Abstract
Background and Aims:
Inflammatory bowel diseases (IBD) lead to high morbidity and unplanned healthcare utilization. We conducted a systematic review with meta-analysis to estimate the cumulative incidence of IBD-related (and all-cause) hospitalization in patients with ulcerative colitis (UC) and Crohn’s disease (CD).
Methods:
Through a systematic review to September 3, 2019, we identified population-based inception cohort studies in patients with IBD that reported patient-level cumulative incidence of hospitalization at 1-, 3- and 5-years after diagnosis. Hospitalization risk was pooled using random-effects meta-analysis, and risk factors analyzed through mixed-effects meta-regression and qualitative synthesis.
Results:
In patients with UC (6 cohorts), 1-, 3- and 5-year risk of UC-related hospitalization was 10.4% (95% CI, 8.2–13.2), 17.0% (95% CI, 14.0–20.4) and 21.5% (95% CI, 18.0–25.4), respectively, with considerable heterogeneity. In patients with CD (6 cohorts), 1-, 3- and 5-year risk of CD-related hospitalization was 29.3% (95% CI, 20.0–40.8), 38.5% (95% CI, 26.8–51.7) and 44.3% (95% CI, 32.7–56.5), respectively, with considerable heterogeneity. On meta-regression, steady decline in risk of hospitalization was observed in patients diagnosed in a more contemporary era. Younger age at onset (both UC and CD), extensive colitis (UC), ileal-dominant CD, perianal CD and penetrating and/or stricturing behavior (CD) and early need for corticosteroids and immunosuppressive therapy (both UC and CD) were associated with increased risk of hospitalization.
Conclusion:
Approximately one in five and one in two patients with UC and CD are hospitalized within 5 years of diagnosis, respectively. Population health management strategies are required to mitigate unplanned healthcare utilization.
Keywords: Natural history, complications, inflammatory bowel diseases, inpatient, biologics
INTRODUCTION
The global incidence and prevalence of inflammatory bowel disease (IBD) is rising.1 By 2030, the disease is estimated to affect 1% of individuals in the Western World. IBD is characterized by a lifelong unpredictable relapsing-remitting course, leading to substantial morbidity, diminished quality of life and healthcare resource utilization.2 Several studies have examined annual rates and trends of hospitalization in patients with IBD.3–6 In a population-based study of countries in the Organization for Economic Co-operation and Development, King and colleagues3 observed variable and high rates of hospitalization in patients with IBD, particularly in Western countries ranging from 31.5 to 72.9 per 100,000 patients. Ma and colleagues4 observed a progressive rise in the annual incidence of hospitalization in patients with IBD in the US over the last decade. Inpatient care accounts for 44.8% of annual healthcare spending in patients with IBD, totaling ~$10 billion, and costs of inpatient care have increased 7.8% annually over the last two decades.7 Similar trends have been observed in other countries, such as Portugal,8 though in South Korea, overall burden of unplanned healthcare utilization in patients with IBD has decreased over time.9
However, these studies do not adequately inform patient-level cumulative incidence and trends of hospitalization, which can be used to educate and inform decision-making in patients with newly diagnosed IBD. Referral-center studies on burden of hospitalization and readmission in patients with IBD may overestimate risks due to selection bias. In contrast, true population-based studies provide more accurate and generalizable risk assessment of adverse outcomes in patients with IBD.
Hence, to better understand patient-level risk of, and risk factors for, hospitalization in patients with IBD, we performed a systematic review with meta-analysis to analyze the cumulative 1-, 3- and 5-year risk of IBD-related (and all-cause) hospitalization in patients with newly diagnosed ulcerative colitis (UC) and Crohn’s disease (CD), in population-based inception cohorts.
METHODS
Study Selection
We included population-based cohort studies in patients with incident UC and/or CD, reporting the cumulative incidence of all-cause and/or IBD-related hospitalization since time of diagnosis, with at least 1-year minimum follow-up. Population-based studies were identified as those that investigated the entire population in a defined geographical area in a defined time period, used appropriate sampling techniques to infer risk for the entire population, or used national registries capturing nearly the entire population in a region (>90%). For inclusion, these studies were required to report number of patients with incident UC or CD, calendar year of cohort recruitment, and cumulative incidence of hospitalization estimated by Kaplan-Meier methodology. When multiple studies reported hospitalization risk from the same cohort, the most comprehensive study reporting from non-overlapping times were included.
We excluded studies that: (1) reported only overall annual hospitalization rates without patient-level cumulative incidence of hospitalization, (2) reported risk of hospitalization in patients with IBD, without distinguishing CD or UC, (3) were not population-based (single- or multi-center referral studies, or clinical trials), or (4) reported incidence rate of hospitalization without cumulative incidence. We also excluded studies published before 1980, since disease-modifying therapies were very uncommon prior to 1980 and a significant proportion of disease evaluation and management occurred as inpatients.
Data Sources and Search Strategy
We performed this systematic review based on an a priori protocol and reported according to the guidelines as prescribed by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).10 The review was not registered. A medical librarian (LJP) designed and performed a comprehensive literature search with input from study investigators utilizing various databases (included Ovid Epub, Medline In-Process & Other Non-Indexed Citations, Ovid MEDLINE, Ovid EMBASE, Ovid Cochrane Central Register of Controlled Trials, Ovid Cochrane Database of Systematic Reviews and Scopus) from inception to September 3, 2019. Controlled vocabulary supplemented with keywords was used to search for population-based cohort studies of natural history and outcomes in inflammatory bowel disease. The references of all identified relevant studies, as well as recent Cochrane reviews on the topic, were also manually reviewed to identify any potentially relevant studies. We search conference proceedings from Digestive Diseases Week and European Crohn’s and Colitis Congress, from 2017 to 2020. Two study reviewers (LT, SS) independently reviewed each title and abstract of all studies to exclude non-relevant studies and reviewed full texts of selected studies for inclusion based on pre-defined selection criteria. Discrepancies in article selection were reviewed by both reviewers together to resolve with discussion, and if unable to, were resolved by a third reviewer (WJS). Details of the search strategy are reported in the Appendix. Figure 1 shows the schematic diagram of study selection.
Figure 1.
