Abstract
Purpose:
To provide a nationally representative description on the prevalences of policies, practices, programs, and supports relating to worksite wellness in US hospitals.
Design:
Cross-sectional, self-report of hospitals participating in Workplace Health in America (WHA) survey from November 2016 through September 2017.
Setting:
Hospitals across the United States.
Participants:
Random sample of 338 eligible hospitals participating in the WHA survey.
Measures:
We used previous items from the 2004 National Worksite Health Promotion survey. Key measures included presence of Worksite Health Promotion programs, evidence-based strategies, health screenings, disease management programs, incentives, work-life policies, barriers to health promotion program implementation, and occupational safety and health.
Analysis:
Independent variables included hospital characteristics (eg, size). Dependent characteristics included worksite health promotion components. Descriptive statistics and χ2 analyses were used.
Results:
Eighty-two percent of hospitals offered a wellness programs during the previous year with larger hospitals more likely than smaller hospitals to offer programs (P < .01). Among hospitals with wellness programs, 69% offered nutrition programs, 74% offered physical activity (PA) programs, and 84% had a policy to restrict all tobacco use. Among those with cafeterias or vending machines, 40% had a policy for healthier foods. Only 47% and 25% of hospitals offered lactation support or healthy sleep programs, respectively.
Conclusion:
Most hospitals offer wellness programs. However, there remain hospitals that do not offer wellness programs. Among those that have wellness programs, most offer supports for nutrition, PA, and tobacco control. Few hospitals offered programs on healthy sleep or lactation support.
Keywords: workplace health promotion, chronic disease prevention, hospitals, policies, programs, environmental supports, Centers for Disease Control and Prevention
Purpose
Hospitals are prominent employers in many communities. Hospitals are important models for health promotion efforts because of their prominence and health-driven missions. More than 6200 hospitals were registered with the American Hospital Association (AHA) in 2017 with more than 36 million admissions.1 Hospitals employ more than 5.2 million full- and part-time salary and wage workers.2 Hospital employees spend most of their nonleisure time at work and because worksite cultural norms play a major role in personal health choices, hospitals can play a leading role in employee health promotion.
Properly designed worksite health promotion programs can improve employees’ health and increase productivity.3 Effective programs address individual, environmental, policy, and cultural factors to target multiple health issues simultaneously.3 Research suggests that these programs may reduce employers’ costs associated with health care and absenteeism.4 Worksite health promotion programs can also have a positive influence on health behaviors (smoking, diet, physical activity [PA], alcohol consumption, and seat belt use), biometric measures (blood pressure and cholesterol levels), overall health of workers, and health-care services utilization.5
As part of their health promotion efforts, hospitals can offer environmental supports for healthy eating and PA, such as healthier food and beverage options in cafeterias, vending machines, and meetings or providing exercise facilities for employees or amenities such as bicycle racks, showers, or walking trails. For the example, the Cleveland Clinic was an early leader in supporting the availability of healthier food choices in hospitals and promoting their selection by employees.6 The Healthy Hospital Food Initiative in New York City is an example of a hospital-system-wide approach at procuring and promoting the selection of healthier food choices for employees.7 Research suggests that these supports may improve health behaviors, including food choices. Employees who report the availability of a cafeteria, snack bar, or food service at the worksite were more likely to consume fruit and vegetables more than twice daily and less likely to consume fast food.8 Efforts to ensure availability of healthier food options in worksite cafeterias and vending have improved employee food choices.8,9 Promotion of diverse, attractive, and walkable neighborhoods around workplaces do support walking, bicycling, and use of public transit.10 Linking these strategies to disease screening and management programs and incentives, such as health risk assessments (HRAs), also support employee health. Health risk assessments are associated with improved health outcomes and lower health-care costs.11 Financial incentives may be used to participate in HRAs.11
Despite the potential benefits of worksite health promotion, many employees report lack of support to be healthy at work.12 In a 2014 survey, only 20% of employed adults reported that their employer provided opportunities to eat a healthy diet, and just 30% reported that their employer provided the opportunity to exercise.13 Tracking national progress in worksite health promotion is difficult because of limited representative data. However, existing data suggest the need for improvement. In 2004, the National Worksite Health Promotion survey found that 80% of worksites had food or beverage vending machines and 24% had cafeterias.14 Only 38% of worksites labeled healthy food choices and only 6% promoted healthy food choices. Furthermore, only 15% of worksites had an on-site fitness facility, 40% completely prohibited smoking on worksite property, and 36% offered screening for hypertension. Data specific to hospital worksites are limited to a 2015 survey of AHA members, which found that 87% of AHA members offered health and wellness programs for employees.15 To support healthy eating, 68% reported posting nutritional information, 82% reported promoting healthy choices with signs, and 71% reported providing healthy options in vending machines. Furthermore, 64% of hospitals reported providing on-site exercise facilities, 92% reported tobacco-free campuses, and almost 80% offered disease management or weight loss programs. However, there is little information on the availability and type of policy and environment supports for healthier choices, as well as the use of lactation, stress, and sleep management programs in hospital settings.
In recent years, hospitals have increasingly focused on population health strategies that include many of the initiatives and examples described above.16 Therefore, the purpose of this analysis was to describe the prevalence of current health and wellness practices and programs in a sample of hospitals in the Workplace Health in America (WHA) 2017 survey and to highlight potential areas for improvement.
Methods
Study Design and Sample
The 2017 WHA survey is a cross-sectional survey of health promotion policies and practices in US worksites. The survey gathered information from a nationally representative sample of US worksites drawn from the Dun and Bradstreet database of all private and public employers with at least 10 employees. Worksites were defined as buildings, unique locations, or business units within an organization where work occurs. A worksite could also encompass a primary work address for field-based or telecommuting employees. A single worksite could include a group of buildings used by the same organization within close proximity, such as hospitals or university campuses.
