Abstract
Objective:
This study evaluates associations between neighborhood-level characteristics and gestational weight gain (GWG) in a population-level study of 2015 New York City births.
Methods:
Generalized linear mixed effects models were used to estimate odds ratios for associations between neighborhood-level characteristics (poverty, food environment, walkability) within 1-km of residential Census block centroid and excessive or inadequate GWG as compared to recommended GWG. All models were adjusted for individual-level sociodemographic characteristics.
Results:
Among the sample of 106,285 births, 41.8% had excessive GWG and 26.3% had inadequate GWG. Residence the highest versus lowest quartile of neighborhood poverty was associated with greater odds of excessive GWG (OR 1.17, 95% CI 1.08, 1.26). Residence in neighborhoods in the quartile of highest walkability compared with the quartile of lowest walkability was associated with lower odds of excessive GWG (OR 0.87, 95% CI 0.81, 0.93). Adjustment for prepregnancy BMI attenuated the associations for neighborhood poverty, but not for walkability. Neighborhood variables were not associated with inadequate GWG.
Conclusions:
These analyses indicate that greater neighborhood walkability is associated with lower odds of excessive GWG, potentially from differences in pedestrian activity during pregnancy. This research provides further evidence for using urban design to support healthy weight status during pregnancy.
Keywords: Gestational weight gain, pregnancy, cross-sectional studies, neighborhood, New York City
1. Introduction
Excessive or inadequate weight gain during pregnancy poses numerous health risks for both pregnant individuals and children.1–6 Inadequate GWG increases the risk of infant mortality, preterm birth and small-for-gestational-age (SGA).1,2 Excessive GWG is associated with higher risk of pregnancy complications, including pregnancy-related hypertension and greater long-term postpartum weight retention.2–4 Excessive GWG is also associated with increased odds of child asthma, obesity, and greater percent body fat and abdominal adiposity.5,6
In 2009, the Institute of Medicine (IOM) issued revised recommendations for gestational weight gain (GWG) based on prepregnancy body-mass index (BMI) categories.7 However, despite the new guidelines, most pregnant individuals in the U.S. still do not gain the recommended amount of weight during pregnancy. Estimates from 2011 show that almost 50% of pregnant individuals gain excess weight during pregnancy, while 21% do not gain enough.8 Prepregnancy BMI is strongly associated with GWG outside the recommendations, particularly for those with higher BMI values, as the recommended weight gain ranges are lower.8
Given the health implications of GWG outside of recommended ranges and the large body of evidence relating neighborhood characteristics to diet, physical activity and weight, more research on environmental factors that support healthy GWG is critical. Of the relatively few studies relating neighborhood factors to GWG, several have shown neighborhood socioeconomic disadvantage to be associated with both inadequate and excessive GWG, while others have found no association.9–12 Even rarer are studies examining the relationship across multiple neighborhood domains and GWG.
While research on environmental factors and GWG is limited, such studies can draw on a much larger literature relating neighborhood features to health in the general population. Numerous studies, evaluating both neighborhood walkability features (e.g. population density, land use mix, density of public transit infrastructure, pedestrian-friendly design, proportion of residents who walk to work) and multi-dimensional walkability indices have found an association between higher walkability and lower BMI or risk of overweight/obesity.13–20 While evidence also supports a relationship between healthfulness of the neighborhood food environment and BMI or risk of overweight/obesity, the findings in this area are not as strong and the direction of association is less consistent. Living closer to food retail has been associated in some studies with decreased BMI.21–23 Higher density of healthy food retail has also been associated with lower BMI, even after controlling for neighborhood walkability, population density and land-use mix.17,24 However, while some studies have found unhealthy food retail density to be associated with higher BMI, particularly for those without car access, others have found no effect.17,24,25
Using a large population of more than 110,000 New York City (NYC) birth records from 2015, we investigated associations between neighborhood-level features previously shown to predict BMI in the general population – poverty rate, healthy and unhealthy retail food environments, and neighborhood walkability – and inadequate and excessive GWG. We hypothesized that lower poverty rates, healthier food environments and more walkable neighborhoods would all be associated with lower odds of unhealthy GWG.
2. METHODS
2.1. Data
This study used NYC Department of Health and Mental Hygiene (DOHMH) Bureau of Vital Statistics birth record data for the year 2015 to examine neighborhood-level risk factors for GWG. Using medical record data, the DOHMH compiles data on all live births in NYC, including basic health and demographic information for the pregnant individual and birth outcome statistics (e.g. birthweight, gestational age).
2.2. Cohort Selection
The analyses included data from 110,744 births reported in the 2015 NYC Vital Statistics records. We excluded all observations missing the pregnant individual’s height or weight data, either prepregnancy or at time of birth (less than 0.6%, n=694). We also excluded observations with multiple births (n=3,746) and with an implausible prepregnancy BMI (n=6), which was defined as BMI <12 or >70. Lastly, we excluded observations missing neighborhood data (n=13). Table 1 provides sample characteristics for the final analytic sample of 106,285 births.
Table 1.
