Abstract
Coronavirus disease 2019 cases in India continue to increase and are expected to peak over the next few weeks. Based on some projection models, India is expected to have more than 10 million cases by September 2020. The spectrum of disease can vary from mild upper respiratory tract symptoms to life-threatening acute respiratory distress syndrome and multi-organ failure requiring intensive care. Even if less than 5% of patients require critical care services, this will still rapidly overwhelm the healthcare system in a country, where intensive care services and resources are scarce and unevenly distributed. In this perspective article, we highlight the critical care preparedness of India for the pandemic and the associated challenges.
Keywords: COVID-19, critical care, India
Introduction
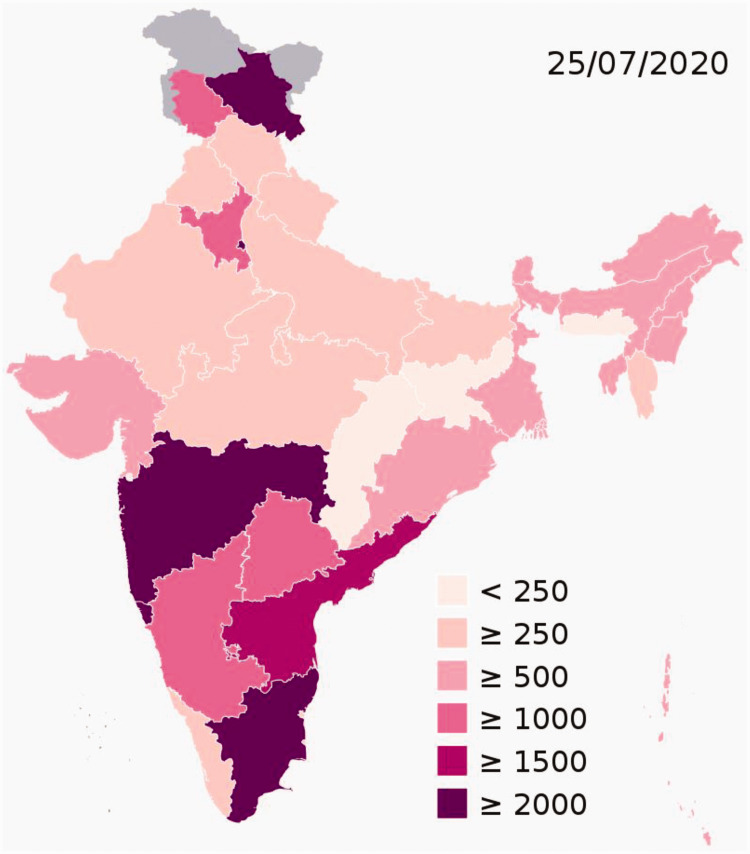
The Coronavirus Disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has resulted in more than 15 million infections and 628,903 deaths worldwide to date. 1 India, currently, has the largest number of confirmed cases in Asia and the third highest number of COVID-19 infections worldwide. 1 As of 25 July 2020, the Ministry of Health and Family Welfare (MoHFW) has confirmed a total of over 1.3 million cases, and 31,358 deaths in the country. 2 India's case fatality rate is relatively lower at 2.40%, 3 against the global 4.7%, as of 25 July. Six cities account for around half of all reported cases in the country – Mumbai, Delhi, Ahmedabad, Chennai, Pune and Kolkata4 (Figure 1).
Figure 1.
Distribution of COVID-19 cases in India.
Source: Adapted from Wikipedia: https://en.wikipedia.org/wiki/COVID-19_pandemic_in_India
India’s approach to the pandemics in the past two decades has been consistent and broadly in keeping with the WHO recommendations. India focused largely on diligent screening of incoming passengers and quarantine, focused testing, isolation of cases, expansion of hospital beds and contact tracing. The emergence and rapid spread of the SARS–CoV-2, however, poses challenges of a hitherto unseen scale.
While there are well promulgated international guidelines for the management of COVID-19,5,6 there are unique challenges to the delivery of critical care in India, given its diversity in cultures, systems, healthcare access and economic disparities. In this commentary, we focus on the challenges of delivering critical care services in India during the pandemic.