The sampling methodology for WHA has been previously described.17 Briefly, worksites were sampled using a stratified simple random sample design with geographic region as the primary strata plus an additional stratum containing all hospital worksites. Workplace Health in America sampled a total of 35 584 worksites, including 2084 hospitals. A trained interviewer contacted each sampled worksite and asked the employer to identify the person most knowledgeable on workplace wellness activities. The most knowledgeable individual was defined as someone familiar with the organization’s benefits plan, policy manual, the health and safety environment, and who has been directly involved in current workplace health initiatives through participation as a member of wellness committee staff. Workplace wellness activities were verified for eligibility as having at least 10 employees engaged and a history of being open for at least 12 months. Interviewers determined that 1944 hospitals were eligible to complete the survey. Respondents were able to complete the survey by web, telephone interview, or mailed paper survey. Further details of the survey methods are available elsewhere.17 Interviewers were able to complete eligibility screening for 703 hospitals, of which 545 agreed to participate. By the end of the data collection period, 338 hospital worksites met criteria to be included in the analyses (overall hospital response rate of 17.3%).
Measures
Hospital characteristics included size (10–99 employees, 100–499 employees, or 500 or more employees), region (designated Northeast [Maine (ME), Vermont (VT), Connecticut (CT), Rhode Island (RI), Massachusetts (MA), New Hampshire (NH), New York (NY), Pennsylvania (PA), New Jersey (NJ), Maryland (MD), and Distric of Columbia (DC)], South [West Virginia (WV), Virginia (VA), North Carolina (NC), South Carolina (SC), Georgia (GA), Florida (FL), Alabama (AL), Tennessee (TN), Kentucky (KY), Mississippi (MS), Louisiana (LA), and Arkansas (AR)], Midwest [Minnesota (MN), Iowa (IA), Missouri (MO), Wisconsin (WI), Illinois (IL), Michigan (MI), Indiana (IN), and Ohio (OH)], Mountain West [Idaho (ID), Montana (MT), North Dakota (ND), South Dakota (SD), Nebraska (NE), Kansas (KS), Colorado (CO), Wyoming (WY), Utah (UT), Oklahoma (OK), Texas (TX), and New Mexico (NM)], or Pacific [Arizona (AZ), Washington (WA), Oregon (OR), California (CA), Nevada (NV), Alaska (AK), and Hawaii (HI)]), employer type (public for profit, private for profit, nonprofit, government, or other), employee health insurance coverage (full, partial, or none), and whether the hospital offered HRAs to employees.
The presence of any worksite wellness program was determined with the following question: “Thinking about this worksite location, did your organization offer any type of health promotion/wellness program for employees in the past 12 months?” This question was intentionally broad to capture many different types of activities. Hospitals that answered “yes” to this question were asked further questions about specific wellness program components and environmental supports within the past 12 months. Further information on measures has been published elsewhere.17 The present analysis focuses on wellness program components (eg, disease management programs and health screenings) as well as policy and environmental supports (eg, healthy food availability policies and onsite fitness facilities) relevant to chronic disease prevention.
Analysis
Analysis weights were calculated based on the inverse of selection probabilities to represent the total number of worksites in each region, size, and industry category, and were adjusted for both nonresponse and coverage. All percentages and analyses were calculated using sample weights and accounted for survey design variables using SAS version 9.4.
We first assessed hospital characteristics overall and according to the presence of workplace wellness programs. We tested for differences in characteristics, according to whether a hospital had a wellness program or not, using χ2 tests. Next, we assessed the presence of specific wellness program attributes among the 276 hospitals that reported having a wellness program. Finally, we used χ2 tests to assess differences in prevalences of nutrition, PA, smoking cessation, chronic disease screening, lactation support, and healthy sleep programs for employees according to hospital size. Hospitals were categorized as large if they had 500 or more employees or small if they had <500 employees.
For each topic module, hospitals were excluded from the analysis if they had missing data for that particular module. This resulted in a final sample size of 257 hospitals for the nutrition and PA modules and 252 hospitals for the modules pertaining to chronic disease health screenings, disease management and awareness, tobacco control, and general wellness and health promotion including lactation support, stress management, and healthy sleep. These exclusions for missing data may result in our estimates differing slightly from WHA survey results presented elsewhere.17
Results
Among the 338 hospitals analyzed, 81.7% offered any health promotion and or wellness programs during the past 12 months (data not shown). The prevalence of programs differed significantly by employer size (P < .01) and type (P < .05; Table 1). Large hospitals with 500 or more employees comprise nearly half (47.1%; 95% confidence interval [CI], 41.2–53.0) of the hospitals with programs, compared to only a fifth (21.0%; 95% CI, 10.8–31.1) of hospitals without programs. Nonprofit hospitals made up nearly 3-quarters (71.4%; 95% CI, 66.0–76.7) of hospitals with programs and less than half (48.4%; 95% CI, 36.0–60.9) of hospitals without such programs. Approximately half of all hospitals offered HRAs (51.2%; 95% CI, 45.8–56.5).
Table 1.
Characteristics of Worksites Participating in Workplace Health in America Survey, Overall and by Any Worksite Health Promotion/ Wellness Program Offered to Employees in the Past 12 Months.
