Abstract
Background
Educating patients regarding thier inflammatory bowel disease (IBD) is important for their empowerment and disease management. We aimed to develop a questionnaire to evaluate patient understanding and knowledge of IBD.
Methods
We have developed the Understanding IBD Questionnaires (U‐IBDQ), consisting of multiple‐choice questions in two versions [for Crohn's disease (CD) and ulcerative colitis (UC)]. The questionnaires were tested for content and face validity, readability, responsiveness and reliability. Convergent validity was assessed by correlating the U‐IBDQ score with physician's subjective assessment scores. Discriminant validity was assessed by comparison to healthy controls (HC), patients with chronic gastrointestinal (GI) conditions other than IBD, and to GI nurses. Multivariate analysis was performed to determine factors associated with a high level of disease understanding.
Results
The study population consisted of IBD patients (n = 106), HC (n = 35), chronic GI disease patients (n = 38) and GI nurses (n = 19). Mean U‐IBDQ score among IBD patients was 56.5 ± 21.9, similar for CD and UC patients (P = 0.941), but significantly higher than that of HC and chronic GI disease patients and lower than that of GI nurses (P < 0.001), supporting its discriminant validity. The U‐IBDQ score correlated with physician's subjective score (r = 0.747, P < 0.001) and was found to be reliable (intra‐class correlation coefficient = 0.867 P < 0.001). Independent factors associated with high U‐IBDQ scores included academic education (OR = 1.21, 95% CI 1.10–1.33, P < 0.001), biologic therapy experience (OR = 1.24, 95% CI 1.01–1.53, P = 0.046), and IBD diagnosis at <21 years of age (OR = 2.97, 95% CI 1.05–8.87, P = 0.050).
Conclusions
The U‐IBDQ is a validated, reliable and short, self‐reported questionnaire that can be used for assessing understanding of disease pathophysiology and treatment by IBD patients.
Keywords: Crohn's disease, IBD‐questionnaires, inflammatory bowel disease (IBD), patient education, patient knowledge, patient understanding, questionnaire validation, self‐reported outcomes, U‐IBDQ, ulcerative colitis
Key summary
Established knowledge on this subject
Inflammatory bowel diseases (IBD) patients' beliefs and knowledge regarding their disease may affect disease management, quality of life and disease‐related psychological health. Therapy‐related disinformation is associated with low adherence to treatment.
A standardized and validated tool for assessment of IBD patients' knowledge and understanding of their disease is lacking.
Significant findings of this study
We developed and meticulously validated the understanding of IBD questionnaire, a short questionnaire aimed at measuring understanding of disease pathophysiology and treatment of IBD.
Inflammatory bowel diseases‐related knowledge was associated with education level and with younger age at IBD diagnosis.
INTRODUCTION
Inflammatory bowel diseases (IBD) are chronic inflammatory diseases of the gastrointestinal (GI) tract with major impact on patients' well‐being and quality of life. During the past 2 decades understanding of disease pathophysiology and the variety of available therapeutic interventions and preventive medicine recommendations have expanded tremendously. 1 , 2 The explosion of information and their public sources, which are often not accurate, may pose a challenge for both treating physicians and patients. 3 Patients' beliefs and knowledge regarding the disease may affect disease management, quality of life and disease‐related psychological health. 4 , 5 , 6 Therapy‐related disinformation is associated with low adherence to treatment, 7 , 8 while understanding of disease course empowers patients, improves their satisfaction 9 and compliance with treatment, 5 , 10 , 11 , 12 probably resulting in better therapeutic efficacy. 13 Furthermore, structured educational programs were associated with increased patient adherence to therapy. 13
Hence, patients' education regarding their disease and therapeutic aims and options have been adopted as an appropriate strategy to empower patients, enhance their autonomy, encourage them to become full healthcare partners and to determine their therapeutic goals. 14 Unfortunately, patient's knowledge and understanding of their disease is not of high priority for most health care systems, and patient education is not implemented in most practices. 15 One of the obstacles to achieving this aim is the lack of a standardized and validated tool for assessing the knowledge of IBD patients.
Current available questionnaires for assessing patients' knowledge regarding IBD do not discriminate between Crohn's Disease (CD) and ulcerative colitis (UC). 16 , 17 The Crohn's and Colitis Knowledge (CCKNOW) score was developed and validated to enable assessment of patients' understanding of their disease, 18 but this questionnaire has not been updated to assess recent knowledge of IBD pathophysiology and treatment, nor does it reflect important IBD‐related topics such as diet, lifestyle and legal rights. 19 A Korean Inflammatory Bowel Disease Knowledge (IBD‐KNOW) questionnaire, 16 and a French IBD‐INFO questionnaire 17 were recently developed and validated. Both questionnaires are based on the CCKNOW questionnaire, which better reflects knowledge about CD than UC. 18 The IBD‐INFO is extensive and its length may reduce patients' compliance. Therefore, we aimed to develop a short questionnaire to evaluate IBD patients' understanding of disease pathophysiology and treatment, with different versions for CD and UC.
MATERIALS AND METHODS
Questionnaire development
Questionnaire items related to IBD pathogenesis and treatment were initially listed after a literature review of IBD patients' interests and self‐reported knowledge gaps. 6 , 19 These items were reviewed by a multidisciplinary steering group, consisting of six IBD gastroenterologists [5 IBD specialists (AH, YR, NAC, RK, NM), one clinical nutrition specialist (LD)], an IBD nurse, an IBD registered dietitian (RA), and a social worker and psychotherapist of the Department of Gastroenterology and Hepatology of the Tel Aviv Medical Center. Eight topics were chosen as important and relevant for IBD patients: (1) disease pathophysiology and risk factors, (2) diagnosis and follow‐up tests, (3) medicinal treatment of IBD, (4) surgical treatment of IBD, (5) preventive medicine in IBD, (6) nutritional status maintenance, (7) dietary therapy of IBD and (8) patients' rights and social support systems in Israel.
