from this study is likely to be of interest to policy makers at various health governing institutions such as the Jamaica Ministry of Health or the Pan American Health Organization (PAHO) as well as academics with an interest in obstetrics and education. The outcomes related to the other obstetric emergencies addressed by JOTTIE may be evaluated by future research.
Hypothesis, Aims and Objectives
The hypothesis was that the implementation of JOTTIE course has had a positive impact on maternal outcomes when compared to the years prior to its introduction, resulting in benefit to the obstetric population. The aims were to determine if there was a statistically significant difference in adverse outcomes post training and whether patients with certain characteristics or co-morbidities were at greater risk for severe haemorrhage. To explore the application of conservative and advanced measures used in PPH management, pre and post training. To determine whether there is a statistically significant difference between the pre and post training arms for the rates of adverse outcomes including: blood transfusion, acute kidney injury (AKI), as defined by the 2012 Kidney Disease Improving Global Outcomes (KDIGO) guidelines, intensive care unit (ICU) admissions, hysterectomy and death.
Definition of Terms
In this study postpartum haemorrhage was defined as haemorrhage in excess of 499 mLs. There were 3 categories of haemorrhage: mild, moderate and severe, corresponding to blood loss of 500 to 999 mLs, 1000 to 1,499mLs and 1500 mLs or more, respectively.
Blood loss post-delivery was calculated by use of a graduated measuring device in which blood is collected and used for all patients in addition to fixed sized gauze pads plus visual estimation of bed linen, drapes and spillage.
Methodology
Study Design and Sampling
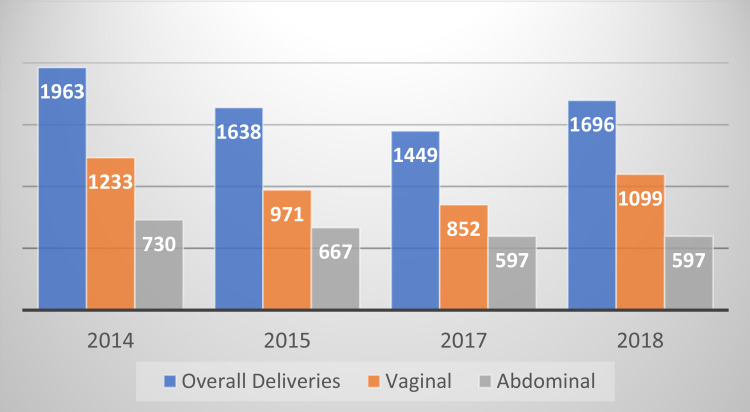
A retrospective comparative study was conducted to assess the impact of the Jamaica core Obstetric Teaching and Training in Emergencies course on PPH at UHWI. Additionally, the study examined the risk factors in relation to severity of bleeding. The sample size was calculated on the assumption that incidence of PPH was approximately 10% and in order to show a 70% reduction to 3%, a two group continuity corrected χ2 test with a 0.050 two-sided significance level would have 80% power to detect the difference between a Group 1 proportion, π1, of 0.050 and a Group 2 proportion, π2, of 0.015 (odds ratio of 0.289) when the sample size in each group is 72. The number of deliveries at UHWI for the years 2014, 2015, 2017 and 2018 were: 1,963, 1,638, 1449 and 1696 respectively 23 . 65% of these deliveries were by the vaginal route.
Patients who delivered neonates during the period January first 2014 to December 31st 2015 were exposed to labour ward staff who did not receive Jamaica core Obstetric Teaching and Training in Emergencies while patients who delivered during the period January first 2017 to December 31st 2018 were exposed to staff who received Jamaica core Obstetric Teaching and Training in Emergencies. Data was collected over a 3 month period from January 2019 to April 2019. Cases of PPH that complicated vaginal deliveries were identified using the details in the UHWI labour and delivery records, docket reviews were then carried out for all identified cases in order to further abstract data related to their management and outcomes.
Study Population
The study population consisted of mothers who delivered vaginally at the UHWI between the years 2014 to 2015, representing the period immediately prior to the introduction of JOTTIE, and 2017 to 2018, the period one year post its introduction, as a greater cohort of staff would have been trained after 2 cycles of the course had been offered. Patients who did not deliver at UHWI, delivered during the year of 2016, when the course was launched, delivered by caesarean section, or appeared in both arms of the study, were excluded. Two hundred and fifty eight (258) patients who had vaginal deliveries and were diagnosed with PPH during the periods January first 2014 to December 31st 2015 (pre course arm, N = 120); and January first 2017-December 31, 2018 (post course arm, N = 138), were identified using labour and delivery records. 67 cases that satisfied the inclusion criteria but whose records could not be found or had insufficient documentation of the events surrounding the management of PPH, were also excluded, reducing our sample to one hundred and ninety-one (191) patients; pre course arm, N = 88 and post course arm, N = 103.
