Abstract
Objective
During the coronavirus disease pandemic, enforced restrictions prevented face-to-face consultations for patients requiring non-emergency medical treatment. In response, there was a rise in telemedical practices, such as teledermatology. This study aimed at understanding the pan-world experiences of patients and healthcare staff who adapted to teledermatology in the coronavirus disease era.
Methods
This study made use of an online survey presented to dermatology professionals using social media and WhatsApp groups. Professionals who applied teledermatology between March and June 2020 were targeted. The survey was designed to identify respondent demographics and the preferred platforms for digital consultations. The most common diagnoses and rates of referral for further evaluation were recorded. Lastly, a platform was provided for practitioners to report their own and their patient's perspectives on the advantages and operational challenges of teledermatology. Data were collated and analyzed in Microsoft Excel.
Results
In total, 653 stakeholders participated, representing countries worldwide. Facebook and WhatsApp services were the most popular mediums of digital consultation. Diagnoses of ailments, such as acne and eczema, as well as skin-related infections, were most common. Of the cases referred for biopsy, 10 patients were subsequently diagnosed with cutaneous malignancies. Practitioners and patients not only reported personal benefit from adopting teledermatology, but also reported concerns regarding data privacy and the levels of technological literacy required.
Conclusions
Teledermatology proved an innovative clinical response to unprecedented challenges. However, further policy development and technological advancement aimed at increasing the diagnostic power of digital consultations are needed to support the continuation of teledermatology in the post-pandemic world.
Keywords: Teledermatology, COVID-19 pandemic, telemedicine, dermatology, remote consultation, social media
Introduction
In early 2020, governments worldwide enforced strict restrictions on human movement to control the spread of coronavirus disease (COVID-19). A primary effect of these so-called lockdowns was the notable diminution of patients requiring non-urgent medical attention in healthcare facilities. Pre-pandemic, dermatology practices often recorded some of the highest numbers of patient consultations, although this was drastically mitigated by the imposed restrictions. Nevertheless, patients with new or existing skin conditions still required treatment, and there was a pressing need for establishing a connecting bridge between patients and healthcare providers despite limitations on face-to-face consultations. In the face of these unprecedented challenges, an innovative means of continuing dermatological care emerged that took advantage of the digital spaces whereby people worldwide were maintaining interpersonal connections. Collectively termed teledermatology, these practices have markedly supported the continuation of patient care during the COVID-19 pandemic. However, nonuniformity in teledermatology services presented new challenges to patients and healthcare providers alike. This study sought to gain a global perspective on the nature of these challenges and to understand the steps taken to ensure the quality of continued patient care.
Methods
This study was conducted using an online digital survey targeting healthcare providers working in the field of dermatology, including dermatologists, nurses, receptionists, information technology staff, and administrative staff of hospitals and clinics worldwide. Consent was obtained during the survey process for publication of the data, and this study was conducted in compliance with the Declaration of Helsinki. The author conceptualized this study on a personal computer and collected data from 653 stakeholders using platforms, such as Facebook dermatology groups, WhatsApp groups, and LinkedIn professional groups. The author invited the participants to fill in the online questionnaire via a posted website link.
The survey was separated into four distinct parts. In the first part, participants were asked questions about their demography and their current position as a healthcare provider or affiliate in the field of dermatology. Respondents who were not directly working in the field of dermatology during the pandemic were excluded from the remainder of the survey, and their data were excluded from the analyses. In the second part of the survey, respondents were asked questions addressing the method of teledermatology conducted and the platform used for these patient interactions. The third part of the survey investigated dermatological diagnoses and patient outcomes. The final (fourth) part of the survey was constructed to elaborate on the associated operational advantages and challenges. The data from the questionnaire responses were collated and analyzed using Microsoft Excel and Microsoft word. Stakeholder data were categorized according to the nature of their participation in the field of dermatology. The method of teledermatology was categorized according to the platform used to conduct consultations. Patient demographics were categorized according to sex. The diagnosis and outcome data were organized according to the final diagnosis made only through a digital consultation and frequency of patients then referred for biopsy or further evaluation at a healthcare facility. Data from each category are presented as percentages.