Population, population density and caseload
India has a population of 1.3 billion people 7 and is one of the most densely populated countries in the world with a population density of 382 people per square kilometre. 8 This, coupled with family structures where several generations live together in the same household limit the ability and efficacy of social distancing measures in containing the pandemic. Consequently, if modelling projections are realized, by October 2020, India will have more than 10 million cases (range 5–15 million). 9 In addition, the prevalence of patients with type 2 diabetes and hypertension in India is one of the highest in the world which places the population at a higher risk of developing severe COVID-19 disease.10,11
Projected number of ICU admissions
About 20% of patients with confirmed infection require hospitalization and 5% require admission to an intensive care unit (ICU) for worsening respiratory failure with hypoxemia or for supportive care for other organ failures.12,13 These numbers are variable between countries and in India, data from the Ministry of Health and Family Welfare (MoHFW) suggest that around 2.5% of patients require intensive care. 14 This is likely an underestimate as several states have not reported the breakdown of illness severity. Even if these numbers are staggered and assuming that 2.5% of patients would need critical care (125,000–375,000), this case-burden would overwhelm any healthcare system in the world.
Management of patients with mild COVID-19: Availability of an oxygen bed
The WHO guidelines recommend the use of oxygen for patients with mild to moderate COVID-19. 5 The WHO estimates that with 1 million new infections a week, the global requirement for oxygen is estimated to be about 620,000 cubic metres per day. 15 According to the MoHFW in India, as of 28 June 2020, there are 1,055 dedicated COVID hospitals with 177,529 isolation beds and 78,060 oxygen supported beds; there are 2,400 dedicated COVID Health Centres with 140,099 isolation beds and 51,371 oxygen supported beds. 16 In total, there are about 120,000 oxygen supported beds. It is estimated that 15% of patients will have mild to moderate infection requiring oxygen beds, which will translate to about 1.5 million patients in India. Even if the need is staggered, this demand will rapidly outstrip supply. This pressure on beds has been evidenced by the need to utilize train carriages as wards to create more bed spaces. 17
Intensive care capacity in India and resource availability
In India, dedicated ICUs began to emerge in the early 1970s with the establishment of the first ICU in Mumbai. 18 In the last three decades, dedicated intensive care facilities have been set up in all the major Indian cities and larger towns.
Despite the progress, there are limited data on organizational aspects such as resource availability (e.g. number of negative pressure rooms, access to non-invasive and invasive ventilation, intravenous fluids, etc.) and personnel (critical care nurses, doctors and allied health specialists).
ICU bed capacity
Estimates from a recent cross-sectional study 19 of 23 Asian countries and regions (covering 92% of the continent’s population) indicate that there are cumulatively 3.6 critical care beds per 100,000 population. In contrast, Germany and Canada have 29.2 and 12.9 beds per 100,000 population, respectively. In India, the estimation is 29,997 ICU beds (3.7% of acute hospital beds) constituting 2.3 beds per 100,000 population (Table 1). 19 Much of the data in this study come from a database held by a private pharmaceutical company in India, and there are no public databases of total ICU bed capacity. These numbers are likely an underestimate, and other models (which assume 5%–8% of hospital beds are critical care beds) estimate total ICU bed capacity to be nearly 95,000. 20
Table 1.
Estimates of critical care resource availability across India.
| Critical care resource | Estimates of availability | Comments |
|---|---|---|
| Beds | 2.3 beds per 100,000 population | In comparison, Germany has 29.2 ICU beds a and Canada has 12.9 ICU beds per 100,000 population. b Among LMICs, Mongolia has 8.8 beds per 100,000 and Nepal has 2.8 beds per 100,000 population. 19 |
| Beds with capacity for O2 supply | 12,0000 beds16 | |
| Ventilators | 15,000–48,000 | Large variations in estimates depending on source of information. |
| Human resources: Total number of doctors ICU doctors Total number of nurses Nurses with ICU training | 1:1457 population No reliable estimate 12,000 ICU doctors registered with ISCCM 1.7:1000 No data available | WHO recommended norm: 3 per 1000. |
| PPE c N95 masks c | 334,000 across hospitals in India 1.2 million masks | No data on individual components of PPE and no estimates of anticipated demand. |
ICU: intensive care unit; ISCCM: Indian Society of Critical Care Medicine; LMICs: lower-middle income settings; PPE: personal protective equipment; WHO: World Health Organization.
