Abstract
Burkitt lymphoma is a highly aggressive B cell non-Hodgkin’s lymphoma characterised by translocation of MYC gene on chromosome 8. This translocation is usually detected by fluorescent in-situ hybridisation (FISH) studies as part of routine diagnostic work-up and prognostication. FISH testing is commonly done with the break-apart probe (BAP). This case illustrates how this testing can be falsely negative. This patient is a young male diagnosed with Stage I low-risk Burkitt with FISH negative for MYC translocation initially on BAP testing. Additional testing with dual FISH probe detected MYC/IGH translocation. FISH testing using BAPs alone may be falsely negative for MYC translocations creating a diagnostic challenge and compromising the treatment approach and assessment of prognosis.
Keywords: pathology, haematology (drugs and medicines), carcinogenesis
Background
Burkitt lymphoma is an aggressive high grade B cell non-Hodgkin’s lymphoma characterised by the presence of translocation involving the MYC oncogene, most commonly t(8;14) with MYC/IGH fusion. This MYC translocation is detected by fluorescent in-situ hybridisation (FISH) studies as part of initial evaluation. However, false negative FISH results can be seen if break-apart probe (BAP) testing is performed alone and may delay or result in inaccurate diagnosis. We present a case of a young HIV positive male who was diagnosed with Burkitt lymphoma but confirmation was delayed by initial negativity by MYC gene BAP testing. Follow-up testing revealed MYC/IGH fusion using a dual fusion probe.
Case presentation
Forty-four years old patient presented with right neck swelling for a month. He denied any other associated complaints including weight or appetite change or constitutional symptoms. Of note, patient was diagnosed with HIV infection a few days prior with low CD4 count of 53 and was started on highly active antiretroviral therapy (HAART). Cytology from fine-needle aspiration of right cervical lymph node was positive for lymphoma with CD10 positivity, and FISH testing using the Vysis probe was positive for MYC rearrangement. Right anterior cervical lymph node excisional biopsy confirmed high grade B cell lymphoma consistent with Burkitt lymphoma and flow cytometry showing monoclonal B cells with CD 10, CD19 and CD20 expression. FISH testing for BCL2 and BCL6 was negative. Also Ki-67 proliferation index was >95%. Patient was started on chemotherapy with dose-adjusted (DA) R-EPOCH. His HIV medications were continued through the treatment. Interim positron emission tomography (PET)/CT scan after three cycles showed complete response with decrease in size of all lymph nodes with no metabolic activity.
Investigations
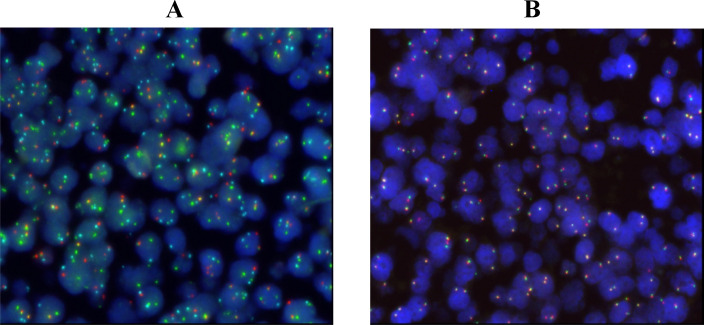
Initial FISH studies on the excision biopsy did not detect MYC rearrangement with a MYC BAP (figure 1A). Repeat FISH testing using the dual fusion MYC/IGH probe set revealed single fusion signals (1R2G1F2A, 60%, negative <9.0%) in the 8;14(MYC/IGH) probe set that was indicative of MYC/IGH/CEN8 fusion or t(8;14) (figure 1B). Of note, in situ hybridisation for Epstein-Barr virus (EBV) was negative. To complete work-up patient underwent PET/CT scan, which showed FDG-avid right cervical chain lymphadenopathy and splenomegaly. No other FDG activity was seen. Bone marrow biopsy as well as cerebrospinal fluid (CSF) fluid analysis on lumbar puncture showed no involvement by lymphoma.
Figure 1.
A: t(8;14) probe set shows fusion signals (yellow/orange) indicative of translocation juxtaposing the IGH and MYC genes. B: MYC break-apart probe shows intact probe sets with adjacent/fused green red signals. This indicates that the translocation did not occur within the gene.
Treatment
Patient completed six cycles of chemotherapy with excellent tolerance. Imaging showed complete disease response.
