Abstract
Background
Cerebrospinal fluid (CSF) tau and beta-amyloid levels in chronic traumatic encephalopathy (CTE), a disease which can be clinically indistinguishable from Alzheimer’s disease (AD), are largely unknown. We examined postmortem CSF analytes among participants with autopsy confirmed CTE and AD.
Methods
In this cross-sectional study 192 participants from the Boston University AD Research Center, VA-BU-CLF Center, and Framingham Heart Study (FHS) had post-mortem CSF collected at autopsy. Participants were divided into pathological groups based on AD and CTE criteria, with 61 CTE participants (18 low, 43 high stage), 79 AD participants (23 low, 56 intermediate to high), 11 participants with CTE combined with AD, and 41 participants lacking both CTE and AD neuropathology. The Meso Scale Discovery immunoassay system was utilized to measure amyloid-beta (Aβ1-40, Aβ1-42), total tau (t-tau), and phosphorylated tau (p-tau181 and p-tau231). CSF analytes were then compared across the pathological groups: no CTE/no AD (control), Low CTE, Low AD, High CTE, Intermediate/High AD, and AD+CTE.
Results
Among the Low disease state groups, the Low CTE group had significantly higher levels of p-tau231 versus the control group and compared to the Low AD group. The Low CTE group was also found to have significantly lower levels of Aβ1-42 compared to the control group. The high CTE group had higher levels of p-tau231 and lower levels of Aβ1-42 compared to Intermediate/High AD group.
Conclusions
Importantly, p-tau231 and Aβ1-42 were predictors of diagnosis of CTE vs. control and CTE vs. AD. Increased CSF p-tau231 is a promising potentially sensitive biomarker of CTE, and CSF Aβ1-42 needs further investigation in CTE.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13195-022-00976-y.
Keywords: Cerebrospinal fluid, Biomarkers, Chronic traumatic encephalopathy, Alzheimer’s disease, Amyloid beta, Tau
Background
Chronic traumatic encephalopathy (CTE) and Alzheimer disease (AD) are neurodegenerative conditions causing memory loss that can only be definitively diagnosed by pathologic examination. CTE is neuropathologically distinct from AD and characterized by hyperphosphorylated tau (p-tau) deposition in neurons, astrocytes, and cell processes around the small blood vessels and at the depths of cortical sulci that often involves the superficial cortical layers II and III [1–3]. AD neuropathology consists of amyloid-β plaques and tau neurofibrillary tangles in a distinct pattern beginning in the brainstem and entorhinal cortex in the early stages and progressing to the medial temporal lobe and finally the neocortex [4]. Analysis of differential profiles of tau-epitope phosphorylation profiles between CTE and AD is not yet fully understood though elevated levels of p-tau181 and p-tau231 have been reported in both AD and CTE [5, 6]. Total tau (t-tau), phosphorylated tau (p-tau), and beta-amyloid (Aβ) measurements in cerebrospinal fluid (CSF) have proven to be reliable biomarkers of AD and reflect changes in brain pathology that precede cognitive decline ante-mortem [7–10]. Biomarkers with the ability to detect and distinguish CTE from AD would be of great value if they show a high degree of correlation with CTE neuropathology.
Given the relatively superficial location of p-tau in the cortex of patients with CTE compared to AD and the lack of notable involvement of amyloid β in CTE, we hypothesized that CTE participants may have increased t-tau, p-tau181, and p-tau231 compared to cases without either CTE or AD (control), as well as relatively higher p-tau181, p-tau231, and Aβ42 concentrations compared to AD cases. Prior studies of Aβ deposition in CTE [11] led us to hypothesize that CSF Aβ1-40 would be decreased in cases with co-occurring CTE and AD compared to non-AD/non-CTE cases, representing a potential interaction between AD and CTE. To test these hypotheses, we measured CSF levels of Aβ1-40, Aβ42, t-tau, p-tau181, and p-tau231 among autopsy-confirmed participants including 61 with CTE, 79 with AD, 11 with concurrent CTE and AD, and 41 control participants lacking both CTE and AD pathology. Low and high stage CTE involve different brain regions and are associated with different clinical symptoms such that high stage disease shows significant medial temporal lobe pathology and is associated with increased frequency of cognitive impairment and dementia [12]. In contrast, intermediate to high degrees of AD pathology are characterized by greater pathological involvement of the neocortex and are also associated with cognitive impairment and dementia [13]. Therefore, because the underlying neuropathology and clinical syndrome is markedly different in low and high stage disease [12], we compared CTE to AD CSF analytes separately in each disease stage.
Methods
Participants
One hundred ninety-two participants with post-mortem CSF available were enrolled from three study groups. 100 donated their brains to the Veteran’s Affairs-Boston University-Concussion Legacy Foundation Brain Bank (VA-BU-CLF) as part of the Understanding Neurologic Injury and Traumatic Encephalopathy (UNITE) study, 38 were donated to the Framingham Heart Study (FHS), and 54 were donated to Boston University’s Alzheimer’s Disease Research Center (ADRC) as part of the Health Outreach Program for the Elderly study. The UNITE group consisted of participants with a history of exposure to contact sports such as football, ice hockey, boxing, soccer, rugby, and martial arts at either the professional or amateur level [14]. For most brain donations, the next of kin contacted the brain bank to donate tissue at or near the time of death. The participants from Boston University’s Alzheimer’s Disease Research Center (BU ADRC) with and without cognitive impairment underwent annual cognitive evaluations using the National Alzheimer’s Disease Coordinating Center (NACC) Uniform Data Set (UDS) protocol [1]. The third cohort consisted of participants from the Framingham Heart Study (FHS), a longitudinal, community-based study. Consents for brain donation and research participation were provided by donor next of kin.
Head injury exposure assessment
For UNITE study participants, retrospective clinical evaluations were performed using semi-structured post-mortem interviews, through online surveys, and review of medical records as described previously [14]. Information was obtained regarding repetitive head impact (RHI) exposure, traumatic brain injury (TBI) exposure, military history, athletic history, and clinical symptoms prior to death. In addition, medical records were examined to provide a determination of clinical symptoms and course. For the FHS participants, an athletic history assessment identical to UNITE was performed with the donor’s next of kin [15]. Athletic history was not available for BU ADRC participants. All interviews were conducted independently and blinded to the results of neuropathological examination.
Pathological criteria
All brains were neuropathologically evaluated for changes consistent with CTE, AD, and other neurodegenerative disorders using previously described selection criteria and protocols. Specifically, participants were separated into pathologic groups: CTE, AD, both (CTE+AD), or neither no CTE/no AD (control). Pathologic diagnosis of CTE was based on consensus criteria [1] and CTE staging I–IV was determined using previously published staging criteria [12, 16]. Participants were stratified using NIA-Reagan criteria to high, intermediate, or low probability of dementia caused by AD, based on Braak Score and CERAD score.
There is growing recognition that with increasing age co-occurring neurodegenerative pathologies become more common [17, 18]; therefore, comorbid neurodegenerative pathologies were not excluded from any of the groups, including the control group. Other neurodegenerative diseases were diagnosed using well-established criteria for Lewy body disease (LBD) [19] and frontotemporal lobar degeneration (FTLD) [20, 21] (Table 1). Participants with Amyotrophic Lateral Sclerosis/motor neuron disease (ALS/MND) pathology were also not excluded and included two participants in the no CTE/no AD (control) group and one participant in the high CTE group. The inclusion of a wider group of participants with concurrent neurodegenerative pathologies increases the generalizability of the current findings as patients presenting for clinical evaluation of cognitive complaints often have multiplane neurodegenerative diagnoses and underlying pathologies.
Table 1.
