Abstract
Objectives
There are few systematic assessments of mass hysteria (MH) attack rates (ARs) in adolescents and children. The study aim was to assess the ARs of MH in this population.
Methods
We used a meta-analysis to systematically review studies and assess ARs.
Results
The reviewed studies included 32,887 participants, of which 2968 were children and adolescents with a history of MH. Twenty-eight studies were included, of which 22 (78.6%) had high to moderate methodological quality. The pooled AR of MH was 9.8% (95% confidence interval [CI] 6.3, 14.0). Of MH studies between 2010 and 2020, 78.6% were conducted between 2010 and 2014. ARs were higher between 2010 and 2014 (10.3%) than between 2015 and 2020 (8.1%). Regarding population characteristics, the AR in girls was 2.43 (95% CI 1.70, 3.46) times higher than in boys. Most studies were on primary school students (46.4%), who showed the highest AR (15.4%). Of six trigger factors, water pollution showed the highest AR (16.3%). ARs were higher in rural areas (11.1%) than in urban areas (5.6%).
Conclusions
MH in children and adolescents seems prevalent and shows some epidemiological characteristics. These findings may assist governments to control and prevent MH epidemics among children and adolescents.
Keywords: Attack rate, mass hysteria, children, adolescent, prevalence, meta-analysis, water pollution
Introduction
Mass hysteria (MH) is a diagnostic term used to characterize unexplained outbreaks or epidemics of subjective somatic complaints among students or other vulnerable people that seem to have no physical, biological, or etiological causes.1–3 According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, 4 MH is the occurrence of shared psychogenic symptoms in a group of individuals in a similar environment, usually over a short time. MH is characterized by a group of symptoms that usually mimic organic disease, but with no identifiable cause. MH occurs in individuals who share a common belief that their symptoms constitute a definite illness. 5
The symptoms of MH are usually caused by stress and anxiety associated with perceived threats. 6 MH is infectious and may be a contributing and amplifying factor in real epidemics. 6 Various other descriptive terms have been used to define this condition, such as collective hysteria, stress reaction, mass psychogenic illness, epidemic hysteria and mass sociogenic illness. MH is a cause of acute illness epidemics and is a complex biopsychosocial phenomenon involving the generation of subjective somatic complaints in patients exposed to various triggers in a particular psychological and social context. 7
Recorded MH outbreaks have occurred in different sociocultural settings, such as schools, villages, homes and workplaces. MH often occurs among otherwise healthy people who suddenly believe they have been made ill by specific trigger factors.1–3,7 MH spreads through visual and auditory contact and occurs most often among adolescents or preadolescent girls. 7 MH may involve the recurrence of a reaction in which the original psychological climate is duplicated or re-established. For instance, adolescents are susceptible to proposal and influence contagion and have a substantial need for acceptance and self-affirmation because they are eager to conform to the group by sharing its beliefs and ideals. 8 Thus, MH easily recurs through duplication or re-establishment of psychological symptoms in collective settings such as schools, particularly among female adolescents. The psychosocial environment is a frequently reported trigger factor for MH; however, there may be other trigger factors, such as concerns about supernaturalism, mass vaccination, air pollution, food poisoning and religious beliefs. 9
Currently, MH in children and adolescents is a neglected social problem that is underreported; often places substantial financial burden on emergency services, public health and environmental agencies; and has a negative effect on social development and stability. 5 The literature on MH comprises mostly reports2,7–9 that rarely include an accurate assessment of the MH attack rate (AR). The aim of this meta-analysis was to assess ARs of MH in children and adolescents. The findings from this analysis will be useful in designing assessment systems for MH in this population. In this study, we addressed two questions: (1) what is the overall AR of MH in children and adolescents? (2) how does the AR of MH in children and adolescents differ according to time period, gender, trigger factors, student type and geography?
Materials and methods
Data sources and search strategies
The present meta-analysis was performed according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. 10 This was a review study and did not involve a research protocol requiring approval by a relevant institutional review board or ethics committee. Informed consent was also not applicable. The study was registered with PROSPERO (https://www.crd.york.ac.uk/prospero/#myprospero) (registration number: CRD42021257401).
We searched the PubMed, Elsevier Science Direct, Cochrane Library, Google Scholar, SpringerLink, ProQuest Dissertations, China National Knowledge Infrastructure (CNKI) and WANFANG databases for the ARs of MH in children and adolescents from 1 January 2010 to 31 October 2020. An inclusive search of each database was performed using subject headings, text words and keywords; the Boolean logic terms ‘or’ and ‘and’ were used to combine searches. A search was conducted for articles pertaining to MH in children and adolescents, using the search term ‘mass hysteria’ and other related terms (e.g., hysteria, epidemic hysteria, mass psychogenic illness, mass sociogenic illness). Studies identified using this search strategy were first screened using titles and abstracts, and then by reviewing full-text articles. Two reviewers independently selected studies using predetermined inclusion and exclusion criteria. Differences in opinion were resolved through consensus.
Study inclusion criteria
Two reviewers independently applied the following inclusion and exclusion criteria to the articles retrieved. The inclusion criteria were (1) published articles/reports; (2) observational studies; (3) investigations of MH in children and adolescents; (4) participants aged from 6 to 20 years; and (5) only Chinese and English language articles.
Study exclusion criteria
The exclusion criteria were (1) participants older than 20 years or younger than 6 years; (2) clinical studies; (3) high-risk adolescents; that is, those with first-degree relatives with hysteria, anxiety, depression or other mental illnesses (to reduce bias owing to family genetic factors); and (4) studies with substantial missing data.