Sample Characteristics for Pregnant Individuals
| IOM Gestational Weight Gain Levels | ||||
|---|---|---|---|---|
| Total (n=106,285) | Inadequate (n=27,990) | Recommended (n=33,887) | Excessive (n=44,408) | |
| No. (%) | No. (%) | No. (%) | No. (%) | |
|
| ||||
| Age in Years, mean (SD) | 29.91 (±6.0) | 30.00 (±6.2) | 30.15 (±5.9) | 29.85 (±5.9) |
| Married | 62,760 (59.1) | 17,138 (61.2) | 21,445 (63.3) | 24,177 (54.4) |
| Education | ||||
| Some High School | 20,702 (19.5) | 6,480 (23.2) | 6,244 (18.4) | 7,978 (18.0) |
| High School Grad | 24,360 (22.9) | 6,825 (24.4) | 7,528 (22.2) | 10,007 (22.5) |
| Some College | 17,039 (16.0) | 3,869 (13.8) | 4,953 (14.6) | 8,217 (18.5) |
| Associate's | 7,098 (6.7) | 1,534 (5.5) | 2,176 (6.4) | 3,388 (7.6) |
| Bachelor's | 20,742 (19.5) | 5,082 (18.2) | 7,062 (20.8) | 8,598 (19.4) |
| Master's | 12,225 (11.5) | 3,110 (11.1) | 4,362 (12.9) | 4,753 (10.7) |
| Doctorate/Prof Degree | 3,889 (2.7) | 1,011 (3.6) | 1,505 (4.4) | 1,373 (3.1) |
| Missing | 230 (0.2) | 79 (0.3) | 57 (0.2) | 94 (0.2) |
| Race/Ethnicity | ||||
| Puerto Rican | 6,868 (6.5) | 1,521 (5.4) | 1,714 (5.1) | 3,633 (8.2) |
| Other Hispanic | 25,800 (24.3) | 6,655 (23.8) | 7,872 (23.2) | 11,273 (25.4) |
| Asian/Pacific Islander | 18,166 (17.1) | 5,812 (20.8) | 6,573 (19.4) | 5,781 (13.0) |
| White Non-Hispanic | 33,149 (31.2) | 8,671 (31.0) | 11,669 (34.4) | 12,809 (28.8) |
| Black Non-Hispanic | 20,754 (19.5) | 4,875 (17.4) | 5,619 (16.6) | 10,260 (23.1) |
| Other/Mixed Race Non-Hispanic | 1,519 (1.4) | 447 (1.6) | 432 (1.3) | 640 (1.4) |
| Missing | 29 (<0.1) | 9 (<0.1) | 8 (<0.1) | 12 (<0.1) |
| Foreign Born | 56,678 (53.3) | 16,169 (57.8) | 18,640 (55.0) | 21,869 (49.3) |
| Missing | 23 (<0.1) | 13 (<0.1) | 6 (<0.1) | 4 (<0.1) |
| WIC* | 55,641 (52.4) | 15,040 (53.7) | 16,845 (49.7) | 23,756 (53.5) |
| Missing | 466 (0.4) | 134 (0.5) | 146 (0.4) | 186 (0.4) |
| Pre-pregnancy BMI Category | ||||
| Underweight | 6,065 (5.7) | 2,176 (7.8) | 2,625 (7.8) | 1,264 (2.9) |
| Normal | 56,060 (52.7) | 18,380 (65.7) | 20,737 (61.2) | 16,943 (38.2) |
| Overweight | 25,876 (24.4) | 4,207 (15.0) | 7,193 (21.2) | 14,476 (32.6) |
| Obese 1 | 11,644 (11.0) | 1,697 (6.1) | 2,118 (6.3) | 7,829 (17.6) |
| Obese 2 | 4,331 (4.1) | 899 (3.2) | 792 (2.3) | 2,640 (5.9) |
| Obese 3 | 2,309 (2.2) | 631 (2.3) | 422 (1.3) | 1,256 (2.8) |
| Total Gestational Weight Gain in kg, mean (SD) | 13.36 (±6.0) | 7.28 (±3.6) | 12.35 (±2.8) | 17.96 (±5.2) |
| Previous Livebirths | ||||
| 0 | 47,182 (44.4) | 11,427 (40.8) | 15,138 (44.7) | 20,617 (46.4) |
| 1 | 32,550 (30.6) | 8,940 (31.9) | 10,577 (31.2) | 13,033 (29.4) |
| 2 | 15,021 (14.1) | 4,170 (14.9) | 4,604 (13.6) | 6,247 (14.1) |
| 3+ | 11,519 (10.8) | 3,451 (12.3) | 3,565 (10.5) | 4,503 (10.1) |
| Missing | 13 (<0.1) | 2 (<0.1) | 3 (<0.1) | 8 (<0.1) |
| Poverty Rate1 | ||||
| Quartile 1 (Low) | 13,060 (12.3) | 3,244 (11.6) | 4,622 (13.6) | 5,194 (11.7) |
| Quartile 2 | 17,750 (16.7) | 4,388 (15.7) | 5,909 (17.4) | 7,453 (16.8) |
| Quartile 3 | 29,226 (27.5) | 7,749 (27.7) | 9,234 (27.3) | 12,243 (27.6) |
| Quartile 4 (High) | 46,249 (43.5) | 12,609 (45.1) | 14,122 (41.7) | 19,518 (44.0) |
| Healthy Food Density2 | ||||
| Quartile 1 (Low Density) | 11,358 (10.7) | 2,722 (9.7) | 3,228 (9.5) | 5,408 (12.2) |
| Quartile 2 | 17,107 (16.1) | 4,165 (14.9) | 5,151 (15.2) | 7,791 (17.5) |
| Quartile 3 | 29,536 (27.8) | 7,706 (27.5) | 8,985 (26.5) | 12,845 (28.9) |
| Quartile 4 (High Density) | 48,284 (45.4) | 13,397 (47.9) | 16,523 (48.8) | 18,364 (41.4) |
| Unhealthy Food Density3 | ||||
| Quartile 1 (Low Density) | 7,658 (7.2) | 1,686 (6.0) | 2,243 (6.6) | 3,729 (8.4) |
| Quartile 2 | 14,270 (13.4) | 3,465 (12.4) | 4,256 (12.6) | 6,549 (14.8) |
| Quartile 3 | 33,109 (31.2) | 8,755 (31.3) | 10,542 (31.1) | 13,812 (31.1) |
| Quartile 4 (High Density) | 51,248 (48.2) | 14,084 (50.3) | 16,846 (49.7) | 20,318 (45.8) |
| Neighborhood Walkability Index4 | ||||
| Quartile 1 (Low) | 10,485 (9.9) | 2,366 (8.5) | 3,114 (9.2) | 5,005 (11.3) |
| Quartile 2 | 19,705 (18.5) | 5,033 (18.0) | 6,044 (17.8) | 8,628 (19.4) |
| Quartile 3 | 34,933 (32.9) | 9,272 (33.1) | 11,207 (33.1) | 14,454 (32.6) |
| Quartile 4 (High) | 41,133 (38.7) | 11,315 (40.4) | 13,516 (39.9) | 16,302 (36.7) |
| Missing | 29 (<0.1) | 4 (<0.1) | 6 (<0.1) | 19 (<0.1) |
| Walkable Destinations Density5 | ||||
| Quartile 1 (Low Density) | 7,676 (7.2) | 1,709 (6.1) | 2,256 (6.7) | 3,711 (8.4) |
| Quartile 2 | 14,669 (13.8) | 3,592 (12.8) | 4,335 (12.8) | 6,742 (15.2) |
| Quartile 3 | 31,758 (29.9) | 8,400 (30.0) | 9,698 (28.6) | 13,660 (30.8) |
| Quartile 4 (High Density) | 52,182 (49.1) | 14,289 (51.1) | 17,598 (51.9) | 20,295 (45.7) |
Poverty rate quartile cut points (Q1: ≤0.097; Q2: >0.097; Q3: >.0.151; Q4: ≥0.230)
Healthy food density quartile cut points (Q1: ≤0.644; Q2: >0.644; Q3: >1.592; Q4: ≥3.409)
Unhealthy food density quartile cut points (Q1: ≤10.310; Q2: >10.310; Q3: >24.531; Q4 ≥50.618)
Neighborhood walkability index quartile cut points (Q1: ≤-1.632; Q2: >-1.632; Q3: >-0.279; Q4: ≥1.067)
Walkable Destinations density quartile cut points (Q1: ≤86.874; Q2: > 86.874; Q3: >175.094; Q4: ≥ 343.820)
Special Supplemental Nutrition Program for Women, Infants and Children (WIC)
2.3. Measures
2.3.1. Outcome Variable
Gestational weight gain (GWG) in kilograms was calculated by the authors by subtracting the pregnant individuals’ prepregnancy weight from weight at time of delivery. Inadequate, recommended and excessive GWG categories were then determined using the IOM recommendations for total weight gain, which are prepregnancy BMI-category specific and used in clinical guidance.7,26
2.3.2. Individual Covariates
Prepregnancy BMI was calculated using the pregnant individual’s weight (kg) and height (m2). The pregnant individual’s prepregnancy BMI was further categorized into the World Health Organization’s BMI categories defined as underweight (< 18.5), normal weight (18.5–24.9), overweight (25–29.9), obese Class I (30–34.9), obese Class II (35–39.9) and obese Class III (≥ 40). Gestational age of the baby (in weeks) was defined as a continuous variable.
