Abstract
Up to 14% of veterans engage in nonsuicidal self-injury (NSSI) in their lifetime and this behavior is a relatively strong predictor of suicidal behavior compared to other identified risk factors. Further, NSSI is a clinically relevant behavior in its own right; it is associated with more severe psychopathology as well as bodily harm that sometimes requires medical intervention. Therefore, a better understanding of NSSI may help inform suicide prevention efforts as well as mental healthcare strategies for veterans. Anger may be relevant to understanding NSSI in veterans. Over 60% of veterans report difficulties managing anger and this emotion is strongly associated with engagement in NSSI. However, no research has explored the extent to which anger is present prior to NSSI or whether anger is associated with specific NSSI methods or functions in veterans. The purpose of this study was to explore whether anger was associated with engagement in specific NSSI methods, and whether anger uniquely predicted any functions of NSSI while controlling for the presence of other basic negative emotions (fear and sadness). An existing dataset of 61 veterans who reported engaging in NSSI in the past year was analyzed. Results indicated anger was the most common emotional antecedent to NSSI. Further, anger was associated with several methods of NSSI including burning oneself with a cigarette, carving pictures, designs or other marks into skin, sticking sharp objects into skin, severely scratching oneself, head banging, punching oneself, and punching walls or objects. Finally, when controlling for the presence of other negative emotions, anger was associated with engaging in NSSI to relieve tension, stop feeling numb, communicate with others, feel alive, get help from others, and prove to oneself how bad things are. These results highlight the importance of assessing and treating dysregulated anger in veterans who engage in self-harming behavior.
Keywords: Anger, nonsuicidal self-injury, veterans, functional analysis
Nonsuicidal self-injury (NSSI) is described as the intentional infliction of damage to one’s body tissue without suicidal intent (American Psychiatric Association, 2013; Klonsky, 2007). This behavior can take many forms including cutting or burning skin, punching oneself, and punching walls/objects. NSSI has received increasing attention, in part due to its association with undesirable outcomes including heightened negative affect, severe injury, and even death (Klonsky, 2009). Additionally, NSSI is a relatively strong predictor of suicidal behavior compared to other identified risk factors. In fact, it is one of the strongest longitudinal predictors of suicide attempts identified to date (Franklin et al., 2017; Ribeiro et al., 2016). Further, NSSI is a clinically relevant phenomenon in its own right; it is associated with more severe clinical presentations, clinical distress, and injuries sometimes require medical intervention (Doshi et al., 2005; Selby et al., 2012).
Originally described in the context of borderline personality disorder, more recent work suggests NSSI is a transdiagnostic phenomenon that occurs across diagnostic boundaries and in individuals who do not meet criteria for a psychiatric diagnosis (Bentley et al., 2014). Further, research has documented the occurrence of this behavior in understudied populations, including veterans, with one study reporting 14% of veterans have a lifetime history of NSSI (Kimbrel et al., 2015). In a study of veterans with PTSD 50% reported current engagement in NSSI (Calhoun et al., 2017). In another study Kimbrel et al. (2018) found 82% of treatment-seeking veterans with PTSD reported a lifetime history of NSSI and 64% engaged in NSSI in the past two weeks. Similar to the general population, NSSI is a relatively strong predictor of suicidal ideation and suicide attempts among veterans (Kimbrel et al., 2016; Villatte et al., 2015) and in one study NSSI was also a predictor of violence towards others (Calhoun et al., 2017). Given rising concerns regarding suicide in the veteran population (e.g., Hoge, 2019) and the association of NSSI with risk for injury and suicide, this behavior represents a targetable risk factor to prevent more dangerous behavior in veterans. Thus, there is a clear need to better understand NSSI in this population in order to develop efficient interventions that reduce risk for suicide and aggression.
One way to better understand NSSI is through the lens of functional analysis. This framework allows for an investigation into the antecedents and consequences associated with a given behavior (Barlow & Nock, 2009; Bentley et al., 2014). Understanding antecedents helps establish situations in which a behavior is likely to occur. On the other hand, examining a behavior’s consequences can lend insight into the reasons an ineffective or dangerous behavior is repeated (e.g., Nock & Prinstein, 2005). This understanding then allows for potent, targeted intervention strategies (Bailey & Burch, 2017; Bentley et al., 2014).
The emotions that precede NSSI are of particular interest because one of the most commonly cited functions of NSSI is to reduce emotional intensity (Taylor et al., 2018). Indeed, research often describes NSSI as functioning to “reduce intense negative emotions” (Nock & Prinstein, 2005). The term “negative emotions” is broad, and can include different discrete emotions depending on the model of emotions one refers to. In this paper, we will focus on the seminal model of basic emotions proposed by Ekman (1992). Ekman posits there are six basic emotions that are neurobiologically derived and consistent across cultures, although this is a point of some debate (e.g., Barrett et al., 2011): happiness, surprise, fear, sadness, anger, and disgust. Given the frequent association of NSSI with psychiatric disorders including mood, anxiety, trauma-related, and obsessive-compulsive disorders (for a meta-analysis see Bentley et al., 2014), which are typically characterized by dysregulated sadness, fear, and anger, those emotions will be the focus of the current study.
There is some evidence, in civilian populations, to suggest discrete emotions may have differential impact on NSSI behavior (Nock et al., 2009). For example, a systematic review indicated thoughts of NSSI tended to occur in relation to sadness and anxiety, whereas the behavior itself more often occurred in response to anger (Rodríguez-Blanco et al., 2018). In one study, 39.9% of participants reported anger at themselves was an antecedent to NSSI and 22.4% reported anger at someone else preceded NSSI (Muehlenkamp et al., 2013). Additionally, Kleiman et al., (2015) reported participants who engaged in NSSI had higher levels of trait anger than those who did not and trait aggression differentiated individuals who engaged in hitting NSSI from those who did not. Thus, not only does anger appear associated with engagement in NSSI but also with specific forms of NSSI.
Anger may be particularly relevant to understanding NSSI in veteran populations. In a national survey 61.2% of US veterans reported difficulties controlling anger (Sippel et al., 2016). Further, anger is a risk factor for suicide among veterans and is also a symptom of posttraumatic stress disorder (PTSD), which is more common in veterans compared to the general population (Smith et al., 2016). Anger has been consistently associated with suicidal ideation and suicide attempts in veterans (Dobscha et al., 2014; Kachadourian et al., 2018; Novaco et al., 2012; Wilks et al., 2019). Changes in anger have also been found to mediate the relationship between changes in PTSD symptom severity and suicidal ideation (Dillon et al., 2020). Furthermore, anger is strongly associated with NSSI urges and behaviors among veterans with NSSI disorder (Dillon et al., under review). Taken together, this research suggests anger often plays an important role in engaging in dangerous behavior among veterans. However, to the best of our knowledge, no research has examined the extent to which anger is present prior to NSSI in comparison to other emotions. Additionally, no research has examined whether anger is associated with engagement in specific methods of NSSI in veterans.