Extraction of data
Data were independently extracted by two reviewers into a standardized scheme for each article on ARs of MH in children and adolescents. Any differences in data extraction between reviewers were resolved by consensus through discussion. Data were obtained directly from the reports and articles. For articles that did not explicitly state the data, data were derived from graphs, tables or charts included in the reports or data supplements. The following data were collected: title, report location, report dates, authors, literature sources, essential characteristics of participants and epidemiologic characteristics of MH in children and adolescents.
The completed extraction form for each study was sent electronically to its first author, with a request to check the accuracy and integrity of the extraction. Of the authors, 11 responded and 6 provided supplementary information11–16 that we used to modify the extracted data.
Determination of ARs
AR refers to the cumulative incidence of infection or disease in a group of people observed over time during an outbreak or an epidemic. It is calculated by dividing the number of exposed individuals who developed the disease by the total number of individuals at risk. 6 Exposed individuals are those individuals who are present in the same setting as the infected individual. ARs are measured from the beginning (the onset of illness in the index case) to the end (the first day of illness of the last person to become ill) of an epidemic.
AR meta-analysis
The primary study outcome was ARs. Therefore, we calculated a pooled AR with 95% confidence interval (CI). We also calculated ARs and 95% CIs for each study. Our secondary outcome was epidemiologic characteristics of ARs, namely, year, gender, trigger factors, geography (i.e., rural/urban), location of occurrence (i.e., China/outside China), education levels and student type (resident/nonresident).
Quality assessment
The principal author (QC) and a coauthor (XD) independently assessed the quality of the included studies using a modified version of the Critical Appraisal Skills Programme tool (CASP) (available at: http://www.casp-uk.net/). The modified CASP consists of 10 questions (available from the authors) on the credibility and relevance of studies and has been used in previous reviews of qualitative studies. 17 Each item was scored as 2 (fully met the quality criteria), 1 (partially met the quality criteria) or 0 (did not meet the quality criteria). Studies scoring in the 75th percentile or higher on quality (≥15) were categorized as high quality studies. Studies scoring between 50% and 75% were rated as moderate quality studies (11–14). Studies scoring lower than 50% were considered low quality studies (≤10).
Statistical analysis
We used the statistical software R, version i386 4.0.3 (www.r-project.org), to conduct all statistical tests and generate associated graphic results. To sum the AR findings, we computed ARs and 95% CIs using the Freeman–Tukey double arcsine transformation (FT) to stabilize the variances: let ‘event’ be the nominator and ‘n’ the denominator for the proportion, then p = event/n. If p < 0.3 or p > 0.7, the FT is given by FT = arcsine (√(n/N + 1)) + arcsine (√(n + 1/N + 1)). Heterogeneity assessments preceded all meta-analytical tests on the retrieved articles. If the sample size of at least one study is very small (<10), back transformation of the pooled effect may be misleading if the FT is used. In such cases, we used other transformations (e.g., sm = ‘PAS’ or sm = ‘PLOGIT’).
There was significant heterogeneity across the studies. Therefore, we calculated the results using a random effects model and reported corresponding p values and I2 values.
Risk of bias
The included studies and reports were based on field investigations, and therefore there was potential heterogeneity in terms of the number of individuals assessed. Owing to the extent to which cross-sectional study designs were used and the nature of the data collected, we assumed the existence of risk of bias (e.g., recall, diagnosis, reporting). We thus collected data and presented ARs based on confirmatory diagnostic criteria and quality control.
Results
Characteristics and methodological quality of included studies
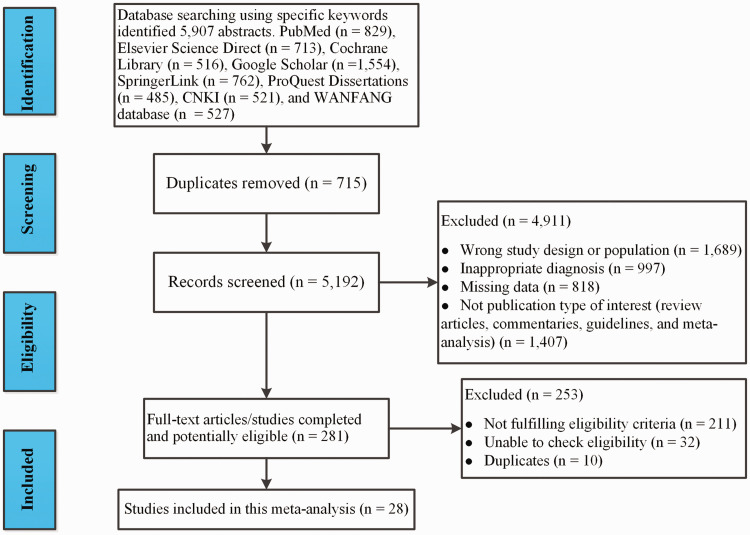
The database search produced 5907 abstracts. Twenty-eight articles11–16,18–39 met the inclusion criteria and were included in the meta-analysis (Figure 1). The characteristics of these studies (N = 32,887)11–16,18–39 were categorized and are shown in Table 1. The meta-analysis incorporated AR data from 2968 children and adolescents with a history of MH. The studies were assessed in terms of publication year, gender, location of occurrence, education level, student type, area and MH trigger factors.
Figure 1.
PRISMA flow chart of study selection.
Table 1.