The initial draft of the questionnaire consisted of 40 questions written in Hebrew (The English translated final versions of the questionnaires appear in Supplementary Information S1 and S2). All questions were multiple choice with a single correct answer and an additional option of ‘I don't know’. Two versions of the questionnaire were developed. Most of the questions were common to all IBD patients, while each version had additional questions specific for CD and UC patients. Content validity of the questionnaire was independently evaluated by the steering committee members who were asked to rank the relevance of each question to the item's concept by a Likert scale of four levels: irrelevant/slightly relevant/relevant/very relevant. 20 , 21 A content validity index (CVI) was calculated for each question, denoted as n e /N (n e ‐ representing the number of members who marked the question as relevant/very relevant, N – representing the total number of committee members). 20 , 21 Questions that scored CVI ≤0.78 were excluded from the questionnaire (n = 5). An Average Content Validity Index (ACVI) was calculated for the entire questionnaire as sum CVI/n (sum CVI – representing the sum of all CVI indexes for all questions included in the questionnaire, and n – representing the number of questions included in the questionnaire), to ensure that ACVI = 0.9 after final inclusion of questions. 20 , 21 , 22
Questionnaire validation
A pilot cohort of 36 IBD patients (CD n = 21, UC n = 15) were asked to review the questions in order to examine face validity and responsiveness. A percent of correct answers was calculated to exclude questions to which 90% of patients answered correctly, for prevention of a ceiling effect (n = 3). Floor effect was not considered as an exclusion criterion since none of the questions had a correct response rate of ≤10%. Two questions were removed in response to patients' remarks regarding their length, readability or inconsistency of content.
Two understanding‐IBD questionnaires (U‐IBDQ) were finally formulated separately for CD and UC, with each including 30 questions (24 common questions and 6 disease‐specific questions in each version [Supplementary Information S1 and S2]). Each correct answer scored 3.33 points, and the total U‐IBDQ score potentially ranged from 0 to 100 points.
To the best of our knowledge there is currently no “gold standard” questionnaire for the assessment of IBD patients' understanding of disease pathophysiology. Therefore, construct validity of the U‐IBDQ was assessed by convergent validity and by discriminant validity. Reliability was assessed by a test of internal consistency and a test‐retest evaluation among a sub‐population of IBD patients (n = 34) who were asked to fill‐in the U‐IBDQ a second time, two weeks after the first. Patients were asked to abstain from actively gaining knowledge about IBD during that time period. Correlation between scores of the first and second questionnaires were assessed using intraclass correlation coefficients (ICC).
Convergent validity was assessed in a sample of 60 IBD patients who filled‐in the U‐IBDQ and then held a 15‐min conversation with the study physician, who was blinded to the scores of the U‐IBDQ. The aim was to assess patients' understanding of disease pathology and treatment by the physician's asking standardized questions about each of the questionnaire's items. Questions were both general and personalized according to the patient's own disease experience. During the conversation, the patients were encouraged to speak freely about their knowledge and experience and ask questions. Each of the eight topic groups was graded by the study physician and a final score was the sum of the sub‐scores (range 0–100). The correlation between the U‐IBDQ and physician‐assessed scores was calculated.
Discriminant validity was assessed by comparison of the mean U‐IBDQ score of the IBD patients to the mean U‐IBDQ score of healthy controls (n = 35), patients with chronic conditions treated at the Department of Gastroenterology and Hepatology for conditions other than IBD (n = 38), and GI nurses (n = 19).
Internal consistency of the questionnaire was assessed as the correlation between each item specific sub‐score and the total U‐IBDQ score using Cronbach's alpha.
Study population and data collection
Sample size was calculated as 180 participants including IBD patients and control participants (5 participants per question; 36 questions). 23 , 24 A minimal sample size of 28 was determined for test‐retest reliability analysis with an alpha of 0.05 and a power of 80%. 25
Participants with IBD/other GI conditions were recruited during their clinical visits at the IBD Unit of the Department of Gastroenterology and Hepatology of the Tel Aviv Medical Center (TLVMC) during 2019–2020. GI nurses consisted of the staff of nurses at the Department of Gastroenterology and Hepatology. Healthy controls were recruited from the study team's personal associates. All study candidates were included if 18 < age <70 years, and excluded if suffering from severe chronic diseases such as heart disease, cancer, end stage liver disease etc., and the inability to complete the study protocol. Similarly, candidates were excluded if they had insufficient computer and internet use skills in order to prevent selection bias of participants with reduced chances of self‐education on disease pathophysiology and treatment. Study participants answered the U‐IBDQ, and a demographic and lifestyle questionnaire, that had been validated for the Israeli population. 26 Information on each patient's medical history, IBD phenotype disease characteristics, and medical treatment was retrieved from their medical files by a single blinded observer (GO).
Statistical analysis
All statistical analyses were performed with SPSS version 25.0 for Windows (SPSS Inc.). Continuous variables are presented as means ± standard deviation (SD) and nominal variables as proportions. Continuous variables, such as U‐IBDQ score, age at diagnosis and disease duration, were categorized as high or low according to the study's respective sample median.
The Pearson Chi‐Square test was used to test the association between nominal variables. Since all continuous variables distributed normally, the dependent samples t‐test was used to compare between U‐IBDQ scores and physician‐assessed scores of the IBD patients. One‐way Anova with Bonferroni adjustment to reduce Type I errors was used to test the difference between U‐IBDQ scores of IBD patients and those of controls. Pearson's correlation was used to evaluate the correlation between U‐IBDQ scores and physician assessed scores of IBD patients, and r > 0.7 was used to determine good correlation. 23 , 27 Cronbach's alpha was used to evaluate internal consistency of questionnaire items and acceptable internal consistency was determined if the test statistic was >0.7. 28 Test‐retest reliability of the U‐IBDQ scores of repeated tests was measured by calculating intraclass correlation coefficient (ICC) by applying a two‐way mixed model for absolute agreement. A test statistic >0.7 was considered good. 25 An independent samples t‐test and the Pearson Chi‐square test were used to compare the demographic and disease‐related characteristics of patients who scored high and low on their U‐IBDQ. A high score was defined as a score >60 points, according to the study sample median. A multivariate analysis by logistic regression with adjustment for potential confounders was used to identify factors that were associated with high U‐IBD scores.
