Abstract
Integrated testing for TB and COVID-19 may help find those TB patients who are not accessing care in the context of the COVID-19 pandemic. Some molecular platforms with assays for both diseases are already commercially available; however, integrated testing approaches need to be systematically evaluated to ensure their appropriate implementation.
Integrated testing for TB and COVID-19 may help find those TB patients who are not accessing care in the context of the COVID-19 pandemic. Some molecular platforms with assays for both diseases are already commercially available; however, integrated testing approaches need to be systematically evaluated to ensure their appropriate implementation.
Main text
The COVID-19 pandemic is wreaking havoc on all realms of global health and tuberculosis (TB) care and services are no exception.1 , 2 After one year of the pandemic, high TB burden countries were reporting drops in TB case notifications ranging from 16% to 41% (mean 23%)—levels not seen since 2008 (https://www.stoptb.org/news/12-months-of-covid-19-eliminated-12-years-of-progress-global-fight-against-tuberculosis). Of the approximately 10 million people who developed TB in 2020, only 5.8 million people were diagnosed and reported to national TB programs, an 18% decrease compared to 2019.1 Reduced access to medical care and TB services as well as the reallocation of existing public health tools, personnel, and infrastructure to COVID-19 efforts could explain this reduction.3 Predictably, the decline in people seeking TB care has led to an increase in TB-related deaths: in 2020, at least 1.5 million people died of TB, a figure not seen since 2017. Evidently, we are off track to meet many of the End TB goals, and without redoubled efforts and innovative strategies to reach those who need testing and treatment, we risk missing these milestones by even larger margins.1
Additionally, emerging data suggest that people with TB who develop COVID-19 are at a higher risk of severe disease and mortality compared to those without COVID-19. As well, a recent systematic review reported that COVID-19 patients with TB were at almost twice the risk of mortality compared to individuals with COVID-19 alone.4 Therefore, reaching people with TB and ensuring they receive appropriate care is urgent. Increasing TB testing and case notifications is a critical and pressing priority.
Proposed action: “Integrated testing”
More people with presumptive TB need to be reaching the second step of the TB care cascade; namely, moving from (1) developing incident TB to (2) accessing testing.5 One proposed catch-up intervention is integrating testing for TB and COVID-19. In the absence of World Health Organization policy, other global stakeholders have proposed frameworks and guidelines for integrated testing, although evidence to support these recommendations is limited.
In early 2021, the US Agency for International Development (USAID) and Stop TB partnership issued a brief document recommending that for people presenting to healthcare facilities with respiratory symptoms, a “simultaneous, integrated approach to testing for TB and COVID-19 should be implemented in countries with a high burden of TB,” namely, “diagnostic tests for both COVID-19 and TB should be done at the same time (simultaneous testing) on a multiplex testing platform (integrated testing).”6 These recommendations are broad and apply to anyone with presumptive TB or COVID-19.
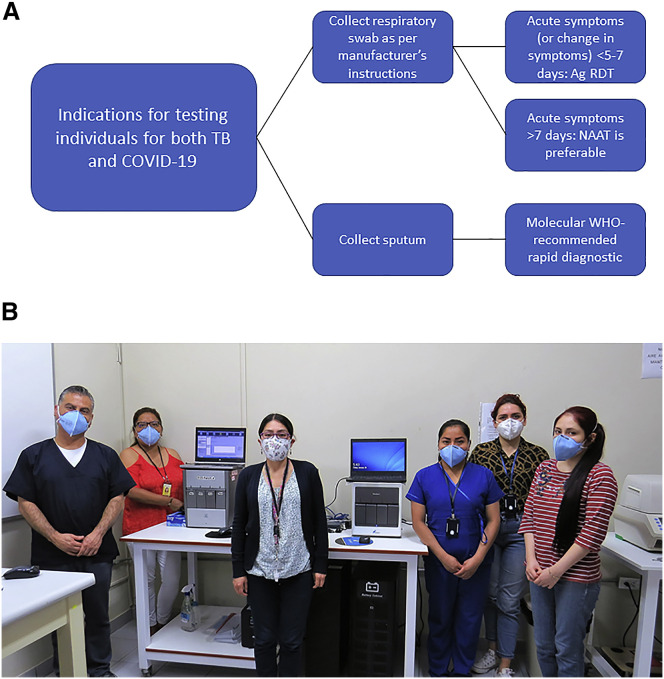
In late 2021, the Global Fund released a briefing note providing guidance regarding testing for TB and COVID-19. In particular, they recommend that in communities with prevalent TB and COVID-19, people whose clinical signs and symptoms meet case definitions for both TB and COVID-19 should undergo “systematic testing for both pathogens.” They also recommend molecular testing in those who have had symptoms for longer than 7 days, and antigen rapid testing for those with symptoms lasting 5-7 days (Figure 1 ).7
Figure 1.