Beyond antecedents, it is important to understand the function NSSI serves in order to understand how it is being reinforced and develop intervention strategies. While the most commonly noted function of NSSI is to reduce intrapersonal distress, other noted functions include engaging in NSSI to increase desired internal states (e.g., generating positive feelings or stimulation), to escape undesirable social situations, or to elicit a desirable social situation (e.g., support from others; Bentley et al., 2014; Nock & Prinstein, 2005). Intervention strategies differ depending on the function NSSI serves an individual. For example, if an individual engages in NSSI to reduce intense anger, interventions might focus on teaching the patient other skills to manage the experience of anger. On the other hand, if an individual engages in NSSI as an attempt to resolve an interpersonal disagreement, different skills may be necessary. Given the hypothesized importance of anger in NSSI, understanding whether anger is uniquely associated with certain functions of NSSI in veterans will provide information needed to create targeted interventions. Currently, to the best of our knowledge, there is no work exploring the functions NSSI serves in the veteran population or exploring whether anger is differentially associated with any functions of NSSI.
Taken together, there is a clear need to better understand the role of anger in NSSI behavior in veterans. Therefore, the purpose of this study was to 1) explore the extent to which anger was present prior to engaging in NSSI in a veteran sample, 2) explore whether the presence of anger prior to NSSI was associated with engagement in specific methods of NSSI, and 3) to explore whether anger antecedent to NSSI uniquely predicted any functions of NSSI when controlling for the presence of other basic negative emotions (i.e., fear and sadness). For all analyses, we compared anger with sadness and fear in order examine the relative importance of these three basic emotions on NSSI behaviors and functions in veterans.
Method
Participants
A total of 124 veterans were recruited to participate in a one-year longitudinal study focused on examining the impact of NSSI on veterans’ functional outcomes. The current study focused solely on the baseline data from the larger study (for additional description of the parent study see (Mann et al., 2020; Patel et al., in press). Participants were recruited via clinician referrals, mailings targeting veterans who had sought care in VA PTSD clinics, and phone calls and letters to veterans who had agreed to be listed in research recruitment databases. The study recruited veterans with NSSI disorder, with a history of NSSI who did not meet criteria for NSSI disorder, and without a history of NSSI to compare longitudinal outcomes between these three groups. NSSI disorder is currently listed as a “disorder under consideration” in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) and thus is not currently a diagnosable condition. Proposed diagnostic criteria include: (1) engaging in NSSI at least five days in the past year, (2) engaging in NSSI to relieve a negative feeling or cognitive state, resolve interpersonal difficulty, or induce a positive feeding, (3) NSSI is preceded by interpersonal difficulties or negative emotional states, preoccupation with NSSI precedes NSSI, or frequent urges/thought regarding NSSI are present, (4) the NSSI behavior is not socially sanctioned or restricted to nail biting or scab picking, (5) NSSI associated with significant distress or impairment, (6) NSSI not better explained by another condition, intoxication, delirium, or psychosis (American Psychiatric Association, 2013). These proposed criteria were used to identify veterans with and without NSSI disorder in this study. Potential participants were first screened by telephone to ensure they met basic eligibility criteria, and final eligibility was determined at the time of the baseline assessment. To be eligible, participants had to be veterans who were at least 18 years of age. Participants were excluded if they met criteria for a lifetime diagnosis of bipolar disorder or psychotic spectrum disorder, or had imminent risk for suicide or homicide warranting immediate intervention.
The current analyses were restricted to participants who endorsed engaging in NSSI at least once in the past year at their baseline assessment visit, yielding a sample size of n = 61 veterans. Forty-one (67.2%) met criteria for current NSSI disorder. Participants in the current analyses reported a mean age of 47.44 (SD = 13.03). Approximately 26% (n = 16) of the sample was female. Regarding racial background, 58.3% identified as African American, 38.3% as White, and 3.3% as more than one race. One participant (1.6%) identified as Hispanic. On average, participants completed 13.63 (SD = 2.98) years of education. Thirty-six participants (59%) also met criteria for borderline personality disorder (BPD) and 54 (88.5%) had current PTSD.
Procedures
The Durham VA Internal Review Board and Research and Development Committee approved all study procedures. After giving written informed consent, participants completed a battery of clinical interviews and self-report measures. Participants received $100 for completing the baseline assessment.
Measures
The Clinician Administered Nonsuicidal Self-injury Disorder Index (CANDI; Gratz et al., 2015) was used to assess NSSI Disorder in the past year. This interview also assesses form, frequency, functions, and antecedents of NSSI. The CANDI exhibits good interrater reliability (κ = .83) and adequate internal consistency (α = .71; Gratz et al., 2015). The Structured Clinical Interview for DSM-5 was administered to assess for other psychiatric disorders (SCID-5; First, Williams, Karg, & Spitzer, 2016), except BPD, which was assessed with the Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV; Zanarini, Frankenburg, Sickel, & Yong, 1996). The SCID-5 has demonstrated excellent internal consistency and test-retest reliability in prior research (Shankman et al., 2018). The DIPD-IV has demonstrated adequate test-retest and inter-rater reliability (Zanarini et al., 2000).
In the current study, all interviews were conducted by masters-level clinicians who were required to complete extensive training procedures prior to conducting interviews independently, including studying interview manuals, watching instructional training videos, rating videotaped interviews, and participating in ongoing weekly supervision. Because NSSID was the focus of the study and is listed as condition for further study in DSM-5, each CANDI was reviewed and discussed in diagnostic review groups led by a licensed clinical psychologist until diagnostic consensus was reached (Dillon et al., in press).
The CANDI asks participants to indicate the functions of their self-harm by assigning a percentage value (0–100%) to 17 types of reasons that people engage in self-harm (e.g., to relieve tension, to punish yourself, to gain a sense of control). Participants are then asked to indicate the percentage of the time (0–100%) that they have experienced 15 different emotions or thoughts prior to engaging in self-injury (e.g., angry, frustrated, irritated, or enraged; tense or agitated; ashamed; like a failure or inferior). The CANDI inquires about these topics with regard to NSSI in the past year and lifetime NSSI; data regarding the past year were used in this study. Because every study interviewer reviewed every case in diagnostic consensus group, we were not able to calculate inter-rater reliability for this measure.
The Deliberate Self-Harm Inventory (DSHI; Gratz, 2001) was administered immediately prior to the CANDI and was used to assess forms and frequency of deliberate self-harm in the past year. The DSHI asks about presence (yes/no) and frequency of 17 different types of intentional self-harm in the past year (e.g., cutting, burning, carving, biting, bone-breaking). The DSHI exhibits high internal consistency (α = .82) and adequate test-retest reliability (φ = .68, p < .001; Gratz, 2001). Although only individual items were examined, internal consistency of the composite DSHI measure in the current sample was adequate (α = .74).