| All Hospitals (n = 338)a |
Hospitals Offering Health Promotion/Wellness Programs (n = 276)a |
Hospitals not Offering Health Promotion/Wellness Programs (n = 62)a |
||||
|---|---|---|---|---|---|---|
| Characteristic | %b | 95% CIb | %b | 95% CIb | %b | 95% CIb |
| Sizec | ||||||
| 10–99 employees | 21.3 | 17.0–25.7 | 17.4 | 12.9–21.9 | 38.7 | 26.6–50.9 |
| 100–499 employees | 36.4 | 31.3–41.5 | 35.5 | 29.9–41.2 | 40.3 | 28.1–52.6 |
| 500 or more employees | 42.3 | 37.0–47.6 | 47.1 | 41.2–53.0 | 21 | 10.8–31.1 |
| Regiond | ||||||
| Northeast | 19.2 | 15.0–23.4 | 19.9 | 15.2–24.6 | 16.1 | 7.0–25.3 |
| South | 27.2 | 22.5–32.0 | 26.1 | 20.9–31.3 | 32.3 | 20.6–44.0 |
| Midwest | 27.2 | 22.5–32.0 | 29.0 | 23.6–34.3 | 19.4 | 9.5–29.2 |
| Mountain West | 16.9 | 12.9–20.9 | 16.0 | 11.6–20.3 | 21.0 | 10.8–31.1 |
| Pacific | 9.5 | 6.3–12.6 | 9.1 | 5.7–12.5 | 11.3 | 3.4–19.2 |
| Employer typee | ||||||
| For profit, public | 10.7 | 7.4–14.0 | 9.4 | 6.0–12.9 | 16.1 | 7.0–25.3 |
| For profit, private | 10.7 | 7.4–14.0 | 8.7 | 5.4–12.0 | 19.4 | 9.5–29.2 |
| Nonprofit | 67.2 | 62.1–72.2 | 71.4 | 66.0–76.7 | 48.4 | 36.0–60.9 |
| Government | 3.3 | 1.4–5.1 | 2.9 | 0.9–4.9 | 4.8 | 0.0–10.2 |
| Other | 0.6 | 0.0–1.4 | 0.4 | 0.0–1.1 | 1.6 | 0.0–4.8 |
| Do not know/missing | 7.7 | 4.8–10.5 | 7.2 | 4.2–10.3 | 9.7 | 2.3–17.1 |
| Health insurance | ||||||
| Full coverage | 44.4 | 39.1–49.7 | 44.2 | 38.3–50.1 | 45.2 | 32.7–57.6 |
| Partial coverage | 47.4 | 42.6–53.3 | 48.6 | 42.6–54.5 | 45.2 | 32.7–57.6 |
| No insurance coverage | 2.1 | 0.5–3.6 | 1.4 | 0.0–2.9 | 4.8 | 0.0–10.2 |
| Do not know/missing | 5.6 | 3.2–8.1 | 5.8 | 3.0–8.6 | 4.8 | 0.0–10.2 |
| Health risk assessmente | ||||||
| Yes | 20.5 | 18.6–22.5 | 38.5 | 34.9–42.2 | 6.3 | 4.8–7.8 |
| No | 60.6 | 58.2–63.0 | 41.8 | 38.3–45.4 | 75.3 | 72.5–78.1 |
| Do not know | 18.9 | 16.9–20.8 | 19.6 | 16.7–22.6 | 18.4 | 15.8–20.9 |
Abbreviation: 95% CI, 95% confidence interval.
Based on employer response of yes/no to the question “Thinking about this worksite location, did your organization offer any type of health promotion/wellness program for employees in the past 12 months?” Respondents who answered “Do not know” (n = 4) were classified as “No”
Unweighted sample size, weighted percentage, and 95% CI.
P < .01 for χ2 test comparing characteristics of hospitals with wellness programs to those without programs.
Northeast includes ME, VT, CT, RI, MA, NH, NY, PA, NJ, MD, and DC, South includes WV, VA, NC, SC, GA, FL, AL, TN, KY, MS, LA, and AR, Midwest includes MN, IA, MO, WI, IL, MI, IN, and OH, Mountain West includes ID, MT, ND, SD, NE, KS, CO, WY, UT, OK, TX, and NM, and Pacific includes AZ, WA, OR, CA, NV, AK, and HI.
P < .05 for χ2 test comparing characteristics of hospitals with wellness programs to those without programs.
Among hospitals who reported any activities or programs in the previous 12 months, 69.3% (95% CI, 63.6%−74.9%) offered programs to address nutrition and/or healthy eating for employees, 53.7% (95% CI, 47.6%−59.8%) provided free or subsidized lifestyle self-management programs that include advice or tools on healthy eating and 59.9% (95% CI, 53.9%−65.9%) offered programs to address obesity/weight management for employees (Table 2). Regarding the food environment, 86.4% (95% CI, 82.2%−90.6%) of hospitals with programs had food vending machines, 91.8% (95% CI, 88.5%−95.2%) had drink vending machines, 87.9% (95% CI, 83.9%−91.9%) provided a cafeteria or snack bar, and 44.4% (95% CI, 38.3%-50.4%) had an on-site or nearby farmers markets. In addition, 57.2% (95% CI, 51.1%−63.3%) of programs had a healthy meeting foods policy. Of those hospitals with on-site food available, a written policy or formal communication that (1) promotes availability of healthier food and drinks or (2) makes more than 50% of available food and drinks healthy was reported by 39.8% (95% CI, 33.5%−45.7%) and 41.6% (95% CI, 35.4%−47.8%) of respondents, respectively. Less than half (48.6%; 95% CI, 42.3%−54.8%) of hospitals with on-site food provided nutritional information on sodium, calories, transfats, or saturated fats, and one-fifth (19.2%; 95% CI, 14.2%-24.1%) subsidized or provided discounts on healthier foods and beverages. Slightly more than half of hospitals with on-site food (54.7%; 95% CI, 48.4%−61.0%) identified healthier food and beverage choices with signs or symbols.
Table 2.