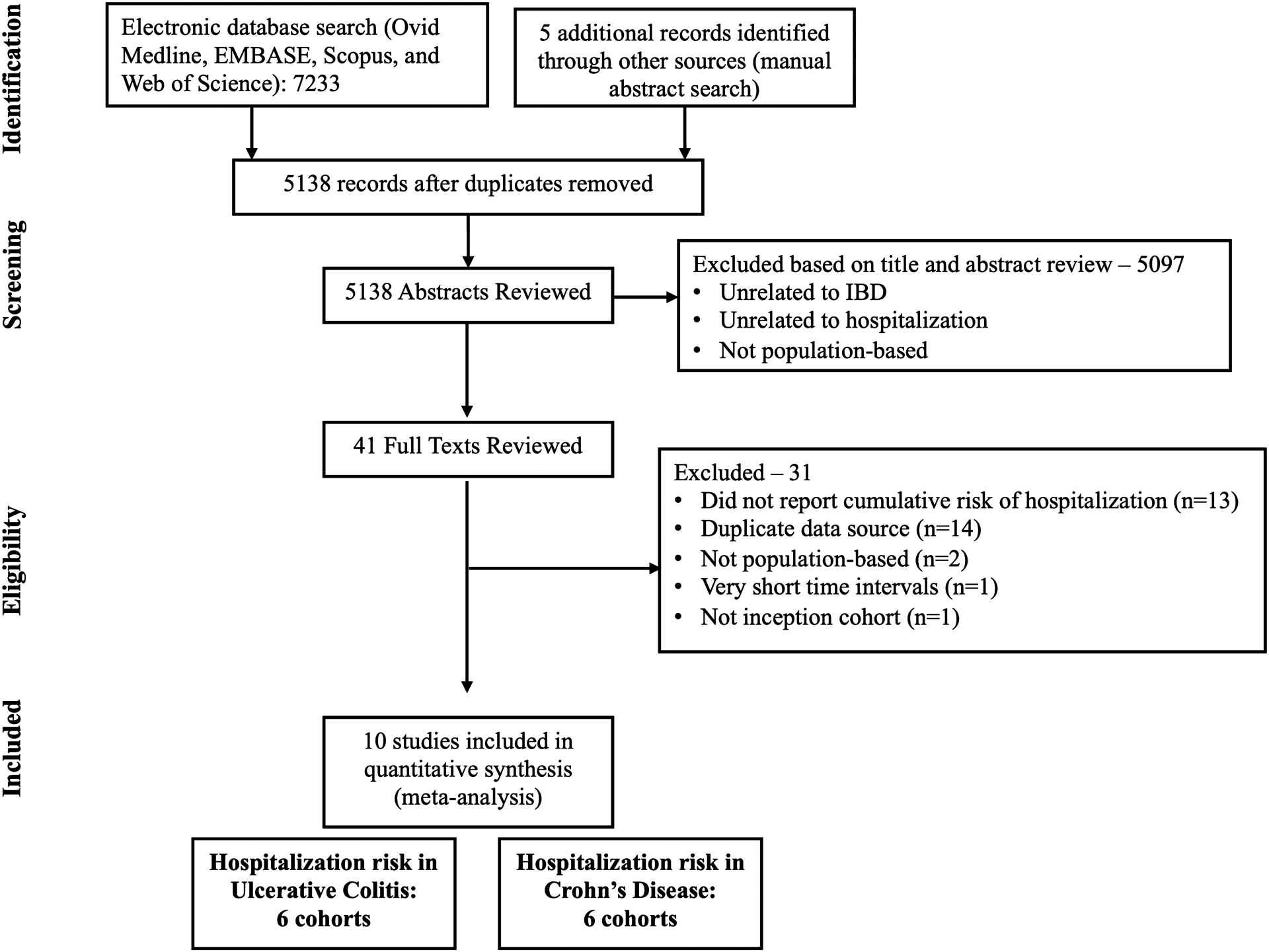
Study selection flowchart
Data Extraction and Risk of Bias Assessment
Data abstraction was conducted with a standardized electronic form to capture data on study-, patient-, disease- and treatment-related characteristics. Two reviewers (LT, SS) independently reviewed and abstracted data with discrepancies resolved by consensus in consultation with a third reviewer (WJS). Risk of bias assessment was adapted for prevalence studies, and focused on identification of appropriate target population, systematic method of data ascertainment, validated criteria for disease diagnosis and hospitalization, complete follow-up for >70% of cohort, and description of patients lost to follow-up.11 Risk of bias assessment was performed by one reviewer (LT), and verified by a second reviewer (SS).
Outcomes
The primary outcome was the cumulative 1-, 3-, and 5-year risk of IBD-related hospitalization in patients with UC and CD. IBD-related hospitalization was identified as hospitalization either due to IBD-related symptoms or complications. Secondary outcomes were (a) 1-, 3-, and 5-year risk of all-cause hospitalization in patients with UC and CD, and (b) 1- and 5-year risk of readmission in patients with initial hospitalization. We qualitatively synthesized risk factors associated with initial hospitalization and readmission.
Subgroup analyses were performed based upon geographical location (North America vs. Europe vs. other geographical locations). To examine sources of heterogeneity in effect estimates, we conducted mixed effects meta-regression based on population composition (mean age at IBD diagnosis, proportion of males), disease characteristics (UC: proportion of patients with extensive colitis [E3 on Montreal classification]; CD: proportion of patients with ileum-dominant CD [L1/L3 on Montreal classification], proportion of patients with penetrating and/or fibrostenotic behavior [B2/B3 on Montreal classification], and proportion of patients with perianal disease), and time-trend based on the mid-point of cohort entry as a continuous variable. To evaluate more contemporary hospitalization risk in the biologic era, we conducted sensitivity analysis of cohorts in which the majority of patients were diagnosed after 2000 (>90% cohort). Additional sensitivity analyses were performed after excluding conference proceedings.
Statistical Analysis
The pooled risk of IBD-related (and all-cause) hospitalization and 95% confidence intervals (CIs) at 1-, 3-, 5-, and 10-years for both UC and CD was estimated using a random effects model.12 To estimate 95% CI for individual study estimates from Kaplan-Meier curves, we assumed complete follow-up of the entire cohort. Heterogeneity between studies was assessed using the inconsistency index (I2) with values >50% suggesting significant heterogeneity.13 We anticipated high statistical heterogeneity as a meta-analysis of cumulative incidence, and took measures to address this in the design stage (strict study inclusion/exclusion criteria) and analysis. Subgroup analyses based on geographical location was performed, with a p-value for differences between subgroups of <0.10 being considered statistically significant. For meta-regression, when the slope of the hospitalization incidence fit by the mixed-effect model had an associated p<0.10, we concluded that the incidence of hospitalization was significantly influenced by variable of interest.14 Due to considerable heterogeneity for all analyses, statistical assessment of publication bias was not performed.15 All analyses were performed using Comprehensive Meta-Analysis (CMA) software, version 2 (Biostat, Englewood, NJ).
