Abstract
Background
Respiratory infections are the most frequent health problem in childhood leading to morbidity and socioeconomic burden. Studying symptoms of respiratory infections in home based settings requires dedicated prospective cohort studies using diaries. However, no information is available on which birth cohort studies using symptom diary data. A review of birth cohort studies with available symptom diary data, follow-up data, and bio samples is needed to support research collaborations and create potential synergies.
Methods
We conducted a scoping review of birth cohort studies using diaries for the collection of respiratory symptoms. The scoping review was conducted in accordance with the PRISMA Extension. We searched the electronic databases PubMed, Embase, Web of science and CINAHL (last search November 2020) resulting in 5872 records (based on title and abstract screening) eligible for further screening.
Results
We examined 735 records as full text articles and finally included 57 according to predefined inclusion criteria. We identified 22 birth cohort studies that collect(ed) data on respiratory symptoms using a symptom diary starting at birth. Numbers of participants ranged from 129 to 8677. Eight studies collected symptom diary information only for the first year of life, nine for the first two years or less and six between three and six years. Most of the cohorts collected biosamples (n = 18) and information on environmental exposures (n = 19).
Conclusion
Information on respiratory symptoms with daily resolution was collected in several birth cohorts, often including related biosamples, and these data and samples can be used to study full spectrum of infections, particularly including those which did not require medical treatment.
Introduction
Acute respiratory infections (ARI) are the most common health problems in early childhood [1], and the most common causes of death in children under the age of 5 years worldwide [2]. Although most of ARI are not severe [1], they are frequent and cause a high number of doctor visits [3, 4], hospitalizations, antibiotic prescriptions [3, 5], a high socioeconomic burden [6, 7], and absenteeism in education and work [8]. Infections with respiratory viruses (e.g. human rhinovirus, enterovirus and adenovirus) in early childhood may influence the development of chronic and immune-mediated diseases such as asthma, type II diabetes and obesity later in life [9, 10], however, it is not clear how. Research in this area therefore remains very important. About half of ARI in infancy do not lead to consultation of a physician, which leads to a significant underestimation of the true incidence [7, 11–14].
For many specific etiologic questions, it is necessary to have information on a light course of infections. However, this requires prospective data, and collecting this information provides a large challenge. Therefore, the accurate recording of ARI during early childhood needs thoroughly planned prospective birth cohort studies using symptom diaries. Symptom diaries are tools for participants to record symptoms daily in a systematic manner over a defined period [15]. This allows analyses of a prospective evolution of symptoms linked to specific pathogens (if biosamples allow identification of pathogens) and accounting for previous infection episodes, age at infection and time since the last episode. Symptom diaries have a long tradition in evaluating acute infections [13, 16], but are also very demanding. Therefore, other approaches such as retrospective questionnaires, reports from clinical visits or retrospective interviews are more often used [17–23], but have to accept the possibility of recall bias [24]. Additionally, retrospective assessment does not allow studying the duration of symptoms or the change of symptoms over time adequately.
In birth cohort studies, newborns or infants are recruited before, at, or shortly after birth and observed over many years to examine associations between early life exposures and outcomes later in life [25]. Many birth cohorts have been focusing on respiratory infectious diseases and various aspects of these studies were covered in systematic and scoping reviews [26–32].
However, none of them focused on the prospective recording of respiratory infections using symptom diaries and the combination with biosamples. This information can be used to study patterns and severity of symptoms associated with pathogens and other factors such as susceptibility, immune system development or the development of chronic diseases later in life.
In this scoping review, we aimed to compile, map, and compare the existing birth cohort studies collecting symptom diary information on respiratory infections in childhood starting at birth to promote potential research collaborations and exploit synergies. We considered respiratory infections, the collection of biosamples and environmental exposures in order to identify studies suitable for providing a holistic understanding of the association of ARI as exposure with potential long-term sequelae in a life course perspective.
Material and methods
Inclusion and exclusion criteria
This scoping review was performed using PRISMA Extension [33]. We included (1) prospective observational birth cohort studies that (2) examined healthy newborns and (3) used a symptom diary related to respiratory infections. We defined a birth cohort study as a study that recruits children prospectively prior to birth or up to the age of four months.
We excluded all other study designs such as randomized controlled trials, case control studies, cross sectional, qualitative studies and publications in languages other than English. In addition, we excluded studies that focused only on children with chronic lung disease, studies that included children only when a specific symptom or virus was identified, studies that recruited children older than 4 months, or studies that focused only on preterm infants. There were no requirements for the duration of the symptom diary or a time limit for the date of publication.
Search strategy
In a first step, we searched four electronic databases (last search 11.2020): MEDLINE; EMBASE; CINAHL; Web of Science. The search strategy was developed to include several terms referring to respiratory infections in children, symptom diary, and study design. In Table 1, we present the search strategy that was used for MEDLINE and was applied with minor changes to the other databases.
Table 1. Search strategy for PubMed.
| (Child [TIAB] OR Children [TIAB] OR Childhood [TIAB] OR newborn [TIAB] OR infant [TIAB] OR newborn [MH] OR infant [MH] OR child [MH]) |
| AND |
| (“birth-cohort” [TIAB] OR birth* [TIAB] OR “Prospective-study” [TIAB] OR “longitudinal study” [TIAB] OR “follow-up study”[TIAB] OR cohort* [TIAB] OR “Birth cohort study” [TIAB]OR “cohort studies”[MH]) |
| AND |
| (“respiratory-tract-infection” [TIAB] OR“Infectious diseases” [TIAB] OR “Infection diseases” [TIAB] OR “communicable diseases” [TIAB] OR “respiratory infections” [TIAB] OR “virology” [TIAB] OR “immunology” [TIAB] OR “virus disease” [TIAB] OR “viral disease” [TIAB] OR “infectious” [TIAB] OR “bacterial infection” [TIAB] OR “infections” [TIAB] “respiratory tract infections"[MH]"communicable diseases"[MH] OR “virology"[MH] OR “allergy and immunology"[MH] OR" virus diseases"[MH] OR "bacterial infections"[MH] OR "infection"[MH]) |
| AND |
| (“Daily-diary-study” [TIAB] OR Diary [TIAB] OR “daily-diary” [TIAB] OR “daily-diaries” [TIAB] OR “daily-observation” [TIAB] OR “daily- records” [TIAB] OR “self-reported-Questionnaire”[TIAB] OR “Symptom records”[TIAB] OR “Symptom questionnaire”[TIAB]OR “Symptom diary” [TIAB] OR “Symptom diaries” [TIAB]) |
Cohort identification took place between January 2019 and November 2020.
One researcher (SL) screened titles and abstracts of identified studies with respect to the inclusion and exclusion criteria. In a second step, two authors (SL and BK) conducted a backward search whereby bibliographies of the included studies were screened to identify any studies that might have been missed in the first screening. Subsequently, titles, abstracts and full text articles of additionally identified references were screened according to the inclusion and exclusion criteria. The results of both screeners were compared and discrepancies were discussed. In a third step, we scanned other sources such as registers of birth cohort studies (BirthCohorts.net (https://www.birthcohorts.net/) (11.2020), Asthma Birth Cohorts Database (https://asthmabirthcohorts.niaid.nih.gov/) and performed a grey-literature search and reviewed other reviews of birth cohorts (last search 11.2020). The final search results were exported into EndNote and duplicates were removed. Two authors (SL and BK) extracted data from all included birth cohorts independently, based on predefined criteria, compared the results, and discussed disparities. Data of interest included: cohort name, country in which the study took place, number of participants, enrollment period, follow-up times without symptom diary, symptom diary duration (from birth), at what age questionnaires were answered, if and at what time communication was via email, telephone and if interviews were conducted, if and when home visits, examinations in the clinic or in general took place. In addition, we extracted data on what biosamples were collected and at what time. In addition, it was of interest which risk factors for respiratory infections were of interest in each study. In only three of the cohorts a cohort profile was available. Thus, information on the study design was often taken from several publications focusing on different aspects of the same cohort study. It was often not possible to extract complete data from these specialized publications. Therefore, the last step was to validate and complement the extracted results by contacting the authors of the most recent publications of the respective birth cohorts via email and asking them to confirm or complete the available information (February-November 2020). Reminders were sent 3–5 weeks later. Investigators of 14 out of 22 studies (63.6%) responded to our inquiries.