Ethical considerations
The study protocol was approved by the Institutional Review Board of the Tel Aviv Medical Center, and all participants provided informed consent prior to study enrollment.
RESULTS
A total of 291 IBD patients were approached during their routine clinical visits at the IBD unit. From these, 106 (36.4%) were included and 33 (11.3%) were excluded based on exclusion criteria and 152 (52.2%) were not interested in participating, primarily (55.5% of non‐responders) due to the will to minimize the time spent in the clinic during the COVID‐19 pandemic. The additional study groups included were healthy controls (n = 35), chronic GI disease patients (n = 38) and GI nurses (n = 19) (Figure 1). Demographic and clinical characteristics of the sample of IBD patients and the control group participants are depicted in Table 1 and Supplementary Table 1.
FIGURE 1.
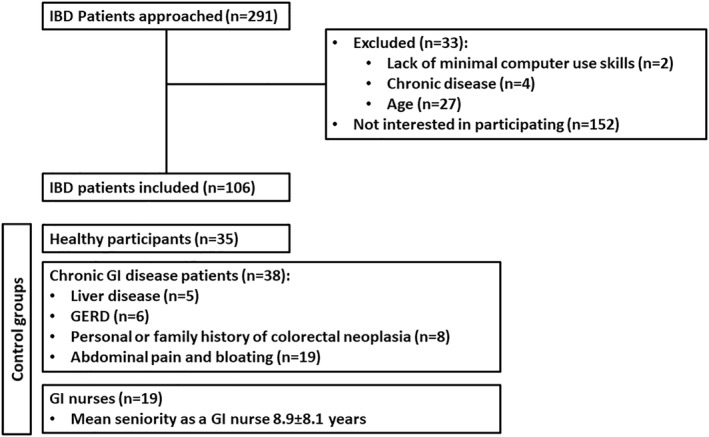
Study population IBD, Inflammatory bowel disease; GERD, Gastroesophageal Reflux Disease; GI, Gastrointestinal
TABLE 1.
Demographics and clinical characteristics of the IBD study population
| Total N = 106 | |
|---|---|
| Demographic characteristics | |
| Age (years, mean ± sd) | 37.6 ± 13.8 |
| Gender – female n, (%) | 46, (43.4) |
| Ever smoking n, (%) | 17, (16.0) |
| BMI (kg/m2, mean ± sd) | 23.6 ± 4.1 |
| Family history of IBD, n, (%) | 26, (24.5) |
| Self‐reported general well‐being n, (%) | |
| Very well | 10, (9.4) |
| Slightly below average | 58, (54.7) |
| Poor | 27, (25.5) |
| Very poor | 9, (8.5) |
| Terrible | 2, (1.9) |
| Education level (n = 105) n, (%) | |
| No high school diploma | 1, (0.9) |
| High school diploma | 17, (16.0) |
| Professional diploma | 33, (31.1) |
| Academic degree | 54, (50.9) |
| Employment status n, (%) | |
| Unemployed | 26, (24.5) |
| Employed | 80, (75.5) |
| IBD characteristics | |
| Disease type n, (%) | |
| CD | 80, (75.5) |
| UC | 26, (24.5) |
| CD montreal phenotype n, (%) among CD patients (n = 80) | |
| A1 – Below 16 years | 19, (13.8) |
| A2 – Between 17 and 40 years | 51, (63.8) |
| A3 – Above 40 years | 10, (12.4) |
| L1 – Ileal | 39, (48.8) |
| L2 – Colonic | 8, (10.0) |
| L3 – Ileo‐colonic | 33, (41.3) |
| B1 – Non‐stricturing, non‐penetrating | 39, (48.8) |
| B2 – Stricturing | 15, (18.8) |
| B3 – Penetrating | 26, (32.5) |
| Perianal disease | 29, (36.3) |
| Harvey Bradshaw Index (HBI) (mean ± sd) among CD patients (n = 80) | 7.5 ± 4.2 |
| UC Montreal phenotype n, (%) among UC patients (n = 26) | |
| E1 – Proctosigmoiditis | 10, (38.5) |
| E2 – Left sided colitis | 6, (23.1) |
| E3 – Extensive colitis (extending beyond the flexure) | 9, (34.6) |
| S0 – Remission (SCCAI ≤ 2) | 4, (15.4) |
| S1 – Mild (SCCAI 3–5) | 12, (46.2) |
| S2 – Moderate (SCCAI 6–10) | 8, (30.8) |
| S3 – Severe (SCCAI ≥ 10) | 2, (7.7) |
| Simple clinical colitis activity index (SCCAI) (mean ± std) among UC patients (n = 26) | 7.9 ± 4.4 |
| Age of diagnosis (years, mean ± sd) | 25.0 ± 11.9 |
| Disease duration (years, mean ± sd) | 12.9 ± 10.9 |
| Past surgery n, (%) | 32, (30.2) |
| Extra‐intestinal manifestations n, (%) | 10, (9.4) |
| Biologic therapy experience n, (%) | |
| Naïve | 30, (29.2%) |
| Past therapy | 11, (10.4%) |
| Current therapy | 64, (60.4) |
Abbreviations: CD, Crohn's disease; HBI, Harvey Bradshaw Index; IBD, inflammatory bowel diseases; SCCAI, Simple Clinical Colitis Activity Index; UC, ulcerative colitis; U‐IBDQ, understanding‐IBD Questionnaire.