Demographic and exposure characteristics of participant groups
| No CTE/No AD | Low CTE | High CTE | Low AD | Int/High AD | CTE+AD | p | |
|---|---|---|---|---|---|---|---|
| Sample size (n) | 41 | 18 | 43 | 23 | 56 | 11 | |
| Age at death (S.E.M.) | 74.1 (3.0)d | 64.6 (4.6)f,d,e | 74.8 (1.3)d | 86.7 (1.1)a,b,c | 81.1 (1.3)b | 79.6 (2.8)b | <.001 |
| Age range (max-min) | 101–17 | 89–25 | 90–53 | 95–72 | 98–54 | 70–100 | |
| Cohort | |||||||
| FHS | 13 | 1 | 0 | 10 | 13 | 1 | |
| UNITE | 17 | 17 | 43 | 1 | 12 | 10 | |
| HOPE | 11 | 0 | 0 | 12 | 31 | 0 | |
| Sex m/f (%male) | 33/8 (80.5%)c,e | 18/0 (100%)e | 43/0 (100%)a,d,e | 14/9 (60.9%)c | 27/29 (48.2%) a,b,c | 10/1 (90.9%) | <.001 |
| CTE stage | |||||||
| Stage I | 0 | 6 (33.3%) | 0 | 0 | 0 | 1 (9.1%) | |
| Stage II | 0 | 12 (66.7%) | 0 | 0 | 0 | 1 (9.1%) | |
| Stage III | 0 | 0 | 18 (41.9%) | 0 | 0 | 0 | |
| Stage IV | 0 | 0 | 25 (58.1%) | 0 | 0 | 9 (81.8%) | |
| Braak Score | |||||||
| 0 | 15 (36.6%) | 7 (38.9%) | 1 (2.3%) | 0 | 0 | 0 | |
| I-II | 12 (29.3%) | 5 (27.8%) | 4 (9.3%) | 6 (26.1%) | 0 | 0 | |
| III-IV | 14 (34.1%) | 5 (27.8%) | 31 (72.1%) | 17 (73.9%) | 7 (12.5%) | 1 (9.1%) | |
| V-VI | 0 | 1 (5.6%) | 7 (16.3%) | 0 | 49 (87.5%) | 10 (90.9%) | |
| CERAD Score | |||||||
| 0 | 41 (100%) | 14 (77.8%) | 21 (48.8%) | 0 | 0 | 0 | |
| 1 | 0 | 4 (22.2%) | 22 (51.2%) | 22 (95.7%) | 8 (14.3%) | 1 (9.1%) | |
| 2 | 0 | 0 | 0 | 1 (4.3%) | 26 (46.4%) | 6 (54.5%) | |
| 3 | 0 | 0 | 0 | 0 | 22 (39.3%) | 4 (36.4%) | |
| FTLD pathology | 10 (27.7%)d,e | 5 (27.8%)d,e | 6 (14.6%) | 0 (0%)a,b | 3 (5.4%)a,b | 2 (18.2%) | <.05 |
| Tau | 9 (25%) | 5 (27.8%) | 6 (14.6%) | 0 | 2 (4.3%) | 2 (18.2%) | |
| TDP 43 | 1 (2.7%) | 5 (27.8%) | 4 (9.8%) | 0 | 2 (4.3%) | 1 (9%) | |
| n total | 36 | 18 | 41 | 15 | 46 | 11 | |
| LBD pathology | 0.31 | ||||||
| Brainstem | 2 (4.4%) | 1 (5.6%) | 6 (14%) | 2 (13.3%) | 2 (4.34%) | 0 (0%) | |
| Limbic/neocortical | 4 (9.8%) | 2 (11.1%) | 10 (23.3%) | 1 (6.6%) | 8 (17.4%) | 4 (36.4%) | |
| n | 36 | 18 | 43 | 15 | 46 | 11 | |
| Contact sports play | Yes 12 (29.2%) | Yes 17 (94.4%) | Yes 43 (100%) | Yes 0 | Yes 9 (16%) | Yes 10 (90%) | .013 |
| No 2 (4.8%) | No 0 | No 0 | No 1 (4%) | No 1 (1.7%) | No NA | ||
| Missing 27 (70.7%) | Missing 1 (5.6%) | Missing 0 | Missing 22 (96%) | Missing 46 (82%) | Missing 1 (9.1%) | ||
| CSF hemoglobin (S.E.M.) | 481.0 (106.6) | 648.3 (261.2) | 465.1 (106.5) | 555.6 (183.6) | 386.5 (93.1) | 370.5 (192.7) | 0.85 |
| n | 36 | 11 | 33 | 23 | 49 | 11 | |
| Postmortem interval (hours) (S.E.M)95% CI | 23.2 (3.15)b 16.82–29.56 | 46.6 (6.34)a,d,e 33.2–59.99 | 33.88(3.02)e 27.77–39.98 | 21.40 (3.85)b 13.43–29.37 | 20.70 (2.31)b,c 16.1–25.32 | 24.99 (4.05) 15.98–34.0 | <.001 |
| N | 40 | 18 | 42 | 23 | 56 | 11 | |
| PMI range (Max-Min) | 80.5.00–1.75 | 101.00–5.5 | 96.00–2.00 | 96.00–5.83 | 99.15–1.75 | 48.00–3.00 | |
| RIN (S.E.M.) n | 6.2 (0.2) 35 | 5.76 (0.5) 16 | 5.6 (0.2) 31 | 5.7 (0.5) 12 | 5.8 (0.2) 39 | 4.7 (0.4) 10 | 0.15 |
| pH (S.E.M.) n | 6.14 (0.08) 26 | 6.14 (0.10) 14 | 6.17 (0.1) 24 | 6.07 (0.13) 11 | 6.08 (0.06) 36 | 5.97 (0.8) 6 | 0.83 |
Data are presented mean with standard error of the (S.E.M.), years for age at death, and contact sports exposure and as #yes/#no (%) unless otherwise indicated
CERAD plaque density was rated as none (0), sparse (1), moderate (2), or frequent (3) for neuritic plaques
Int/High intermediate/high, AD Alzheimer disease, CERAD Consortium to Establish a Registry for Alzheimer’s disease, CTE chronic traumatic encephalopathy, FTLD frontotemporal lobar degeneration, LBD Lewy body disease, RIN RNA integrity number
aDifferent from no CTE/no AD (p <.05, Bonferroni corrected)
bDifferent from low CTE (p <.05, Bonferroni corrected)
cDifferent from high CTE (p <.05, Bonferroni corrected)
dDifferent from low AD (p <.05, Bonferroni corrected)
eDifferent from intermediate/high AD (p <.05, Bonferroni corrected)
fDifferent from CTE+AD (p <.05, Bonferroni corrected)
#ANOVA with Bonferroni correction
*χ2 test for proportions between all pathology groups
Participants were divided into pathological groups based on NIA-Reagan Criteria and CTE stage as follows. Participants with no evidence of CTE and no elements of NIA-Reagan were labeled as “No CTE/no AD” and were used and referenced as the control group throughout. Participants with CTE Stage of I–II were determined to have early stage disease and termed “Low CTE,” while those with CTE Stage of III–IV were determined to have late stage disease and were termed “High CTE.” Those with no evidence of CTE and NIA-Reagan of high or intermediate probability were termed “Intermediate/High AD,” while those with no evidence of CTE and NIA-Reagan of low probability were classified as “Low AD.” Subjects with CTE and intermediate or high probability of AD were combined to “CTE+AD.”
CSF sampling and analysis
CSF was obtained post-mortem from the foramen magnum by gently lifting the frontal lobes to access with a large bore needle. CSF was then mixed by gently inverting the tube 5 times. The tubes were centrifuged at 1500 g for 15 min at 4°C. The CSF supernatant was removed with a transfer pipet and aliquoted into 1.5mL microcentrifuge polypropylene tubes. CSF was stored at −80 C prior to use. CSF was then diluted 1:2 with 1% Blocker A (MSD, Rockville, MD, USA, #R93BA) in wash buffer. Immunoassay was performed for Aβ1-42 and Aβ1-40, using a multiplex plate from MSD (#K15200E), as well as for levels of p-tau231 and total tau (MSD #K15121D) according to manufacturer’s protocol. To capture tau phosphorylated at Thr residue 181, antibody AT270 was used and the detecting antibody was the biotinylated HT7 that recognizes residue 159–163 of tau (Thermo Scientific, Rockford, IL). For hemoglobin quantification, CSF was diluted 1:3000 and applied to the RayBio Human Hemoglobin ELISA kit (# ELH-Hgb). All standards and samples were run in duplicate.