Results
Search results
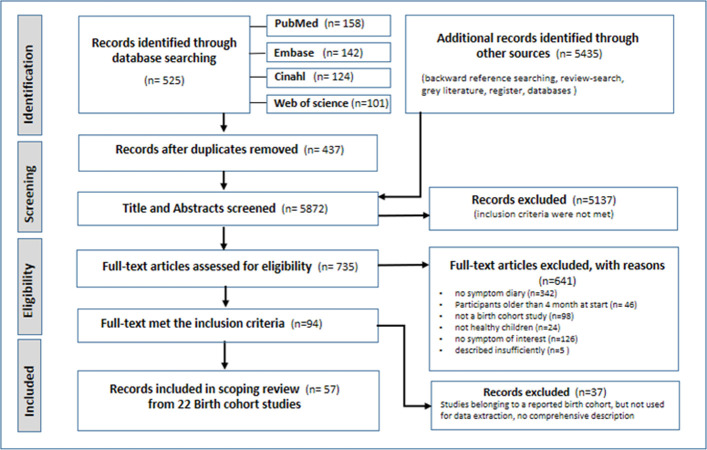
We identified 5960 records by database search and by backward reference, register and review search (Fig 1).
Fig 1. PRISMA-flow diagram.
After removing duplicates, 5872 records were included in the screening of abstracts and titles of which 735 were found eligible for full-text analysis based on our inclusion criteria. Of these, a final number of 57 full-text articles met the inclusion criteria. Based on the articles, we identified 22 birth cohort studies that collect data or have already completed data collection on respiratory symptoms using a symptom diary (Table 2).
Table 2. Study characteristics sorted by descending enrollment period of birth cohort studies with approximately N = 26000 participants.
| REF | COUN-TRY | PARTICIPANTS (newborns) | ENROLLMENT PERIOD | SYMPTOM DIARY DURATION (from birth) | FOLLOW UP (FU) (without symptom diary) | QUESTIONNAIRE | CALLS/ INTERVIEW/ EMAIL | HOME-VISITS | CLINICAL VISITS/EXAMINATIONS | |
|---|---|---|---|---|---|---|---|---|---|---|
| PittsburghCohort(*)† | [42] | USA | n = 244 | 07/1985-04/1886 | until 3 yrs | every 2 wks | - | every 2 wks | - | - |
| Adelaide-Cohort (*)† | [38] | South AUS | n = 1981 | 05/1987 04/1988 |
until 2 yrs | after birth, once every 3 m until 24 m | 9 and 18 m | after delivery and discharge, then every 3 m until 2 yrs | - | - |
| New Mexico-Cohort(*)† | [11, 16, 36] | USA | n = 1205 χ [17] | 01/ 1988 06/1990 χ |
until 18 m | every 2 wks calls/ Interview | - | every 2 wks, up to age 18 m | at enrolment | - |
| Raine Study * | [43–46] | West AUS | n = 2868 χ [46] | 05/1989-11/1991 χ (53) | first y of life | 18, 34 wks gestation, birth, 1,2,3,5,8,10,14, 17,18,20,22,27 yrs | at age of 1, 2, 3, 4, 5, 8, 10, 14,17, 20 and 22, 27 yrs | telephone FU/ interviews ϕ | - | at age of 1, 2, 3, 5, 8, 10, 14, 17, 18, 20, 22 yrs |
| Perth-Cohort (*)† | [5, 47] | AUS | n = 263 | 07/1996-06/1998 | until 5 yrs | birth, 6 wks, 6, 12 m of age, then yl | not described in detail | telephone calls until resolution of the child’s symptoms | home visit for respiratory symptoms | at 6 wks, 6 and 12 m of age, and then yl |
| VIGALL (*) | [34] | NLD | n = 126 | 08/1996-11/1998 | wkly symptom card until 2 yrs | birth, 3m, 6m, 12m, 18m, 24m | birth, 3, 12, 24 m | - | during signs of URI | 6 m, 12 m, 18 m, 24 m |
| PEIC (*)‡ | [41, 48] | CAN | n = 332 | 06/1997 1999 |
until 2 yrs | twice mtly until 2 yrs | - | phoned twice mtly | - | - |
| Allergy-flora (*) | [49, 50] | SWE | n = 187 | 1998 2003 |
first y of life | 6, 12 m until 18 m Contact to parents at wk 1, 2, 4 and 8 until 2005 | - | at enrolment, then 6 and 12 m | - | at 18 m of age and if allergic symptoms occur |
| COPSAC 2000 (*) | [51, 52] | DK | n = 411 | 08/1998 12/2001 | until 6 yrs ϕ | 2, 4 wks ϕ, every 6 m until the age of 7 yrs, then at the age of 9, 12, 18 yrs | - | at enrolment, 1, 6, 12 m | - | at the age of 2 wks, every 6 m until the age of 7; if symptoms occur |
| WHIST-LER * | [53–57] | NLD | n = 2133 [58] | 12/2001-01/2013 | first y of life | at birth, mtly during the first 12 m, 5, 8 yrs | birth, mtly during first y, then yl | as reminder | to collect dust | 2nd or 3rd wk of life /FU 5 and 8 yrs |
| PASTURE (*) | [58–60] | AUT DEU FIN FRA CHE | n = 1133 | 08/2002 03/2005 |
2 m until 1 y | before birth 2, 12, 18, 24, 36, 48, 60, 72 m, at the age of 6 yrs, 10,5 yrs (until 2015) | before birth, 2, 12, 18, 24 m, and then yl until age of 6, 10,5 yrs | before birth, 2, 12, 18, 24 m, and then yl until age of 6 yrs | age of 2 m | age of 1y |
| Kopen-hagen-Cohort(*)† | [37, 61, 62] | DK | n = 242 χ | 05/2004 05/2005 |
first y of life | mtly until 1 y (1 May 2006) | - | at the first home visit, repeated every second m | mtly | mtly home visits |
| TEDDY Study * | [35, 63, 64] | USA/EUR | n = 8677 | 12/2004-02/2010 | 3 m until 2 yrs, then appropriate book | every 3 m until 4 yrs, then yl until the age of 15 yrs | 3, 9 m, up-dated after 2 yrs, then every 4 y | during visits biannually at 4 yrs of age | - | every 3 m until the age of 4yrs, then biannual, subgroup every 3 m |
| Madigan Childcare Study (*) ‡ | [65–67] | USA | n = 225 ¥ | 02/2006-04/2008 10/2008-06/2009 |
STA was completed by the child’s parent for 10 days following illness onset for 2 y | interviews until 40 m of age χ | - | at enrolment and if symptoms occurred | at illness onset | a study physician documented visit/ nurse contact in childcare site |
| Utrecht-Cohort (*)† | [68–71] | NLD | n = 291 χ (39) | 03/2006-02/2010χ | first y of life | 1 and 12 m | at 1m and 1 y of age | around birth, 3 wks after delivery | first respi-ratory infection | to withdraw blood at first m |
| STEPS * | [72–75] | FIN | n = 1827 | 01/2008-04/2010 | first two yrs of life daily, then wkly until 5 yrs of age | before and after birth, 13, 18, 24 m. until the age of 2 yrs | before birth, birth, 13, 18, 24 m, then yl | no | no | if symptoms occur/ age of 2, 13, and 24 m. |
| COPSAC 2010 * | [76] | DK | n = 700 | 2008/2010 | until 3 yrs ϕ | 24, 36 wks gestation,1 wk, 1, 3, 6 m, then every 6 m until 36 m, then yl until 6 yrs, then at the age of 8, 10 yrs | online survey from 2016 onwards ϕ | at regular intervals between visits | - | week 24 of gestation, 1, 3, 6 m, then every 6 m until 36 m, then yl until 7yrs; if symptoms occur |
| DIABIMMUNE | [77–80] | FIN EST RUS | n = 563 | 09/2008–10/2013 | 3m until 3 yrs | 3, 6, 12, 18, 24, 36 m | 3, 6, 12, 18, 24, 36 m | - | - | 3, 6, 12, 18, 24, 36-m |
| OrChid (*) | [12, 81–83] | AUS | n = 158 | 09/2010-10/2014 | until 2 yrs | every 3 m until 2nd birthday | no | telephone-interview 3‐mtly | no | after delivery |
| NPICS (*) | [39, 84] | NIC | n = 518 n = 1705 ¥ | 2011–2013 | until 2 yrs (subgroup) | until 2 yrs, wkly in diary subgroup | at enrollment, then yl. | yl calls and email as reminder | for part who did not attend FU | yl/ first signs of influenza-like illness |
| PATCH (*) | [85, 86] | TWN | n = 387 | 01/2012-11/2014 | first y of life | 1, 2, 4, 6, 12 m | at each planned visit | calls, interviews, emails | - | regular visits at clinic and examinations, if symptoms occur |
| Loewen KIDS * | [87] | DEU | n = 782 | 11/2014-02/2018 | until 6 yrs | at birth, 3,6,12,18, 24 m, then yl until age of 15 y | at birth, 6 m, age 1 till 15 yl. | email as reminder | no | to withdraw blood |
|
wk
wkly m mtly y yl part |
week
weekly months monthly year yearly participant |
¥ (*) * - χ † |
over all sample size
complete active data not reported varies according to publication if no study name was known the location of the primary centre is given |
‡
‡ Madigan Childcare-Study ‡PEIC URI ϕ - |
abbreviated cohort name
Madigan Army Medical Centre-Childcare Study Prince Eduard Island Cohort upper respiratory infection validated through study stuff- different to data in publication Data not reported |
|||||
Characteristics of included cohorts
The majority of included birth cohorts were conducted in Europe (n = 12), four were conducted in Australia, four in the United States of America and one each in Canada, Nicaragua and in Taiwan. Three of those were conducted in several countries, such as the TEDDY Study, which was conducted in the United States and Europe.