Data analytic plan
Analyses were conducted in SPSS 26.0 and R (version 4.0.3), using the sample of participants who reported engaging in any NSSI in the past year.
In order to explore the relationship of different basic negative emotions, NSSI methods, and functions of NSSI, we used the following CANDI emotion-related variables: anger (“anger, frustrated, irritated, or enraged”), sad (“sad, depressed, or down”), and fear (“fearful, anxious, afraid, or panicked”). First, descriptive statistics were used to describe the frequency with which each emotion was present prior to engaging in NSSI.
Next, we explored the relationships between anger antecedent to NSSI, engagement in different NSSI methods, and different functions of NSSI. The anger, NSSI methods, and NSSI function variables were non-normally distributed (see Table 1). The nature of these distributions and regression diagnostics was distinct for each variable, meaning no one parametric distribution was appropriate to fit for each item.
Table 1.
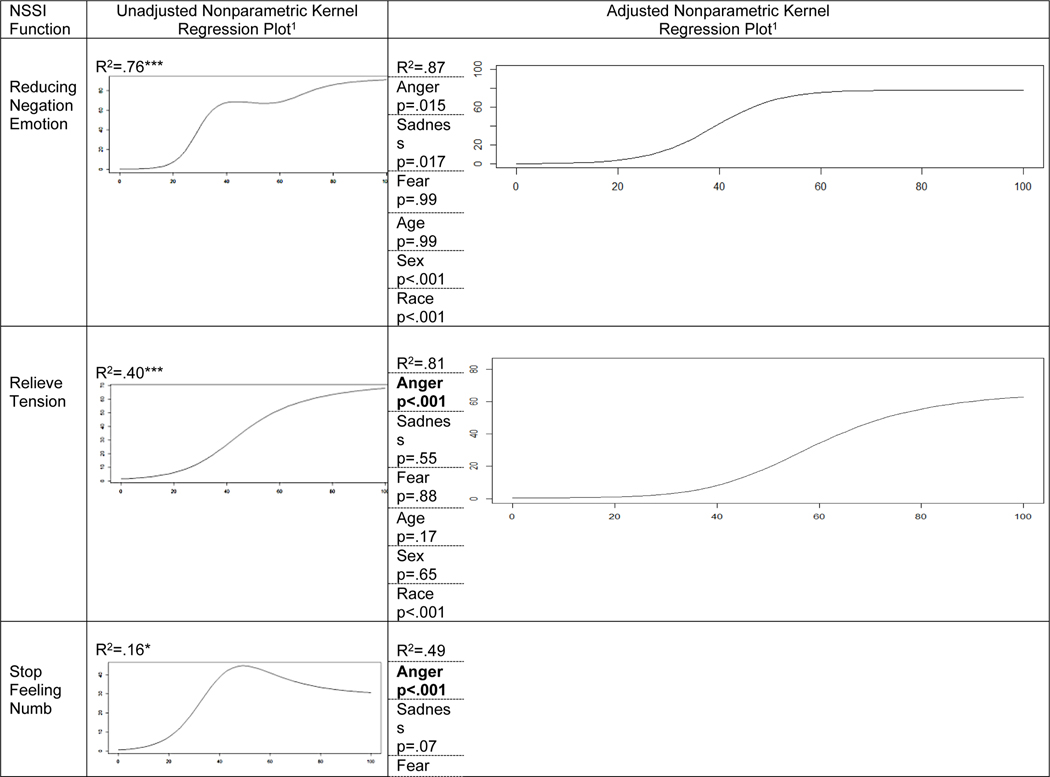
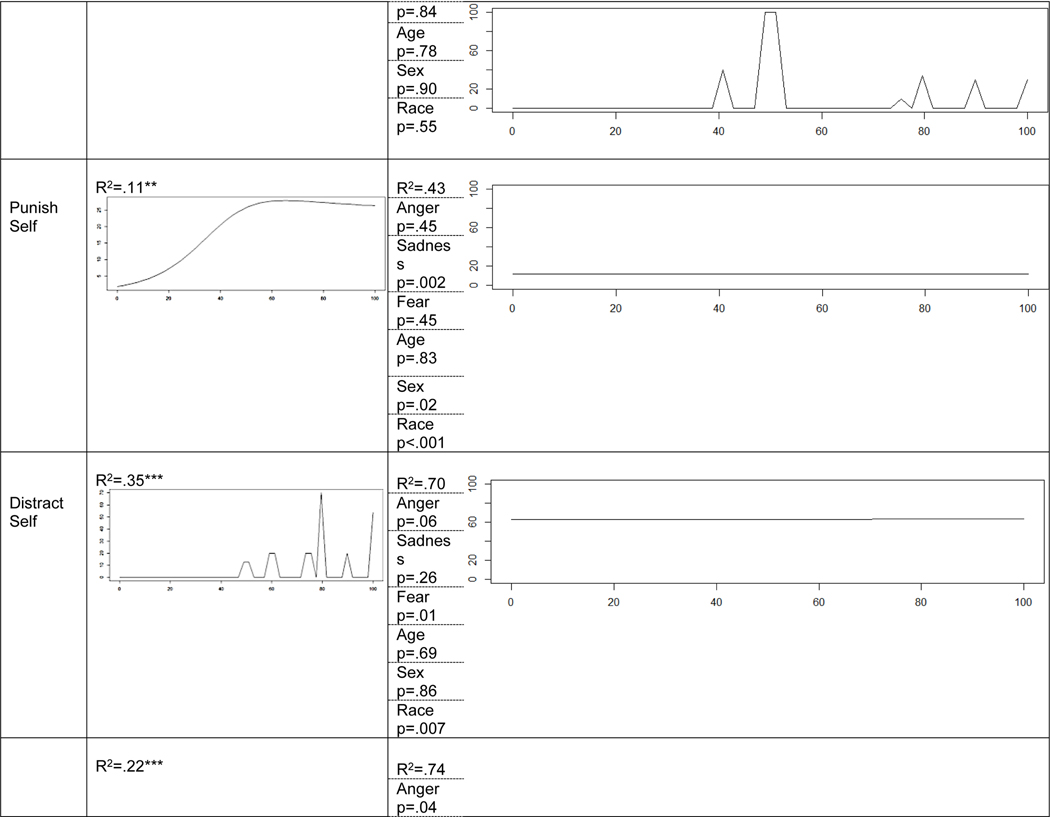
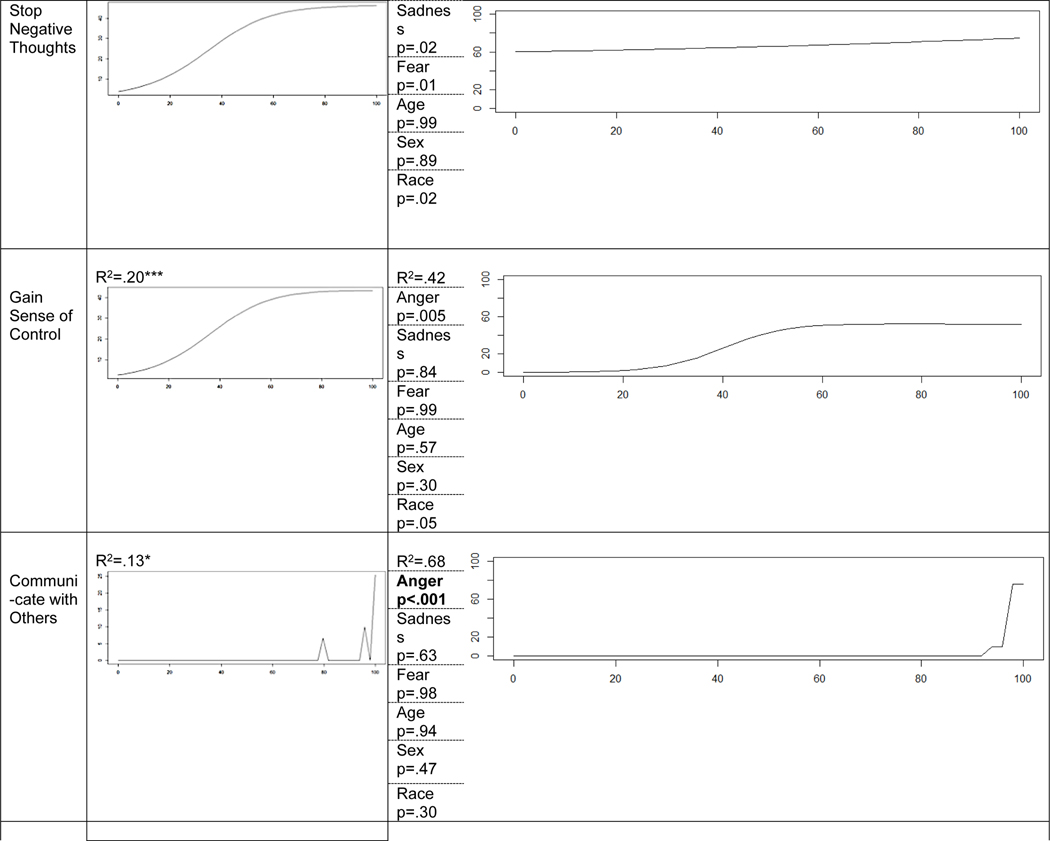
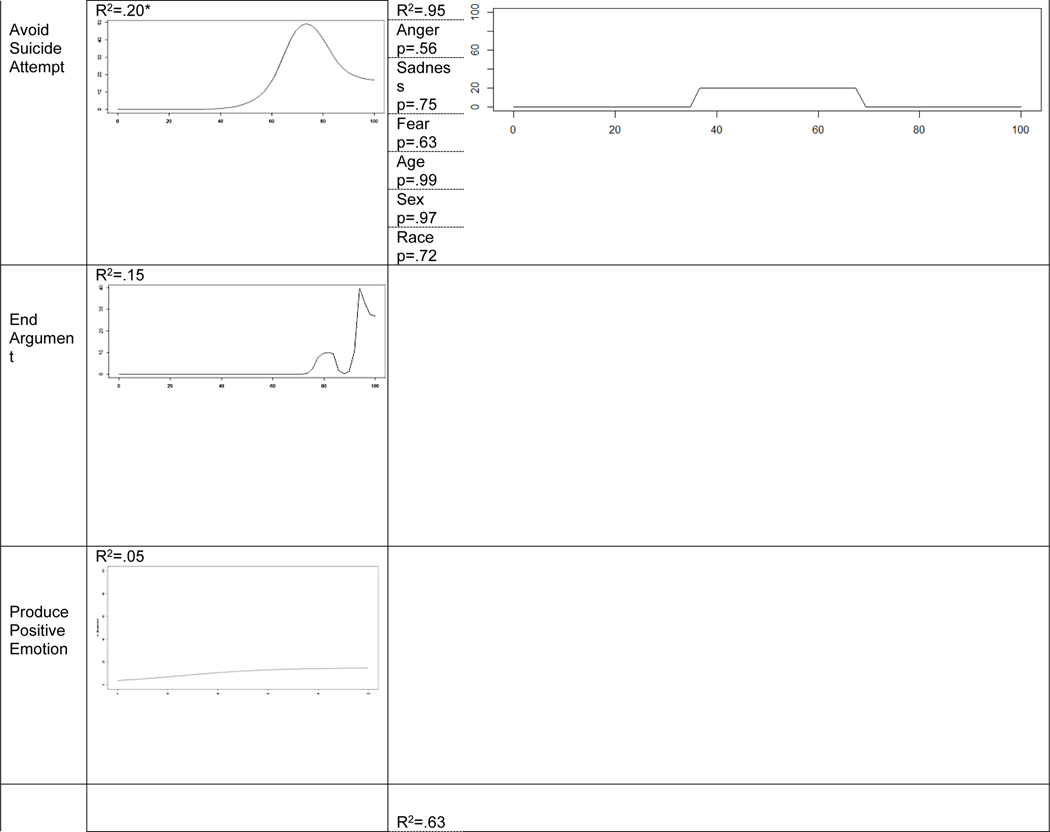
Anger Predicting Functions of NSSI
|
|
|
|
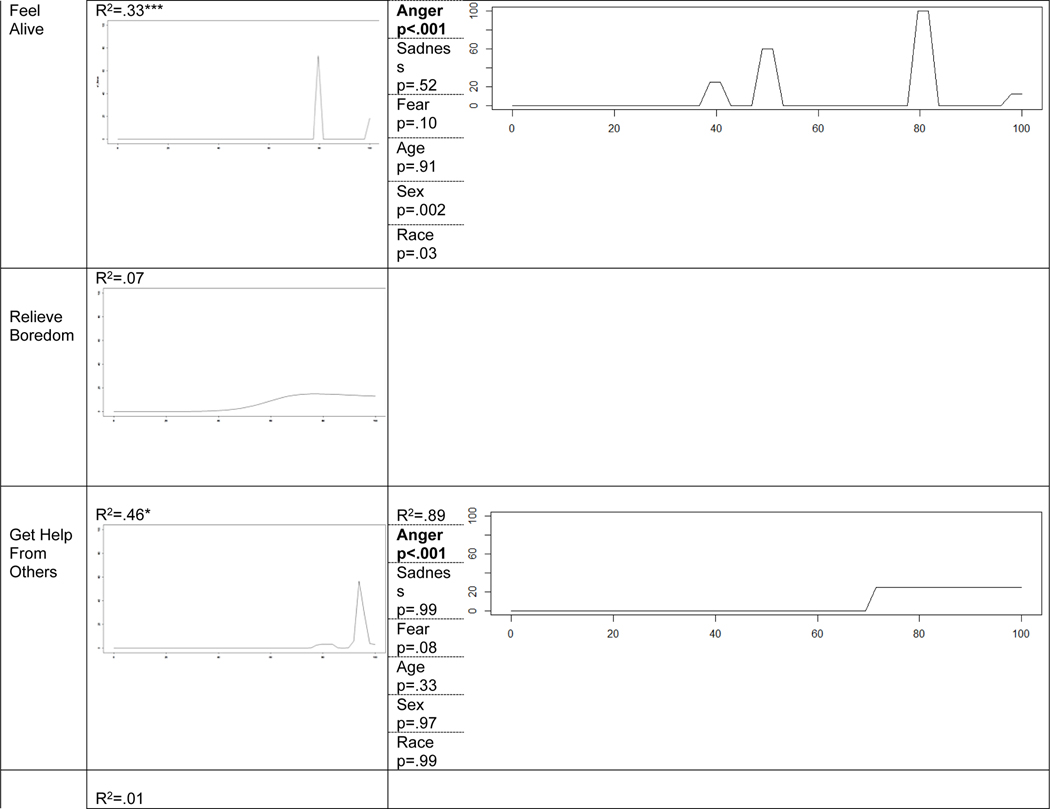
|
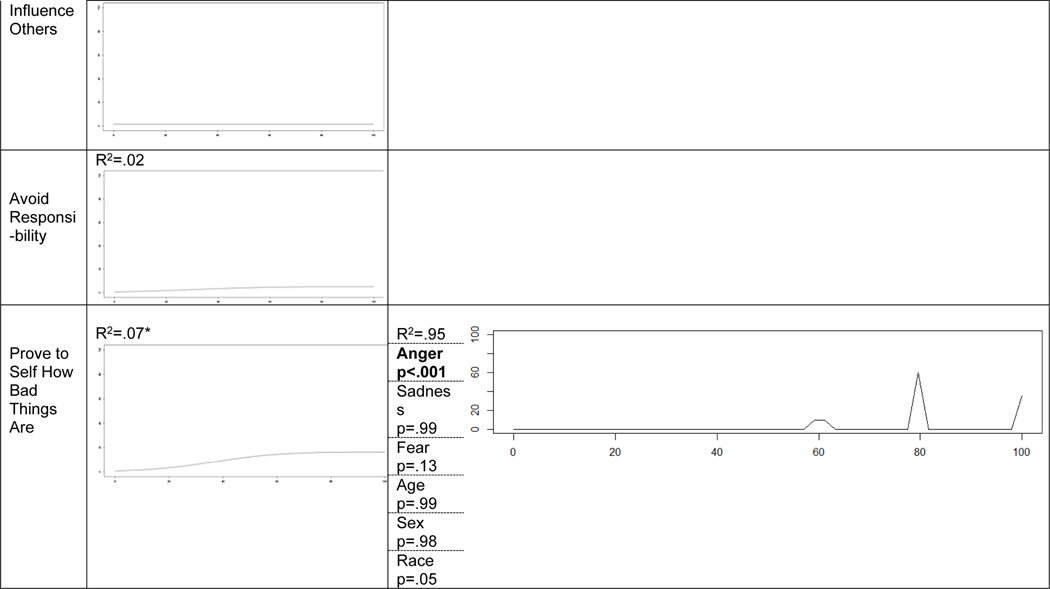
|
Note.
For all graphs the x-axis is the percent of time anger experienced antecedent to NSSI and the y-axis is the percent of time NSSI fulfilled a given function. All adjusted models are also controlling for age, sex, and race. Because Nonparametric Kernel Regression does not estimate parameters, there is no single coefficient to report for these predictors. P-values calculated with independent and identically distributed (IID) boostrapping with 399 replications. Bolded Anger p-values reflect significant association at p<.05 after Bonferroni correction for 12 tests (i.e., p<.004).