The mean U‐IBDQ score among the sample of IBD patients was 56.5 ± 21.9 (range 7–90). Scores did not differ significantly between patients with CD and UC (56.4 ± 21.9 vs. 56.8 ± 22.3 respectively, P = 0.941).
The U‐IBDQ demonstrated high convergent validity
A sub‐sample of 60 IBD patients filled‐in the U‐IBDQ and additionally underwent assessment of disease understanding by a study physician, who was* blinded to the results of the U‐IBDQ. There was a strong correlation between the U‐IBDQ score and the physician's subjective score (r = 0.747, P < 0.001) (Figure 2). Specific knowledge items which were scored individually by both the physician and the U‐IBDQ, yielded weaker correlations (Table 2).
FIGURE 2.
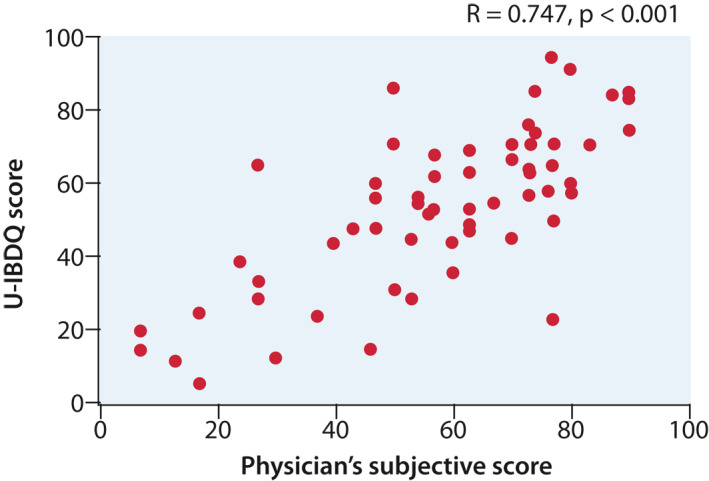
Pearson's correlation between the physician's subjective disease understanding score and the U‐IBDQ score
TABLE 2.
Correlations between physician's subjective item sub‐scores and U‐IBDQ item sub‐scores
| Questionnaire item | Physician's subjective disease understanding score | |
|---|---|---|
| r | p | |
| Disease pathophysiology and risk factors | 0.530 | <0.001 |
| Diagnosis and follow‐up tests | 0.437 | <0.001 |
| Medical treatment of IBD | 0.412 | 0.001 |
| Surgical treatment of IBD | 0.463 | <0.001 |
| Preventive medicine in IBD | 0.495 | <0.001 |
| Nutritional status maintenance | 0.585 | <0.001 |
| Dietary therapy of IBD | 0.274 | 0.032 |
| Patients' rights and social support mechanisms | 0.453 | <0.001 |
Abbreviations: IBD, inflammatory bowel diseases; U‐IBDQ, Understanding‐IBD Questionnaire.
The U‐IBDQ demonstrated high discriminant validity
Significant differences were found in the U‐IBDQ scores between IBD patients and control groups. The mean U‐IBDQ score of IBD patients was significantly higher than that of the healthy controls and the chronic GI disease patients, and lower than that of the GI nurses. These differences were significant with stratification to both questionnaire versions (CD vs. UC) (Figure 3).
FIGURE 3.
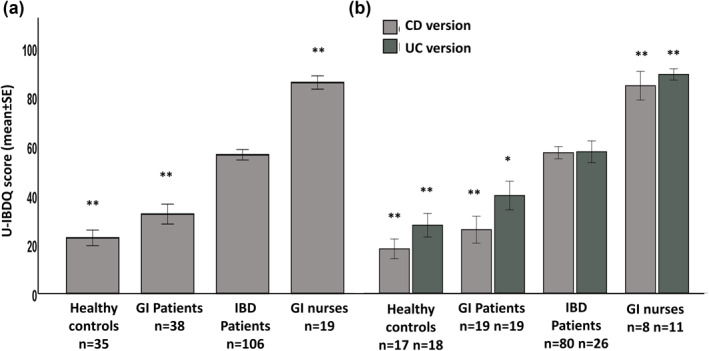
Mean U‐IBDQ scores among the study groups (a) and stratified by questionnaire version (b) A significant difference from IBD patients *P < 0.05, **P < 0.001
A higher U‐IBDQ score among all IBD patients was associated with being a non‐smoker, having an academic education, a younger age at diagnosis, and biologic therapy experience (Table 3). Correlations between age of diagnosis and U‐IBDQ total score and item sub‐scores were consistent (Supplementary Table 2). Among patients with CD, a higher U‐IBDQ score was associated with a perianal disease. Disease duration was not significantly associated with higher disease understanding (Table 3).
TABLE 3.