Tissue sampling and analysis
The buffer conditions, protease inhibitors, and centrifugation protocols have been reported previously [11]. A 4-mm-tissue punch was used to isolate and remove gray matter from the gyral crests and sulcal depths of the middle frontal gyrus and neighboring sulci and superior temporal gyrus and sulcus. The brain tissue was homogenized in five-fold volume of 5 M Guanidine Hydrocholride/50 mM Tris-HCL, pH 8.0, with protease inhibitors (Thermo Scientific, 78439) and phosphatase inhibitors (Sigma, P5726 and P0044). The tissue was homogenized using a mechanical homogenizer for 25 strokes followed by ultrasonic disruption on ice. The homogenates were shaken at room temperature overnight. The lysate was diluted 1:80 with 1% Blocker A (MSD, #R93BA) in wash buffer, and immunoassay was performed for Aβ1-42 using a multiplex plate from MSD.
Statistical analysis
Statistical analysis was performed using SPSS 26.0 (IBM Corp, Armonk, NY) and Prism v8 (Graph-Pad Software, La Jolla, CA). A one-way analysis of variance (ANOVA) was used to compare age among groups. Levels of Aβ1-40, Aβ1-42, p-tau181, p-tau231, and total tau that were outside 3X the interquartile range were eliminated as outliers and included n=1 from no CTE/no AD (control) group, n=1 from low CTE group, n=1 high CTE group, n=1 from low AD group, and n=1 from intermediate/high AD group for ptau 181 analysis, n=3 from the control group, n=1 from low AD group, n= 1 for the high CTE group, n=6 from intermediate/high AD group, and n=1 from CTE+AD group for ptau 231 analysis, n=1 from no CTE/no AD (control) group, n=2 from high CTE group for total tau analysis, n=5 from control group, n=3 from low CTE group, n=4 from high CTE group, n=1 from intermediate/high AD group, n= 1 for the CTE+AD group for Aβ1-42 analysis, n=2 from the control group, n=1 from low CTE group, n=3 from high CTE group, n=1 from low AD group, and n=2 from intermediate/high AD group for Aβ1-40 analysis. A two-sample chi-square test weighted by sample size was used to compare the frequency of men in each pathologic group, as well as the frequency of FTLD and LBD pathologies between pathologic groups. CSF analyte levels were used in a Kruskal-Wallis test performed to compare levels of analytes between pathologic groups. CSF measures were also rank-normalized (supplementary Figures e-1 and e-2) and used in one-way ANCOVAs in order to correct for age as a covariate to compare relative amounts of biomarkers between groups (supplementary results).
Statistical significance was set to p<0.05 following adjustments for multiple comparisons for all planned analyses. Binary logistic regression analyses were used to determine association between p-tau231 and Aβ1-42 and CTE or AD pathologic diagnosis controlling for age, sex, PMI, and other variables where appropriate. Linear regressions were performed to determine the relationship between CSF and brain Aβ1-42 levels in AD and CTE. Receiver operating characteristic (ROC) curve analysis was used to determine sensitivity and specificity of CSF analytes between diagnoses.
Results
Study population
Participants were grouped based on the presence or absence of CTE and/or AD pathology. Group demographic differences for age at death, post-mortem interval (PMI), sex, RNA integrity number (RIN), pH, and presence/absence of FTLD and LBD pathologies are listed in Table 1. Pathologic groups differed in age at death (p <0.001) and PMI (p <0.001) (Table 1). The low CTE group (M= 64.6± 4.6) was younger than the low AD (M= 86.7±1.1, p <.05), intermediate/high AD (M= 81.1±1.3, p < 0.05), and CTE+AD groups (M= 79.6 ± 2.8, p <0.05). The low AD group was older than the high CTE and control groups. The low CTE group had significantly longer PMIs (M= 46.6±6.4) than the control (M= 23.2±3.15 p<0.001), low AD (M= 21.4±3.85, p <0.001), and intermediate/high AD group (M= 20.7±2.3, p < 0.05). The high CTE group (M= 33.88±3.02) had significantly longer PMIs than the intermediate/high AD group (M= 20.7±2.3, p < 0.05). Despite these differences in PMI, there was no difference in RIN, pH, or CSF hemoglobin between groups. A majority of men were present in each pathological group for all groups except for the intermediate/high AD group which had a majority of women. Years of contact sports differed between groups (p =0.013) for the subset of participants that had this history taken (n=95); post hoc pairwise comparisons revealed the control group (M= 9.46±2.97) had decreased years of contact sports compared to mild CTE group (M= 20.85±3.43, p=0.036 Bonferroni-corrected).
All groups
Comparing all pathological groups using the Kruskal-Wallis test, there were significant differences in p-tau231 H(5)= 16.28, p=0.006 and Aβ1-42 H(5) = 19.32, p=0.002. The low CTE group had significantly higher amount of p-tau231 (mean rank= 121.1) compared to the Int/high AD group (mean rank= 74.2, p=0.014). Both the high CTE group (mean rank= 58.74) and low CTE (mean rank =58.14) groups were found to have significantly lower levels of Aβ1-42 compared to no CTE/no AD (control) (mean rank= 102.1, p<0.002 and p < 0.05, respectively). There was no significant difference in relative amounts of p-tau181, total tau, and Aβ1-40 between all groups.
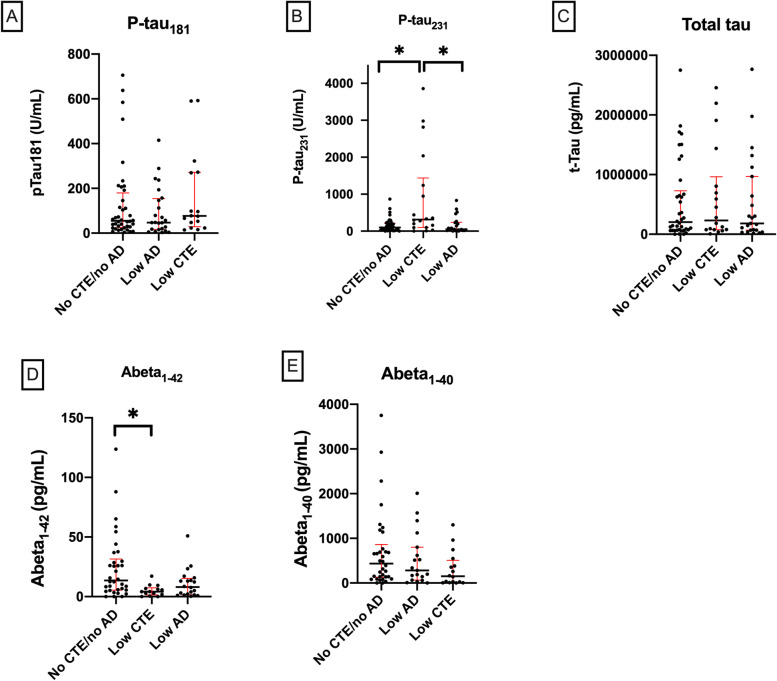
Early stage disease
Comparing no CTE/no AD (control), low CTE, and low AD pathological groups using the Kruskal-Wallis test, a difference in p-tau231 H(2)= 8.93, p=0.015 and Aβ1-42 H(2)= 10.27, p=0.006 was found. The low CTE group (mean rank= 52.61) had significantly higher levels of p-tau231 versus the no CTE/no AD (control) group (mean rank= 35.93, p=0.03) and compared to the low AD group (mean rank= 33.02, p=0.017) (Fig. 1). The low CTE group (mean rank 22.18) was also found to have significantly lower levels of Aβ1-42 compared to the no CTE/no AD (control) (mean rank= 41.51, p=0.006) (Fig. 1). The low AD group had lower levels of Aβ1-42 compared to the no CTE/no AD (control) group, but this difference was not significant (p=0.19). There was no significant difference in relative amount of p-tau181, total tau, or Aβ1-40 between the no CTE/no AD (control), low CTE, and low AD groups.