RESULTS
Literature Search
A total 5138 unique studies were identified using our search strategy. Of these, 41 full text articles were reviewed, and 10 studies were included in quantitative synthesis, reporting on 6 cohorts of patients with UC,16–21 and 6 cohorts of patients with CD.20–25 Thirty-one studies were excluded with detailed reasons reported in Figure 1.
Risk of Hospitalization in Patients with Ulcerative Colitis
Table 1 details the characteristics of 6 studies in patients with UC.16–21 These studies included patients diagnosed between 1970 to 2015, with sample sizes ranging from 96 to 14,000 patients with UC; the largest study was a Canadian provincial database study.21 All studies were published as full texts. Study-level risk-of-bias assessment demonstrated unclear risk of bias, specifically for cohort attrition and reasons for loss to follow-up (Appendix Table 1).
Table 1.
Characteristics of included studies on hospitalization risk in ulcerative colitis
| Burisch et al, 2018 | Multiple European Countries | EPI-IBD | 2010 | 717 | Adults | M (55), F (45) | E1 (20), E2 (41), E3 (39) | 1, 3, and 5 | All-cause |
| Golovics et al, 2015 | Hungary | Veszprem Province | 2000 – 2010 | 347 | - | M (58), F (42) | E1 (28), E2 (44), E3 (28) | 1, 3, 5, and 10 | UC-related |
| Jeuring et al, 2015 | Netherlands | IBD-SL | 1991 – 2010 | 1661 | Adults | M (53), F (47) | E1 (34), E2 (48), E3 (18) | 1, 2, 3, and 5 | All-cause and UC-related |
| Niewiadomski et al, 2015 | Australia | Barwon Area | 2007 – 2008, 2010 – 2013 | 96 | All Ages | M (41), F (59) | E1 (32), E2 (31), E3 (36) | 1 and 5 | All-cause |
| Samuel et al, 2013 | USA | Olmsted County | 1970 – 2004 | 369 | All Ages | M (58), F (42) | E1 (29), E2 (37), 117 (32) | 1, 3, 5, 10, 20, 30 | UC-related |
| Verdon et al, 2020 | Canada | RAMQ | 1996 – 2015 | 14000 | All Ages | M (50), F (50) | - | 5 | All-cause |
M: Male, F: Female, E1: Proctitis, E2: Left-sided Colitis, E3: Extensive Colitis, UC: Ulcerative Colitis
Median (range) cumulative 1-, 3- and 5-year risk of UC-related hospitalization were 8.7% (8.6–15.5%), 15.5% (13.5–23.0%) and 19.5% (18.3–29.4%), respectively. On meta-analysis, the cumulative incidence of UC-related hospitalization at 1-, 3-, and 5-years after diagnosis was 10.4% (95% CI, 8.2–13.2), 17.0% (95% CI, 14.0–20.4) and 21.5% (95% CI, 18.0–25.4), respectively, with considerable heterogeneity (I2=75–79%) (Figure 2). Two studies reported 34.3% to 38.5% 10-year cumulative incidence of UC-related hospitalization. Meta-analytic cumulative incidence of all-cause hospitalization at 1-, 3- and 5-years after diagnosis of UC were 15.5% (95% CI, 8.9–25.8) (4 cohorts, I2=92%), 26.1% (95% CI, 12.4–46.8) (3 cohorts, I2=97%) and 31.3 % (95% CI, 23.5–40.4) (5 cohorts, I2=95%), respectively (eFigure 1). In cohorts reporting risk of UC-related hospitalization in the biologic era, 1-, 3- and 5-year risks were 8.6% (95% CI, 7.3–10.1), 14.6% (95% CI, 13.0–16.5) and 18.9% (95% CI, 17.1–21.0), respectively. In 4 cohorts, median 5-year risk of UC-related re-hospitalization after initial UC-related hospitalization was 46.7% (range, 37.2–51.1). Due to limited data on total person-year follow-up, we were unable to ascertain incidence rate of initial hospitalization and readmission.
Figure 2.
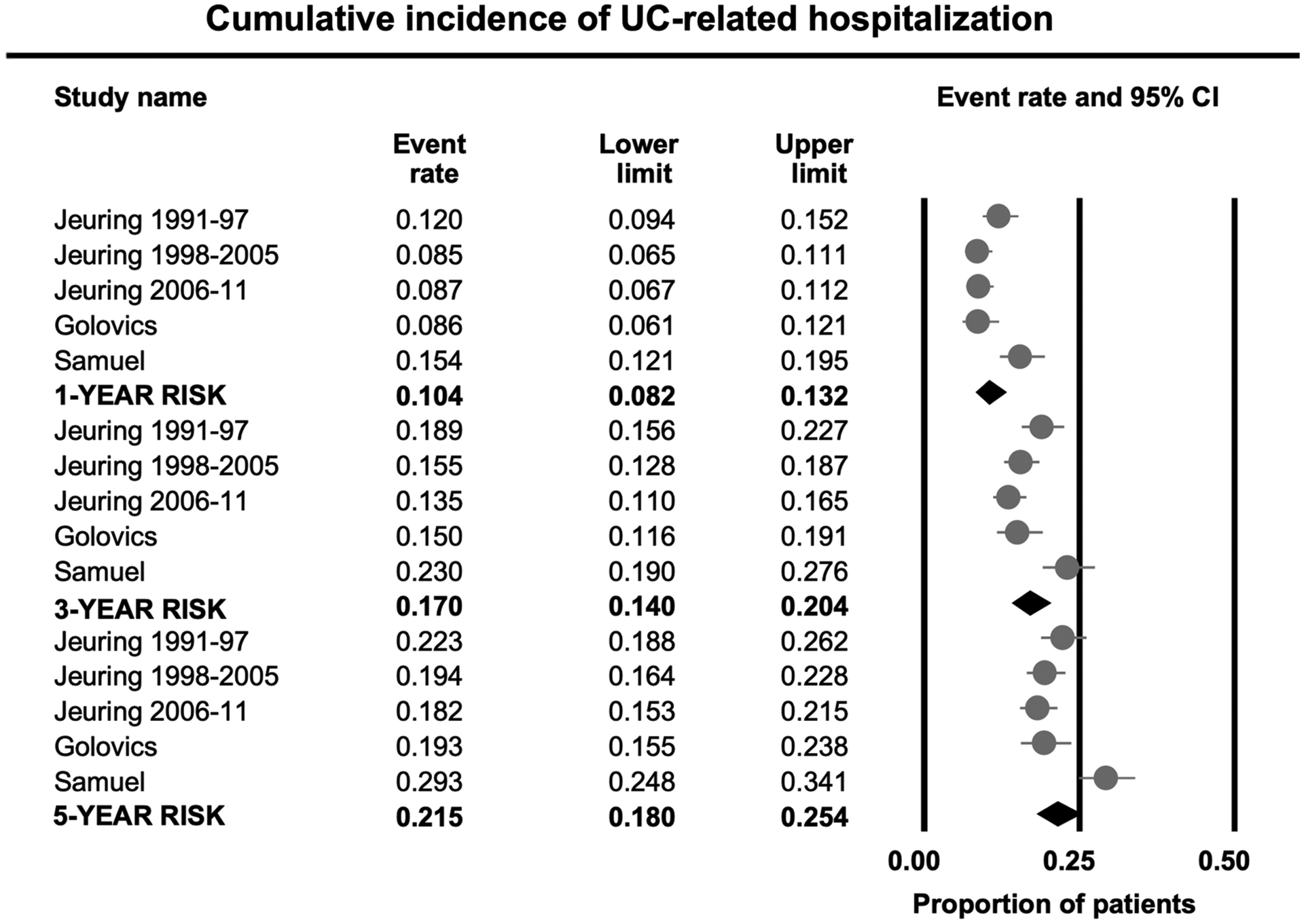
Cumulative 1-, 3- and 5-year risk of UC-related hospitalization in patients with ulcerative colitis.