Ethical Considerations
The study was considered low risk and the research protocol was approved by the UWI ethical review board and institutional permission from UHWI for access to patient records was also sought via the appropriate channels and was granted. The utmost care was taken to ensure patient anonymity and confidentiality while the data was being collected during docket reviews and statistical analysis, by identifying patients only by study number and only storing data, which was only accessible to the researchers, for the duration of time needed to analyse it. Some of the researchers make up a part of the team of trainers and organizers of the JOTTIE course, who aided in the design of the study and the selection of the outcome parameters to be evaluated. These individuals had no role in collection or analysis of data to remove potential researcher bias or bias in presentation of results.
Statistical Methods
Microsoft Excel 2016 was used to generate figures in the descriptive statistics. The two main inferential statistical methods used were the Pearson’s Chi-Square Test and the Binary Logistic Regression. A relationship was said to be statistically significant if p < 0.05. Patients’ age group were recoded into 4 age group categories: 15 to 19 years, 20 to 25 years, 26 to 34 years and 35 years and over. A patient outcome index was created using the following binary variables: transfusion of blood products, hysterectomy, AKI, ICU admissions and death. The minimum and maximum score a patient could receive were 0 and 5 respectively. Patients who scored 0 were categorised as having no adverse outcome while patients with a score of 1 or more were categorised as having an adverse outcome.
Additionally, the severity of blood loss variable was coded into 3 categories: Mild, moderate and severe. Furthermore, a method of treatment score was created using first-line and second-line conservative measures transformed into binary variables: oxytocin infusion, Methergine ®, catheterisation/voiding, misoprostol, tranexamic acid, Duratocin ® and bimanual compression. Patients who scored 0 were categorised as not using a conservative method while patients who score 1 or more were categorised as using a conservative method. Similarly, an advanced method of treatment score was created using the following binary variables: balloon tamponade, uterine packing, B-Lynch suture, uterine artery embolization, and uterine artery ligation. Patients who score 0 suggests that that the doctors did not use any advanced methods while patients who had a score of 1 or more suggested that doctors used advanced methods to arrest bleeding. Conservative methods of treatment were categorised as such based on whether a first year resident would be able to apply them, if not the method was categorised as advanced.
Results
Descriptive Statistics
The sample consisted of 191 patients who delivered at UHWI that had PPH during the periods 2014 to 2015 and 2017 to 2018. Of the study participants 96.32% received antenatal care at UHWI. Approximately, 52% of the women sampled were either married or in common-law unions. Majority of the women (approximately 79%) were employed. Almost 60% of the sample had tertiary level education. The average age of the sample was 29.10 years ± SD 5.67. The minimum and maximum age of the sample were 15 and 44 years respectively. Females within the 15 to 19 age group reported the smallest proportion sampled (approximately 2.6%) while half of the sample were between the ages of 26 to 35 years. Approximately 58.1% of patients were nulliparous, 29.8% were para 1, and 12.1% were para 2 or greater. There were no grand multiparous patients (para 5 or greater) represented in the study. The majority of patients delivered at 37 weeks and beyond, approximately 91.1%.
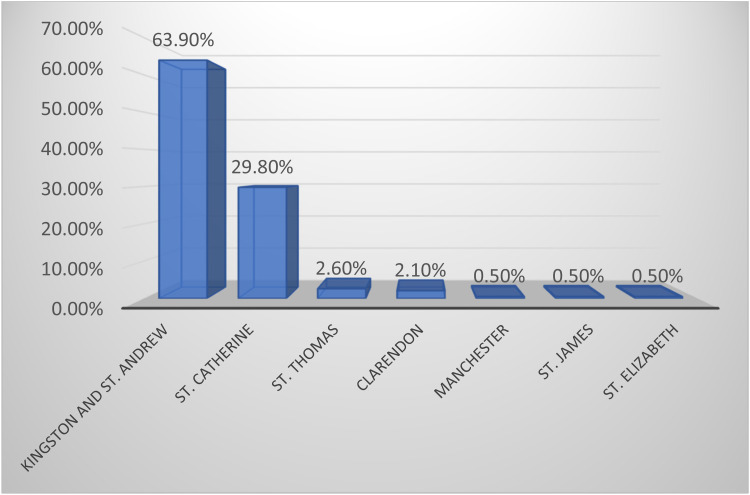
Figure 1 reveals that majority of the patients sampled resided in the corporate area (approximately 64%). Approximately 30% of the sample resided in the parish of St. Catherine. The proportions of residents who lived further way from Kingston were less than 3% and no patients were found to reside in the parishes of Hanover, Westmoreland, St. Ann, Portland and Trelawny.
Figure 1.
Residence of patients sampled.
Figure 2 represents the total number of deliveries at UHWI for 2014, 2015, 2017 and 2018, which was 1,963, 1,638, 1449 and 1696 respectively. The total number of vaginal deliveries across the period of study were: 1,233, 971, 852 and 1,099, respectively.
Figure 2.
Data regarding total deliveries at UHWI and route by year of study.
