Abstract
Background
To help implement behavior change interventions (BCIs) it is important to be able to characterize their key components and determine their effectiveness.
Purpose
This study assessed and compared the components of BCIs in terms of intervention functions identified using the Behaviour Change Wheel Framework (BCW) and in terms of their specific behavior change techniques (BCTs) identified using the BCT TaxonomyV1, across six behavioral domains and the association of these with cost-effectiveness.
Methods
BCIs in 251 studies targeting smoking, diet, exercise, sexual health, alcohol and multiple health behaviors, were specified in terms of their intervention functions and their BCTs, grouped into 16 categories. Associations with cost-effectiveness measured in terms of incremental cost-effectiveness ratio (ICER) upper and lower estimates were determined using regression analysis.
Results
The most prevalent functions were increasing knowledge through education (72.1%) and imparting skills through training (74.9%). The most prevalent BCT groupings were shaping knowledge (86.5%), changing behavioral antecedents (53.0%), supporting self-regulation (47.7%), and providing social support (44.6%). Intervention functions associated with better cost-effectiveness were those based on training (βlow = −15044.3; p = .002), persuasion (βlow = −19384.9; p = .001; βupp = −25947.6; p < .001) and restriction (βupp = −32286.1; p = .019), and with lower cost-effectiveness were those based on environmental restructuring (β = 15023.9low; p = .033). BCT groupings associated with better cost-effectiveness were goals and planning (βlow = −8537.3; p = .019 and βupp = −12416.9; p = .037) and comparison of behavior (βlow = −13561.9, p = .047 and βupp = −30650.2; p = .006). Those associated with lower cost-effectiveness were natural consequences (βlow = 7729.4; p = .033) and reward and threat (βlow = 20106.7; p = .004).
Conclusions
BCIs that focused on training, persuasion and restriction may be more cost-effective, as may those that encourage goal setting and comparison of behaviors with others.
Keywords: BCT, Smoking, Diet, Exercise, Sexual health, Alcohol
Behaviour change interventions that focus on training, persuasion and restriction may be more cost-effective, as may those that encourage goal setting and comparison of behaviors with others
Introduction
Physical inactivity, smoking, excessive alcohol consumption, unprotected sex, and poor diet cost the National Health Service (NHS) in England more than £14 billion per year [1–4] and also adversely affect the local economy [5–7]. Although developing interventions to change behavior (BCIs) is a key objective of public health there is a significant challenge of translating such interventions into routine practice [8]. Many factors contribute to this problem including poor specification of the key components of BCIs [9]. Thus this study aims to provide an evidence synthesis of the key components of BCIs across six domains (smoking, diet, physical activity, alcohol, sexual health, and multiple behaviors) and the association of these with cost-effectiveness using a reliable theory-based coding system [10, 11]. Consideration of cost-effective and not just effective interventions is important as it will aid evidence-based practice and the application of BCIs in the public domain. Part of the failure to implement interventions in the real world results not only from the ability to duplicate the components of the original intervention but also the availability of key resources. Identifying the key components of cost-effective interventions will help decision makers maximize the public’s health with the allocated resources.
BCIs are “coordinated sets of activities designed to change specified behavior patterns,” for example, to help people stop smoking or to increase their exercise levels [10]. BCIs can be characterized in terms of both “content” (active ingredients of the intervention) and “delivery” (manner in which the content is applied, for example, level of intensity of the intervention and setting). Although the complexity of BCIs means that it is not possible to capture every aspect of the content, it is possible to record some key features using coding systems that can be used with an acceptable degree of reliability [11]. One of these coding systems is known as the Behaviour Change Wheel (BCW) [10, 12]. The BCW is a behavioral system, the hub of which specifies that for behavior change to occur one needs three conditions: capability, opportunity and motivation (COM-B). Around this hub, nine intervention functions are positioned which capture ways in which an intervention can change behavior: education, persuasion, incentivization, coercion, training, restriction, environmental restructuring, modeling, and enablement. These intervention functions can then be implemented in an intervention using one of 93 proposed behavior change techniques (BCTs) [11].
Examples of studies that have attempted to identify intervention features associated with effectiveness can be seen across behavioral domains. Diet interventions using the BCTs barrier identification/problem solving, plan social support/social change, goal setting (outcome), use of follow-up prompts, and provide feedback on performance have been associated with greater fruit and vegetable consumption compared with studies not using these BCTs [13]. Physical activity interventions using feedback have been deemed more effective than those not using this, while interventions providing information on where and when to perform the behavior and information on consequences of behavior to the individual appear to be less effective than interventions not using these [14]. Several BCTs have been identified in effective smoking cessation interventions aimed at pregnant smokers including facilitate goal setting, advise on social support, and action planning [15, 16]. It is important to extend these findings to include the association with cost-effectiveness, given that implementing recommendations for providing interventions depends not only on the potential benefits but also on the cost of the intervention under consideration. Although intervention functions and BCTs present in cost-effective interventions have been identified before, with the most prevalent being education and shaping knowledge respectively [17], no study to our knowledge has considered both cost-effective and ineffective interventions and the features commonly associated with each of these.
The current study therefore aimed to:
Characterize BCIs according to their intervention functions [10, 12] and BCTs [11].
Compare the intervention functions and BCTs used to address smoking, diet, physical activity, alcohol, sexual health, and multiple health behaviors.
Identify associations between intervention characteristics and cost-effectiveness (using a threshold of £20,000–£30,000 per quality-adjusted life years (QALY))
Methods
Stage 1: Identification and Retrieval of Source Material
The search strategy was conducted by Bazian Ltd for the National Institute for Health and Care Excellence (formally the National Institute for Clinical Excellence) in the databases ECONLIT, NHS EED, and HEED for papers/reviews published between January 2003 and September 2012. Studies were included if they: (a) covered interventions aimed at behavior change in relation to at least one of the following: alcohol, diet, physical activity, sexual behavior, smoking, or multiple behaviors, (b) had conducted an economic analysis, and (c) were randomized controlled trials or systematic reviews published in English. In cases where insufficient detail was provided on intervention content in systematic reviews/meta-analyses, such reviews were excluded as limited resources did not allow retrieval of all primary data and the limited information provided would have biased results. Studies were excluded if they focused on people younger than 16 years and national policy, fiscal and legislative measures.
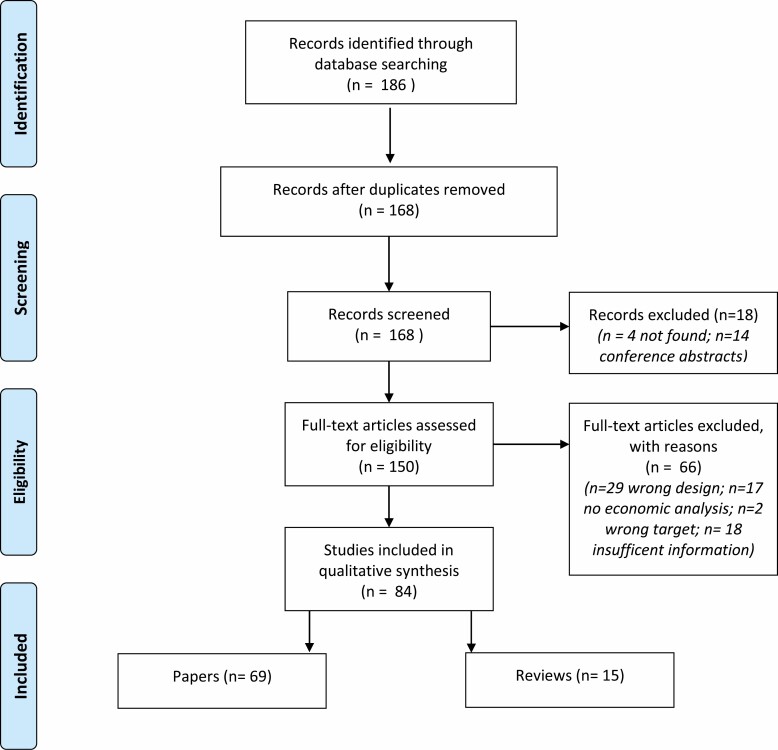
Sixty-nine papers and 15 reviews were identified (see Fig. 1), which covered 251 eligible interventions (see Appendix 1 for further details). The majority of these reported cost-effectiveness (CEA) (n = 65) or a cost-utility (CUA) (n = 102) economic analysis. Both CEA and CUA focus on the cost per unit of health gained of one compared with another intervention, yielding an incremental cost-effectiveness ratio (ICER). While CEA express this in cost per unadjusted health gain (e.g., measures the benefit using single unidimensional outcomes, for example, life-years (LY) saved), CUA is a special form of CEA which also adjusts health benefits for quality of life (e.g., QALY which captures both duration and quality of life). Where necessary estimates were converted into GBP at the time of the original analysis or, when this information was not available, at the time of the paper publication.
Fig. 1.
PRISMA flow diagram of included and excluded studies.
As some of the economic assessments carried out sensitivity analyses, varying cost-effectiveness estimates based on several factors such as user characteristics, and time horizons were calculated, and so, both lower (most optimistic) and upper (most pessimistic) limits of cost-effectiveness estimates were recorded. In cases where no sensitivity analysis was carried out, the single estimate was included as both the lower and upper limits. Cost-effectiveness was determined according to the National Institute for Health and Care Excellence (NICE) guidelines. NICE have adopted a CUA-based cost-effectiveness threshold of £20,000–£30,000 per QALY above which interventions are unlikely to be recommended [18].