Association between patient and disease characteristics and U‐IBDQ scores
| Low U‐IBDQ score (≤60) n = 50 | High U‐IBDQ score (>60) n = 56 | p | |
|---|---|---|---|
| Demographic characteristics | |||
| Age (years, mean ± sd) | 39.7 ± 14.7 | 35.8 ± 12.8 | 0.153 |
| Gender – female (%) | 38.0 | 48.2 | 0.290 |
| Ever smoking (%) | 24.0 | 8.9 | 0.035 |
| BMI (kg/m2, mean ± sd) | 24.0 ± 4.2 | 23.3 ± 3.9 | 0.434 |
| Family history of IBD | 12.0 | 8.9 | 0.605 |
| Self‐reported general well‐being (%) | |||
| Very well | 5.7 | 3.8 | 0.540 |
| Slightly below average | 58.0 | 51.8 | |
| Poor | 22.0 | 28.6 | |
| Very poor | 8.0 | 8.9 | |
| Terrible | 0.0 | 3.6 | |
| Education level (%) | |||
| No high school diploma | 2.0 | 0.0 | 0.003 |
| High school diploma | 20.4 | 12.5 | |
| Professional diploma | 44.9 | 19.6 | |
| Academic degree | 32.7 | 67.9 | |
| Employment status (%) | |||
| Unemployed | 30.0 | 19.6 | 0.216 |
| Employed | 70.0 | 80.4 | |
| IBD characteristics | |||
| Disease type (%) | |||
| CD | 80.0 | 71.4 | 0.306 |
| UC | 20.0 | 28.6 | |
| CD montreal phenotype (%) among CD patients (n = 80) | |||
| A1 – below 16 years | 15.0 | 32.5 | 0.039 |
| A2 – Between 17 and 40 years | 65.0 | 62.5 | |
| A3 – above 40 years | 20.0 | 5.0 | |
| L1 – Ileal | 52.5 | 45.0 | 0.679 |
| L2 – Colonic | 12.5 | 7.5 | |
| L3 – Ileo‐colonic | 35.0 | 47.5 | |
| B1 – Non‐stricturing, non‐penetrating | 52.5 | 45.0 | 0.061 |
| B2 – Stricturing | 27.5 | 10.0 | |
| B3 – Penetrating | 20.0 | 45.0 | |
| Perianal disease | 23.7 | 52.6 | 0.009 |
| Harvey Bradshaw Index (HBI) (mean ± sd) among CD patients (n = 80) | 7.8 ± 5.2 | 8.2 ± 4.9 | 0.709 |
| UC Montreal phenotype (%) among UC patients (n = 26) | |||
| E1 – Proctosigmoiditis | 50.0 | 67.6 | 0.470 |
| E2 – Left sided colitis | 10.0 | 31.3 | |
| E3 – Extensive colitis (extending beyond the flexure) | 40.0 | 31.1 | |
| S0 – remission (SCCAI ≤ 2) | 20.0 | 12.6 | 0.510 |
| S1 – mild (SCCAI 3–5) | 60.0 | 37.5 | |
| S2 – moderate (SCCAI 6–10) | 10.0 | 43.8 | |
| S3 – severe (SCCAI ≥ 10) | 10.0 | 6.3 | |
| Simple Clinical Colitis Activity Index (SCCAI) (mean ± sd) among UC patients (n = 26) | 6.3 ± 3.6 | 6.8 ± 3.4 | 0.464 |
| Age of diagnosis (years, mean ± sd) | 28.5 ± 12.4 | 22.0 ± 10.6 | 0.005 |
| Disease duration (years, mean ± td) | 11.8 ± 10.5 | 13.8 ± 11.2 | 0.346 |
| Past surgery (%) | 24.5 | 35.7 | 0.213 |
| Extra‐intestinal manifestations (%) | 10.6 | 9.1 | 0.793 |
| Biologic therapy experience | |||
| Naïve | 44.0 | 9.2 | 0.004 |
| Past therapy | 28.0 | 35.4 | |
| Current therapy | 46.0 | 73.2 | |
Note: The U‐IBDQ score was categorized as high and low score according the study sample median score.
Abbreviations: CD, Crohn's disease; HBI, Harvey Bradshaw Index; IBD, inflammatory bowel diseases; SCCAI, Simple Clinical Colitis Activity Index; UC, ulcerative colitis; U‐IBDQ, understanding of inflammatory bowel diseases.
The U‐IBDQ scores of IBD patients diagnosed at a young age (≤21 years, n = 54) were higher compared to those of patients with IBD diagnosed at an older age (>21 years, n = 51), (63.3 ± 19.3 vs. 49.5 ± 22.5 respectively, P = 0.001). Also, the U‐IBDQ scores of IBD patients with an academic education (n = 51) were higher compared to those with no academic education (n = 54) (49.3 ± 21.7 vs. 63.5 ± 20.1 respectively, P = 0.001). On the other hand, the score of patients with short disease duration (≤10 years, n = 52) did not differ from those with a long disease duration (>10 years, n = 52), (53.6 ± 22.1 vs. 59.0 ± 21.5 respectively, P = 0.206). The highest U‐IBDQ scores were documented among IBD patients diagnosed at a young age, and had an academic education (Figure 4).
FIGURE 4.
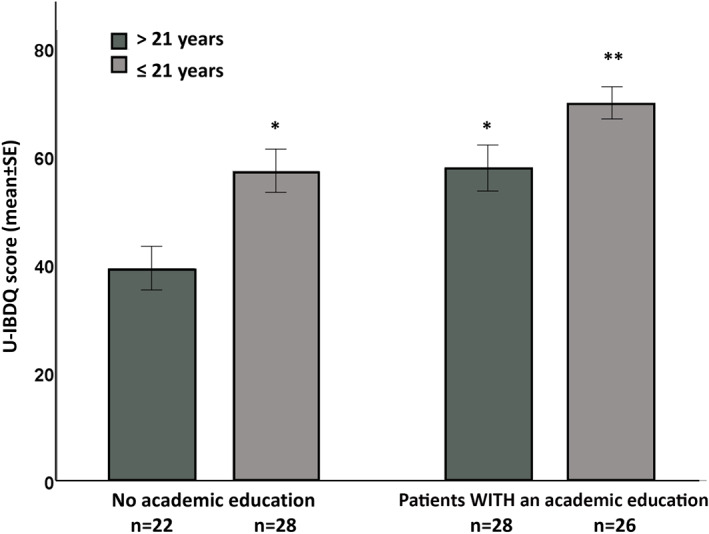
U‐IBDQ scores of IBD patients categorized by age of diagnosis and academic education
A multivariate analysis adjusted to age, gender, disease duration and disease activity, demonstrated an independent association between a high level of disease understanding and academic education (OR = 1.21, 95% CI 1.10–1.33, P < 0.001), biologic therapy experience (OR = 1.24, 95% CI 1.01–1.53, P = 0.046), and IBD diagnosis before the age of 21 years (OR = 2.97, 95% CI 1.05–8.87, P = 0.050).