Mixed-effects meta-regression suggested a higher 5-year risk of UC-related hospitalization in cohorts with younger age at disease onset (p=0.07) (Table 2). Over time, there was a decline in 1- and 5-year risk of UC-related hospitalization based on mid-point of cohort entry (p<0.01). On subgroup analysis by study location, risk of UC-related hospitalization was higher in one cohort in North America (29.4% [95% CI, 24.8–34.1]) as compared to four cohorts in Europe (19.8% [95% CI, 18.1–21.6]) (p-value for difference between groups <0.01).
Table 2.
Meta-regression – p-value for difference in 1- and 5-year risk of IBD-related hospitalization in patients with ulcerative colitis and Crohn’s disease, based on study-level factors using mixed effects meta-regression
| 1y risk of hospitalization | 5y risk of hospitalization | |||
|---|---|---|---|---|
| Coefficient | p-value | Coefficient | p-value | |
| Ulcerative colitis | ||||
| Mean age at UC diagnosis | −0.061 | 0.05 | −0.063 | 0.07 |
| Proportion of males | 0.015 | 0.69 | 0.031 | 0.42 |
| Proportion of patients with extensive colitis | 0.020 | 0.42 | 0.015 | 0.57 |
| Mid-point of cohort entry | −0.009 | 0.78 | −0.005 | 0.84 |
| Crohn’s disease | ||||
| Mean age at CD diagnosis | −0.034 | 0.61 | −0.058 | 0.38 |
| Proportion of females | −0.017 | 0.63 | −0.009 | 0.69 |
| Proportion of patients with ileum-dominant CD (L1/L3) | 0.055 | 0.04 | 0.041 | 0.23 |
| Proportion of patients with perianal CD | 0.097 | 0.13 | 0.130 | 0.03 |
| Proportion of patients with penetrating or stricturing CD | 0.020 | 0.40 | 0.035 | 0.12 |
| Mid-point of cohort entry | −0.084 | 0.02 | −0.062 | 0.01 |
[Abbreviations: B1/B3=ileal of ileocolonic location based on Montreal classification; CD=Crohn’s disease; UC=ulcerative colitis]
Risk of Hospitalization in Patients with Crohn’s Disease
Table 3 details the characteristics of 6 studies in patients with CD.20–25 These studies included patients diagnosed between 1970 to 2015, with sample sizes ranging from 146 to 20,644 patients with CD; the largest study was a Canadian provincial database study.21 All studies, except one,25 were published as full texts. Study-level risk-of-bias assessment demonstrated unclear risk of bias, specifically for cohort attrition and reasons for loss to follow-up (Appendix Table 1).
Table 3.
Characteristics of included studies on hospitalization risk in Crohn’s Disease
| Biroulet et al, 2010 | USA | Olmsted County | 1970 – 2004 | 310 | All Ages | - | - | - | - | 5, 10, 30 | All-cause |
| Burisch et al, 2018 | Multiple European Countries | EPI-IBD | 2010 | 488 | Adults | M (50), F (50) | L1 (27), L2 (28), L3 (23), L4 (6) | 9 | B1 (71), B2 (21), B3 (8) | 1, 3, and 5 | All-cause and CD-related |
| Golovics et al, 2015 | Hungary | Veszprem Province | 2000 – 2010 | 331 | - | M (53), F (47) | L1 (35), L2 (32), L3 (33), L4 (1) | 17.8 | B1 (55), B2 (20), B3 (25) | 1, 3, and 5 | All-cause and CD-related |
| Jeuring et al, 2017 | Netherlands | IBD-SL | 1991 – 2011 | 1162 | Adults | M (37), F (63) | L1 (43), L2 (32), L3 (23), L4 (2) | 8.1 | B1 (82), B2 (12), B3 (6) | 1, 3, 5, and 10 | CD-related |
| Niewiadomski et al, 2015 | Australia | Barwon Area | 2007 – 2008, 2010 – 2013 | 146 | All Ages | M (47), F (53) | L1 (32), L2 (30), L3 (38), L4 (-) | 12 | B1 (80), B2 (10), B3 (10) | 1 and 5 | All-cause |
| Verdon et al, 2020 | Canada | RAMQ | 1996 – 2015 | 20644 | All Ages | M (43), F (57) | - | - | - | 5 | All-cause |
M: Male, F: Female, L1: Ileal, L2: Colonic, L3: Ileocolonic, L4: Upper GI Tract, B1: Inflammatory, B2: Fibrostenotic, B3: Penetrating, CD: Crohn’s Disease
Median (range) cumulative 1-, 3- and 5-year risk of CD-related hospitalization were 31.2% (range, 13.3–52.0%), 41.8% (range, 20.0–64.0%) and 48.9% (range, 23.9–65.9%), respectively. On meta-analysis, the cumulative incidence of CD-related hospitalization at 1-, 3-, and 5-years after diagnosis was 29.3% (95% CI, 20.0–40.8), 38.5% (95% CI, 26.8–51.7) and 44.3% (95% CI, 32.7–56.5), respectively, with considerable heterogeneity (I2=96–97%) (Figure 3). Two cohorts reported 59% to 72% 10-year cumulative incidence of CD-related hospitalization. Meta-analytic cumulative incidence of all-cause hospitalization at 1-, 3- and 5-years after diagnosis of CD were 31.0% (95% CI, 14.9–53.6), 44.1% (95% CI, 16.2–76.3), and 49.4% (95% CI, 37.5–61.4), respectively, with considerable heterogeneity (I2=97–99%) (eFigure 2). In cohorts reporting risk of CD-related hospitalization in the biologic era, 1-, 3- and 5-year risks were 25.6% (95% CI, 17.7–35.4), 33.7% (95% CI, 23.7–45.6) and 40.0% (95% CI, 29.2–51.8), respectively. In 4 cohorts, median 5-year risk of CD-related re-hospitalization after initial CD-related hospitalization was 32.3% (range, 29.8–38.4). Due to limited data on total person-year follow-up, we were unable to ascertain incidence rate of initial hospitalization and readmission.