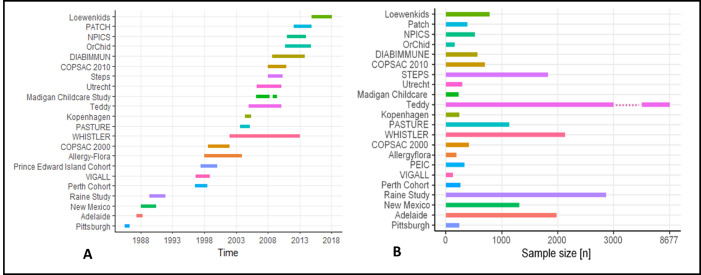
The number of participants ranged from 126 in the VIGALL- Study [34] to 8677 in the Teddy-Study [35] (Fig 2A). The most recent study is the LoewenKIDS study from Germany which recruited participants between 2014 and 2016, while the oldest study is a cohort study from Pittsburgh, which enrolled subjects from July 1985 to April 1986 (Fig 2B).
Fig 2.
A. Time of enrollment B. Number of participants in considered studies.
Recruitment period had a median of 30 months and ranged between 9 and 133 months. Five studies are still collecting data at the time of writing, while 17 studies are completed.
Symptom diary and follow up
In most cases, symptom diary entries were only noted when study participants showed symptoms, in others, participants were asked to enter all days including those without symptoms. The response rate of symptom diary data was reported rarely. Six years was the longest period for which symptom recording by diary was planned, while the shortest was ten months (Table 2). Seven studies collected data by symptom diary only for the first year of life or less, seven studies for the first two years, three for three years or less, two for six years, and the other studies for five years, 21 months and 18 months.
Besides using symptom diaries, thirteen studies used questionnaires to conduct the follow-up of their participants. The mode of follow-up by questionnaires ranged between monthly assessments to a follow-up interval of 17 years, but the majority of birth cohorts sent out questionnaires very frequently in the first two years after birth. In addition to questionnaires, telephone calls, interviews, email contact, home visits, and clinical examinations were used to contact the participants and collect data. Most studies used phone calls and interviews to conduct follow-ups. Nine studies carried out home visits in order to collect data, to remind participants, or to conduct routine visits during the first respiratory infection or in cases where subjects could not come to the study center. Clinical visits or medical examinations took place in 18 studies, which were usually part of a fixed follow-up-appointment. A smaller proportion of these studies encouraged their participants to visit a health center when symptoms of respiratory infections occurred.
Almost all studies analyzed individual symptoms, such as dry or wet cough, wheezing, runny or stuffy nose, sore throat, fever, chills, loss of appetite and attachment. From these symptoms, most studies derived acute respiratory infections (ARI) as outcome variables. Lower and upper respiratory tract infection (LRTI, URTI) were reported in thirteen of the studies listed. Some studies considered only individual diseases such as pneumonia, acute otitis media, or rhinitis.
We also considered the drop-out rates of the identified studies. However, not all studies reported a clear rate and those that did are very heterogeneous and not very comparable.
After six months, the New Mexico cohort recorded a drop-out rate of 12.5% [36]. The identified drop-out rates in the first year of life ranged from 10.3% in the Perth Cohort [6] and the Copenhagen Cohort [37] to 47% in the Adelaide Cohort [38]. The NPICS Cohort study was also in the lower third with 14.8% within at the first year [39]. In contrast, the STEPS study [40] reported a drop-out rate of 6% after 13 months. Three of the identified studies reported a drop-out rate of 12% after 2 years in the LoewenKIDS cohort (personal request), 32.5% in the Vigall cohort [34] and 58% in the Adelaide cohort. The PEIC cohort [41] reported a drop-out rate of 20.5% after three years. The data of all other studies considered here could not be clearly and comparably identified.
Biosamples
Eighteen studies collected biosamples from participants during follow up periods.
Blood samples
The collection of blood from children was part of the protocol in thirteen studies (Table 3). Eight of these studies took additional blood samples, including umbilical cord blood (n = 8) and maternal blood (n = 7). One study collected umbilical cord blood samples only.
Table 3. Biological samples collected in the birth cohorts studies.
| COHORT -NAME | CHILD BLOOD | ASYMPTOMATIC NASAL SWAB | SYMPTOMATIC NASAL SWAB | ASYMPTOMATIC STOOL SAMPLE | MATERNAL BLOOD | CORD BLOOD | OTHER SAMPLES |
|---|---|---|---|---|---|---|---|
| Raine | age of 5, 8, 14, 17, 18, 20, 22 yrs | - | - | - | 18 wks, 34 wks before birth | yes | placental-, semen-, urine-, saliva sample |
| VIGALL-Study | - | - | if symptoms occur | - | - | - | - |
| Perth-Cohort | 5 yrs | one in winter and a second in summer | onset of respiratory symptoms | - | - | - | - |
| Allergyflora | age of 18 m | - | - | wk 1, 2, 4, and at 6, 8, 12, 18 m, part born after 07/2000 additionally at age of 36 m | - | - | - |
| COPSAC 2000 | 6 m, 18 m, 1, 4, 6 yrs | during infancy | 1m, 1y and if symptoms occur until 3 yrs | 1w, 1, 12, 18 yrs | ad-hoc but at least 2 yrs after birth | yes | hair-, urine-, breast-milk-, saliva-sample |
| COPSAC 2010 | 6, 18 m, 6,8,10 yrs | 1 w, 1 m, 3 m | if symptoms occur | 1w, 1m, yl until 6 yrs, then at the age of 8, 10 yrs | 24th wk of pregnancy | yes | hair-, urine-, breast-milk-, saliva-, skin-, dried blood sample |
| PASTURE | 1, 4, 6, 10,5 y | - | - | - | at birth, at age of 1 year | yes | breast milk (2 m) |
| Kopenhagen | age 5 days, 12 m | at every home visit (mtly) | - | - | at enrolment | - | - |
| Madigan Childcare Study | - | a sample at time of enrolment | at symptom onset and wkly thereafter until asymptomatic | study 2008–2009 wkly asymptomatic and symptomatic samples | - | - | - |
| TEDDY Study | every 3 m until to the end | at 9 m of age and at each visit thereafter | - | mtly until 48 m of age, then every three m until 10 yrs, then every six m until 08/2018. | gestation/ at birth | yes | toe nail clipping, urine, saliva sample |
| Utrecht-Cohort | age of 1 m | - | at every respiratory episode | - | - | - | - |
| STEPS | 1, 2 and 3 yrs | 2, 13 and 24 m | during respiratory infection | at the age of one year | yes | yes | breastmilk |
| WHISTLER | - | the start of every m (subgroup) | second day of a wheezing episode (only subgroup) | - | - | - | buccal sample at birth |
| DIABIMMUNE | 3, 6, 12, 18, 24, 36m | during each visit of study clinic | - | every m starting at age of 1 m | - | yes | - |
| NPICS | yl for children > 6 m | - | during visits at health centre with symptoms | - | - | - | - |
| OrChid | - | at birth and wkly | - | at birth and once a week | - | yes | |
| PATCH | - | 1, 2, 4, 6, 12 m | during acute wheezy episodes | - | - | - | - |
| LoewenKIDS | age of 1 y and 2 yrs in subcohort | once per year (age 0–6 yrs; complete cohort) four times per year (age 0–2; subcohort) | if respiratory symptoms occur | once per year (age 0–6 years; complete cohort) four times per year (age 0–2; subcohort) additionally symptomatic sample if symptoms occur | - | yes | buccal sample at the age of 1 y |
| wk | - | Week | yrs | years | data not reported | ||
| wks | wks | y | year | ||||
| wkly | weekly | yl | yearly | ||||
| m | months | Mtly part | Monthly participant |
Nasal swabs
A total of fifteen studies collected nasal swabs in different frequencies. In eight of fifteen studies, nasal swabs were taken when the child was free of respiratory infection symptoms and every time symptoms occurred, whereas in three of the fifteen studies, only asymptomatic swabs were taken.