Additionally, these resources are likely to be further limited in smaller cities, towns and districts. In a cross-sectional survey 21 of intensive care facilities from the state of Madhya Pradesh, a large state in central India, 30 of 49 districts had no ICU facility. Of the remaining 19, more than two-thirds were concentrated in 4 urban districts. These data highlight the huge disparities in access to acute care in India.
Equipment
It has been estimated that about 50% of ICU beds in India have capacity for mechanical ventilation, which puts the number of available ventilators around 15,000. 19 Other estimates have suggested the total number of ventilators to be around 48,000, still far below the numbers that would be essential in the event of a surge (Table 1). 20 To meet the anticipated increase in demand, several Indian companies have been roped in by the Government to rapidly manufacture and deliver ventilators. 22
Although consensus statements from the Indian Society of Critical Care Medicine (ISCCM) have stipulated the minimum number of bedside equipment per bed, 23 there are no published data on the precise number of specific equipment such as infusion pumps, which are essential for the delivery of vital medications such as sedatives, analgesics, inotropes and vasopressors.
Staffing in intensive care units
India currently has 1 doctor for every 1457 citizens (WHO target 1:1000). 24 While the total number of doctors with intensive care training in India is unknown, the ISCCM has 12,046 registered members (including trainees) (Table 1). 25 However, this membership is not evenly distributed, and some states such as Maharashtra have a higher representation (2944 members) when compared to other states which have less than 50 members.
There are similar constraints with nursing capacity, 26 and with major gaps in the availability of trained critical care nurses. Crucially, workforce shortages will be exacerbated due to staff needing to isolate because they develop COVID-19 or come in contact with an infected person. In India, there have been reports of the entire staff of a hospital being asked to isolate when a positive case was reported in that hospital.27,28
Training of healthcare workers
While the position statement of the ISCCM calls for concerted action on training as part of the surge response, 29 concerns have been expressed about the total annual intake of fellows across training programmes in the country. 30 Recognizing the limited availability of trained critical care doctors and nurses, training of non-ICU healthcare professionals has been initiated by some state governments. Thiruvananthapuram, a district in Kerala, was able to train as many as 320 doctors and 180 nurses in the first phase of a critical care training course. 31 Non-ICU healthcare personnel were trained in general ICU care which included operation of various equipment, with an emphasis on ventilator management. The Ministry of Health through the All India Institute of Medical Sciences, New Delhi, has also implemented online training on aspects of critical care management for ICU and non-ICU doctors. 32
Personal protective equipment availability and risk of HCW infection
Appropriate personal protective equipment (PPE) is crucial in ICUs where common treatments for critical illness such as non-invasive ventilation and endotracheal intubation come with a significant risk of aerosol generation. Global data suggest that between 4% and 12% of the total number of COVID cases have been in healthcare workers (HCWs).12,33 In a recent international multi-centre study of HCWs performing intubation for COVID-19 patients, 10.7% developed symptoms suggestive of or laboratory-confirmed COVID-19 infection. 34 In another recent Lancet publication, 44% of 200 frontline HCWs were either positive by a reverse transcriptase-polymerase chain reaction SARS-CoV-2 test or through serology. 35 In India, there are several media reports of HCWs being infected36,37; however, there are no reliable estimates. In a recent press release, the Indian Medical Association has reported over 90 deaths of medical personnel on duty from its database. 38
While early reports indicated widespread shortage of PPE in India, in a recent report from the government of India, an estimated 600,000 PPE kits are being manufactured every day, with a surplus available for export, 39 although concerns remain about quality. 40 With the increasing caseload, any loss of healthcare personnel to infections would pose additional challenges in controlling the pandemic.
Challenges in implementing International Critical Care Guidelines for COVID-19 in India
In March 2020, the European Society of Intensive Care Medicine and the Society of Critical Care Medicine (SCCM) jointly published the Surviving Sepsis Campaign guidelines for the management of critically ill adults with COVID-19. 6 Although the scope of these guidelines extends to both high and low-middle income settings, there are several challenges in implementing these recommendations in lower-middle income settings.
