Highlights
-
•
Health coaching is an effective intervention to improve adolescent contraceptive use outcome.
-
•
A microsimulation model of teen pregnancy was developed and used to assess the health and economic impact of a health coaching intervention to prevent teen pregnancy.
-
•
Health coaching intervention for adolescent contraceptive use is cost-effective.
Keywords: Teen pregnancy, Community health, Health coaching, Economic evaluation
Abstract
Teenage pregnancy is an important public health issue in the United States, presenting significant health and economic risks to adolescents and the society. Health coaching is a potentially effective intervention in preventing teen pregnancy. In 2017, the Children’s Hospital of Philadelphia implemented a health coaching program among sexually active teenage girls, which improved their contraceptive continuation rates. However, the cost-effectiveness of the health coaching program is not clear. We developed a microsimulation model of teen pregnancy that can predict the number of teen pregnancies and related birth outcomes. Model parameters were estimated from the literature and the health coaching program. The teen pregnancy model was used to assess how the program could influence direct health care costs and pregnancy outcomes. Our model projected that the health coaching program could prevent 15 teen pregnancies per 1000 adolescents compared to no intervention. The incremental cost-effectiveness ratio (ICER) for the intervention was $309 per pregnancy prevented, which was less than the willingness-to-pay threshold of $4,206 per pregnancy. Thus, the health coaching intervention was cost-effective. Our study provides promising data on the effectiveness and cost-effectiveness of a health coaching intervention to reduce the burden of teen pregnancies. Health practitioners should consider implementing the program for a longer term and at a larger scale.
1. Introduction
Despite years of national decline, teen pregnancy rates remain high in many states (Centers for Disease Control and Prevention, 2020). In the state of Pennsylvania, there were 5,264 births among teens aged 15–19 in 2019, which represented a teen birth rate of 13.3 births per 1,000 girls (Power to Decide, 2020). The teen birth rate in Pennsylvania has decreased by 72% from 1991 to 2019; however, disparities remain among racial and ethnic minorities (Power to Decide. Pennsylvania Data.;, 2020, Carlson et al., 2014). In 2019, the teen birth rate for non-Hispanic Black and Hispanic teens in the state was more than triple the rate of their non-Hispanic White counterparts (Power to Decide, 2020). These disparities reinforce the reality that systemic issues perpetuate disproportionality in teen pregnancy rates and must be addressed to reduce rates of teen pregnancy among vulnerable subpopulations.
Over half of the cost burden of unintended teen pregnancy can be linked to poor contraceptive continuation, a key driver of unintended teen pregnancy (Martin et al., 2011). A teen’s decision to continue or discontinue using their contraceptives is influenced by community and societal factors such as education, access to family planning and health services, and cost (Cohen et al., 2016, Furstenberg et al., 1983). Yet, most teen pregnancy prevention interventions focus on addressing individual-level factors, rather than multi-level factors. Addressing these systemic, multi-level influences calls for more high-level complex interventions that incorporate multiple and/or inter-linking strategies that take a “whole of problem” approach to teen pregnancy prevention (TPP) (Willis et al., 2012). These types of TPP interventions are in direct juxtaposition with the traditional interventions targeting individual behavior change like contraception use with the underlying assumption that behavior change occurs in a siloed, individual fashion (Goesling et al., 2014, Garney et al., 2019, McLeroy et al., 1988).
In 2017, the Children’s Hospital of Philadelphia (CHOP) implemented a systems-focused health coaching program among sexually active teenage girls to improve contraceptive continuation rates and prevent teen pregnancies. The effectiveness of the program has been documented (Amutah et al., 2021, Fields et al., 2021). Specifically, Amutah et al. compared intervention completion rates among adolescents and young adults with and without a previous pregnancy or sexually transmitted infection participating in the health coaching program to improve contraception adherence rate (Amutah et al., 2021). The study included females ages 14 to 22, sexually active in the past year, not desiring pregnancy in the next year, and starting a new contraception. The patients underwent monthly health coaching intervention to improve contraception continuation, which was continued for 5 months. The study found those with previous adverse reproductive outcome (history of sexually transmitted infections and/or previous pregnancy) to be less likely to engage in sexual risk reduction interventions, such as the health coaching sessions. In addition, the study by Fields et al. sought to identify opportunities to incorporate HIV pre-exposure prophylaxis (PrEP) education in contraceptive counseling in adolescent females and young women (Fields et al., 2021). This study was a secondary analysis of data from the Health Coaching for Contraceptive Continuation pilot study, which is the main pilot study used for our study model building. It included 21 participants who completed more than four monthly health coaching sessions. The researchers found multiple opportunities to introduce PrEP counseling within contraception counseling to this age group. Although both studies found the health coaching intervention effective, its cost-effectiveness is unknown.