Individual demographic variables were self-reported. The pregnant individual’s age was included as a continuous variable. Education was a categorical variable ranging from less than high school up to doctorate or professional degree. Nativity was included as a dichotomous variable for U.S. born (including U.S. territories) or foreign born. Parity was defined as an ordinal variable using previous livebirths. We included pregnant individual’s race/ethnicity as a confounder, not because there is a biological basis for difference in GWG by race/ethnicity, but because race/ethnicity may serve as a proxy for social factors (e.g., dietary practices, pregnancy behavior norms, or structural racism) that influence GWG and are not captured by other individual-level or neighborhood characteristics.27
2.3.3. Neighborhood Exposure Variables
The pregnant individual’s residential address was geocoded to the Census block of residence. A 1 kilometer (km) radial buffer was created around the geographic centroid of each 2010 Census block, areas of water removed, and the radial buffers’ land areas were characterized for socio-demographic composition and built environment features. One km buffers are commonly used in the literature to define residential neighborhood areas and urban planners consider this a walkable area around a residence.28 Furthermore, the neighborhood walkability indexes were developed and validated using a 1 km buffer neighborhood definition in NYC.29,30
Retail food establishments and walkable destinations were identified using the National Establishment Time Series (NETS) dataset from 2014.31,32 The NETS provides a census of businesses, commercial entities, institutions, and not-for-profits in the U.S. with business names, addresses and Standardized Industry Classification (SIC) codes for each establishment. We a priori grouped food outlets into categories hypothesized to provide foods healthy or unhealthy for BMI and calculated the density of healthy and unhealthy food establishments for each radial buffer.17 The healthy retail food category included supermarkets, fruit and vegetable markets and natural food stores. The BMI-unhealthy category included fast-food outlets, convenience stores, meat markets, pizzerias, bakeries and candy and nut stores.
Walkable destinations were defined as businesses, institutions and municipal resources that serve as destinations for pedestrian trips or that contribute to a pleasant, lively, or interesting pedestrian experience.29 Walkable destinations were identified using SIC codes listed in the NETS data and the included SIC codes were a slight modification of establishments defined previously.29,32
The neighborhood walkability index (NWI) includes five components, each receiving equal weight: (1) residential density; (2) street intersection density; (3) land use mix for five types of land use—residential, office, retail, education, and entertainment; (4) subway stop density; and (5) the ratio of retail building floor area to retail land area.30,33,34 Residential density data were derived from the 2012–2016 American Community Survey; land use data were derived from the 2015 Primary Land Use Tax Lot Output data produced by the NYC Department of City Planning (DCP); street intersection density data were derived from 2015 LION street base map data, also produced by the NYC DCP; and subway stop density data were derived from the NYC Metropolitan Transit Authority in 2015. Each scale component was calculated for the land area of each 1-km radial buffer around a Census block centroid and Z-score transformed; the Z-score transformed components were summed for each buffer. Prior work has shown that variation in the NWI across New York City predicts resident’s BMI, total physical activity and engagement in active transport.30,34,35
The proportion of people living below the Federal poverty line (poverty rate) was estimated for each radial buffer using U.S. Census 2012–2016 American Community Survey data. Tract level poverty rate data were apportioned to the radial buffers using standard areal weighting interpolation methods.36
To preserve the confidentiality of the birth records, the linkage between Census block of residence and neighborhood variables was completed at the NYC DOHMH and the combined individual- and neighborhood-level data were analyzed with neighborhood-level variables categorized into quartiles. Quartile cut-points were established using the distribution of the neighborhood-level variables across all Census blocks in NYC.
2.4. Statistical Analysis
Statistical analyses were performed using Stata 15.1.37 Generalized linear mixed effects models with a binomial distribution were used to analyze the association between neighborhood-level variables and excessive GWG compared to recommended weight gain, adjusting for individual-level covariates.38,39 Likewise, generalized linear mixed effects models were used to analyze associations between neighborhood-level variables and inadequate GWG compared to recommended weight gain. The models included a random intercept for NYC community district, which represents the most local unit of government in NYC and typically reflects well-known neighborhood areas.17 All models were adjusted for individual characteristics: age, race/ethnicity, education, nativity, parity, receipt of Special Supplemental Nutrition Program for Women, Infants and Children (WIC) benefits, and baby’s gestational age at birth. Due to high collinearity between neighborhood food environment and walkability variables (see Table S1), three separate models were fit. Model 1 assessed neighborhood healthy and unhealthy food density and neighborhood poverty as predictors of GWG, Model 2 assessed NWI scores and neighborhood poverty, and Model 3 assessed density of neighborhood walkable destinations and neighborhood poverty. All three models were fit adjusting for the individual-level variables described above.
Research in NYC has found that these neighborhood-level characteristics predict BMI among adults, and prepregnancy BMI is also predictive of under and over GWG.8,17,18 Thus, neighborhood-level factors may be associated with GWG via links to prepregnancy BMI. However, neighborhood-level factors may also influence energy balance related behaviors during pregnancy. Thus to provide guidance on which of these pathways may be operating, all three models were also fit further adjusting for prepregnancy BMI categories. A reduction in an association between a neighborhood-level factor and under or over GWG upon further adjustment for prepregnancy BMI, is interpreted to indicate that the neighborhood-level effect on GWG is due to associations between the neighborhood feature and prepregnancy BMI. However, if further adjustment for prepregnancy BMI does not alter the association between a neighborhood-level factor and GWG, the interpretation is that the neighborhood-level feature is associated with energy balance related behaviors during pregnancy, which in turn influence GWG.
Additionally, we ran sensitivity analyses deliveries prior to 37 weeks gestational age were excluded from the data (see Table S2). Lastly, as a further sensitivity analysis, we used hierarchical linear models (HLM) to assess whether neighborhood characteristics predicted GWG standardized for gestational age (GWG z-score) as the primary outcome (see Table S3).
2.7. Ethics Approval
This study was approved by the Columbia University Irving Medical Center Institutional Review Board.
3. RESULTS
Table 1 provides sample characteristics for the final analytic sample of 106,285 births. (See Table S4 for GWG by prepregnancy BMI class and IOM categories.) As Table 1 also shows, that while neighborhood quartiles were defined based on distribution of neighborhood variables across all NYC Census blocks, the pregnancies in the dataset were not evenly distributed across quartiles, but the pregnant individuals tended to live in higher poverty rate, food dense, and walkable areas of the city. As expected, prepregnancy weight classes were associated with inadequate and excessive GWG; compared to those in the normal weight class, individuals experiencing obesity and overweight were more likely to experience excessive GWG.
