Abstract
The COVID-19 pandemic has had a major impact on university students, particulary on their mental health. However, little is yet known about how to prevent and/or reduce this impact. Prior to COVID-19, some studies have shown that online stress management programs were successful enough to improve students' mental health and stress adjustment strategies, suggesting that these interventions should be further developed during the pandemic. Our study explored the effects on mental health of an online program that targeted stress management and learning. A total of 347 university students were initially recruited to take part in a non-randomized controlled study. After dropout, our final sample consisted of 114 participants, divided into two groups: an intervention group (participants who took part in the program) and the control group (participants who did not participate in the program). The variables measured were: anxiety and depressive symptoms, academic burnout, learned helplessness, and coping strategies. Means comparisons between baseline (T0) and an assessment at 8 weeks (T1) revealed reductions in anxiety symptoms and learned helplessness in the intervention group, but not in the control group. Our pilot study reports promising effects of an online program on students' psychological state.
Keywords: COVID-19 pandemic, University students, Anxiety, Coping, Learning, Online intervention
1. Introduction
The closure of universities owing to the COVID-19 pandemic brought about a digital revolution in higher education (Strielkowski, 2020), but came with undesirable consequences in terms of students’ stress levels (IAU, 2020). The multiple challenges (e.g., widespread transition to remote online learning, changes in assessment and examinations) the students faced had deleterious effects on their mental health (Lee, 2020; Sahu, 2020). More specifically, very high levels of anxiety and depressive symptoms were observed in university students during lockdown (Charbonnier et al., 2021; Essadek & Rabeyron, 2020; Husky et al., 2020; Le Vigouroux et al., 2021). These symptoms are associated with greater academic difficulty (Mills & Blankstein, 2000) and less use of effective learning strategies (Warr & Downing, 2000).
High levels of academic burnout were also identified (Fernández-Castillo, 2021; Zis et al., 2021). Academic burnout is defined as a contextual psychological syndrome caused by excessive and long-term academic pressure, which can lead students to gradually lose their energy, exhibit reduced enthusiasm for learning, and experience a lower sense of achievement (Meier, 1983). It has three dimensions (Maslach et al., 1996; Schaufeli et al., 2002): emotional exhaustion (i.e., feeling of being overworked and exhausted by university studies); cynicism (i.e., indifferent or distant attitude toward studies and learning), and a sense of accomplishment (i.e., tendency to view one's university studies positively; reverse-scored). High academic burnout can have detrimental effects on students' academic achievement and performance (Fiorilli et al., 2017; Rahmati, 2015), as well as their mental health (Schaufeli et al., 2002). Furthermore, burnout is closely associated with learned helplessness (Campbell & Martinko, 1998; McMullen & Krantz, 1988; Tayfur et al., 2013), which leads students to view academic tasks as being beyond their control (Carden et al., 2004), and to make poor strategy choices after failure (Dickhäuser et al., 2011; Ruthig et al., 2008), thus affecting their academic success (Macher et al., 2012; Peixoto & Almeida, 2010).
Prior to the COVID-19 pandemic, a central element of a students' psychological distress was difficulty coping with an accumulation of hassles (Réveillère et al., 2001). Public health measures in response to COVID-19 exposed students to new events that challenged their coping strategies (de Oliveira Araújo et al., 2020; Zhai & Du, 2020). Coping strategies can be defined as cognitive and behavioral efforts undertaken by individuals to deal with stressful situations (Lazarus & Folkman, 1984). They can be divided into maladaptive and adaptive strategies. Adaptive strategies, such as acceptance, include efforts to promote resolution and reduce stress (Muller & Spitz, 2003). Conversely, maladaptive strategies, such as behavioral disengagement, involve rigid and inappropriate adaptation that does not improve the situation and may increase stress (Carver et al., 2010; Carver & Scheier, 1990; Folkman, 1997). Maladaptive coping is positively correlated with academic burnout (Vizoso et al., 2019) and learned helplessness (Wang et al., 2017). Furthermore, recent research has shown that the more university students used avoidance strategies during lockdown, the more likely they were to have anxiety and depression symptoms (Dawson & Golijani-Moghaddam, 2020; Le Vigouroux et al., 2021).
Taken together, these findings should convince universities of the need to pay close attention to their students’ health. Indeed, Bonnano et al. (2007) and Lee et al. (2007) who tracked the long-term consequences of previous pandemics concluded that psychological problems may persist for months and even years after the event. In the current context, there are many obstacles to implementing conventional psychological interventions (e.g., face-to-face psychotherapy). To limit physical contact, online self-help interventions (e.g., web page, Facebook page, e-learning) have seemed a promising tool during the COVID-19 pandemic (Yang et al., 2020). Even before the pandemic, online self-help had proven to be effective for a range of mental health problems (Epping-Jordan et al., 2016; Moser et al., 2019; Zetterqvist et al., 2003). It was identified as being particularly valuable for university students, given their limited help-seeking behavior (Lintvedt et al., 2008; Ryan et al., 2010). In this regard, a systematic review and meta-analysis (Davies et al., 2014) suggests that online interventions might be beneficial in improving depressive symptoms, anxiety, and psychological distress outcomes in university students. More precisely, online self-help stress management programs can help reduce stress, anxiety and depression for students (Van Vliet & Andrews, 2009) and improve their coping strategies (George et al., 2013).
In the present research, we aimed to study the effects on students' psychological state of an online self-help program combining stress management and learning strategies. We hypothesized that university students who completed the program would have less anxiety symptoms (Hypothesis 1), fewer depressive symptoms (Hypothesis 2), less academic burnout (Hypothesis 3), less learned helplessness (Hypothesis 4), and would use fewer maladaptive strategies (Hypothesis 5), and more adaptive ones (Hypothesis 6), compared with students who did not participate in the program.
2. Methods
2.1. Ethics statement
This study respected the ethics code of the American Psychological Association (2002). Ethical review and approval were waived for this study, as it involved experiments in humanities and social sciences in the field of health, and was therefore not regarded as research involving human persons according to Article R1121-1 of the French Public Health Code. During the pre-inclusion information meetings, students were reminded that they could be seen by the university health service if they were experiencing difficulties. In addition, they were given contact information and appointment procedures. It should be noted that no students reported seeking psychological counseling during the 8 weeks of our study.