p < .001
p < .01
p < .05
To examine the relationship between anger and engagement in different NSSI methods, we employed bivariate nonparametric regression using kernel density estimation procedures to estimate the predictive utility of anger across NSSI methods using the ‘np’ package in R (Hayfield & Racine, 2008). For specific NSSI methods, cutting, burning self with a cigarette, burning self with a lighter or match, carving words into skin, carving other marks into skin, scratching self, biting self, rubbing sandpaper on body, intentionally sticking sharp objects into skin, rubbing glass into skin, head banging, punching oneself, preventing wounds from healing, and punching/hitting walls or objects were explored. Dripping acid onto skin, ingesting cleaning products, and breaking one’s bones could not be analyzed because they were not endorsed.
Finally, we examined the relationship between the emotion variables and functions of NSSI to identify whether anger uniquely predicted any NSSI functions. For these analyses, we first employed bivariate nonparametric regression using kernel density estimation procedures to estimate the predictive utility of anger across all 17 NSSI functions using the ‘np’ package in R. We then followed up with multivariate nonparametric regressions for NSSI functions (controlling additionally for sadness, fear, age, sex, and race) that showed significant bivariate relationships with anger. Nonparametric regression using kernel density estimation is a two-step procedure that first uses the observed distributions of both predictor and outcome variables to estimate the optimal bandwidth of observations in which to apply the kernel function (Altman, 1992). This kernel function is then derived from the relationships between predictor and outcome