Abstract
This special article outlines the background to bereavement in critical care and scopes the current provision and evidence for bereavement support following death in critical care. Co-authored by a family member and former critical care patient, we aim to draw out the current challenges and think about how and where support can be implemented along the bereavement pathway. We draw on the literature to examine different trajectories of dying in critical care and explore how these might impact bereavement, highlighting important points and risk factors for complicated grief. We present graphic representation of the critical junctures for bereavement in critical care. Adjustment disorders around grief are explored and the consequences for families, including the existing evidence base. Finally, we propose new areas for research in this field.
Keywords: Bereavement, critical care, dying, families, grief
Background
This article aims to outline dying in critical care and why this presents unique challenges for families and staff providing services, summarise the research evidence and current bereavement services and suggest future areas of development. One of our co-authors is a patient and family representative to ensure that this view is an integral aspect to this article. In this article, we define family as anyone close to the patient and concerned with their welfare, encompassing relatives, next of kin, and friends.
Death in critical or intensive care unit (ICU) can be one of the most profound events for families. Experiencing what can be a sudden and traumatic death, and a lack of formalised bereavement follow-up, highlighted in a UK survey 1 creates a significant challenge for families who may well experience a difficult death. This can lead to complicated grief (CG) trajectories, prolonged grief disorder (PGD), and increased risk of post-traumatic stress disorders.2–6
One in seven people admitted to UK ICUs die each year, this equates to 27,000 people. 7 Critical illness onset, and death, may be sudden, unexpected, or it may be protracted and anticipated. Both can be traumatic for patients and families, although literature suggests the sudden nature of death can be more traumatic. 8 Dying and death in critical care is arguably unique for several reasons, including the technologically mediated nature of decline in critical care, which can lead to what has been termed a medicalised death. 9 The rapidity of death and dying is also a factor. Epidemiological data show us that from admission to death is short, less than three days on average10,11 and withdrawal to death is very short (2.4 h). 12 Moreover, patients are often ventilated and the mechanics of withdrawal can lead to a different death and subsequent bereavement experience, which cannot be captured in epidemiological studies.
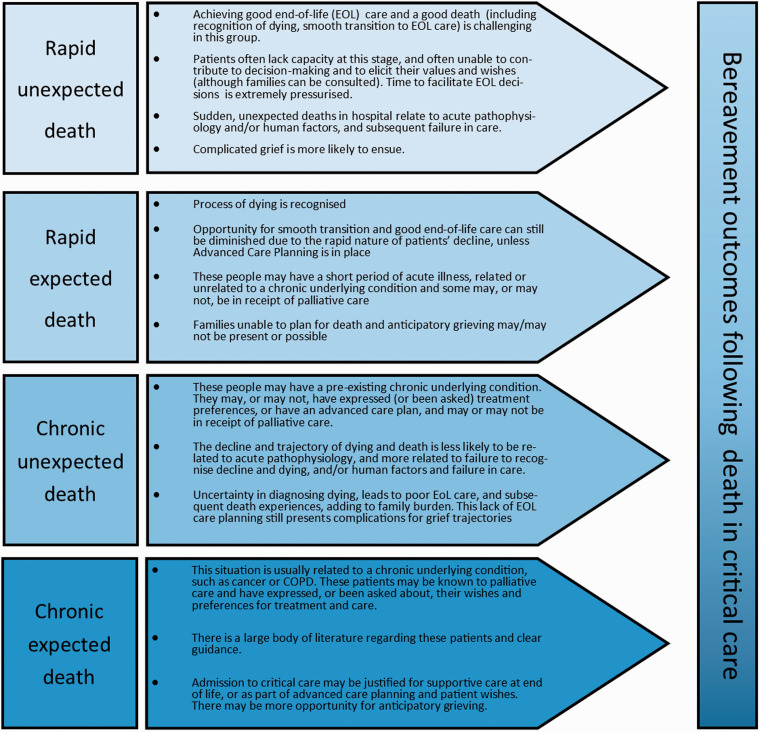
The nature of the dying trajectory will affect dying, death and subsequent experience of grief for families. Four key trajectories for dying in critical care can be described (more detail is given in Figure 1):
Rapid unexpected death, where patients are unexpectedly deteriorating (and where end-of-life (EoL) decisions are unlikely to have been made, nor EoL care plans initiated).