Simulation modeling can help public health practitioners and policymakers assess the cost-effectiveness of an intervention (McGill et al., 2021, Ramsey et al., 2005). In particular, a well-designed simulation model can generate a synthetic patient cohort similar to the population of interest, predict their health outcomes and health care costs under the studied intervention and no intervention, and calculate the comparative cost-effectiveness of the studied intervention.
In this study, we used a microsimulation model of teen pregnancy outcomes to assess the health and economic impact of the health coaching program implemented by the CHOP. The health coaching program, named the Health Coaching for Contraceptive Continuation (HC3) program, is a systems-focused, theory-driven intervention that aims to address barriers in contraceptive use at multiple levels. Using data from the HC3 program, we aim to examine the cost-effectiveness of the program, which may provide additional evidence supporting the potential large-scale implementation of the program.
2. Methods
2.1. Program description
The HC3 program was implemented in 2017 in Philadelphia, PA. Participants were recruited from three urban clinics affiliated with the CHOP, including an adolescent specialty clinic and two Title X adolescent family planning clinics. Ethical review and approval were provided by the CHOP Institutional Review Board and AccessMatters, the local Title X funding agency that oversaw operations at the Title X sites. A Federal Certificate of Confidentiality was obtained to provide further privacy protections for research subjects.
The HC3 program was designed based on the theory of the Integrative Model of Behavioral Prediction (IMBP), which has been used to guide evidence-based pregnancy prevention interventions and includes constructs with strong, empirical evidence that they predict both contraceptive use and pregnancy risk (Sutton and Walsh-Buhi, 2017). In the IMBP, engagement in a target behavior is determined by behavioral intentions. The HC3 program requested health coaches to increase behavioral intentions by providing tailored reproductive health education that addresses sexual health knowledge gaps and contraception misconceptions. The program will also improve cognitive and interpersonal factors related to teen pregnancy prevention such as shared contraceptive decision-making, method satisfaction, quality of life, distress tolerance, experiential avoidance, patient-coach alliance, and expectations of treatment effect.
In the HC3 program, two sexual health educators with more than five years of experience completed a manualized four-week health coach training program. The program oriented the coaches to the health coaching role relative to other care team members; highlighted effective communication strategies; taught strategies for tapping into participants’ learning styles; and provided tools and activities for facilitating goal setting, measuring behavior change, building self-management skills and accountability. In addition, health coaches received training for motivational interviewing, a communication strategy used to facilitate client behavior change by activating intrinsic motivation to consistently use contraception. Motivational interviewing has been used in previous studies for contraception use and pregnancy prevention (Lopez et al., 2013, Lopez et al., 2016, Halpern et al., 2013). Health coaches also learned behavior change strategies grounded in Acceptance and Commitment Therapy, which increases willingness to experience undesired thoughts, feelings, and sensations, while maintaining engagement in certain behaviors (Mak and Loke, 2015, DuFrene and Wilson, 2012). This translated to helping young women to recognize and accept undesired thoughts and feelings about contraceptive uses (e.g., about undesired side effects, or the inconvenience of dosing requirements). Health coaches fostered clients’ willingness to experience these cognitions without acting upon them. Finally, the HC3 program was developmentally tailored to improve emotional regulation and problem-solving skills related to contraceptive use. This was achieved through augmenting contraceptive knowledge, refocusing attention on family planning goals when barriers to contraceptive use were encountered, supporting cognitive information processing that maximized goal achievement, and highlighting motivational difficulties.