Characteristics and methodical quality of included studies.
| First author (references) | Publication year | Event | N | Gender (event/n) | Location of occurrence | Education level | Student type | Area | Trigger factors | Quality score |
|---|---|---|---|---|---|---|---|---|---|---|
| Wang et al. 11 | 2012 | 24 | 105 | NA | China | PS | Nonresident | Urban | WP | 11 |
| Shang et al. 12 | 2010 | 41 | 322 | NA | China | JMS | Resident | Urban | SFP | 12 |
| Chen L et al. 13 | 2013 | 5 | 1,250 | NA | China | JMS | Nonresident | Urban | TT | 11 |
| Luo 14 | 2011 | 84 | 226 | NA | China | PS | Nonresident | Rural | MV | 10 |
| Lin et al. 15 | 2010 | 4 | 1,176 | Girls: 3/452; Boys: 1/717 | China | PS | Resident | Rural | MV | 10 |
| Zhang 16 | 2012 | 71 | 555 | NA | China | JMS | Nonresident | Rural | SFP | 12 |
| He 18 | 2010 | 37 | 395 | NA | China | HS | Resident | Urban | PE | 10 |
| Xin et al. 19 | 2011 | 3 | 600 | NA | China | JMS | Nonresident | Urban | MV | 12 |
| Chen Y et al. 20 | 2010 | 66 | 938 | NA | China | JMS | Nonresident | Rural | MV | 14 |
| Yang et al. 21 | 2012 | 29 | 1,098 | NA | China | JMS | Resident | Rural | PS | 12 |
| Li et al. 22 | 2013 | 22 | 79 | NA | China | PS | Resident | Rural | S | 13 |
| Zhang et al. 23 | 2012 | 23 | 386 | NA | China | PS | Nonresident | Rural | MC | 10 |
| Qi et al. 24 | 2013 | 41 | 193 | NA | China | PS | Resident | Rural | MV | 9 |
| Song et al. 25 | 2010 | 136 | 1,746 | Girls: 91/845; Boys: 45/901 | China | ES | Resident | Rural | SFP | 15 |
| Qin et al. 26 | 2015 | 215 | 1,850 | Girls: 98/675; Boys: 117/975 | China | JMS | Resident | Rural | WP | 16 |
| Zhou et al. 27 | 2015 | 34 | 538 | Girls: 28/293; Boys: 6/245 | China | JMS | Resident | Rural | SS | 13 |
| Ren et al. 28 | 2015 | 43 | 269 | NA | China | PS | Resident | Rural | SFP | 14 |
| Liu et al. 29 | 2014 | 902 | 1,782 | NA | China | PS | Nonresident | Rural | SFP | 10 |
| Zhu et al. 30 | 2014 | 24 | 326 | NA | China | PS | Nonresident | Rural | SFP | 15 |
| Huang et al. 31 | 2010 | 272 | 9,115 | Girls: 184/4,404; Boys: 88/4,711 | Taiwan, China | ES | Nonresident | Urban | MV | 15 |
| Al Mamun et al. 32 | 2018 | 50 | 1,054 | Girls: 39/632; Boys: 11/422 | Narsinghdi, Bangladesh | JMS | Nonresident | Rural | SS | 17 |
| Beyene et al. 33 | 2014 | 44 | 1,283 | NA | Amhara Region, Ethiopia | HS | Nonresident | Rural | S | 14 |
| Lake et al. 34 | 2016 | 32 | 1,000 | NA | Northwest Ethiopia | PS | Nonresident | Rural | S | 13 |
| Haque et al. 35 | 2013 | 98 | 1,173 | NA | Gaibandh, Bangladesh | PS | Nonresident | Rural | SFP | 15 |
| Dominus 36 | 2012 | 45 | 600 | Girls: 44/432; Boys: 1/168 | New York, USA | HS | Nonresident | Rural | PS | 14 |
| Loa Zavala 37 | 2010 | 512 | 4,000 | Girls: 512/4,000 | Mexico | HS | Resident | Rural | S | 16 |
| Poudel et al. 38 | 2020 | 47 | 435 | Girls: 37/244; Boys: 10/191 | Puythan, Nepal | PS | Nonresident | Rural | EST | 17 |
| Jie 39 | 2010 | 64 | 393 | Boys: 64/393 | China | PS | Nonresident | Rural | PS | 14 |
PS, primary school; JMS, junior middle school; HS, high school; ES, entire school; SFP, suspected food poisoning; PS, psychological suggestion; PE, physical examination; MV, mass vaccination; WP, water pollution; EST, emotional stress; S, supernaturalism; MC, mumps case; SS, stress of studying; OA, oral anthelmintic; TT, tuberculin testing; NA, not available.
The evaluation of the methodological quality of the 28 full articles reviewed by two authors (QC and XD) yielded the following results. The mean quality score was 13.0 with a standard deviation of 2.3 and a range of 9 to 17. There were 8 articles (29%)25,26,30–32,35,37,38of high quality, 14 articles (50%)11–13,16,19–22,27,28,33,34,36,39 of moderate quality and 6 articles (21%)14,15,18,23,24,29 of low quality (See Table 1 for quality scores of the studies).
ARs of MH for children and adolescents
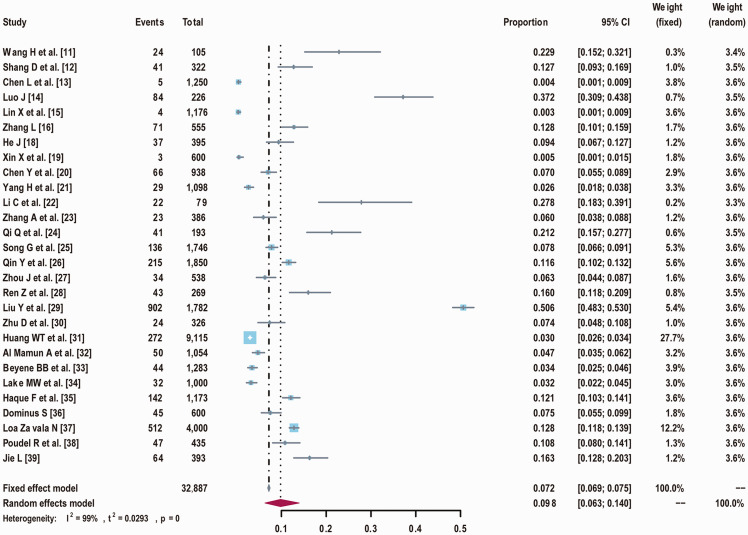
There was statistical heterogeneity (I2 = 99.0%) among the 28 studies.11–16,18–39 A random effects meta-analysis model was used. The results showed that the total AR of MH was 9.8% (95% CI 6.3, 14.0, p < 0.001) for children and adolescents (Figure 2).