Three of the best practice statements from these guidelines relate to infection control - performing aerosol-generating procedures on ICU patients with COVID-19 in a negative pressure room, using fitted respirator masks (N95 respirators, FFP2 or equivalent) and tracheal intubations to be performed by the most experienced airway operator. While the latter is feasible, the first two will be challenging to implement uniformly across India. Few ICUs have negative pressure rooms. While PPE availability has substantially improved since April, there is variability in the access to N95, FFP2 or equivalent masks, and resource limitations have forced some centres to use surgical masks with face shields or hoods. 41 The fourth statement relates to patients receiving non-invasive ventilation (NIV) or high flow nasal oxygen (HFNO). However, NIV and HFNO are not uniformly available in India. To overcome these limitations, there is a pressing need for investment in home-grown frugal innovations in oxygen delivery devices that may be able to reduce the need for higher level care and in the design of physical spaces that can provide the capacity for isolation.
Potential innovations in delivery of pandemic critical care
With increase in case load and hospitalization, there is an urgent need for innovative and context-specific solutions. Globally, the use of tele-medicine for the delivery of COVID and non-COVID care in ICUs has sparked great interest. 42 The advantages of tele-critical care include efficient screening and triage of patients to appropriate levels of care (telemetry unit vs high dependency unit (HDU) vs ICU), ability to provide remote monitoring and consultation decreasing the time of direct HCW exposure, increased compliance with evidence-based best practices and in counselling families of critically ill patients. The enhanced efficiency of care provided by a central tele-critical care unit in managing several HDUs/ICUs is of particular relevance to resource-constrained settings. 43 However, technological challenges such as lack of bandwidth in remote locations are a barrier to widespread adoption.
Affordable healthcare innovations are being attempted for patients without the requirement for mechanical ventilation, but still needing oxygen therapy. These include the use of prone high flow and 3D-printed PEEP valve fitted O2 masks. 45 Ideally, these treatments must be evaluated in randomized controlled trials.
Lack of negative pressure rooms may be addressed by adequately ventilated single rooms, cohorting confirmed mild cases in larger well ventilated rooms with adequate space between beds, and the use of multiple exhaust fans in single rooms with the addition of stand-alone HEPA filters. 46
Research response
As the second most populous country in the world and with a unique set of challenges, India must participate in the global research response. This can assume several forms – describing COVID-19 case mix and outcomes among patients requiring intensive care, observational research on long-term outcomes for survivors of critical illness, and research in diagnostics and therapeutics. This is important, since the differences in demographic characteristics of populations have been postulated as an important reason for variations in presentations and outcomes from COVID-19.
It is vital that ICUs focus on harmonized data collection to accurately describe case-mix and outcomes. There are existing tools for such an undertaking such as the ISARIC-WHO template. 47 Another approach involves the use of existing critical care registries such as CHITRA (Customized Health in Intensive Care, Trainable Research and Analysis Tool), 48 and the Indian Registry of IntenSive care (IRIS) 49 for describing epidemiology and outcomes. IRIS currently links 15 ICUs in India and has already enabled a pandemic data collection form on the registry.
In a welcome move, India has joined the WHO-led SOLIDARITY trial. The country has contributed over 450 participants to the trial, and over 5800 patients have been enrolled globally. There are, however, several challenges to the deployment of the research response in India, 50 and investigators across the country should work in collaboration with Indian Council of Medical Research and other regulatory bodies to generate high-quality and context-specific data.
Conclusion
The COVID-19 pandemic has placed an unprecedented demand on the healthcare system in India. With a population exceeding 1.3 billion and the majority living in rural and remote regions, critical care and public health capacity in India face enormous pressure. Moreover, the pandemic is expected to persist for a longer duration, and given India’s unique circumstances, the flattening of the curve will take longer. With the anticipated increase in case numbers, a coordinated effort by various public health organizations and the ISCCM will be crucial for ensuring adequate delivery of intensive care to critically ill COVID-19 patients.
Footnotes
Declaration of conflicting interest: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: BKTV is Site Investigator for the SOLIDARITY trial. JVD reports personal fees paid to his institute from Edwards India, outside the submitted work.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Bharath Kumar Tirupakuzhi https://orcid.org/0000-0002-1801-0667
References
- 1.https://covid19.who.int/ (accessed 25 July 2020).