Table 2 shows adjusted odds of inadequate or excessive GWG (compared to reference group of recommended GWG) for each quartile of neighborhood food environment and poverty rate. In Model 1, where both healthy and unhealthy food retail were key exposure variables, higher neighborhood poverty was associated with increased odds of excessive GWG (Q4 OR 1.17; 95% CI 1.08, 1.26). Neighborhood density of healthy food retail was not associated with GWG (either inadequate or excessive), however greater density of unhealthy food retail was associated with lower odds of excessive GWG, especially when comparing the top two quartiles to the bottom quartile (Q3 OR 0.83; 95% CI 0.76, 0.91; Q4 OR 0.83; 95% CI 0.75, 0.92). After adjustment for prepregnancy BMI, the association between higher levels of neighborhood poverty rate and excessive GWG was attenuated, but ORs remain statistically significant (Q4 OR 1.09; 95% CI 1.01, 1.17). None of the neighborhood characteristics in Model 1 were associated with inadequate GWG.
Table 2.
Associations of neighborhood food environment factors and IOM recommended gestational weight gain (GWG) levels
| Inadequate GWG vs Recommended | Excessive GWG vs Recommended | |||||||
|---|---|---|---|---|---|---|---|---|
| OR | p>|t| | 95% CI | OR | p>|t| | 95% CI | |||
|
| ||||||||
| Model 1 | ||||||||
|
| ||||||||
| Poverty Rate1 | ||||||||
| Quartile 1 (Low) | ref | ref | ||||||
| Quartile 2 | 0.99 | 0.70 | 0.92 | 1.06 | 1.09 | 0.01 | 1.02 | 1.16 |
| Quartile 3 | 1.02 | 0.69 | 0.94 | 1.09 | 1.16 | <0.01 | 1.08 | 1.25 |
| Quartile 4 (High) | 1.06 | 0.16 | 0.98 | 1.15 | 1.17 | <0.01 | 1.08 | 1.26 |
| Healthy Food Density2 | ||||||||
| Quartile 1 (Low Density) | ref | ref | ||||||
| Quartile 2 | 0.96 | 0.27 | 0.89 | 1.03 | 0.98 | 0.45 | 0.92 | 1.04 |
| Quartile 3 | 1.01 | 0.82 | 0.93 | 1.09 | 0.98 | 0.65 | 0.92 | 1.06 |
| Quartile 4 (High Density) | 1.00 | 0.93 | 0.91 | 1.09 | 0.94 | 0.09 | 0.87 | 1.01 |
| Unhealthy Food Density3 | ||||||||
| Quartile 1 (Low Density) | ref | ref | ||||||
| Quartile 2 | 1.06 | 0.22 | 0.97 | 1.15 | 0.91 | 0.01 | 0.84 | 0.98 |
| Quartile 3 | 1.03 | 0.53 | 0.94 | 1.14 | 0.83 | <0.01 | 0.76 | 0.91 |
| Quartile 4 (High Density) | 1.01 | 0.82 | 0.91 | 1.13 | 0.83 | <0.01 | 0.75 | 0.92 |
| Model 1 (adjusted for prepregnancy BMI) | ||||||||
|
| ||||||||
| Poverty Rate1 | ||||||||
| Quartile 1 (Low) | ref | ref | ||||||
| Quartile 2 | 0.99 | 0.79 | 0.92 | 1.06 | 1.04 | 0.17 | 0.98 | 1.11 |
| Quartile 3 | 1.03 | 0.47 | 0.95 | 1.11 | 1.09 | 0.01 | 1.02 | 1.17 |
| Quartile 4 (High) | 1.08 | 0.08 | 0.99 | 1.17 | 1.09 | 0.03 | 1.01 | 1.17 |
| Healthy Food Density2 | ||||||||
| Quartile 1 (Low Density) | ref | ref | ||||||
| Quartile 2 | 0.96 | 0.32 | 0.89 | 1.04 | 0.96 | 0.23 | 0.90 | 1.03 |
| Quartile 3 | 1.01 | 0.72 | 0.94 | 1.10 | 0.98 | 0.64 | 0.92 | 1.06 |
| Quartile 4 (High Density) | 1.00 | 0.97 | 0.91 | 1.09 | 0.95 | 0.23 | 0.88 | 1.03 |
| Unhealthy Food Density3 | ||||||||
| Quartile 1 (Low Density) | ref | ref | ||||||
| Quartile 2 | 1.05 | 0.27 | 0.96 | 1.15 | 0.91 | 0.02 | 0.84 | 0.98 |
| Quartile 3 | 1.02 | 0.65 | 0.93 | 1.13 | 0.83 | <0.01 | 0.76 | 0.90 |
| Quartile 4 (High Density) | 1.00 | 0.98 | 0.90 | 1.11 | 0.82 | <0.01 | 0.74 | 0.90 |
Models adjusted for the pregnant individual’s age, race/ethnicity, education, marital status, foreign born status, WIC receipt status, parity, and gestational age.
Percent poverty quartile cut points (Q1: ≤0.097; Q2: >0.097; Q3: >.0.151; Q4: ≥0.230)
Healthy food density quartile cut points (Q1: ≤0.644; Q2: >0.644; Q3: >1.592; Q4: ≥3.409)
Unhealthy food density quartile cut points (Q1: ≤10.310; Q2: >10.310; Q3: >24.531; Q4 ≥50.618)
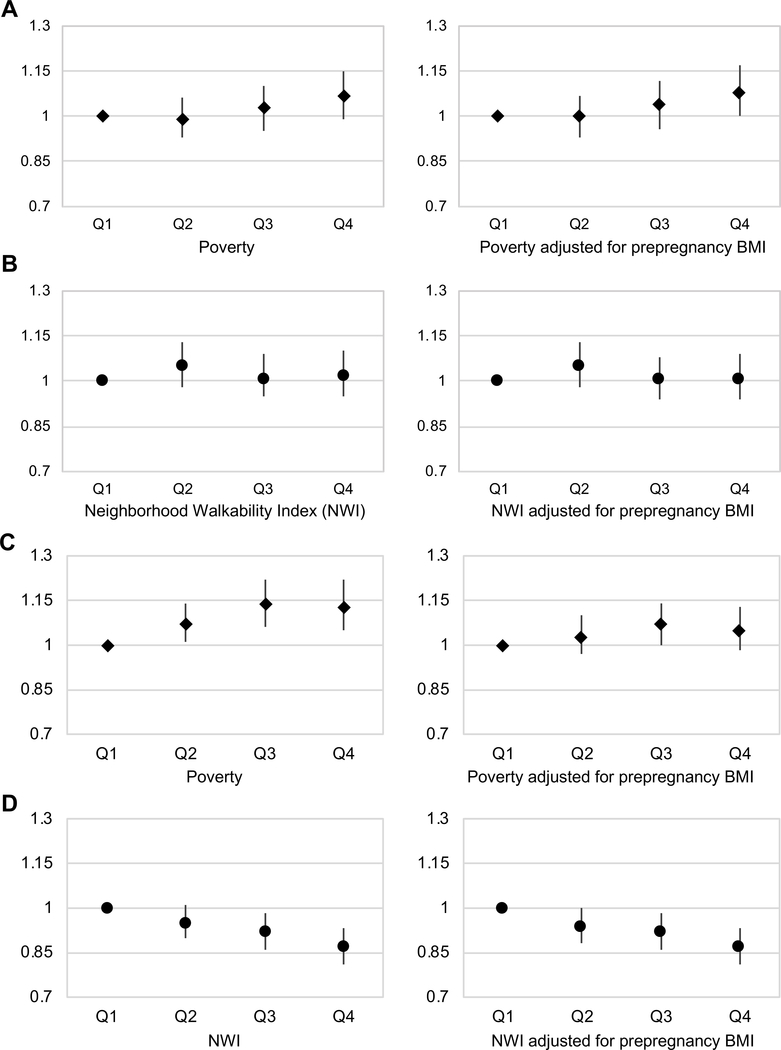
Higher NWI scores and a higher density of walkable destinations were both associated with lower odds of excessive GWG (Table 3 and Figure 1). For those pregnant individuals living in a neighborhood with the highest quartile NWI score, the odds of excessive GWG were 13 percent lower (95% CI 0.81, 0.93) than among those living in the lowest quartile of walkability. Further adjustment for pre-pregnancy BMI did not alter the associations between excessive GWG and NWI scores or between excessive GWG and walkable destinations. As in Model 1, neither walkability nor poverty rate were associated with inadequate GWG in Models 2 and 3 (see Table 3).