Stool samples
Nine studies collected stool samples when children were free of gastrointestinal symptoms. Of these, one study additionally collected stool samples in symptomatic subjects.
Other biomaterials
In eight studies, genetic swabs (n = 6), urine samples (n = 4), placental sample (n = 1), toe nail clipping (n = 1), hair sample (n = 2), dried blood (n = 1), skin sample (n = 1), semen (n = 1), and samples of breastmilk (n = 4) were collected.
Exposures and potential risk factors for respiratory infections
In most studies, known exposures and risk factors such as environmental exposures in households and outside of households, information on social contacts, socioeconomic factors, birth mode, breastfeeding, presence of siblings, animal contact, daycare-attendance, vaccination, nutrition, stress, and information about the family history were part of the collected data (Table 4). Seven studies assessed all mentioned risk factors.
Table 4. Recorded variables for exposures/ risk factors for respiratory infections.
| COHORT NAME | RISK FACTORS | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ENVIRONMENTAL | HOUSEHOLD EXP. | SOCIAL RELATION SHIP | SOCIOOE CONOMIC STATUS | BIRTH MODE | BREAST FEEDING | SIBLINGS | ANIMAL CONTACT | DAY CARE ATTENDANCE | VACCI NATION | NUTRITION | STRESS | FAMILY HISTORY | |
| Pittsburgh | - | - | - | + | - | - | + | - | + | - | - | - | + |
| Adelaide-Cohort | + | - | + | - | + | + | + | - | + | - | - | - | + |
| Raine Study | + | + | + | + | + | + | + | + | + | + | + | + | + |
| New Mexico | + | + | + | + | + | + | + | - | + | - | - | - | + |
| VIGALL | - | + | + | + | + | + | + | + | + | - | + | - | + |
| Perth-Cohort | + | + | + | - | - | + | + | + | + | - | - | - | + |
| PEIC | + | + | + | + | - | + | - | + | + | - | - | - | + |
| Allergyflora | + | + | + | + | + | + | + | + | + | - | + | - | + |
| COPSAC 2000 | + | + | + | + | + | + | + | + | + | + | + | + | + |
| COPSAC 2010 | + | + | + | + | + | + | + | + | + | + | + | + | + |
| PASTURE | + | + | + | + | + | + | + | + | + | + | + | - | + |
| Kopenhagen-Cohort | + | + | + | + | + | + | + | + | + | + | + | - | + |
| Madigan Childcare Study | + | - | + | + | + | - | + | + | + | - | - | - | + |
| TEDDY | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Utrecht-Cohort | - | + | + | + | + | + | + | + | + | - | + | - | + |
| STEPS | + | + | + | + | + | + | + | + | + | + | + | + | + |
| WHISTLER | + | + | + | + | + | + | + | + | + | - | + | - | + |
| DIABIMMUNE | + | + | - | - | + | + | + | + | + | + | + | - | + |
| NPICS | + | + | + | + | + | + | + | + | + | + | + | + | + |
| OrChid | + | + | + | + | + | + | + | + | + | + | + | - | + |
| PATCH | + | + | + | + | + | + | + | + | + | + | + | - | + |
| LoewenKIDS | + | + | + | + | + | + | + | + | + | + | + | + | + |
+ yes
- data not recorded
Discussion
In this scoping review, we identified 22 birth cohort studies using a symptom diary to collect symptoms of respiratory infections beginning within the first four months after birth. These studies varied in terms of number of participants, duration of data collection, follow-up times, as well as in respiratory outcomes, collected biosamples and assessed environmental exposures.
The number of detected birth cohort studies employing diaries is small compared to the overall number of birth cohort studies that were established on bronchial asthma, allergies, and respiratory infections over the past 35 years. Some excluded studies used symptom diaries after the first year of life and the majority of the excluded studies used other approaches like retrospective questionnaires, interviews and clinical visits to estimate the burden of respiratory diseases [17–23].
While episodes of respiratory infections can be recalled fairly well over a period of two months [88–90], it is unlikely that daily symptom evolution can be accurately recalled without prospective daily collection. Therefore, it is unlikely that the sequence of symptoms, especially if they were frequent and less severe, can be recalled with any degree of accuracy using retrospective records, thereby introducing recall bias into these studies [91]. Preventing this is particularly important for transient symptoms of childhood infections, especially when we are interested in the prospective evolution of symptoms. This includes duration, intensity, and whether only one or multiple symptoms occurred [52]. Therefore, symptom diaries have been used for many decades. They produce more valid data, i.e. higher reporting and incidence rates thereby mitigating recall bias [13, 91, 92].
Causes of low symptom diary use in birth cohort studies
An overall aim of this review was to map birth cohorts that use(d) symptom diaries to identify respiratory diseases. Of the numerous birth cohort studies identified, relatively few really used a symptom diary to identify respiratory illness. Substantial administrative study efforts, the effort involved in data analysis, but also possible upcoming problems due to drop-out rates, could be possible barriers from the researchers’ point of view. In addition, filling out a daily symptom diary is a considerable burden for participants. Some studies show that, although the respondents themselves report good compliance, data collection protocols are often not followed, and a large number of missing records might occur [93, 94]. On the other hand, one reason for the rather infrequent use may be the risk of "hoarding", which is known as a problem where participants enter data into their diary retrospectively [93]. Unfortunately, hoarding is almost impossible to detect unless the time of data entry is recorded electronically. Weariness can also lead to a decline in diary completion rates over time [95]. It is therefore important to have a well-staffed and well-trained study team that can maintain good contact with the study participants to avoid missing data and drop-out.
This review shows that especially immediately after birth, when infants show a high susceptibility to respiratory illness, few studies use symptom diaries to record respiratory symptoms[96]. Because the immune system undergoes crucial developmental maturation during this time, detailed recording of all potential exposures, including infections, is crucial in understanding the development of the immune system and other outcomes. Most of the studies identified here were conducted in Europe, North America, and Australia, which may limit the generalizability of results and thus require more birth cohorts from other regions of the world.
Some studies retrieved either ARI, URTI or LRTI as respiratory outcomes from the symptom diary data, yet there is no consensus how to use the collected data in harmonized manner. This also makes it difficult to compare respiratory outcomes in this ScR. Additionally, most studies collected a broad range of environmental exposures, but only a few collected a broad range of biosamples. Nevertheless, biosamples are important because, they complement associations and research questions. For example, nasal swabs can be used to identify pathogens responsible for the development of ARI and to study them in relation to a specific combination of symptoms. Analysis of other biosamples, such as blood samples, can help to understand the immune system’s response to the development of ARI.
Strengths and limitations
To our knowledge, this scoping review is the first comprehensive attempt to summarize, map and compare birth cohort studies with symptom diary information for respiratory symptoms beginning from birth. The strength of our review is the comprehensive search of the literature. Our rather specific search strategy was comprehensively extended by a systematic search in four databases, an additional extensive search in registers and a very elaborate search in reference lists of the identified publications from all four databases. We assume that due to this extended search strategy the probability of having overlooked a birth cohort study with the use of symptom diaries from birth is low.
We also conducted additional searches of the gray literature to avoid omitting cohorts that had recently started. Finally, to ensure the accuracy of the extracted data, we contacted one or two authors of all included birth cohorts to confirm the extracted information or clarify, if questions remained open. Our study also had several limitations. It is possible that we failed to identify some cohort studies applying symptom diaries due to no uniform wording for symptom diaries. Not all birth cohort studies offer detailed cohort profiles, and information had to be collected in different publications. In addition, it may be possible that a birth cohort study could not be identified because it is neither registered in one of the web-based registers nor published in a way that met our search criteria. We hope that the broad search allowed to minimize these problems.
Conclusions
We have been able to provide a comprehensive review with all birth cohort studies that are suitable for providing a holistic understanding of the association of ARI as exposure with potential long-term sequelae in a life course perspective. We found 22 birth cohort studies that use(d) symptom diaries for respiratory infections. While, symptom diaries provide a powerful tool for prospective data collection, their long-term application is very challenging, so this is why it is not often applied. Our review shows that is possible and was done in several studies. Many questions related to the role on infections in the development of the immune system require information on symptom evolution and infection history over time. When combined with biosamples, this detailed information is very valuable. This overview helps to establish collaborations between researches in order to investigate the pattern, timing and sequence of respiratory infections and their association with the developing immune system and other exposures in a life-course perspective.