Rapid expected death, where the patient's condition deteriorates, and their death follows a clear decline in the patient's condition. This decline is often related to an acute episode related to a pre-existing chronic illness.
Chronic unexpected death, where people often have a period of protracted illness leading to an ICU admission.
Chronic expected death, where it is recognised that the patient is dying and this is likely to occur in critical care. Here, professionals have communicated this expectation to families, who have confirmed their understanding.
The speed with which rapid unexpected and chronic unexpected death occurs in critical care represents a particular burden for families. These quotes are from research with bereaved families of critically ill patients 13 (see Box 1).
Figure 1.
Four trajectories of death in critical care. COPD: Chronic Obstetric Pulmonary Disease.
There is little evidence to understand the scale of the problem of grief for each of these trajectories, with the exception of chronic, expected death (particularly in the cancer/COPD literature). Several issues that arise in these dying trajectories that have a bearing on the patient's death, and subsequent bereavement and grief experiences, including adaptation and adjustment are as follows:
Prognostication (and timing thereof), the recognition of dying and the rapidity of death
Process of transition to palliation and EoL care in critical care (including transferring home to die), and ongoing support from these services once bereaved
Interventions to support transitions, EoL care and anticipatory grief, including: Symptom management; Communication/Family Support; Continuity of Care; Raising awareness
Presence of anticipatory grief, grief prior to loss (death), associated with expected death. 14 In people who are also caregivers prior to death, anticipatory grief can be associated with poor bereavement outcomes, including complex and disordered grief trajectories, 15 which can be contrary to the connotations of expected death, where it might be thought that a person was more prepared for death in knowing it was expected.
Family context (such as social situation, family dynamics)
Individual pre-existing mental health and wellbeing
Social support and social networks/family structures
Box 1.
Sudden death and rapidity of dying in critical care.
| ‘I got a telephone call at four o’clock in the morning saying, “come in, things are critical”. And I was going “What do they mean? What do they mean?” because it had not crossed my mind for a second that he would die. Not for a millisecond’. |
| ‘… I must say that the ending happened very, very fast but I think they didn't realise how fast it … That was very fast ‘cos you see, you know … You watch things on telly and you see these dramas and it takes, you know … but it was seconds, it was all happening too fast’. |
| ‘The general consensus was they couldn't have fought harder than they fought. They did everything that was in their power to do … A lot of the cases that are in there [ICU], they in there because they are chronic cases and they are expected to die … and their relatives are somewhat prepared. In our case, he was cured from his illness but it was far more like a traumatic death as far as we were concerned’. |
Source: Pattison et al. 13
Consequences for families and societal impact
Bereavement and grief-related disorders
Bereaved family members often struggle to understand and adjust to events that occur in critical care leading up to and around the time of death. For this reason, some family members report experiencing intense grief that affects physical, mental, emotional and social health, and wellbeing. Some authors argue grief models have shifted towards increasing medicalisation,16–18 particularly since the inclusion of grief disorders in diagnostic manuals (Diagnostic and Statistical Manual of Mental Disorders (DSM) and International Classification of Diseases (ICD)). Some of these authors advocate that grief should not be regarded as a problem to be resolved but a necessary process after loss. 19 However, while it can be challenging to classify an individual's grief reaction as ‘pathological’, published frameworks provide a description of normal and disturbed grief. 20
In one such model, the bereavement process is understood to represent the accomplishment of tasks comprising personal, practical, spiritual, and existential adjustments to loss 20 : accepting the reality of the loss, processing the pain associated with grief, adjusting to a world without the deceased, and finding a way to remember the deceased while continuing to live the rest of one's life. Family members who have difficulties achieving these ‘tasks’ even after a period of time has passed may be experiencing a disturbance in the grieving process.