2.2. Program participants
There were 33 participants in the HC3 program. Eligible participants were aged 14–22 years, sexually active with a male in the prior 12-months, not desiring pregnancy in the next 12-months, English-speaking, able to provide written informed consent, and had started a new contraceptive method in the prior 14 days. Women were eligible if they had initiated a short acting reversible contraceptive method (SARC: progestin-only pill, combination estrogen-progestin pill, transdermal patch, vaginal ring, intramuscular progestin shot) or a long-acting reversible contraceptive method (LARC: IUD or subdermal implant). Women were approached in-person at the visit when a new method was started, or by phone within 14 days following initiation of a new method. Study participants completed a baseline visit during which coaches conducted a semi-structured interview to identify factors that influenced participants’ decisions to use contraception and the method selected. Coaches used the baseline interview to collaboratively develop a coaching plan – a structured tool for identifying and addressing each participant’s reproductive health information gaps, contraceptive self-management needs, and individualized unique supports and perceived personal and systemic (e.g., transportation, health care access, social support) barriers to correct, consistent contraceptive use. A baseline questionnaire assessed participants’ demographics, medical and sexual histories, pregnancy intentions, and attitudes towards pregnancy.
After the baseline visit, participants engaged in monthly coaching sessions during the 6 months after initiation of a new contraceptive. Sessions lasted approximately 30 min and participants had the same coach for all study visits. Monthly questionnaires assessed self-reported contraceptive continuation and method adherence for users of short-acting methods, which were corroborated through review of electronic medical records and pharmacy refill records. Three months and 6-months after enrollment, follow-up questionnaires were administered to update participants’ medical and sexual histories. After completing the program, participants completed an exit interview to assess program acceptability.
The main outcome measure for the HC3 program is contraceptive continuation, which was defined as correct, consistent contraceptive use throughout the six-month study period and assigned based on self-report (on the monthly survey and coaching visit transcripts) and corroborated by EMR data.
2.3. Model development
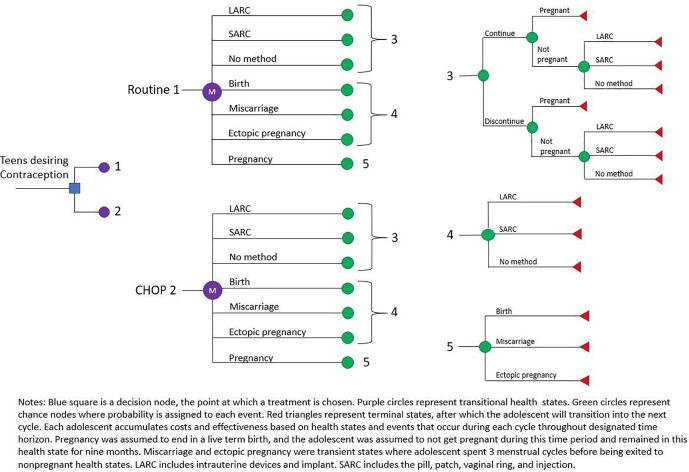
We used a microsimulation model of teen pregnancy to assess the cost-effectiveness of the HC3 program. In a previous study, we used the model to assess the cost-effectiveness of a school-based teen pregnancy prevention program in New York City (Kim et al., 2021). For the current study, we recalibrated the model based on the specific program data from the CHOP. Fig. 1 shows the structure of the model. Briefly, the model can generate a cohort of adolescents with specified characteristics and simulates their contraceptive activities, pregnancy rate, and birth outcomes. For the simulation experiments, we simulated 10,000 hypothetical adolescents in each of the two arms – the HC3 program (Fig. 1, CHOP 2) and routine care (Fig. 1, Routine 1). The basic simulation cycle was one month.
Fig. 1.
Structure of the teen pregnancy model.
When we run the model, in the first cycle, adolescents enter one of the two intervention arms and select a contraceptive method: SARC, LARC or no method. Subsequent cycles reflect contraceptive continuation rates and pregnancy states. At the pregnancy chance node, the adolescent will either give birth, have a miscarriage, or have an ectopic pregnancy based on probabilities drawn from the literature (Table 1). The model does not include induced abortion as Pennsylvania Medicaid does not cover costs of induced abortion. To simplify the model, we assumed that individuals in the birth state will remain for nine cycles (months), whereas individuals in miscarriage and ectopic pregnancy nodes will remain for three cycles. The same assumptions were made in other recent cost-effectiveness analysis studies (Kim et al., 2021, Bellows et al., 2018), where nine cycles were chosen to reflect the time a person remains pregnant with term pregnancy birth and three cycles were chosen to reflect the conservative amount of time before ovulation returns after a miscarriage or ectopic pregnancy. The model was programmed using the software TreeAge Pro 2020 (Pro and Software, 2015).