Table 3.
Associations of neighborhood walkability factors with IOM recommended gestational weight gain (GWG) levels
| Inadequate GWG vs Recommended | Excessive GWG vs recommended | |||||||
|---|---|---|---|---|---|---|---|---|
| OR | p>|t| | 95% CI | OR | p>|t| | 95% CI | |||
|
| ||||||||
| Model 2 | ||||||||
|
| ||||||||
| Poverty Rate1 | ||||||||
| Quartile 1 (Low) | ref | ref | ||||||
| Quartile 2 | 0.99 | 0.79 | 0.93 | 1.06 | 1.07 | 0.02 | 1.01 | 1.14 |
| Quartile 3 | 1.03 | 0.51 | 0.95 | 1.10 | 1.14 | <0.01 | 1.06 | 1.22 |
| Quartile 4 (High) | 1.07 | 0.10 | 0.99 | 1.15 | 1.13 | <0.01 | 1.05 | 1.22 |
| Neighborhood Walkability Index2 | ||||||||
| Quartile 1 (Low Score) | ref | ref | ||||||
| Quartile 2 | 1.05 | 0.14 | 0.98 | 1.13 | 0.95 | 0.12 | 0.90 | 1.01 |
| Quartile 3 | 1.01 | 0.70 | 0.95 | 1.09 | 0.92 | 0.01 | 0.86 | 0.98 |
| Quartile 4 (High Score) | 1.02 | 0.60 | 0.95 | 1.10 | 0.87 | <0.01 | 0.81 | 0.93 |
| Model 2 (adjusted for prepregnancy BMI) | ||||||||
|
| ||||||||
| Poverty Rate1 | ||||||||
| Quartile 1 (Low) | ref | ref | ||||||
| Quartile 2 | 1.00 | 0.89 | 0.93 | 1.07 | 1.03 | 0.32 | 0.97 | 1.10 |
| Quartile 3 | 1.04 | 0.32 | 0.96 | 1.12 | 1.07 | 0.06 | 1.00 | 1.14 |
| Quartile 4 (High) | 1.08 | 0.05 | 1.00 | 1.17 | 1.05 | 0.17 | 0.98 | 1.13 |
| Neighborhood Walkability Index2 | ||||||||
| Quartile 1 (Low Score) | ref | ref | ||||||
| Quartile 2 | 1.05 | 0.15 | 0.98 | 1.13 | 0.94 | 0.06 | 0.88 | 1.00 |
| Quartile 3 | 1.01 | 0.77 | 0.94 | 1.08 | 0.92 | 0.01 | 0.86 | 0.98 |
| Quartile 4 (High Score) | 1.01 | 0.74 | 0.94 | 1.09 | 0.87 | <0.01 | 0.81 | 0.93 |
| Model 3 | ||||||||
|
| ||||||||
| Poverty Rate1 | ||||||||
| Quartile 1 (Low) | ref | ref | ||||||
| Quartile 2 | 0.99 | 0.72 | 0.92 | 1.06 | 1.07 | 0.02 | 1.01 | 1.14 |
| Quartile 3 | 1.01 | 0.70 | 0.94 | 1.09 | 1.14 | <0.01 | 1.07 | 1.22 |
| Quartile 4 (High) | 1.06 | 0.16 | 0.98 | 1.14 | 1.15 | <0.01 | 1.07 | 1.24 |
| Walkable Destinations3 | ||||||||
| Quartile 1 (Low Density) | ref | ref | ||||||
| Quartile 2 | 1.04 | 0.32 | 0.96 | 1.14 | 0.93 | 0.04 | 0.86 | 1.00 |
| Quartile 3 | 1.06 | 0.16 | 0.98 | 1.16 | 0.88 | <0.01 | 0.81 | 0.95 |
| Quartile 4 (High Density) | 1.02 | 0.63 | 0.94 | 1.12 | 0.80 | <0.01 | 0.73 | 0.87 |
| Model 3 (adjusted for prepregnancy BMI) | ||||||||
|
| ||||||||
| Poverty Rate1 | ||||||||
| Quartile 1 (Low) | ref | ref | ||||||
| Quartile 2 | 0.99 | 0.81 | 0.93 | 1.06 | 1.03 | 0.34 | 0.97 | 1.10 |
| Quartile 3 | 1.03 | 0.47 | 0.95 | 1.11 | 1.07 | 0.04 | 1.00 | 1.15 |
| Quartile 4 (High) | 1.07 | 0.09 | 0.99 | 1.16 | 1.07 | 0.08 | 0.99 | 1.14 |
| Walkable Destinations3 | ||||||||
| Quartile 1 (Low Density) | ref | ref | ||||||
| Quartile 2 | 1.04 | 0.36 | 0.96 | 1.13 | 0.92 | 0.04 | 0.86 | 1.00 |
| Quartile 3 | 1.06 | 0.19 | 0.97 | 1.16 | 0.87 | <0.01 | 0.80 | 0.94 |
| Quartile 4 (High Density) | 1.01 | 0.83 | 0.92 | 1.11 | 0.81 | <0.01 | 0.75 | 0.88 |
Models adjusted for pregnant individual’s age, race/ethnicity, education, marital status, foreign born status, WIC receipt status, parity, and gestational age.