There is no clear, accepted definition of CG currently; however, there are clear definitions for pronged grief disorder (in ICD-11) and persistent complex bereavement disorder (in DSM5). CG is a more widely used term but the official definitions are now linked to PGD and persistent complex bereavement disorder. Shear 17 suggests there is no consensus for criteria and naming of CG, and that PGD is the natural successor to CG.
Suggested diagnostic criteria for bereavement-related disorders include symptoms such as longing for and preoccupation with the person who died, emotional distress, and significant functional impairment that persist beyond six months after the loss of a significant other. 21 Three broad diagnostic concepts have been proposed to characterise bereavement-related disorders: PGD, persistent complex bereavement disorder, and CG. 22 In this article, we focus on CG as this has been associated with critical care bereavement. 3
Prevalence and risk factors for CG
Emerging research within the field of critical care demonstrates that family members can experience high levels of CG and other psychological morbidity. One such study evaluated these outcomes for families of 475 patients who died in 41 critical care units in France. This study found 52% experienced CG and 44% had post-traumatic stress disorder symptomatology at six months after their loss. 3 In contrast, the prevalence of CG in the general population is 5–10%.23–25
Factors associated with increased risk of developing CG included the family member not able to say goodbye to the patient, witnessing the death, and the patient dying while intubated. Where a patient was involved in decision-making and declined treatments, family members had a 76% reduction in odds of developing CG. 3 It is also of note that family members who found communication unsatisfactory with ICU staff had a three times increase in odds of developing CG. These findings suggest potential targets for research with interventions to improve care, including decision-making, which might impact on later psychological morbidity.
Fixed characteristics such as younger age of the decedent, and the person who has been bereaved being the spouse or living alone also increased the risk of CG. 4 These non-modifiable characteristics could be used to identify family members at higher risk of morbidity and allow better targeting of bereavement support where and when it is needed, and to expand bereavement follow-up services.
Impact of CG
Numerous studies conducted in general populations demonstrate that bereavement is associated with impacts on mental, physical, and socioeconomic health and wellbeing. For example, bereaved family members seek more primary care consultations and receive more prescriptions for antidepressants. 26 Research shows that bereaved spouses experience worse physical functioning and increased mortality.27–29 Furthermore, a recent Scottish study found that bereavement was associated with increased healthcare utilisation (including longer hospital stays when ill), shown by additional primary care consultations costing £2 million, and reduced employment in the two years after bereavement. 30
The consequences of bereavement in the ICU, and hence associated costs for supporting families, are likely to be more severe due to the higher prevalence of CG and psychological morbidity in families bereaved in critical care settings. However, UK-specific data are lacking to identify family members at higher risk of CG and to ensure their needs are met during their bereavement.
Current evidence for supporting families bereaved in ICU
Little evidence exists on ways to support ICU families through grief trajectories, from anticipatory grief during EoL decision-making, withdrawal, and dying, and in the months beyond.2,31
Recent reviews highlight insufficient evidence for specific interventions, models of delivery, or timing of support, as all studies were contextually bound, with no UK intervention studies reported.32,33 Efstathiou et al.'s 32 systematic review identified 14 papers evaluating nine bereavement support interventions. Interventions included personal mementos, condolence letters, meetings with critical care staff after the death, and story-telling. Adequately powered studies demonstrated no effect in a range of interventions, and one study even suggested worse psychological morbidity in families randomised to receive a personalised condolence letter compared with usual care. All the evidence reviewed was appraised as weak with little potential for generalisability. However, interventions were viewed as acceptable by bereaved families. Furthermore, a qualitative scoping review highlights the need to better understand bereaved critical care families' experiences in order to develop appropriate interventions grounded in a sound theoretical framework. 34
Most of the reviewed studies were conducted in countries other than the UK. However, findings from other countries may not be easily generalisable to the UK due to cultural differences. These differences are not limited to culturally specific bereavement experiences, but extend to the practice of intensive care, where organisation, patient case-mix, and outcomes differ substantially between countries. 35 Despite this limitation, research in non-UK settings has not identified how we can better support bereaved families in critical care, in terms of models of service delivery or types of intervention, nor has it identified the appropriate timing of support. In particular, we do not understand bereavement needs of those affected by the death of family member in critical care settings.