within each of these bandwidths. Thus, the kernel function is a complex equation representing the relationship between outcome and predictor and different levels of the predictor. This kernel function replaces the single-estimate regression weight which represents the same relationship between outcome and predictor across all levels of the predictor. This kernel function is represented most easily by a line of best fit, and bootstrapped standard errors are used to evaluate the overall probability that the observed kernel function is due to chance (represented as a standard p-value, such that values less than .05 can be described as a “significant association” between predictor and outcome; Hardle & Marron, 1991).
Results
Descriptive Statistics.
Participants (N = 61) reported anger was present prior to engaging in NSSI 71.80% of the time, on average (range 0 – 100, SD = 41.60), sadness was present an average of 46.07% of the time (range 0 – 100, SD = 45.04) and fear was present 31.48% of the time on average (range 0 – 100, SD = 41.28). Thirty-five participants reported anger was present 100% of the time prior to NSSI, 19 reported sadness present 100% of the time, and 12 indicated fear was present 100% of the time. With regard to which emotion was most often present prior to NSSI, 21 participants reported anger, seven reported sadness, and one reported fear. Additionally, several participants reported more than one emotion was present an equivalent percent of the time prior to NSSI. Six indicated anger and sadness were present, one reported anger and fear, one reported sadness and fear, and 24 reported all three emotions were equally present. Overall, 52 participants (85.25%) indicated anger was at least one of the most common emotions antecedent to NSSI, 37 indicated sadness (60.7%), and 27 reported fear (44.3%).