Figure 2.
Forest plot for pooled attack rates of mass hysteria in children and adolescents.
CI, confidence interval.
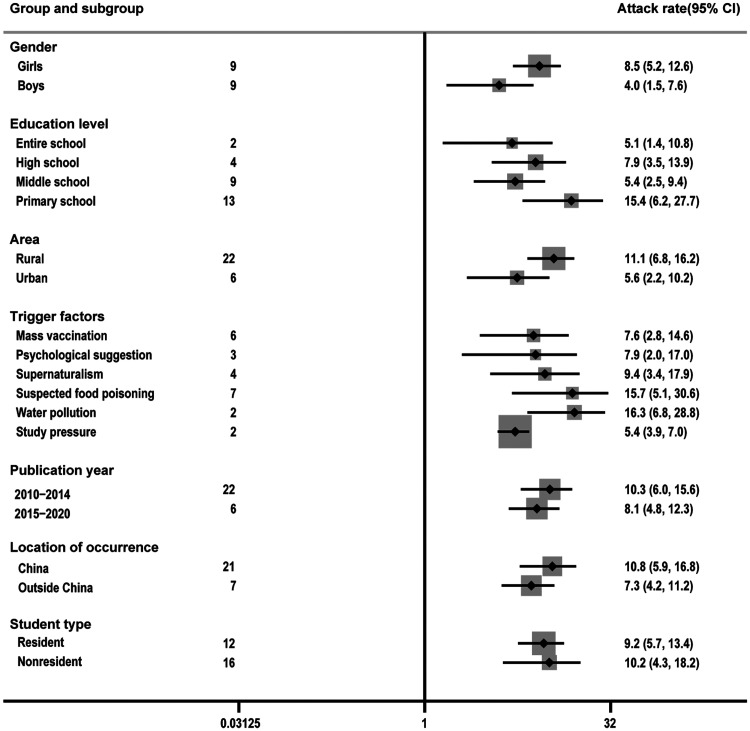
As can be seen from Figure 3 and Table 2, the random effects meta-analysis model showed significant heterogeneities (I2 > 50.0%) among the included studies. Meta-analysis indicated that the AR of MH in boys was 4.0% (95% CI 1.5, 7.6, p < 0.001, nine studies15,25–27,31,32,36,38,39) and in girls was 8.5% (95% CI 5.2, 12.6 p < 0.001, nine studies15,25–27,31,32,36–38). The AR of MH in girls was 2.43 (95% CI 1.70, 3.46, p < 0.001) times higher than in boys.
Figure 3.
Forest plot for attack rates of subgroups of mass hysteria among children and adolescents.
CI, confidence interval.
Table 2.
Assessments of heterogeneity and publication bias for studies on attack rates of mass hysteria in children and adolescents.
| Subgroups | Sample size | Number of studies | Heterogeneity |
Begg test | Egger test | |
|---|---|---|---|---|---|---|
| I2 (%) | p-value | Z value (p-value) | t value (p-value) | |||
| Gender | ||||||
| Girl | 11,977 | 9 | 95.0 | <0.001 | −1.64 (0.152) | −1.95 (0.099) |
| Boy | 8,723 | 9 | 96.0 | <0.001 | −0.61 (0.453) | −0.36 (0.452) |
| Education level | ||||||
| Entire school | 10,861 | 2 | 99.0 | <0.010 | 1.24 (0.115) | 1.88 (0.067) |
| High school | 6,278 | 4 | 98.0 | <0.010 | 0.58 (0.464) | 0.35 (0.789) |
| Middle school | 8,205 | 9 | 98.0 | <0.010 | −1.91 (0.202) | −2.55 (0.037) |
| Primary school | 7,543 | 13 | 99.0 | <0.001 | 0.89 (0.251) | −3.05 (0.011) |
| Area | ||||||
| Rural | 21,100 | 22 | 99.0 | <0.001 | −1.95 (0.051) | 1.99 (0.048) |
| Urban | 11,787 | 6 | 98.0 | <0.010 | 0.89 (0.224) | 2.64 (0.035) |
| Trigger factors | ||||||
| Mass vaccination | 12,248 | 6 | 99.0 | <0.001 | −0.74 (0.112) | 2.19 (0.022) |
| Psychological suggestion | 2,091 | 3 | 97.0 | <0.010 | −1.26 (0.127) | 1.98 (0.046) |
| Supernaturalism | 6,362 | 4 | 99.0 | <0.010 | 0.89 (0.184) | 2.57 (0.031) |
| Suspected food poisoning | 6,173 | 7 | 99.0 | <0.001 | 1.98 (0.088) | 1.75 (0.109) |
| Water pollution | 1,955 | 2 | 91.0 | <0.001 | 2.11 (0.077) | 2.77 (0.023) |
| Study pressure | 1,592 | 2 | 43.0 | 0.020 | 0.85 (0.144) | −1.03 (0.104) |
| Location of occurrence | ||||||
| China | 23,342 | 21 | 99.0 | 0.001 | −2.85 (0.041) | 2.63 (0.026) |
| Outside China | 9,545 | 7 | 97.0 | <0.010 | 1.04 (0.235) | 0.89 (0.364) |
| Publication year | ||||||
| 2010–2014 | 27,741 | 22 | 99.0 | <0.001 | 0.94 (0.207) | 1.59 (0.126) |
| 2015–2020 | 5,146 | 6 | 96.0 | <0.010 | −0.77 (0.164) | 1.87 (0.061) |
| Student type | ||||||
| Resident | 20,781 | 12 | 99.0 | <0.010 | 1.74 (0.091) | 1.02 (0.303) |
| Nonresident | 12,106 | 16 | 99.0 | <0.001 | 1.49 (0.094) | −2.87 (0.025) |
The meta-analysis indicated that most studies of MH (46.4%, 13/28) were on primary school students.11,14,15,22–24,28–30,34,35,38,39 In contrast, studies on MH in the whole school population (including middle and high school students) comprised the lowest percentage of reviewed studies (7.1%, 2/28).25,31 The highest AR of MH (15.4%, 95% CI 6.2, 27.7, p < 0.001) was for primary school students (Figure 3). Conversely, the lowest AR of MH (5.1%, 95% CI 1.4, 10.8, p < 0.010) was for the whole school population.25,31 As seen in Figure 3, there were six main potential trigger factors for MH in children and adolescents. The highest AR (16.3%, 95% CI 6.8, 28.8, p < 0.001) was for water pollution,11,26 followed by suspected food poisoning (15.7%, 95% CI 5.1, 30.6, p < 0.001).12,16,25,28–30,35 The lowest AR (5.4%, 95% CI 3.9, 7.0, p < 0.001)27,32 was for the trigger factor of study pressure.