Figure 3.
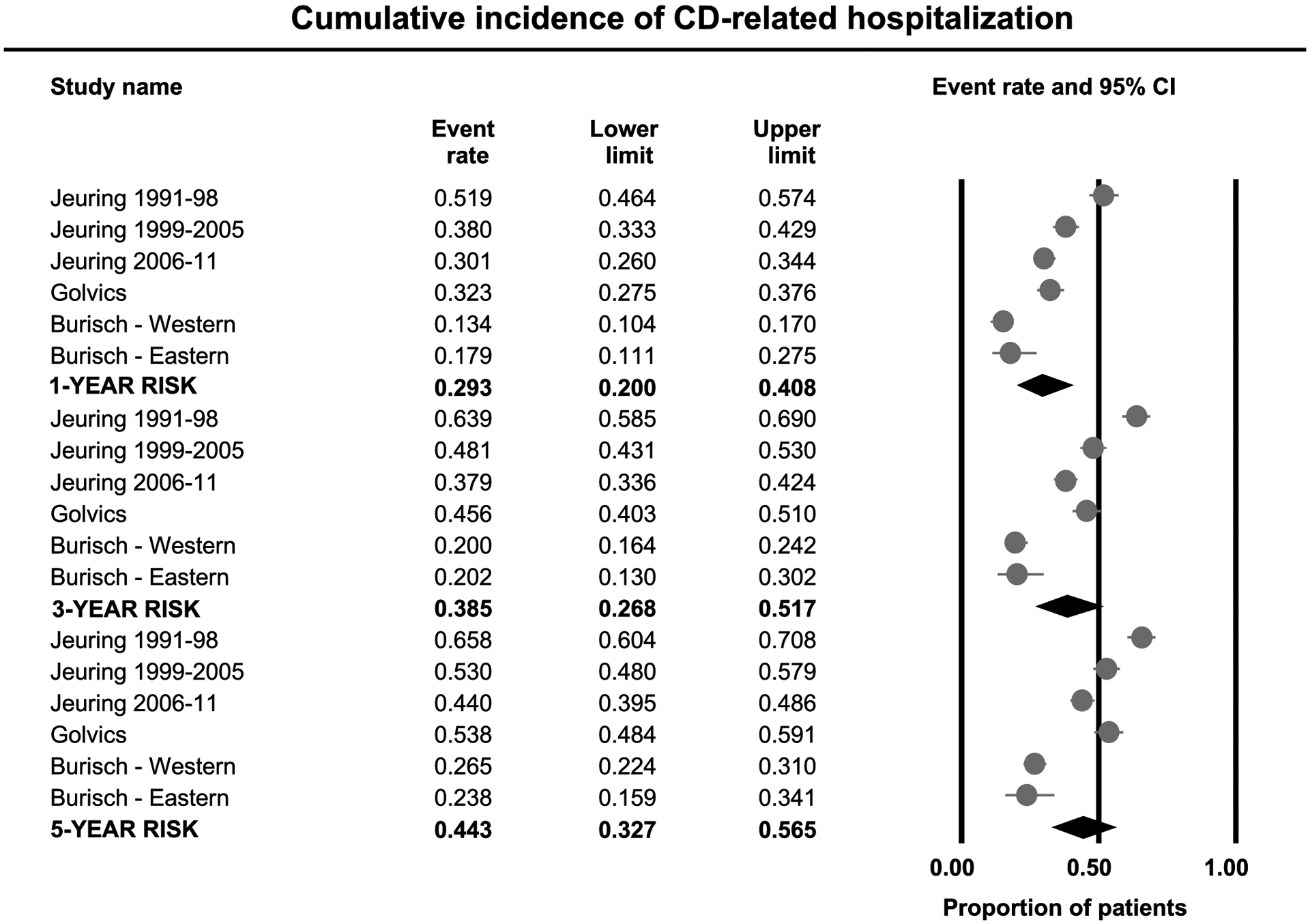
Cumulative 1-, 3- and 5-year risk of CD-related hospitalization in patients with Crohn’s disease.
Mixed-effects meta-regression suggested a higher 5-year risk of CD-related hospitalization in cohorts with higher prevalence of perianal CD (Table 2). Over time, there was a decline in 1- and 5-year risk of CD-related hospitalization based on mid-point of cohort entry (p<0.01). Subgroup analysis based on location was not feasible since studies outside Europe only reported all-cause hospitalization.
Risk Factors for Hospitalization in Patients with IBD
In patients with UC, extensive colitis (4 studies)16–19 and early need for corticosteroids and/or immunomodulators (3 studies)16, 18, 19 were most consistently associated with higher risk of hospitalization. Younger age at diagnosis, and high inflammatory burden (measured using C-reactive protein) were also associated with higher risk of hospitalization in one study each.
In patients with CD, penetrating and/or fistulizing disease (4 studies),20, 23–25 perianal disease (2 studies),20, 24 ileum-dominant disease (2 studies),20, 25 younger age at disease onset (2 studies) and early need for corticosteroids, immunomodulators and/or tumor necrosis factor-α antagonists (4 studies)22–25 were associated with increased risk of hospitalization.