All 17 NSSI function variables, NSSI method variables, and the anger variable were non-normally distributed (defined as skewness ≥ |1|, kurtosis ≥ |3|, and/or bi-modal). The anger variable was bi-modal. Thirteen function variables were highly positively skewed and four were bi-modal. Fourteen NSSI method variables were highly positively skewed and three were not endorsed by any participants. Table 1 presents each of these distributions.
Anger and NSSI Method
To explore whether specific methods of NSSI were associated with specific emotions non-parametric bivariate regressions were conducted to correlate anger antecedent to NSSI with the following methods: cutting, burning self with a cigarette, burning self with a lighter or match, carving words into skin, carving other marks into skin, scratching self, biting self, rubbing sandpaper on body, intentionally sticking sharp objects into skin, rubbing glass into skin, head banging, punching oneself, preventing wounds from healing, and punching/hitting walls or objects were explored. Results indicated anger was significantly associated with burning oneself with a cigarette (R2 = .16, p < .001), carving pictures, designs or other marks into skin (R2 = .12, p < .001), sticking sharp objects into skin (R2 = .33, p = .005), severely scratching oneself (R2 = .26, p < .001), head banging (R2 = .15, p = .02), punching oneself (R2 = .14, p < .001), and punching walls or objects to the point of bruising or bleeding (R2 = .13, p = .02).
Anger and Function of NSSI
Unadjusted and adjusted model results are displayed in Table 1. In unadjusted non-parametric models, anger antecedent to NSSI was significantly predictive of the following functions: reducing negative emotions (R2=.76, p<.001), relieving tension (R2=.40, p<.001), stopping feeling numb (R2=.16, p=.02), punishing self (R2=.11, p=.005), distracting (R2=.35, p<.001), stopping negative thoughts (R2=.22, p<.001), gaining a sense of control (R2=.20, p<.001), communicating to others (R2=.13, p=.03), avoiding attempting suicide (R2=.20, p=.03), feeling alive (R2=.33, p<.001), getting help from others (R2=.46, p=.02), and proving to self how bad things are (R2=.07, p=.03).
When these 12 associations were tested in adjusted non-parametric models, controlling for sadness, fear, age, sex, and race, anger antecedent to NSSI was significantly predictive of the following functions after Bonferroni correction: relieving tension (p<.001), stopping feeling numb (p<.001), communicating with others (p<.001), feeling alive (p<.001), getting help from others (p<.001), and proving to oneself how bad things are (p<.001). No other covariate was significantly predictive of more than three NSSI functions after Bonferroni correction, with race (3 NSSI functions), sex (1 NSSI function), and sadness (1 NSSI function) being the only covariates that were significantly predictive of any NSSI functions.
Discussion
The goal of the present study was to explore the role of anger in NSSI behavior in veterans by assessing (1) the extent to which anger was antecedent to engaging in NSSI, (2) whether the presence of anger was associated with specific methods of NSSI, and (3) whether the presence of anger antecedent to NSSI uniquely predicted any functions of NSSI when controlling for the presence of sadness and fear, two other emotions implicated in this behavior.
Results suggest anger was a common antecedent emotion to NSSI in this sample of veterans. In fact, 85% of participants reported that anger was one of the most common emotions antecedent to NSSI, whereas this was the case for 61% for sadness and 44% for fear. Furthermore, 57% of participants reported that their episodes of self-injury were preceded by anger 100% of the time. This result is consistent with previous literature indicating anger is often associated with engagement in NSSI behavior, whereas fear and sadness are associated with thoughts of NSSI but not the behavior itself (Kleiman et al., 2015; Muehlenkamp et al., 2013; Rodriguez-Seijas et al., 2015). This result also makes conceptual sense. While sadness, fear, and anger are all negatively valanced emotions, sadness and fear are typically associated with avoidance and withdrawal. However, anger is an activating emotion typically associated with an increase in physiological arousal and approach-oriented behavior (Carver & Harmon-Jones, 2009). Thus, of these basic emotions, anger may be the most likely to motivate self-harming behavior.
With regard to methods of NSSI, anger was significantly associated with burning oneself with a cigarette, carving pictures, designs or other marks into skin, sticking sharp objects into skin, severely scratching oneself, head banging, punching oneself, and punching walls or objects. The finding that anger is associated with punching walls or objects is particularly interesting in the context of a veteran population, many of whom report difficulties regulating anger (Sippel et al., 2016). Punching walls or objects is a stereotypically angry behavior, especially for men. However, the results of the current study suggest it can also be a behavior that is engaged in with the intent to inflict self-harm. In a study of veterans seeking treatment for PTSD, 43% of the sample endorsed engaging in wall/object punching as a form of NSSI (Kimbrel et al., 2018). Further, Kimbrel and colleagues (2018) found strong support for the construct validity of wall/object punching as a form of NSSI. The current findings lend additional support to the importance of focusing on this under-recognized method of NSSI.
Regarding functions of NSSI, anger was significantly associated with 12 of the 17 functions assessed. In multivariate analyses, when covarying for demographics as well as fear and sadness, anger remained significantly related to relieving tension, stopping feeling numb, communicating with others, feeling alive, getting help from others, and proving to oneself how bad things are. Furthermore, for all of these functions, anger was the only emotion that was significantly associated with the different functions in the regression models. These results suggest anger is related to a wide range of functions of NSSI. The association of anger with a myriad of functions of NSSI highlights its role in this phenomenon and its importance when understanding NSSI behavior in veterans. These results also again raise the need for careful functional analysis to understand the factors reinforcing NSSI behavior.
Findings from a recent meta-analysis suggest NSSI most often serves an intrapersonal function, specifically reducing aversive internal states (Taylor et al., 2018). In this study the intrapersonal functions related to anger were relieving tension, stopping feeling numb, feeling alive, and proving to oneself how bad things are. Interestingly, while the first two functions are consistent with efforts to reduce unwanted internal states the latter two can be conceptualized as increasing a desirable state. Anger is associated with an increase in sympathetic nervous system activation, and so it is perhaps not surprising that NSSI preceded by anger would produce activating internal states.
Interestingly, anger was also associated with communicating with others and getting help from others. Indeed, anger was the only emotion in this study that was associated with interpersonal functions of NSSI. This preliminary result suggests anger may be uniquely associated with interpersonal functions of NSSI in veterans, a hypothesis that necessitates additional research. The association of these interpersonal functions of NSSI with anger makes strong conceptual sense. Anger-driven behavior can intimidate or coerce others, often resulting in individuals getting what they want in the short-term. However, this behavior often has deleterious effects on relationships in the long-term.
Intervention strategies often differ depending on the function of a given behavior. The association of anger with a wide range of functions of NSSI indicates a range of interventions may help reduce engagement in this behavior among veterans. For NSSI reinforced by lessening distressing internal states (e.g., tension, numbness), emotion regulation skills may provide alternative methods for reducing emotional intensity. NSSI maintained by interpersonal reinforcement (e.g., communication, getting help from others) might be targeted by teaching interpersonal skills such as effective communication, assertiveness, and problem solving. Given the myriad of NSSI functions associated with anger, it is also possible that teaching anger management broadly could be helpful to veterans who engage in NSSI. Future research focused on interventions that reduce engagement in NSSI in veterans is needed.