Figure 3 indicates an AR difference between rural (11.1%, 95% CI 6.8, 16.2, p < 0.001)14–16,20–30,32–39 and urban areas (5.6%, 95% CI 2.2, 10.2, p < 0.010)11–13,18,19,31 for MH in children and adolescents. The AR of MH within China was 10.8% (95% CI 5.9, 16.8, p < 0.001),11–16,18–31,39 and outside China AR was 7.3% (95% CI 4.2, 11.2, p < 0.010).32–38 This suggests a difference in the occurrence of the AR of MH in China compared with other countries included in the analysis (i.e. Nepal, Ethiopia, Bangladesh, Mexico and the USA).
The meta-analysis showed the following time differences in the AR of MH in children and adolescents: (1) of all studies conducted between 2010 and 2020, 78.6% (22/28) were conducted from 2010 to 2014;11–16,18–25,29–31,33,35–37,39 (2) The highest AR (16.5%, 95% CI 0.1, 57.3, p < 0.001) was for 2014;29–31 (3) the AR for the period 2010 to 2014 (10.3%, 95% CI 6.0, 15.6, p < 0.001)11–16,18–25,29–31,33,35–37,39 was higher than that for the period 2015 to 2020 (8.1%, 95% CI 4.8, 12.3, p < 0.010)26–28,32,34,38 (Figure 3).
Assessment of heterogeneity and publication bias
For each meta-analysis outcome, Table 2 shows the heterogeneity variance between studies (measured by the I2 statistics) and publication bias assessments using the Egger test and the Begg test. The I2 statistics indicated that there was significant heterogeneity in the included studies (Table 2). Thus, the random effects model was selected for analysis.
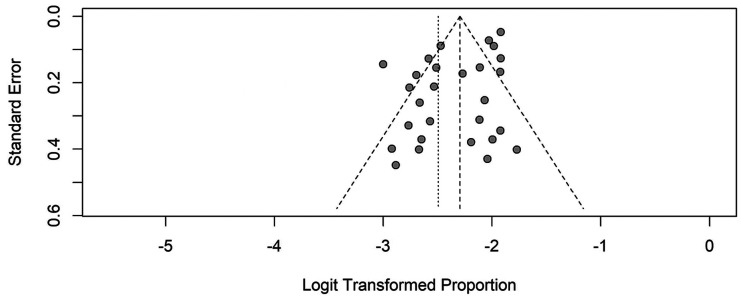
The funnel plot presents the association between the log of the odds ratio of the x-axis and the standard error of the y-axis. It shows the results of the meta-analysis; each point represents a study (Figure 4). The funnel plot, and the results of the Egger and Begg tests, showed no evidence of publication bias among the included observational studies (Table 2).
Figure 4.
Funnel plot for meta-analysis of pooled attack rates of mass hysteria in children and adolescents.
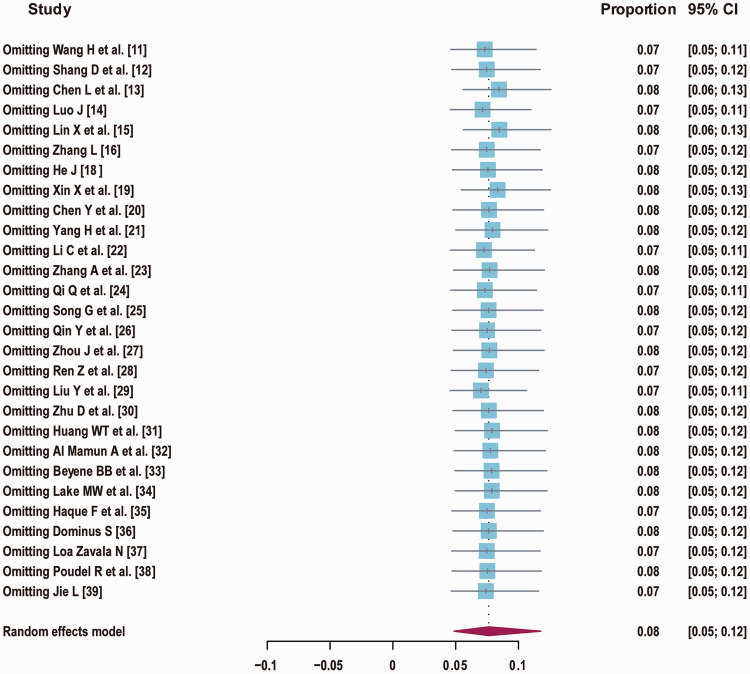
Sensitivity analysis
The sensitivity analysis indicated that the omission of any one study led to no significant changes in estimates (Figure 5). For instance, the pooled estimate of the AR of MH in children and adolescents was between 9.0% (95% CI 6.0, 14.0) and 10.0 (95% CI 6.0, 15.0) (Figure 5). Furthermore, the estimated effect sizes after adjusting (i.e. the omission of any of the studies) for the effects of gender, education level, area, publication year, trigger factors, location of occurrence and student type in the statistical model, showed no significant differences for the included observational studies.