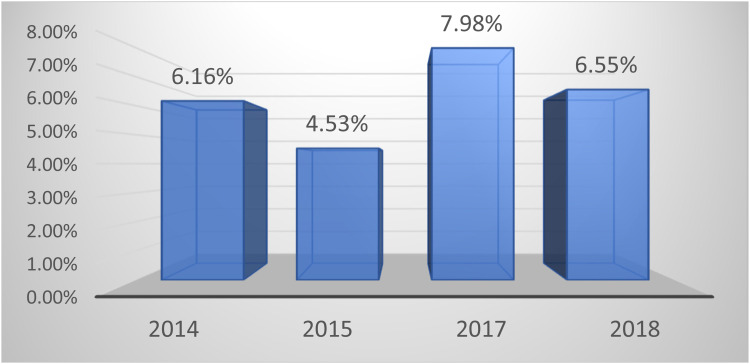
Figure 3 represents the gross incidence of postpartum haemorrhage for patients who had vaginal deliveries which was calculated for all years of study, prior to the application of exclusion criteria: 2014 = 6.16% (N = 76), 2015 = 4.53% (N = 44), 2017 = 7.98% (N = 68), 2018 = 6.55% (N = 72).
Figure 3.
Incidence of postpartum haemorrhage arising from vaginal deliveries by year.
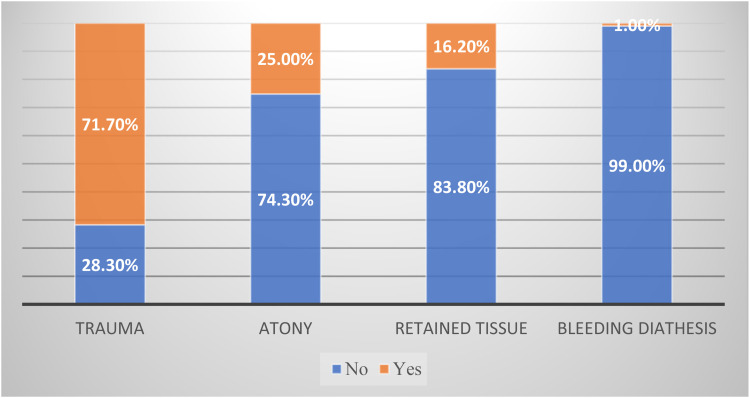
Figure 4 reveals that trauma (approximately 71%) and atony (25%) were the highest proportion of recorded causes of PPH while retained tissue (approximately 16%) and bleeding diatheses (1%) were the least recorded causes of PPH.
Figure 4.
Causes of postpartum haemorrhage.
The medical comorbidities of patients were recorded and asthma (approximately 12%), anaemia (approximately 6.8%) and hypertension (approximately 5.8%) represented the most common chronic illnesses encountered. Pregnancy induced hypertension (approximately 8.9%) and gestational diabetes (approximately 7.9%) represented the most commonly encountered pregnancy related illnesses. The frequency and percentages of all medical comorbidities in the study are represented in Table 2 below.
Table 2.
Distribution of comorbidities and parameters of obstetric significance among patients.
| CHARACTERISTIC | FREQUENCY | PERCENT |
|---|---|---|
| Chronic Illnesses Anaemia |
13 | 6.8 |
| Asthma | 23 | 12.0 |
| Crohn's Disease* | 2 | 1.0 |
| Diabetes | ||
| Endometriosis | 1 | 0.5 |
| Epilepsy | 2 | 1.0 |
| Human Immunodeficiency Virus | 0 | 0 |
| Hypercholesterolemia | 1 | 0.5 |
| Hypertension | 11 | 5.8 |
| Hyperthyroidism | 1 | 0.5 |
| Idiopathic Thrombocytopenic Purpura | 1 | 0.5 |
| Obesity | 2 | 1.0 |
| Polycystic Ovarian Syndrome | 5 | 2.6 |
| Rheumatic Heart Disease | 1 | 0.5 |
| Sickle Cell Disease | 2 | 1.0 |
| Pregnancy Related Illnesses Pregnancy Induced Hypertension |
17 | 8.9 |
| Preeclampsia | 8 | 4.2 |
| Eclampsia | 0 | 0 |
| Gestational Diabetes | 15 | 7.9 |
| Autoimmune Diseases Antiphospholipid Antibody Syndrome |
1 | 0.5 |
| Polymyositis | 2 | 1.0 |
| Systemic Lupus Erythematosus | 1 | 0.5 |
| Undifferentiated Connective Tissue Disease | 1 | 0.5 |
| Structural Abnormalities Uterine Fibroids* |
5 | 2.6 |
| Cervical Insuffiency | 13 | 6.8 |
| Characteristics of Obstetric Significance Rhesus negative |
16 | 8.4 |
| Miscellaneous Pituitary Apoplexy/Pituitary Mass |
2 | 1.0 |
Inferential Statistics
Table 3 reveals that there exists statistically significant relationship between patients with PPH having any medical comorbidity and severity of blood loss,(p < 0.05). Patients with PPH who were found to have a medical condition were more likely to experience moderate and severe bleeding in comparison to patients with PPH without any medical condition. In contrast, patients with PPH with no medical condition are more likely to experience mild blood loss in comparison to those with a medical condition.
Table 3.