Table 1.
Model parameters and data sources.
| Parameter | Base Case (%) | Range in sensitivity analysis | Data sources |
|---|---|---|---|
| Baseline contraceptive use rate | Obijuru et al. (Obijuru et al., 2016) | ||
| Implant | 3 | 2.25–3.75 | |
| Intrauterine device | 3 | 2.25–3.75 | |
| DMPA | 13 | 9.75–16.25 | |
| Oral contraceptive pills | 2 | 1.5–2.5 | |
| Patch | 2 | 1.5–2.5 | |
| Condom | 35 | 26.25–43.75 | |
| No method | 42 | 31.5–52.5 | |
| Annual Contraceptive failure rate | Trussell and Wynn25 | ||
| Implant | 0.05 | 0.0375–0.0625 | |
| Levonorgestrel intrauterine device | 0.2 | 0.15–0.25 | |
| Copper intrauterine device | 0.8 | 0.6–1.0 | |
| DMPA | 6 | 4.5–7.5 | |
| Combined hormonal pill, patch, ring | 9 | 6.75–11.25 | |
| Condom | 18 | 13.5–22.5 | |
| No method | 85 | 63.7–100 | |
| Continuation rates for teens 14–19 at 1 year | Rosenstock et al. (Rosenstock et al., 2012) | ||
| Nexplanon | 82.2 | ||
| Copper intrauterine device | 76.5 | ||
| Levonorgestrel intrauterine device | 80.6 | ||
| DMPA | 47.3 | ||
| Oral contraceptive pills | 46.7 | ||
| Patch | 40.9 | ||
| Ring | 31 | ||
| Pennsylvania teen pregnancy outcomes | Kost et al. (Kost et al., 2017) | ||
| Live birth | 59 | ||
| Spontaneous abortion | 14.4 | ||
| Ectopic pregnancy22 | 0.8 | ||
| CHOP HC3 program outcomes at 6 months | The HC3 program | ||
| LARC continuation rate | 60 | ||
| SARC continuation rate | 76.9 | ||
| Cost on contraceptive methods | IBM Micromedex RED BOOK27 | ||
| Implant | $1,068.36 | ||
| Levonorgestrel intrauterine device | $11,117.49 | ||
| Copper intrauterine device | $970.20 | ||
| DMPA | $81.52 | ||
| Oral contraceptive pills | $32.00 | ||
| Patch | $152.69 | ||
| Vaginal ring | $195.16 | ||
| Cost on pregnancy outcomes | Sonfield et al. (Sonfield and Kost, 2015) | ||
| Live birtha (PA) | $11,015.00 | ||
| Spontaneous abortion (PA) | $1,080.00 | ||
| Ectopic pregnancy (national) | $7,590.00 | Bellows et al. (Bellows et al., 2018) |
Live birth period includes prenatal, labor and delivery, and 12 months of infant care.
2.4. Model parameters
Table 1 presents major model parameters and their data sources. In our study, SARCs include progestin-only pill, combination estrogen-progestin pill, transdermal patch, vaginal ring, and intramuscular progestin shot. LARCs include IUD and the subdermal contraceptive implant. We used the weighted average of each contraceptive method to calculate the overall weighted averages of SARCs and LARCs. For example, we used the failure rate for each method from the literature and multiplied this rate by the proportion of adolescents who used the method to obtain the weighted failure rate. We then calculated the sum of the weighted averages to obtain the overall failure rates for SARCs and LARCs. We used logarithmic conversion to transform the calculated annual rates into monthly rates to be consistent with our model specification.