The remaining 84 interventions used either cost–benefit analysis (CBA) or cost-consequence analysis (CCA) which yield data not expressed in (adjusted) life-years saved. CBA expresses all direct and indirect costs and benefits in a common unit, in monetary terms, and enables calculation of net benefit (unit difference of benefits minus costs). CCA is a special form of CBA which does not attempt to express all costs and benefits in the same unit of measurement and therefore does not aggregate findings into a single indicator.
Stage 2: Characterization of Interventions
The content of interventions was characterized using two methods. The first identified their intervention functions as defined in the Behaviour Change Wheel (BCW) framework [12] (see Electronic Supplementary Table 1). Interventions were also coded using a taxonomy of 93 BCTs (BCT Taxonomy v1 [11]), with 16 groupings. Following Michie et al.’s [11] guidelines, BCTs were coded only where coders believed that there was unequivocal evidence of their inclusion in a given intervention. All papers were coded by EB and a subset of 28 papers (29.2%) was coded in batches by a second coder (FL) with disagreements resolved through discussion after each batch. Agreement was 99.2%, with a mean Cohen’s kappa of .89, indicating good inter-rater reliability [19].
Interventions were also categorized in terms of a range of factors relating to their context and delivery: intervention level (e.g., individual vs. population), delivery agent type (e.g. health care professional vs. physicians), and intensity (e.g., high vs. medium vs. low e.g. minimal contact, some contact and multiple contacts) [20–22] (see Electronic Supplementary Table 2).
Analysis
All data were extracted into a data extraction form and then transferred into IBM SPSS. Interventions were assigned to one of six categories: alcohol, diet, smoking, physical activity, sexual-health interventions, and interventions targeting multiple health behaviors. Differences according to intervention characteristics were analyzed using t-tests or one-way ANOVAs and χ2 or Fisher Exact tests for continuous and categorical variables, respectively. The Tukey correction was applied in post hoc analyses.
To meaningfully interpret data and maintain consistency with NICE guidelines, only the 102 interventions where cost-effectiveness status was based on analyses expressed in cost per DALY/QALY gained were included in the primary analysis comparing BCTs of interventions appraised as cost-effective and cost-ineffective according to NICE threshold. Sixty-two percent (n = 63) used a single CUA estimate and 38% (n = 39) provided multiple upper and lower CUA estimates. Data were analyzed using linear regression models with the estimates entered as a continuous dependent variable.
As a sensitivity analysis, we included all studies with a binary outcome (n = 251) of cost-effective versus cost-ineffective. For this variable, cost-effectiveness was based on meeting at least one out of five cost-effectiveness conditions. These conditions were: being below the £20,000 threshold for the upper limit; below £20,000 for the lower limit; below £30,000 for the upper limit; below £30,000 for the lower limit or the original authors’ appraisal that the intervention was cost-effective. Thus if either the lower or upper estimates or both were less than the specified threshold the intervention was deemed cost-effective. Data were analyzed using logistic regression models with the estimate as a binary variable of cost-effective versus not cost-effective.
Unadjusted and adjusted regression models are reported, with variables selected using forward stepwise selection based on the Likelihood Ratio. Analyses were not conducted for individual health behaviors given the small sample size and lack of power.
Results
More than a third of the 251 identified interventions were smoking cessation interventions (n = 92). The next most prevalent category was multiple health-related behavior interventions (n = 48) and interventions to improve sexual health (n = 44). Thirty-nine interventions considered diet and 28 interventions focused on physical activity, while only 8 alcohol interventions were identified. There was a fairly equal split between different intervention categories with the exception of mass media interventions which featured only five times. Control conditions mostly consisted of usual care, and fewer than 10% of interventions studies used a matched control condition (see Table 1).
Table 1.
Intervention characteristics by health behavior
| All (n = 251) | Smoking (n = 92) | Diet (n = 39) | Physical activity (n = 20) | Alcohol (n = 8) | Sexual health (n = 44) | Multiple targets (n = 48) | p* | |
|---|---|---|---|---|---|---|---|---|
| Category | a | b | b, c | b, c | c | b, c | ||
| Med | 14.7 (37) | 29.3 (27) | 20.5 (8) | 0.0 (0) | 0.0 (0) | 2.3 (1) | 2.1 (1) | |
| BI | 22.3 (56) | 13.0 (12) | 30.8 (12) | 55.0 (10) | 75.0 (6) | 15.9 (7) | 18.8 (9) | |
| Med + BI | 13.9 (35) | 26.1 (24) | 2.6 (1) | 0.0 (0) | 0.0 (0) | 18.2 (8) | 4.2 (2) | <.001 |
| Comp | 34.7 (87) | 10.9 (10) | 38.5 (15) | 45.0 (9) | 25.0 (2) | 43.2 (19) | 66.7 (32) | |
| Med + Comp | 12.4 (31) | 20.7 (19) | 2.6 (1) | 0.0 (0) | 0.0 (0) | 15.9 (7) | 8.3 (4) | |
| Mass media | 2.0 (5) | 0.0 (0) | 5.1 (2) | 5.0 (1) | 0.0 (0) | 4.5 (2) | 0.0 (0) | |
| Control condition | a | a, b | a, b | a, b | b | a, b | ||
| Nothing/UC | 66.9 (168) | 55.4 (51) | 61.5 (24) | 75.0 (15) | 50.0 (4) | 88.6 (39) | 72.9 (35) | |
| Lower impact | 25.1 (63) | 34.8 (32) | 33.3 (13) | 20.0 (4) | 37.5 (3) | 6.8 (3) | 16.7 (8) | <.001 |
| Matched impact | 8.0 (20) | 9.8 (9) | 5.1 (2) | 5.0 (1) | 12.5 (1) | 4.5 (2) | 10.4 (5) | |
| Intervention intensity | a | b | a, b | a, b, c | a | c | ||
| Unclear | 4.8 (12) | 0.0 (0) | 12.8 (5) | 5.0 (1) | 0.0 (0) | 2.3 (1) | 10.4 (5) | |
| Low | 38.2 (96) | 57.6 (53) | 43.6 (17) | 40.0 (8) | 25.0 (2) | 29.5 (13) | 6.2 (3) | <.001 |
| Medium | 24.3 (61) | 20.7 (19) | 10.3 (4) | 30.0 (6) | 25.0 (2) | 40.9 (18) | 25.0 (12) | |
| High | 32.7 (82) | 21.7 (20) | 33.3 (13) | 25.0 (5) | 50.0 (4) | 27.3 (12) | 58.3 (28) | |
| Setting | a | b, c | c | a, b | b, c | b, c | ||
| Primary care | 65.3 (164) | 85.9 (79) | 53.8 (21) | 40.0 (8) | 75.0 (6) | 65.9 (29) | 43.1 (21) | |
| Secondary care | 6.4 (16) | 2.2 (2) | 15.4 (6) | 0.0 (0) | 25.0(2) | 0.0 (0) | 12.5 (6) | |
| Community | 17.1 (43) | 7.6 (7) | 15.4 (6) | 35.0 (7) | 0.0 (0) | 20.5 (9) | 29.2 (14) | <.001 |
| Workplace | 1.6 (4) | 3.3 (3) | 2.6 (1) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) | |
| Unclear/other≠ | 9.6 (24) | 1.1 (1) | 12.8 (5) | 25.0 (5) | 0.0 (0) | 13.6 (6) | 14.6 (7) | |
| Delivery mode | a | a, b | b | a, b | a, b | a, b | ||
| Physician | 9.2 (23) | 15.4 (14) | 17.9 (7) | 0.0 (0) | 0.0 (0) | 2.3 (1) | 2.1 (1) | |
| HP | 66.4 (166) | 65.9 (60) | 43.6 (17) | 65.0 (13) | 100.0 (15) | 77.3 (34) | 70.8 (34) | |
| Media | 4.0 (10) | 0.0 (0) | 7.7 (3) | 15.0 (3) | 0.0 (0) | 4.5 (2) | 4.2 (2) | .015 |
| Mix | 4.4 (11) | 4.4 (4) | 7.7 (3) | 5.0 (1) | 0.0 (0) | 2.3 (1) | 4.2 (2) | |
| Unclear/other± | 16.0 (40) | 14.3 (13) | 23.1 (9) | 15.0 (3) | 0.0 (0) | 13.6 (6) | 18.8 (9) | |
| Target level | ||||||||
| Individual | 84.1 (211) | 94.6 (87) | 74.4 (29) | 85.0 (17) | 62.5 (5) | 79.5 (35) | 79.2 (38) | |
| Groups | 8.4 (21) | 3.3 (3) | 10.3 (4) | 10.0 (2) | 37.5 (3) | 6.8 (3) | 12.5 (6) | .037 |
| Population | 2.4 (6) | 0.0 (0) | 5.1 (2) | 5.0 (1) | 0.0 (0) | 4.5 (2) | 2.1 (1) | |
| Mix | 5.2 (13) | 2.2 (2) | 10.3 (4) | 0.0 (0) | 0.0 (0) | 9.1 (4) | 6.2 (3) | |
| Population | a | b,c | b,c | b,c | b | c | ||
| General | 49.0 (123) | 14.1 (13) | 64.1 (25 | 55.0 (11) | 87.5 (7) | 56.8 (25) | 87.5 (42) | <.001 |
| Vulnerable* | 51.0 (128) | 85.9 (79) | 35.9 (14) | 45.0 (9) | 12.5 (1) | 43.2 (19) | 12.5 (6) | |
| Supporting material | ||||||||
| None | 70.5 (177) | 69.6 (64) | 76.9 (30) | 55.0 (11) | 87.5 (7) | 79.5 (35) | 62.5 (30) | |
| Self-help | 9.2 (23) | 14.1 (13) | 7.7 (3) | 15.0 (3) | 12.5 (1) | 2.3 (1) | 4.2 (2) | .178 |
| Electronic | 10.4 (26) | 8.7 (8) | 5.1 (2) | 15.0 (3) | 0.0 (0) | 9.1 (4) | 18.8 (9) | |
| Mix | 10.0 (25) | 7.6 (7) | 10.3 (4) | 15.0 (3) | 0.0 (0) | 9.1 (4) | 14.6 (7) | |
| Pharmacological support | 43.8 (110) | 78.3 (72)a | 33.3 (13)b | 0 (0)c | 0.0 (0)b,c | 36.4 (16)b | 18.8(9)b,c | <.001 |
| Social marketing | 4.0 (10) | 0 (0) | 5.1 (2) | 15.0 (3) | 0 (0) | 6.8 (3) | 4.2 (2) | .025 |
| Incentives | 4.4 (11) | 4.3 (4) | 2.6 (1) | 20.0 (4) | 0 (0) | 2.3 (1) | 2.1 (1) | 0.116 |
| Cost-effective^ | 87.6 (220) | 93.5 (86)a | 84.6 (35)a, b | 95.0 (21)a, b | 100.0 (8)a, b | 88.6 (44)a, b | 72.9 (36)b | 0.012 |
Note: ≠Refers to state/policy level interventions (e.g., changes in legislation/physical infrastructure) or interventions in nonspecific settings (e.g., online/phone interventions).