Potentially, focused critical care interventions could reduce family burden, particularly in relation to returning to work while grieving. 36 Given poor family experiences and outcomes after the death of a family member in critical care,37–39 current support mechanisms, including those post-critical care, do not meet families' needs. Crucially, evidence to understand and address these needs is also lacking.
Current provision and guidance for bereavement care in critical care
Recent guidance by the Faculty of Intensive Care Medicine written specifically to address EoL care in critical care settings focuses on advanced care planning, EoL decisions, and EoL care. It emphasises family involvement in EoL care to help prepare for bereavement and the role of the healthcare team in guiding the family towards an understanding of death from both individual and cultural perspectives. Bereavement care services were highlighted as invaluable for helping families who may struggle to understand death in critical care, particularly when compared to deaths in other environments. 40 However, service provision guidance for UK critical care units does not specifically outline bereavement service configuration, 41 nor does recent NICE guidance for EoL services. 42 Current service models, 1 or lack thereof, demonstrate how critical care units fail to meet national bereavement service standards. 43 Berry et al.'s 1 survey conducted across 78% of eligible units (n=113/144) in England found limited, inconsistent provision of bereavement care. These were mainly information leaflets that signpost to bereavement services (services which are predominantly based in the charity/third sector and not specific to critical care bereavement), and 17% of units provided no bereavement support services.
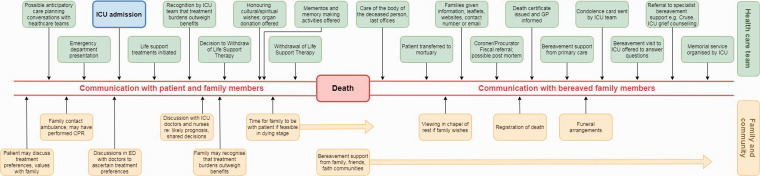
CRUSE, the largest bereavement charity in the UK, outlines seven key standards for bereavement service configuration: Planning, Awareness and Access, Assessment, Education and Training, Support and Supervision, Resources and Evaluation and Monitoring. 44 However, these standards are not routinely considered in critical care related-bereavement, and primary care professionals may not fully understand the risk factors for CG, as highlighted by Sealey et al., 45 or implications following bereavement in critical care. Moreover, lack of data in this area means we do not know the scale of the problem. A multi-agency approach underpins UK bereavement services, with provision spanning acute care (palliative care and pastoral/spiritual care services) through to primary care and third sector (hospice/charity/volunteer groups), and variable access. This relies on much provision outside of the NHS, but may be partially/wholly commissioned by the NHS (see Figure 2).
Figure 2.
Bereavement pathway in critical care. CPR: cardiopulmonary resuscitation; ED: emergency department; GP: general practitioner; ICU: intensive care unit.
The national commissioning standards for bereavement support suggest three components of grief support for families 46 :
Information about what to expect in bereavement, including normal trajectories of grief so families can understand that grief is to be expected and the forms that it can take, and what support is available to them
Formalised support and the opportunity to reflect on grief and bereavement experiences, which may involve lay support through volunteers
Access to specialist intervention through psychological support, mental health and counselling services, and palliative care/bereavement services.
Following death in critical care, there are additional challenges for families and staff as any bereavement service provision is usually disengaged from critical care services. In the absence of formalised critical care bereavement follow-up, bereavement care can fall to community services, in particular primary care, GPs, and district nurses. This is problematic, due to GPs being ill-equipped to provide advice following bereavement in the ICU (even where GPs have expressed an interest to provide pro-active bereavement follow-up), the time constraints in which they work, and increasing service pressures. 47 Even where GPs were trained to deliver bereavement interventions, there was a lack of sustained improvement in families, and in GPs' ability a year later to recognise CG, suggesting these approaches may be limited. 48
Components of bereavement care in critical care units vary significantly. Options such as family meetings are generally focused on reviewing what happened to the patient (event review), rather than meaning-making and therapeutic interactions. Memorial services for former critical care patients have gained popularity in the UK, as a way of supporting families bereaved in critical care. Mementoes (locks of hair, electrocardiograms) are also increasingly used, alongside critical care diaries. Bereaved families can attend critical care support groups. However, we do not know whether initiatives like these offer support that help families grieving trajectory, as formalised research into the effect of these support mechanisms does not currently exist. As such, we do not understand what families' bereavement support needs are following death in critical care, nor how to meet individual and changing needs, and which interventions might be helpful to families, particularly in the UK.