Results of this study should be considered in light of its limitations. First, there is potential lack of generalizability due to the limited sample size and potential overfitting of the data from nonparametric estimation. While the limited sample size did not allow for splitting into a learning set and validation set to test generalizability, the bandwidth estimation procedure was set to constant instead of variable to minimize overfitting. The use of non-parametric statistics is also a strength of this study. Non-parametric modeling of items has been proposed to combat some of the misleading results that can arise with parametric models, specifically in personality and psychopathology item analysis (Meijer & Baneke, 2004). With regard to generalizability, several characteristics our sample may limit external validity. Veterans with severe clinical presentations (e.g., bipolar disorder, psychotic spectrum disorders, or imminent suicide/homicide risk) were excluded. Future research will be needed to examine the role of anger in NSSI among veterans with these presentations. Additionally, this study’s focus on veterans may limits our ability to draw conclusions about the applicability of our results to non-veteran samples (e.g., college students, community members, non-veteran clinical populations). Given the potential importance of anger in understanding NSSI behavior as indicated by our results, future research should evaluate the role of anger in NSSI with other populations.
Second, data were derived from retrospective self-report provided by participants and all data were cross-sectional. Therefore, these data are subject to the biases and insight of the individuals providing the information. Future studies utilizing methods such as ecological momentary assessment (EMA), that can remediate some of the problems associated with retrospective cross-sectional self-report will be useful for examining the role of anger in NSSI. Third, emotions were assessed using single items from a semi-structured interview. While the use of semi-structured interviews is a strength of this study and provided opportunity to clarify points of confusion, this research would have been strengthened by multiple items assessing emotions present prior to engaging in NSSI. Fourth, inter-rater reliability could not be calculated for the CANDI because all study interviewers participated in diagnostic consensus meetings. Thus, reliability of the assessment in this study is not known. Finally, it was not possible to tease apart the relationship between different emotions and corresponding forms and functions of NSSI for the same person. For example, we were unable to assess whether NSSI served a different function for an individual when it was preceded by anger compared to sadness. This is another question on which EMA can shed light. By assessing NSSI as it occurs in real time, it will be possible to assess whether distinct emotions are associated with unique functions of NSSI.
Despite these limitations, the results of this study highlight the potential importance of focusing on anger as a precursor to NSSI in veterans. Results also emphasize the need for careful functional analysis when examining NSSI in veterans. Behaviors such as wall/object punching that appear impulsively aggressive may actually be NSSI, and NSSI may serve many functions in this population. While results of this study are preliminary, they also suggest veterans may benefit from treatment that teaches anger management and interpersonal skills in order to reduce NSSI and associated negative outcomes.
Acknowledgments
This work was supported by Merit Award #I01CX001486 to Dr. Kimbrel from the Clinical Sciences Research and Development Service (CSR&D) of VA Office of Research and Development (VA ORD). Dr. Dillon was supported by a Career Development Award (IK2RX002965) from the Rehabilitation Research and Development Service of VA ORD. Dan Blalock, PhD is supported by CDA 19-035 and by the Center of Innovation to Accelerate Discovery and Practice Transformation (CIN 13-410) at the Durham VA Health Care System
Dr. Beckham was supported by a Senior Research Career Scientist award (1K6BX003777) from the CSR&D of VA ORD. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the VA or the United States government or any of the institutions with which the authors are affiliated.
References
- Altman NS (1992). An introduction to kernel and nearest-neighbor nonparametric regression. The American Statistician, 46(3), 175–185. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub. [Google Scholar]
- Bailey JS, & Burch MR (2017). Research Methods in Applied Behavior Analysis. Routledge. [Google Scholar]
- Barlow DH, & Nock MK (2009). Why can’t we be more idiographic in our research? Perspectives on Psychological Science, 4(1), 19–21. [DOI] [PubMed] [Google Scholar]
- Barrett LF, Mesquita B, & Gendron M (2011). Context in Emotion Perception. Current Directions in Psychological Science, 20(5), 286–290. 10.1177/0963721411422522 [DOI] [Google Scholar]
- Bentley KH, Nock MK, & Barlow DH (2014). The Four-Function Model of Nonsuicidal Self-Injury: Key Directions for Future Research. Clinical Psychological Science, 2(5), 638–656. 10.1177/2167702613514563 [DOI] [Google Scholar]
- Calhoun PS, Van Voorhees EE, Elbogen EB, Dedert EA, Clancy CP, Hair LP, Hertzberg M, Beckham JC, & Kimbrel NA (2017). Nonsuicidal self-injury and interpersonal violence in U.S. veterans seeking help for posttraumatic stress disorder. Psychiatry Research, 247, 250–256. 10.1016/j.psychres.2016.11.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, & Harmon-Jones E (2009). Anger is an approach-related affect: Evidence and implications. Psychological Bulletin, 135(2), 183–204. 10.1037/a0013965 [DOI] [PubMed] [Google Scholar]
- Dillon KH, Van Voorhees EE, & Elbogen EB (2020). Associations between anger and suicidal ideation and attempts: A prospective study using the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Psychiatric Research, 122, 17–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobscha SK, Denneson LM, Kovas AE, Teo A, Forsberg CW, Kaplan MS, Bossarte R, & McFarland BH (2014). Correlates of suicide among veterans treated in primary care: Case–control study of a nationally representative sample. Journal of General Internal Medicine, 29(4), 853–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doshi A, Boudreaux ED, Wang N, Pelletier AJ, & Camargo CA (2005). National Study of US Emergency Department Visits for Attempted Suicide and Self-Inflicted Injury, 1997–2001. Annals of Emergency Medicine, 46(4), 369–375. 10.1016/j.annemergmed.2005.04.018 [DOI] [PubMed] [Google Scholar]
- Ekman P (1992). An argument for basic emotions. Cognition & Emotion, 6(3–4), 169–200. [Google Scholar]
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, Musacchio KM, Jaroszewski AC, Chang BP, & Nock MK (2017). Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychological Bulletin, 143(2), 187. [DOI] [PubMed] [Google Scholar]