Figure 5.
Sensitivity analysis plot for meta-analysis of pooled attack rates of mass hysteria in children and adolescents.
CI, confidence interval.
Discussion
There is a lack of systematic reviews and meta-analyses of the AR of MH in adolescents and children. One main reason for this is that many studies report the results of case and investigation analyses rather than the prevalence of MH. 39 In this study, we performed an epidemiological analysis of MH using MH prevalence data. The aim was to obtain data that could assist in the control and prevention of MH in adolescents and children. The meta-analysis results produced valuable information.
To our knowledge, this is the first comprehensive meta-analysis of the AR of MH among adolescents and children. Although only 28 articles met the criteria for inclusion in the meta-analysis, the findings may facilitate the identification of the AR of MH in children and adolescents. We confirmed that time period, population and area were important factors associated with the AR of MH in adolescents and children. The most important population characteristics were as follows. (1) Boys seemed to have a lower AR than girls, suggesting that gender may affect the risk of MH in children and adolescents. 40 The ARs for MH in boys and girls in the present study were very similar to those reported in previous studies.40,41Many studies40–42 have shown that women/girls are more likely than men/boys to experience hysteria. (2) The meta-analysis identified three main trigger factors for MH in children and adolescents: water pollution, suspected food poisoning and supernaturalism. Previous studies8,43 indicate that public health emergencies easily trigger the onset of hysteria. Our findings support this link. This association may partly be explained by individuals feeling particularly anxious or nervous 2 during public health emergencies. This finding has important implications for the control and prevention of MH in children and adolescents, and suggests the need to modify these risk factors. (3) We also found that MH outbreaks often occur in younger participants (i.e., primary school pupils). Our findings support those of previous studies 44 demonstrating that primary school children are likely to experience MH. A possible explanation for this finding may be a lack of adequate psychological coping ability in younger age groups. 44 Therefore, the government should enhance MH detection and intervention for younger students.
Interestingly, there were some main effects of time. We found that most studies of MH in children and adolescents were conducted between 2010 and 2014. Additionally, the highest AR was in 2014, and the general trend was that the AR of MH in adolescents and children declined between 2010 and 2020. The drop in AR may have been partly caused by recent improvements in the classification and diagnosis of MH.42,45,46 An alternative explanation is that the Chinese government has improved the provision of mental health care for adolescents and children in the last decade. 47 However, we found an increase in MH in adolescents and children in the context of the COVID-19 pandemic in 2020, which supports recent similar findings. 1 This observed increase may be explained by the fact that children and adolescents have experienced clinical levels of posttraumatic stress disorder during the COVID-19 pandemic. 48 This finding provides further evidence that in response to public health emergencies, governments at all levels should actively strengthen mental health education for children and adolescents.
The meta-analysis also showed an effect for residential area, indicating a difference in the AR of MH between rural and urban areas. This supports the findings of Mink 49 and those of Serinken et al.,46, who showed that socioeconomic status often plays a major role in the occurrence of hysteria (e.g., individuals living in rural areas have low economic levels). This difference in economic levels may reflect low educational levels caused by poverty.42,46
Surprisingly, MH reports were not equally distributed throughout the world. Our meta-analysis did not include any studies from Europe, South America or Australia. It is possible that this reflects the different sociocultural backgrounds of Europe, South America and Australia. There is evidence that cognitive ability can be developed by engaging with people from different cultural backgrounds. 50 Recent reports of MH may be scarce because advanced educational programs have been developed to improve the mental health of adolescents in Europe. 51 It is also possible that Europeans are more likely to experience individual functional disorders than group disorders. Moreover, some physicians may not use the term MH because they may not understand the disorder and its symptoms, or may interpret the symptoms differently.
Limitations
There are several study limitations. First, there is a dearth of adequate data on this topic. We did not include unpublished articles or articles from non–peer-reviewed journals. Moreover, some clinical studies on related disorders are ongoing, and new research will probably be added to the existing literature in the near future, necessitating an updated systematic review. Second, the quality of the included studies was poor to moderate. Finally, the data may have been incomplete, which would have increased the bias. Despite these limitations, we believe that these findings provide important information about MH and could help in controlling and preventing MH epidemics among children and adolescents. Additional work may be required to confirm the validity of ARs using ecological study designs to investigate MH in children and adolescents.
Conclusion
We can conclude that there is a prevalent MH trend (9.8%) in children and adolescents. We found that the AR of MH in girls was higher than in boys, and that primary school students may be a high-risk population for MH. There may be three main MH trigger factors (water pollution, suspected food poisoning and supernaturalism) that contribute to the AR of MH in children and adolescents. This meta-analysis indicated a declining trend between 2010 and 2020 in the AR of MH in children and adolescents.