Cross tabulation between blood loss versus patients having any medical comorbidity.
| SEVERITY OF HAEMORRHAGE | PATIENTS HAVE ANY MEDICAL COMORBIDITIES | ||
|---|---|---|---|
| NO | YES | P | |
| Mild | 88.0(73) | 71.3(77) | 0.020 |
| Moderate | 8.4(7) | 18.5(20) | |
| Severe | 3.6(3) | 10.2(11) | |
| Total | 100.0(83) | 100.0(108) | |
Statistical significance was not achieved in assessing the relationship between patient outcome and time of training, (p > 0.05). The data revealed that patients who were exposed to labour ward staff during the pre-JOTTIE era similarly likely to have no adverse outcome in comparison to patients who were exposed post- JOTTIE. Table 4 illustrates approximately 92% of women who were exposed to doctors during the pre-training who had PPH had no adverse outcome while approximately 92% of women who delivered at the hospital post training had no adverse outcome.
Table 4.
Statistical analysis of measured outcomes Pre & post JOTTIE training.
| CHARACTERISTIC | PRE-JOTTIE | POST-JOTTIE | P-VALUE |
|---|---|---|---|
Adverse Outcome n (%)
|
81 (92) 7 (8) |
95 (92.2) 8 (7.8) |
0.962 |
Severity of haemorrhage n (%)
|
67 (76.1) 16 (18.2) 5 (5.7) |
83 (80.6) 11 (10.7) 9 (8.7) |
0.271 |
Basic Conservative methods to treat PPH n(%)
|
15 (17) 73 (83) |
14 (13.6) 89 (86.4) |
0.507 |
Type of basic method used to treat PPH n (%)
|
34 (46.6) 62 (84.9) 21 (28.8) 6 (8.2) 1 (1.4) 2 (2.7) 0 (0) |
42 (47.2) 78 (87.6) 35 (39.3) 0 (0) 1 (1.1) 1 (1.1) 0 (0) |
|
Advanced methods used to treat PPH n (%)
|
1 (1.1) 87 (98.9) |
4 (3.9) 99 (96.1) |
0.236 |
Type of Advanced methods to treat PPH n (%)
|
1 0 0 0 0 |
4 0 0 0 0 |
|
Transfusion of patient n (%)
|
7 (8) 81 (92) |
8 (7.8) 95 (92.2) |
0.962 |
There exists no real statistically significant relationship between time of patient exposure to doctors’ training and severity of patients’ bleeding, (p > 0.05). The data reveals that approximately 76% of patients who were exposed to doctors who did not receive the Jamaica core Obstetric Teaching and Training in Emergencies were similarly likely to have mild bleeding in comparison to patients exposed to doctors who received Jamaica core Obstetric Teaching and Training in Emergencies. Table 5.
Table 5.
Spss output of binary logistic regression on patient experiencing severe bleeding in relation to maternal age, fibroids and crohn’s disease.
| VARIABLES IN THE EQUATION | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| B | S.E. | WALD | DF | SIG. | EXP(B) | 95% C.I.FOR EXP(B) | |||
| LOWER | UPPER | ||||||||
| Step 1 a | Ages 15 to 19 | 1.999 | 1.336 | 2.240 | 1 | .135 | 7.384 | .538 | 101.277 |
| Ages 26 to 34 | -.531 | .964 | .303 | 1 | .582 | .588 | .089 | 3.890 | |
| Ages 35 to 44 | 1.538 | .865 | 3.165 | 1 | .075 | 4.656 | .855 | 25.345 | |
| Fibroids | 1.640 | .697 | 5.531 | 1 | .019 | 5.154 | 1.314 | 20.212 | |
| Crohn’s Disease | 2.882 | 1.674 | 2.965 | 1 | .085 | 17.848 | .672 | 474.365 | |
| Constant | -3.386 | .731 | 21.429 | 1 | .000 | .034 | |||
Variable(s) entered on step 1: first_age_cat, third_age_cat, fourth_age_cat, fibroids, Crohn’s_ Disease.
The data revealed that patients in the 15 to 19 and 26 to 34 age groups in comparison to patients in the 20 to 25 age group were similarly likely to experience severe bleeding,(p > 0.05). Marginal significance was found in comparing patients in the oldest age group category (ages 35-44) to patients in the 20 to 25 age group category in relation to experience with severe bleeding (p = 0.075). Patients 35 and older were 4.7 times more likely to experience severe bleeding in comparison to their counterparts in the 20 to 25 age group, (p = 0.075, OR = 4.656, CI = 0.855-25.345). Additionally, patients with Crohn’s disease were 17.848 times more likely to experience severe bleeding than patients without this disease (p = 0.085,OR = 17.848,CI = 0.672-474.365). Patients with fibroids were 5.154 times more likely to experience severe bleeding in comparison to patients that do not have fibroids (p = 0.0.19,OR = 5.154,CI = 1.314-20.212).
Statistical significance was not achieved when assessing the relationship between patients’ history of PPH and severity of blood loss, (p > 0.05). Table 6 reveals that patients with a history of PPH were similarly likely to experience mild blood loss. Approximately 92% of patients with a history of PPH had mild blood loss in comparison to 84% of patients without a history of PPH who had mild blood loss.