Supporting information
(DOCX)
Abbreviations
- ARI
Acute respiratory infection
- ScR
Scoping Review
- AUS
Australia
- CAN
Canada
- SWE
Sweden
- CHE
Switzerland
- FRA
France
- AUT
Austria
- EUR
Europe
- USA
United States of America
- DK
Denmark
- NLD
Netherlands
- FIN
Finland
- NIC
Nicaragua
- AUS
Australia
- TWN
Taiwan
- DEU
Germany
- RUS
Russia
- EST
Estonia
Data Availability
All relevant data are within the article, Table 2, and Table 3. This Scoping Review is based on purely descriptive data contained in these tables. The graphs are also based on the data in the tables. No other data are available. No mean values, standard deviations were reported, and no analysis in figures was carried out, only a purely qualitative evaluation with a few counts in the tables for the graph. All extracted information from each publication of the Scoping Review is reported in Table 2 and Table 3. There is no additional raw data.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Grüber C, Keil T, Kulig M, Roll S, Wahn U, Wahn V, et al. History of respiratory infections in the first 12 yr among children from a birth cohort. Pediatric Allergy and Immunology. 2008;19(6):505–12. doi: 10.1111/j.1399-3038.2007.00688.x [DOI] [PubMed] [Google Scholar]
- 2.Denny FW Jr. The clinical impact of human respiratory virus infections. Am J Respir Crit Care Med. 1995;152(4 Pt 2):S4–12. Epub 1995/10/01. doi: 10.1164/ajrccm/152.4_Pt_2.S4 . [DOI] [PubMed] [Google Scholar]
- 3.Thompson M, Vodicka TA, Blair PS, Buckley DI, Heneghan C, Hay AD. Duration of symptoms of respiratory tract infections in children: systematic review. BMJ. 2013;347:f7027. Epub 2013/12/18. doi: 10.1136/bmj.f7027 ; PubMed Central PMCID: PMC3898587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hay AD, Heron J, Ness A, team tAs. The prevalence of symptoms and consultations in pre-school children in the Avon Longitudinal Study of Parents and Children (ALSPAC): a prospective cohort study. Family Practice. 2005;22(4):367–74. doi: 10.1093/fampra/cmi035 [DOI] [PubMed] [Google Scholar]
- 5.Kusel MM, de Klerk N, Holt PG, Sly PD. Antibiotic use in the first year of life and risk of atopic disease in early childhood. Clin Exp Allergy. 2008;38(12):1921–8. Epub 2008/11/29. doi: 10.1111/j.1365-2222.2008.03138.x . [DOI] [PubMed] [Google Scholar]
- 6.Kusel MM, de Klerk N, Holt PG, Landau LI, Sly PD. Occurrence and management of acute respiratory illnesses in early childhood. J Paediatr Child Health. 2007;43(3):139–46. Epub 2007/02/24. doi: 10.1111/j.1440-1754.2007.01033.x . [DOI] [PubMed] [Google Scholar]
- 7.Fendrick AM, Monto AS, Nightengale B, Sarnes M. The economic burden of non-influenza-related viral respiratory tract infection in the United States. Arch Intern Med. 2003;163(4):487–94. Epub 2003/02/18. doi: 10.1001/archinte.163.4.487 . [DOI] [PubMed] [Google Scholar]
- 8.Hay AD, Anderson E, Ingle S, Beck C, Hollingworth W. Respiratory Tract Infections in Children in the Community: Prospective Online Inception Cohort Study. Ann Fam Med. 2019;17(1):14–22. Epub 2019/01/24. doi: 10.1370/afm.2327 ; PubMed Central PMCID: PMC6342588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Meel ER, Jaddoe VWV, Bønnelykke K, de Jongste JC, Duijts L. The role of respiratory tract infections and the microbiome in the development of asthma: A narrative review. Pediatr Pulmonol. 2017;52(10):1363–70. Epub 2017/09/05. doi: 10.1002/ppul.23795 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bartlett NW, McLean GR, Chang YS, Johnston SL. Genetics and epidemiology: asthma and infection. Curr Opin Allergy Clin Immunol. 2009;9(5):395–400. Epub 2009/08/01. doi: 10.1097/ACI.0b013e32833066fa . [DOI] [PubMed] [Google Scholar]
- 11.Lambert WE, Samet JM, Hunt WC, Skipper BJ, Schwab M, Spengler JD. Nitrogen dioxide and respiratory illness in children. Part II: Assessment of exposure to nitrogen dioxide. Res Rep Health Eff Inst. 1993;(58):33–50; discussion 1–80. Epub 1993/06/01. [PubMed] [Google Scholar]
- 12.Sarna M, Ware RS, Sloots TP, Nissen MD, Grimwood K, Lambert SB. The burden of community-managed acute respiratory infections in the first 2-years of life. Pediatr Pulmonol. 2016;51(12):1336–46. Epub 2016/05/27. doi: 10.1002/ppul.23480 . [DOI] [PubMed] [Google Scholar]
- 13.Verbrugge LM. Health diaries. Med Care. 1980;18(1):73–95. Epub 1980/01/01. doi: 10.1097/00005650-198001000-00006 . [DOI] [PubMed] [Google Scholar]
- 14.Poehling KA, Edwards KM, Weinberg GA, Szilagyi P, Staat MA, Iwane MK, et al. The Underrecognized Burden of Influenza in Young Children. New England Journal of Medicine. 2006;355(1):31–40. doi: 10.1056/NEJMoa054869 . [DOI] [PubMed] [Google Scholar]
- 15.Hodge B. The use of symptom diaries in outpatient care. Family practice management. 2013;20(3):24–8. Epub 2013/08/14. . [PubMed] [Google Scholar]
- 16.Samet JM, Lambert WE, Skipper BJ, Cushing AH, Hunt WC, Young SA, et al. Nitrogen dioxide and respiratory illnesses in infants. Am Rev Respir Dis. 1993;148(5):1258–65. Epub 1993/11/01. doi: 10.1164/ajrccm/148.5.1258 . [DOI] [PubMed] [Google Scholar]
- 17.Subbarao P, Anand SS, Becker AB, Befus AD, Brauer M, Brook JR, et al. The Canadian Healthy Infant Longitudinal Development (CHILD) Study: examining developmental origins of allergy and asthma. Thorax. 2015;70(10):998–1000. Epub 2015/06/13. doi: 10.1136/thoraxjnl-2015-207246 . [DOI] [PubMed] [Google Scholar]
- 18.Asher MI, Keil U, Anderson HR, Beasley R, Crane J, Martinez F, et al. International Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur Respir J. 1995;8(3):483–91. Epub 1995/03/01. doi: 10.1183/09031936.95.08030483 . [DOI] [PubMed] [Google Scholar]
- 19.Caudri D, Wijga A, Scholtens S, Kerkhof M, Gerritsen J, Ruskamp JM, et al. Early daycare is associated with an increase in airway symptoms in early childhood but is no protection against asthma or atopy at 8 years. Am J Respir Crit Care Med. 2009;180(6):491–8. Epub 2009/06/23. doi: 10.1164/rccm.200903-0327OC . [DOI] [PubMed] [Google Scholar]
- 20.Clarisse B, Nikasinovic L, Poinsard R, Just J, Momas I. The Paris prospective birth cohort study: which design and who participates? Eur J Epidemiol. 2007;22(3):203–10. Epub 2007/02/07. doi: 10.1007/s10654-007-9109-2 . [DOI] [PubMed] [Google Scholar]
- 21.Larkin EK, Gebretsadik T, Moore ML, Anderson LJ, Dupont WD, Chappell JD, et al. Objectives, design and enrollment results from the Infant Susceptibility to Pulmonary Infections and Asthma Following RSV Exposure Study (INSPIRE). BMC Pulm Med. 2015;15:45. Epub 2015/05/30. doi: 10.1186/s12890-015-0040-0 ; PubMed Central PMCID: PMC4506623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schooling CM, Hui LL, Ho LM, Lam TH, Leung GM. Cohort profile: ’children of 1997’: a Hong Kong Chinese birth cohort. International journal of epidemiology. 2012;41(3):611–20. Epub 2011/01/13. doi: 10.1093/ije/dyq243 . [DOI] [PubMed] [Google Scholar]
- 23.Monto AS, Napier JA, Metzner HL. The Tecumseh study of respiratory illness. I. Plan of study and observations on syndromes of acute respiratory disease. Am J Epidemiol. 1971;94(3):269–79. Epub 1971/09/01. doi: 10.1093/oxfordjournals.aje.a121320 . [DOI] [PubMed] [Google Scholar]