2.2. Participants
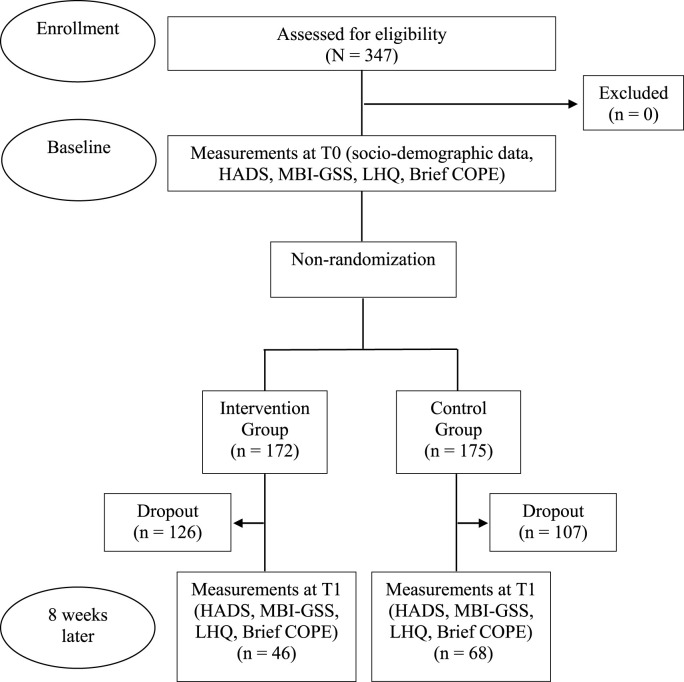
We initially recruited 347 participants. After dropout, our final sample was composed of 114 university students, divided into two groups (see Fig. 1 ). The only inclusion criterion was to be enrolled as a student at Nîmes University. The intervention group contained participants who completed the program (n = 46; 84.8% female; M age = 20.06 ± 3.09 years). They came from various disciplines (28 in psychology, 6 in law, 4 in litterature and languages, 3 in history, 2 in physical activity and sports, 2 in biology, and 1 in mathematics), and had different higher education levels (16 in first year, 18 in second year, 7 in third year, 4 in fourth year and 1 in fifth year). The control group was composed of participants who did not take part in the program (n = 68; 88.2% female; M age = 22.76 ± 8.01 years; U = 1233, p = .05, rank biserial correlation, rbb = −0.21). They came from various disciplines (33 in psychology, 10 in litterature and languages, 8 in law, 6 in design, 5 in biology, 2 in sport and physical activities science, 2 in history, 1 in mathematics, and 1 in double degree), and different higher education levels (29 in first year, 18 in second year, 14 in third year, 5 in fourth year, and 2 in fifth year).
Fig. 1.
Flowchart of study participants.
HADS = Hospital Anxiety and Depression Scale; MBI-GSS = Maslach Burnout Inventory – General Student Survey; LHQ = Learned Helplessness Questionnaire.
2.3. Measures
Anxiety and depressive symptoms were assessed using a French version of the Hospital Anxiety and Depression Scale (HADS; Lepine et al., 1985). This 14-item self-report questionnaire assesses anxiety and depressive symptoms (7 items for each dimension) with labels varying from one item to the next. Scores range from 0 to 21 for each dimension, with higher scores reflecting higher levels of anxiety or depressive symptoms. According to Bjelland et al. (2002), this scale has satisfactory correlations with other scales measuring depressive symptoms (r between 0.62 and 0.69) and anxiety (r between 0.44 and 0.65). Test-retest reliability is satisfactory, and the reliability coefficient is above 0.80 after 15 days. Internal consistency of the scale is good for both anxiety (α between 0.68 and 0.92) and depressive symptoms (α between 0.67 and 0.90). Although this scale has not been specifically validated with students, it is frequently administered in epidemiological studies in the general population (Bjelland et al., 2002; Hinz & Brähler, 2011), and was used in the first French epidemiological study of mental health in relation to COVID-19 (Chan-Chee et al., 2020). In our study, the internal consistency of both subscales was satisfactory (see Table 3).
Table 3.
Comparisons between students who left the study and those who completed it on clinical issues and coping strategies.
| Control Group |
Intervention Group |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| α | Final sample (n = 68) |
Dropouts (n = 107) |
U | p | rrb [95% CI] | Final sample (n = 46) |
Dropouts (n = 126) |
U | p | rrb [95% CI] | |||||
| M | SD | M | SD | M | SD | M | SD | ||||||||
| Age in years | 20.1 | (3.09) | 19.8 | (1.85) | 3523 | .72 | -.03 [-.21, .14] | 22.8 | (8.02) | 21.3 | (5.01) | 3023 | .66 | .04 [-.15, .23] | |
| Clinical issues | |||||||||||||||
| Anxiety | .74 | 9.49 | (4.14) | 10.1 | (4.42) | 3352 | .38 | -.08 [-.25, .10] | 10 | (3.88) | 12.3 | (4.03) | 1941 | <.001 | -.33 [-.49, −.15] |
| Depression | .71 | 11.5 | (4.23) | 11.4 | (4.43) | 3532 | .75 | -.03 [-.20, .15] | 10.7 | (4.79) | 10.3 | (3.85) | 3202 | .29 | .11 [-.09, .29] |
| Academic burnout | .86 | 2.83 | (1.09) | 3.21 | (1.13) | 2917 | .03 | -.20 [-.36, −.03] | 2.67 | (1.01) | 3.19 | (1.05) | 1977 | <.001 | -.32 [-.48, −.13] |
| Exhaustion | .87 | 3.3 | (1.51) | 3.81 | (1.50) | 2952 | .04 | -.19 [-.35, −.02] | 3.35 | (1.40) | 3.86 | (1.45) | 2282 | .03 | -.21 [-.39, −.02] |
| Academic efficacy | .80 | 2.86 | (1.22) | 3.08 | (1.35) | 3357 | .45 | -.07 [-.24, .11] | 2.56 | (1.22) | 3.11 | (1.36) | 2222 | .02 | -.23 [-.41, −.04] |
| Cynicism | .77 | 2.33 | (1.44) | 2.77 | (1.58) | 3045 | .09 | -.16 [-.32, .02] | 2.13 | (1.44) | 2.61 | (1.51) | 2319 | .05 | -.20 [-.38, −.01] |
| Learned helplessness | .87 | 25.6 | (8.28) | 28.7 | (10.30) | 3038 | .07 | -.17 [-.33, .01] | 26.7 | (8.35) | 30 | (9.52) | 2302 | .04 | -.21 [-.38, −.01] |
| Coping | |||||||||||||||
| Active Coping | .70 | 4.47 | (1.57) | 4.29 | (1.71) | 3897 | .42 | .07 [-.10, .24] | 4.67 | (1.66) | 4.5 | (1.63) | 3071 | .55 | .06 [-.14, .25] |
| Planning | .76 | 4.93 | (1.80) | 4.67 | (1.69) | 3948 | .34 | -.09 [-.09, .26] | 5.24 | (1.55) | 4.79 | (1.58) | 3457 | .05 | .19 [0, .37] |
| Using instrumental support | .81 | 4.04 | (1.63) | 4.35 | (1.65) | 3229 | .20 | -.11 [-.28, .06] | 4.89 | (1.73) | 4.71 | (1.80) | 3101 | .48 | .07 [-.13, .26] |
| Using emotional support | .81 | 4.16 | (1.68) | 4.5 | (1.91) | 3310 | .31 | -.09 [-.26, .09] | 5.17 | (1.76) | 5.18 | (1.89) | 2865 | .91 | -.01 [-.20, .18] |
| Venting | .72 | 4.16 | (1.67) | 4.42 | (1.57) | 3234 | .21 | -.11 [-.28, .06] | 5.02 | (1.77) | 4.6 | (1.77) | 3290 | .17 | .14 [-.06, .32] |
| Positive reframing | .78 | 4.56 | (1.90) | 4.79 | (1.78) | 3372 | .41 | -.07 [-.24, .10] | 4.89 | (1.51) | 4.52 | (1.60) | 3337 | .12 | .15 [-.04, .34] |
| Humor | .79 | 3.21 | (1.57) | 3.45 | (1.66) | 3321 | .31 | -.09 [-.26, .09] | 2.87 | (1.33) | 2.98 | (1.34) | 2726 | .51 | -.06 [-.25, .14] |
| Acceptance | .75 | 5.63 | (1.53) | 5.24 | (1.80) | 4020 | .24 | .11 [-.07, .27] | 4.96 | (1.63) | 4.98 | (1.47) | 2853 | .87 | -.02 [-.21, .18] |
| Religion | .86 | 2.5 | (1.11) | 2.67 | (1.40) | 3486 | .55 | -.04 [-.21, .13] | 3.28 | (1.72) | 3.47 | (1.98) | 2807 | .74 | -.03 [-.22, .16] |
| Behavioral disengagement | .80 | 3.49 | (1.52) | 3.78 | (1.93) | 3474 | .60 | -.05 [-.22, .13] | 3.17 | (1.54) | 3.84 | (1.68) | 2164 | .01 | -.25 [-.43, −.06] |
| Self-blame | .76 | 4.53 | (1.47) | 4.26 | (1.54) | 4035 | .22 | .11 [-.07,28] | 4.85 | (1.63) | 5.36 | (1.66) | 2398 | .08 | -.17 [-.35, .02] |
| Self-distraction | .28 | 5.09 | (1.72) | 5.13 | (1.41) | 3596 | .90 | -.01 [-.19, .16] | 5.3 | (1.46) | 5.18 | (1.49) | 2971 | .80 | .03 [-.17, .22] |
| Denial | .67 | 2.59 | (1.04) | 3.06 | (1.45) | 3054 | .05 | -.16 [-.33, .01] | 3.22 | (1.71) | 3.24 | (1.52) | 2778 | .66 | -.04 [-.23, .15] |
| Substance use | .97 | 2.25 | (0.74) | 2.69 | (1.51) | 3193 | .05 | -.12 [-.29, .05] | 2.59 | (1.34) | 3.09 | (1.78) | 2453 | .06 | -.15 [-.34, .04] |