DISCUSSION
In this systematic review of 10 population-based inception cohort studies, we made several key observations regarding risk of hospitalization. First, we observed that approximately one in 10 patients with UC will experience disease-related hospitalization within 1 year of diagnosis, and approximately one in five patients will experience the same within 5 years of diagnosis. In contrast, approximately one in 3 patients with CD will experience disease-related hospitalization within 1 year of diagnosis, and approximately one in two will experience the same within 5 years of diagnosis. This suggests a higher risk of hospitalization in patients with CD, as compared with UC. In contrast, among patients who have been hospitalized, we observed higher risk of readmission in patients with UC, as compared with CD. Second, we observed a steady decline in risk of hospitalization in patients diagnosed in a more contemporary era, both on meta-regression and sensitivity analysis. Third, in examining risk factors for hospitalization, through meta-regression and qualitative analysis of individual studies, we confirmed that phenotypes conventionally associated with more severe disease were associated with higher risk of hospitalization. Younger age at onset (both UC and CD), extensive colitis (UC), ileal-dominant CD, perianal CD and penetrating and/or stricturing behavior (CD) and early need for corticosteroids and immunosuppressive therapy (both UC and CD) were associated with increased risk of hospitalization. Overall, these findings from population-based cohort studies help contextualize anticipated cumulative incidence of unplanned healthcare utilization in newly diagnosed patients with IBD.
Prior studies have suggested a similar burden impact of UC and CD on patients’ quality of life and advocated for similar treatment goals and targets.26 However, untreated CD is associated with progressive bowel damage leading to strictures, fistulas or abscesses, leading to a high risk of surgery. While UC can be associated with bowel damage such as colonic strictures and post-inflammatory polyps, the burden and impact of damage is lower. In contemporary cohorts, cumulative 1- and 5-year risk of major abdominal surgery is significantly higher in patients with CD (12.3% and 18%) as compared to patients with UC (2.8% and 7.0%).27 We observed a similar pattern in risk of hospitalization, with a roughly 3-fold higher risk of disease-hospitalization in patients with CD as compared with patients with UC. Hence, while the impact of disease on quality of life may be comparable, CD is associated with higher rates of unplanned healthcare utilization. In contrast to initial hospitalization, risk of readmission was higher in patients with UC, as compared with CD. The reason for this is unclear, but may be related to difference in the nature of symptoms – persistent urgency and rectal bleeding, typical of UC, may prompt patients to seek urgent treatment, compared with pain-dominant CD. Similar trends regarding higher 30- and 90-day readmission were observed in chart-review based cohort studies. In a systematic review, Nghia and colleagues28 observed that risk of 30- and 90-day readmission was higher in studies in which the majority of patients had UC as compared to studies in which the majority of patients had CD.
Prior studies have cross-sectionally examined population-level annual trends in hospitalization in patients with IBD. Using multiple national databases, Ma and colleagues4 observed increased rates of unplanned healthcare utilization in patients with IBD, with increase in IBD-related hospitalization and ED visits, with plateauing of outpatient visits between 2006–15. Similar patterns were observed in healthcare spending in patients with IBD over the last two decades with disproportionate increase in spending on inpatient and ED care, without an increase in ambulatory care.7 In contrast, Rahman and colleagues5 observed a 32% decline in CD-related hospitalizations from 2003 to 2014 from 154/1000 patients to 104/1000 in a study using administrative data from Ontario, Canada. While these studies are helpful in informing the overall burden of IBD-related hospitalization to the health system, they do not provide patient-level risk estimates that are critical for prognostication for both patient care and development of risk-based treatment algorithms. Moreover, these studies could not comment on the effect of era of diagnosis on risk of hospitalization. Similar to the decline in risk of surgery in more contemporary cohorts, we observed that patients diagnosed in the biologic era (after 2000) had lower cumulative incidence of hospitalization, though the small number of studies precluded detailed analysis. The exact factors at play contributing to decrease in risk of hospitalization in patients with IBD are unclear, though the causes are likely multifactorial and merit further assessment. Over the last two decades, several therapeutic measures have improved disease outcomes including: (1) earlier and improved diagnosis, (2) increased number of, and potentially improved access to, gastroenterologists specializing in IBD, (3) introduction and increasing uptake of biologic agents like tumor necrosis factor-α antagonists, and (4) changes in approach to management of IBD with early use of disease-modifying immunosuppressive therapy and proactive disease monitoring and step-wise treatment intensification resulting in superior control of inflammation. In the 1980s, Munkholm and colleagues29 reported that 83% of patients with CD were hospitalized within 1 year of diagnosis; however, per their practice, hospitalization was encouraged to expedite evaluation. With increased understanding and improved diagnostic strategies, hospitalization is infrequently recommended now for expedited work-up. Nguyen and colleagues30 examined hospitalization rate (per 100 person-years) in patients diagnosed with CD between 1988–95, 1996–2000 and 2001–08, and observed no significant decline in rate of hospitalization within 1 year, 1–3 years and 3–5 years of diagnosis, based on era of diagnosis. While specialist gastroenterology care was associated with lower risk of surgery in their cohort, no effect was seen of specialist care was seen on hospitalization rate. In an updated analysis, access to specialists was associated with reduced risk of emergency department visits.31 Through claims-based analyses in Ontario, Murthy and colleagues32 determined that introduction of infliximab may not have resulted in substantial decline in risk of CD- and UC-related hospitalization, despite high market penetration in patients with CD. They attributed these findings to “misguided use of infliximab in CD patients and underuse of infliximab in UC”. Clinical monitoring and algorithmic treatment escalation may also decrease the risk of hospitalization in patients with CD.33, 34 54, 55 The population-wide, patient-level impact evolving treat-to-target strategies remains to be seen and will be better examined in the coming decade when there is penetration into routine clinical practice.
Despite the merits and strengths of our synthesis, there are important limitations. First, considerable heterogeneity was observed in most analyses. However, it is important to note that the implications and interpretation of a statistical measure as the inconsistency index is not the same for studies of incidence and prevalence, as for comparative observational or interventional studies. High statistical heterogeneity is often observed in these analyses, and only partly explained through meta-regression. Meta-regression was also limited by the small number of included studies. At the study design phase, we tried to minimize conceptual heterogeneity through strict inclusion and exclusion criteria. We did not account for within-study correlation, when examining different time points from the same study. Second, as noted earlier, we were unable to examine factors that may have contributed to a decline in risk of hospitalization. Threshold for hospitalization may vary geographically, based on access to healthcare resources. Future individual patient-level syntheses are required to comprehensively understand the multitude of factors that may contribute to declining hospitalization risks. Third, studies did not adequately report reasons for hospitalization and some studies only reported risk of all-cause hospitalization. While disease flare is the most common cause of hospitalization, treatment complications such as serious infections may be a cause for hospitalization in a small subset of patients, such as older and/or frail patients. Finally, in pooling cumulative incidence, we assumed complete follow-up of cohort which may lead to bias; however, mean duration of follow-up was generally in excess of 5-years for most of the population-based cohorts.