Employer-Reported Worksite Food Environment and Nutrition Supports Among Hospitals Who Reported Any Wellness Activities or Programs During the Previous 12 Months.a
| Strategy | Yes | CI | No | 95% CI | Do not Know | 95% CI |
|---|---|---|---|---|---|---|
| Nutrition programs | ||||||
| Offer programs to address nutrition and/or healthy eating for employees (n = 257) | 69.3 | 63.6–74.9 | 24.1 | 18.9–29.4 | 6.6 | 3.6–9.7 |
| Free or subsidized lifestyle self-management programs that include advice or tools on healthy eating (n = 257) | 53.7 | 47.6–59.8 | 38.1 | 32.2–44.1 | 8.2 | 4.8–11.5 |
| Offer programs to address obesity/weight management for employees (n = 257) | 59.9 | 53.9–65.9 | 30.7 | 25.1–36.4 | 9.3 | 5.8–12.9 |
| Food environment amenitites and supports for healthy eating | ||||||
| Food vending machine (n = 257) | 86.4 | 82.2–90.6 | 12.8 | 8.7–17.0 | 0.8 | 0.0–1.9 |
| Drink vending machine (n = 257) | 91.8 | 88.5–95.2 | 7.7 | 4.5–11.1 | 0.4 | 0.0–1.2 |
| Cafeteria or snack bar (n = 257) | 87.9 | 83.9–91.9 | 12.1 | 8.1–16.1 | 0.0 | N/A |
| Break room with refrigerator and microwave (n = 257) | 90.3 | 86.6–93.9 | 7.0 | 3.9–10.1 | 2.7 | 0.7–4.7 |
| Food trucks that come to the worksite every day (n = 257) | 6.6 | 3.6–9.7 | 91.1 | 87.6–94.5 | 2.3 | 0.5–4.2 |
| On-site or nearby farmers market (n = 257) | 44.4 | 38.3–50.4 | 48.2 | 42.1–54.4 | 7.4 | 4.2–10.6 |
| Healthy meeting foods policy (n = 257) | 57.2 | 51.1–63.3 | 30.4 | 24.7–36.0 | 12.5 | 8.4–16.5 |
| Written policy or formal communication that makes healthier food and beverage choices available in cafeterias, vending, snack bars food trucksb (n = 245) | 39.6 | 35.4–47.8 | 47.8 | 41.5–54.0 | 12.7 | 8.5–16.8 |
| Written policy or formal communication that makes most (more than 50%) of the food and beverage choices available in cafeterias/snack bars, vending, catering trucks be healthy food itemsb (n = 245) | 41.6 | 35.4–47.8 | 44.9 | 38.7–51.1 | 13.5 | 9.2–17.8 |
| Provide nutritional information (beyond standard info on labels) on sodium, calories, trans-fats, or saturated fats for foods and beverages sold in worksite cafeterias, snack bars, vending, or food trucksb (n = 245) | 48.6 | 42.3–54.8 | 42.0 | 35.8–48.2 | 9.4 | 5.7–13.0 |
| Identify healthier food and beverage choices with signs or symbolsb (n = 245) | 54.7 | 48.4–61.0 | 35.9 | 29.9–42.0 | 9.4 | 5.7–13.0 |
| Subsidize or provide discounts on healthier foods and beverages offered in vending machines, cafeterias, snack bars, or food trucksb (n = 245) | 19.2 | 14.2–24.1 | 71.8 | 66.2–77.5 | 9.0 | 5.4–12.6 |
Abbreviation: 95% CI, 95% confidence interval.
Among hospitals that reported any wellness activities or programs in the previous 12 months, specific questions about food environment and nutrition supports were asked. Unweighted sample size, weighted percentage, and 95% CI.
Question only asked to respondents who reported having a food source (cafeteria and/or vending machine) available at their worksite.
Nearly three-quarters (73.5%; 95% CI, 68.1%−78.9%) of hospital wellness programs offered PA programs for employees, 35.8% (95% CI, 29.9%−41.7%) provided or subsidized physical fitness assessments, and 49.8% (95% CI, 43.7%-55.9%) offered free or subsidized lifestyle self-management programs that included advice on PA (Table 3). Regarding PA environmental amenities, 54.5% (95% CI, 48.4%−60.6%) provided an on-site exercise facility, and 61.5% (95% CI, 55.5%−67.4%) provided environmental supports such as walking trails or tracks, maps of measured walking/jogging routes, bicycle racks, showers, and changing rooms. Only 35.4% (95% CI, 27.3%−38.9%) of hospital programs used signs to encourage employees to use the stairs. More than half of hospital wellness programs (54.9%; 95% CI, 48.8%−61.0%) provided organized individual or group PA programs for employees (other than use of exercise facility), 33.1% (95% CI, 27.3%-38.9%) provided PA tracking devices for free or at a discounted rate, and 22.6% (95% CI, 17.4%−27.7%) encouraged active transportation to and from work.
Table 3.
Employer-Reported Worksite Physical Activity Supports Among Hospitals Who Reported Any Wellness Activities or Programs During the Previous 12 Monthsa
| Strategy | Yes | 95.%CI | No | 95% CI | Do not Know | 95% CI |
|---|---|---|---|---|---|---|
| Physical activity programs | ||||||
| Offer programs to address physical activity/fitness/sedentary behavior for employees (n = 257) | 73.5 | 68.1–78.9 | 19.8 | 15.0–24.7 | 6.6 | 3.6–9.7 |
| Provide or subsidize physical fitness assessments, follow-up counseling, and exercise recommendations either on-site or through a community exercise facility (n = 257) | 35.8 | 29.9–41.7 | 56.0 | 50.0–62.2 | 8.2 | 4.8–11.5 |
| Provide free or subsidized lifestyle self-management programs that include advice on physical activity (n = 257) | 49.8 | 43.7–55.9 | 42.4 | 36.4–48.5 | 7.8 | 4.5–11.1 |
| Physical activity environment amenitites and supports | ||||||
| Provide an exercise facility onsite (n = 257) | 54.5 | 48.4–60.6 | 43.2 | 37.1–49.3 | 2.3 | 0.5–4.2 |
| Subsidize or discount the cost of on-site and/or offsite exercise facilities (0 = 257) | 60.3 | 54.3–66.3 | 35.8 | 29.9–41.7 | 3.9 | 1.5–6.3 |
| Provide environmental supports for physical activity or recreation such as walking trails or tracks, maps of measured walking/jogging routes, bicycle racks, shower, and changing room (n = 257) | 61.5 | 55.5–67.4 | 34.6 | 28.8–40.5 | 3.9 | 1.5–6.3 |
| Post signs at elevators, stairwell entrances/exits, and other key locations that encourage employees to use the stairs (n = 257) | 35.4 | 29.6–41.3 | 59.1 | 53.1–65.2 | 5.4 | 2.7–8.2 |
| Provide organized individual or group physical activity programs for employees (other than use of an exercise facility; n = 257) | 54.9 | 48.8–61.0 | 39.7 | 33.7–45.7 | 5.4 | 2.7–8.2 |
| Provide a pedometer or FITBIT or other physical activity tracking device for free or discounted rate to employees (n = 257) | 33.1 | 27.3–38.9 | 61.1 | 55.1–67.1 | 5.8 | 3.0–8.7 |
| Provide the option of using active work stations (n = 257) | 28.8 | 23.4–34.3 | 64.6 | 58.7–70.4 | 6.6 | 3.6–9.7 |
| Offer employees paid time to be physically active during work hours, including fitness breaks, walking meetings, or other options (n = 257) | 18.7 | 13.9–23.5 | 75.5 | 70.2–80.8 | 5.8 | 3.0–8.7 |
| Encourage active transportation to and from work by providing things such as bike parking, shower access, pretax contributions for public transportation or providing parallel benefits to those who bike, walk to work (n = 257) | 22.6 | 17.4–27.7 | 71.2 | 65.7–76.8 | 6.2 | 3.3–9.2 |
Abbreviation: 95% CI, 95% confidence interval.