We have mapped the current landscape for bereavement provision related to adult critical care in Figure 2.
Developing the evidence
General bereavement care has been identified as a priority for research in several pieces of patient and family focused work, including the NIHR, 49 and the James Lind Alliance priority setting exercises in both palliative49,50 and critical care. 51 They specifically highlighted the impact of continuity of care across clinical settings, from tertiary specialist and secondary hospital care into the community via primary care and social care. However, there is a lack of research into pro family and patient-centred interventions to achieve effective bereavement care, especially with patients who are acutely deteriorating and at-risk of dying.
Evidence to drive practice is limited, and more research is needed to understand experiences and meaning-making practice, but also to prevent long- and short-term grief complications. The reasons for the lack of research are multifold, and include a reluctance to approach families for bereavement-related research, even when there is evidence to show that families find it cathartic and useful.52–54
The heterogeneity of existing studies in critical care means it is hard to draw meaningful conclusions about effective practices, as recently outlined in a systematic review. 32 Moreover, there is a tension between what happens in practice and what the limited evidence tells us we should be doing. A good example of this is sending condolence letters, a common practice in UK critical care, which Kentish Barnes et al.'s 4 randomised controlled trial identified was associated with increased depression and PTSD at six months. This emphasises how seemingly innocuous actions in early bereavement can have lasting consequences. The authors present a number of hypotheses for this finding, including the unique nature of ICU means this might exacerbate painful memories, but without qualitative understanding it is hard to draw definitive conclusions. Qualitative studies around EoL and bereavement suggest there may be value in certain practices (such as creating mementoes), 33 which need to be explored in more depth across a range of critical care settings and in multi-centre studies. A broad range of research, encompassing mixed methods may improve understanding around the effectiveness, or not, of bereavement interventions. Theoretical frameworks of bereavement, such as the Integrated Risk Factors Framework, 15 can also help in developing the evidence base as they provide comprehensive constructs to apply to what is a complex field, with social, familial, emotional, psychological, physical, and societal components. We have to understand the mediating factors that influence bereavement and outcomes, in order to address them, therefore approaching research through a theoretical lens is also important. No core outcome set measures exist for EoL in critical care research currently, although development is underway for bereavement support research studies more broadly, which will help address these issues in the future. 55
Moreover, by looking to novel areas of practice in mental health, such as locally commissioned mental health provision in GP practices (rather than requiring additional referrals to external mental health services) may be one way forward. Approaches such as social prescribing (where health professionals refer to community services, including voluntary sector, with a focus on health/wellbeing) and by learning from areas such as paediatric critical care and maternity, bereavement care in adult critical care can potentially be advanced.
Conclusions
We have outlined how trajectories of death in critical care may impact on grief and CG, in particular, and the unique nature of bereavement in this context. The patchy service provision, which falls well short of national guidance, and lack of UK-centred research means we do not fully understand the landscape of bereavement care, nor what optimal care looks like, following death in critical care. We have to work with patients, public, and families and colleagues in driving forward services, and ensuring the care we provide is robustly underpinned with good evidence. In practice, we need to have mechanisms that ensure families' and public views in developing these services are fully integrated, requiring unit staff to know how and when to approach families, and knowing the appropriate things to ask.