Results
Distribution of stakeholder participation
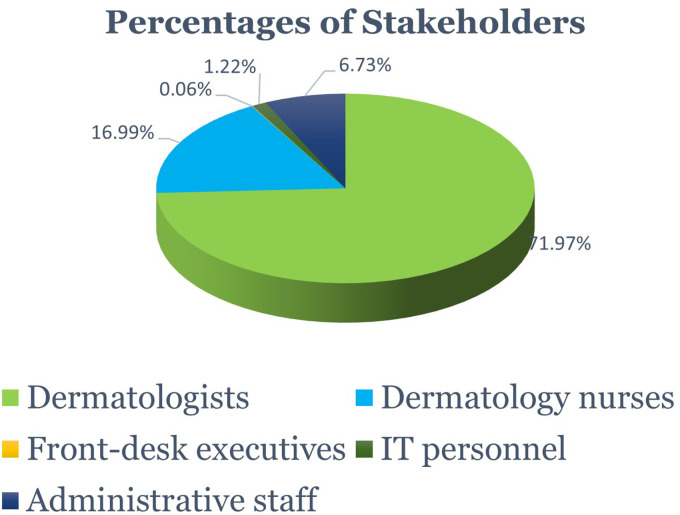
Of all included respondents, 98.16% of stakeholders were directly or indirectly associated with teledermatology between March and June 2020. In total, 71.97% of respondents were dermatologists, while 16.99% were dermatology nurses. The final 11.04% included non-clinical staff (Figure 1).
Figure 1.
Distribution of stakeholder respondents involved in teledermatology practices between March and June 2020. IT, information technology.
Platforms used for teledermatology consultations
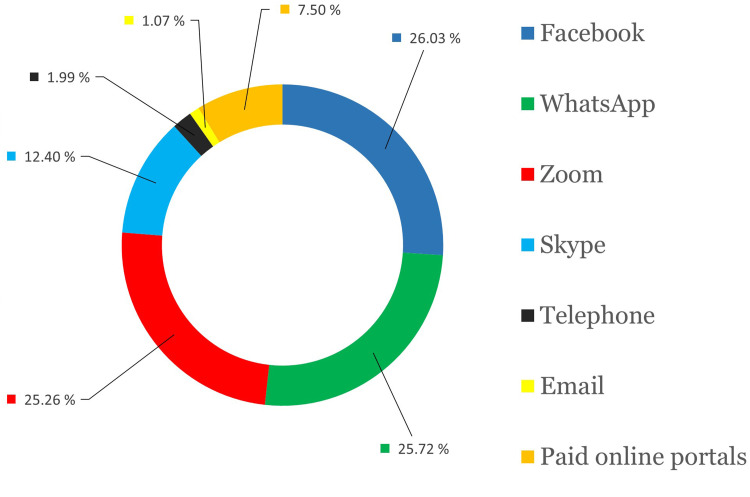
A large proportion (26.03%) of respondents received patient queries and performed subsequent consultations through the messaging application of Facebook (i.e. Facebook Messenger). Facebook Messenger, Facebook Messenger calls, and Facetime consultations were included in a single package for ease of counting. A total of 25.72% of respondents received patient requests and performed consultations through the WhatsApp messaging application. Zoom calls and video meetings were common, with 25.26% of patient requests received via messaging applications or email culminating in Zoom consultations. Many patients contacted hospitals and clinics telephonically, although the final teledermatology consultations with clinicians took place on Zoom. Regardless of the means of initial contact, Zoom was considered the final platform in all cases where the final two-way interaction with the specialist was on Zoom only. Skype video call was utilized in 12.40% of consultations. The proportion of telephonic consultations and off-line telephonic text messages was low, accounting for only 1.99% of total consultations. Actionable clinician–patient dialogue via email accounted for only 1.07% of all teledermatology consultations. Online portals (counted as one group) such as MyDerm Portal, Mend Family Portal, CareNA, opdox, eVisit, and Practo accounted for 7.50% of reported teledermatology consultations worldwide (Figure 2).