In conclusion, based on a systematic review of 10 population-based cohorts, we provide contemporary cumulative incidence of IBD-related and all-cause hospitalization in patients with UC and CD. Cumulative 5-year risk of hospitalization of 18.9% in UC, and 40.0% in CD in patients diagnosed early in the 21st century; this risk is lower than rates observed in patients diagnosed in the 20th century. These contemporary risks would help inform shared decision-making and health policy. Population health management strategies are required to identify patients at high risk of hospitalization and develop strategies to mitigate unplanned healthcare utilization.35
Supplementary Material
eFigure 1. Cumulative 1-, 3- and 5-year risk of all-cause hospitalization in patients with ulcerative colitis.
eFigure 2. Cumulative 1-, 3- and 5-year risk of all-cause hospitalization in patients with Crohn’s disease.
Disclosures:
Dr. Nguyen is supported by NIH/NIDDK (T32DK007202) and NIH/NLM (T15LM011271). Dr. Sandborn is supported in part by NIDDK-funded San Diego Digestive Diseases Research Center (P30 DK120515). Dr. Singh is supported by NIH/NIDDK (K23DK117058).
Conflicts of Interest:
Lester Tsai - None to declare
Nghia Nguyen - None to declare
Christopher Ma - consulting fees from AbbVie, Janssen, Takeda, Pfizer, Roche, Alimentiv (formerly Robarts Clinical Trials, Inc.); speaker’s fees from AbbVie, Janssen, Takeda, and Pfizer; research support from Pfizer
Larry J. Prokop - None to declare
William J. Sandborn - research grants from Abbvie, Abivax, Arena Pharmaceuticals, Boehringer Ingelheim, Celgene, Genentech, Gilead Sciences, Glaxo Smith Kline, Janssen, Lilly, Pfizer, Prometheus Biosciences, Seres Therapeutics, Shire, Takeda, Theravance Biopharma; consulting fees from Abbvie, Abivax, Admirx, Alfasigma, Alimentiv (Robarts Clinical Trials, owned by Health Academic Research Trust [HART]), Alivio Therapeutics, Allakos, Amgen, Applied Molecular Transport, Arena Pharmaceuticals, Bausch Health (Salix), Beigene, Bellatrix Pharmaceuticals, Boehringer Ingelheim, Boston Pharmaceuticals, Bristol Meyers Squibb, Celgene, Celltrion, Cellularity, Cosmo Pharmaceuticals, Escalier Biosciences, Equillium, Forbion, Genentech/Roche, Gilead Sciences, Glenmark Pharmaceuticals, Gossamer Bio, Immunic (Vital Therapies), Index Pharmaceuticals, Intact Therapeutics, Janssen, Kyverna Therapeutics, Landos Biopharma, Lilly, Oppilan Pharma, Otsuka, Pandion Therapeutics, Pfizer, Progenity, Prometheus Biosciences, Protagonists Therapeutics, Provention Bio, Reistone Biopharma, Seres Therapeutics, Shanghai Pharma Biotherapeutics, Shire, Shoreline Biosciences, Sublimity Therapeutics, Surrozen, Takeda, Theravance Biopharma, Thetis Pharmaceuticals, Tillotts Pharma, UCB, Vendata Biosciences, Ventyx Biosciences, Vimalan Biosciences, Vivelix Pharmaceuticals, Vivreon Biosciences, Zealand Pharma; and stock or stock options from Allakos, BeiGene, Gossamer Bio, Oppilan Pharma, Prometheus Biosciences, Progenity, Shoreline Biosciences, Ventyx Biosciences, Vimalan Biosciences. Spouse: Iveric Bio - consultant, stock options; Progenity - stock; Oppilan Pharma - consultant, stock options; Prometheus Biosciences - employee, stock options; Ventyx Biosciences - stock options; Vimalan Biosciences - stock options.
Siddharth Singh - research grants from AbbVie, Janssen
Footnotes
Publisher's Disclaimer: This AM is a PDF file of the manuscript accepted for publication after peer review, when applicable, but does not reflect post-acceptance improvements, or any corrections. Use of this AM is subject to the publisher’s embargo period and AM terms of use. Under no circumstances may this AM be shared or distributed under a Creative Commons or other form of open access license, nor may it be reformatted or enhanced, whether by the Author or third parties. See here for Springer Nature’s terms of use for AM versions of subscription articles: https://www.springernature.com/gp/open-research/policies/accepted-manuscript-terms
REFERENCES
- 1.Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet 2018;390:2769–2778. [DOI] [PubMed] [Google Scholar]
- 2.Coward S, Clement F, Benchimol EI, et al. Past and Future Burden of Inflammatory Bowel Diseases Based on Modeling of Population-Based Data. Gastroenterology 2019;156:1345–1353.e4. [DOI] [PubMed] [Google Scholar]
- 3.King JA, Underwood FE, Panaccione N, et al. Trends in hospitalisation rates for inflammatory bowel disease in western versus newly industrialised countries: a population-based study of countries in the Organisation for Economic Co-operation and Development. The Lancet Gastroenterology & Hepatology 2019;4:287–295. [DOI] [PubMed] [Google Scholar]
- 4.Ma C, Smith MK, Guizzetti L, et al. Assessing National Trends and Disparities in Ambulatory, Emergency Department, and Inpatient Visits for Inflammatory Bowel Disease in the United States (2005–2016). Clin Gastroenterol Hepatol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rahman A, Jairath V, Feagan BG, et al. Declining hospitalisation and surgical intervention rates in patients with Crohn’s disease: a population-based cohort. Aliment Pharmacol Ther 2019;50:1086–1093. [DOI] [PubMed] [Google Scholar]
- 6.Peery AF, Crockett SD, Murphy CC, et al. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2018. Gastroenterology 2019;156:254–272 e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dieleman JL, Cao J, Chapin A, et al. US Health Care Spending by Payer and Health Condition, 1996–2016. JAMA 2020;323:863–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dias CC, Santiago M, Correia L, et al. Hospitalization trends of the Inflammatory Bowel Disease landscape: A nationwide overview of 16 years. Dig Liver Dis 2019;51:952–960. [DOI] [PubMed] [Google Scholar]
- 9.Huh G, Yoon H, Choi YJ, et al. Correction: Trends in emergency department visits and hospitalization rates for inflammatory bowel disease in the era of biologics. PLoS One 2019;14:e0216768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009;151:264–9, W64. [DOI] [PubMed] [Google Scholar]