Title. Using integrated approaches to test individuals for both TB and COVID-19
(A) Global Fund’s algorithm for testing for both TB and SARS-CoV-2.7
(B) GeneXpert modules and study team at Instituto de Medicina Tropical Alexander von Humboldt, Lima, Peru (Courtesy: Luz Villa-Castillo, Lima, Peru).
The Global Fund brief also suggests action in case people with TB are suspected to have developed COVID-19 symptoms. Should this situation arise, TB must continue to be properly managed, and then testing for SARS-CoV-2 infection should be performed if individuals “meet the COVID-19 case definition or when there is persistence or worsening of their condition despite appropriate treatment for the specific form of TB.”7
Certain countries have launched their own integrated testing efforts. In India, for example, this approach is termed bi-directional screening for TB and COVID-19. The Indian Ministry of Health and Family Welfare recommends that “COVID screening for all diagnosed TB patients and TB screening for all COVID positive patients should be conducted,” TB screening should be undertaken in all individuals with influenza-like illness, and all individuals with severe acute respiratory illness should be screened for TB.8 Recently, the ministry also issued guidance that all individuals undergoing COVID-19 treatment with a cough that lasts longer than 2 weeks should be tested for TB.9
The differences in these approaches demonstrate that there is not yet a clear consensus of who exactly should be prioritized: the target population for integrated testing needs to be more well-defined. The Global Fund’s testing algorithm (Figure 1) is narrower than the catch-all approach proposed by Stop TB Partnership and USAID. However, the two documents ultimately may not lead to much difference in practice, as discerning between the two diseases based on clinical picture alone can be difficult. Also, because COVID-19 has been impacting TB-endemic countries in waves, the need for integrated testing changes over time. When COVID-19 incidence rates are low, it is not completely obvious why TB programs would also need testing for COVID-19. And while this approach may assist in finding cases, the yield of integrated testing and its cost-effectiveness is unclear.
Possible testing platforms
Despite this ambiguity, there are some products already available that may be utilized for integrated testing. As countries have greatly scaled up their testing capabilities to deal with the large-scale demand for COVID-19 testing, this infrastructure could be expanded to include more testing for TB. In some cases, molecular testing for COVID-19 was originally possible due to existing laboratory infrastructure and diagnostics networks used by national TB and HIV programs.10 Single cartridges that can detect multiple pathogens as well as non-PCR-based platforms for multi-disease testing are becoming commercially available. The work to create “fast follower” assays has begun, with some TB tests that utilize the same platform or technical basis as novel COVID-19 tests under development. Some products that may be considered for integrated TB and COVID-19 testing are shown in Table 1 , including GeneXpert, a technology that has been scaled-up in many high TB burden countries (Figure 1).
Table 1.
Platforms for integrated testing for TB and COVID-19
| Platform | Type of assay | TB test | Commercially available for TB? | COVID-19 | Commercially available for COVID-19? |
|---|---|---|---|---|---|
| GeneXpert (Cepheid, USA) | cartridge-based real-time PCR | Xpert MTB/RIF; Xpert MTB/RIF Ultra | yes and WHO-approved | Xpert Xpress SARS-CoV-2; Xpert Xpress SARS-CoV-2/Flu/RSV | yes and US FDA EUA |
| Truenat (Molbio, India) | chip-based real-time PCR | Truenat MTBa | yes and WHO-approved | Truenat SARS CoV 2 | yes and EU CE-IVD |
| RealTime (Abbott, USA) | high-throughput centralized PCR system | RealTime MTB | yes and WHO-approved | RealTime SARS-CoV-2 | yes and US FDA EUA |
| BD MAX (BD, USA) | high-throughput centralized PCR system | max MDR-TB | yes and WHO-approved | BD SARS-CoV-2 reagents for BD MAX | yes and US FDA EUA |
| Hain FluoroType (Brukner, Germany) | high-throughput centralized PCR system | FluoroType MTB | yes and WHO-approved | FluoroType SARS-CoV-2 evo, plus, and varID Q | yes and EU CE-IVD |
| Loopamp (Eiken Chemical Co., Japan) | loop-mediated isothermal-amplification | Loopamp MTBC Detection Kit | yes and WHO-approved | Loopamp SARS-CoV-2 Detection Kit | yes and EU CE-IVD |
| Cobas 6800/8800 (Roche, Switzerland) | high-throughput centralized PCR system | cobas MTB-RIF/INH | no but WHO-approved | cobas SARS-CoV-2 & Influenza A/B Assay; cobas SARS-CoV-2 | yes and US FDA EUA |
| Standard M (SD. Biosensor, Republic of Korea) | cartridge-based real-time PCR | STANDARD M MDR-TB | under evaluation | STANDARD M nCoV Real-Time Detection Kit; STANDARD M Flu/SARS-CoV-2 | yes and US FDA EUA |
| EasyNAT (UStar Biotechnol-ogies, China) | portable cross-priming amplification | EasyNAT MTB | yes and CFDA-approved | EasyNAT SARS-CoV-2 | yes and EU CE-IVD |
Combined TB and COVID-19 chip is under evaluation. CFDA, China Food and Drug Administration; CE IVD, CE marked in vitro diagnostics; EU, European Union; EUA, emergency use authorization; TB, tuberculosis; US FDA, United States Food and Drug Administration; WHO, World Health Organization.