Academic burnout was measured with the French version of the Maslach Burnout Inventory-General Survey for Students (MBI-GSS; Copyright ©1996, 2016 Schaufeli, Leiter, Maslach & Jackson, used with the approval of Mind Garden Inc). This 16-item self-report questionnaire captures three dimensions of academic burnout: emotional exhaustion (e.g., “I feel exhausted at the end of a day at the university”), academic efficacity (reversed score; e.g., “I feel fulfilled when I achieve my academic goals”), and cynicism (e.g., “I feel less enthusiastic about my studies”). Each item is rated on a 7-point Likert-type scale, with responses ranging from 0 (Never) to 6 (Always). A high score indicates high academic burnout. When Schaufeli et al. (2002) examined the factorial validity and invariance of the MBI-GSS with European students, they showed that the three-factor structure (i.e., exhaustion, cynicism, and efficacy) of the MBI-GSS fitted the data. In our study, the internal consistency of these three dimensions was satisfactory (see Table 3).
Learned helplessness was assessed using a French version of the Learned Helplessness Questionnaire (LHQ; Sorrenti et al., 2014). Only the subscale measuring learned helplessness was included. Its 12 items are rated on a 5-point Likert scale ranging from Not true to Absolutely true. Higher scores reflect higher levels of an inability to learn. This scale has been validated with Italian students and has good internal reliability (α = 0.77). In our study, internal consistency was also satisfactory (see Table 3).
Coping strategies were assessed using a French version of the situational version of the Brief-COPE (Muller & Spitz, 2003). Participants were instructed to refer to a stressful situation related to the COVID-19 pandemic. This self-report scale assesses 14 coping strategies (two items per strategy): active coping, planning, instrumental support, use of emotional support, venting, behavioral disengagement, self-distraction, self-blame, positive reframing, humor, denial, acceptance, religion, and substance use. Participants rate each of the 28 items on a 4-point Likert scale ranging from Never to Always. Higher scores reflect higher levels of strategy use. The French validation of this scale was performed with French students and revealed good psychometric properties. This scale has good external validity, showing consistent correlations with instruments assessing psychological equilibrium. It also has good structural validity. In our study, the internal consistency of the various factors was satisfactory, except for self-distraction (see Table 3).
2.4. Intervention
The 8-week program featured eight modules on the following themes: stress information, learning information, emotion and stress regulation strategies, cognitive and metacognitive learning strategies, cognitive reappraisal and self-blame, motivation for learning, managing worry and uncertainty, and synthesis. Each module was composed of two 10-min videos containing information, tools, student experiences, and quizzes, which were published each week on a private Facebook group. After watching the videos, participants had to validate the module on Facebook. The program is described in detail in Table 1 .
Table 1.
Program description.
| Theme | Content | Medium used | Exercises and additional information | |
|---|---|---|---|---|
| Module 1 | Stress information | - Program schedule | - 2 videos (one with student interviews) - 1 information brochure | - Mindfulness - Breathing control |
| - Definition of stress and stressors | ||||
| - Definition of implicit theory of emotion | ||||
| - Introduction to Mindfulness | ||||
| - Sleep advice | ||||
| Module 2 | Learning information | - Definition of learning | - 2 videos (one with student interviews) | - Invitation to reflect on their learning strategies |
| - Strategies for learning | ||||
| - Distance learning strategies | ||||
| Module 3 | Acceptance and avoidance | - Definition of avoidance | - 2 videos based on fictional student situations | - Exercise to observe emotions |
| - Avoidance effects (short and long term) | ||||
| - Definition of acceptance | ||||
| - Acceptance effects (short and long term) | ||||
| Module 4 | Cognitive and metacognitive learning strategies | - Misconceptions about failure | - 2 videos (one with student interviews) | - Invitation to reflect on their learning strategies |
| - Metacognition | ||||
| - Promotion of most effective learning strategies | ||||
| Module 5 | Cognitive reappraisal and self-blame | - Definition of self-blame and its effects | - 2 videos (one with student interviews) | - ACT matrix |
| - Training in cognitive reappraisal | ||||
| - Introduction to ACT matrix | ||||
| Module 6 | Motivation and learning goals | - Different learning goals (control and performance goals) | - 4 videos (one with student interviews) | - Learning Goals Questionnaire - Physical activity - Diet |
| - Processes involved in motivation | ||||
| - Beliefs about intelligence | ||||
| - Physical activity | ||||
| - Diet | ||||
| Module 7 | Uncertainty and worry | - Definition of uncertainty | - 2 videos | - Cognitive restructuring exercise |
| - Definition of worry and the usefulness of worrying | ||||
| - Introduction to defusion | ||||
| Module 8 | Synthesis | - Presentation of the highlights of the different modules | - 1 video |
Our program was based on modules from previous online mental health interventions that had already proven to be effective with students (Lintvedt et al., 2008; Ryan et al., 2010; Van Vliet & Andrews, 2009), but had two innovative aspects: 1) elements and examples specific to the COVID-19 pandemic, and 2) the addition of modules focused on learning strategies (Modules 2, 4 and 6). It was therefore an original program, designed for the purposes of this research, and adapted to the context of the COVID-19 pandemic (notably concerning the themes of worry, stressors, and distance learning courses). The different modules were designed by five associate professors: two specializing in cognitive psychology, both experts in learning; two specializing in clinical psychology and cognitive and behavioral therapy, experts in stress and emotion regulation; and one specializing in health psychology, an expert in acceptance and commitment therapy. Two clinical psychology Master's students and two psychology undergraduates were involved in the process. All the modules were the result of a collaborative effort between the associate professors, who contributed their expertise, and the students, who pre-tested the modules and helped improve their design so that they would be attractive to other students.