Table 6.
Cross tabulation between severity of blood loss versus history of PPH.
| SEVERITY OF PATIENTS’ BLEEDING | PATIENTS HAVE HISTORY OF PPH | ||
|---|---|---|---|
| NO | YES | P | |
| Mild | 91.7 (11) | 84.2 (32) | 0.304 |
| Moderate | 0.0 (0) | 13.2 (5) | |
| Severe | 8.3 (1) | 2.6(1) | |
| Total | 100.0 (12) | 100.0 (38) | |
Table 4 illustrates that that labour ward staff in the pre and post training categories were similarly likely to use basic conservative methods to arrest haemorrhage in patients with PPH, (p > 0.05). Prior to training 83% of staff used conservative methods on patients with PPH to stop bleeding, in comparison to approximately 86% post training.
Oxytocin had the highest proportion (approximately 85% vs. 88%) of use by the labour ward staff to arrest haemorrhage in patients with PPH prior to training and post training respectively. Additionally, catheterisation/voiding (approximately 47% vs. 47%) had the second largest proportion in use by the staff pre and post training to stop patients with PPH from bleeding. (see Table 4) Misoprostol (approximately 29% vs. 39%) recorded the third largest proportion of conservative methods used by doctors in both pre and post-test. Tranexamic acid and Duratocin ® were the least used basic methods by doctors in the pre and post-test to arrest patient bleeding.
Majority of the doctors equally did not use advanced methods in both pre and post tests for their patients with PPH to arrest bleeding, (p > 0.05). The data revealed that approximately 99% of doctors did not use advanced methods prior to training to arrest bleeding in patients with PPH, in comparison to approximately 96% of doctors who did not use advanced methods post training.
Only the Balloon Tamponade advanced method was used by doctors to stop patients with PPH from bleeding.
Doctors in the pre-training era were as equally likely as doctors in the post training era to transfuse patients with PPH, (p > 0.05). Approximately 92% of doctors in the pre and post training group were found to equally not offer transfusion to their patients.
Table 7 revealed that types of labour was not statistically significantly related to severity of blood loss, (p > 0.05). The data revealed that at least 77% of patients who had spontaneous labour and induction reported having mild blood loss.
Table 7.
Cross tabulation between severity of blood loss and type of labour.
| TYPE OF LABOUR | |||
|---|---|---|---|
| SPONTANEOUS | INDUCED | P | |
| Severity of blood loss Mild | 77.3 (102) | 81.4 (48) | 0.805 |
| Moderate | 15.2 (20) | 11.9 (7) | |
| Severe | 7.6 (10) | 6.8 (4) | |
| Total | 100.0 (132) | 100.0 (59) | |
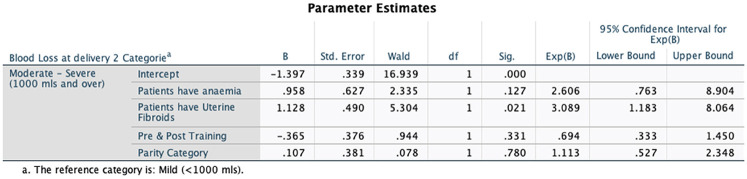
If a new classification of blood loss at delivery was used (mild <100mls and moderate to severe ≥1000 ml) as the dependent variable (outcome), and JOTTIE training as one of the independent (predictor)variables, then correcting for anaemia, parity and presence of fibroids, the only predictor of outcome that was statistically significant was the presence of fibroids (p-value 0.021) with an odds ratio of 3 (95% confidence interval of 1-8).
Discussion
The Jamaica core Obstetric Teaching and Training in Emergencies (JOTTIE) was designed in order to reinforce the knowledge and necessary skills required to manage the most common obstetric emergencies through simulation training, to empower labour ward staff to act confidently and cohesively when faced with these challenges and to reduce medical errors. Worldwide, postpartum haemorrhage (PPH) has continued to be a major cause of maternal morbidity and mortality with an estimated incidence of 10.8% 22 . In Jamaica, for the year of 2014, 18% of maternal deaths were attributed to PPH 22 .
Simulation training has been shown to be an effective method of teaching in obstetrics and has been applied across many disciplines and proven useful to various categories of health care professionals. This study was based at the University Hospital of the West Indies (UHWI), the only teaching hospital in Jamaica, wherein the number of deliveries per year ranged from 1400 to 2000 on average. Our study determined an incidence of PPH ranging from approximately 4% to 6% in the pre-training arm of the study to approximately 7% to 8% in the post-training arm. The low incidence is likely attributable to the routine use of prophylactic uterotonics (oxytocin 5 units given intramuscularly upon birth of the anterior shoulder of the foetus) 29 . The increase in PPH post training may have been attributed to labour ward staff becoming more astute at estimating blood loss post-training, enabling better recognition of PPH, hence an increase in the incidence would arise. A finding somewhat anomalous to our study was that genital tract trauma represented the most common documented cause for PPH (at approximately 71%), in contrast to atony (estimated at 25%), which is generally accepted as the leading cause of PPH 29,32. This unique finding may have been due to the labour ward staff having a higher propensity to record a traumatic event which can be confirmed visually, although the delivery may also have been complicated by atony.