Figure 2.
Distribution of digital platforms and channels through which teledermatology consultations with respondents took place between March and June 2020.
Patient demographics, diagnoses, and outcomes
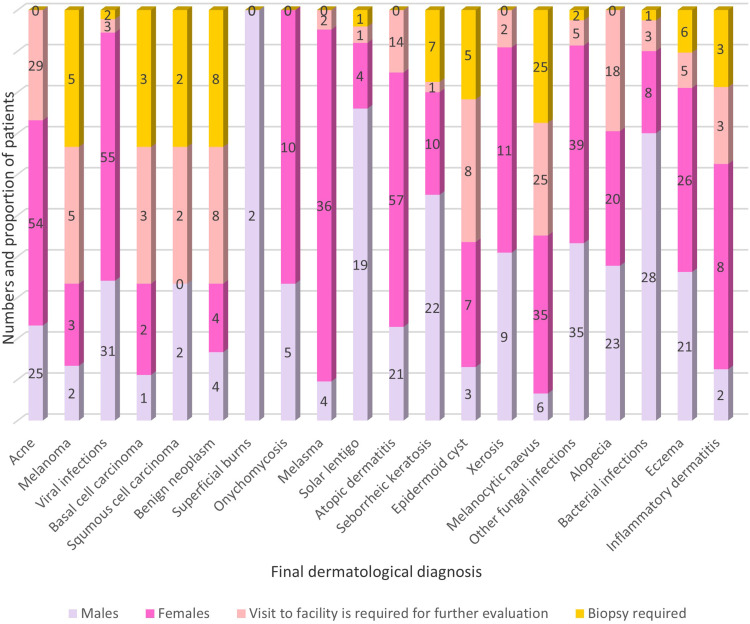
There was a predominance of female patients who sought teledermatology consultations (59.72%) when compared with the number of male patients (40.28%) utilizing these healthcare services. The common dermatological conditions presented during consultations were further categorized according to the sex of the patient. Notable sex-based differences were observed in the types of conditions presented during consultation. Women more commonly presented with acne, viral infections, and atopic dermatitis, while men only sought assistance with fungal, viral, and bacterial infections. The questionnaire enquired whether these patients were then referred for biopsy, in-person consultations, or blood tests. The distribution of dermatological diagnoses and consequent clinical actions are outlined in Figure 3.
Figure 3.
Final dermatological diagnoses of the patients who sought teledermatology consultations with the respondents between March and June 2020. The total number of patients with each diagnosis is indicated and is proportioned according to sex, further requirements for visits to healthcare facilities, and need for biopsy.
Respondents’ perspectives on the benefits and challenges of teledermatological practice
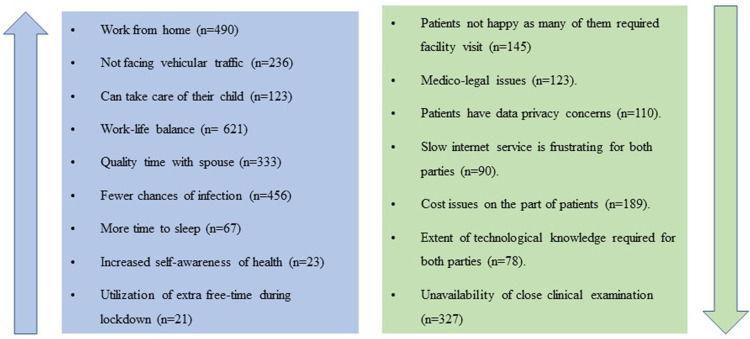
The questionnaire provided the opportunity for stakeholders to elaborate on the advantages and operational difficulties faced during the provision of teledermatology services, including patients’ perspectives and complaints that were usually processed by the administrative staff. Many dermatologists expressed empathy for their patients and made sincere efforts to keep patients' visits to healthcare facilities at a minimum for their safety. Overall, these efforts contributed to the reduced numbers of clinical investigations and biopsies performed when compared with pre-pandemic records (Figure 4).