Participants were repeatedly reminded that the program was not a substitute for medical and/or psychotherapeutic care. They were also informed of the services provided by the university (in particular, preventive medicine and health promotion services) that could support them if need be.
2.5. Procedure
There were two program sessions. During the first session, data were collected between 1 and 25 October 2020 (T0), and between 11 and 20 December 2020 (T1). During the second session, data were collected between 15 and 23 February 2021 (T0), and between 20 and 30, 2021 (T1). Each participant was identified by a code, in order to aggregate their data from the two measurement times and preserve anonymity. Recruitment was based on voluntary participation, and no compensation was offered to participants. The latter signed an informed consent and were told that their information would remain anonymous. Their participation was voluntary and could be withdrawn at any time. All data were collected online and were stored on a secure university computer.
2.5.1. Intervention group
All students at Nîmes University were informed by email of the possibility of taking part in an online program focused on stress and learning, and were invited to two information meetings. Students who were interested in the program were then invited to answer an online survey after signing a consent form. Once they had completed the survey, participants were given access to the 8-week (excluding vacation periods) program via Facebook. For ethical reasons, participants in the intervention group were free to contact the program coordinators (via email or Facebook) if, at any point during the program, they had personal questions about stress management, learning, or technical issues. It is important to note that during our program, only two participants contacted the coordinators, and exclusively to request technical assistance in accessing the group or watching the videos. They could also comment on the materials used in the different modules and discuss with the other members of the program. Participation in the program was not anonymous, as participants could see each others’ Facebook pseudonyms. However, the anonymity of their responses to the different measurement tools was guaranteed by the researchers. Finally, one week after the last module, participants once again completed an online survey after signing a consent form.
2.5.2. Control group
Meanwhile, an associate professor from Nîmes University sent an email to all the students at the university inviting them to participate in an online longitudinal study exploring students' psychological state during the COVID-19 pandemic. Interested students were asked to answer an online survey after signing a consent form. At the very beginning of the survey, we screened them to ensure for the possibility that they had not already taken part in the program. The questionnaire stopped for participants who answered “yes”. Participants who answered “no” formed the control group. Nine weeks later, they received an email asking them to complete an online survey again after signing a consent form. Given the major mental issues observed during the pandemic, we decided not to randomize our sample by placing participants on a waiting list. Instead, we considered it all the more important to offer the program to any student who wished to take part. The different stages of the study are illustrated in Fig. 1.
2.6. Statistical analysis
As our data did not follow the normal distribution, we conducted non-parametric analyses to perform comparisons between and within groups at T0 and T1 (using respectively Mann-Whitney tests and Wilcoxon tests), and comparisons between those who dropped out and those who completed the program (Wilcoxon tests). Effect sizes are expressed as the rank biserial correlation (rrb). Data were analyzed using the Jasp software (version 0.11.1).
3. Results
Before reporting our main analyses, we describe the profiles of the students who dropped out. The majority of these students were first-year undergraduates (see Table 2 ). In the intervention group, students who dropped out had higher levels of anxiety (rrb = −.33) and learned helplessness (rrb = −0.21) than students who completed the program, and exhibited more behavioral disengagement (rrb = 0.25). In both groups, those who dropped out had higher levels of academic burnout (rrb = −0.20 and 0.32). However, as effect sizes were low, these differences can be considered small (see Table 3 ).
Table 2.
Comparisons between students who left the study and those who completed it on university grade.
| Control Group (chi2 = 7.05, p = .32) |
Intervention Group (chi2 = 7.27, p = .40) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Final sample (n = 68) |
Dropouts (n = 107) |
Final sample (n = 46) |
Dropouts (n = 126) |
|||||
| n | % | n | % | n | % | n | % | |
| 1st year of Bachelor's degree | 29 | 42.65 | 47 | 43.93 | 16 | 34.78 | 67 | 53.17 |
| 2nd year of Bachelor's degree | 18 | 26.47 | 34 | 31.78 | 18 | 39.13 | 29 | 23.02 |
| 3rd year of Bachelor's degree | 12 | 17.65 | 20 | 18.69 | 7 | 15.22 | 18 | 14.29 |
| Professional degree | 2 | 2.94 | 3 | 2.80 | 1 | 0.79 | ||
| 1st year of Master's degree | 5 | 7.35 | 1 | 0.93 | 4 | 8.70 | 7 | 5.56 |
| 2nd year of Master's degree | 2 | 2.94 | 1 | 0.93 | 1 | 2.17 | 2 | 1.59 |
| PhD student | 1 | 0.93 | 1 | 0.79 | ||||
| Other | 1 | 0.79 | ||||||
Second, means, standard deviations, and comparison analyses between T0 and T1 for both groups are set out in Table 4 . First, results showed that the two groups were comparable on most of our variables of interest at T0, except for some coping strategies (see Appendix 1). Second, mean comparisons between T0 and T1 in the intervention group showed reductions in anxiety (rrb = 0.49) and learned helplessness (rrb = 0.51), and an increase in the use of humor to cope with stress (rrb = −0.55). This was not observed in the control group. Moreover, while participants in the control group reported a moderate increase in substance use to cope with stress (rrb = −.76) and academic burnout (rrb = −0.40), more precisely exhaustion (rrb = −0.34), this was not the case in the intervention group.
Table 4.