±This refers to delivery by peers, teachers, researchers or the state.
^ Based on CUA (N = 102) and non-CUA (N = 149) cost-effectiveness studies.
*Vulnerable includes pregnant women, individuals at risk of disease, those from low socio-economic groups and patient populations.
a, b, c: Comparison of interventions targeting different health-related behaviors, different letters indicate significant difference at p < .05 (Bonferroni-corrected).
BI, brief intervention; Med, medication; Comp, comprehensive; UC, usual care; HP, healthcare professional (nurse, pharmacist, psychologist etc.).
Broad Characterization of Interventions
Overall
Table 1 shows the broad characteristics of the identified interventions. Over a third of interventions were classified as being of low intensity (i.e., mostly brief or pharmacological interventions), mainly set in primary care and were delivered by health professionals. Interventions most frequently targeted individuals from both general and vulnerable populations (e.g., pregnant women, individuals at risk of disease, those from low socio-economic groups and patient populations). Over four-fifths of interventions were considered cost-effective.
By behavioral domain
Smoking cessation interventions compared with others most commonly involved medication. The majority of smoking cessation and alcohol interventions were set in primary care compared with less than half of physical activity interventions. While the majority of smoking cessation and sexual health intervention was aimed at vulnerable populations, other heath behavior interventions tended to target the general population, in particular those aimed at changing multiple behaviors (see Table 1)
Intervention Functions
Overall
The most prevalent functions, identified in three-quarters of interventions, were to increase knowledge and/or understanding through education as well as to impart skills through training (see Table 2). Nearly half of the interventions aimed to increase capability and/or opportunity and a quarter of interventions used persuasion to encourage behavior change. Environmental restructuring by changing physical or social contexts or using incentives to create an expectation of reward was relatively uncommon as were restriction and modeling, while none used coercion.
Table 2.
Intervention characteristics by health-related behavior
| All (n = 251) | Smoking (n = 92) | Diet (n = 39) | Physical activity (n = 20) | Alcohol (n = 8) | Sexual health (n = 44) | Multiple targets (n = 48) | p* | |
|---|---|---|---|---|---|---|---|---|
| Training | 74.9 (188) | 78.2 (72)a,c | 92.3 (36)c | 35.0 (7)b | 50.0 (4)a,b,c | 56.8 (25)a,b | 91.7 (42)c | <.001 |
| Education | 72.1 (181) | 62.0 (57)a | 66.7 (26)a,b | 65.0 (13)a,b | 100.0 (8)a,b | 77.3 (34)a,b | 89.6 (43)b | .001 |
| Enablement | 45.8 (115) | 72.8 (67)a | 30.8 (12)b | 10.0 (2)b | 0 (0)b | 36.4 (16)b | 37.5 (18)b | <.001 |
| Persuasion | 24.7 (62) | 33.7 (31)a,c | 2.6 (1)b | 35.0 (7)a,c | 62.5 (5)a | 27.3 (12)a,c | 12.5 (6)b,c | <.001 |
| Environmental restructuring | 5.2 (13) | 6.5 (6) | 7.7 (3) | 15.0 (3) | 0 (0) | 0 (0) | 2.1 (1) | .071 |
| Incentivization | 4.0 (10) | 4.3 (4) | 2.6 (1) | 10.0 (2) | 0 (0) | 2.3 (1) | 4.2 (2) | .730 |
| Restriction | 2.8 (7) | 0 (0)a | 15.4 (6)b | 0 (0)a,b | 0 (0)a,b | 0 (0)a,b | 2.1 (1)a,b | .001 |
| Modelling | 1.2 (3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2.3 (1) | 4.2 (2) | .273 |
| Coercion | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | NC |
Note: *Significant overall differences are in italics.
a, b, c: Comparison of interventions targeting different health-related behaviors, different letters indicate significant difference at p < .05 (Bonferroni-corrected).
NC, cannot be computed.
By behavioral domain
Intervention functions differed according to the health-related behavior targeted. The use of training was significantly more prevalent in diet interventions and interventions aimed at changing multiple behaviors than in physical activity and sexual health interventions. The use of education was lowest in smoking cessation interventions compared with multiple behavior interventions. Smoking cessation interventions were much more likely than interventions aimed at changing any other health-related behavior to employ the enablement function (see Table 2). Alcohol and smoking cessations were also more likely than interventions targeting multiple health-related behaviors or diet interventions to employ persuasion, whereas restriction was more prevalent in the diet than in smoking cessation interventions.
BCT Groupings in Interventions
Overall
BCTs were grouped as shown in Table 3. Out of a total of 16 BCT groupings, four (shaping knowledge, antecedents, regulation and social support) were particularly prevalent, evident in about half of the interventions considered. A further five BCT groupings (comparison of outcomes, feedback and monitoring, goals and planning, natural consequences, and self-beliefs) were commonly identified, evident in a fifth to a third of interventions. The remainder were coded in less than 10% of interventions with very few using identity, scheduled consequences and covert learning.
Table 3.
BCT groupings and total number of BCTs by health-related behavior
| All (n = 251) | Smoking (n = 92) | Diet (n = 39) | Physical activity (n = 20) | Alcohol (n = 8) | Sexual health (n = 44) | Multiple targets (n = 48) | p* | |
|---|---|---|---|---|---|---|---|---|
| % (n) | ||||||||
| Shaping knowledge (BCT36–39) | 86.5 (217) | 92.4 (85)a,c | 89.7 (35) a,b,c | 55.0 (11)b | 50.0 (4)a,b | 95.5 (42)c | 83.3 (40)a,b,c | <.001 |
| Antecedents (BCT30–35) | 53.0 (133) | 76.1 (70)a | 56.4 (22)a,b | 35.0 (7)b,c | 0 (0)c | 43.2 (19)b,c | 31.2 (15)b,c | <.001 |
| Regulation (BCT4–7) | 47.7 (119) | 78.3 (72)a | 35.9 (14)b,d | 0 (0)c | 0 (0)b,c | 52.3 (23)b | 20.8 (10)c,d | <.001 |
| Social support (BCT1–3) |
44.6 (112) | 43.5 (40) | 33.3 (13) | 50.0 (10) | 87.5 (7) | 38.6 (17) | 52.1 (25) | .062 |
| Comparison of outcomes (BCT74–BCT76) | 37.1 (93) | 44.6 (41)a,b | 20.5 (8)a | 25.0 (5)a,b | 25.0 (2)a,b | 22.7 (10)a | 56.3 (27)b | .001 |
| Feedback and monitoring (BCT8–14) | 27.1 (68) | 9.8 (9)a | 38.5 (15)b | 20.0 (4)a,b | 75.0 (6)b | 25.0 (11)a,b | 47.9 (23)b | <.001 |
| Goals and planning (BCT65–73) |
26.7 (67) | 16.3 (15)a | 20.5 (8)a | 30.0 (6)a,b | 50.0 (4)a,b | 20.5 (9)a | 52.1 (25)b | <.001 |
| Natural consequences (BCT82–87) | 22.7 (57) | 8.7 (8)a | 23.1 (9)a,b | 15.0 (3)a,b | 12.5 (1)a,b | 45.5 (20)b | 33.3 (16)b | <.001 |
| Self-beliefs (BCT40–43) | 22.3 (56) | 28.3 (26)a | 2.6 (1)b | 40.0 (8)a | 37.5 (3)a,b | 27.3 (12)a | 12.5 (6)a,b | <.001 |
| Repetition and substitution (BCT23–29) | 10.0 (25) | 0 (0)a | 7.7 (3)a | 10.0 (2)a,b | 0 (0)a,b | 4.5 (2)a | 37.5 (18)b | <.001 |
| Comparison of behavior (BCT88–90) | 9.6 (24) | 1.1 (1)a | 7.7 (3)a,b | 0 (0)a,b | 0 (0)a,b | 13.6 (6)a,b | 29.2 (14)b | <.001 |
| Associations (BCT15–22) | 9.2 (23) | 8.7 (8) | 7.7 (3) | 15.0 (3) | 0 (0) | 9.1 (4) | 10.4 (5) | .783 |
| Reward and threat (BCT54–64) |
6.8 (17) | 6.5 (6) | 2.6 (1) | 20.0 (4) | 0 (0) | 2.3 (1) | 10.4 (5) | .107 |
| Identity (BCT77–81) |
0.8(2) | 1.1 (1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2.1 (1) | .768 |
| Scheduled consequences (BCT44–53) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | NC |
| Covert learning (BCT91–93) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | NC |
| Mean (range) | ||||||||
| Number of BCT groupings | 4.0 (1-9) | 4.2 (1-8)a,b | 3.5 (1-6)a | 3.2 (1-7)a | 3.4 (2-4)a,b | 4.0 (2-7)a,b | 4.8 (1-9)b | <.001 |
Note: *Significant overall differences are in italics.
a, b, c, d: Comparison of interventions targeting different health-related behaviors, different letters indicate significant difference at p < .05 (Bonferroni-corrected).