Concluding view from a family member (CW, co-author)
Just as the long and complex recovery and rehabilitation of critical care patients is often hidden from view from critical care staff (because it happens away from the unit), so are the repercussions for families after the death of their relative. There are particular facets to a death in critical care, which means general bereavement services are not sufficient, but the critical care expertise does not sit in the community. Family members may present to many different places seeking support or due to the consequences of what happened, but all this is hidden from view. There is likely to be more incidence of complicated grief with the separation of patients and families (which is an thinkable thing to go through). This disconnect means that not only do services not improve for families while in critical care, but there is no impetus to improve the care afterwards. Investing in good quality research to know which interventions are effective pre and post death in ICU, is a necessity.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Natalie A Pattison https://orcid.org/0000-0002-6771-8733
Nazir I Lone https://orcid.org/0000-0003-2707-2779
References
- 1.Berry M, Brink E, Metaxa V. Time for change? A national audit on bereavement care in intensive care units. J Intensive Care Soc 2017; 18: 11–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson WG, Arnold RM, Angus DC, et al. Posttraumatic stress and complicated grief in family members of patients in the intensive care unit. J Gen Intern Med 2008; 23: 1871–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kentish-Barnes N, Chaize M, Seegers V, et al. Complicated grief after death of a relative in the intensive care unit. Eur Respir J 2015; 45: 1341–1352. [DOI] [PubMed] [Google Scholar]
- 4.Kentish-Barnes N, Chevret S, Champigneulle B, et al. Effect of a condolence letter on grief symptoms among relatives of patients who died in the ICU: a randomized clinical trial. Intensive Care Med 2017; 43: 473–484. [DOI] [PubMed] [Google Scholar]
- 5.Azoulay E, Pochard F, Kentish-Barnes N, et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med 2005; 171: 987–994. [DOI] [PubMed] [Google Scholar]
- 6.Downar J, Koo E, des Ordons AR, et al. Prevalence and predictors of severe grief reactions and desire for support following a death in the intensive care unit: a multicentre observational study. Intensive Care Med 2018; 44: 521–522. [DOI] [PubMed] [Google Scholar]
- 7.Intensive Care National Audit and Research Centre. Key statistics from the case mix programme – adult, general critical care units, 2019. Available at: https://www.icnarc.org/Our-Audit/Audits/Cmp/Reports/Summary-Statistics. (accessed 1 October 2019).
- 8.Keyes KM, Pratt C, Galea S, et al. The burden of loss: unexpected death of a loved one and psychiatric disorders across the life course in a national study. Am J Psychiatry 2014; 171: 864–871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seymour J. Critical moments – death and dying in intensive care, Buckingham: Oxford University Press, 2001. [Google Scholar]
- 10.Khandelwal N, Benkeser D, Coe NB, et al. Patterns of cost for patients dying in the intensive care unit and implications for cost savings of palliative care interventions. J Palliat Med 2016; 19: 1171–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wunsch H, Linde-Zwirble WT, Harrison DA, et al. Use of intensive care services during terminal hospitalizations in England and the United States. Am J Respir Crit Care Med 2009; 180: 875–880. [DOI] [PubMed] [Google Scholar]
- 12.Wunsch H, Harrison DA, Harvey S, et al. End-of-life decisions: a cohort study of the withdrawal of all active treatment in intensive care units in the United Kingdom. Intensive Care Med 2005; 31: 823–831. [DOI] [PubMed] [Google Scholar]
- 13.Pattison N, Carr SM, Turnock C, et al. ‘Viewing in slow motion’: patients’, families’, nurses’ and doctors’ perspectives on end-of-life care in critical care. J Clin Nurs 2013; 22: 1442–1454. [DOI] [PubMed] [Google Scholar]