Descriptive analyses of our variables of interest and pre-versus post-intervention comparison.
| Control Group (n = 68) |
Intervention Group (n = 46) |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T0 |
T1 |
W | p | rrb [95% CI] | T1 |
T2 |
W | p | rrb [95% CI] | |||||
| M | (SD) | M | (SD) | M | (SD) | M | (SD) | |||||||
| Age in years | 20.06 | (3.1) | 22.76 | (8.02) | ||||||||||
| Clinical issues | ||||||||||||||
| Anxiety | 9.49 | (4.14) | 9.57 | (4.28) | 815.5 | .60 | -.08 [-.36, .21] | 10.02 | (3.88) | 8.74 | (3.86) | 552.5 | .01 | 0.49 [.17, .72] |
| Depression | 11.49 | (4.23) | 11.75 | (4.25) | 653 | .32 | -.15 [-.43, .15] | 10.7 | (4.79) | 9.7 | (5.39) | 558.5 | .18 | 0.24 [-.11, .53] |
| Academic burnout | 2.83 | (1.09) | 3.01 | (1.14) | 341.5 | .02 | -.40 [-.63, −.09] | 2.67 | (1.01) | 2.71 | (1.05) | 118.5 | .81 | −0.06 [-.49, .39] |
| Exhaustion | 3.30 | (1.51) | 3.58 | (1.61) | 641.5 | .02 | -.34 [-.57, −.07] | 3.35 | (1.40) | 3.28 | (1.58) | 461.5 | .70 | 0.07 [-.27, .40] |
| Academic efficacy | 2.86 | (1.22) | 2.77 | (1.21) | 1037 | .51 | .10 [-.19, .37] | 2.56 | (1.22) | 2.55 | (1.19) | 522 | .96 | 0.01 [-.32, .33] |
| Cynicism | 2.33 | (1.44) | 2.62 | (1.43) | 691.5 | .10 | -.24 [-.49, .04] | 2.13 | (1.44) | 2.29 | (1.44) | 382 | .71 | −0.07 [-.40, .28] |
| Learned helplessness | 25.63 | (8.28) | 25.57 | (8.60) | 538 | .98 | -.01 [-.32, .32] | 26.7 | (8.35) | 24.78 | (8.21) | 190.5 | .04 | 0.51 [.08, .76] |
| Coping | ||||||||||||||
| Active coping | 4.47 | (1.57) | 4.63 | (1.41) | 407 | .42 | -.14 [-.45, .20] | 4.67 | (1.66) | 5.11 | (1.58) | 165 | .06 | −0.38 (−.66, 0] |
| Planning | 4.93 | (1.80) | 4.91 | (1.47) | 469.5 | .99 | .003 [-.32, .33] | 5.24 | (1.55) | 5.28 | (1.68) | 275.5 | .93 | −0.02 [-.39, .36] |
| Using instrumental support | 4.04 | (1.63) | 4.16 | (1.80) | 308.5 | .36 | -.17 [-.49, .19] | 4.89 | (1.73) | 4.91 | (1.64) | 309.5 | .84 | 0.04 [-.33, .40] |
| Using emotional support | 4.16 | (1.68) | 4.27 | (1.74) | 403 | .72 | -.06 [-.39, .28] | 5.17 | (1.76) | 4.83 | (1.98) | 318 | .31 | 0.21 [-.19, .54] |
| Venting | 4.16 | (1.67) | 4.31 | (1.67) | 44.5 | .38 | -.15 [-.45, .18] | 5.02 | (1.77) | 5.26 | (1.79) | 249.5 | .28 | −0.21 [-.53, .17] |
| Positive reframing | 4.56 | (1.90) | 4.59 | (1.96) | 523.5 | .95 | .01 [-.31, .33] | 4.89 | (1.51) | 5.26 | (1.57) | 285.5 | .14 | −0.27 [-.56, .09] |
| Humor | 3.21 | (1.57) | 3.18 | (1.49) | 269.5 | .92 | .02 [-.36, .39] | 2.87 | (1.33) | 3.24 | (1.66) | 34.5 | .04 | −0.55 [.82, .08] |
| Acceptance | 5.63 | (1.53) | 5.4 | (1.58) | 642.5 | .15 | .24 [-.09, .52] | 4.96 | (1.63) | 5.22 | (1.76) | 230 | .16 | −0.27 [-.58, .10] |
| Religion | 2.50 | (1.11) | 2.47 | (1.06) | 44.5 | .69 | .14 [-.46, .65] | 3.28 | (1.72) | 3.46 | (1.81) | 70 | .31 | −0.26 [-.65, .24] |
| Behavioral disengagement | 3.49 | (1.52) | 3.52 | (1.36) | 406 | .96 | -.01 [-.35, .33] | 3.17 | (1.54) | 3 | (1.41) | 264 | .30 | 0.21 [-.20, .56] |
| Self-blame | 4.53 | (1.47) | 4.54 | (1.60) | 389 | .99 | -.003 [-.35, .34] | 4.85 | (1.63) | 4.7 | (1.58) | 389.5 | .56 | 0.11 [-.26, .45] |
| Self-distraction | 5.09 | (1.72) | 5.02 | (1.72) | 704.5 | .69 | .06 [-.25, .36] | 5.3 | (1.46) | 5.22 | (1.49) | 312.5 | .80 | 0.05 [-.32, .41] |
| Denial | 2.59 | (1.04) | 2.47 | (0.94) | 175 | .47 | .17 [-.28, .56] | 3.22 | (1.71) | 3.04 | (1.46) | 125 | .46 | 0.19 [-.30, .60] |
| Substance use | 2.25 | (0.74) | 2.57 | (1.40) | 9.5 | .02 | -.76 [-.93, −.33] | 2.59 | (1.34) | 2.41 | (1.22) | 51.5 | .34 | 0.32 [-.30, .75] |
4. Discussion
The COVID-19 pandemic and the resulting abrupt changes in daily life and ways of learning have had a substantial impact on university students, especially their mental health. However, little is yet known about how to prevent and/or reduce this impact. Before the pandemic, several studies had shown that online stress management programs can improve students' mental health and stress adjustment strategies (Davies et al., 2014; George et al., 2013; Van Vliet & Andrews, 2009), suggesting that these interventions could be developed further. Our nonrandomized controlled study explored the effects of an online self-help program targeting stress management and learning strategies on anxiety and depressive symptoms, academic burnout, learned helplessness and coping strategies among university students.
In line with our first hypothesis, results showed a decrease in anxiety for the university students who completed the program, whereas no change was observed for participants who did not take part. We can assume that the program, especially Modules 1 “stress information” and 7 “uncertainty and worry”, was able to help them better understand and manage their stress and concerns, not least by leading them to mobilize new resources (e.g., breathing control, mindfulness). As Hatta (2020) states in his editorial, developing a simple way to manage stress appears to be particularly useful in dealing with the inconveniences, hassles and problems of the COVID-19 pandemic. The level of intolerance of uncertainty has been a key component of the decline in psychological well-being during the COVID-19 pandemic (Seligman, 1975). Thus, the university students who benefited from the program may have been able to better understand their concerns and stress, and develop new resources, including ways of the coping with their pandemic-related worries. These factors may in turn have helped reduce their anxiety symptoms.