NC, cannot be computed.
By behavioral domain
The prevalence of BCT groupings differed by behavioral domain (see Table 3). Shaping knowledge and the use of antecedents was prevalent in smoking, diet, and sexual health interventions. Regulatory BCTs were particularly prevalent in smoking cessation interventions but not present in physical activity or alcohol interventions. Interventions with multiple behavioral targets often focused on comparison of outcomes and goals and planning, the former being less prevalent in diet and sexual health interventions and the latter in smoking cessation interventions. The use of feedback and monitoring was most prevalent in interventions for diet, alcohol and multiple health behavior targets but relatively rare in smoking cessation interventions. BCTs concerning self-beliefs were particularly uncommon in diet interventions. BCTs that highlighted natural consequences were present in nearly half of sexual health interventions and a third of interventions with multiple behavioral targets but relatively uncommon in other interventions, particularly smoking cessation interventions. Smoking cessation also rarely include BCTs that involved repetition and substitution or which instigated comparison of behavior, particularly when compared with multiple health-related behavior interventions. The only BCT grouping that was equally present across all health-related behavioral interventions was social support.
BCTs in Interventions
Overall
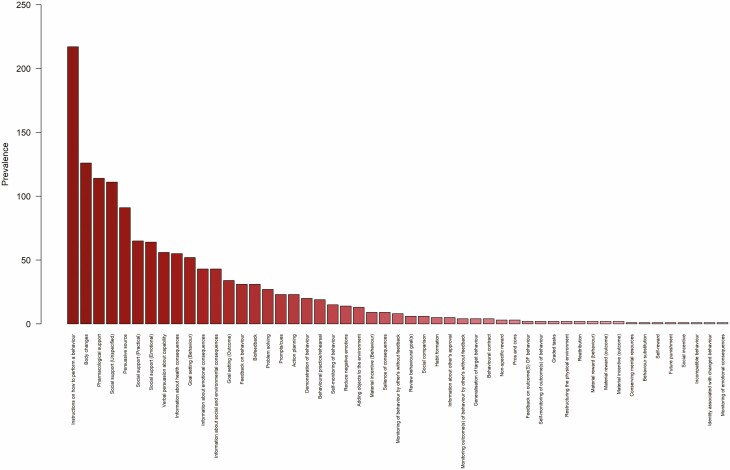
Out of 93 possible BCTs, the average intervention contained just five BCTs. A total of 51 BCTs were coded for in at least one interventions (see Fig. 2). Instructions on how to perform a behavior (e.g., advise the person how to use nicotine replacement therapy) was by far the most prevalent of BCTs, being reported in nearly nine out of ten interventions. Body changes (e.g., prompt strength training), pharmacological support (e.g., suggest the patient asks the family physician for nicotine replacement therapy) and unspecified social support (e.g., live information about a self-help alcohol group) were also prevalent in nearly half of all interventions analyzed. A third of interventions made use of a persuasive source (e.g., present a speech given by a high status professional to emphasize the importance of a healthy diet) and a quarter included practical or emotional social support (e.g., ask a partner of the patient to exercise with them) or used verbal persuasion (e.g., tell the person they can successfully increase their physical activity)to increase capability.
Fig. 2.
Prevalence of individual BCTs across all interventions. Note: Only BCTs described in at least one interventions are shown.
By behavioral domain
There were significant differences in the number of BCTs included in interventions across the behavioral domains (F(5, 245) = 4.29, p = .001). Interventions with multiple behavior targets included significantly more BCTs (mean = 7.1, median = 6.5, mode = 4), than smoking cessation (mean = 4.9, median = 4, mode = 4; p = .001), diet (mean = 4.7, median = 4, mode = 3; p = .005) and physical activity (mean = 4.6, median = 4, mode = 4; p = 0.042) interventions. There were no differences in the number of BCTs included in sexual health (mean = 5.9, median = 5, mode = 3) or alcohol interventions (mean = 5.8, median = 6, mode = 7).
A total of 30 distinct BCTs were coded at least once in 92 smoking cessation interventions, 29 BCTs in 39 diet interventions and 27 BCTs in 20 physical activity interventions (see Electronic Supplementary Figs. 1–3). The most prevalent BCT (recorded in over 90% of the diet and smoking cessation interventions and over 50% of physical activity interventions) was the inclusion of instructions on how to perform a behavior. The next most prevalent used BCT in diet and smoking cessation interventions was bodily changes, while nonspecific support was the second most prevalent in physical activity interventions. Three-quarters of smoking cessation interventions also discussed providing pharmacological support and just under half involved the inclusion of a persuasive source and provided nonspecific social support. Around a third of diet interventions also provided unspecified social support and pharmacological support and a quarter included practical and emotional social support.
Alcohol interventions included the fewest number of BCTs (n = 13) (see Electronic Supplementary Fig. 4). Nearly all alcohol interventions provided unspecified social support and three quarters also offered practical and emotional social support and provided biomarker feedback (e.g., inform the person of their blood pressure reading to improve adoption of health behaviors). Across 44 sexual health interventions, 30 BCTs were coded (see Electronic Supplementary Fig. 5). Most of the interventions included instructions on how to perform a desired behavior and around half also provided pharmacological support or information about health consequences (e.g., present the likelihood of contracting a sexually transmitted infection following unprotected sexual behavior). Finally, 40 BCTs were coded across the 48 interventions targeting multiple behaviors (see Electronic Supplementary Fig. 6). The most common ones were instructions of how to perform a behavior, persuasive source, and social support.
Cost-effectiveness of the Behavioural Interventions
When looking at the lower but not higher bound estimates (F(5, 96) = 0.972, p = .439) of cost-effectiveness estimates provided in the 102 cost-utility analyses, significantly more smoking cessation interventions than interventions targeting multiple health-related behaviors were considered cost-effective (F(5, 96) = 3.47, p = .006) (see Table 4). Similarly, using the £20,000 threshold to define cost-effectiveness, only with the lower estimate (F(5, 96) = 2.356, p = .046) but not the higher estimate (F(5, 96) = 0.961, p = .446) was there a significant difference between smoking cessation and multiple health-related behavior interventions (see Table 4). By contrast, when using the £30,000 threshold to define cost-effectiveness, there were no differences between interventions.
Table 4:
Prevalence of cost-effective interventions as a function of NICE threshold and lower/upper cost-effectiveness estimates
| All (n = 102) | Smoking (n = 37) | Diet (n = 20) | Physical activity (n = 3) | Alcohol (n = 2) | Sexual health (n = 13) | Multiple targets (n = 27) | p* | |
|---|---|---|---|---|---|---|---|---|
| Mean (SEM) | ||||||||
| Lower estimate | £8,025 (1,528) | £2,382a (648) | £6,098a,b (1,265) | £109a,b (109) | £4,858a,b (572) | £11,012a,b (6,360) | £16,864b (4,286) | .006 |
| Higher Estimate | £11,470 (1,898) | £7,593 (2,769) | £11,812 (3,714) | £4,962 (4,962) | £4,858 (572) | £11,763 (6,540) | £17,601 (4,310) | .439 |
| % (N) below £20,000 threshold | ||||||||
| Lower estimate | 91.2 (93) | 100.0 (37)a | 95.0 (19)a,b | 100.0 (3)a,b | 100.0 (2)a,b | 84.6 (11)a,b | 77.8 (21)b | .046 |
| Higher Estimate | 85.3 (87) | 91.9 (34) | 85.0 (17) | 100.0 (3) | 100.0 (2) | 84.6 (11) | 74.1 (20) | .446 |
| % (N) below £30,000 threshold | ||||||||
| Lower estimate | 95.1 (97) | 100.0 (37) | 100.0 (20) | 100.0 (3) | 100.0 (2) | 92.3 (12) | 85.2 (23) | .105 |
| Higher Estimate | 90.2 (92) | 94.6 (35) | 95.0 (19) | 100.0 (3) | 100.0 (2) | 84.6 (11) | 81.5 (22) | .473 |
Note: *Significant overall differences are in italics.
a, b, c: Comparison of interventions targeting different health-related behaviors, different letters indicate significant difference at p < .05 (Bonferroni-corrected).
Factors associated with cost-effectiveness
In the stepwise adjusted regression model for the continuous limit (see Table 5) interventions using a matched impact control group were associated with less cost-effectiveness than those based on usual care (β = 13480.1, p = .003), those of high intensity were also associated with less cost-effectiveness than those of low intensity (β = 14140.3, p = .001). In contrast, those targeting groups (β = 16628.1, p < .001) or a mixture of groups and individuals (β = 19666.4, p < .001) were associated with more cost-effectiveness than those targeting individuals only, as were those recruiting non-vulnerable participants (β = −10858.3, p = .001). Those offering self-help supporting materials were associated with less cost-effectiveness than those not offering any such materials (β = 14783.3, p = .003). In terms of intervention functions, those based on training (β = −15044.3, p = .002) and persuasion (β = −19384.9, p = .001) were associated with more cost-effective, and those based on environmental restructuring were associated with less cost-effectiveness (β = 15023.9, p = .033). Several BCT groupings were also associated with greater (goals and planning β = −8537.3, p = .019; comparison of behavior β = −13561.9, p = .047) or lower cost-effectiveness (natural consequences β = 7729.4, p = 0.033; reward and threat β = 20106.7, p = 0.004).