Fig. 1.
A p-tau181, B p-tau231, C total tau, D Aβ1-42, and E Aβ1-40 for no CTE/no AD (control), low CTE, and low AD groups. Scatter plots show individual values, median, and interquartile range (25–75%) as bars, *p< 0.05 corrected for multiple comparisons; Kruskal-Wallis test
Similar results for between group difference for early disease stages were obtained by rank-normalizing CSF measures (supplementary Figure e-1), followed by one-way ANCOVAs in order to correct for age as a covariate (supplementary results).
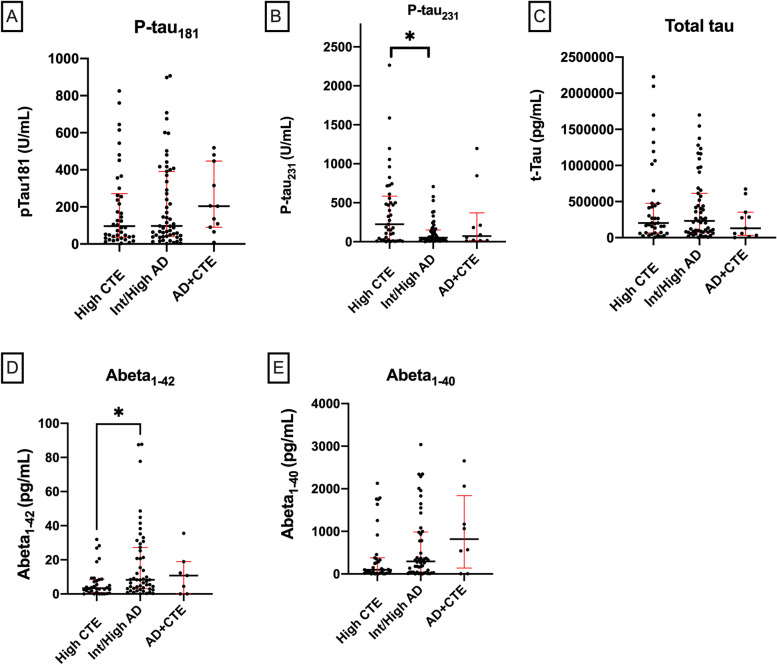
Late stage disease
Comparing high CTE, AD, and CTE+AD pathological groups using the Kruskal-Wallis test, a difference in p-tau231 H(2)= 7.096, p=0.029 and Aβ1-42 H(2) = 7.98, p = 0.019 was found overall. The High CTE group had significantly higher levels of p-tau231 (mean rank = 59.61) compared to intermediate/high AD (mean rank=43.3, p=0.024) (Fig. 2). The High CTE group also had significantly lower levels of Aβ1-42 (mean rank= 36.34) compared to the intermediate/high AD group (mean rank =52.99, p=0.015) (Fig. 2). There was no significant difference in relative amount of p-tau181, total tau, or Aβ1-40 between High CTE, AD, and CTE+AD groups. Although there was no significant difference between groups for ptau181, all late stage group levels were all numerically greater than the control, indicating that ptau181 was elevated in late stage disease above the control group’s levels as expected.
Fig. 2.
A p-tau181, B p-tau231, C total tau, D Aβ1-42, and E Aβ1-40 for high CTE, intermediate/high AD, and CTE+AD groups. Scatter plots show individual values, median, and interquartile range (25–75%) as bars, *p < 0.05 corrected for multiple comparisons; Kruskal-Wallis test
Results for between group difference for late disease stages were also obtained by rank-normalizing CSF measures (supplementary Figure e-2), followed by one-way ANCOVAs in order to correct for age as a covariate (supplementary results).
Regression analyses
We performed a binary logistic regression analysis to determine the contributions of p-tau231 and Aβ1-42 in predicting pathological diagnosis of CTE (low and high CTE combined, excluding CTE +AD cases) vs. control. Variables included in the model were p-tau231, Aβ1-42, age at death, and sex (n= 77). Both p-tau231 (OR 1.53, 95% CI 1.08–2.16) and Aβ1-42 (OR 0.35, 95% CI 0.17–0.74) were significant predictors of CTE status while controlling for age and sex, neither of which were significant predictors (Table 2). Secondary analyses including PMI, pH, and presence of LBD pathology as additional variables did not substantially change the results and were not significant predictors of CTE diagnosis. Although RIN and FTLD were associated with CTE, their presence in the model did not change the associations between ptau231, Aβ1-42, and CTE status.
Table 2.
CSF predictors of CTE pathology versus no CTE/no AD (control)
| OR | 95% Confidence Interval | p value | |
|---|---|---|---|
| p-tau231 (U/10μL) | 1.53 | 1.08–2.16 | 0.016 |
| Aβ1-42 (pg/100μL) | 0.35 | 0.17–0.74 | 0.006 |
Binary logistic regression comparing CTE all stages with no CTE/no AD (control) group while adjusting for age and sex (n=77)
We also performed a binary logistic regression to determine the contributions of p-tau231 and Aβ1-42 in predicting pathological diagnosis of CTE (low and high CTE combined) vs. AD (low AD and intermediate/high AD combined) (Table 3). Variables included in the model were p-tau231, Aβ1-42, age at death, and sex (n= 111). Both p-tau231 (OR 1.34, 95% CI 1.02–1.76, p = 0.036) and Aβ1-42 (OR 0.51, 95% CI 0.28–0.91) were found to distinguish between CTE and AD diagnoses, controlling for age at death (OR 0.91, 95% CI 0.84–0.97) and sex which was not a significant predictor. A secondary analysis adjusting for PMI (n= 102), demonstrated that this trend continued but with a decrease in significance most likely due to decreased power, with p-tau231 (OR 1.23, 95% CI 0.90–1.72), Aβ1-42 (OR 0.60, 95% CI 0.31–1.15), adjusting for age (OR 0.88, 95% CI 0.81–0.97), PMI (OR 1.06, 95% CI 1.01–1.12), and sex, which was not a significant predictor. Additional secondary analyses included the addition of RIN and pH separately as well as presence/absence of FTLD pathology and LBD pathology, none of which were significant predictors of CTE diagnosis.
Table 3.
CSF predictors of CTE versus AD pathology
| OR | 95% confidence interval | p value | |
|---|---|---|---|
| p-tau231 (U/10μL) | 1.34 | 1.02–1.76 | 0.036 |
| Aβ1-42 (pg/100μL) | 0.51 | 0.28–0.91 | 0.022 |
| Age of death | 0.91 | 0.84–0.97 | 0.006 |
Binary logistic regression comparing CTE all stages with AD all stages adjusting for age and sex (n=111)
Given the surprisingly low levels of Aβ1-42 in CTE, we performed a secondary analysis to test the hypothesis CSF beta-amyloid levels reflect brain tissue Aβ1-42 levels in AD, but not in CTE. Using a linear regression it was found that a model including age, sex, and CSF Aβ1-42 levels predicted a significant amount of the variance of brain Aβ1-42 levels among the AD and control groups combined (F(3, 100)=5.42, p=0.002, R2= 0.14, adjusted R2= 0.114) and both CSF Aβ1-42 (β = −0.21, p =0.032) and age (β = 0.21, p =0.036) predicted frontal cortex Aβ1-42 while sex (β = 0.13, p =0.19) did not. In a separate linear regression among the combined CTE and control groups, the overall regression model including CSF Aβ1-42 levels, age, and sex predicted a significant amount of the variance of brain Aβ1-42 levels (F(3, 77)= 4.52, p=0.006, R2= 0.15, adjusted R2= .117), though CSF Aβ1-42 levels (β = −0.17, p =0.11) and sex (β = −0.14, p =0.21) were not found to be a significant predictors of cortical Aβ1-42 levels while age was found to be a significant predictor (β = 0.38, p =0.001).