- 14.Nielsen MK, Neergaard MA, Jensen AB, et al. Do we need to change our understanding of anticipatory grief in caregivers? A systematic review of caregiver studies during end-of-life caregiving and bereavement. Clin Psychol Rev 2016; 44: 75–93. [DOI] [PubMed] [Google Scholar]
- 15.Stroebe MS, Folkman S, Hansson RO, et al. The prediction of bereavement outcome: development of an integrative risk factor framework. Soc Sci Med 2006; 63: 2440–2451. [DOI] [PubMed] [Google Scholar]
- 16.Breen LJ, O'Connor M. The fundamental paradox in the grief literature: a critical reflection. OMEGA J Death Dying 2007; 55: 199–218. [DOI] [PubMed] [Google Scholar]
- 17.Shear MK. Clinical practice and Complicated grief. N Engl J Med 2015; 372: 153–160. [DOI] [PubMed] [Google Scholar]
- 18.Shear MK, Simon N, Wall M, et al. Complicated grief and related bereavement issues for DSM-5. Depress Anxiety 2011; 28: 103–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moules NJ, Simonson K, Prins M, et al. Making room for grief: walking backwards and living forward. Nurs Inq 2004; 11: 99–107. [DOI] [PubMed] [Google Scholar]
- 20.Worden JW. Grief counseling and grief therapy: a handbook for the mental health practitioner, 4th ed. New York: Springer Publishing Company, 2008. [Google Scholar]
- 21.World Health Organisation. International classification of diseases – diagnostics and statistics manual version 11, Geneva: WHO, 2018. [Google Scholar]
- 22.Maciejewski PK, Maercker A, Boelen PA, et al. “Prolonged grief disorder” and “persistent complex bereavement disorder”, but not “complicated grief”, are one and the same diagnostic entity: an analysis of data from the Yale Bereavement Study. World Psychiatry 2016; 15: 266–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lundorff M, Holmgren H, Zachariae R, et al. Prevalence of prolonged grief disorder in adult bereavement: a systematic review and meta-analysis. J Affect Disord 2017; 212: 138–149. [DOI] [PubMed] [Google Scholar]
- 24.Fujisawa D, Miyashita M, Nakajima S, et al. Prevalence and determinants of complicated grief in general population. J Affect Disord 2010; 127: 352–358. [DOI] [PubMed] [Google Scholar]
- 25.Kersting A, Brähler E, Glaesmer H, et al. Prevalence of complicated grief in a representative population-based sample. J Affect Disord 2010; 131: 339–343. [DOI] [PubMed] [Google Scholar]
- 26.King M, Vasanthan M, Petersen I, et al. Mortality and medical care after bereavement: a general practice cohort study. PLoS One 2013; 8: e52561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Boyle PJ, Feng Z, Raab GM. Does widowhood increase mortality risk? Testing for selection effects by comparing causes of spousal death. Epidemiology 2011; 22: 1–5. [DOI] [PubMed] [Google Scholar]
- 28.Lee C, Rodríguez G, Glei DA, et al. Increases in blood glucose in older adults: the effects of spousal health. J Aging Health 2014; 26: 952–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee M-A, Carr D. Does the context of spousal loss affect the physical functioning of older widowed persons? A longitudinal analysis. Res Aging 2007; 29: 457–487. [Google Scholar]
- 30.Stephen AI, Macduff C, Petrie DJ, et al. The economic cost of bereavement in Scotland. Death Stud 2015; 39: 151–157. [DOI] [PubMed] [Google Scholar]
- 31.van der Klink MA, Heijboer L, Hofhuis JG, et al. Survey into bereavement of family members of patients who died in the intensive care unit. Intensive Crit Care Nurs 2010; 26: 215–225. [DOI] [PubMed] [Google Scholar]
- 32.Efstathiou N, Walker W, Metcalfe A, et al. The state of bereavement support in adult intensive care: a systematic review and narrative synthesis. J Crit Care 2018; 50: 177–187. [DOI] [PubMed] [Google Scholar]
- 33.Riegel M, Randall S, Buckley T. Memory making in end-of-life care in the adult intensive care unit: a scoping review of the research literature. Aust Crit Care 2019; 32: 442–447. [DOI] [PubMed] [Google Scholar]
- 34.Coombs M. A scoping review of family experience and need during end of life care in intensive care. Nurs Open 2015; 2: 24–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Adhikari NK, Fowler RA, Bhagwanjee S, et al. Critical care and the global burden of critical illness in adults. Lancet 2010; 376: 1339–1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosenberg K. When grief and work collide. BMJ Support Palliat Care 2015; 5: A4. [DOI] [PubMed] [Google Scholar]