Table 5.
Factors associated with continuous upper and lower cost-effectiveness estimates (based on CUA studies N = 102)
| Lower cost-effectiveness estimate | Upper cost-effectiveness estimate | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | |||||||||
| Β | 95% CI | p | β | 95% CI | p | β | 95% CI | p | Β | 95% CI | p | |
| Category | ||||||||||||
| Med | Ref | Ref | ||||||||||
| BI | 6188.8 | −3927.8 to 16305.5 | 0.228 | −7676.3 | −20302.2 to 4949.7 | 0.230 | ||||||
| Med + BI | 212.7 | −11601.0 to 1206.4 | 0.972 | −12642.5 | −27386.5 to 2101.5 | 0.092 | ||||||
| Comp | 9831.8 | 909.7 to 18753.8 | 0.031* | −1645.7 | −127780.7 to 9489.4 | 0.770 | ||||||
| Med + Comp | 1621.7 | −9896.6 to 13140.0 | 0.780 | 12062.5 | −26437.8 to 2312.9 | 0.099 | ||||||
| Mass media | −2020.8 | −21006.3 to 16946.7 | 0.832 | −16103.9 | −39787.3 to 77579.6 | 0.180 | ||||||
| Control condition | ||||||||||||
| Nothing/UC | Ref | Ref | Ref | |||||||||
| Lower impact | −1924.9 | −9366.7 to 6616.8 | 0.609 | 3878 | −2800.5 to 10556.4 | 0.251 | −183.4 | −9556.6 to 9189.8 | 0.969 | |||
| Matched impact | 8384.8 | −1482.9 to 18252.5 | 0.095 | 13480.1 | 4857.5 to 22102.8 | 0.003* | 5099.5 | −77329.3 to 17528.2 | 0.418 | |||
| Intervention intensity | ||||||||||||
| Low | Ref | Ref | Ref | Ref | ||||||||
| Medium | 6100.6 | −149.8 to 13951.1 | 0.126 | 3866.2 | −3430.3 to 11162.7 | 0.294 | 1486.6 | −8346.7 to 11319.8 | 0.765 | −353.5 | −10660.1 to 9953.2 | |
| High | 7140.5 | −360.3 to 14641.3 | 0.062 | 14140.3 | 6302.8 to 21977.8 | 0.001* | 6405.6 | −2989.8 to 15800.9 | 0.179 | 13071.2 | 1686.8 to 24455.6 | 0.946 |
| Unclear | 3397.7 | −8018.6 to 14814.0 | 0.556 | 998.1 | −9118.6 to 11114.8 | 0.845 | −1972.4 | −16272.1 to 12327.4 | 0.785 | −16263 | −32726.4 to 200.4 | 0.025* |
| Setting | .053 | |||||||||||
| Primary care | Ref | Ref | ||||||||||
| Secondary care | −1459.3 | −14648.3 to 117729.6 | 0.827 | −6838.2 | −23280.5 to 9604.1 | 0.411 | ||||||
| Community | 5121.1 | −2657.3 to 11729.6 | 0.827 | −231.6 | −9928.8 to 9465.5 | 0.962 | ||||||
| Workplace | −7306.3 | −38420.1 to 23807.4 | 0.642 | −47785.2 | −43573.7 to 34003.3 | 0.807 | ||||||
| Unclear/other | −1647.0 | −11734.4 to 8440.5 | 0.747 | −6662.2 | −19237.9 to 5913.5 | 0.296 | ||||||
| Delivery mode | ||||||||||||
| Physician | Ref | Ref | Ref | |||||||||
| HP | 7416.0 | −2442.8 to 17274.9 | 0.139 | 12519.8 | 453.1 to 24586.5 | 0.042* | −6717.8 | −23311.1 to 9875.6 | .422 | |||
| Media | 7784.8 | −7579.0 to 23148.7 | 0.137 | 7213.8 | −11590 to 26018.4 | 0.448 | −14227.7 | −48178.7 to 19723.3 | .406 | |||
| Mix | −967.9 | −15581.9 to 13646.0 | 0.896 | 4162.0 | −13724.8 to 22048.8 | 0.645 | −9358.9 | −32811.5 to 14093.7 | .429 | |||
| Unclear/other± | 3003.3 | −7787.9 to 13794.5 | 0.582 | 3012.0 | −10195.9 to 16219.9 | 0.652 | −14518.1 | −33014.3 to 3978.1 | .122 | |||
| Target level | ||||||||||||
| Individual | Ref | Ref | Ref | Ref | ||||||||
| Groups | −3031.7 | −12236.9 to 6173.4 | 0.515 | −16628.1 | −24982.3 to −8274 | <0.001* | −4911.9 | −16339.6 to 6515.7 | 0.396 | −21653.4 | −34161.5 to −9145.3 | .001* |
| Population | −8344.7 | −26425.4 to 97746.0 | 0.362 | 15176 | −13703.3 to 44055.2 | 0.298 | −12199.3 | −34577.8 to 10339.2 | 0.287 | 49323.7 | 1980.1 to 96667.4 | .041* |
| Mix | −6701.6 | −18830.2 to 5426.9 | 0.276 | −19666.4 | −31361.8 to −7971 | 0.001* | −6405.4 | −21462.2 to 8651.5 | 0.401 | −20204.7 | −37115 to −3294.3 | .020* |
| Population | ||||||||||||
| Vulnerable | Ref | Ref | Ref | |||||||||
| General | −97794.3 | −15590.2 to −3998.4 | 0.001* | −10858.3 | −16932.3 to −4784.3 | 0.001* | −11784.0 | −19007.2 to −4560.8 | 0.002* | −24183.7 | −33696.4 to −14671 | <.001* |
| Supporting material | ||||||||||||
| None | Ref | Ref | Ref | |||||||||
| Self-help | −1345.77 | −11049.2 to 8357.7 | 0.784 | −4025.6 | −13579.3 to 5528.1 | 0.404 | 14770.1 | −10920.9 to 13861.1 | 0.814 | 9361.7 | −4894.3 to 23617.7 | .195 |
| Electronic | 8478.1 | −1225.3 to 18181.6 | 0.086 | 14783.3 | 5134.5 to 24432.1 | 0.003* | 6104.4 | −6286.6 to 18495.4 | 0.331 | 14386.2 | 441.4 to 28331 | .043* |
| Mix | 11602.4 | 1488.3 to 21716.4 | 0.025* | 9832.3 | −1127.2 to 20791.7 | 0.078 | 7836.6 | −5078.7 to 207751.1 | 0.231 | −1541.1 | −21343.3 to 18261.1 | 0.877 |
| Pharmacological support | −4047.7 | −10165.7 to 2070.4 | 0.192 | −14847.2 | −31139.4 to 1445 | 0.073 | −221.5 | −77885.0 to 7442.1 | 0.954 | |||
| Social marketing | −4460.0 | −18545.0 to 9624.9 | 0.531 | −22411.5 | −42218.2 to −2604.8 | 0.027* | −7966.6 | −25422.9 to 9489.7 | 0.367 | −31072.9 | −58935.4 to −3210.4 | .029* |
| Incentives | −5782.3 | −36686.9 to 25122.3 | 0.711 | −9260.7 | −47625.9 to 29104.5 | 0.633 | ||||||
| Intervention functions | ||||||||||||
| Training | −3078.1 | −10728.4 to 4572.2 | 0.427 | −15044.3 | −24157.8 to −5930.8 | 0.002* | −9260.7 | −4625.9 to 29104.5 | 0.633 | −6439.9 | −18308.2 to 5428.3 | .283 |
| Education | 6572.1 | −130.2 to 13274.3 | 0.055 | 933.5 | −8596.5 to 10463.5 | 0.846 | ||||||
| Enablement | −2494.0 | −8665.5 to 3677.5 | 0.425 | 235.77 | −5727.0 to 11198.4 | 0.523 | ||||||
| Persuasion | −4394.6 | −11633.5 to 2844.4 | 0.231 | −19384.9 | −30087 to −8682.9 | 0.001* | 1565.9 | −6117.3 to 9249.0 | 0.687 | −25947.6 | −38411.8 to −13483.4 | <.001* |
| Environmental restructuring | −3626.1 | −17621.4 to 10569.3 | 0.621 | 15023.9 | 1272.7 to 28775.1 | 0.033* | −8241.5 | −177148.2 to 655.3 | 0.069 | 16475.1 | −2072.7 to 35022.8 | .081 |
| Incentivization | 13003.4 | −8821.6 to 34828.4 | 0.240 | −7147.9 | −24618.1 to 10322.4 | 0.419 | 21868.6 | −7845.9 to 51583.1 | .147 | |||
| Restriction | −1834.3 | −17527.9 to 13859.3 | 0.817 | 9490.2 | −17739.6 to 36720.0 | 0.491 | −32286.1 | −59066.5 to −5505.8 | .019* | |||
| Modeling | −1370.3 | −32295 to 29554.3 | 0.930 | −18938.3 | −45216.1 to 7339.5 | 0.155 | −5419.1 | −24885.8 to 14047.5 | 0.582 | −27701.8 | −63850.8 to 8447.1 | .131 |
| Coercion | NA | NA | NA | NA | NA | NA | −4648.7 | −43245.8 to 33548.4 | 0.803 | NA | NA | |
| BCT groupings | ||||||||||||
| Shaping knowledge | 813.5 | −8039.8 to 9666.8 | 0.856 | 8856.8 | −105.6 to 17819.2 | 0.053 | NA | NA | NA | |||
| Antecedents | −2359.9 | −8446.6 to 3726.9 | 0.444 | 47887.77 | −6167.6 to 157745.0 | 0.388 | ||||||
| Regulation | −2058.4 | −8149.5 to 4032.6 | 0.504 | 11193.4 | −3264.9 to 25651.6 | 0.127 | −105.8 | −7687.7 to 7476.1 | 0.9778 | |||
| Social support | 2430.4 | −3674.3 to 8535.0 | 0.431 | 1008.9 | −65770.4 to 8588.1 | 0.792 | ||||||
| Comparison of outcomes | −379.4 | −9516.3 to 8757.6 | 0.935 | 3907.6 | −1759.9 to 9575.1 | 0.174 | −148.5 | −7753.8 to 77456.9 | 0.969 | −8906.1 | −18760 to 947.9 | .076 |
| Feedback and monitoring | 3813.2 | −3330.2 to 10956.7 | 0.292 | −3450.9 | −14788.5 to 77876.6 | 0.547 | ||||||