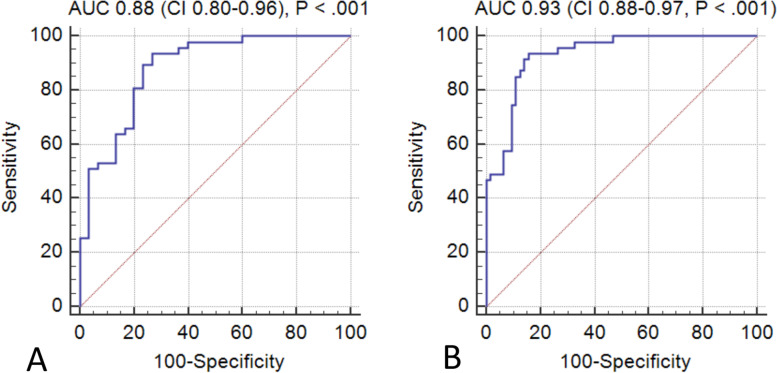
Receiver Operating Characteristic curve (ROC) analyses
To assess the diagnostic accuracy of CSF p-tau231 and Aβ1-42 levels, an ROC analysis was performed to determine if p-tau231, Aβ1-42, age at death, and sex were predictive of CTE vs. control diagnosis. Area under the curve (AUC) was 0.88 (SEM= 0.04, p <0.001) (Fig. 3A). A separate ROC analysis was performed for CTE vs. AD diagnosis to determine if p-tau231, Aβ1-42, age at death, and sex were predictive and demonstrated that AUC was 0.93 (SEM= 0.023, p <0.001) (Fig. 3B).
Fig. 3.
Diagnostic accuracy of A p-tau231, Aβ1-42, age at death, sex for CTE vs. no CTE/no AD (control) diagnosis (n= 77) and B p-tau231, Aβ1-42, age at death, and sex were predictive of CTE vs. AD (n= 111). AUC area under the receiver operating characteristic curve; CI confidence interval
Discussion
In summary, our results indicate that in post-mortem CSF, p-tau231 levels were significantly higher in both the low and high CTE groups compared to the no CTE/no AD (control) group and compared to the AD groups. Furthermore, surprisingly CSF Aβ1-42 was found to be decreased in both low stage CTE compared to the no CTE/no AD (control) group as well as in high stage CTE compared to Int/high AD. Overall, increased levels of p-tau231 and decreased levels of Aβ1-42 in combination were found to be significant predictors of CTE compared to controls and AD.
While three repeat and four repeat tau species are present in both AD and CTE [22, 23], unique folding patterns of tau have been reported to predominate in CTE as compared to AD [24]. Beyond a limited number of studies, little is known regarding the exact tau species present in CTE and how they can be distinguished at the epitope level from the tauopathy of AD, though we recently found that both ptau202 and p-tau231 are associated with increased years of RHI from American football [25]. Increased p-tau231 levels in CTE may be due to tau leakage from cells into the CSF, which may be present even relatively early on in the disease course when clinical symptoms are relatively mild. P-tau231 was significantly increased in low CTE, and there was a trend towards an increase for high stage CTE groups compared to AD groups, which could reflect increased neuron and axonal damage in CTE. Studies in AD have revealed that increased phosphorylated tau levels, including both p-tau181 and p-tau231, correlate with neocortical neurofibrillary burden in AD [26, 27], though a similar relationship in CTE between elevated CSF p-tau231 levels and increased p-tau accumulation in the neocortex has not been well-investigated. While t-tau may be a more general marker of neurodegeneration reflecting axonal injury, CSF p-tau181 and p-tau231 may be specific for the intraneuronal tau pathology seen in both CTE and AD. Our findings from the current study suggest that p-tau231 CSF levels may be more sensitive and specific than both t-tau and p-tau181 in distinguishing CTE from non-CTE and non-AD participants as well as in distinguishing CTE from AD.
The role of Aβ accumulation in CTE pathophysiology is not well understood. In the current study, the low CTE group exhibited lower Aβ1-42 levels in post-mortem CSF compared to those in the control group and surprisingly the High CTE group had decreased Aβ1-42 levels compared to the intermediate/high AD group. Decreased CSF Aβ1-42 in combination with elevations in tau species and relatively unchanged Aβ1-40 are well-established markers of AD and predict the conversion of mild cognitive impairment (MCI) to AD [28–30]. In vivo studies of former NFL players with objective memory deficits have not been found to have increased Aβ deposition compared to controls as measured by florbetapir PET, indicating that cognitive decline in former players at risk of possible CTE was not related to AD or Aβ deposition [31]. In contrast, post-mortem evidence has shown that Aβ accumulation can occur in CTE; however, it is not a consistent pathologic feature and is absent in about half of cases, tending to form diffuse rather than neuritic plaques when present [11]. However, there does appear to be an age-dependent acceleration of Aβ deposition in CTE compared to a normal autopsy population [11]. Furthermore, RHI associated with CTE likely damages blood vessels and is associated with the development of frontal leptomeningeal cerebral amyloid angiopathy (CAA) which is distinct from AD [32]. This preferential localization of Aβ associated with CAA in the leptomeningeal vessels suggests that the mechanism of decreased Aβ1-42 seen in CTE may be related to impaired CSF clearance of Aβ, rather than to amyloid sequestration in plaques. We found that there was a significant relationship between CSF and brain levels of Aβ1-42 in AD, but not between CSF and brain levels in CTE. This may indicate that sequestration of Aβ1-42 in plaques may drive CSF levels of Aβ1-42 in AD, but that CSF Aβ1-42 is determined by a different mechanism in CTE.
The relationship of the two pathologies underlying AD and CTE is not well understood and as a starting point this study has sought to investigate the levels of several CSF AD biomarkers in the CTE population with the general hypothesis that alterations in these analytes would allow improved discrimination of AD and CTE. Older individuals with CTE pathology are more likely to have concurrent amyloid-beta (Aβ) plaques consistent with AD [16] and may also develop Aβ accumulation at a younger age than individuals without head injuries [11]. In prior studies 13 % of neuropathologically confirmed CTE cases also had AD pathology [33]. In cases where CTE co-occurs with AD, it is unclear if individuals developed a mixed pathology neurodegenerative disorder or whether there is a synergistic relationship between the two pathophysiological processes. An additional possibility is that decreases in CSF Aβ may not correlate as closely with increased Aβ plaque deposition in CTE, a potential departure from the well-established inverse correlation between CSF Aβ levels and Aβ plaque burden in AD. Although we did not find overall group differences in p-tau181 and t-tau between any of the pathologic groups, the intermediate/severe AD did show the expected increases in p-tau181 and t-tau compared to the no AD/no CTE group.
When controlling for age and sex, both p-tau231 and Aβ1-42 were able to discriminate CTE from controls using binary logistic regressions. p-tau231 and Aβ1-42 were still significant when controlling for PMI, RIN, or pH individually. PMI, RIN, and pH all generally correlate with one another. p-tau231 and Aβ1-42 were also able to discriminate CTE from AD when controlling for age and sex, but lost significance when controlling for PMI, possibly related to decreased power.