Reliability of the U‐IBDQ
The internal consistency of the U‐IBDQ was demonstrated by the correlations between the U‐IBDQ total score and item specific sub‐scores (Cronbach's alpha = 0.77). Furthermore, item specific scores of the questionnaire were correlated with each other. Weaker correlations were detected between the “Dietary therapy of IBD” and “Patients' rights and social support mechanisms” and “Diagnosis and follow‐up tests” sub‐scores, and the rest of all item specific sub‐scores (Supplementary Table 3).
The U‐IBDQ of 34 IBD patients who filled‐in in the U‐IBDQ twice, had a good reliability as determined by ICC = 0.867 (95%CI 0.735–0.934, P < 0.001), and was similar between patients with CD [ICC = 0.870 (95%CI 0.704–0.942, P < 0.001)], and patients with UC [ICC = 0.872 (95%CI 0.402–0.972, P < 0.001)].
DISCUSSION
Management of IBD is a lifelong challenge for patients. Their beliefs and knowledge regarding disease pathology and treatment may affect self‐efficacy, disease management and behavioral choices such as diet and physical activity performance, as well as coping with anxiety and depression, and overall quality of life. 4 In this study, we have developed and validated the U‐IBDQ questionnaire, an updated, comprehensive and simple questionnaire, aimed at assessing the knowledge and understanding of patients with IBD.
Development of the U‐IBDQ questionnaires was performed by the collaboration of a diverse team of professional and experienced IBD care‐givers and patients with IBD. The U‐IBDQ questionnaires are patient‐centered and integrative. 29 Items selected for the questionnaire are diverse and include novel items, that had not been assessed in previous IBD knowledge questionnaires such as “Patients rights” and “Nutritional status maintenance.” 16 , 17 These knowledge items can now be assessed in a valid way for the first time. Compared to the few previously published questionnaires addressing patient knowledge of IBD, 16 , 17 , 18 the U‐IBDQ has some additional advantages, including addressing recent and up‐to‐date advances in the multidisciplinary treatment of IBD, being relatively short and easily accessible, and consisting of unique CD/UC population‐specific versions.
Validity of the questionnaire was tested in several ways and shown to be high. Convergent validation of the U‐IBDQ was achieved by a single, blinded and trained physician, who assessed patient knowledge and understanding of their disease through a personal interview. The correlation between the physician's subjective score of patient's knowledge, and the U‐IBDQ score was high for both the total score and for item‐specific scores. Thus, the U‐IBDQ score may represent the physician's perceived patient knowledge, which had been previously associated with better communication with medical professionals, better disease control and higher patient satisfaction. 30 , 31
The U‐IBDQ had good discriminant validity, with the trained professional nurses scoring the highest, and the IBD patients' scores being higher than those of healthy controls and of other patients with chronic GI disorders. This suggests that the U‐IBDQ is a measurement of the understanding of IBD, rather than any other chronic condition of the GI tract. High U‐IBDQ scores were associated with an academic education, medical experience, and disease diagnosed at a younger age, independently of other features of the disease itself, such as disease duration and disease activity. This is compatible with previously reported knowledge levels in IBD patients, 16 , 17 and is similar to those of other chronic diseases. 32 , 33 The highest scores of the U‐IBDQ were seen among patients diagnosed at a young age, with an academic education. This might be explained by the potential accessibility of younger patients to the internet and new social medias, which have been shown to be the most common platforms of self‐education. 34 Furthermore, research suggests that most of the available online material on IBD are too difficult to comprehend for a substantial portion of the patient population, 35 and may mostly be understandable by patients with a higher education. Surprisingly, disease duration and activity were not associated with understanding of disease in the current study, as opposed to previous reports, 17 perhaps reflecting older age and lower access to modern media platforms. Finally, the U‐IBDQ has an internal consistency, and is stable over time, with high test re‐test reliability among participants who reported not having actively increased their understanding of their disease during the 2 weeks gap between filling the same questionnaires.
The results of this study are compatible with previous reports that showed a mean understanding score of ∼50% of total score. 16 , 17 This relatively low score emphasizes the need to prioritize patient education and understanding of their disease. The sample of IBD patients who participated in both the development and the validation cohorts was large, in addition to having been recruited systematically and non‐differentially from all clinics of our IBD unit. In spite of the relatively low response rate, our study sample included patients from a wide spectrum of demographic and clinical characteristics. Study population heterogeneity was also reflected by the wide range of U‐IBDQ scores. We assume that our results apply to the general population of IBD patients since the main reason for refusal to participate in the study had not been directly related to the questionnaire itself.
Several other possible limitations of this study include the possible referral filter bias and limited validity to pediatric patients who were excluded in this validation cohort. Also, information bias may exist regarding the capture of knowledge items, which had not been included in the U‐IBDQ, and may be important to specific patient groups, such as reproduction and family planning, and transition from pediatric to adult clinics. 36 , 37 Also, in future studies, use of the U‐IBDQ will require the adaptation of the ‘legal and social rights' item questions, to the population under investigation. These items should be implemented in future population‐specific questionnaires developed in future studies. Also, due to lack of an empirical gold standard for assessing patients' knowledge of their disease, U‐IBDQ scores were compared to a subjective score given by the same study physician, in a blinded and standardized manner for all patients. Thus, the potential information bias is expected to be non‐differential between patients.
CONCLUSIONS
We have developed and meticulously validated the U‐IBDQ, a short, self‐report questionnaire that has demonstrated good reliability and validity in measuring understanding of disease pathophysiology and treatment in IBD. Future studies should correlate disease understanding with adherence to therapy, and long‐term clinical and patient‐reported outcomes.
CONFLICT OF INTEREST
No financial disclosures or conflicts of interest to any of the authors.