| Goals and planning | 3812.8 | −2973.0 to 10598.77 | 0.268 | −8537.3 | −15613.6 to −1461 | 0.019* | 25778.4 | −6328.5 to 11485.3 | 0.567 | −12416.9 | −24062.3 to −771.5 | .037* |
| Natural consequences | 7775.6 | 1124.2 to 14426.9 | 0.022* | 7729.4 | 661.6 to 14797.3 | 0.033* | 1307.0 | −7169.1 to 9783.1 | 0.760 | |||
| Self-beliefs | −2914.9 | −10886.8 to 5057.1 | 0.470 | 6848.6 | −3182.7 to 16879.9 | 0.178 | 6848.0 | −1522.6 to 15218.5 | 0.108 | |||
| Repetition and substitution | 492.9 | −9753.5 to 107739.2 | 0.924 | 14037.2 | −47.4 to 28121.9 | 0.051 | −6101.2 | −15954.2 to 3751.7 | 0.222 | 14828.5 | −7033.1 to 36690 | .181 |
| Comparison of behavior | −3779.4 | −9516.3 to 8757.6 | 0.935 | −13561.9 | −26950.5 to −173.3 | 0.047* | −2224.4 | −14943.0 to 10494.3 | 0.729 | −30650.2 | −52403 to −8897.3 | .006* |
| Associations | 3186.1 | −14827.3 to 21209.6 | 0.727 | −3450.9 | −14778.5 to 7876.6 | 0.547 | ||||||
| Reward and threat | 23339.0 | 10007.5 to 36670.5 | 0.001 | 20106.7 | 6750.8 to 33462.7 | 0.004* | −362.5 | −22760.9 to 22035.8 | 0.974 | |||
| Identity | 11355.7 | −19487.9 to 42199.4 | 0.467 | 19717.2 | 2631.6 to 36802.7 | 0.024* | 37685.8 | −3784.3 to 79155.9 | .074 | |||
| Scheduled consequences | NA | NA | NA | 77877.4 | −30500.0 to 46254.7 | 0.685 | ||||||
| Covert learning | NA | NA | NA | NA | NA | NA | ||||||
| Number of BCTS | 1256.2 | 2877.6 to 2224.7 | 0.012* | 991.1 | −235.3 to 2217.5 | 0.112 | 1763.1 | −243.3 to 3769.6 | .084 | |||
Note: * indicates significance, lower and upper cost-effectiveness analyses were based on n = 102 studies which provided cost-utility analyses.
NA, not applicable as this category was not coded in any intervention.
In the stepwise adjusted model for the upper limit (see Table 5), interventions of high intensity were associated with less cost effective than those of low intensity (β = 13071.2, p = .025), as were those aimed at the population compared to individuals (β = 49323.7, p = .041), while those aimed at groups or a mixture were associated with more cost-effectiveness (β = −21652.4, p = .001 and β = −20204.7, p = .020). Interventions recruiting the general population were generally associated with more cost-effectiveness (β = −24183.7, p < .001) as were those based on social marketing (β = −31072.9, p = .029). The functions persuasion and restriction were associated with higher cost-effectiveness (β = −25947.6, p < .001 and β = = 32286.1, p = 0.019) as were the BCT groupings goals and planning and comparison of behavior (β = −12416.9, p = .037 and β = −30650.2, p = .006).
In sensitivity analyses using a binary estimate of cost-effectiveness involving all 251 studies, those studies where the control condition was classified as having a lower impact (being less comprehensive) had higher odds of being cost-effective compared with those with a standard control condition, that is, receiving usual care (OR 5.374, 95% CI 1.200 to 23.674, p = 0.026). Additionally, higher intervention intensity was associated with lower cost-effectiveness (OR 0.283, 0.112 to 0.727, p = .009) (see Table 6).
Table 6.
Factors associated with binary cost effective versus cost-ineffective interventions (based on all studies n = 251)
| Unadjusted | Adjusted | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95%CI | p | |
| Category | ||||||
| Med | Ref | |||||
| BI | 1.594 | 0.427 to 5.942 | 0.488 | |||
| Med + BI | 5.313 | 0.588 to 47.976 | 0.137 | |||
| Comp | 0.599 | 0.204 to 1.756 | 0.35 | |||
| Med + Comp | 2.266 | 0.408 to 12.590 | 0.35 | |||
| Mass media | NA | NA | NA | |||
| Control condition | ||||||
| Nothing/UC | Ref | Ref | ||||
| Lower impact | 5.332 | 1.225 to 23.217 | .026* | 5.374 | 1.200 to 23.674 | .026* |
| Matched impact | 0.699 | 0.216 to 2.265 | 0.551 | 0.733 | 0.219 to 2.450 | 0.614 |
| Intervention intensity | ||||||
| Low | Ref | Ref | ||||
| Medium | 0.721 | 0.230 to 2.257 | 0.574 | 0.691 | 0.218 to 2.190 | 0.53 |
| High | 0.28 | 0.110 to 0.709 | .007* | 0.283 | 0.112 to 0.727 | .009* |
| Unclear | NA | NA | NA | NA | NA | NA |
| Setting | ||||||
| Primary care | Ref | |||||
| Secondary care | 0.705 | 0.146 to 3.400 | 0.663 | |||
| Community | 0.38 | 0.154 to 0.941 | .037* | |||
| Workplace | NA | NA | NA | |||
| Unclear/other | 0.383 | 0.125 to 1.171 | 0.92 | |||
| Delivery mode | ||||||
| Physician | NA | NA | ||||
| HP | Ref | |||||
| Media | NA | NA | ||||
| Mix | NA | NA | ||||
| Unclear/other± | 2.502 | 0.721 to 8.688 | 0.149 | |||
| Target level | ||||||
| Individual | Ref | |||||
| Groups | 1.514 | 0.355 to 6.844 | 0.59 | |||
| Population | NA | NA | NA | |||
| Mix | NA | NA | NA | |||
| Population | ||||||
| Vulnerable | Ref | |||||
| General | 1.126 | 0.531 to 2.390 | 0.756 | |||
| Supporting material | ||||||
| None | Ref | |||||
| Self-help | 1.49 | 0.327 to 6.7798 | 0.606 | |||
| Electronic | 1.088 | 0.302 to 3.927 | 0.897 | |||
| Mix | 0.745 | 0.234 to 2.374 | 0.619 | |||
| Pharmacological support | 1.488 | 0.680 to 3.252 | 0.32 | |||
| Social marketing | NA | NA | NA | |||
| Incentives | NA | NA | NA | |||
| Intervention functions | ||||||
| Training | 0.73 | 0.349 to 2.090 | 0.73 | |||
| Education | 0.727 | 0.298 to 1.772 | 0.483 | |||
| Enablement | 1.197 | 0.559 to 2.562 | 0.643 | |||
| Persuasion | 1.143 | 0.467 to 2.798 | 0.77 | |||
| Environmental restructuring | 0.763 | 0.161 to 3.617 | 0.733 | |||
| Incentivization | 1.28 | 0.157 to 10.461 | 0.818 | |||
| Restriction | NA | NA | NA | |||
| Modeling | NA | NA | NA | |||
| Coercion | NA | NA | NA | |||
| BCT groupings | ||||||
| Shaping knowledge | 0.189 | 0.025 to 1.433 | 0.107 | |||
| Antecedents | 1.431 | 0.672 to 3.045 | 0.353 | |||
| Regulation | 1.499 | 0.694 to 3.237 | 0.302 | |||
| Social support | 0.626 | 0.294 to 1.333 | 0.224 | |||
| Comparison of outcomes | 0.68 | 0.318 to 1.453 | 0.32 | |||
| Feedback and monitoring | 1.078 | 0.457 to 2.541 | 0.863 | |||
| Goals and planning | 0.734 | 0.326 to 1.653 | 0.456 | |||
| Natural consequences | 0.481 | 0.215 to 1.074 | 0.074 | |||
| Self-beliefs | 0.982 | 0.400 to 2.416 | 0.969 | |||
| Repetition and substitution | 0.52 | 0.180 to 1.504 | 0.227 | |||
| Comparison of behavior | 0.68 | 0.318 to 1.453 | 0.32 | |||
| Associations | 0.933 | 0.260 to 3.344 | 0.916 | |||
| Reward and threat | 0.634 | 0.172 to 2.346 | 0.495 | |||
| Identity | NA | NA | NA | |||
| Scheduled consequences | NA | NA | NA | |||
| Covert learning | NA | NA | NA | |||
| Number of BCTS | 0.931 | 0.836 to 1.036 | 0.189 | |||
Note: *Significance, all studies were included in the binary analysis of cost-effective versus cost-ineffective interventions (n = 251).
NA, not applicable as complete separation.