While all the molecular platforms in Table 1 require sputum samples for TB testing, the conventional sample for COVID-19 testing is a nasopharyngeal (NP) swab. This poses challenges for performing integrated testing with a single clinical sample, and data are needed to show whether sputum could be a viable and useful sample for COVID-19 testing. In high TB burden countries, healthcare workers have experience in coaching patients to produce sputum samples and within the context of pandemic-related medical equipment stock-outs, specimen types that do not require specialized equipment are appealing.
The massive investment into research and development of COVID-19 diagnostics will hopefully be leveraged to produce a variety of new diagnostic tests for TB, a chronically underfunded area. Consider the advances in molecular tests that have made some COVID-19 tests available at lower levels of healthcare systems, including the point-of-care and even self-testing at-home, or the development of tests that can run on a broad variety of samples. Tests incorporating either of these user-friendly advances have the potential to reach people in remote areas and may make obtaining good quality samples easier from people with all forms of presumptive TB.10
Supporting evidence for integrated testing?
Evidence describing the disruptions to TB programs and services since the beginning of the COVID-19 pandemic is accumulating,3 , 4 and although it is well-recognized that there has been a global decline in TB testing,3 reports of interventions to recover these losses are very limited. This is also true for integrated TB and COVID-19 testing.
One study in Madagascar reported that the Ministry of Public Health had decided to use existing GeneXpert platforms for COVID-19 testing, which were in place for TB testing. The authors noted that automated platforms like GeneXpert require less trained staff than traditional PCR due to the decreased number of hands-on steps, and because the network was already existing, the country could quickly take advantage of its services.11
In high TB burden settings like South Africa, it has been suggested that community-based screening networks deployed for COVID-19 could also support TB testing and lead to improved linkage to care. For individuals who test positive for TB, there is an opportunity to test for COVID-19 at the time of TB contact tracing.12
A publication of public health efforts in Kerala, India, has shown that systematic integration of COVID-19 and TB testing is possible.13 When health authorities noted that their capacity was entirely being directed to COVID-19 control efforts, they adopted strategies to incorporate those efforts with other disease programs’ work. Anyone who was eligible for COVID-19 testing was screened for TB if they met any of the four conditions: (1) presence of influenza-like illness in an individual with risk factors for developing TB (e.g., close contact, elderly, living with diabetes), (2) individuals testing negative for COVID-19 but whose symptoms lasted for >14 days, (3) any individual hospitalized for due to COVID-19, or (4) positive for COVID-19 and four-symptom (cough >2 weeks, fever >2 weeks, weight loss, night sweats) screen positive for TB. Those who screened positive were offered molecular TB testing using new and existing Truenat and GeneXpert platforms, with tests for TB and COVID-19 run on both systems. The authors reported that their integrated testing efforts comprised 8% of total TB diagnoses made state-wide in a 1-month period.13
Currently, we are recruiting adults with presumptive TB or COVID-19 in Lima, Peru, to investigate integrated TB and COVID-19 testing using the GeneXpert platform.14 Each participant is providing us with a sputum sample and an NP swab, which are then tested for both TB and COVID-19. So far, we have observed that with a single sputum sample, we can identify 98% of culture-confirmed TB cases and 84% of RT-PCR-confirmed COVID-19 cases. Our in-study prevalence of concurrent TB and COVID-19 is around 2%, which does raise some questions about the efficiency and cost-effectiveness of this approach on a large scale.14
Further answers are needed
Integrated testing for TB and COVID-19 has the potential to help recover a proportion of the missing people who developed TB in the pandemic era, but many important unknowns remain regarding its implementation. Implementing integrated testing within existing laboratory and specimen collection workflows is likely feasible, but patient acceptability of introducing testing for COVID-19 and TB, a disease that is typically accompanied by substantial social stigma, is not known.