The data revealed that no statistically significant difference existed for the severity of bleeding or incidence of adverse outcomes when the pre and post training groups were compared. This may have been due to a type 2 error because the incidence of postpartum haemorrhage at UHWI was slightly lower than the 10.8% that entailed in other territories and this figure was used to calculate the required sample size. Therefore the study may have been underpowered and could be repeated after more cases of PPH have arisen. A similar study by Nelissen et al evaluating the effect of simulation based training on clinical performance and patient outcome for prevention and management of PPH, also utilised a rate of 10% for sample size calculation 24 . That study also determined a lower than expected incidence of PPH, but still determined a statistically significant reduction in PPH incidence of PPH [ 24 ]. Blood transfusion was considered an adverse outcome in this study and although there was no difference in its use in both arms of the study, it would be interesting to explore whether patients managed in the post training arm were transfused at a lower threshold of blood loss, due to doctors having a better understanding of the implications or PPH and the management.
Oxytocin uptake had increased in that study and others with statistical significance24,26 but remained relatively unchanged in our study pre and post training, use of other basic conservative adjuncts used to arrest haemorrhage were not statistically significant, similar to what was found in our study. Oxytocin uptake likely increased due to its low cost and availability. It is present in all delivery suites and is therefore quickly accessible and easy to administer as an infusion. Methergine® use decreased due to it being out of stock at UHWI since 2015. Other agents such as Duratocin® and tranexamic acid are also not readily available. Misoprostol requires a doctor to administer it and is kept locked away, as it is classified as a dangerous drug due to its abortifacient properties, which remains illegal in Jamaica to date.
As it relates to the advanced conservative methods utilised to arrest bleeding during PPH, there was no statistically significant difference among the labour ward staff pre and post training, for use of advanced methods. This may be due to several reasons, namely, availability and feasibility. B-Lynch suture and uterine artery ligation require access to the abdomen by a laparotomy and are therefore more useful at caesarean section. This study focussed on vaginal delivery and therefore the incidence of these techniques are expected to be low. Uterine artery embolization requires a radiologist and is very expensive, and therefore may not always be available.
A prospective study conducted by Marshall et al in 2014, evaluated the impact of simulation training on PPH management, and determined improved response times once PPH was diagnosed [ 24 ]. Some of the management parameters assessed were: use of uterine massage, as well as medical management with use of 3 indicated medications 24 . Therefore, although the post-training arm of labour ward staff would be better skilled in the use of advanced methods, these adjuncts may not have been necessary due to faster response in instituting the management of PPH which would result in a more timely arrest of bleeding and no need for further intervention within the advanced category, such as uterine packing or intrauterine balloon insertion. Timeliness of the use of conservative measures were not assessed in this study. The inability to detect a statistically significant difference in the uptake of conservative measure may also have been a type 2 error.
The only medical comorbidities significantly associated with severe PPH were fibroids and Crohn’s disease, with approximately 5 times a greater risk and 18 times respectively. The association of both conditions with PPH has been demonstrated in other studies 30,31. Marginal significance was found in comparing patients of advanced maternal age (p = 0.075), with these patients being 4.7 times more likely to experience severe bleeding in comparison to their counterparts in the 20 to 25 age group, consistent with other studies 31 . History of PPH was not found to be statistically significant.
Has the effect of the knowledge and skills gained from JOTTIE already waned?
Participants of 1-day simulation training courses such as JOTTIE, have been shown to have a decline in knowledge after 3 months post training 8 . In contrast, for long term courses, lasting 1 to 8 weeks 6 , knowledge is often retained up to 3 years after the initial training intervention 6,7,10,11. A statistically significant outcome for reducing adverse outcomes may not have been detected simply because the knowledge gained by participants was short lived. Whether the effect of JOTTIE on the expansion of knowledge and skills regarding the management of obstetric emergencies has been sustained or has deteriorated is unknown. A similar prospective study by Lutgendorf et al, determined a statistically significant reduction in PPH up to 6 months post training 26 . However, this was likely before the expected deterioration of knowledge would occur.
The recommendation by van de Ven et al in their 2017 evaluation of simulation based team training in obstetric emergencies, was that the most cost-effective strategy, taking into account cost of administering the course and funds saved by preventing obstetric complications, is multi-professional simulation training delivered in a simulation centre with on-site repetition of the course within 6 months of its initial delivery 16 . Alwy Al-beity conducted weekly 30 to 40 minute sessions of specific scenarios for 8 weeks after the initial one day simulation course on PPH management and determined a significant reduction in long term morbidity associated with near misses 28 . Thus far none of the 122 trained personnel have experienced any such follow up training sessions post JOTTIE. This may be in order if a significant impact on the long term reduction in morbidity related to PPH is to occur 16,28. Williams et al also demonstrated that this “low dose high frequency” approach with simulators was found to be beneficial with health care providers within health centres in Uganda. [ 27 ]
Limitations of the study include the lower than expected incidence of PPH and the sample size obtained over both 2 year periods, which may have underpowered the study. Estimation of PPH is low resource settings has been plagued with poor reliability. Another limitation was the lack of electronic medical records to centrally store the necessary patient data. As a result of missing physical patient records, 65 cases were excluded from analysis. Our study was conducted retrospectively, and ideally highly powered, multi-centre, prospective cohort study should be carried out to more robustly assess the effect of the course on the management and maternal outcomes related to PPH.