Supporting information
Supporting Information S1
Supporting Information S2
Table S1
Table S2
Table S3
ACKNOWLEDGMENTS
We would like to thank the Israeli foundation of Crohn’s Disease and Ulcerative Colitis for its support. We thank Sigalit Lahav (IBD nurse at the IBD unit), Alona Borochov (social worker and psychotherapist), and the participating nurses of the Department of Gastroenterology and Liver Diseases, Tel Aviv Medical Center, for their help in questionnaire development and validation. We also thank Ester Eshkol for assistance with manuscript preparation.
Ostromohov G, Fibelman M, Hirsch A, Ron Y, Cohen NA, Kariv R, et al. Assessment of patients' understanding of inflammatory bowel diseases: development and validation of a questionnaire. United European Gastroenterol J. 2022;10(1):104–14. 10.1002/ueg2.12182
Gaiana Ostromohov, Morin Fibelman, Nitsan Maharshak, Naomi Fliss‐Isakov contributed equally to this work.
DATA AVAILABILITY STATEMENT
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to ongoing analysis for further publication.
REFERENCES
- 1. Guan Q. A comprehensive review and update on the pathogenesis of inflammatory bowel disease. J Immunol Res. 2019;2019:7247238. 10.1155/2019/7247238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kuhnen A. Genetic and environmental considerations for inflammatory bowel disease. Surg Clin. 2019;99(6):1197–207. 10.1016/j.suc.2019.08.014 [DOI] [PubMed] [Google Scholar]
- 3. Bernstein CN, Fried M, Krabshuis JH, Cohen H, Eliakim R, Fedail S, et al. World Gastroenterology organization practice guidelines for the diagnosis and management of IBD in 2010. Inflamm Bowel Dis. 2010;16(1):112–24. 10.1002/ibd.21048 [DOI] [PubMed] [Google Scholar]
- 4. Reusch A, Weiland R, Gerlich C, Dreger K, Derra C, Mainos D, et al. Self‐management education for rehabilitation inpatients suffering from inflammatory bowel disease: a cluster‐randomized controlled trial. Health Educ Res. 2016;31(6):782–91. 10.1093/her/cyw042 [DOI] [PubMed] [Google Scholar]
- 5. Coenen S, Weyts E, Jorissen C, De Munter P, Noman M, Ballet V, et al. Effects of education and information on vaccination behavior in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2017;23(2):318–24. 10.1097/MIB.0000000000001013 [DOI] [PubMed] [Google Scholar]
- 6. Lesnovska KP, Börjeson S, Hjortswang H, Frisman GH. What do patients need to know? Living with inflammatory bowel disease. J Clin Nurs. 2014;23(11‐12):1718–25. 10.1111/jocn.12321 [DOI] [PubMed] [Google Scholar]
- 7. Broekman MMTJ, Coenen MJH, Wanten GJ, van Marrewijk CJ, Kievit W, Klungel OH, et al. Patients’ beliefs about medicine are associated with early thiopurine discontinuation in patients with inflammatory bowel diseases. Eur J Gastroenterol Hepatol. 2018;30(2):167–73. 10.1097/MEG.0000000000001025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fu N, Jacobson K, Round A, Evans K, Qian H, Bressler B. Transition clinic attendance is associated with improved beliefs and attitudes toward medicine in patients with inflammatory bowel disease. World J Gastroenterol. 2017;23(29):5405–11. 10.3748/wjg.v23.i29.5405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Waters BM, Jensen L, Fedorak RN. Effects of formal education for patients with inflammatory bowel disease: a randomized controlled trial. Can J Gastroenterol J Can Gastroenterol. 2005;19(4):235–44. 10.1155/2005/250504 [DOI] [PubMed] [Google Scholar]
- 10. Wang L, Fan R, Zhang C, Hong L, Zhang T, Wang Z, et al. Patients’ educational program could improve azathioprine adherence in Crohn’s disease maintenance therapy. Gastroenterol Res Pract. 2020;2020:6848293. 10.1155/2020/6848293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Elkjaer M, Shuhaibar M, Burisch J, Bailey Y, Scherfig H, Laugesen B, et al. E‐health empowers patients with ulcerative colitis: a randomised controlled trial of the web‐guided “Constant‐care” approach. Gut. 2010;59(12):1652–61. 10.1136/gut.2010.220160 [DOI] [PubMed] [Google Scholar]
- 12. Kamat N, Rajan Mallayasamy S, Sharma PSVN, Kamath A, Pai CG. Video assisted patient education improves compliance with follow up and depression scores in Inflammatory Bowel Diseases. Postgrad Med. 2018;130(3):355–60. 10.1080/00325481.2018.1442978 [DOI] [PubMed] [Google Scholar]
- 13. Park J, Yoon H, Shin CM, Park YS, Kim N, Lee DH. Higher levels of disease‐related knowledge reduce medical acceleration in patients with inflammatory bowel disease. PLoS One. 2020;15(6):e0233654. 10.1371/journal.pone.0233654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jotterand F, Amodio A, Elger BS. Patient education as empowerment and self‐rebiasing. Med Health Care Philos. 2016;19(4):553–61. 10.1007/s11019-016-9702-9 [DOI] [PubMed] [Google Scholar]
- 15. Kapasi R, Glatter J, Lamb CA, Acheson AG, Andrews C, Arnott ID, et al. Consensus standards of healthcare for adults and children with inflammatory bowel disease in the UK. Frontline Gastroenterol. 2020;11(3):178–87. 10.1136/flgastro-2019-101260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yoon H, Yang S‐K, So H, Lee KE, Park SH, Jung S‐A, et al. Development, validation, and application of a novel tool to measure disease‐related knowledge in patients with inflammatory bowel disease. Korean J Intern Med. 2019;34(1):81–9. 10.3904/kjim.2017.104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Danion P, Buisson A, Roblin X, Mathieu N, Charlois A‐L, Borgerding JN, et al. IBD‐INFO questionnaire: a multicenter French up‐to‐date survey of patient knowledge in inflammatory bowel disease. Inflamm Bowel Dis. 2018;24(5):943–52. 10.1093/ibd/izx073 [DOI] [PubMed] [Google Scholar]