Outcome and follow-up
Patient showed excellent tolerance to chemotherapy treatment. He completed all six cycles as proposed without any treatment interruptions or delays. His PET/CT scan post cycle 6 showed complete response. He continues to do well and is on active surveillance.
Discussion
Burkitt lymphoma is a highly aggressive non-Hodgkin’s lymphoma. It has three distinct clinical forms: endemic, sporadic and immunodeficiency related. It is characterised by translocation of MYC oncogene on chromosome 8 (8q24) to an immunoglobulin gene, either the heavy chain (IGH) (most common approx. 80%), or kappa light chain (IGK) t(2;8) seen in approx. 15%, or lambda light chain (IGL) t(8;22) seen in approx. 5%.1
Detection of MYC rearrangement in high grade B cell lymphomas including Burkitt’s can be done either with FISH breakapart probe or with MYC/IGH dual fusion (D-FISH) probe. The break-point region of 8q24 can vary widely, particularly if partner gene is not IGH.2 Hence, MYC BAP is more sensitive and frequently used alone for screening. However, several studies have shown that there can be discordance between these two probe tests.1 3 King et al showed that out of a total 3489 cases studied using both MYC BAP and MYC/IGH D-FISH probe sets, there was 4.1% false negative rate using MYC BAP alone and 22.1% false negative with MYC-IGH fusion probes.3 This can often be explained by the complex nature of 8q24 rearrangements involving the MYC gene region. Sequencing the gene using Next Generation Sequencing (NGS) technology called mate pair sequencing (MPseq) has been used to further characterise the discrepancy in FISH testing by detecting complex structural abnormalities not appreciable on FISH testing.4 Given this discrepancy, laboratories should routinely screen for both MYC BAP and MYC-IGH upfront in order to avoid missing these translocations. Ideally, MYC BAP needs to be used first to detect MYC-IGH, MYC-IGK as well as MYC-IGL. If it is negative however morphologically suspicious or if IGH BAP is showing rearrangement, one should do a follow-up testing with the dual fusion probe. Occasionally cryptic MYC insertions can be present within IG locus and may not be detected with molecular cytogenetic approaches. These would require targeted sequencing of structural variant break-point regions to establish MYC status.5
Learning points.
As determination of MYC rearrangement is crucial for diagnosis and prognostication of Burkitt lymphoma, clinicians should be aware of the false negative rates of the commonly used detection methods.
It is important to use both IGH/MYC D-fluorescent in-situ hybridisation (D-FISH) and MYC break-apart probe (BAP) sets to detect potential cryptic rearrangements in MYC gene.
NGS technology such as mate pair sequencing (MPseq) can help identify novel gene rearrangements undetectable by FISH.
Footnotes
Contributors: PS: Conception, acquisition of data, interpretation of data, drafting the article. SS: Conception, acquisition of data, interpretation of data, revising the article. PC: Conception, interpretation of data, revising the article, final approval. KK: Conception, interpretation of data, revising the article, final approval.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1.Muñoz-Mármol AM, Sanz C, Tapia G, et al. Myc status determination in aggressive B-cell lymphoma: the impact of fish probe selection. Histopathology 2013;63:418–24. 10.1111/his.12178 [DOI] [PubMed] [Google Scholar]
- 2.Einerson RR, Law ME, Blair HE, et al. Novel fish probes designed to detect IGK-MYC and IGL-MYC rearrangements in B-cell lineage malignancy identify a new breakpoint cluster region designated BVR2. Leukemia 2006;20:1790–9. 10.1038/sj.leu.2404340 [DOI] [PubMed] [Google Scholar]
- 3.King RL, McPhail ED, Meyer RG, et al. False-negative rates for MYC fluorescence in situ hybridization probes in B-cell neoplasms. Haematologica 2019;104:e248–51. 10.3324/haematol.2018.207290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peterson JF, Pitel BA, Smoley SA, et al. Elucidating a false-negative MYC break-apart fluorescence in situ hybridization probe study by next-generation sequencing in a patient with high-grade B-cell lymphoma with IGH/MYC and IGH/BCL2 rearrangements. Molecular Case Studies 2019;5:a004077. 10.1101/mcs.a004077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wagener R, Bens S, Toprak UH, et al. Cryptic insertion of MYC exons 2 and 3 into the immunoglobulin heavy chain locus detected by whole genome sequencing in a case of "MYC-negative" Burkitt lymphoma. Haematologica 2020;105:e202–5. 10.3324/haematol.2018.208140 [DOI] [PMC free article] [PubMed] [Google Scholar]