- 24.Zoch B, Karch A, Dreesman J, Monazahian M, Baillot A, Mikolajczyk RT. Feasibility of a birth cohort study dedicated to assessing acute infections using symptom diaries and parental collection of biomaterials. BMC infectious diseases. 2015;15. ARTN 436 doi: 10.1186/s12879-015-1189-0 WOS:000363099400001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bousquet J, Gern JE, Martinez FD, Anto JM, Johnson CC, Holt PG, et al. Birth cohorts in asthma and allergic diseases: report of a NIAID/NHLBI/MeDALL joint workshop. The Journal of allergy and clinical immunology. 2014;133(6):1535–46. Epub 03/15. doi: 10.1016/j.jaci.2014.01.018 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grosser A, Razum O, Vrijkotte TGM, Hinz I-M, Spallek J. Inclusion of migrants and ethnic minorities in European birth cohort studies—a scoping review. European Journal of Public Health. 2016;26(6):984–91. doi: 10.1093/eurpub/ckw068 [DOI] [PubMed] [Google Scholar]
- 27.Silvestri M, Franchi S, Pistorio A, Petecchia L, Rusconi F. Smoke exposure, wheezing, and asthma development: a systematic review and meta-analysis in unselected birth cohorts. Pediatr Pulmonol. 2015;50(4):353–62. Epub 2014/03/22. doi: 10.1002/ppul.23037 . [DOI] [PubMed] [Google Scholar]
- 28.Leder K, Sinclair MI, Mitakakis TZ, Hellard ME, Forbes A. A community-based study of respiratory episodes in Melbourne, Australia. Aust N Z J Public Health. 2003;27(4):399–404. Epub 2004/01/07. doi: 10.1111/j.1467-842x.2003.tb00416.x . [DOI] [PubMed] [Google Scholar]
- 29.Townsend ML, Riepsamen A, Georgiou C, Flood VM, Caputi P, Wright IM, et al. Longitudinal Intergenerational Birth Cohort Designs: A Systematic Review of Australian and New Zealand Studies. PloS one. 2016;11(3):e0150491–e. doi: 10.1371/journal.pone.0150491 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bowatte G, Lodge C, Lowe AJ, Erbas B, Perret J, Abramson MJ, et al. The influence of childhood traffic-related air pollution exposure on asthma, allergy and sensitization: a systematic review and a meta-analysis of birth cohort studies. Allergy. 2015;70(3):245–56. Epub 2014/12/17. doi: 10.1111/all.12561 . [DOI] [PubMed] [Google Scholar]
- 31.Campbell A, Rudan I. Systematic review of birth cohort studies in Africa. Journal of global health. 2011;1(1):46–58. . [PMC free article] [PubMed] [Google Scholar]
- 32.Al-Rifai RH, Ali N, Barigye ET, Al Haddad AHI, Al-Maskari F, Loney T, et al. Maternal and birth cohort studies in the Gulf Cooperation Council countries: a systematic review and meta-analysis. Syst Rev. 2020;9(1):14. Epub 2020/01/18. doi: 10.1186/s13643-020-1277-0 ; PubMed Central PMCID: PMC6964097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Annals of Internal Medicine. 2018;169(7):467–73. doi: 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 34.Van Benten I, Koopman L, Niesters B, Hop W, Van Middelkoop B, De Waal L, et al. Predominance of rhinovirus in the nose of symptomatic and asymptomatic infants. Pediatric Allergy and Immunology. 2003;14(5):363–70. doi: 10.1034/j.1399-3038.2003.00064.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Group TS. The Environmental Determinants of Diabetes in the Young (TEDDY) Study. Annals of the New York Academy of Sciences. 2008;1150:1–13. doi: 10.1196/annals.1447.062 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cushing AH, Samet JM, Lambert WE, Skipper BJ, Hunt WC, Young SA, et al. Breastfeeding Reduces Risk of Respiratory Illness in Infants. American Journal of Epidemiology. 1998;147(9):863–70. doi: 10.1093/oxfordjournals.aje.a009540 [DOI] [PubMed] [Google Scholar]
- 37.von Linstow ML, Høgh M, Nordbø SA, Eugen-Olsen J, Koch A, Høgh B. A community study of clinical traits and risk factors for human metapneumovirus and respiratory syncytial virus infection during the first year of life. Eur J Pediatr. 2008;167(10):1125–33. Epub 2008/01/04. doi: 10.1007/s00431-007-0643-4 ; PubMed Central PMCID: PMC7086915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.DOUGLAS RM, WOODWARD A, MILES H, BUETOW S, MORRIS D. A Prospective Study of Proneness to Acute Respiratory Illness in the First Two Years of Life. International journal of epidemiology. 1994;23(4):818–26. doi: 10.1093/ije/23.4.818 [DOI] [PubMed] [Google Scholar]
- 39.Gresh L, Kuan G, Sanchez N, Azziz-Baumgartner E, Ojeda S, Melendez M, et al. Burden of Influenza and Influenza-associated Pneumonia in the First Year of Life in a Prospective Cohort Study in Managua, Nicaragua. Pediatr Infect Dis J. 2016;35(2):152–6. Epub 2015/10/01. doi: 10.1097/INF.0000000000000944 ; PubMed Central PMCID: PMC4711382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lagström H, Rautava P, Kaljonen A, Räihä H, Pihlaja P, Korpilahti P, et al. Cohort profile: Steps to the healthy development and well-being of children (the STEPS Study). International journal of epidemiology. 2013;42(5):1273–84. Epub 2012/11/13. doi: 10.1093/ije/dys150 . [DOI] [PubMed] [Google Scholar]
- 41.Dales R, Ruest K, Guay M, Marro L, David Miller J. Residential fungal growth and incidence of acute respiratory illness during the first two years of life. Environmental Research. 2010;110(7):692–8. doi: 10.1016/j.envres.2010.07.007 [DOI] [PubMed] [Google Scholar]
- 42.Wald ER, Guerra N, Byers C. Frequency and severity of infections in day care: three-year follow-up. J Pediatr. 1991;118(4 Pt 1):509–14. Epub 1991/04/01. doi: 10.1016/s0022-3476(05)83370-0 [DOI] [PubMed] [Google Scholar]
- 43.Kozyrskyj AL, Kendall GE, Jacoby P, Sly PD, Zubrick SR. Association between socioeconomic status and the development of asthma: analyses of income trajectories. Am J Public Health. 2010;100(3):540–6. Epub 2009/08/22. doi: 10.2105/AJPH.2008.150771 ; PubMed Central PMCID: PMC2820073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Oddy WH, de Klerk NH, Sly PD, Holt PG. The effects of respiratory infections, atopy, and breastfeeding on childhood asthma. Eur Respir J. 2002;19(5):899–905. Epub 2002/05/28. doi: 10.1183/09031936.02.00103602 . [DOI] [PubMed] [Google Scholar]
- 45.Straker L, Mountain J, Jacques A, White S, Smith A, Landau L, et al. Cohort Profile: The Western Australian Pregnancy Cohort (Raine) Study-Generation 2. International journal of epidemiology. 2017;46(5):1384–5j. Epub 2017/01/09. doi: 10.1093/ije/dyw308 ; PubMed Central PMCID: PMC5837608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Straker LM, Hall GL, Mountain J, Howie EK, White E, McArdle N, et al. Rationale, design and methods for the 22 year follow-up of the Western Australian Pregnancy Cohort (Raine) Study. BMC Public Health. 2015;15:663. Epub 2015/07/15. doi: 10.1186/s12889-015-1944-6 ; PubMed Central PMCID: PMC4501054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kusel MMH, de Klerk NH, Holt PG, Kebadze T, Johnston SL, Sly PD. Role of Respiratory Viruses in Acute Upper and Lower Respiratory Tract Illness in the First Year of Life: A Birth Cohort Study. The Pediatric infectious disease journal. 2006;25(8). doi: 10.1097/01.inf.0000226912.88900.a3 [DOI] [PubMed] [Google Scholar]
- 48.Dales R, Miller D, Ruest K, Guay M, Judek S. Airborne endotoxin is associated with respiratory illness in the first 2 years of life. Environmental health perspectives. 2006;114(4):610–4. doi: 10.1289/ehp.8142 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hesselmar B, Saalman R, Rudin A, Adlerberth I, Wold A. Early fish introduction is associated with less eczema, but not sensitization, in infants. Acta Paediatr. 2010;99(12):1861–7. Epub 2010/07/31. doi: 10.1111/j.1651-2227.2010.01939.x . [DOI] [PubMed] [Google Scholar]