- 18. Eaden JA, Abrams K, Mayberry JF. The Crohn’s and Colitis Knowledge Score: a test for measuring patient knowledge in inflammatory bowel disease. Am J Gastroenterol. 1999;94(12):3560–6. 10.1111/j.1572-0241.1999.01536.x [DOI] [PubMed] [Google Scholar]
- 19. Pittet V, Vaucher C, Maillard MH, Girardin M, de Saussure P, Burnand B, et al. Information needs and concerns of patients with inflammatory bowel disease: what can we learn from participants in a bilingual clinical cohort? PLoS One. 2016;11(3):e0150620. 10.1371/journal.pone.0150620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bolarinwa OA. Principles and methods of validity and reliability testing of questionnaires used in social and health science researches. Niger Postgrad Med J. 2015;22(4):195–201. 10.4103/1117-1936.173959 [DOI] [PubMed] [Google Scholar]
- 21. Liang N, Zhao Q, He Y, Li J, Yang L. Development and validity of a questionnaire on dyslipidemia dietary knowledge. BioMed Res Int. 2019;2019: 5382130. 10.1155/2019/5382130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Arat S, Van den Zegel A, Van Rillaer M, Moons P, Vandenberghe J, De Langhe E, et al. Development and preliminary evaluation of the validity and reliability of a revised illness perception questionnaire for healthcare professionals. BMC Nurs. 2016;15:34. 10.1186/s12912-016-0156-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tsang S, Royse CF, Terkawi AS. Guidelines for developing, translating, and validating a questionnaire in perioperative and pain medicine. Saudi J Anaesth. 2017;11((Suppl 1)):S80–9. 10.4103/sja.SJA_203_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rattray J, Jones MC. Essential elements of questionnaire design and development. J Clin Nurs. 2007;16(2):234–43. 10.1111/j.1365-2702.2006.01573.x [DOI] [PubMed] [Google Scholar]
- 25. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–63. 10.1016/j.jcm.2016.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kaluski DN, Goldsmith R, Arie OM, Mayer C, Green M. The first Israeli national health and nutrition survey (MABAT) as a policy maker. Publ Health Rev. 2000;28(1‐4):23–6. [PubMed] [Google Scholar]
- 27. Kazi AM, Khalid W. Questionnaire designing and validation. JPMA J Pak Med Assoc. 2012;62(5):514–16. [PubMed] [Google Scholar]
- 28. Tavakol M, Dennick R. Making sense of Cronbach’s alpha. Int J Med Educ. 2011;2:53–5. 10.5116/ijme.4dfb.8dfd [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kennedy ST, Maddux MH, System IPILH. Patient‐clinician collaboration in the development of an IBD transfer toolkit. Pediatrics. 2019;144(3):e20190558. 10.1542/peds.2019-0558 [DOI] [PubMed] [Google Scholar]
- 30. Aelbrecht K, Rimondini M, Bensing J, Moretti F, Willems S, Mazzi M, et al. Quality of doctor‐patient communication through the eyes of the patient: variation according to the patient’s educational level. Adv Health Sci Educ Theory Pract. 2015;20(4):873–84. 10.1007/s10459-014-9569-6 [DOI] [PubMed] [Google Scholar]
- 31. Hagihara A, Tarumi K. Doctor and patient perceptions of the level of doctor explanation and quality of patient‐doctor communication. Scand J Caring Sci. 2006;20(2):143–50. 10.1111/j.1471-6712.2006.00420.x [DOI] [PubMed] [Google Scholar]
- 32. Gautam SK, Gupta V. Impact of knowledge, attitude and practice in the management of Type 2 diabetes mellitus in developing countries: a review. Curr Diabetes Rev. 2021;17. Published online January 5, 2021. 10.2174/1573399817666210106104230 [DOI] [PubMed] [Google Scholar]
- 33. Yuan N, Boscardin C, Lisha NE, Dudley RA, Lin GA. Is better patient knowledge associated with different treatment preferences? A survey of patients with stable coronary artery disease. Patient Prefer Adherence. 2021;15:119–26. 10.2147/PPA.S289398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Keller R, Fusco S, Stange EF, Malek NP, Wehkamp J, Klag T. Infodemiology of Crohn’s disease and Ulcerative colitis using Google Trends ‐ an approach to investigate patient needs. Z Gastroenterol. 2020;58(3):224–33. 10.1055/a-1068-2877 [DOI] [PubMed] [Google Scholar]
- 35. van der Marel S, Duijvestein M, Hardwick JC, van den Brink GR, Veenendaal R, Hommes DW, et al. Quality of web‐based information on inflammatory bowel diseases. Inflamm Bowel Dis. 2009;15(12):1891–6. 10.1002/ibd.20976 [DOI] [PubMed] [Google Scholar]
- 36. Malter L, Jain A, Cohen BL, Gaidos JKJ, Axisa L, Butterfield L, et al. Identifying IBD providers’ knowledge gaps using a prospective web‐based survey. Inflamm Bowel Dis. 2020;26(9):1445–50. 10.1093/ibd/izaa032 [DOI] [PubMed] [Google Scholar]
- 37. Krauthammer A, Harel T, Zevit N, Shouval DS, Shamir R, Weiss B. Knowledge of disease and self‐management of adolescents with inflammatory bowel diseases. Acta Paediatr Oslo Nor 1992. 2020;109(10):2119–24. 10.1111/apa.15211 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information S1
Supporting Information S2
Table S1
Table S2
Table S3
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to ongoing analysis for further publication.