Percent poverty quartile cut points (Q1: ≤0.097; Q2: >0.097; Q3: >.0.151; Q4: ≥0.230)
Neighborhood walkability index quartile cut points (Q1: ≤-1.632; Q2: >-1.632; Q3: >-0.279; Q4: ≥1.067)
Walkable destinations density quartile cut points (Q1: ≤86.874; Q2: > 86.874; Q3: >175.094; Q4: ≥ 343.820)
Figure 1.
Panels A and B depict odds ratios for inadequate GWG compared to recommended GWG. Panels C and D depict odds ratios for excessive GWG compared to recommended GWG. All models are adjusted for pregnant individual’s age, race/ethnicity, education, marital status, foreign born status, WIC receipt status, parity, and gestational age.
Sensitivity analyses excluding births prior to 37 weeks gestational age from the data produced results that were similar to results for analyses of all births for all three models and for both inadequate and excessive GWG outcomes. Analyses of GWG z-scores produced results that were consistent with the results of analyses of categorical GWG outcomes.
4. Discussion
Our study is the first, to our knowledge, to use population level data to evaluate the associations between GWG and multiple neighborhood characteristics, including the food environment. In this study of neighborhood characteristics and GWG in NYC, we found that greater neighborhood poverty and lower neighborhood walkability were associated with higher odds of excessive GWG. This aligns with prior studies in NYC that have found that both neighborhood poverty and walkability predict BMI in the general population.17 Prepregnancy BMI categories were strongly associated with excessive GWG. Adjustment for prepregnancy BMI attenuated the association between neighborhood poverty and excessive GWG, but had little impact on the magnitude of association between neighborhood walkability and excessive GWG. None of the neighborhood-level variables were associated with inadequate GWG.
Contrary to expectations, the density of unhealthy food retail outlets was associated with lower odds of excessive GWG. The literature on healthy or unhealthy food outlets and obesity is inconsistent. In a prior study, the density of unhealthy food retail was not associated with BMI and in a subsequent study of New Yorkers from 2002 to 2006 unhealthy food retail was associated with higher BMI after adjustment for total retail food density and diversity of retail food establishments.17,18 Indeed, there are also prior findings suggesting unhealthy food retail is associated with lower obesity risk, including a study of children enrolled in NYC public schools in 2008; a higher density of fast food restaurants was associated with lower odds of obesity.40 However, a “placebo test” found that banks--a measure of overall neighborhood retail ecology--also predicted lower obesity prevalence among these school children, to a similar extent as fast food restaurants. The findings of the placebo test were interpreted to suggest that higher overall retail and economic activity was associated with a lower prevalence of childhood obesity.
In the current analyses of food outlets, we suggest that a phenomenon similar to that observed in the study of school children is occurring. In the past decade, the density of unhealthy food outlets has increased and is now highly correlated with overall walkable retail destinations and neighborhood walkability. We hypothesize that the negative association between the density of unhealthy food establishments and excessive GWG does not reflect a healthful feature of these food establishments, but rather the link between higher neighborhood walkability (or possibly associated constructs such as employment density) with lower odds of excessive GWG.
Prior studies have shown that neighborhood food environments and neighborhood walkability are associated with BMI in adulthood.17,18 Thus, associations between neighborhood features and GWG could arise due to links between neighborhood features and prepregnancy BMI, and in turn, the linkages between prepregnancy BMI and GWG. However, it is possible that associations between neighborhood features and GWG reflect differences in behavior of pregnant individuals during pregnancy that are influenced by neighborhood features. Analyses with and without control for prepregnancy BMI provide evidence for which of these theorized pathways is more likely.
For instance, in our analyses the observed associations between neighborhood poverty rate and excessive GWG were reduced, but remained statistically significant, after adjustment for pregnant individual’s prepregnancy BMI category. This suggests that some of the association between neighborhood poverty rate and excessive GWG is explained by associations between neighborhood poverty and prepregnancy BMI. In contrast, the association between higher neighborhood walkability and excessive GWG was essentially unaffected by adjustment for prepregnancy BMI, suggesting that neighborhood walkability is associated with GWG due to differences in behaviour during pregnancy – presumably pedestrian activity (e.g. walking for exercise, daily activities, commuting, etc) – and not solely by influences on prepregnancy BMI. This hypothesis is supported by prior research in the general population showing that, within NYC, variation in neighborhood walkability predicts differences in BMI, total physical activity and engagement in active transportation.30,34,35 Literature on perceptions around physical activity during pregnancy further supports this hypothesis. Qualitative studies with pregnant individuals have highlighted the importance of access to safe places to exercise and incorporation of movement in everyday activities (e.g. walking, household chores) as facilitators to physical activity during pregnancy.41,42 Studies have also noted a common concern among pregnant individuals around the safety of physical activity for the foetus, with many expressing that gentle exercise (e.g. walking, stretching) was preferable to other forms of exercise.41–43 Prior studies have shown a positive association between mid-pregnancy walking and reduced odds of excessive GWG.44
4.1. Strengths of the study
The large sample size and variability and diversity of NYC’s neighborhoods with respect to walkability and density of food resources are both strengths of the study. Additionally, the study provides new evidence on an understudied topic that has clear public health importance.
4.2. Limitations of the data
This study has several limitations. First given the high density of the city and low car ownership, NYC has unique food retail environments and walkability features.45 This may limit the generalizability of the findings to populations in other geographic areas, particularly rural and suburban locations. However, as of 2018, more than 55 percent of the world’s population lived in urban areas and this number is projected to grow to 68 percent by the year 2050, thus findings from urban settings including NYC have relevance for large portions of the global population.46
Another limitation is possible reliance on self-report of height and weight data for some of the sample, though medical record data and anthropometric measurements in a clinical setting are expected to be used in most instances. Other socio-demographic variables such as education and race/ethnicity were also self-reported into the medical records. Potential error in the height and weight data are unlikely to alter the conclusions of the analyses, however. Previous research indicates that self-reported anthropometric data and measured anthropometric data produce near identical estimates in health effects studies, especially if estimates are adjusted for individual-level sociodemographic factors known to be associated with measurement error from self-report.47
Lastly, the measures of walkability are based purely on urban form/planning concepts and do not incorporate data on other, more experiential, characteristics such as perceptions of safety or aesthetic qualities.33 However, many of these experiential qualities are expected to correlate with neighborhood socioeconomic conditions and the analyses adjusted for neighborhood poverty rate.33
5. CONCLUSION
The research reported here provides further data on how neighborhood environment characteristics influence health and health behaviors. Neighborhood factors, including poverty, appear to be associated with prepregnancy weight status, which is a significant risk factor for excessive GWG. Additionally, neighborhood walkability appears to be associated with GWG even after accounting for associations with prepregnancy weight. Multiple guidelines exist for planners and architects on how to design for health, including the NYC Active Design Guidelines, the WELL Community Standard, the American Institute of Architects Healthy Design Research Consortium, and the Department of Health and Human Service’s Healthy People 2020 guidelines. However, due to limited research on the implications of active design for health during pregnancy, few such guides explicitly consider pregnant individuals and their infants. Given the long-lasting benefits of healthy pregnancies for parental and child health, this research provides further impetus for the use of urban design to support healthy weight and reduce the risk of excessive GWG and associated sequalae. If further research replicates the findings presented here, supporting the health of young children should be factored into cost-benefit analyses of built environment interventions to create walkable neighborhoods.