Limitations
This study is limited in that age is a major risk factor for neurodegenerative conditions and the CTE groups were younger than the AD groups. As a result, age at death was included in the regression analysis but there is still the possibility that age could act as a potential confounder in the current study. Differences in years of play generally differ by diagnosis with CTE groups having increased years of play exposure; however, this variable was missing in a significant percentage of cases and as such contact sports play is a potential confounder that could not be accounted for in our models. Furthermore, the groups did not have individuals of each gender evenly distributed and the AD group had increased numbers of women compared to the CTE groups which did not have women. This is a concern as gender differences in neuropathology have previously been reported [34]. However, we have attempted to correct for this in part by running regression and sensitivity analyses among men only and have found similar results for both ptau231 and Aβ1-42 compared to analyses run with both men and women. In addition, this study was autopsy-based and thus potentially subject to selection bias as individuals whose brains are donated by family may not represent the population more broadly. However, grouping by known pathology allows for definitive associations not possible in a clinical sample where the pathology is unknown. The current study was also limited in that it is post-mortem, and CSF abeta and total tau levels are known to be altered from antemortem levels in post-mortem samples [35]. Both the low and high CTE groups had significantly longer PMIs than the no CTE/no AD (control), low AD, and intermediate/high AD groups which raises concern that a longer PMI could lead to increased tau levels in the CTE groups. We attempted to take this into account by controlling for PMI when possible. Furthermore, given its post-mortem nature, the current study serves not to set a definitive cut-off but to warrant ante-mortem comparison of these amyloid and tau levels in CSF among patients with suspected CTE and AD. Of note, t-tau, p-tau181, and Aβ42 have been previously evaluated during life in former professional American football players, at increased risk of CTE, and it was found that increased cumulative head impact exposure in former players predicted t-tau levels [36].
Several promising modalities have been investigated for their use as in vivo CTE biomarkers including PET imaging of p-tau [31], peripheral blood levels of total tau and exosomal tau [37, 38], and CSF biomarkers [39, 40]. CSF biomarkers are particularly promising as they closely reflect the dynamic relationship of solute clearance in the glymphatic space [41] and thus may provide a window to relatively early neuropathological changes. Future studies should investigate other tau isoforms that have recently shown promise in AD including p-tau217 [42] as well as plasma biomarkers of tau isoforms [7, 43, 44].
Conclusions
Overall, the current study revealed that levels of post-mortem CSF p-tau231 and Aβ1-42 were selectively altered in groups with CTE compared to those with AD, and compared to those without CTE and without AD. Both p-tau231 and Aβ1-42 were also predictive of CTE diagnosis compared to AD group and compared to non-CTE/non-AD groups, indicating that p-tau231 represents a potentially sensitive and specific biomarker of CTE, and that decreases in CSF Aβ1-42 should be further investigated in vivo among possible CTE patients.
Supplementary Information
Additional file 2: Figure e-1. Rank-normalized fold change of A. p-tau181, B. p-tau231, C. total tau, D. Aβ1-42 and E. Aβ1-40 for no CTE/no AD (control), Low CTE, and Low AD groups. Scatter plots show individual values, median and interquartile range (25-75%) as bars, *p < 0.05 corrected for multiple comparisons; ANCOVA adjusting for age.
Additional file 3: Figure e-2. Rank-normalized fold change of A. p-tau181, B. p-tau231, C. total tau, D. Aβ1-42 and E. Aβ1-40 for High CTE, Intermediate/High AD, and CTE+AD groups. Scatter plots show individual values, median and interquartile range (25-75%), *p < 0.05 corrected for multiple comparisons; ANCOVA adjusting for age.
Additional file 4: Table e-1. Estimated Marginal Means and SEM in parentheses for rank normalized CSF analyte measurements from No CTE/no AD (control) group; showing ANCOVA adjusted for age, p <0.05. Table e-2. Estimated Marginal Means and SEM in parentheses for rank normalized CSF analyte measurements from No CTE/no AD (control) group; showing ANCOVA adjusted for age, sex, and PMI, p <0.05.
Acknowledgements
We gratefully acknowledge the use of resources and facilities at the Edith Nourse Rogers Memorial Veterans Hospital (Bedford, MA) as well as all the individuals whose participation and contributions made this work possible.
Abbreviations
- CSF
Cerebrospinal fluid
- CTE
Chronic traumatic encephalopathy
- AD
Alzheimer’s disease
- Aβ
Amyloid-beta
- t-tau
Total tau
- p-tau
Phosphorylated tau
- VA-BU-CLF
Veteran’s Affairs-Boston University-Concussion Legacy Foundation Brain Bank
- UNITE
Understanding Neurologic Injury and Traumatic Encephalopathy
- BU ADRC
Boston University’s Alzheimer’s Disease Research Center
- NACC)
National Alzheimer’s Disease Coordinating Center
- UDS
Uniform Data Set
- FHS
Framingham Heart Study
- RHI
Repetitive head impact
- LBD
Lewy body disease
- FTLD
Frontotemporal lobar degeneration
- ALS/MND
Amyotrophic Lateral Sclerosis/motor neuron disease
- ANOVA
One-way analysis of variance
- PMI
Post-mortem interval
- RIN
RNA integrity number
- ROC
Receiver Operating Characteristic curve
- AUC
Area under the curve
- MCI
Mild cognitive impairment
- CAA
Cerebral amyloid angiopathy
Authors’ contributions
KWT played a major role in drafting manuscript writing, revisions, and data analysis and interpretation. AG helped with the initial manuscript drafting and data entry and analysis. VEA helped with the data generation and provided a critical manuscript review for content. WX helped with the brain and CSF ELISA data generation and analysis, and critical manuscript review for content. JDC provided assistance with data interpretation, critical manuscript review for content. RN provided assistance with brain and CSF data generation and analyses. GM helped with brain and CSF ELISA data generation and analysis. SD helped with brain and CSF ELISA data generation. YT provided assistance with statistical plan, data generation, and critical manuscript review for content. BH helped with data generation, analyses, and critical manuscript review for content. AEB provided assistance with data analysis and critical manuscript review for content. BD provided assistance with data analysis and critical manuscript review for content. NK provided assistance with data analysis and critical manuscript review for content. RCC provided assistance with data analysis and critical manuscript review for content. LEG provided assistance with data analysis and critical manuscript review for content. DIK provided assistance with data analysis and critical manuscript review for content. RAS provided assistance with data analysis and critical manuscript review for content. MLA provided assistance with data analysis and critical manuscript review for content. JM provided assistance with statistical plan, data analysis, and critical manuscript review for content. ACM provided assistance with data analysis and critical manuscript review for content. TDS led all aspects of study including concept and design, data analysis and interpretation, and critical manuscript writing and editing. The author(s) read and approved the final manuscript.
Funding
This work was supported by the United States (U.S.) Department of Veterans Affairs, Veterans Health Administration, Clinical Sciences Research and Development Merit Awards (I01-CX001038) (CX001698-01A2); Career Development Award-2 (# IK2 CX002065) Alzheimer’s Association (NIRG-305779, NIRG-362697); National Institute of Aging (RF1AG054156, R56AG057768, RF1AG057768, K23AG046377, U19AG068753, AG08122, AG054076); National Institute of Neurological Disorders and Stroke (U54NS115266, U01NS086659, K23NS102399); National Institute of Aging Boston University AD Center (P30-AG072978; supplement 0572063345-5; pilot award 50204517); National Heart, Lung and Blood Institute (75N92019D00031 and HHSN2682015000011); Department of Defense Peer Reviewed Alzheimer’s Research Program (PRARP #13267017); and the Concussion Legacy Foundation. This work was also supported by unrestricted gifts from the Andlinger Foundation and WWE.
Availability of data and materials
Anonymized data not published within the article will be shared upon reasonable request.
Declarations
Ethics approval and consent to participate
All study protocols were approved by the VA Bedford Healthcare System and Boston University Medical Center Institutional Review Boards. Written and informed consent was obtained from all patients and family members participating.
Consent for publication
Not applicable.