Similarly, in line with our fourth hypothesis, results revealed a decrease in learned helplessness among university students who benefited from the program, whereas no change was observed in participants who did not participate in the program. This program, especially Modules 2 “learning information”, 4 “cognitive and metacognitive learning strategies” and 6 “motivation and learning goals”, which included information about learning, learning strategies, and motivation to learn, may have allowed students to reflect on their strategies, opening the door to modifying some of them. This may have contributed to a decrease in learned helplessness, which is positively associated with maladaptive learning strategies (Dickhäuser et al., 2011; Ruthig et al., 2008). Given that a high level of learned helplessness is associated with more academic failures (Macher et al., 2012; Peixoto & Almeida, 2010), we can assume that a lowering of this level increases students' academic success. Future research would be worthwhile, to assess both the psychological state of the students, and their academic performance. Finally, although a decrease in depressive symptoms was not observed at the end of the program (refuting Hypothesis 2), we are nevertheless confident in the beneficial effects of the program, as it positively impacted learned helplessness, a central component of the behavioral model of depression (Seligman, 1975). Although we refrain from speculating too much, we call for further research to deepen this understanding and explore the effect of the program on long-term depressive symptoms.
Finally, contrary to Hypotheses 5 and 6, our program had little effect on students' stress coping strategies. However, it is important to note that we observed an increase in substance abuse to cope with stressful situations over the semester among students who did not participate in the program. This is consistent with the notion that the pandemic may have made it harder for individuals to use their coping strategies efficiently (Dawson & Golijani-Moghaddam, 2020). Finally, contrary to Hypothesis 3, the program had no impact on students' academic burnout. However, it is important to note that an increase in academic exhaustion was observed among students who did not participate in the program, but there was no change for students who did participate. This suggests that the program may have protected participants against exhaustion.
The present results, albeit promising, need to be interpreted with caution, for the following reasons. First, our sample was small, which limited the generalization of results and the use of certain approaches, such as clustering. We also observed a high dropout rate consistent with the literature (George et al., 2013; Zetterqvist et al., 2003). This is an important issue, as the participants who dropped out had higher levels of clinical outcomes (e.g., anxiety, academic burnout), especially in the intervention group. In addition, recruitment for the two groups was carried out on an exclusively voluntary basis, without randomization, and without stratified random sampling or clustering by characteristics. Consequently, reservations can legitimately be expressed about the representativeness of our sample and the homogeneity of our groups. It is nonetheless important to note that at inclusion, participants in the two groups had similar scores on our main variables of interest, except for some coping strategies, suggesting we should consider the results on coping strategies with more caution. Finally, all our participants came from a single university. Taken together, these factors reduce the generalizability of our results. Results need to be replicated with a more representative sample before they can be generalized. A second limitation is that our program was designed within the framework of this research, and adapted to the context of the COVID-19 pandemic, albeit inspired by programs that had already proven effective with students. Therefore, we had no prior evidence of the effectiveness of our program. Third, although our results indicated a promising effect of our program in the short term, further research efforts will be needed to assess its long-term impact. As the measures were obtained just a few days after the end of the program, we must refrain from overgeneralizing these findings, and from considering that the positive effects will persist over time. These results therefore deserve to be consolidated by research that includes several weeks after of follow up after the intervention.
To our knowledge, our study is the first to have assessed the effects of an innovative program targeting students’ mental health during the COVID-19 pandemic. Further research efforts will be needed to confirm the beneficial effects of this type of program on university students and to explore the duration of this effect over time. This is all the more essential given the known effects of the pandemic on mental health, both during (Charbonnier et al., 2021; Essadek & Rabeyron, 2020; Husky et al., 2020; Le Vigouroux et al., 2021) and after (Charbonnier et al., 2021; Woon et al., 2020) lockdown. The pandemic has also had a major impact in other areas, including diet and physical activity (Ammar et al., 2020; Goncalves et al., 2021; Hatta & Srijit, 2021), which may in turn have had psychological consequences (Hatta, 2020). For this reason, information on physical activity and diet was included in Module 6, and should be given greater importance in future research.
5. Conclusions
The COVID-19 pandemic and the abrupt changes it brought about in daily life and ways of learning have had a severe impact on university students, especially their mental health. It is therefore urgency for universities to take steps to prevent any further deterioration. Our pilot study highlighted promising effects on students' psychological state of an online self-help program focusing on stress and learning. More specifically, results revealed reductions in anxiety and learned helplessness among students who completed the program. The latter also appeared to prevent a deterioration in students' ability to cope with stress and an increase in their academic exhaustion. Further research efforts are needed to confirm the beneficial effects of this type of program among university students.
Declaration of competing interest
None declared.
Acknowledgements
The researchers of this study would like to thank the students who participated in the design and delivery of the modules and interviews. By alphabetical order: BEUCHER Antoine, DE THUIN Nina, FERNANDEZ Audrey, HUSSEINI Sofia, MOULIN Chloé, PALERMO Angèle.
Footnotes
This research was funded by National Research Agency, grant number ANR-21-COVR-0005.
Appendix 1. Comparison between control group and intervention group at T0
| Comparaison at T0 |
|||||
|---|---|---|---|---|---|
| U | P | rrb | 95% CI for rrb |
||
| Lower | Upper | ||||
| Age | −1233 | .05 | -.21 | -.41 | 0.002 |
| Clinical Issues | |||||
| Anxiety | 1416.5 | .39 | -.09 | -.30 | 0.12 |
| Depression | 1691 | .46 | .08 | -.14 | 0.29 |
| Academic burnout | 1701.5 | .43 | .09 | -.13 | 0.30 |
| Exhaustion | 1547.5 | .92 | -.01 | -.22 | 0.20 |