Baseline contraceptive use rates for this age group, failure rates, and continuation rates were derived from the literature (Obijuru et al., 2016, Trussell and Wynn, 2008, Rosenstock et al., 2012). For example, based on Obijuru et al, 35% of adolescents used condoms and only 3% of them used implants as contraceptive methods (Obijuru et al., 2016). Based on Trussell and Wynn, condoms had an 18% failure rate, and the failure rate for contraceptive implants, in comparison, was only 0.05% (Trussell and Wynn, 2008). Based on data from the HC3 program, 10 out of 13 LARC users and 12 out of 20 SARC users continued their use at 6 months, which gives 76.9% (10/13) and 60% (12/20) continuation rates for LARC and SARC, respectively. We used a US payer perspective for our analysis and included only direct medical costs. Baseline costs of contraceptives were based on the Red Book online database (Analytics et al., 2020). We used data from the Centers for Disease Control and Prevention to estimate Pennsylvania specific teen birth rates and pregnancy outcomes (Power to Decide, 2020). We used consistent data in both intervention and control arms except for continuation rates to minimize reasons for variation. Any difference between the two arms can be attributed to the intervention (HC3) and not to any other causes.
In the simulation experiments, we reported the number of averted pregnancies as the difference in the projected number of pregnancies between the HC3 program and routine care. We also calculated the estimated healthcare costs for adolescents participating in the HC3 program and routine care. Finally, we calculated the incremental cost-effectiveness ratio (ICER), which measures the average incremental cost associated with one additional pregnancy averted.
3. Results
3.1. Baseline results
Table 2 summarizes results from our baseline analysis, which showed that the total healthcare costs for adolescents participating in the HC3 program were $4,584/person (95% CI $4,367 - $4,799) compared to $4,579/person (95% CI $4,364 - $4,793) for those receiving regular family planning services after one year. Although the intervention program would cost more compared to regular health care in one year, it could prevent an additional 15 teen pregnancies per 1,000 adolescents compared to regular health care based on the simulation results. The ICER for the HC3 program was $309 per pregnancy prevented, which was less than our willingness-to-pay threshold of $4,206 per pregnancy (Kim et al., 2021, Kost et al., 2017). This means that the HC3 program was cost-effective compared to regular health care.
Table 2.
Baseline cost effectiveness results in 1, 3, and 5 years.
| Costs ($) | No. of pregnancies averted (per 1000 persons) | ICER ($/pregnancy) | Less than WTP | ||
|---|---|---|---|---|---|
| Year 1 | Baseline | 4,579 (4,364–4,793) | |||
| HC3 | 4,584 (4,367–4,799) | 15 | 309 | YES | |
| Year 3 | Baseline | 17,076 (16,669–17,483) | |||
| HC3 | 17,049 (16,635–17,463) | 42 | 630 | YES | |
| Year 5 | Baseline | 29,662 (29,131–30,193) | |||
| HC3 | 29,654 (29,130–30,178) | 72 | 101 | YES |
Notes: Numbers in parentheses are 95% confidence intervals.
HC3 = Health Coaching for Contraceptive Continuation; ICER = incremental cost-effectiveness ratio; WTP = willingness to pay=$4,206.
3.2. Sensitivity analysis
Table 2 also presents results from one of our sensitivity analyses by varying the time horizon from one to three, and five years. In a three-year time frame, the cumulative healthcare costs for participants in the HC3 program would be $17,049/person (95% CI $16,635 - $17,463) compared to $17,076/person (95% CI $16,669 - $17,483) for regular health care. The HC3 program would prevent 42 additional pregnancies per 1,000 adolescents compared to regular health care over three years. Thus, the HC3 program would be both cost-saving and cost-effective after three years. In five years, the HC3 program would cost $29,654/person (95% CI $29,130 - $30,178) compared to regular health care of $29,662/person (95% CI $29,131 - $30,193). Provision of HC3 program would cost less compared to regular health care and prevent 72 more pregnancies per 1,000 adolescents. Our results showed that the longer the HC3 program is implemented, the greater the cost savings and pregnancies averted. A longer HC3 program would also lead to more positive cost-effectiveness results.
We also conducted one-way sensitivity analysis by varying continuation rates for LARC and SARC among participants in the HC3 program (Table 3). We did not vary costs since cost parameters were assumed to be the same under both the HC3 program and regular health care. Under these conditions, the HC3 program continued to be cost-effective even when the continuation rates for LARC and SARC were varied by 25% compared to regular health care. In these sensitivity analyses, ICER remained below the WTP threshold.
Table 3.