- 50.Hesselmar B, Hicke-Roberts A, Lundell AC, Adlerberth I, Rudin A, Saalman R, et al. Pet-keeping in early life reduces the risk of allergy in a dose-dependent fashion. PLoS One. 2018;13(12):e0208472. Epub 2018/12/20. doi: 10.1371/journal.pone.0208472 ; PubMed Central PMCID: PMC6300190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bisgaard H. The Copenhagen Prospective Study on Asthma in Childhood (COPSAC): design, rationale, and baseline data from a longitudinal birth cohort study. Ann Allergy Asthma Immunol. 2004;93(4):381–9. Epub 2004/11/04. doi: 10.1016/S1081-1206(10)61398-1 . [DOI] [PubMed] [Google Scholar]
- 52.Bisgaard H, Pipper CB, Bønnelykke K. Endotyping early childhood asthma by quantitative symptom assessment. J Allergy Clin Immunol. 2011;127(5):1155–64.e2. Epub 2011/03/29. doi: 10.1016/j.jaci.2011.02.007 . [DOI] [PubMed] [Google Scholar]
- 53.Arabkhazaeli A, Ahmadizar F, Leusink M, Arets HGM, Raaijmakers JAM, Uiterwaal C, et al. The association between a genetic risk score for allergy and the risk of developing allergies in childhood-Results of the WHISTLER cohort. Pediatric allergy and immunology: official publication of the European Society of Pediatric Allergy and Immunology. 2018;29(1):72–7. Epub 2017/10/20. doi: 10.1111/pai.12824 . [DOI] [PubMed] [Google Scholar]
- 54.de Hoog ML, Venekamp RP, van der Ent CK, Schilder A, Sanders EA, Damoiseaux RA, et al. Impact of early daycare on healthcare resource use related to upper respiratory tract infections during childhood: prospective WHISTLER cohort study. BMC Med. 2014;12:107. Epub 2014/06/27. doi: 10.1186/1741-7015-12-107 ; PubMed Central PMCID: PMC4098954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Katier N, Uiterwaal CS, de Jong BM, Kimpen JL, Verheij TJ, Grobbee DE, et al. The Wheezing Illnesses Study Leidsche Rijn (WHISTLER): rationale and design. Eur J Epidemiol. 2004;19(9):895–903. Epub 2004/10/27. doi: 10.1023/b:ejep.0000040530.98310.0c ; PubMed Central PMCID: PMC7087709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Prins-van Ginkel AC, de Hoog MLA, Uiterwaal C, Smit HA, Bruijning-Verhagen PC. Detecting Acute Otitis Media Symptom Episodes Using a Mobile App: Cohort Study. JMIR mHealth and uHealth. 2017;5(11):e181–e. doi: 10.2196/mhealth.7505 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zomer-Kooijker K, Uiterwaal CS, van der Gugten AC, Wilbrink B, Bont LJ, van der Ent CK. Decreased lung function precedes severe respiratory syncytial virus infection and post-respiratory syncytial virus wheeze in term infants. Eur Respir J. 2014;44(3):666–74. Epub 2014/07/06. doi: 10.1183/09031936.00009314 . [DOI] [PubMed] [Google Scholar]
- 58.Bergroth E, Remes S, Pekkanen J, Kauppila T, Büchele G, Keski-Nisula L. Respiratory tract illnesses during the first year of life: effect of dog and cat contacts. Pediatrics. 2012;130(2):211–20. Epub 2012/07/11. doi: 10.1542/peds.2011-2825 . [DOI] [PubMed] [Google Scholar]
- 59.Loss G, Bitter S, Wohlgensinger J, Frei R, Roduit C, Genuneit J, et al. Prenatal and early-life exposures alter expression of innate immunity genes: the PASTURE cohort study. J Allergy Clin Immunol. 2012;130(2):523–30.e9. Epub 2012/08/01. doi: 10.1016/j.jaci.2012.05.049 . [DOI] [PubMed] [Google Scholar]
- 60.von Mutius E, Schmid S. The PASTURE project: EU support for the improvement of knowledge about risk factors and preventive factors for atopy in Europe. Allergy. 2006;61(4):407–13. Epub 2006/03/04. doi: 10.1111/j.1398-9995.2006.01009.x . [DOI] [PubMed] [Google Scholar]
- 61.von Linstow ML, Holst KK, Larsen K, Koch A, Andersen PK, Høgh B. Acute respiratory symptoms and general illness during the first year of life: a population-based birth cohort study. Pediatr Pulmonol. 2008;43(6):584–93. Epub 2008/04/26. doi: 10.1002/ppul.20828 . [DOI] [PubMed] [Google Scholar]
- 62.von Linstow ML, Høgh M, Høgh B. Clinical and epidemiologic characteristics of human bocavirus in Danish infants: results from a prospective birth cohort study. Pediatr Infect Dis J. 2008;27(10):897–902. Epub 2008/08/30. doi: 10.1097/INF.0b013e3181757b16 . [DOI] [PubMed] [Google Scholar]
- 63.Lönnrot M, Lynch K, Larsson HE, Lernmark Å, Rewers M, Hagopian W, et al. A method for reporting and classifying acute infectious diseases in a prospective study of young children: TEDDY. BMC pediatrics. 2015;15:24. Epub 2015/04/18. doi: 10.1186/s12887-015-0333-8 ; PubMed Central PMCID: PMC4377063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rewers M, Hyöty H, Lernmark Å, Hagopian W, She JX, Schatz D, et al. The Environmental Determinants of Diabetes in the Young (TEDDY) Study: 2018 Update. Curr Diab Rep. 2018;18(12):136. Epub 2018/10/26. doi: 10.1007/s11892-018-1113-2 ; PubMed Central PMCID: PMC6415767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fairchok MP, Martin ET, Chambers S, Kuypers J, Behrens M, Braun LE, et al. Epidemiology of viral respiratory tract infections in a prospective cohort of infants and toddlers attending daycare. J Clin Virol. 2010;49(1):16–20. Epub 2010/07/24. doi: 10.1016/j.jcv.2010.06.013 ; PubMed Central PMCID: PMC7108368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Martin ET, Fairchok MP, Kuypers J, Magaret A, Zerr DM, Wald A, et al. Frequent and prolonged shedding of bocavirus in young children attending daycare. The Journal of infectious diseases. 2010;201(11):1625–32. doi: 10.1086/652405 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Martin ET, Fairchok MP, Stednick ZJ, Kuypers J, Englund JA. Epidemiology of multiple respiratory viruses in childcare attendees. J Infect Dis. 2013;207(6):982–9. Epub 2013/01/05. doi: 10.1093/infdis/jis934 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Belderbos ME, Houben ML, van Bleek GM, Schuijff L, van Uden NO, Bloemen-Carlier EM, et al. Breastfeeding modulates neonatal innate immune responses: a prospective birth cohort study. Pediatric allergy and immunology: official publication of the European Society of Pediatric Allergy and Immunology. 2012;23(1):65–74. Epub 2011/11/23. doi: 10.1111/j.1399-3038.2011.01230.x . [DOI] [PubMed] [Google Scholar]
- 69.Belderbos ME, Knol EF, Houben ML, van Bleek GM, Wilbrink B, Kimpen JL, et al. Low neonatal Toll-like receptor 4-mediated interleukin-10 production is associated with subsequent atopic dermatitis. Clin Exp Allergy. 2012;42(1):66–75. Epub 2011/11/19. doi: 10.1111/j.1365-2222.2011.03857.x . [DOI] [PubMed] [Google Scholar]
- 70.Houben ML, Bont L, Wilbrink B, Belderbos ME, Kimpen JL, Visser GH, et al. Clinical prediction rule for RSV bronchiolitis in healthy newborns: prognostic birth cohort study. Pediatrics. 2011;127(1):35–41. Epub 2010/12/29. doi: 10.1542/peds.2010-0581 . [DOI] [PubMed] [Google Scholar]
- 71.Houben ML, Coenjaerts FE, Rossen JW, Belderbos ME, Hofland RW, Kimpen JL, et al. Disease severity and viral load are correlated in infants with primary respiratory syncytial virus infection in the community. J Med Virol. 2010;82(7):1266–71. Epub 2010/06/01. doi: 10.1002/jmv.21771 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nylund A, Toivonen L, Korpilahti P, Kaljonen A, Peltola V, Rautakoski P. Recurrent respiratory tract infections or acute otitis media were not a risk factor for vocabulary development in children at 13 and 24 months of age. Acta Paediatr. 2019;108(2):288–94. Epub 2018/08/21. doi: 10.1111/apa.14546 . [DOI] [PubMed] [Google Scholar]