| Professional efficacy | 1805 | .16 | .15 | -.06 | 0.36 |
| Cynicism | 1713 | .39 | .09 | -.12 | 0.30 |
| Learned helplessness | 1438 | .47 | -.08 | -.29 | 0.14 |
| Coping | |||||
| Active Coping | 1471 | .59 | -.06 | -.27 | 0.16 |
| Planning | 1372.5 | .26 | -.12 | -.33 | 0.09 |
| Using instrumental support | 1110 | .007 | -.29 | -.47 | −0.08 |
| Using emotional support | 1081.5 | .004 | -.31 | -.49 | −0.10 |
| Venting | 1125.5 | .01 | -.28 | -.47 | −0.07 |
| Positive reframing | 1381.5 | .29 | -.12 | -.32 | 0.10 |
| Humor | 1753.5 | .23 | .12 | -.10 | 0.33 |
| Acceptance | 1940 | .03 | .24 | .03 | 0.43 |
| Religion | 1144.5 | .004 | -.27 | -.46 | −0.06 |
| Behavioral disengagement | 1785 | .18 | .14 | -.08 | 0.35 |
| Self-blame | 1408.5 | .36 | -.10 | -.31 | 0.12 |
| Self-distraction | 1462 | .55 | -.07 | -.28 | 0.15 |
| Denial | 1274.5 | .06 | -.19 | -.38 | 0.03 |
| Substance use | 1428 | .21 | -.09 | -.30 | 0.13 |
References
- Ammar A., Brach M., Trabelsi K., Chtourou H., Boukhris O., Masmoudi L., ECLB-COVID19 Consortium Effects of COVID-19 home confinement on eating behaviour and physical activity: Results of the ECLB-COVID19 international online survey. Nutrients. 2020;12(6):1583. doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjelland I., Dahl A., Haug T.T., Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: An updated literature review. Journal of Psychosomatic Research. 2002;52(2):69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- Campbell C.R., Martinko M.J. An integrative attributional perspective of empowerment and learned helplessness: A multimethod field study. Journal of Management. 1998;24(2):173–200. doi: 10.1177/014920639802400203. [DOI] [Google Scholar]
- Carden R., Bryant C., Moss R. Locus of control, test anxiety, academic procrastination, and achievement among college students. Psychological Reports. 2004;95(2):581–582. doi: 10.2466/pr0.95.2.581-582. [DOI] [PubMed] [Google Scholar]
- Carver C.S., Scheier M.F. Origins and functions of positive and negative affect: A control-process view. Psychological Review. 1990;97(1):19–35. doi: 10.1037/0033-295X.97.1.19. [DOI] [Google Scholar]
- Carver C.S., Scheier M.F., Segerstrom S.C. Optimism. Clinical Psychology Review. 2010;30(7):879–889. doi: 10.1016/j.cpr.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan-Chee C., Léon C., Lasbeur L., Lecrique J.M., Raude J., Arwidson P., du Roscoät E. La santé mentale des Français face au Covid-19: Prévalences, évolutions et déterminants de l’anxiété au cours des deux premières semaines de confinement. Bulletin Epidémiologique Hebdomadaire. 2020;13:260–269. http://beh.santepubliquefrance.fr/beh/2020/13/2020_13_1.html [Google Scholar]
- Charbonnier E., Le Vigouroux S., Goncalves A. Psychological vulnerability of French university students during the COVID-19 pandemic: A four-wave longitudinal survey. International Journal of Environmental Research and Public Health. 2021;18(18):9699. doi: 10.3390/ijerph18189699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies E.B., Morriss R., Glazebrook C. Computer-delivered and web-based interventions to improve depression, anxiety, and psychological well-being of university students: A systematic review and meta-analysis. Journal of Medical Internet Research. 2014;16(5):1–22. doi: 10.2196/jmir.3142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson D.L., Golijani-Moghaddam N. COVID-19: Psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. Journal of Contextual Behavioral Science. 2020;17:126–134. doi: 10.1016/j.jcbs.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickhäuser O., Reinhard M.A., Englert C. Of course I will...”: The combined effect of certainty and level of expectancies on persistence and performance. Social Psychology of Education. 2011;14(4):519–528. doi: 10.1007/s11218-011-9159-x. [DOI] [Google Scholar]
- Epping-Jordan J.E., Harris R., Brown F.L., Carswell K., Foley C., Garcia-Moreno C., Kogan C., van Ommeren M. Self-help plus (SH1): A new WHO stress management package. World Psychiatry. 2016;15(3):295–296. doi: 10.1002/wps.20355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essadek A., Rabeyron T. Mental health of French students during the Covid-19 pandemic. Journal of Affective Disorders. 2020;277:392–393. doi: 10.1016/j.jad.2020.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández-Castillo A. State-anxiety and academic burnout regarding university access selective examinations in Spain during and after the COVID-19 lockdown. Frontiers in Psychology. 2021;12:1–9. doi: 10.3389/fpsyg.2021.621863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorilli C., De Stasio S., Di Chiacchio C., Pepe A., Salmela-Aro K. School burnout, depressive symptoms and engagement: Their combined effect on student achievement. International Journal of Educational Research. 2017;84(May):1–12. doi: 10.1016/j.ijer.2017.04.001. [DOI] [Google Scholar]
- Folkman S. Positive psychological states and coping with severe stress. Social Science & Medicine. 1997;45(8):1207–1221. doi: 10.1016/S0277-9536(97)00040-3. [DOI] [PubMed] [Google Scholar]
- George D.R., Dellasega C., Whitehead M.M., Bordon A. Facebook-based stress management resources for first-year medical students: A multi-method evaluation. Computers in Human Behavior. 2013 doi: 10.1016/j.chb.2012.12.008. [DOI] [Google Scholar]
- Goncalves A., Le Vigouroux S., Charbonnier E. University students' lifestyle behaviors during the COVID-19 pandemic: A four-wave longitudinal survey. International Journal of Environmental Research and Public Health. 2021;18(17):8998. doi: 10.3390/ijerph18178998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatta S. The psychological sequelae during mental health and COVID-19 pandemic: Learning from the past for today's coping styles. Medecine & Health. 2020;15(1):1–4. [Google Scholar]
- Hatta S., Srijit D. Obesity during COVID-19 lockdown: Interesting facts. Medecine & Health. 2021;16(1):1–3. [Google Scholar]
- Hinz A., Brähler E. Normative values for the hospital anxiety and depression scale (HADS) in the general German population. Journal of Psychosomatic Research. 2011;71(2):74–78. doi: 10.1016/j.jpsychores.2011.01.005. [DOI] [PubMed] [Google Scholar]
- Husky M.M., Kovess-Masfety V., Swendsen J.D. Stress and anxiety among university students in France during Covid-19 mandatory confinement. Comprehensive Psychiatry. 2020;102:152191. doi: 10.1016/j.comppsych.2020.152191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IAU . 2020. Covid-19: Higher education challenges and responses. The global voice of higher education.https://www.iau-aiu.net/COVID-19-Higher-Education-challenges-and-responses [Google Scholar]
- Lazarus R.S., Folkman S. In: The handbook of behavioral medicine. Gentry W.D., editor. Guilford; 1984. Coping and adaptation; pp. 282–325. [Google Scholar]
- Le Vigouroux S., Goncalves A., Charbonnier E. The psychological vulnerability of French university students to the COVID-19 confinement. Health Education & Behavior. 2021;48(2):123–131. doi: 10.1177/1090198120987128. [DOI] [PubMed] [Google Scholar]
- Lee A.M., Wong J.G., McAlonan G.M., Cheung V., Cheung C., Sham P.C., Chua S.E. Stress and psychological distress among SARS survivors 1 year after the outbreak. Canadian Journal of Psychiatry. 2007;52(4):233–240. doi: 10.1177/070674370705200405. [DOI] [PubMed] [Google Scholar]