Competing interests
Andrew E. Budson has been a speaker for Eli Lilly, a consultant for General Electric, Eli Lilly, and Axovant. Lee E. Goldstein has received funding from the WWE and Ivivi Health Sciences. Robert A. Stern is a member of the Mackey-White Committee of the NFL Players Association. He is a paid consultant to BioGen (Cambridge, MA, USA) and Eli Lilly (Indianapolis, IN, USA). He receives royalties for published neuropsychological tests from Psychological Assessment Resources, Inc. (Lutz, FL, USA) and is a member of the Board of Directors of King-Devick Technologies (Chicago, IL, USA). Robert C. Cantu is a paid consultant to the NFL Head Neck and Spine Committee, NOCSAE, Concussion Legacy Foundation, receives royalties from book publications, and compensation from expert legal opinion. He is a member of the Mackey-White Committee of the NFL Players Association. Ann C. McKee is a member of the Mackey-White Committee of the NFL Players Association. The other authors have no competing interests or disclosures to report.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Katherine W. Turk and Alexandra Geada contributed equally to this work.
References
- 1.McKee AC, Cairns NJ, Dickson DW, Folkerth RD, Keene CD, Litvan I, et al. The first NINDS/NIBIB consensus meeting to define neuropathological criteria for the diagnosis of chronic traumatic encephalopathy. Acta Neuropathol. 2016;131(1):75–86. doi: 10.1007/s00401-015-1515-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hof PR, Bouras C, Buee L, Delacourte A, Perl DP, Morrison JH. Differential distribution of neurofibrillary tangles in the cerebral cortex of dementia pugilistica and Alzheimer’s disease cases. Acta Neuropathol. 1992;85(1):23–30. doi: 10.1007/BF00304630. [DOI] [PubMed] [Google Scholar]
- 3.Tokuda T, Ikeda S, Yanagisawa N, Ihara Y, Glenner GG. Re-examination of ex-boxers' brains using immunohistochemistry with antibodies to amyloid beta-protein and tau protein. Acta Neuropathol. 1991;82(4):280–285. doi: 10.1007/BF00308813. [DOI] [PubMed] [Google Scholar]
- 4.Braak H, Braak E. Staging of Alzheimer’s disease-related neurofibrillary changes. Neurobiol Aging. 1995;16(3):271–278. doi: 10.1016/0197-4580(95)00021-6. [DOI] [PubMed] [Google Scholar]
- 5.Katsumoto A, Takeuchi H, Tanaka F. Tau pathology in chronic traumatic encephalopathy and Alzheimer’s disease: similarities and differences. Front Neurol. 2019;10:980. doi: 10.3389/fneur.2019.00980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schmidt ML, Zhukareva V, Newell KL, Lee VM, Trojanowski JQ. Tau isoform profile and phosphorylation state in dementia pugilistica recapitulate Alzheimer’s disease. Acta Neuropathol. 2001;101(5):518–524. doi: 10.1007/s004010000330. [DOI] [PubMed] [Google Scholar]
- 7.Ashton NJ, Leuzy A, Karikari TK, Mattsson-Carlgren N, Dodich A, Boccardi M, et al. The validation status of blood biomarkers of amyloid and phospho-tau assessed with the 5-phase development framework for AD biomarkers. Eur J Nucl Med Mol Imaging. 2021;48:2140-56. [DOI] [PMC free article] [PubMed]
- 8.Zetterberg H, Blennow K. Moving fluid biomarkers for Alzheimer’s disease from research tools to routine clinical diagnostics. Mol Neurodegener. 2021;16(1):10. doi: 10.1186/s13024-021-00430-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McGrowder DA, Miller F, Vaz K, Nwokocha C, Wilson-Clarke C, Anderson-Cross M, et al. Cerebrospinal fluid biomarkers of Alzheimer’s disease: current evidence and future perspectives. Brain Sci. 2021;11(2):215. doi: 10.3390/brainsci11020215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ehrenberg AJ, Khatun A, Coomans E, Betts MJ, Capraro F, Thijssen EH, et al. Relevance of biomarkers across different neurodegenerative diseases. Alzheimers Res Ther. 2020;12(1):56. doi: 10.1186/s13195-020-00601-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stein TD, Montenigro PH, Alvarez VE, Xia W, Crary JF, Tripodis Y, et al. Beta-amyloid deposition in chronic traumatic encephalopathy. Acta Neuropathol. 2015;130(1):21–34. doi: 10.1007/s00401-015-1435-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alosco ML, Cherry JD, Huber BR, Tripodis Y, Baucom Z, Kowall NW, et al. Characterizing tau deposition in chronic traumatic encephalopathy (CTE): utility of the McKee CTE staging scheme. Acta Neuropathol. 2020;140(4):495–512. doi: 10.1007/s00401-020-02197-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nelson PT, Jicha GA, Schmitt FA, Liu H, Davis DG, Mendiondo MS, et al. Clinicopathologic correlations in a large Alzheimer disease center autopsy cohort: neuritic plaques and neurofibrillary tangles "do count" when staging disease severity. J Neuropathol Exp Neurol. 2007;66(12):1136–1146. doi: 10.1097/nen.0b013e31815c5efb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mez J, Solomon TM, Daneshvar DH, Murphy L, Kiernan PT, Montenigro PH, et al. Assessing clinicopathological correlation in chronic traumatic encephalopathy: rationale and methods for the UNITE study. Alzheimers Res Ther. 2015;7(1):62. doi: 10.1186/s13195-015-0148-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adams JW, Alvarez VE, Mez J, Huber BR, Tripodis Y, Xia W, et al. Lewy Body pathology and chronic traumatic encephalopathy associated with contact sports. J Neuropathol Exp Neurol. 2018;77(9):757–768. doi: 10.1093/jnen/nly065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McKee AC, Stern RA, Nowinski CJ, Stein TD, Alvarez VE, Daneshvar DH, et al. The spectrum of disease in chronic traumatic encephalopathy. Brain. 2013;136(Pt 1):43–64. doi: 10.1093/brain/aws307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boyle PA, Yu L, Wilson RS, Leurgans SE, Schneider JA, Bennett DA. Person-specific contribution of neuropathologies to cognitive loss in old age. Ann Neurol. 2018;83(1):74–83. doi: 10.1002/ana.25123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karanth S, Nelson PT, Katsumata Y, Kryscio RJ, Schmitt FA, Fardo DW, et al. Prevalence and clinical phenotype of quadruple misfolded proteins in older adults. JAMA Neurol. 2020;77(10):1299-307. [DOI] [PMC free article] [PubMed]
- 19.McKeith IG. Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB): report of the Consortium on DLB International Workshop. J Alzheimers Dis. 2006;9(3 Suppl):417–423. doi: 10.3233/jad-2006-9s347. [DOI] [PubMed] [Google Scholar]
- 20.Mackenzie IR, Neumann M, Bigio EH, Cairns NJ, Alafuzoff I, Kril J, et al. Nomenclature and nosology for neuropathologic subtypes of frontotemporal lobar degeneration: an update. Acta Neuropathol. 2010;119(1):1–4. doi: 10.1007/s00401-009-0612-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cairns NJ, Bigio EH, Mackenzie IR, Neumann M, Lee VM, Hatanpaa KJ, et al. Neuropathologic diagnostic and nosologic criteria for frontotemporal lobar degeneration: consensus of the Consortium for Frontotemporal Lobar Degeneration. Acta Neuropathol. 2007;114(1):5–22. doi: 10.1007/s00401-007-0237-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cherry JD, Esnault CD, Baucom ZH, Tripodis Y, Huber BR, Alvarez VE, et al. Tau isoforms are differentially expressed across the hippocampus in chronic traumatic encephalopathy and Alzheimer’s disease. Acta Neuropathol Commun. 2021;9(1):86. doi: 10.1186/s40478-021-01189-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cherry JD, Kim SH, Stein TD, Pothast MJ, Nicks R, Meng G, et al. Evolution of neuronal and glial tau isoforms in chronic traumatic encephalopathy. Brain Pathol. 2020;30(5):913–925. doi: 10.1111/bpa.12867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Falcon B, Zivanov J, Zhang W, Murzin AG, Garringer HJ, Vidal R, et al. Novel tau filament fold in chronic traumatic encephalopathy encloses hydrophobic molecules. Nature. 2019;568(7752):420–423. doi: 10.1038/s41586-019-1026-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stathas S, Alvarez VE, Xia W, Nicks R, Meng G, Daley S, et al. Tau phosphorylation sites serine and serine are differently altered in chronic traumatic encephalopathy and Alzheimer’s disease. Alzheimers Dement. 2021. 10.1002/alz.12502. [DOI] [PMC free article] [PubMed]