Among hospitals that reported any wellness activities or programs in the previous 12 month, specific questions about physical activity supports were asked. Unweighted sample size, weighted percentage, and 95% CI.
Most hospital wellness programs included screenings for chronic diseases with prevalence of specific screening ranging from 65.9% (95% CI, 60.0%−71.7%) for obesity to 77.4% (95% CI, 72.2%−82.6%) for blood pressure (Table 4). Provision of informational materials for hypertension, cardiovascular disease, and obesity was reported in less than half of hospital wellness programs with prevalences ranging from 41.8% for cardiovascular disease to 45.4% for hypertension. One-on-one counseling for these conditions was available less often among wellness programs, with prevalences ranging from 23.3% for cardiovascular disease to 33.3% for diabetes/prediabetes. Most hospital wellness programs offered tobacco control supports. Regarding cessation support, 67.1% (95% CI, 61.2%−72.9%) offered tobacco cessation programs, 57.1% (95% CI, 51.0%-63.3%) referred tobacco users to a tobacco quit line, and 58.3% (95% CI, 52.2%−64.4%) provided free or subsidized tobacco cessation counseling. Regarding tobacco polices, 83.7% (95% CI, 79.2%−88.3%) had a written policy to restrict all tobacco use and 79.4% (95% CI, 74.4%−84.4%) actively enforced a written policy banning tobacco use. Less than half of hospital programs (47.2%; 95% CI, 41.0%−53.4%) offered lactation support and only a quarter (25.0%; 95% CI, 19.6%−30.4%) offered healthy sleep programs. However, most programs (62.7%; 95% CI, 56.7%−68.7%) included stress management.
Table 4.
Employee-Reported Workplace Health and Wellness Supports for Chronic Disease Prevention and Management Among Hospitals Who Reported Any Wellness Activities or Programs During the Previous 12 Months.a
| Strategy | Yes | 95% CI | No | 95% CI | Do not Know | 95% CI |
|---|---|---|---|---|---|---|
| Chronic disease health screenings | ||||||
| Blood pressure screening (n = 252) | 77.4 | 72.2–82.6 | 17.1 | 12.4–21.7 | 5.6 | 2.7–8.4 |
| Cholesterol screening (n = 252) | 66.7 | 60.8–72.5 | 26.6 | 21.1–32.1 | 6.7 | 3.6–9.8 |
| Diabetes/prediabetes screening (n = 252) | 67.9 | 62.1–73.6 | 25.8 | 20.4–31.2 | 6.3 | 3.3–9.4 |
| Obesity screening (n = 252) | 65.9 | 60.0–71.7 | 27.0 | 21.5–32.5 | 7.1 | 4.0–10.3 |
| Disease management and awareness | ||||||
| Cardiovascular disease informational materials (n = 252) | 41.8 | 35.6–47.9 | 42.2 | 36.0–48.3 | 16.1 | 11.5–20.6 |
| Cardiovascular disease seminars and workshops (n = 252) | 26.5 | 21.0–32.0 | 57.4 | 51.3–63.6 | 16.1 | 11.5–20.6 |
| Cardiovascular disease one-on-one counseling (n = 252) | 23.3 | 18.0–28.6 | 60.6 | 54.6–66.7 | 16.1 | 11.5–20.6 |
| Diabetes/prediabetes informational materials (n = 252) | 44.2 | 38.0–50.4 | 41.4 | 35.2–47.5 | 14.5 | 10.1–18.8 |
| Diabetes/prediabetes seminars and workshops (n = 252) | 36.1 | 30.2–42.1 | 49.4 | 43.2–55.6 | 14.5 | 10.1–18.8 |
| Diabetes/prediabetes one-on-one counseling (n = 252) | 33.3 | 24.5–39.2 | 52.2 | 46.0–58.4 | 14.5 | 10.1–18.8 |
| Hypertension informational materials (n = 252) | 45.4 | 39.2–51.6 | 37.3 | 31.3–43.7 | 17.3 | 12.6–22.0 |
| Hypertension seminars and workshops (n = 252) | 24.1 | 18.8–29.4 | 58.6 | 52.5–64.8 | 17.3 | 12.6–22.0 |
| Hypertension one-on-one counseling (n = 252) | 27.7 | 22.1–33.3 | 55.0 | 48.8–61.2 | 17.3 | 12.6–22.0 |
| Obesity informational materials (n = 252) | 44.6 | 38.4–50.8 | 37.3 | 31.3–43.4 | 18.1 | 13.3–22.9 |
| Obesity seminars and workshops (n = 252) | 26.9 | 21.4–32.4 | 55.0 | 48.8–61.2 | 18.1 | 13.3–22.9 |
| Obesity one-on-one counseling (n = 252) | 24.9 | 19.5–30.3 | 57.0 | 50.9–63.2 | 18.1 | 13.3–22.9 |
| Tobacco control | ||||||
| Offer tobacco cessation programs (n = 252) | 67.1 | 61.2–72.9 | 23.4 | 18.2–28.7 | 9.5 | 5.9–13.2 |
| Refer tobacco users to tobacco quitline (n = 252) | 57.1 | 51.0–63.3 | 25.0 | 19.6–30.4 | 17.9 | 13.1–22.6 |
| Provide free or subsidized tobacco cessation counseling (n = 252) | 58.3 | 52.2–64.4 | 25.0 | 19.6–30.4 | 16.7 | 12.1–21.3 |
| Have a written policy to restrict all tobacco use (n = 252) | 83.7 | 79.2–88.3 | 6.0 | 3.0–8.9 | 10.3 | 6.6–14.1 |
| Actively enforce a written policy banning tobacco use (n = 252) | 79.4 | 74.4–84.4 | 9.1 | 5.6–12.7 | 11.5 | 7.6–15.5 |
| General wellness and health promotion | ||||||
| Lactation support programs (n = 252) | 47.2 | 41.0–53.4 | 35.3 | 29.4–41.2 | 17.5 | 12.8–22.2 |
| Stress management programs (n = 252) | 62.7 | 56.7–68.7 | 26.6 | 21.1–32.1 | 10.7 | 6.9–14.5 |
| Healthy sleep programs (n = 252) | 25.0 | 19.6–30.4 | 54.4 | 48.2–60.5 | 20.6 | 15.6–25.6 |
Abbreviation: 95% CI, 95% confidence interval.