- Lee J. Mental health effects of school closures during COVID-19. The Lancet Child & Adolescent Health. 2020;4(6):421. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lepine J.P., Godchau M., Brun P. Evaluation de l’anxiété et de la dépression chez des patients hospitalisés dans un service de médecine interne. Annales Medico-Psychologiques. 1985;143:175–189. [PubMed] [Google Scholar]
- Lintvedt O.K., Sorensen K., Ostvik A.R., Verplanken B., Wang C.E. The need for web-based cognitive behavior therapy among university students. Journal of Technology in Human Services. 2008;26(2–4):239–258. [Google Scholar]
- Macher D., Paechter M., Papousek I., Ruggeri K. Statistics anxiety, trait anxiety, learning behavior, and academic performance. European Journal of Psychology of Education. 2012;27(4):483–498. doi: 10.1007/s10212-011-0090-5. [DOI] [Google Scholar]
- Maslach C., Jackson S.E., Leiter M.P. Consulting Psychologists Press; 1996. The Maslach burnout inventory manual. [Google Scholar]
- McMullen M.B., Krantz M. Burnout in day care workers: The effects of learned helplessness and self-esteem. Child & Youth Care Quarterly. 1988;17(4):275–280. doi: 10.1007/BF01083908. [DOI] [Google Scholar]
- Meier S.T. Toward a theory of burnout. Human Relations. 1983;36(10):899–910. doi: 10.1177/001872678303601003. [DOI] [Google Scholar]
- Mills J.S., Blankstein K.R. Perfectionism, intrinsic vs extrinsic motivation, and motivated strategies for learning: A multidimensional analysis of university students. Personality and Individual Differences. 2000;29(6):1191–1204. doi: 10.1016/S0191-8869(00)00003-9. [DOI] [Google Scholar]
- Moser C., Bachem R., Berger T., Maercker A. ZIEL: Internet-based self-help for adjustment problems: Results of a randomized controlled trial. Journal of Clinical Medicine. 2019;8(10):1655. doi: 10.3390/jcm8101655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller L., Spitz E. Évaluation multidimensionnelle du coping: Validation du Brief COPE sur une population française. Encephale. 2003;29(6 I):507–518. [PubMed] [Google Scholar]
- de Oliveira Araújo F.J., de Lima L.S.A., Cidade P.I.M., Nobre C.B., Neto M.L.R. Impact of Sars-Cov-2 and its reverberation in global higher education and mental health. Psychiatry Research. 2020;288:112977. doi: 10.1016/j.psychres.2020.112977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peixoto F., Almeida L.S. Self-concept, self-esteem and academic achievement: Strategies for maintaining self-esteem in students experiencing academic failure. European Journal of Psychology of Education. 2010;25(2):157–175. doi: 10.1007/s10212-010-0011-z. [DOI] [Google Scholar]
- Rahmati Z. The study of academic burnout in students with high and low level of self-efficacy. Procedia - Social and Behavioral Sciences. 2015;171:49–55. doi: 10.1016/j.sbspro.2015.01.087. 1996. [DOI] [Google Scholar]
- Réveillère C., Nandrino J., Sailly F., Mercier C., Moreel V. Étude des tracas quotidiens des étudiants : Liens avec la santé perçue. Annales Medico-Psychologiques. 2001;159(6):460–465. doi: 10.1016/S0003-4487(01)00070-1. [DOI] [Google Scholar]
- Ruthig J.C., Perry R.P., Hladkyj S., Hall N.C., Pekrun R., Chipperfield J.G. Perceived control and emotions: Interactive effects on performance in achievement settings. Social Psychology of Education. 2008;11(2):161–180. doi: 10.1007/s11218-007-9040-0. [DOI] [Google Scholar]
- Ryan M.L., Shochet I.M., Stallman H.M. Universal online interventions might engage psychologically distressed university students who are unlikely to seek formal help. Advances in Mental Health. 2010;9(1):73–83. [Google Scholar]
- Sahu P. Closure of universities due to coronavirus disease 2019 (COVID-19): Impact on education and mental health of students and academic staff. Cureus. 2020 doi: 10.7759/cureus.7541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaufeli W.B., Martinez I.M., Pinto A.M., Salanova M., Bakker A.B. Burnout and engagement in university students: A cross-national study. Journal of Cross-Cultural Psychology. 2002;33(5):464–481. [Google Scholar]
- Seligman M.E.P. W. H. Freeman; 1975. Helplessness: On depression, development, and death. [Google Scholar]
- Sorrenti L., Filippello P., Costa S., Buzzai C. Preliminary evaluation of a self-report tool for learned helplessness and mastery orientation in Italian students. Mediterranean Journal of Clinical Psychology. 2014;2(3):1–14. doi: 10.6092/2282. [DOI] [Google Scholar]
- Strielkowski W. 2020. COVID-19 pandemic and the digital revolution in academia and higher education. Preprints. [DOI] [Google Scholar]
- Tayfur O., Karapinar P.B., Camgoz S.M. The mediating effects of emotional exhaustion cynicism and learned helplessness on organizational justice-turnover intention linkage. International Journal of Stress Management. 2013;20(1):193–221. [Google Scholar]
- Van Vliet H., Andrews G. Internet-based course for the management of stress for junior high schools. Australian and New Zealand Journal of Psychiatry. 2009;43(4):305–309. doi: 10.1080/00048670902721145. [DOI] [PubMed] [Google Scholar]
- Vizoso C., Arias-Gundín O., Rodríguez C. Exploring coping and optimism as predictors of academic burnout and performance among university students. Educational Psychology. 2019;39(6):768–783. [Google Scholar]
- Wang C.Y., Zhang K., Zhang M. Dysfunctional attitudes, learned helplessness, and coping styles among men with substance use disorders. Social Behavior and Personality: International Journal. 2017;45(2):269–280. [Google Scholar]
- Warr P., Downing J. Learning strategies, learning anxiety and knowledge acquisition. British Journal of Psychology. 2000;91(3):311–333. doi: 10.1348/000712600161853. [DOI] [PubMed] [Google Scholar]
- Woon L.S.C., Hatta S., Nik Jaafar N.R., Leong Bin Abdullah M.F.I. Mental health status of university healthcare workers during the COVID-19 pandemic: A post–movement lockdown assessment. International Journal of Environmental Research and Public Health. 2020;17(24):9155. doi: 10.3390/ijerph17249155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L., Yin J., Wang D., Rahman A., Li X. Urgent need to develop evidence-based self-help interventions for mental health of healthcare workers in COVID-19 pandemic. Psychological Medicine. 2020;7:7–8. doi: 10.1017/S0033291720001385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zetterqvist K., Maanmies J., Ström L., Andersson G. Randomized controlled trial of internet-based stress management. Cognitive Behaviour Therapy. 2003;32(3):151–160. doi: 10.1080/16506070302316. [DOI] [PubMed] [Google Scholar]
- Zhai Y., Du X. Mental health care for international Chinese students affected by the COVID-19 outbreak. The Lancet Psychiatry. 2020;7(4):e22. doi: 10.1016/S2215-0366(20)30089-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zis P., Artemiadis A., Bargiotas P., Nteveros A., Hadjigeorgiou G.M. Medical studies during the COVID-19 pandemic: The impact of digital learning on medical students' Burnout and mental health. International Journal of Environmental Research and Public Health. 2021;18(1):1–9. doi: 10.3390/ijerph18010349. [DOI] [PMC free article] [PubMed] [Google Scholar]