- 2.https://www.mohfw.gov.in/ (accessed 25 July 2020).
- 3.http://covidindiaupdates.in/ (accessed 25 July 2020).
- 4.https://en.wikipedia.org/wiki/COVID-19_pandemic_in_India (accessed 25 July 2020).
- 5.https://www.who.int/publications/i/item/clinical-management-of-covid-19 (accessed 25 July 2020).
- 6.Alhazzani W, Moller MH, Arabi YM, et al. Surviving Sepsis Campaign: Guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Intens Care Med 2020; 46: 854–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.https://data.worldbank.org/indicator/SP.POP.TOTL?locations=IN (accessed 25 July 2020).
- 8.https://www.niti.gov.in/niti/content/population-density-sq-km (accessed 25 July 2020).
- 9.https://cddep.org/wp-content/uploads/2020/04/India-Shutdown-Modeling-Slides-Final-2.pdf (accessed 7 July 2020).
- 10.https://www.medrxiv.org/content/10.1101/2020.03.17.20037572v1.full.pdf (accessed 25 July 2020).
- 11.Geldsetzer P, Manne-Goehler J, Theilmann M, et al. Diabetes and hypertension in India: A nationally representative study of 1.3 million adults. JAMA Intern Med 2018; 178: 363–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019(COVID-19) outbreak in China: Summary of a report of 72314 cases from the Chinese centre for disease control and prevention. JAMA 2020; 323: 1239–1242. [DOI] [PubMed] [Google Scholar]
- 13.Guan W, Ni Z, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382: 1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.https://www.indiaspend.com/few-covid-19-patients-need-ventilators-yet-mumbai-is-falling-short-heres-why/ (accessed 25 July 2020).
- 15.https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—24-june-2020 (accessed 25 July 2020).
- 16.https://content.pib.iostechtools.com/1634928/web.html (accessed 25 July 2020).
- 17.https://economictimes.indiatimes.com/news/politics-and-nation/rail-coaches-for-isolation-of-covid-19-patients-operationalised/articleshow/76514580.cms (accessed 25 July 2020).
- 18.Prayag S. ICUS worldwide: Critical care in India. Crit Care 2002; 6: 479–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Phua J, Faruq OM, Kulkarni AP, et al. Critical care bed capacity in Asian countries and regions. Crit Care Med 2020; 48: 654–662. [DOI] [PubMed] [Google Scholar]
- 20.https://cddep.org/wp-content/uploads/2020/04/State-wise-estimates-of-current-beds-and-ventilators_24Apr2020.pdf (accessed 25 July 2020).
- 21.Saigal S, Sharma JP, Pakhare A, et al. Mapping the characteristics of critical care facilities: assessment, distribution, and level of critical care facilities from central India. Indian J Crit Care Med 2017; 21: 625–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.https://www.thehindu.com/news/national/covid-19-bel-to-make-30000-ventilators-within-two-months-defence-ministry/article31377555.ece (accessed 25 July 2020).
- 23.https://isccm.org/pdf/Section1.pdf (accessed 25 July 2020).
- 24.https://www.business-standard.com/article/pti-stories/india-has-one-doctor-for-every-1-457-citizens-govt-119070401127_1.html (accessed on 25 July 2020).
- 25.https://isccm.org/ (accessed 25 July 2020).
- 26.https://www.indiaspend.com/indias-shortage-of-doctors-nurses-may-hamper-covid19-response/ (accessed 25 July 2020).
- 27.https://timesofindia.indiatimes.com/city/hyderabad/50-niloufer-staff-quarantined/articleshow/75240281.cms (accessed 25 July 2020).
- 28.https://www.businessinsider.in/india/news/lucknow-private-hospital-shut-kgmu-staff-quarantined-after-man-tests-positive-for-covid-19/articleshow/75139783.cms (accessed 25 July 2020).