Figure 4.
Stakeholders’ and patients’ perspectives on advantages and operational challenges associated with teledermatology services.
Discussion
Before the outbreak of COVID-19, patients worldwide preferred the traditional mode of face-to-face consultation when seeking medical treatment. Although telemedicine was already in effect pre-pandemic, only a small percentage of patients believed it to be a viable alternative to physical examination. Of all the telemedical and e-healthcare disciplines, teledermatology has been one of the most practiced forms of digital healthcare on a global scale, and its usage increased rapidly in response to the turbulent disruptions associated with the COVID-19 pandemic.
The rise in demand for teledermatology was accelerated because of the World Health Organization guidelines regarding social distancing and minimizing physical contact to prevent the spread of infection. 1 This was particularly relevant in the dermatology sector where close contact between practitioners and patients had been linked to increases in severe acute respiratory syndrome coronavirus 2 and other skin-related infections. 2 Teledermatology has helped prevent such occurrences, thereby protecting the lives of doctors and patients alike. 3 The rise of teledermatology during 2020 is accurately reflected in the results of this study. Interestingly, the respondents of this study reported having never been directly or indirectly involved in any form of teledermatology before the COVID-19 pandemic. Therefore, the data indicate that 653 healthcare personnel who were previously unaccustomed to virtual consultations readily embraced teledermatology as a means of continuing patient care. The adaptability and resilience displayed by healthcare workers in the face of unprecedented challenges are commendable.
Being a dermatologist herself, the author sought to connect with the global dermatology fraternity and to utilize her professional social media groups to extract information that would help the world better understand the multifaceted digital response that allowed the continuation of dermatological practice during the pandemic. In addition to supporting the exchange of digital data, teledermatology practitioners prefer platforms that allow for visual and audio connections with their patients. Knowing the importance of social media platforms, such as Facebook and WhatsApp, informed practitioners have adapted these technologies to support their practices in the modern age. Before the pandemic, WhatsApp was the preferred platform for patients to communicate directly with their practitioners, probably because of familiarity with the platform and ease of use. The continual advancement of mobile phone camera quality enables relatively clear visual inspection. Data gathered in this study emphasize patient familiarity with these platforms, and Facebook and WhatsApp were the platforms of choice by notable margins when compared with other means of digital connection. However, the emerging popularity of Zoom for telemedical practice was also reflected in stakeholder responses. Skype, which offers similar services to Zoom, was not nearly as popular. Very few patients used traditional landline telephonic and audio-only mobile calls, as well as emails, to communicate with practitioners. Previous studies on teledermatology have concentrated their efforts on divisions, such as mobile calls, video calls, emails, and WhatsApp messaging 4 ; this study has expanded this picture to show that social media platforms are a popular medium through which patients interacted with their consulting doctors.
Before the pandemic, social media and audio–visual digital platforms were used by practitioners to facilitate follow-up consultations; however, their use poses challenges to keeping detailed records and tracing medical histories, and there have always been questions about the security of patient data. In response to these challenges, modern online portals were developed that capture patient details and keep track of clinical courses. The relative security of these portals helped prevent data leakage to third parties and gained the trust of patients previously suspicious of telemedical approaches. However, data from the current study show that very few patients still preferred communication through paid digital online portals over the course of the pandemic. Clearly, patients and healthcare workers became avid participants in the virtual revolution during the COVID-19 era.