One-way sensitivity analyses over one year.
| Variable | Baseline (%) | Range (+/- 25%) | Baseline ICER | ICER range |
|---|---|---|---|---|
| SARC continuation rate at HC3 | 60 | 35–85 | 309 | 140–4,492 |
| LARC continuation rate at HC3 | 76.9 | 51.9–100 | 309 | 60–2,121 |
Abbreviation: ICER = incremental cost-effectiveness ratio; SARC = short-acting reversible contraception; LARC = long-acting reversible contraception; HC3 = Health Coaching for Contraceptive Continuation.
4. Discussion
This study applied a microsimulation model of teen pregnancy to evaluate the impact of a systems-focused intervention—the HC3 health coaching program—on pregnancy outcomes and healthcare costs. Our findings indicate that the HC3 program would be cost-effective from a public-payer perspective when compared to regular teen pregnancy prevention services for adolescents. These findings are meaningful given the fiscal pressure involved in the financing of public health programs and healthcare services in teen pregnancy prevention, as well as policymakers’ desires to use public payer dollars more efficiently through the support of cost-effective programs.
Beyond the return-on-investment perspective, this study builds on the existing evidence supporting health coaching for pregnancy prevention and behavior change (Goesling et al., 2014, Garney et al., 2019). Data insights demonstrate positive uptake and maintenance of contraceptive use among adolescents involved in health coaching, indicating that program participants can successfully move through health transitions potentially sustain such a behavior change. The health coaching method utilizes a non-traditional, socioecological approach to building complex health navigation skills and health-related knowledge by incorporating tailored health education approaches using existing and interventional interpersonal, community, and organizational-level influences. The simulation model provides a means to study the health and economic impacts from these influences. In addition, results from simulation modeling provide us with a solid foundation for larger, more rigorous evaluation trials as this methodology helps evaluators to better identify what to look for from an influence perspective, how and when to measure this influence, and why the proposed systems-focused intervention is important in a broader context (Green et al., 2013).
Our study provides promising data on the effectiveness and cost-effectiveness of the multi-level teen pregnancy program to increase and sustain uptake of contraception among the target population in Philadelphia. Our modeling results are particularly valuable given the limited data on the utility of contraceptive patient-centered counseling approaches and the paucity of randomized clinical trials in this area (Hoopes et al., 2020). If the program is continued for a longer term and at a larger scale, our modeling results indicate that it has the potential to save public payer funding associated with reduced cases of teen pregnancies. These findings are relevant not only for the program as it is currently designed, but for other programs and potential expansion to other high-need areas in the United States.
Limitations of the present study include uncertainties around several model parameters. Although our sensitivity analyses can partially account for the impact of these uncertainties, they cannot eliminate uncertainties. Future research is needed to provide more empirical data to inform the development of the simulation model and increase model validity. In addition, while the teen pregnancy simulation model captures the influence of health coaching on contraceptive behaviors, the model is a simplification of the real world and, thus, includes assumptions that need to be fully understood before interpreting the results. Finally, our data were from only one health coaching program. It would be better if we could have data from multiple programs to cross validate the model development and research findings.
Despite these limitations, findings from this study may provide evidence to support the implementation of the systems-focused health coaching program at a larger scale or in other settings. If successful, this effort could optimize public funding for teen pregnancy prevention, promote more sustainable teen pregnancy prevention programs, and potentially reduce teen pregnancy rate in the country.
Funding
This research was funded by DHHS-PHS-Office of Adolescent Health under award number TP2AH000046. It was also partly supported by the National Heart, Lung, And Blood Institute of the NIH under Award Number R01HL141427. The study sponsors had no involvement in the study.
CRediT authorship contribution statement
Chi-Son Kim: Data curation, Formal analysis, Methodology, Writing – original draft. Aletha Akers: Conceptualization, Data curation, Writing – review & editing. Daenuka Muraleetharan: Data curation, Writing – original draft. Ava Skolnik: Data curation, Writing – review & editing. Whitney Garney: Conceptualization, Funding acquisition, Validation, Writing – review & editing. Kelly Wilson: Funding acquisition, Validation, Writing – review & editing. Aditi Sameer Rao: Data curation, Writing – review & editing. Yan Li: Conceptualization, Methodology, Supervision, Validation, Writing – original draft.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Centers for Disease Control and Prevention. Teen Birth Rate by State. National Center for Health Statistics, CDC Accessed August 20, 2020. https://www.cdc.gov/nchs/pressroom/sosmap/teen-births/teenbirths.htm.