- 11.Frolkis AD, Dykeman J, Negron ME, et al. Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta-analysis of population-based studies. Gastroenterology 2013;145:996–1006. [DOI] [PubMed] [Google Scholar]
- 12.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177–88. [DOI] [PubMed] [Google Scholar]
- 13.Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Richardson MGP, Donegan S. Interpretation of subgroup analyses in systematic reviews: A tutorial. Clin Epidemiol Glob Health 2019;7:192–8. [Google Scholar]
- 15.Sterne JA, Egger M, Smith GD. Systematic reviews in health care: Investigating and dealing with publication and other biases in meta-analysis. BMJ 2001;323:101–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Burisch J, Katsanos KH, Christodoulou DK, et al. Natural Disease Course of Ulcerative Colitis During the First Five Years of Follow-up in a European Population-based Inception Cohort-An Epi-IBD Study. Journal of Crohn’s & colitis 2019;13:198–208. [DOI] [PubMed] [Google Scholar]
- 17.Jeuring SFG, Bours PHA, Zeegers MP, et al. Disease Outcome of Ulcerative Colitis in an Era of Changing Treatment Strategies: Results from the Dutch Population-Based IBDSL Cohort. Journal of Crohn’s & colitis 2015;9:837–45. [DOI] [PubMed] [Google Scholar]
- 18.Golovics PA, Lakatos L, Mandel MD, et al. Does Hospitalization Predict the Disease Course in Ulcerative Colitis? Prevalence and Predictors of Hospitalization and Re-Hospitalization in Ulcerative Colitis in a Population-based Inception Cohort (2000–2012). Journal of Gastrointestinal & Liver Diseases 2015;24:287–92. [DOI] [PubMed] [Google Scholar]
- 19.Samuel S, Ingle SB, Dhillon S, et al. Cumulative incidence and risk factors for hospitalization and surgery in a population-based cohort of ulcerative colitis. Inflammatory Bowel Diseases 2013;19:1858–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Niewiadomski O, Studd C, Hair C, et al. Prospective population-based cohort of inflammatory bowel disease in the biologics era: Disease course and predictors of severity. Journal of Gastroenterology & Hepatology 2015;30:1346–53. [DOI] [PubMed] [Google Scholar]
- 21.Verdon C, Reinglas J, Coulombe J, et al. Surgery and hospitalisations rates in inflammatory bowel disease patients in the Quebec provincial database from 199–6 to 2015. Journal of Crohn’s and Colitis 2019;13 (Supplement 1):S075–S076. [Google Scholar]
- 22.Jeuring SFG, van den Heuvel TRA, Liu LYL, et al. Improvements in the Long-Term Outcome of Crohn’s Disease Over the Past Two Decades and the Relation to Changes in Medical Management: Results from the Population-Based IBDSL Cohort. American Journal of Gastroenterology 2017;112:325–336. [DOI] [PubMed] [Google Scholar]
- 23.Burisch J, Kiudelis G, Kupcinskas L, et al. Natural disease course of Crohn’s disease during the first 5 years after diagnosis in a European population-based inception cohort: an Epi-IBD study. Gut 2018;01:23. [DOI] [PubMed] [Google Scholar]
- 24.Golovics PA, Lakatos L, Mandel MD, et al. Prevalence and predictors of hospitalization in Crohn’s disease in a prospective population-based inception cohort from 2000–2012. World Journal of Gastroenterology 2015;21:7272–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Biroulet LP, Loftus EV, Harmsen WS, et al. Emergency room visits and hospitalizations for Crohn’s disease in a population-based cohort. Gastroenterology 2010;1):S532. [Google Scholar]
- 26.Le Berre C, Ananthakrishnan AN, Danese S, et al. Ulcerative Colitis and Crohn’s Disease Have Similar Burden and Goals for Treatment. Clin Gastroenterol Hepatol 2020;18:14–23. [DOI] [PubMed] [Google Scholar]
- 27.Burr NE, Lord R, Hull MA, et al. Decreasing Risk of First and Subsequent Surgeries in Patients With Crohn’s Disease in England From 1994 through 2013. Clinical Gastroenterology & Hepatology 2019;17:2042–2049.e4. [DOI] [PubMed] [Google Scholar]
- 28.Nguyen NH, Koola J, Dulai PS, et al. Rate of Risk Factors for and Interventions to Reduce Hospital Readmission in Patients With Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bernstein CN, Loftus EV Jr., Ng SC, et al. Hospitalisations and surgery in Crohn’s disease. Gut 2012;61:622–9. [DOI] [PubMed] [Google Scholar]
- 30.Nguyen GC, Nugent Z, Shaw S, et al. Outcomes of patients with Crohn’s disease improved from 1988 to 2008 and were associated with increased specialist care. Gastroenterology 2011;141:90–7. [DOI] [PubMed] [Google Scholar]
- 31.Nguyen GC, Bouchard S, Diong C, et al. Access to Specialists and Emergency Department Visits in Inflammatory Bowel Disease: A Population-Based Study. Journal of Crohn’s & colitis 2019;13:330–336. [DOI] [PubMed] [Google Scholar]
- 32.Murthy SK, Begum J, Benchimol EI, et al. Introduction of anti-TNF therapy has not yielded expected declines in hospitalisation and intestinal resection rates in inflammatory bowel diseases: a population-based interrupted time series study. Gut 2019;12:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Colombel JF, Panaccione R, Bossuyt P, et al. Effect of tight control management on Crohn’s disease (CALM): a multicentre, randomised, controlled phase 3 trial. Lancet 2018;390:2779–2789. [DOI] [PubMed] [Google Scholar]
- 34.Khanna R, Bressler B, Levesque BG, et al. Early combined immunosuppression for the management of Crohn’s disease (REACT): a cluster randomised controlled trial. Lancet 2015;386:1825–34. [DOI] [PubMed] [Google Scholar]
- 35.Dulai PS, Singh S, Ohno-Machado L, et al. Population Health Management for Inflammatory Bowel Disease. Gastroenterology 2018;154:37–45. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Cumulative 1-, 3- and 5-year risk of all-cause hospitalization in patients with ulcerative colitis.
eFigure 2. Cumulative 1-, 3- and 5-year risk of all-cause hospitalization in patients with Crohn’s disease.