MH in children and adolescents may constitute a serious public health issue. MH in schools may lead to social/school dysfunction and public panic. The Chinese government should assess and improve the management of MH by enhancing public health monitoring and education regarding MH in children and adolescents. To prevent and control MH in this population, governments should establish an evaluation index system to assist professional and technical personnel to improve prevention, diagnosis and treatment measures, and strengthen mental health education. The present findings could provide a reference for governments when considering such regulatory measures.
Acknowledgment
This study was part of research supported by the School of Medicine, Hangzhou Normal University, and Hangzhou Center for Disease Control and Prevention.
Footnotes
Author contributions: QC conceptualized and designed the study, carried out the literature search, analyzed the data and drafted the initial manuscript. XD performed the data analyses and assisted in the constructive discussions. LX contributed to analysis and manuscript preparation.
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by grants from the Basic Public Welfare Research Project of Zhejiang Province (grant number: LGF21H260007), the Medical Science and Technology Project of Zhejiang Province (grant number: 2020PY064) and the Health Science and Technology Project of Hangzhou Municipality (grant number: 0020190783).
ORCID iD: Qinglin Cheng https://orcid.org/0000-0003-2899-7626
References
- 1.Dubey S, Biswas P, Ghosh R, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr 2020; 14: 779–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kar SK andDwivedi S.. Braid cut anxiety in females: a newly emerged epidemic of mass hysteria in North India. Asian J Psychiatr 2018; 32: 116–117. [DOI] [PubMed] [Google Scholar]
- 3.Bell V, Oakley DA, Halligan PW, et al. Dissociation in hysteria and hypnosis: evidence from cognitive neuroscience. J Neurol Neurosurg Psychiatry 2011; 82: 332–339. [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and statistical manual of mental disorders: fifth edition text revision. Washington D.C: American Psychiatric Press, 2013. [Google Scholar]
- 5.Bagus P Peña-Ramos JA andSánchez-Bayón A.. COVID-19 and the political economy of mass hysteria. Int J Environ Res Public Health 2021; 18: 1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lyssenko L, Schmahl C, Bockhacker L, et al. Dissociation in psychiatric disorders: a meta-analysis of studies using the Dissociative Experiences Scale. Am J Psychiatry 2018; 175: 37–46. [DOI] [PubMed] [Google Scholar]
- 7.Ajemu KF, Weldearegay TW, Bezabih NM, et al. Mass psychogenic illness in Haraza Elementary School, Erop District, Tigray, Northern Ethiopia: investigation to the nature of an episode. Psychiatry J 2020; 2020: 2693830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Penna C. Psychosocial approaches to mass hysteria phenomena: a case study in Mozambique. Journal of Psychosocial Studies 2019; 12: 157–169. [Google Scholar]
- 9.Agoramoorthy G. Dealing the occasional episodes of mass hysteria in India. Int J Soc Psychiatry 2017; 63: 470. [DOI] [PubMed] [Google Scholar]
- 10.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang H Ben Z andQian G.. A quick survey report on suspected mass hysteria in the students. Chinese Journal of School Doctor 2012; 26: 622–623. (In Chinese) [Google Scholar]
- 12.Shang D, Liu X, Chen W, et al. A survey of mass psychogenic reaction was triggered by 2 students’ suicide. Health Vocational Education 2010; 28: 124–125. (In Chinese) [Google Scholar]
- 13.Chen L andSong J.. An investigation on mass psychogenic reaction was triggered by PPD injection. Medical Frontier 2013; 35: 281–283. (In Chinese) [Google Scholar]
- 14.Luo J. A clinical analysis of 84 cases of children mass hysteria. Chinese Journal of Practical Nervous Diseases 2011; 14: 68–69. (In Chinese) [Google Scholar]
- 15.Lin X, Xu Y, Wang XM, et al . Psychological intervention of mass hysteria after immunized with pandemic influenza A (H1N1) vaccine. Disease Surveillance 2010; 25: 1006–1008. (In Chinese) [Google Scholar]
- 16.Zhang L. A report on mass hysteria in middle school. China Health Industry 2012; 10: 141. (In Chinese) [Google Scholar]
- 17. Campbell R, Pound P, Pope C, et al. Evaluating meta-ethnography: a synthesis of qualitative research on lay experiences of diabetes and diabetes care. Soc Sci Med 2003; 56: 671–684. [DOI] [PubMed] [Google Scholar]
- 18.He J. The epidemiological investigation analysis on mass hysteria among students with college entrance examinations. Chinese Journal of School Health 2010; 31: 245–246. (In Chinese) [Google Scholar]
- 19.Xin X Re Z andRe B.. Investigation analysis of mass psychogenic reaction was triggered by the inoculation of influenza A (H1N1) vaccine. Chinese Journal of Vaccines and Immunization 2011; 17: 482. (In Chinese) [Google Scholar]
- 20.Chen Y Liang L andLuo W.. Investigation analysis of mass hysteria after the inoculation of measles vaccine. Modern Preventive Medicine 2010; 37: 3169–3170. (In Chinese) [Google Scholar]
- 21.Yang H andCai M.. An investigation analysis on students’ mass hysteria in rural areas. Chinese Primary Health Care 2012; 26: 87–88. (In Chinese) [Google Scholar]
- 22.Li C andZhang X.. A survey on students’ mass psychogenic reaction in a rural primary school. Chinese Journal of Pest Control 2013; 30: 132–133. (In Chinese) [Google Scholar]