- Power to Decide. Pennsylvania Data.; 2020. Accessed August 20, 2020. https://powertodecide.org/what-we-do/information/national-state-data/pennsylvania.
- Carlson D.L., McNulty T.L., Bellair P.E., Watts S. Neighborhoods and racial/ethnic disparities in adolescent sexual risk behavior. J. Youth Adolesc. 2014;43(9):1536–1549. doi: 10.1007/s10964-013-0052-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin J., Slade P., Sheeran P., Wright A., Dibble T. ‘If-then’ planning in one-to-one behaviour change counselling is effective in promoting contraceptive adherence in teenagers. BMJ Sex Reprod Health. 2011;37(2):85–88. doi: 10.1136/jfprhc.2010.0016. [DOI] [PubMed] [Google Scholar]
- Cohen R., Sheeder J., Arango N., Teal S.B., Tocce K. Twelve-month contraceptive continuation and repeat pregnancy among young mothers choosing postdelivery contraceptive implants or postplacental intrauterine devices. Contraception. 2016;93(2):178–183. doi: 10.1016/j.contraception.2015.10.001. [DOI] [PubMed] [Google Scholar]
- Furstenberg F.F., Shea J., Allison P., Herceg-Baron R., Webb D. Contraceptive continuation among adolescents attending family planning clinics. Fam. Plann. Perspect. 1983;15(5):211. doi: 10.2307/2135275. [DOI] [PubMed] [Google Scholar]
- Willis K., Small R., Brown S. Using documents to investigate links between implementation and sustainability in a complex community intervention: the PRISM study. Soc. Sci. Med. 2012;75(7):1222–1229. doi: 10.1016/j.socscimed.2012.05.025. [DOI] [PubMed] [Google Scholar]
- Goesling B., Colman S., Trenholm C., Terzian M., Moore K. Programs to reduce teen pregnancy, sexually transmitted infections, and associated sexual risk behaviors: a systematic review. J. Adolesc. Health. 2014;54(5):499–507. doi: 10.1016/j.jadohealth.2013.12.004. [DOI] [PubMed] [Google Scholar]
- Garney W., Wilson K., Nelon J., Muraleetharan D., McLeroy K., Baletka D.-M. Ecological approaches to teen pregnancy prevention: an examination of evidence-based interventions. Health Promot Pract. 2019;20(4):494–501. doi: 10.1177/1524839918815463. [DOI] [PubMed] [Google Scholar]
- McLeroy K.R., Bibeau D., Steckler A., Glanz K. An ecological perspective on health promotion programs. Health Educ. Q. 1988;15(4):351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- Amutah, C., Petsis, D, Fields, N.F., Wood, S., Timko, A., Akers, A.Y., Effect of Previous Adverse Reproductive Health Outcomes on Young Women’s Engagement in a Health Coaching Intervention to Improve Contraceptive Continuation. J. Pediatr. Adolesc. Gynecol. Published online 2021. [DOI] [PMC free article] [PubMed]
- Fields, N.F., Wood, S., Amutah, C., Timko, C.A., Petsis, D., Akers, A.Y., Identifying Opportunities to Discuss Pre-Exposure Prophylaxis During Contraceptive Coaching Discussions With Urban Adolescent Women. J. Adolesc. Health. Published online 2021. [DOI] [PMC free article] [PubMed]
- McGill, E., Er, V., Penney, T., et al., Evaluation of public health interventions from a complex systems perspective: a research methods review. Soc. Sci. Med. Published online 2021:113697. [DOI] [PubMed]
- Ramsey S., Willke R., Briggs A., Brown R., Buxton M., Chawla A., Cook J., Glick H., Liljas B., Petitti D., Reed S. Good research practices for cost-effectiveness analysis alongside clinical trials: the ISPOR RCT-CEA Task Force report. Value Health. 2005;8(5):521–533. doi: 10.1111/j.1524-4733.2005.00045.x. [DOI] [PubMed] [Google Scholar]
- Sutton J.A., Walsh-Buhi E.R. Factors influencing college women’s contraceptive behavior: An application of the integrative model of behavioral prediction. J. Am. Coll. Health. 2017;65(5):339–347. doi: 10.1080/07448481.2017.1312414. [DOI] [PubMed] [Google Scholar]