Evidence is urgently needed to understand who exactly should be tested for both TB and COVID-19. Considering that COVID-19 is typified by acute but short-term symptoms, while TB is characterized by longer-term clinical symptoms, who is the ideal target population for integrated testing? As resources are not unlimited, an efficient strategy that can identify cases at a relatively high rate would be desirable. Certain sub-populations, such as immunocompromised people, will need particular attention to ensure integrated testing policies reach them. Evaluations of integrated testing in large populations with diverse epidemiologic history, clinical symptoms, and varied symptom duration distributions will help draw conclusions regarding who should undergo integrated testing.
Examining integrated testing in a variety of settings is needed to understand where this intervention should immediately be rolled-out. Example settings include urban locales with very high TB prevalence where there are many shared risk factors for COVID-19; rural settings in high TB burden countries where integrated disease testing could greatly improve quality of care; or countries with a higher proportion of people who are immunocompromised. It is also important to account for the fact that COVID-19 has been impacting countries in waves: in countries with high TB prevalence, integrated testing may therefore be irrelevant when COVID-19 incidence is low, but may again become highly relevant during COVID-19 surges. Good surveillance for both infections is necessary to make adjustments in testing policies.
Against the background of global supply chain issues, further investigation into alternative but acceptable sampling strategies is warranted. Although NP swabs are considered the gold standard for COVID-19 molecular testing, other samples may yield a sufficiently high proportion of cases. Other sample types such as tongue swabs, nasal swabs, throat swabs, aerosol collection in face masks, or conventional sputum could be candidates for testing of both conditions, and strategies like sample batching and at-home sample collection should be considered. More work is needed to understand these approaches in the context of integrated testing.
Modeling studies to understand the cost and cost-effectiveness of integrated TB and COVID-19 testing will help aid decision making and setting priorities. Simulations should be run for different iterations of testing strategies, target populations, incidence triggers, and settings. Despite the calls for integrated disease testing, it is not yet known whether the yield will be worth the additional costs. Molecular testing for Covid-19 is expensive for many low- and middle-income countries. Adding a second molecular test for TB for all people with respiratory symptoms might be prohibitively expensive in many settings unless the strategy is worth the effort and costs. Understanding this piece will help countries plan and allocate resources, as well as inform future policies.
Concluding remarks
Ostensibly, integrated testing for TB and COVID-19 seems to be a beneficial intervention, but it has yet to be systematically evaluated and data are lacking. Available multiplex platforms can facilitate this testing, with more products emerging. As new SARS-CoV-2 variants of concern arise, integrated testing policies will need to be re-examined and updated as needed. Careful design of studies and outcomes will need to be considered to ensure the real impact of integrated testing can be identified and measured.
Acknowledgments
Author contributions
Conceptualization, M.P., E.L.M.; Supervision, M.P.; Writing – Original draft preparation, E.L.M.; Writing – Review & Editing, E.L.M., L.V.C., M.R., C.U.G., M.P.
Declaration of Interest
E.L.M., L.V.C., C.U.G., and M.P. declare no competing interests.
M.R. is an employee of FIND. FIND is a not-for-profit foundation whose mission is to find diagnostic solutions to overcome diseases of poverty in low- and middle-income countries (LMICs). It works closely with the private and public sectors and receives funding from some of its industry partners. It has organizational firewalls to protect it against any undue influences in its work or the publication of its findings. All industry partnerships are subject to review by an independent scientific advisory committee or another independent review body, based on due diligence, TTPs and public sector requirements. FIND catalyzes product development, leads evaluations, takes positions, and accelerates access to tools identified as serving its mission. It provides indirect support to industry (e.g., access to open specimen banks, a clinical trial platform, technical support, expertise, laboratory capacity strengthening in LMICs) to facilitate the development and use of products in these areas. FIND also supports the evaluation of publicly prioritized TB assays and the implementation of WHO-approved (guidance and performance qualification [PQ]) assays using donor grants. In order to carry out test evaluations, FIND has product evaluation agreements with several private sector companies for TB and other diseases, which strictly defines its independence and neutrality vis-à-vis the companies whose products get evaluated and describes roles and responsibilities.