- Gratz KL (2001). Measurement of deliberate self-harm: Preliminary data on the Deliberate Self-Harm Inventory. Journal of Psychopathology and Behavioral Assessment, 23(4), 253–263. [Google Scholar]
- Gratz KL, Dixon-Gordon KL, Chapman AL, & Tull MT (2015). Diagnosis and characterization of DSM-5 nonsuicidal self-injury disorder using the clinician-administered nonsuicidal self-injury disorder index. Assessment, 22(5), 527–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardle W, & Marron JS (1991). Bootstrap simultaneous error bars for nonparametric regression. The Annals of Statistics, 778–796. [Google Scholar]
- Hayfield T, & Racine JS (2008). Nonparametric econometrics: The np package. Journal of Statistical Software, 27(5), 1–32. [Google Scholar]
- Hoge CW (2019). Suicide Reduction and Research Efforts in Service Members and Veterans—Sobering Realities. JAMA Psychiatry, 76(5), 464–466. 10.1001/jamapsychiatry.2018.4564 [DOI] [PubMed] [Google Scholar]
- Kachadourian LK, Gandelman E, Ralevski E, & Petrakis IL (2018). Suicidal ideation in military veterans with alcohol dependence and PTSD: The role of hostility. The American Journal on Addictions, 27(2), 124–130. [DOI] [PubMed] [Google Scholar]
- Kimbrel NA, DeBeer BB, Meyer EC, Gulliver SB, & Morissette SB (2016). Nonsuicidal self-injury and suicide attempts in Iraq/Afghanistan war veterans. Psychiatry Research, 243, 232–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, Gratz KL, Tull MT, Morissette SB, Meyer EC, DeBeer BB, Silvia PJ, Calhoun PC, & Beckham JC (2015). Non-suicidal self-injury as a predictor of active and passive suicidal ideation among Iraq/Afghanistan war veterans. Psychiatry Research, 227(2–3), 360–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, Thomas SP, Hicks TA, Hertzberg MA, Clancy CP, Elbogen EB, Meyer EC, DeBeer BB, Gross GM, & Silvia PJ (2018). Wall/object punching: An important but under-recognized form of nonsuicidal self-injury. Suicide and Life-Threatening Behavior, 48(5), 501–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiman EM, Ammerman BA, Kulper DA, Uyeji LL, Jenkins AL, & McCloskey MS (2015). Forms of non-suicidal self-injury as a function of trait aggression. Comprehensive Psychiatry, 59, 21–27. 10.1016/j.comppsych.2014.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky ED (2007). The functions of deliberate self-injury: A review of the evidence. Clinical Psychology Review, 27(2), 226–239. 10.1016/j.cpr.2006.08.002 [DOI] [PubMed] [Google Scholar]
- Klonsky ED (2009). The functions of self-injury in young adults who cut themselves: Clarifying the evidence for affect-regulation. Psychiatry Research, 166(2–3), 260–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann AJ, Van Voorhees EE, Patel TA, Wilson SM, Gratz KL, Calhoun PS, Beckham JC, & Kimbrel NA (2020). Nail-biting, scab-picking, and tattooing as nonsuicidal self-injury (NSSI): A deviant case series analysis of the proposed NSSI disorder diagnostic criteria. Journal of Clinical Psychology, 76(12), 2296–2313. [DOI] [PubMed] [Google Scholar]
- Meijer RR, & Baneke JJ (2004). Analyzing psychopathology items: A case for nonparametric item response theory modeling. Psychological Methods, 9(3), 354. [DOI] [PubMed] [Google Scholar]
- Muehlenkamp J, Brausch A, Quigley K, & Whitlock J (2013). Interpersonal Features and Functions of Nonsuicidal Self-injury. Suicide and Life-Threatening Behavior, 43(1), 67–80. 10.1111/j.1943-278X.2012.00128.x [DOI] [PubMed] [Google Scholar]
- Nock MK, & Prinstein MJ (2005). Contextual features and behavioral functions of self-mutilation among adolescents. Journal of Abnormal Psychology, 114(1), 140. [DOI] [PubMed] [Google Scholar]
- Nock MK, Prinstein MJ, & Sterba SK (2009). Revealing the form and function of self-injurious thoughts and behaviors: A real-time ecological assessment study among adolescents and young adults. Journal of Abnormal Psychology, 118(4), 816–827. 10.1037/a0016948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novaco RW, Swanson RD, Gonzalez OI, Gahm GA, & Reger MD (2012). Anger and postcombat mental health: Validation of a brief anger measure with US Soldiers postdeployed from Iraq and Afghanistan. Psychological Assessment, 24(3), 661. [DOI] [PubMed] [Google Scholar]
- Ribeiro JD, Franklin JC, Fox KR, Bentley KH, Kleiman EM, Chang BP, & Nock MK (2016). Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: A meta-analysis of longitudinal studies. Psychological Medicine, 46(2), 225–236. 10.1017/S0033291715001804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Blanco L, Carballo JJ, & Baca-García E (2018). Use of Ecological Momentary Assessment (EMA) in Non-Suicidal Self-Injury (NSSI): A systematic review. Psychiatry Research, 263, 212–219. 10.1016/j.psychres.2018.02.051 [DOI] [PubMed] [Google Scholar]
- Rodriguez-Seijas C, Eaton NR, & Krueger RF (2015). How transdiagnostic factors of personality and psychopathology can inform clinical assessment and intervention. Journal of Personality Assessment, 97(5), 425–435. psyh. 10.1080/00223891.2015.1055752 [DOI] [PubMed] [Google Scholar]
- Selby EA, Bender TW, Gordon KH, Nock MK, & Joiner TE (2012). Non-suicidal self-injury (NSSI) disorder: A preliminary study. Personality Disorders: Theory, Research, and Treatment, 3(2), 167–175. 10.1037/a0024405 [DOI] [PubMed] [Google Scholar]
- Sippel LM, Mota NP, Kachadourian LK, Krystal JH, Southwick SM, Harpaz-Rotem I, & Pietrzak RH (2016). The burden of hostility in US Veterans: Results from the National Health and Resilience in Veterans Study. Psychiatry Research, 243, 421–430. [DOI] [PubMed] [Google Scholar]
- Smith SM, Goldstein RB, & Grant BF (2016). The association between post-traumatic stress disorder and lifetime DSM-5 psychiatric disorders among veterans: Data from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). Journal of Psychiatric Research, 82, 16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor PJ, Jomar K, Dhingra K, Forrester R, Shahmalak U, & Dickson JM (2018). A meta-analysis of the prevalence of different functions of non-suicidal self-injury. Journal of Affective Disorders, 227, 759–769. 10.1016/j.jad.2017.11.073 [DOI] [PubMed] [Google Scholar]
- Villatte JL, O’Connor SS, Leitner R, Kerbrat AH, Johnson LL, & Gutierrez PM (2015). Suicide Attempt Characteristics Among Veterans and Active-Duty Service Members Receiving Mental Health Services: A Pooled Data Analysis. Military Behavioral Health, 3(4), 316–327. 10.1080/21635781.2015.1093981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilks CR, Morland LA, Dillon KH, Mackintosh M-A, Blakey SM, Wagner HR, & Elbogen EB (2019). Anger, social support, and suicide risk in U.S. military veterans. Journal of Psychiatric Research, 109, 139–144. 10.1016/j.jpsychires.2018.11.026 [DOI] [PubMed] [Google Scholar]