- Lopez, L.M., Tolley, E.E., Grimes, D.A., Chen, M., Stockton, L.L., Theory-based interventions for contraception. In: The Cochrane Collaboration, ed. Cochrane Database of Systematic Reviews. John Wiley & Sons, Ltd; 2013:CD007249.pub4. [DOI] [PubMed]
- Lopez, L.M., Grey, T.W., Tolley, E.E., Chen, M., Brief educational strategies for improving contraception use in young people. Cochrane Fertility Regulation Group, ed. Cochrane Database Syst. Rev. Published online March 30, 2016. [DOI] [PMC free article] [PubMed]
- Halpern, V., Lopez, L., Grimes, D., Stockton, L., Gallo, M., Strategies to improve adherence and acceptability of hormonal methods of contraception. Cochrane Database Syst. Rev. 2013Oct26;10. [DOI] [PubMed]
- Mak Y.W., Loke A.Y. The acceptance and commitment therapy for smoking cessation in the primary health care setting: a study protocol. BMC Public Health. 2015;15(1):1–7. doi: 10.1186/s12889-015-1485-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DuFrene T., Wilson K. New Harbinger Publications; 2012. The Wisdom to Know the Difference: An Acceptance and Commitment Therapy Workbook for Overcoming Substance Abuse. [Google Scholar]
- Kim C.-S., Lunde B., MacIsaac L., Arden M., Garney W.R., Wilson K.L., Li Y. Provision of contraceptive implants in school-based health centers: a cost-effectiveness analysis. Contraception. 2021;103(2):107–112. doi: 10.1016/j.contraception.2020.11.009. [DOI] [PubMed] [Google Scholar]
- Bellows B.K., Tak C.R., Sanders J.N., Turok D.K., Schwarz E.B. Cost-effectiveness of emergency contraception options over 1 year. Am. J. Obstet. Gynecol. 2018;218(5):508.e1–508.e9. doi: 10.1016/j.ajog.2018.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TreeAge Pro. TreeAge Software, Inc., MA, USA. Accessed August 5, 2015. https://www.treeage.com/.
- Obijuru L., Bumpus S., Auinger P., Baldwin C.D. Etonogestrel implants in adolescents: experience, satisfaction, and continuation. J. Adolesc. Health. 2016;58(3):284–289. doi: 10.1016/j.jadohealth.2015.10.254. [DOI] [PubMed] [Google Scholar]
- Trussell J., Wynn L.L. Reducing unintended pregnancy in the United States. Contraception. 2008;77(1):1–5. doi: 10.1016/j.contraception.2007.09.001. [DOI] [PubMed] [Google Scholar]
- Rosenstock J.R., Peipert J.F., Madden T., Zhao Q., Secura G.M. Continuation of reversible contraception in teenagers and young women. Obstet. Gynecol. 2012;120(6):1298–1305. doi: 10.1097/aog.0b013e31827499bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Truven Health Analytics. Red Book. Accessed August 20, 2020. http://www.micromedexsolutions.com/micromedex2/librarian.
- Kost K., Maddow-Zimet I., Pregnancies A.A. Race and Ethnicity.; 2017. Births and Abortions among Adolescents and Young Women in the United States, 2013: National and State Trends by Age. [Google Scholar]
- Green, L.W., Sim, L., Breiner, H., Effort C on EP of OP. Systems and Evaluation: Placing a Systems Approach in Context. In: Evaluating Obesity Prevention Efforts: A Plan for Measuring Progress. National Academies Press (US); 2013. [PubMed]
- Hoopes, A., Timko, C.A., Akers, A.Y., What’s Known and What’s Next: Contraceptive Counseling and Support for Adolescents and Young Adult Women. J. Pediatr. Adolesc. Gynecol. Published online 2020. [DOI] [PubMed]
- Sonfield, A., Kost, K., Public Costs from Unintended Pregnancies and the Role of Public Insurance Programs in Paying for Pregnancy-Related Care. Guttmacher Institute; 2015. https://www.guttmacher.org/sites/default/files/report_pdf/public-costs-of-up-2010.pdf.