Discussion
Around a third of cost-effective interventions were of low intensity, mostly set in primary care and delivered by healthcare professionals. Although there was a large amount of variation across the six behavioral domains, increasing knowledge and/or understanding through education and imparting skills through training were the most prevalent intervention functions, while few used restriction, modeling or coercion. The majority of interventions included around 5% of the potential BCTs specified in the 93-item taxonomy, with the most prevalent BCT groupings being shaping knowledge, antecedents, regulation and social support. Several intervention features were associated with greater cost-effectiveness (those targeting groups or a mixture of groups and individuals versus individuals only; those aimed at the general versus vulnerable populations; and those based on social-marketing) and lower cost-effectiveness (matched control group versus usual care; high intensity versus low intensity; and those offering self-help materials). In terms of intervention functions, those based on training, persuasion and restriction yielded better cost-effectiveness estimates and those based on environmental restructuring and incentivization worse estimates. Several BCT groupings were also associated with greater cost-effectiveness (goals and planning and comparison of behavior) or lower cost-effectiveness estimates (natural consequences and reward and threat).
Extensive evidence exists for the effectiveness of the most prevalent intervention functions and BCT clusters. For example, educational materials and imparting knowledge have been shown to increase the uptake of cervical cancer screening [23], social support appears beneficial in weight loss maintenance [24], restructuring the environment (e.g., removing alcohol) and avoiding exposure to alcohol related cues reduces alcohol consumption [25], and coping skills training in relapse prevention can help those with dependency disorders [26, 27]
At the same time, several functions and BCTs which have demonstrated efficacy were underused or neglected. For example, few used the principles of operant learning (e.g., techniques which involve the manipulation of environmental contingencies such as rewarding behavior, using prompts and cues, agreeing on a behavioral contract and encouraging practice) or encouraged the construction of a new self-identity, both of which underpin much of human behavior [28–31]. This could be because of insufficient intervention descriptions in published/available information [32] or it may reflect intervention developers’ narrow implicit theoretical assumptions regarding causes of behavior and how it might be changed.
It is perhaps unsurprising that interventions were deemed less cost-effective if study design (e.g., matched impact control versus usual care), mode of delivery (e.g., to the individual rather than group) and the intervention itself (e.g., intensity and the provision of self-help) were more complex. This should nonetheless be considered during intervention design. The fact that the incremental effect of the intervention was smaller in more closely matched impact controls, underlines the need to examine mechanisms and intervention processes through the use of appropriate control groups. Choice of control groups or comparison strategies is acknowledged to influence ICER [33]. Usual care is commonly recommended for pragmatic trials which aim to improve current practice and is the primary recommended control group for the calculation of ICERs by NICE [34]. Usual care reflects the care usually received by patients in daily practice and therefore the current “gold standard” [35, 36]. However, usual care controls have also been criticized. Usual care may include many sources of variance and therefore results may not generalize and larger sample sizes may be required. Although conversely, they more likely reflect real-world practice and therefore enhance ecological validity [37].
Use of vulnerable populations also likely increase cost due to difficulties in recruitment and the additional care needed during the programmes’ implementation. Interventions coded for social marketing were deemed particularly cost-effective. Social marketing has been defined as the application of concepts and techniques drawn from the commercial sector (e.g., the four P’s of marketing: Product, Price, Place and Promotion) to promote changes in socially important health behaviors such as drug use and smoking [38]. Previous studies have found that social marketing can form an effective framework for behavior change interventions and provide a useful toolkit for organizations that are trying to change health behaviors [39, 40]. However, findings highlight an ongoing lack of use or underreporting of the use of theory in social marketing campaigns and this may limit its effectiveness [39].
Although the available evidence suggests that financial incentive interventions are more effective than usual care for encouraging healthy behavior change, in our analysis rewards were associated with lower cost-effectiveness [41]. This may be because rewards do not necessarily match up to financial incentives and few studies were explicitly coded as providing incentives and so power may have been low to detect an effect. Environmental restructuring (i.e. removing or adding objects to the environment) and natural consequences, which involves providing information on social, health and emotional consequences, monitoring of emotional consequences and inducing regret, were also associated with lower cost-effectiveness. This would support arguments against a focus on approaches such as that advocated by “Nudge,” which is based on changing the surrounding environment, some incentivization and forms of subtle persuasion to influence behavior, eschewing the use of coercion or other BCW intervention functions [10, 12, 42].
In contrast, goals and planning and comparison of behavior were associated with greater cost-effectiveness. Forming detailed plans of what, when, and how to achieve behavior change have been found to be effective across behavioral domains [43]. Implementation intentions, which take the format of if–then plans, have also been found to be effective not only in promoting initial changes in behavior [44], but also enduring long term changes [45]. Demonstration of behavior and social comparison form part of several behavior change theories including Social Comparison Theory and Social Learning Theory [46, 47], and have been associated previously with smoking cessation success [48], perception of alcohol-related negative consequences [49] and greater weight loss [50].
Implications
These findings have several implications. First, they may aid evidence-based practice and the application of BCIs in the public domain by providing some of the key BCTs associated with cost-effectiveness. Secondly, studying the types of components of behavioral interventions in this manner may help enable scientific replication, by clearly specifying which components have been employed previously [51]. Finally, elucidating and summarizing the components of interventions may be a valuable resource to intervention designers, with guidelines recommending a full literature review of the components of efficacious interventions before development [52]. As further data accumulates, it will be important to assess if these findings are applicable to individual behavioral domains and other health behaviors not considered in the current review.
Limitations
To our knowledge, this is the first attempt to synthesize BCIs in terms of their functions and “active ingredients” and to assess the association with cost-effectiveness. However, this study also has several limitations. First, the BCT taxonomy coding approach was applied conservatively, in that a technique was coded as present only when there was unequivocal evidence from written materials that it was used. This is problematic since many intervention reports are poorly specified [53]. Secondly, it is not possible to make a causal attribution of cost-effectiveness to specific BCTs because the BCIs typically contain many of these. Although multiple regression can be used to help discern these effects, caution should be taken during interpretation due to the small sample sizes and possible lack of power i.e. a non-significant effect may reflect no effect or data insensitivity. Thirdly, this paper used the NICE threshold of cost effectiveness of £20,000−£30,000 per QALY. However, there is debate about the correct level of this threshold which is considered implicit rather than explicit [54] and varies enormously between countries [55]. Fourthly, irrespective of the methodology used to evaluate cost-effectiveness, relatively few interventions were considered not to be cost-effective, which likely reduced our ability to detect anything other than relatively large associations with interventions being cost-effective or not. Finally, due to the number of papers (particularly for alcohol and physical activity interventions) it was not possible to consider the predictors of cost-effectiveness as a function of behavioral domain. It remains possible that a combination of functions and techniques are more effective for a given health behavior and that the results do not generalize to health behaviors not included in the current review.
Conclusion
In conclusion, this study reliably categorized and coded the BCTs used in BCIs across six behavioral domains and assessed the association with cost-effectiveness. These interventions heavily relied on education and training, with substantial variations found across the interventions targeting the six health behaviors. Although most interventions used relatively few BCTs, those employing goal setting and comparison of behavior were deemed more cost-effective. These findings will be of interest to intervention developers and policy makers attempting to implement BCIs in the real world.
Supplementary Material
Funding
This study was funded by the UK’s National Institute for Health and Care Excellence (NICE).
Compliance with Ethical Standards
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards E.B. has received unrestricted funding from Pfizer. L.S. has received honoraria for talk and travel expenses from manufacturers of medications for smoking cessation to attend meetings and workshops. E.B. is funded by the NIHR SPHR and CRUK also provide support. SPHR is a partnership between the Universities of Sheffield; Bristol; Cambridge; Exeter; UCL; The London School for Hygiene and Tropical Medicine; the LiLaC collaboration between the Universities of Liverpool and Lancaster and Fuse; The Centre for Translational Research in Public Health, a collaboration between Newcastle, Durham, Northumbria, Sunderland and Teesside Universities. The views expressed are those of the authors(s) and not necessarily those of the NHS, NIHR, or Department of Health. No funders had any involvement in the design of the study, the analysis or interpretation of the data, the writing of the report, or the decision to submit the paper for publication. L.O.’s salary is funded by NICE. B.G. and F.L. have nothing to declare.
Authors’ Contributions
E.B. wrote the first draft. E.B. and L.S. ran the analysis. E.B., F.L. and B.G. collected the data. All authors commented on the first draft and contributed to the final version.
Data Availability Data are available from the lead author E.B.
References
- 1. Scarborough P, Bhatnagar P, Wickramasinghe KK, Allender S, Foster C, Rayner M. The economic burden of ill health due to diet, physical inactivity, smoking, alcohol and obesity in the UK: An update to 2006-07 NHS costs. J Public Health (Oxf). 2011;33:527–535. [DOI] [PubMed] [Google Scholar]
- 2. Nash R, Featherstone H. Cough up: Balancing tobacco income and costs in society. Policy Exchange Web site. http://www.policyexchange.org.uk/publications/category/item/cough-up-balancing-tobacco-income-and-costs-in-society. 2010. Date accessed 1 February 2019.
- 3. NHS National Treatment Agency for Substance Misuse. Alcohol treatment in England 2011-12. NHS National Treatment Agency for Substance Misuse, https://www.nice.org.uk/guidance/ph49/resources/costing-statement-69190813. 2013. Date accessed 1 February 2019. [Google Scholar]
- 4. Development Economics. Unprotected nation: The financial and economic impacts of restricted contraceptive and sexual health services. http://www.fpa.org.uk/sites/default/files/unprotected-nation-sexual-health-full-report.pdf. 2013. Date accessed 1 February 2019.