Unweighted sample size, weighted percentage, and 95% CI.
Compared to hospitals with <500 employees, hospitals with 500 or more employees were more likely to report having employee nutrition programs (76.4% vs 62.6%, P = .02), employee PA programs (79.7% vs 67.9%, P = .03), tobacco cessation programs (75.8% vs 59.1%, P < .01), lactation support programs (62.5% vs 33.3%, P < .0001), or healthy sleep programs (30.8% vs 19.7%, P = .04; Figure 1). However, the prevalence of having at least 1 chronic disease screening program did not differ according to hospital size.
Figure 1.
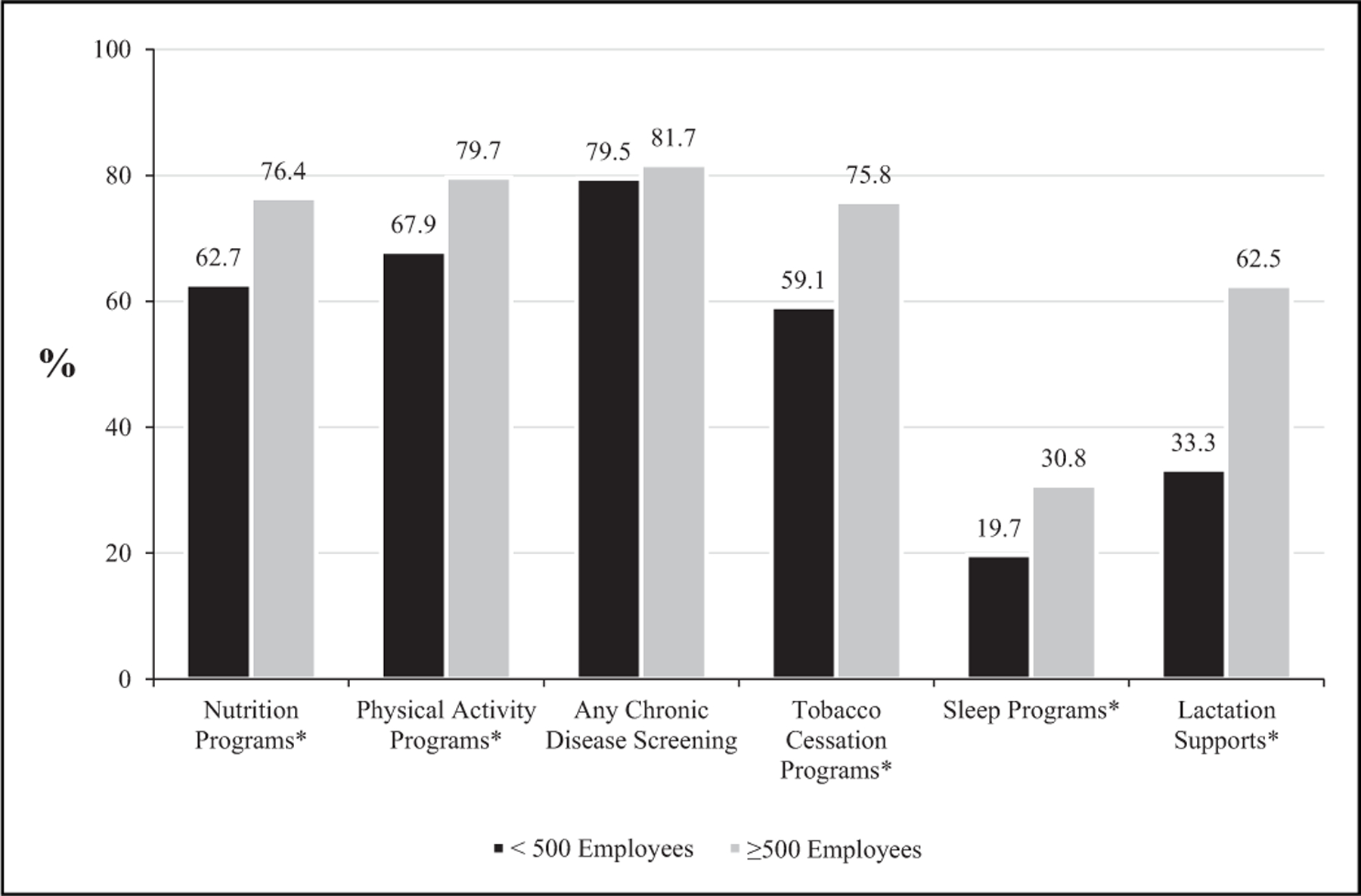
Prevalence of nutrition, physical activity, chronic disease screening, tobacco cessation, sleep, and lactation support programs among US hospitals according to number of hospital employees. Chi-square P-value < .05 comparing prevalence of support according to number of hospital employees.
Discussion
The results of this study suggest that most hospitals in the United States offer health promotion and or wellness programs. To our knowledge, this is the most recent national survey assessing wellness policies and practices for chronic disease prevention in US hospitals. Our study augments the evidence base by providing national estimates across several areas not previously reported including, but not limited to, policy and environment strategies regarding lactation support, healthy sleep, and healthy meetings food policy. Although our results are purely descriptive in nature, the findings are important in describing the current state of hospital wellness practices and programs, tracking their prevalence over time, and highlighting where improvement needs to occur.