Supplementary Material
Study Importance Questions.
What is already known about this subject?
Most pregnant individuals do not gain the recommended amount of weight during pregnancy and both inadequate and excessive gestational weight gain can negatively impact the long term health of pregnant individuals and children.
Very little research examines the relationship between neighborhood characteristics and gestational weight gain.
What are the new findings in your manuscript?
Living in a more walkable neighborhood is associated with lower odds of excessive gestational weight gain, which could be due to differences in pedestrian activity during pregnancy.
How might your results change the direction of research or the focus of clinical practice?
Given the long-lasting benefits of healthy pregnancies for parental and child health, this research provides further impetus for the use of urban design to support healthy weight and reduce the risk of excessive GWG and associated sequalae.
Acknowledgments
Funding: This research was supported by Eunice Kennedy Shriver National Institute of Child Health and Human Development grants K99HD101657 (Kinsey), R00HD086304 (Widen) and P2CHD042849 (UT Population Research Center). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Disclosure: The authors declared no conflict of interest.
References
- 1.Davis RR, Hofferth SL, Shenassa ED. Gestational Weight Gain and Risk of Infant Death in the United States. Am J Public Health. 2014;104(Suppl 1):S90–S95. doi: 10.2105/AJPH.2013.301425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldstein RF, Abell SK, Ranasinha S, et al. Association of Gestational Weight Gain With Maternal and Infant Outcomes: A Systematic Review and Meta-analysis. JAMA. 2017;317(21):2207–2225. doi: 10.1001/jama.2017.3635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu J, Gallagher AE, Carta CM, Torres ME, Moran R, Wilcox S. Racial differences in gestational weight gain and pregnancy-related hypertension. Ann Epidemiol. 2014;24(6):441–447. doi: 10.1016/j.annepidem.2014.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Widen EM, Whyatt RM, Hoepner LA, et al. Excessive gestational weight gain is associated with long-term body fat and weight retention at 7 y postpartum in African American and Dominican mothers with underweight, normal, and overweight prepregnancy BMI. Am J Clin Nutr. 2015;102(6):1460–1467. doi: 10.3945/ajcn.115.116939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dumas O, Varraso R, Gillman MW, Field AE, Camargo CA. Longitudinal study of maternal body mass index, gestational weight gain, and offspring asthma. Allergy. 2016;71(9):1295–1304. doi: 10.1111/all.12876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Widen EM, Whyatt RM, Hoepner LA, et al. Gestational weight gain and obesity, adiposity and body size in African–American and Dominican children in the Bronx and Northern Manhattan. Matern Child Nutr. 2016;12(4):918–928. doi: 10.1111/mcn.12174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Institute of Medicine (US) and National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines. Weight Gain During Pregnancy: Reexamining the Guidelines. (Rasmussen KM, Yaktine AL, eds.). National Academies Press; (US: ); 2009. Accessed October 10, 2019. http://www.ncbi.nlm.nih.gov/books/NBK32813/ [PubMed] [Google Scholar]
- 8.Deputy NP, Sharma AJ, Kim SY, Hinkle SN. Prevalence and Characteristics Associated With Gestational Weight Gain Adequacy. Obstet Gynecol. 2015;125(4):773–781. doi: 10.1097/AOG.0000000000000739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mendez DD, Thorpe RJ, Amutah N, et al. Neighborhood racial composition and poverty in association with pre-pregnancy weight and gestational weight gain. SSM - Popul Health. 2016;2:692–699. doi: 10.1016/j.ssmph.2016.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mendez DD, Doebler DA, Kim KH, Amutah NN, Fabio A, Bodnar LM. Neighborhood socioeconomic disadvantage and gestational weight gain and loss. Matern Child Health J. 2014;18(5):1095–1103. doi: 10.1007/s10995-013-1339-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Headen I, Mujahid M, Deardorff J, Rehkopf DH, Abrams B. Associations between cumulative neighborhood deprivation, long-term mobility trajectories, and gestational weight gain. Health Place. 2018;52:101–109. doi: 10.1016/j.healthplace.2018.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Headen I, Laraia B, Coleman-Phox K, Vieten C, Adler N, Epel E. Neighborhood Typology and Cardiometabolic Pregnancy Outcomes in the Maternal Adiposity Metabolism and Stress Study. Obesity. 2019;27(1):166–173. doi: 10.1002/oby.22356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Casagrande SS, Gittelsohn J, Zonderman AB, Evans MK, Gary-Webb TL. Association of Walkability With Obesity in Baltimore City, Maryland. Am J Public Health. 2011;101(S1):S318–S324. doi: 10.2105/AJPH.2009.187492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Creatore MI, Glazier RH, Moineddin R, et al. Association of Neighborhood Walkability With Change in Overweight, Obesity, and Diabetes. JAMA. 2016;315(20):2211–2220. doi: 10.1001/jama.2016.5898 [DOI] [PubMed] [Google Scholar]
- 15.Frank LD, Sallis JF, Conway TL, Chapman JE, Saelens BE, Bachman W. Many Pathways from Land Use to Health: Associations between Neighborhood Walkability and Active Transportation, Body Mass Index, and Air Quality. J Am Plann Assoc. 2006;72(1):75–87. doi: 10.1080/01944360608976725 [DOI] [Google Scholar]
- 16.Hoehner CM, Handy SL, Yan Y, Blair SN, Berrigan D. Association between neighborhood walkability, cardiorespiratory fitness and body-mass index. Soc Sci Med. 2011;73(12):1707–1716. doi: 10.1016/j.socscimed.2011.09.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rundle A, Neckerman KM, Freeman L, et al. Neighborhood Food Environment and Walkability Predict Obesity in New York City. Environ Health Perspect. 2009;117(3):442–447. doi: 10.1289/ehp.11590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rundle A, Roux AVD, Freeman LM, Miller D, Neckerman KM, Weiss CC. The Urban Built Environment and Obesity in New York City: A Multilevel Analysis. Am J Health Promot. 2007;21(4_suppl):326–334. doi: 10.4278/0890-1171-21.4s.326 [DOI] [PubMed] [Google Scholar]
- 19.Smith KR, Brown BB, Yamada I, Kowaleski-Jones L, Zick CD, Fan JX. Walkability and Body Mass Index: Density, Design, and New Diversity Measures. Am J Prev Med. 2008;35(3):237–244. doi: 10.1016/j.amepre.2008.05.028 [DOI] [PubMed] [Google Scholar]