- 73.Peltola V, Teros-Jaakkola T, Rulli M, Toivonen L, Broberg E, Waris M, et al. Pandemic influenza A (H1N1) virus in households with young children. Influenza and other respiratory viruses. 2012;6(3):e21–e4. Epub 09/23. doi: 10.1111/j.1750-2659.2011.00289.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schuez-Havupalo L, Toivonen L, Karppinen S, Kaljonen A, Peltola V. Daycare attendance and respiratory tract infections: a prospective birth cohort study. BMJ Open. 2017;7(9):e014635. doi: 10.1136/bmjopen-2016-014635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Toivonen L, Karppinen S, Schuez-Havupalo L, Teros-Jaakkola T, Vuononvirta J, Mertsola J, et al. Burden of Recurrent Respiratory Tract Infections in Children: A Prospective Cohort Study. Pediatr Infect Dis J. 2016;35(12):e362–e9. Epub 2016/07/28. doi: 10.1097/INF.0000000000001304 . [DOI] [PubMed] [Google Scholar]
- 76.Bisgaard H, Vissing NH, Carson CG, Bischoff AL, Følsgaard NV, Kreiner-Møller E, et al. Deep phenotyping of the unselected COPSAC2010 birth cohort study. Clin Exp Allergy. 2013;43(12):1384–94. Epub 2013/10/15. doi: 10.1111/cea.12213 ; PubMed Central PMCID: PMC4158856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Peet A, Kool P, Ilonen J, Knip M, Tillmann V. Birth weight in newborn infants with different diabetes-associated HLA genotypes in three neighbouring countries: Finland, Estonia and Russian Karelia. Diabetes/metabolism research and reviews. 2012;28(5):455–61. Epub 2012/04/12. doi: 10.1002/dmrr.2303 . [DOI] [PubMed] [Google Scholar]
- 78.Seppälä EM, Oikarinen S, Lehtonen JP, Neupane S, Honkanen H, Tyni I, et al. Association of Picornavirus Infections With Acute Otitis Media in a Prospective Birth Cohort Study. The Journal of infectious diseases. 2020;222(2):324–32. doi: 10.1093/infdis/jiaa087 [DOI] [PubMed] [Google Scholar]
- 79.Simre K, Uibo O, Peet A, Tillmann V, Kool P, Hämäläinen AM, et al. Exploring the risk factors for differences in the cumulative incidence of coeliac disease in two neighboring countries: the prospective DIABIMMUNE study. Digestive and liver disease: official journal of the Italian Society of Gastroenterology and the Italian Association for the Study of the Liver. 2016;48(11):1296–301. Epub 2016/10/25. doi: 10.1016/j.dld.2016.06.029 . [DOI] [PubMed] [Google Scholar]
- 80.Vatanen T, Plichta DR, Somani J, Münch PC, Arthur TD, Hall AB, et al. Genomic variation and strain-specific functional adaptation in the human gut microbiome during early life. Nature Microbiology. 2019;4(3):470–9. doi: 10.1038/s41564-018-0321-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lambert SB, Ware RS, Cook AL, Maguire FA, Whiley DM, Bialasiewicz S, et al. Observational Research in Childhood Infectious Diseases (ORChID): a dynamic birth cohort study. BMJ Open. 2012;2(6):e002134. doi: 10.1136/bmjopen-2012-002134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sarna M, Lambert SB, Sloots TP, Whiley DM, Alsaleh A, Mhango L, et al. Viruses causing lower respiratory symptoms in young children: findings from the ORChID birth cohort. Thorax. 2018;73(10):969–79. Epub 2017/12/17. doi: 10.1136/thoraxjnl-2017-210233 ; PubMed Central PMCID: PMC6166599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sarna M, Ware RS, Lambert SB, Sloots TP, Nissen MD, Grimwood K. Timing of First Respiratory Virus Detections in Infants: A Community-Based Birth Cohort Study. J Infect Dis. 2018;217(3):418–27. Epub 2017/11/23. doi: 10.1093/infdis/jix599 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gordon A, Kuan G, Aviles W, Sanchez N, Ojeda S, Lopez B, et al. The Nicaraguan pediatric influenza cohort study: design, methods, use of technology, and compliance. BMC infectious diseases. 2015;15:504. Epub 2015/11/11. doi: 10.1186/s12879-015-1256-6 ; PubMed Central PMCID: PMC4640204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tsai MH, Chiu CY, Shih HJ, Liao SL, Hua MC, Huang SH, et al. Longitudinal investigation of nasopharyngeal methicillin-resistant Staphylococcus aureus colonization in early infancy: The PATCH birth cohort study. Clinical Microbiology and Infection. 2017;23(2):121.e1–.e7. doi: 10.1016/j.cmi.2016.10.020 [DOI] [PubMed] [Google Scholar]
- 86.Tsai M-H, Huang S-H, Chen C-L, Chiu C-Y, Hua M-C, Liao S-L, et al. Pathogenic Bacterial Nasopharyngeal Colonization and Its Impact on Respiratory Diseases in the First Year of Life: The PATCH Birth Cohort Study. The Pediatric infectious disease journal. 2015;34(6):652–8. doi: 10.1097/INF.0000000000000688 00006454-201506000-00023. [DOI] [PubMed] [Google Scholar]
- 87.Gottschick C, Raupach-Rosin H, Langer S, Hassan L, Horn J, Dorendorf E, et al. Cohort Profile: The LoewenKIDS Study–life-course perspective on infections, the microbiome and the development of the immune system in early childhood. International journal of epidemiology. 2019;48(4):1042–3h. doi: 10.1093/ije/dyz001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cantwell LB, Henao OL, Hoekstra RM, Scallan E. The effect of different recall periods on estimates of acute gastroenteritis in the United States, FoodNet Population Survey 2006–2007. Foodborne pathogens and disease. 2010;7(10):1225–8. Epub 2010/06/29. doi: 10.1089/fpd.2010.0567 . [DOI] [PubMed] [Google Scholar]
- 89.Viviani L, van der Es M, Irvine L, Tam CC, Rodrigues LC, Jackson KA, et al. Estimating the Incidence of Acute Infectious Intestinal Disease in the Community in the UK: A Retrospective Telephone Survey. PLoS One. 2016;11(1):e0146171. Epub 2016/01/26. doi: 10.1371/journal.pone.0146171 ; PubMed Central PMCID: PMC4725772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Schlinkmann KM, Bakuli A, Mikolajczyk R. Incidence and comparison of retrospective and prospective data on respiratory and gastrointestinal infections in German households. BMC infectious diseases. 2017;17(1):336. Epub 2017/05/12. doi: 10.1186/s12879-017-2434-5 ; PubMed Central PMCID: PMC5426066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Freer CB. Health diaries: a method of collecting health information. J R Coll Gen Pract. 1980;30(214):279–82. . [PMC free article] [PubMed] [Google Scholar]
- 92.Anwar M, Green JA, Norris P, Bukhari NI. Prospective daily diary study reporting of any and all symptoms in healthy adults in Pakistan: prevalence and response. BMJ Open. 2017;7(11):e014998. doi: 10.1136/bmjopen-2016-014998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Stone AA, Shiffman S, Schwartz JE, Broderick JE, Hufford MR. Patient non-compliance with paper diaries. BMJ (Clinical research ed). 2002;324(7347):1193–4. doi: 10.1136/bmj.324.7347.1193 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hyland ME, Kenyon CA, Allen R, Howarth P. Diary keeping in asthma: comparison of written and electronic methods. BMJ (Clinical research ed). 1993;306(6876):487–9. Epub 1993/02/20. doi: 10.1136/bmj.306.6876.487 PubMed Central PMCID: PMC1676776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.McColl E. Best practice in symptom assessment: a review. Gut. 2004;53(suppl 4):iv49–iv54. doi: 10.1136/gut.2003.034355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gallacher DJ, Hart K, Kotecha S. Common respiratory conditions of the newborn. Breathe (Sheff). 2016;12(1):30–42. doi: 10.1183/20734735.000716 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
All relevant data are within the article, Table 2, and Table 3. This Scoping Review is based on purely descriptive data contained in these tables. The graphs are also based on the data in the tables. No other data are available. No mean values, standard deviations were reported, and no analysis in figures was carried out, only a purely qualitative evaluation with a few counts in the tables for the graph. All extracted information from each publication of the Scoping Review is reported in Table 2 and Table 3. There is no additional raw data.