- 26.Buerger K, Ewers M, Pirttila T, Zinkowski R, Alafuzoff I, Teipel SJ, et al. CSF phosphorylated tau protein correlates with neocortical neurofibrillary pathology in Alzheimer’s disease. Brain. 2006;129(Pt 11):3035–3041. doi: 10.1093/brain/awl269. [DOI] [PubMed] [Google Scholar]
- 27.Tapiola T, Alafuzoff I, Herukka SK, Parkkinen L, Hartikainen P, Soininen H, et al. Cerebrospinal fluid {beta}-amyloid 42 and tau proteins as biomarkers of Alzheimer-type pathologic changes in the brain. Arch Neurol. 2009;66(3):382–389. doi: 10.1001/archneurol.2008.596. [DOI] [PubMed] [Google Scholar]
- 28.Hampel H, Burger K, Teipel SJ, Bokde AL, Zetterberg H, Blennow K. Core candidate neurochemical and imaging biomarkers of Alzheimer’s disease. Alzheimers Dement. 2008;4(1):38–48. doi: 10.1016/j.jalz.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 29.Hansson O, Zetterberg H, Buchhave P, Londos E, Blennow K, Minthon L. Association between CSF biomarkers and incipient Alzheimer’s disease in patients with mild cognitive impairment: a follow-up study. Lancet Neurol. 2006;5(3):228–234. doi: 10.1016/S1474-4422(06)70355-6. [DOI] [PubMed] [Google Scholar]
- 30.Mattsson N, Zetterberg H, Hansson O, Andreasen N, Parnetti L, Jonsson M, et al. CSF biomarkers and incipient Alzheimer disease in patients with mild cognitive impairment. JAMA. 2009;302(4):385–393. doi: 10.1001/jama.2009.1064. [DOI] [PubMed] [Google Scholar]
- 31.Stern RA, Adler CH, Chen K, Navitsky M, Luo J, Dodick DW, et al. Tau positron-emission tomography in former national football league players. N Engl J Med. 2019;380(18):1716–1725. doi: 10.1056/NEJMoa1900757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Standring OJ, Friedberg J, Tripodis Y, Chua AS, Cherry JD, Alvarez VE, et al. Contact sport participation and chronic traumatic encephalopathy are associated with altered severity and distribution of cerebral amyloid angiopathy. Acta Neuropathol. 2019;138(3):401–413. doi: 10.1007/s00401-019-02031-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McKee AC, Stein TD, Kiernan PT, Alvarez VE. The neuropathology of chronic traumatic encephalopathy. Brain Pathol. 2015;25(3):350–364. doi: 10.1111/bpa.12248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mielke MM, Vemuri P, Rocca WA. Clinical epidemiology of Alzheimer’s disease: assessing sex and gender differences. Clin Epidemiol. 2014;6:37–48. doi: 10.2147/CLEP.S37929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morihara T, Kudo T, Ikura Y, Kashiwagi Y, Miyamae Y, Nakamura Y, et al. Increased tau protein level in postmortem cerebrospinal fluid. Psychiatry Clin Neurosci. 1998;52(1):107–110. doi: 10.1111/j.1440-1819.1998.tb00981.x. [DOI] [PubMed] [Google Scholar]
- 36.Alosco ML, Tripodis Y, Fritts NG, Heslegrave A, Baugh CM, Conneely S, et al. Cerebrospinal fluid tau, Abeta, and sTREM2 in Former National Football League Players: modeling the relationship between repetitive head impacts, microglial activation, and neurodegeneration. Alzheimers Dement. 2018;14(9):1159–1170. doi: 10.1016/j.jalz.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stern RA, Tripodis Y, Baugh CM, Fritts NG, Martin BM, Chaisson C, et al. Preliminary study of plasma exosomal tau as a potential biomarker for chronic traumatic encephalopathy. J Alzheimers Dis. 2016;51(4):1099–1109. doi: 10.3233/JAD-151028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shahim P, Tegner Y, Wilson DH, Randall J, Skillback T, Pazooki D, et al. Blood biomarkers for brain injury in concussed professional ice hockey players. JAMA Neurol. 2014;71(6):684–692. doi: 10.1001/jamaneurol.2014.367. [DOI] [PubMed] [Google Scholar]
- 39.Washnik NJ, Anjum J, Lundgren K, Phillips S. A review of the role of auditory evoked potentials in mild traumatic brain injury assessment. Trends Hear. 2019;23:2331216519840094. doi: 10.1177/2331216519840094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Muraoka S, Jedrychowski MP, Tatebe H, DeLeo AM, Ikezu S, Tokuda T, et al. Proteomic profiling of extracellular vesicles isolated from cerebrospinal fluid of former national football league players at risk for chronic traumatic encephalopathy. Front Neurosci. 2019;13:1059. doi: 10.3389/fnins.2019.01059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nedergaard M. Neuroscience. Garbage truck of the brain. Science. 2013;340(6140):1529–1530. doi: 10.1126/science.1240514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Janelidze S, Stomrud E, Smith R, Palmqvist S, Mattsson N, Airey DC, et al. Cerebrospinal fluid p-tau217 performs better than p-tau181 as a biomarker of Alzheimer’s disease. Nat Commun. 2020;11(1):1683. doi: 10.1038/s41467-020-15436-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Simren J, Leuzy A, Karikari TK, Hye A, Benedet AL, Lantero-Rodriguez J, et al. The diagnostic and prognostic capabilities of plasma biomarkers in Alzheimer’s disease. Alzheimers Dement. 2021;17(7):1145–1156. doi: 10.1002/alz.12283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ashton NJ, Pascoal TA, Karikari TK, Benedet AL, Lantero-Rodriguez J, Brinkmalm G, et al. Plasma p-tau231: a new biomarker for incipient Alzheimer’s disease pathology. Acta Neuropathol. 2021;141(5):709–724. doi: 10.1007/s00401-021-02275-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 2: Figure e-1. Rank-normalized fold change of A. p-tau181, B. p-tau231, C. total tau, D. Aβ1-42 and E. Aβ1-40 for no CTE/no AD (control), Low CTE, and Low AD groups. Scatter plots show individual values, median and interquartile range (25-75%) as bars, *p < 0.05 corrected for multiple comparisons; ANCOVA adjusting for age.
Additional file 3: Figure e-2. Rank-normalized fold change of A. p-tau181, B. p-tau231, C. total tau, D. Aβ1-42 and E. Aβ1-40 for High CTE, Intermediate/High AD, and CTE+AD groups. Scatter plots show individual values, median and interquartile range (25-75%), *p < 0.05 corrected for multiple comparisons; ANCOVA adjusting for age.
Additional file 4: Table e-1. Estimated Marginal Means and SEM in parentheses for rank normalized CSF analyte measurements from No CTE/no AD (control) group; showing ANCOVA adjusted for age, p <0.05. Table e-2. Estimated Marginal Means and SEM in parentheses for rank normalized CSF analyte measurements from No CTE/no AD (control) group; showing ANCOVA adjusted for age, sex, and PMI, p <0.05.
Data Availability Statement
Anonymized data not published within the article will be shared upon reasonable request.