Conclusion
The benefit of simulation-based training in the practice of modern obstetrics is undeniable. However, for training to remain effective against morbidity associated with obstetric emergencies, repeat sessions are necessary to persistently reinforce management strategies. Further studies, ideally prospectively, are needed to evaluate the outcomes related to the other obstetric emergencies addressed by JOTTIE, such as sepsis and shoulder dystocia, in order to assess the effect of the course as a whole. However, the incidence of these events is even lower than PPH and therefore these studies may not be forthcoming any time soon, in order to allow time to achieve an appropriate sample size. Consideration should be given to creating a registry of these obstetric emergencies at UHWI, where the details surrounding their occurrence are immediately entered into a database and stored, to facilitate future audits and analysis of outcomes with greater ease. Development of a formal PPH management protocol would be of great merit to aid in standardising the management of this potentially life-threatening obstetric emergency for all labour ward staff, ideally further reducing maternal morbidity and mortality 29 .
Acknowledgements
We would like to thank all the participants in our JOTTIE programme, the administrative staff at the University Hospital of the West Indies and particularly the team from the Scottish Core Obstetric Teaching and Training in Emergencies Course (SCOTTIE) after which the JOTTIE course was modelled.
Footnotes
Declaration of Conflicts of Interest: To the best of our knowledge we have no conflicts of interest to declare.
Funding: All costs related to this research was provided by the involved researchers.
Ethical Approval: Not applicable, because this article does not contain any studies with human or animal subjects.
Informed Consent: Not applicable, because this article does not contain any studies with human or animal subjects.
Trial Registration: Not applicable, because this article does not contain any clinical trials.
References
- 1.Larson C. Global health indicators: an overview. CMAJ. 2004;171(10):1199‐1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.[Internet]. Who.int. 2019 [cited 11 January 2019]. Available from: https://www.who.int/gho/maternal_health/countries/jam.pdf?ua = .
- 3.. UNICEF Jamaica - Early Childhood Development - Safe Motherhood Campaign [Internet]. Unicef.org. 2019 [cited 11 January 2019]. Available from: https://www.unicef.org/jamaica/early_childhood_15276.htm.
- 4.[Internet]. 2019 [cited 11 January 2019]. Available from: https://www.moh.gov.jm/programmes-policies/promac/.
- 5.Jamaica [Internet]. Health in the Americas 2017. 2019 [cited 11 January 2019]. Available from: https://www.paho.org/salud-en-las-americas-2017/?page_id = 135.
- 6.ACOG. Hypertension in pregnancy. ACOG; 2013. [Google Scholar]
- 7.Crofts J, Fox R, Draycott T, Winter C, Hunt L, Akande V. Retention of factual knowledge after practical training for intrapartum emergencies. International Journal of Gynecology & Obstetrics. 2013;123(1):81‐85. [DOI] [PubMed] [Google Scholar]
- 8.van de Ven J, Fransen A, Schuit E, van Runnard Heimel P, Mol B, Oei S. Does the effect of one-day simulation team training in obstetric emergencies decline within one year? A post-hoc analysis of a multicentre cluster randomised controlled trial. European Journal of Obstetrics & Gynecology and Reproductive Biology. Sept 2017;216:79‐84. [DOI] [PubMed] [Google Scholar]
- 9.Draycott T, Sibanda T, Owen L, et al. Does training in obstetric emergencies improve neonatal outcome? BJOG. 2006;113(2):177‐182. [DOI] [PubMed] [Google Scholar]
- 10.Draycott T, Collins K, Crofts J, et al. Myths and realities of training in obstetric emergencies. Best Practice & Research Clinical Obstetrics & Gynaecology. 2015;29(8):1067‐1076. [DOI] [PubMed] [Google Scholar]
- 11.Crofts J, Bartlett C, Ellis D, Hunt L, Fox R, Draycott T. Management of shoulder dystocia. Obstet Gynecol. 2007;110(5):1069‐1074. [DOI] [PubMed] [Google Scholar]
- 12.Fransen A, van de Ven J, Merién A, et al. Effect of obstetric team training on team performance and medical technical skills: a randomised controlled trial. BJOG: An International Journal of Obstetrics & Gynaecology. 2012;119(11):1387‐1393. [DOI] [PubMed] [Google Scholar]
- 13.To W. Training in emergency obstetric skills: is it evidence-based?. Hong Kong Medical Journal [Internet]. 2011 [cited 8 January 2019];17(2):141-6. Available from: http://www.hkmj.org/abstracts/v17n2/141.htm. [PubMed]
- 14.Cornthwaite K, Crofts J, Draycott T, Siassakos D, Winter C. Training for obstetric emergencies: PROMPT and shoulder dystocia. The Health Foundation; 2015. [Google Scholar]