- 23.Zhang A, Heng W, Zhang T, et al. Investigation of an outbreak of mumps among primary students. Journal of Tropical Medicine 2012; 12: 227–228. (In Chinese) [Google Scholar]
- 24.Qi Q andYang X.. Investigation on group psychogenic reaction after vaccination. Bulletin of Disease Control and Prevention 2013; 28: 46–47. (In Chinese) [Google Scholar]
- 25.Song G Zhang B andZhang Z.. Zigong City Rong xian a school in groups of heart diseases due to epidemiological survey. Medical Information 2010; 23: 3–5. (In Chinese) [Google Scholar]
- 26.Qin Y, Shi Z, Zhou Q, et al. An investigation into a mass hysteria event caused by the peculiar smell of bottled water. Preventive Medicine Tribune 2015; 21: 294–295. (In Chinese) [Google Scholar]
- 27.Zhou J, Dong Z, Zhou X, et al. Surveys of epidemic hysteria in junior middle school students. Journal of Clinical Psychosomatic Diseases 2015; 21(3): 108–111. (In Chinese) [Google Scholar]
- 28.Ren Z, Jin D, Wu J. Epidemiological investigation on a mass hysteria caused by eating suspected food. Special Health 2017; 20: 203–204. (In Chinese) [Google Scholar]
- 29.Liu Y andLi Z.. Investigation on mass psychogenic illness in a primary school. Chinese Journal of School Health 2014; 35: 1113–1114. (In Chinese) [Google Scholar]
- 30.Zhu D andZhao X.. Epidemiological investigation and analysis among students with mass hysteria in a rural primary school. Medical Journal of Chinese People’s Health 2014; 26: 76–78. (In Chinese) [Google Scholar]
- 31.Huang WT, Hsu CC, Lee PI, et al. Mass psychogenic illness in nationwide in-school vaccination for pandemic influenza A (H1N1) 2009, Taiwan, November 2009–January 2010. Euro Surveill 2010; 15: 19575. [DOI] [PubMed] [Google Scholar]
- 32.Al Mamun A, Maruf MM, Bhowmik AD, et al. Mass psychogenic illness: comparison on selected variables between cases and non-cases. Bangladesh Journal of Psychiatry 2016; 30: 14–19. [Google Scholar]
- 33.Beyene BB Teka A andLuce R.. Outbreak of mass psychogenic illness at a high school, Amhara Region, Ethiopia, April 2010. Int Invent J Med Sci 2014; 1: 157–161. [Google Scholar]
- 34.Lake MW, Erku MM, Hailu HA, et al. Hysteria outbreak investigation in Kombolcha Town among school girls, Northwest Ethiopia, January 2013. Sci J Public Health 2016; 4: 37–42. [Google Scholar]
- 35.Haque F, Kundu SK, Islam MS, et al. Outbreak of mass sociogenic illness in a school feeding program in northwest Bangladesh, 2010. PLoS One 2013; 8: e80420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dominus S. What happened to the girls in Le Roy. The New York Times Magazine; 2012. http://web.missouri.edu/∼segerti/3830/LeRoy Girls.pdf. Accessed October 15, 2020.
- 37.Loa Zavala N. The expulsion of evil and its return: an unconscious fantasy associated with a case of mass hysteria in adolescents. Int J Psychoanal 2010; 91: 1157–1178. [DOI] [PubMed] [Google Scholar]
- 38.Poudel R, Aich TK, Bhandary K, et al. Recurrent mass hysteria in schoolchildren in Western Nepal. Indian J Psychiatry 2020; 62: 316–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jie L. Koro endemic among school children in Guangdong, China. World Cult Psychiatry Res Rev 2010; 5: 102–105. [Google Scholar]
- 40.Dmytriw AA. Gender and sex manifestations in hysteria across medicine and the arts. Eur Neurol 2015; 73: 44–50. [DOI] [PubMed] [Google Scholar]
- 41.Wong WI Shi SY andChen Z.. Students from single-sex schools are more gender-salient and more anxious in mixed-gender situations: results from high school and college samples. PLoS One 2018; 13: e0208707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Folger T. Mass hysteria. Sci Am 2017; 316: 46–53. [DOI] [PubMed] [Google Scholar]
- 43.Aybek S, Nicholson TR, O'Daly O, et al. Emotion-motion interactions in conversion disorder: an FMRI study. PLoS One 2015; 10: e0123273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nakalawa L, Musisi S, Kinyanda E, et al. Demon attack disease: a case report of mass hysteria after mass trauma in a primary school in Uganda. African Journal of Traumatic Stress 2010; 1: 43–48. [Google Scholar]
- 45.Martinsen KD, Rasmussen LMP, Wentzel-Larsen T, et al. Prevention of anxiety and depression in school children: effectiveness of the transdiagnostic EMOTION program. J Consult Clin Psychol 2019; 87: 212–219. [DOI] [PubMed] [Google Scholar]
- 46.Serinken M andKarcioglu O.. Patients with acute stroke presenting like conversion disorder. Prehosp Disaster Med 2018; 33: 451–453. [DOI] [PubMed] [Google Scholar]
- 47.Dekker MCJ, Urasa SJ, Kellogg M, et al. Psychogenic non-epileptic seizures among patients with functional neurological disorder: a case series from a Tanzanian referral hospital and literature review. Epilepsia Open 2018; 3: 66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sharma S, Mustanski B, Dick D, et al. Protective factors buffer life stress and behavioral health outcomes among high-risk youth. J Abnorm Child Psychol 2019; 47: 1289–1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mink JW. Conversion disorder and mass psychogenic illness in child neurology. Ann N Y Acad Sci 2013; 1304: 40–44. [DOI] [PubMed] [Google Scholar]
- 50.Bender A andBeller S.. The cultural fabric of human causal cognition. Perspect Psychol Sci 2019; 14: 922–940. [DOI] [PubMed] [Google Scholar]
- 51.Tuomainen H, Schulze U, Warwick J, et al. Managing the link and strengthening transition from child to adult mental health Care in Europe (MILESTONE): background, rationale and methodology. BMC Psychiatry 2018; 18: 167. [DOI] [PMC free article] [PubMed] [Google Scholar]