- 20.Paulo Dos Anjos Souza Barbosa J, Henrique Guerra P, de Oliveira Santos C, de Oliveira Barbosa Nunes AP, Turrell G, Antonio Florindo A. Walkability, Overweight, and Obesity in Adults: A Systematic Review of Observational Studies. Int J Environ Res Public Health. 2019;16(17). doi: 10.3390/ijerph16173135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fiechtner L, Kleinman K, Melly SJ, et al. Effects of Proximity to Supermarkets on a Randomized Trial Studying Interventions for Obesity. Am J Public Health. 2016;106(3):557–562. doi: 10.2105/AJPH.2015.302986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Caspi CE, Sorensen G, Subramanian SV, Kawachi I. The local food environment and diet: A systematic review. Health Place. 2012;18(5):1172–1187. doi: 10.1016/j.healthplace.2012.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ghosh-Dastidar B, Cohen D, Hunter G, et al. Distance to Store, Food Prices, and Obesity in Urban Food Deserts. Am J Prev Med. 2014;47(5):587–595. doi: 10.1016/j.amepre.2014.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stark JH, Neckerman K, Lovasi GS, et al. Neighbourhood food environments and body mass index among New York City adults. J Epidemiol Community Health. 2013;67(9):736–742. doi: 10.1136/jech-2013-202354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Inagami S, Cohen DA, Brown AF, Asch SM. Body mass index, neighborhood fast food and restaurant concentration, and car ownership. J Urban Health Bull N Y Acad Med. 2009;86(5):683–695. doi: 10.1007/s11524-009-9379-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gilmore LA, Redman LM. Weight gain in pregnancy and application of the 2009 IOM guidelines: Toward a uniform approach. Obesity. 2015;23(3):507–511. doi: 10.1002/oby.20951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jones CP. Invited Commentary: “Race,” Racism, and the Practice of Epidemiology. Am J Epidemiol. 2001;154(4):299–304. doi: 10.1093/aje/154.4.299 [DOI] [PubMed] [Google Scholar]
- 28.Lovasi GS, Grady S, Rundle A. Steps Forward: Review and Recommendations for Research on Walkability, Physical Activity and Cardiovascular Health. Public Health Rev. 2012;33(4):484–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rundle AG, Chen Y, Quinn JW, et al. Development of a Neighborhood Walkability Index for Studying Neighborhood Physical Activity Contexts in Communities across the U.S. over the Past Three Decades. J Urban Health Bull N Y Acad Med. 2019;96(4):583–590. doi: 10.1007/s11524-019-00370-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rundle AG, Sheehan DM, Quinn JW, et al. Using GPS Data to Study Neighborhood Walkability and Physical Activity. Am J Prev Med. 2016;50(3):e65–e72. doi: 10.1016/j.amepre.2015.07.033 [DOI] [PubMed] [Google Scholar]
- 31.Berger N, Kaufman TK, Bader MDM, et al. Disparities in trajectories of changes in the unhealthy food environment in New York City: A latent class growth analysis, 1990–2010. Soc Sci Med 1982. 2019;234:112362. doi: 10.1016/j.socscimed.2019.112362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hirsch JA, Moore KA, Cahill JP, et al. Methods for Collecting, Processing, and Linking Longitudinal Retail Data for Neighborhood- and Individual-Level HealthMethods for Collecting, Processing, and Linking Longitudinal Retail Data for Neighborhood- and Individual-Level Health. In:; 2020. Accessed September 30, 2020. https://spr.confex.com/spr/spr2020/meetingapp.cgi/Person/32923
- 33.Neckerman KM, Lovasi GS, Davies S, et al. Disparities in urban neighborhood conditions: evidence from GIS measures and field observation in New York City. J Public Health Policy. 2009;30 Suppl 1:S264–285. doi: 10.1057/jphp.2008.47 [DOI] [PubMed] [Google Scholar]
- 34.Freeman L, Neckerman K, Schwartz-Soicher O, et al. Neighborhood walkability and active travel (walking and cycling) in New York City. J Urban Health Bull N Y Acad Med. 2013;90(4):575–585. doi: 10.1007/s11524-012-9758-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stark JH, Neckerman K, Lovasi GS, et al. The impact of neighborhood park access and quality on body mass index among adults in New York City. Prev Med. 2014;64:63–68. doi: 10.1016/j.ypmed.2014.03.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Flowerdew R, Green M. Data integration: Statistical methods for transferring data between zonal systems. In: Masser I, Blakemore M, eds. Handling Geographical Information: Methodology and Potential Applications. Longman; 1991:38–54. [Google Scholar]
- 37.StataCorp. Stata Statistical Software: Release 15. StataCorp LP; 2017. [Google Scholar]
- 38.Agresti A An Introduction to Categorical Data Analysis. 3rd ed. John Wiley & Sons; 2019. [Google Scholar]
- 39.Begg CB, Gray R. Calculation of polychotomous logistic regression parameters using individualized regressions. Biometrika. 1984;71(1):11–18. doi: 10.1093/biomet/71.1.11 [DOI] [Google Scholar]
- 40.Bader MDM, Schwartz-Soicher O, Jack D, et al. More neighborhood retail associated with lower obesity among New York City public high school students. Health Place. 2013;23:104–110. doi: 10.1016/j.healthplace.2013.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Weir Z, Bush J, Robson SC, McParlin C, Rankin J, Bell R. Physical activity in pregnancy: a qualitative study of the beliefs of overweight and obese pregnant women. BMC Pregnancy Childbirth. 2010;10(1):18. doi: 10.1186/1471-2393-10-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vanstone M, Kandasamy S, Giacomini M, DeJean D, McDonald SD. Pregnant women’s perceptions of gestational weight gain: A systematic review and meta-synthesis of qualitative research. Matern Child Nutr. 2017;13(4):e12374. doi: 10.1111/mcn.12374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Faucher MA, Mirabito AM. Pregnant Women with Obesity Have Unique Perceptions About Gestational Weight Gain, Exercise, and Support for Behavior Change. J Midwifery Womens Health. n/a(n/a). doi: 10.1111/jmwh.13094 [DOI] [PubMed] [Google Scholar]
- 44.Stuebe AM, Oken E, Gillman MW. Associations of diet and physical activity during pregnancy with risk for excessive gestational weight gain. Am J Obstet Gynecol. 2009;201(1):58.e1–58.e8. doi: 10.1016/j.ajog.2009.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Residential Parking Study: Rates and Off-Street Parking Requirements in Portions of New York City. New York City: Department of City Planning; 2009. [Google Scholar]
- 46.United Nations, Department of Economic and Social Affairs, Population Division. World Urbanization Prospects: The 2018 Revision (ST/ESA/SER.A/420). United Nations; 2019. [Google Scholar]
- 47.Hodge JM, Shah R, McCullough ML, Gapstur SM, Patel AV. Validation of self-reported height and weight in a large, nationwide cohort of U.S. adults. PLOS ONE. 2020;15(4):e0231229. doi: 10.1371/journal.pone.0231229 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.