- 29.Mehta Y, Chaudhry D, Abraham OC, et al. Critical care for COVID-19 patients: Position statement of the Indian Society of Critical Care Medicine. Indian J Crit Care Med 2020; 24): 222–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ozair A, Agrawal A, Siddiqui SS. Training and delivery of critical care medicine in India: Concerns revealed by COVID-19 pandemic. Indian J Crit Care Med 2020; 24: 285–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.https://www.newindianexpress.com/cities/thiruvananthapuram/2020/may/03/hands-on-training-in-critical-care-to-take-on-covid-19-pandemic-2138462.html (accessed 25 July 2020).
- 32.https://www.mohfw.gov.in/pdf/MechanicalVentilationWebinarAIIMSNewDelhi.pdf (accessed 25 July 2020).
- 33.https://www.epicentro.iss.it/en/coronavirus/bollettino/Infografica_22maggio%20ENG.pdf (accessed 25 July 2020).
- 34.El-Boghdadly K, Wong DJN, Owen R, et al. Risks to healthcare workers following tracheal intubation of patients with COVID-19: a prospective international multicentre cohort study. Anaesthesia. Epub ahead of print 09 June 2020. DOI: 10.1111/anae.15170. [DOI] [PMC free article] [PubMed]
- 35.Houlihan CF, Vora N, Byrne T, et al. Pandemic peak SARS CoV-2 infection and seroconversion rates in London frontline healthcare workers. Lancet 2020; 396: e6–e7, 10.1016/S0140-6736(20)31484-7. [DOI] [PMC free article] [PubMed]
- 36.https://timesofindia.indiatimes.com/city/chennai/17-stanley-hospital-doctors-test-positive/articleshow/75905204.cms (accessed 25 July 2020).
- 37.https://www.thehindu.com/data/how-many-doctors-and-nurses-have-tested-positive-for-coronavirus-in-india/article31410464.ece (accessed 25 July 2020).
- 38.https://southasiamonitor.org/india/100-doctors-die-covid-ima-issues-red-alert-healthcare-staff (accessed 25 July 2020).
- 39.https://theprint.in/health/modi-govt-to-allow-ppe-ventilator-exports-as-indian-companies-are-mass-producing-them-now/447460/ (accessed 25 July 2020).
- 40.https://www.hindustantimes.com/india-news/new-rules-to-improve-ppe-quality-issued-after-medics-flag-concerns/story-hbEBQOCxLFyRhqv9prxaUN.html (accessed 25 July 2020).
- 41.https://www.thenewsminute.com/article/are-indian-healthcare-workers-being-provided-right-kind-masks-126025 (accessed 25 July 2020).
- 42.Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med 2020; 382: 1679–1681. [DOI] [PubMed] [Google Scholar]
- 43.Ramakrishnan N, Tirupakuzhi Vijayaraghavan BK and Venkataraman R. Breaking barriers to reaching farther: a call for urgent action on Tele-ICU services. Indian J Crit Care Med 2020 ; 24(6): 393–397, https://www.ijccm.org/doi/IJCCM/pdf/10.5005/jp-journals/-10071-23447. [DOI] [PMC free article] [PubMed]
- 44.Sartini C, Tresoldi M, Scarpellini P, et al. Respiratory parameters in patients with COVID-19 after using noninvasive ventilation in the prone position outside the intensive care unit. JAMA 2020; 323(22): 2338–2340, doi:10.1001/jama.2020.7861. [DOI] [PMC free article] [PubMed]
- 45.https://www.materialise.com/en/blog/3d-printed-peep-mask-alleviate-ventilator-shortage (accessed 7 July 2020).
- 46.Phua J, Weng L, Egi M, et al. Intensive care management of coronavirus disease 2019(COVID-19): challenges and recommendations. Lancet Respir Med 2020; 8: 506–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.https://isaric.tghn.org/covid-19-clinical-research-resources/ (accessed 25 July 2020).
- 48.https://isccm.org/chitra.aspx (accessed 25 July 2020).
- 49.http://www.irisicuregistry.org/ (accessed 25 July 2020).
- 50.Tirupakuzhi Vijayaraghavan BK, Venkataraman R, Ramakrishnan N. Critical care epidemiology and research in the face of a pandemic: an opportunity in a crisis. Indian J Crit Care Med 2020; 24: 242–244. [DOI] [PMC free article] [PubMed] [Google Scholar]