References
- 1.World Health Organization . World Health Organization; 2021. Global Tuberculosis Report 2021. Geneva. [Google Scholar]
- 2.Pai M., Kasaeva T., Swaminathan S. Covid-19's Devastating Effect on Tuberculosis Care - A Path to Recovery. N. Engl. J. Med. 2022 doi: 10.1056/NEJMp2118145. [DOI] [PubMed] [Google Scholar]
- 3.McQuaid C.F., Vassall A., Cohen T., Fiekert K., White R.G. The impact of COVID-19 on TB: a review of the data. Int. J. Tuberc. Lung Dis. 2021;25:436–446. doi: 10.5588/ijtld.21.0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aggarwal A.N., Agarwal R., Dhooria S., Prasad K.T., Sehgal I.S., Muthu V. Active pulmonary tuberculosis and coronavirus disease 2019: A systematic review and meta-analysis. PLoS ONE. 2021;16:e0259006. doi: 10.1371/journal.pone.0259006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Subbaraman R., Jhaveri T., Nathavitharana R.R. Closing gaps in the tuberculosis care cascade: an action-oriented research agenda. J. Clin. Tuberc. Other Mycobact. Dis. 2020;19:100144. doi: 10.1016/j.jctube.2020.100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.USAID . Stop TB Partnership; 2021. Stop TB Partnership. Simultaneous, integrated diagnostic testing approach to detect COVID-19 and TB in high TB burden countries. Geneva. [Google Scholar]
- 7.The Global Fund Briefing Note: Testing for both Tuberculosis and SARS-CoV-2. Geneva: The Global Fund. 2021. https://www.theglobalfund.org/media/11438/covid19_tb-testing_briefingnote_en.pdf October 13, 2021.
- 8.Ministry of Health and Family Welfare . In: Welfare IMoHaF, editor. Government of India; 2020. Guidance note on bi-directional TB-COVID screening and screening of TB among ILI/SARI cases.https://www.mohfw.gov.in/pdf/1TBCOVIDscreeningguidancenote.pdf New Delhi. [Google Scholar]
- 9.Express Weekly Desk . The Indian Express; New Delhi: 2022. Avoid steroids, get tested for TB if cough persists, says Centre in new Covid guidelines.https://indianexpress.com/article/india/covid-clinical-care-updated-guidelines-tb-steroids-7727006/ [Online newspaper] ([updated 18 January 2022; cited 2022 26 January], Available from. [Google Scholar]
- 10.Ruhwald M., Carmona S., Pai M. Learning from COVID-19 to reimagine tuberculosis diagnosis. Lancet Microbe. 2021;2:e169–e170. doi: 10.1016/S2666-5247(21)00057-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rakotosamimanana N., Randrianirina F., Randremanana R., Raherison M.S., Rasolofo V., Solofomalala G.D., Spiegel A., Heraud J.-M. GeneXpert for the diagnosis of COVID-19 in LMICs. Lancet Glob. Health. 2020;8:e1457–e1458. doi: 10.1016/S2214-109X(20)30428-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Loveday M., Cox H., Evans D., Furin J., Ndjeka N., Osman M., et al. The National Tb Think Tank “Optimising Tb Treatment Outcomes” Task Team, Opportunities from a new disease for an old threat: Extending COVID-19 efforts to address tuberculosis in South Africa. S. Afr. Med. J. 2020;110:1160–1167. doi: 10.7196/SAMJ.2020.v110i12.15126. [DOI] [PubMed] [Google Scholar]
- 13.Khobragade R.N., Murthy N., Aloysius S., Surendran D., Rakesh P.S., Balakrishnan S. Experience of integrated screening and testing for TB and COVID19 from Kerala, India. Public Health Pract (Oxf) 2021;2:100198. doi: 10.1016/j.puhip.2021.100198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.MacLean, E., Villa-Castillo, L., Cáceres-Nakiche, T., et al., eds (2021). Validation of rapid molecular testing for Covid-19 and integration with tuberculosis TB diagnostics in Lima, Peru. 52nd World Conference on Lung Health of the International Union Against Tuberculosis and Lung Disease (The Union); 2021 19-22 October 2022; Virtual: The Union.