- 15.Fransen A, de Boer L, Kienhorst D, Truijens S, van Runnard Heimel P, Oei S. Assessing teamwork performance in obstetrics: a systematic search and review of validated tools. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2017;216:184‐191. [DOI] [PubMed] [Google Scholar]
- 16.van de Ven J, van Baaren G, Fransen A, van Runnard Heimel P, Mol B, Oei S. Cost-effectiveness of simulation-based team training in obstetric emergencies (TOSTI study). European Journal of Obstetrics & Gynecology and Reproductive Biology. 2017;216:130‐137. [DOI] [PubMed] [Google Scholar]
- 17.Egenberg S, Masenga G, Bru L, et al. Impact of multi-professional, scenario-based training on postpartum hemorrhage in Tanzania: a quasi-experimental, pre- vs. Post-intervention study. BMC Pregnancy Childbirth 2017;17:287. 10.1186/s12884-017-1478-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Merién A, van de Ven J, Mol B, Houterman S, Oei S. Multidisciplinary team training in a simulation setting for acute obstetric emergencies. Obstet Gynecol. 2010;115(5):1021‐1031. [DOI] [PubMed] [Google Scholar]
- 19.Boet S, Bould M, Fung L, et al. Transfer of learning and patient outcome in simulated crisis resource management: a systematic review. Canadian Journal of Anesthesia/Journal canadien d'anesthésie. 2014;61(6):571‐582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dresang L, González M, Beasley J, et al. The impact of advanced life support in obstetrics (ALSO) training in low-resource countries. International Journal of Gynecology & Obstetrics. 2015;131(2):209‐215. [DOI] [PubMed] [Google Scholar]
- 21.Weiner C, Samuelson L, Collins L, Satterwhite C. 61: 5-year experience with PROMP (PRactical obstetric multidisciplinary training) reveals sustained and progressive improvements in obstetric outcomes at a US hospital. Am J Obstet Gynecol. 2014;210(1):S40. [Google Scholar]
- 22.Evans C, Johnson P, Bazant E, Bhatnagar N, Zgambo J, Khamis A. Competency-based training “helping mothers survive: bleeding after birth” for providers from central and remote facilities in three countries. International Journal of Gynecology & Obstetrics. 2014;126(3):286‐290. [DOI] [PubMed] [Google Scholar]
- 23.Thompson M, Forbes M. Perinatal Audit 2018. Presentation presented at the annual perinatal conference; 2019; The University Hospital of the West Indies [UNPUBLISHED DATA].
- 24.Marshall N, Vanderhoeven J, Eden K, Segel S, Guise J. Impact of simulation and team training on postpartum hemorrhage management in non-academic centers. J Matern Fetal Neonatal Med. 2014;28(5):495‐499. [DOI] [PubMed] [Google Scholar]
- 25.Nelissen E, Ersdal H, Mduma E, et al. Clinical performance and patient outcome after simulation-based training in prevention and management of postpartum haemorrhage: an educational intervention study in a low-resource setting. BMC Pregnancy Childbirth. 2017;17(1):301. 10.1186/s12884-017-1481-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lutgendorf M, Spalding C, Drake E, Spence D, Heaton J, Morocco K. Multidisciplinary In situ simulation-based training as a postpartum hemorrhage quality improvement project. Mil Med. 2017;182(3):e1762‐e1766. [DOI] [PubMed] [Google Scholar]
- 27.Williams E, Bazant E, Holcombe S, et al. “Practice so that the skill does not disappear”: mixed methods evaluation of simulator-based learning for midwives in Uganda. Hum Resour Health. 2019;17(1):24. 10.1186/s12960-019-0350-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Al-beity F A, Pembe A, Hirose A, et al. Effect of the competency-based helping mothers survive bleeding after birth (HMS BAB) training on maternal morbidity: a cluster-randomised trial in 20 districts in Tanzania. BMJ Global Health. 2019;4(2):e001214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sheldon W, Blum J, Vogel J, Souza J, Gülmezoglu A, Winikoff B. Postpartum haemorrhage management, risks, and maternal outcomes: findings from the world health organization multicountry survey on maternal and newborn health. BJOG: An International Journal of Obstetrics & Gynaecology. 2014;121:5‐13. [DOI] [PubMed] [Google Scholar]
- 30.Zhao R, Wang X, Zou L, et al. Adverse obstetric outcomes in pregnant women with uterine fibroids in China: a multicenter survey involving 112,403 deliveries. PLOS ONE. 2017;12(11):e0187821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Abdul Sultan A, West J, Ban L, et al. Adverse pregnancy outcomes Among women with inflammatory bowel disease. Inflamm Bowel Dis. 2016;22(7):1621‐1630. [DOI] [PubMed] [Google Scholar]
- 32.Oyelese Y, Ananth C. Postpartum hemorrhage: epidemiology, risk factors, and causes. Clin Obstet Gynecol. 2010;53(1):147‐156. [DOI] [PubMed] [Google Scholar]