Compared to practices in other industry sectors, hospitals support health promotion practices to a greater degree. For example, 35.7% of hospitals offered comprehensive workplace health promotion programs compared to only 11.8% of all US worksites.17 These findings may be partially due to the health-driven mission of hospitals and the ability of larger employers to support health promotion activities. However, we also found that smaller hospitals were less likely to report many types of wellness supports compared to larger hospitals, which coincides with data reported for employers overall.13,17 Conceivably, the efforts and strategies hospitals develop for employee health promotion programs can be leveraged to support similar programs for local communities. Hospitals should increasingly engage in such efforts because they further the larger population health agenda.18
Our study found that 59.9% of hospital programs offered weight management for employees. This is lower than the 77% of hospitals that reported offering a weight loss program in the 2015 AHA member survey.15 The discrepancy with our finding may be related to the difference in terminologies and methodologies used by the 2 surveys. However, many of our results are comparable to those in the 2015 AHA member survey where questions are similarly phrased. Therefore, differences in results for weight management programs likely reflect true changes in practice. Based on our sample, there remains room for improvement in the provision of comprehensive weight management programs for employees.
Hospitals engaged in a variety of environment supports for healthy food and beverage options. For example, 57.2% of hospital wellness programs featured a healthy meeting policy to ensure availability of healthy options when foods or beverages are served at meetings and/or events. Most hospitals with wellness programs had on-site vending machines and cafeterias or snack bars for employees. Only 40% of these hospitals had a written policy to require healthier choices among foods and beverages offered or had a policy or written communication that required ≥50% of the available food and beverage choices in cafeterias or vending machines to be healthy. Finally, we found that only 48.6% of hospitals that offered food also provided nutritional information, lower than the 68% reported by the 2015 AHA survey.15 Efforts to improve healthier food and drink access in hospitals should include adapting nutrition and environmental standards such as those in the Food Service Guidelines for Federal Facilities.19 Hospitals could support sustainable food system approaches that lead to accessing healthier foods.20 Such efforts align with community health benefit investments that are relevant to tax exemptions for nonprofit hospitals.21 Indeed, despite the availability of such options to improve community health, few hospitals have engaged in such efforts.22
We found that most hospital wellness programs offered programs to address PA, but only 59.8% provided or subsidized self-management programs that included PA. Because self-management strategies may be important in improving outcomes in some chronic illnesses,23,24 increasing the availability of self-management supports in hospital programs is critical. Our estimate that 54.5% of hospital wellness programs offering an exercise facility is similar to the 57% reported in the 2015 AHA survey.15 Our study is unique in documenting specific information on environment supports and amenities for PA. For example, only 35.4% of hospital programs used signs to promote use of stairwells and 61.5% provided or supported efforts such as walking trails, bicycle racks, and shower rooms. Providing access to facilities and environments that support PA in hospitals may be particularly important because hospital employees who work night shifts may be less likely to engage in regular muscle-strengthening PA and may have fewer opportunities for quality leisure-time PA.25,26
Most hospital programs offered chronic disease health screenings, but a smaller proportion offered educational materials, seminars, or one-on-one counseling for cardiovascular disease, diabetes, or hypertension. By comparison, most hospitals offered tobacco cessation programs or services. Our finding that 62.7% of hospital wellness programs offered stress management programs is lower than the 77% reported by the 2015 AHA survey.15
Our study provides new information in that only 47.2% and 25.0% of hospital wellness programs offer lactation support or healthy sleep programs, respectively. These 2 supports are particularly relevant to hospitals and this information highlights the opportunity for more hospitals to provide employees with the appropriate resources for lactation and healthy sleep. The Surgeon General’s Call to Action to Support Breastfeeding recommended that employers establish and maintain lactation support programs for employees.27 As birthing facilities, hospitals are in a unique position to model lactation support for employees. Hospitals can use this unique position to galvanize other employers by demonstrating the benefits of lactation support for maternal and child health, and employee retention. Finally, the shift-work nature of hospital work schedules and potential patient health consequences of medical errors makes healthy sleep programs especially important in hospital worksites.28,29
Overall, 37.5% of WHA survey respondents reported that the most common barrier to health promotion programs was lack of employee interest.17 These results show that employee viewpoints should be used when developing new programs.
Additional research is needed to determine which programs and supports, including those addressing lactation and healthy sleep, should be offered consistently in health promotion efforts. Furthermore, very little is known about the utilization and effectiveness of these programs and supports. Finally, research efforts should investigate how to effectively combine self-management strategies with wellness programs and other supports.
There are several limitations to our study. First, WHA had only a 17.3% response rate among hospitals. As such selection bias may limit the representativeness of our results. Second, questions regarding nutrition, PA, tobacco control, and other this study only examined the presence of programs and supports but did not examine the quality of implementation, whether employees participated in programs or whether the programs and supports improved health outcomes or reduced expenditures.
In conclusion, we find that almost one-fifth of hospitals do not offer wellness programs and, among those that have wellness programs, most offer supports for nutrition, PA, and tobacco control. However, less than half of hospital wellness programs provided lactation support and only a quarter provided healthy sleep programs. Hospitals have the opportunity to improve employee health by implementing environment supports for healthier choices, such as increasing the proportion of healthier food and beverage choices or using signage to encourage use of stairwells or walking trails. Hospitals are chronic disease prevention areas were only asked of worksites that reported having a wellness program. It is possible that some of these supports were present among hospitals that did not report wellness programs, particularly food supports such as cafeterias and vending machines. Third, although efforts were made to have the most knowledgeable employer staff members answer our survey, there remained a proportion of survey items for which respondents did not know the answers. This may threaten the external validity of our study. Finally, often large employers in their communities, and as worksites with health-driven missions, they have the opportunity to model effective health promotion strategies.16 Future health promotion efforts should leverage hospitals’ unique position in this regard and by aligning such work to further population health.
So What?
What is already known on this topic?
Hospitals are prominent and important employers that engage in health promotion. However, many hospital employees report lack of supports for health and active living while at work.
What does this article add?
This article provides an update to the prevalence of current health and wellness practices and programs in a antional sample of hospitals. Furthermore, this article highlights new areas for focusing wellness strategies including healthy meeting policies, self management programs, lactation support, stress management and healthy sleep.
What are the implications for health promotion practice?
Future health promotion efforts should leverage hospitals’ unique position and align wellness strategies to further population health.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.American Hospital Association. Fast Facts on U.S. Hospitals; 2019. https://www.aha.org/statistics/fast-facts-us-hospitals. Accessed December 2019.