- 5. van Duijvenbode DC, Hoozemans MJ, van Poppel MN, Proper KI. The relationship between overweight and obesity, and sick leave: a systematic review. Int J Obes (Lond). 2009;33:807–816. [DOI] [PubMed] [Google Scholar]
- 6. de Vocht F, Heron J, Angus C, et al. . Measurable effects of local alcohol licensing policies on population health in England. J Epidemiol Community Health. 2016;70:231–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Parrott S, Godfrey C, Raw M. Costs of employee smoking in the workplace in Scotland. Tob Control. 2000;9:187–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Elliott DS, Mihalic S. Issues in disseminating and replicating effective prevention programs. Prev Sci. 2004;5:47–53. [DOI] [PubMed] [Google Scholar]
- 9. Clarke GN. Improving the transition from basic efficacy research to effectiveness studies: Methodological issues and procedures. J Consult Clin Psychol. 1995;63:718–725. [DOI] [PubMed] [Google Scholar]
- 10. Michie S, van Stralen MM, West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Michie S, Richardson M, Johnston M, et al. . The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46:81–95. [DOI] [PubMed] [Google Scholar]
- 12. Michie S, Atkins L, West R.. The Behaviour Change Wheel: A Guide to Designing Interventions. Great Britain: Silverback Publishing; 2015. [Google Scholar]
- 13. Lara J, Evans EH, O’Brien N, et al. . Association of behaviour change techniques with effectiveness of dietary interventions among adults of retirement age: A systematic review and meta-analysis of randomised controlled trials. BMC Med. 2014;12:177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. O’Brien N, McDonald S, Araújo-Soares V, et al. . The features of interventions associated with long-term effectiveness of physical activity interventions in adults aged 55-70 years: A systematic review and meta-analysis. Health Psychol Rev. 2015;9:417–433. [DOI] [PubMed] [Google Scholar]
- 15. Lorencatto F, West R, Michie S. Specifying evidence-based behavior change techniques to aid smoking cessation in pregnancy. Nicotine Tob Res. 2012;14:1019–1026. [DOI] [PubMed] [Google Scholar]
- 16. West R, Walia A, Hyder N, Shahab L, Michie S. Behavior change techniques used by the English Stop Smoking Services and their associations with short-term quit outcomes. Nicotine Tob Res. 2010;12:742–747. [DOI] [PubMed] [Google Scholar]
- 17. Beard E, West R, Lorencatto F, et al. . What do cost-effective health behaviour-change interventions contain? A comparison of six domains. PLoS One. 2019;14:e0213983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. National Institute for Health and Care Excellence. How NICE measures value for money in relation to public health interventions. 2013. https://www.nice.org.uk/Media/Default/guidance/LGB10-Briefing-20150126.pdf.
- 19. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 20. National Institute for Health and Care Excellence (NICE). Behaviour change at population, community and individual levels (Public Health Guidance 6). London; 2007. https://www.nice.org.uk/guidance/ph6.
- 21. Prochaska JJ, Prochaska JO. A Review of multiple health behavior change interventions for primary prevention. Am J Lifestyle Med. 2011;5(3):10.1177/1559827610391883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Glazier RH, Bajcar J, Kennie NR, Willson K. A systematic review of interventions to improve diabetes care in socially disadvantaged populations. Diabetes Care. 2006;29:1675–1688. [DOI] [PubMed] [Google Scholar]
- 23. Forbes CA, Jepson RG, Martin‐Hirsch PP.. Interventions targeted at women to encourage the uptake of cervical screening. Cochrane Database Syst Rev. 2002;3:CD002834. [DOI] [PubMed] [Google Scholar]
- 24. Karfopoulou E, Anastasiou CA, Avgeraki E, Kosmidis MH, Yannakoulia M. The role of social support in weight loss maintenance: results from the MedWeight study. J Behav Med. 2016;39:511–518. [DOI] [PubMed] [Google Scholar]
- 25. Jones A, Field M. Alcohol-related and negatively valenced cues increase motor and oculomotor disinhibition in social drinkers. Exp Clin Psychopharmacol. 2015;23:122–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jafari E, Eskandari H, Sohrabi F, Delavar A, Heshmati R. Effectiveness of coping skills training in relapse prevention and resiliency enhancement in people with substance dependency. Procedia Soc Behav Sci. 2010;5:1376–1380. [Google Scholar]
- 27. Song F, Huttunen-Lenz M, Holland R. Effectiveness of complex psycho-educational interventions for smoking relapse prevention: An exploratory meta-analysis. J Public Health (Oxf). 2010;32:350–359. [DOI] [PubMed] [Google Scholar]
- 28. Tombor I, Shahab L, Brown J, West R. Positive smoker identity as a barrier to quitting smoking: Findings from a national survey of smokers in England. Drug Alcohol Depend. 2013;133:740–745. [DOI] [PubMed] [Google Scholar]
- 29. Johnston M. What more can we learn from early learning theory? The contemporary relevance for behaviour change interventions. Br J Health Psychol. 2016;21:1–10. [DOI] [PubMed] [Google Scholar]
- 30. Skinner BF. Operant behavior. Am Psychologist. 1963;18(8):503. [Google Scholar]
- 31. Murtagh N, Gatersleben B, Uzzell D. Self-identity threat and resistance to change: Evidence from regular travel behaviour. J Environ Psychol. 2012;32(4):318–326. [Google Scholar]
- 32. Makic MB, VonRueden KT, Rauen CA, Chadwick J. Evidence-based practice habits: Putting more sacred cows out to pasture. Crit Care Nurse. 2011;31:38–61; quiz 62. [DOI] [PubMed] [Google Scholar]
- 33. Maudgil DD. Cost effectiveness and the role of the National Institute of Health and Care Excellence (NICE) in interventional radiology. Clin Radiol. 2021;76:185–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Stevens JW. NICE work: how NICE decides what we should pay for. Br J Gen Pract. 2010;60:7–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Roland M, Torgerson DJ. What are pragmatic trials? BMJ. 1998;316:285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Thompson BT, Schoenfeld D. Usual care as the control group in clinical trials of nonpharmacologic interventions. Proc Am Thorac Soc. 2007;4:577–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mohr DC, Spring B, Freedland KE, et al. . The selection and design of control conditions for randomized controlled trials of psychological interventions. Psychother Psychosom. 2009;78:275–284. [DOI] [PubMed] [Google Scholar]
- 38. Andreasen AR. Marketing Social Change. San Francisco, CA: Jossey-Bass; 1995. [Google Scholar]
- 39. Gordon R, McDermott L, Stead M, Angus K. The effectiveness of social marketing interventions for health improvement: what’s the evidence? Public Health. 2006;120:1133–1139. [DOI] [PubMed] [Google Scholar]
- 40. Kotler P, Roberto EL.. Social Marketing. Strategies for Changing Public Behavior. New York: The Free Press; 1989. [Google Scholar]
- 41. Luca NR, Suggs LS. Theory and model use in social marketing health interventions. J Health Commun. 2013;18:20–40. [DOI] [PubMed] [Google Scholar]
- 42. Thaler Richard H, Sunstein Cass R.. Nudge: Improving Decisions About Health, Wealth, and Happiness. New Haven, CT: Yale University Press; 2008. [Google Scholar]
- 43. Gollwitzer PM, Sheeran P. Implementation intentions and goal achievement: A meta‐analysis of effects and processes. Adv Exp Soc Psychol. 2006;38:69–119. [Google Scholar]
- 44. Sheeran P, Orbell S. Implementation intentions and repeated behaviour: Augmenting the predictive validity of the theory of planned behaviour. Eur J Soc Psychol. 1999;29(23):349–369. [Google Scholar]
- 45. Achtziger A, Gollwitzer PM, Sheeran P. Implementation intentions and shielding goal striving from unwanted thoughts and feelings. Pers Soc Psychol Bull. 2008;34:381–393. [DOI] [PubMed] [Google Scholar]
- 46. Festinger L. A theory of social comparison processes. Hum Relat. 1954;7(2):117–140. [Google Scholar]
- 47. Bandura A, McClelland DC.. Social Learning Theory. Englewood cliffs, NJ: Prentice Hall; 1977. [Google Scholar]
- 48. Gerrard M, Gibbons FX, Lane DJ, Stock ML. Smoking cessation: Social comparison level predicts success for adult smokers. Health Psychol. 2005;24:623–629. [DOI] [PubMed] [Google Scholar]
- 49. Litt DM, Lewis MA, Stahlbrandt H, Firth P, Neighbors C. Social comparison as a moderator of the association between perceived norms and alcohol use and negative consequences among college students. J Stud Alcohol Drugs. 2012;73:961–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hartmann-Boyce J, Johns DJ, Jebb SA, Aveyard P; Behavioural Weight Management Review Group . Effect of behavioural techniques and delivery mode on effectiveness of weight management: Systematic review, meta-analysis and meta-regression. Obes Rev. 2014;15:598–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Michie S, West R. Behaviour change theory and evidence: A presentation to government. Health Psychology Rev. 2013;7(1):1–22. [Google Scholar]
- 52. Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M; Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Lorencatto F, West R, Stavri Z, Michie S. How well is intervention content described in published reports of smoking cessation interventions? Nicotine Tob Res. 2013;15:1273–1282. [DOI] [PubMed] [Google Scholar]
- 54. Appleby J, Devlin N, Parkin D. NICE’s cost effectiveness threshold. BMJ. 2007;335:358–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Eichler HG, Kong SX, Gerth WC, Mavros P, Jönsson B. Use of cost-effectiveness analysis in health-care resource allocation decision-making: How are cost-effectiveness thresholds expected to emerge? Value Health. 2004;7:518–528. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.