- 37.Bournival N, Siegel MD, Akgun KM. Not “out of sight, out of mind”: interventions to relieve suffering for bereaved families after an ICU death. Crit Care Med 2017; 45: 134–136. [DOI] [PubMed] [Google Scholar]
- 38.Prior A, Fenger-Gron M, Davydow DS, et al. Bereavement, multimorbidity and mortality: a population-based study using bereavement as an indicator of mental stress. Psychol Med 2018; 48: 1437–1443. [DOI] [PubMed] [Google Scholar]
- 39.Wendlandt B, Ceppe A, Choudhury S, et al. Modifiable elements of ICU supportive care and communication are associated with surrogates' PTSD symptoms. Intensive Care Med 2019; 45(5):619–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Faculty of Intensive Care Medicine. CARE AT THE END OF LIFE: a guide to best practice, discussions and decision-making in and around critical care, London: FICM, 2019. [Google Scholar]
- 41.Faculty of Intensive Care Medicine. Guidelines for the provision of intensive care services version 2, London: FICM, 2019. [Google Scholar]
- 42.National Institute for Health and Care Excellence (NICE). End of life care for adults: service delivery (NG142), London: NICE, 2019. [PubMed] [Google Scholar]
- 43.National Bereavement Alliance. Bereavement care service standards, 2014. Available at: https://nationalbereavementalliance.org.uk/bereavement-care-service-standards/ (accessed 15 September 2019).
- 44.CRUSE. Bereavement care service standards, 2013. Available at: https://www.cruse.org.uk/sites/default/files/default_images/pdf/Documents-and-fact-sheets/Bereavement_Standards_Mar2014.pdf (accessed 1 October 2019).
- 45.Sealey M, O'Connor M, Aoun SM, et al. Exploring barriers to assessment of bereavement risk in palliative care: perspectives of key stakeholders. BMC Palliat Care 2015; 14: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.National Bereavement Alliance. A guide to commissioning bereavement services in England, 2017. Available at: https://nationalbereavementalliance.org.uk/wp-content/uploads/2017/07/A-Guide-to-Commissioning-Bereavement-Services-in-England-WEB.pdf. (accessed 15 September 2019).
- 47.Nagraj S, Barclay S. Bereavement care in primary care: a systematic literature review and narrative synthesis. Br J Gen Pract 2011; 61: e42–e48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Guldin BM, Vedsted P, Jensen AB, et al. Bereavement care in general practice: a cluster-randomized clinical trial. Fam Pract 2013; 30: 134–141. [DOI] [PubMed] [Google Scholar]
- 49.NIHR Dissemination Centre. Better endings: right care, right place, right time, 2015. Available at: https://evidence.nihr.ac.uk/themedreview/better-endings-right-care-right-place-right-time/ (accessed 15 September 2019).
- 50.Palliative and end of life care Priority Setting Partnership. Palliative and end of life care Priority Setting Partnership (PeolcPSP): putting patients, carers and clinicians at the heart of palliative and end of life care research, 2015. Available at: https://www.mariecurie.org.uk/globalassets/media/documents/research/PeolcPSP_Final_Report.pdf (accessed 1 October 2019).
- 51.Reay H, Arulkumaran N, Brett S. Priorities for future intensive care research in the UK: results of a James Lind alliance priority setting partnership. J Intensive Care Soc 2014; 15: 288–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sque M, Walker W, Long-Sutehall T. Research with bereaved families: a framework for ethical decision-making. Nurs Ethics 2014; 21: 946–955. [DOI] [PubMed] [Google Scholar]
- 53.Beck AM, Konnert CA. Ethical issues in the study of bereavement: the opinions of bereaved adults. Death Stud 2007; 31: 783–799. [DOI] [PubMed] [Google Scholar]
- 54.Alexander SJ. ‘As long as it helps somebody’: why vulnerable people participate in research. Int J Palliat Nurs 2010; 16: 173–178. [PubMed] [Google Scholar]
- 55.COMET Initiative. Supporting people bereaved through advanced illness: a systematic review of the evidence and development of a core outcome set for bereavement research in palliative care, http://www.comet-initiative.org/studies/details/739?result=true (2018, accessed 1 October 2019).