- 2.Current Population Survey, Bureau of Labor Statistics. Table 7: Most Recent Industry-Specific Employment Peak and Trough, and Changes From Peak and Trough to Current Employment, Seasonally Adjusted (in Thousands) https://www.bls.gov/ces/#tables. Accessed December 2019.
- 3.Goetzel R, Ozminkowski R. The health and cost benefits of worksite health-promotion programs. Annu Rev Public Health 2008; 29:303–323. [DOI] [PubMed] [Google Scholar]
- 4.Baicker K, Cutler D, Song Z. Workplace wellness programs can generate savings. Health Aff 2010:29(2):304–311. [DOI] [PubMed] [Google Scholar]
- 5.Goetzel RZ, Henke RM, Tabrizi M, et al. Do workplace health promotion (wellness) programs work? J Occup Environ Med 2014;56(9):927–934. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Healthy Hospital Practice to Practice Series (P2P) Issue 1: Improving Hospital Food and Beverage Environments https://www.cdc.gov/obesity/downloads/p2p/p2p_food_issue1.pdf. Accessed December 2019.
- 7.Moran A, Krepp EM, Curtis CJ, Lederer A. An intervention to increase availability of healthy foods and beverages in New York City hospitals: the Healthy Hospital Food Initiative, 2010–2014. Prev Chronic Dis 2016;13:E77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dodson E, Hipp J, Gao M, Tabak RG, Yang L, Brownson RC. The impact of worksite supports for healthy eating on dietary behaviors. J Occup Environ Med 2017:58(8): e278–e293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davy B, You W, Almeida F, et al. Impact of individual and worksite environmental factors on water and sugar-sweetened beverage consumption among overweight employees. Prev Chronic Dis 2014:11: E71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adlakha D, Hipp A, Marx C, et al. Home and workplace built environment supports for physical activity. Am J Prev Med 2015; 48(1):104–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rothstein M, Harrell H. Health risk reduction programs in employer-sponsored health plans: part 1—efficacy. J Occup Environ Med 2009;51(8):943–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Payne J, Cluff L, Lang J, Matson-Koffman D, Morgan-Lopez A. Elements of a workplace culture of health, perceived organizational support for health, and lifestyle risk. Am J Health Prom 2018;32(7):1555–1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Onufrak S, Watson K, Kimmons J, et al. Worksite food and physical activity environments and wellness supports reported by employed adults in the United States, 2013. Am J Health Promotion 2018:32(1):96–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Linnan L, Bowling M, Childress J, et al. Results of the 2004 National Worksite Health Promotion survey. Am J Public Health 2008;98(8):1503–1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Health Research & Educational Trust. Health and Wellness Programs for Hospital Employees: Results From a 2015 American Hospital Association Survey Chicago, IL: Health Research & Educational Trust; 2016. http://www.hpoe.org/Reports-HPOE/2016/2016-Health-and-Wellness-Brief-FINAL-10-12-16.pdf. Accessed December 2019. [Google Scholar]
- 16.Begun JW, Potthoff S. Moving upstream in U.S. hospital care toward investments in population health. J Healthcare Manag 2017;62(5):343–353. [DOI] [PubMed] [Google Scholar]
- 17.Linnan LA, Cluff L, Lang JE, Penne M, Leff MS. Results of the workplace health in America survey. Am J Health Prom 2019; 33(5):652–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Collaborative on Childhood Obesity Research. Evaluating Clinical-Community Engagement to Address Childhood Obesity: Implications and Recommendations for the Field 2016. https://www.nccor.org/downloads/2016/11/nccor-community-engagement-workshop-summary-v7.pdf. Accessed December 2019.
- 19.Food Service Guidelines Federal Workgroup. Food Service Guide lines for Federal Facilities Washington, DC: U.S. Department of Health and Human Services; 2017. https://www.cdc.gov/obesity/downloads/guidelines_for_federal_concessions_and_vending_operations.pdf. Accessed December 2019. [Google Scholar]
- 20.Wisconsin Comprehensive Cancer Control Program. Farm to Hospital Community of Practice https://wicancer.org/healthyhospitals/farm-to-hospital-community-of-practice/. Accessed December 2019.
- 21.Internal Revenue Service. New Requirements for 501(c)(3) Hospitals Under the Affordable Care Act https://www.irs.gov/charities-non-profits/charitable-organizations/new-requirements-for-501c3-hospitals-under-the-affordable-care-act. Accessed December 2019.
- 22.Young GA, Flaherty S, Zepeda ED, Singh SR, Rosen Cramer G. Community benefit spending by tax-exempt hospitals changed little after ACA. Health Aff 2018;37(1):121–124. [DOI] [PubMed] [Google Scholar]
- 23.Shieh C, Knisely MR, Clark D, Carpenter JS. Self-weighing in weight management interventions: a systematic review of literature. Obes Res Clin Pract 2016;10(5):493–519. [DOI] [PubMed] [Google Scholar]
- 24.Vas A, Devi ES, Vidyasagar S, et al. Effectiveness of self-management programmes in diabetes management: a systematic review. Int J Nurs Pract 2017;23(5). doi: 10.1111/ijn.12571. [DOI] [PubMed] [Google Scholar]
- 25.Chin DL, Nam S, Lee SJ. Occupational factors associated with obesity and leisure-time physical activity among nurses: a cross sectional study. Int J Nursing Stud 2016; 57: 60–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Atkinson G, Davenne D. Relationships between sleep, physical activity and human health. Physiol Behav 2007;90(2–3):229–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.U.S. Department of Health and Human Services. The Surgeon General’s Call to Action to Support Breastfeeding Washington, DC: U.S. Department of Health and Human Services, Office of the Surgeon General; 2011. [Google Scholar]
- 28.Starmer AJ, Spector ND, Srivastava R, et al. Changes in medical errors after implementation of a handoff program. NEJM 2014; 371(19):1803–1812. [DOI] [PubMed] [Google Scholar]
- 29.Richter K, Acker J, Adam S, Niklewski G. Prevention of fatigue and insomnia in shift workers—a review of non-pharmacological measures. EPMA J 2016;7:16. doi: 10.1186/s13167-016-0064-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