Despite the ever-improving audio–visual technologies, there are still challenges associated with their use for remote evaluation of skin conditions 5 and practitioners must take this into account when making diagnoses. As revealed by the gathered data, teledermatology consultations performed by respondents between March and June 2020 primarily dealt with skin abnormalities such as acne, as well as viral and fungal skin infections. A study conducted in Turkey during the first half of the pandemic reported that teledermatology could be appropriately applied to 72.8% of their caseload. 6 In comparison, the current study showed that 68.3% of patients were adequately managed using teledermatology alone. The remaining 31.7% of patients went on to visit healthcare facilities for further evaluation or biopsy.
A preponderance of women seeking teledermatological care was evident, with atopic dermatitis being the most common diagnosis among this cohort. On the other hand, male patients primarily sought consultation for infections, with most diagnoses being fungal infections at sites other than the nails. Ten patients referred for biopsy after a teledermatology consultation during the reporting period were later diagnosed with cutaneous malignancies, which is an indication that the occurrence of skin cancers was not halted by the pandemic. The fact that suspicious skin neoplasia was adequately identified during non-contact digital sessions gives credence to the value of telemedical practice. However, some patients and doctors still do not completely trust telemedicine to be an effective clinical approach to addressing severe health conditions, such as skin cancer. Further education and published evidence supporting the effectiveness of global telemedical approaches may help change these steadfast views. 7
Most practitioners who opted for teledermatology consultations worked in large cities, and many have chosen to maintain their teledermatology practices, even though restrictions have been eased. 8 Interestingly, teledermatology was more readily adopted by younger practitioners working in private medical facilities. However, doctors working with high patient numbers in government institutions and teaching hospitals would also benefit from adopting telemedical advancements. Virtual consultations may help curb problems of overcrowding and optimize the use of limited medical resources. 9 Further, the convenience and remote applicability of these technologies will help patients minimize time spent in hospitals. For example, one may attend a consultation while still at their workplace. There is an economic benefit to people not having to take time off work when requiring routine medical follow-up and traveling costs as well as other miscellaneous costs are also alleviated. 10 This may be especially relevant for dermatologists dealing with aesthetic cases.
Evidence shows that at least 71% of the global population has embraced telemedical innovation, and it is predicted that telemedical systems will remain in use even after the pandemic is over. 9 However, the continued use of teledermatology in the post-pandemic era when lockdowns become uncommon is a controversial topic of open debate. A study conducted in Austria opined that teledermatology should not replace traditional face-to-face consultation and should be restricted to the exchange of information between healthcare staff and routine follow-up examinations. 9 Similar views were expressed by a study conducted in the Department of Dermatology at the Yale School of Medicine in which 96% of all faculty members believed that total body skin examination should only be undertaken during physical consultation. 11 However, the COVID-19 pandemic has been an unusual time, and most patients had no other option other than seeking medical assistance through digital platforms.
The last section of the questionnaire was designed to elaborate on patient and practitioner experiences of teledermatology in practice. Participants were given the space to state their own and their patients' perspectives, which were categorized according to the general theme and counted; these data are summarized in Figure 4. Overall, healthcare providers enjoyed better work–life balance as a benefit of working from home. On the other hand, practitioners were despondent about the absolute unavailability of physical examination because of enforced restrictions, especially in the more serious cases. In these cases, teledermatology cannot totally substitute classical physical examination and the need to visit a clinical facility; however, during the pandemic, many patients expressed distress when referred to a healthcare facility for further evaluation.
The protection and securitization of private data is a topic of global relevance, and this is of particular importance in telemedical practices dealing with sensitive medical information. A potential disadvantage of digital medicine using social media and popular platforms is compromised patient security and privacy. For example, when two parties exchange contact details, it is possible that these details may be used later to satisfy private agendas, such as unsolicited advertising. This study identified data security as a concern raised by the majority of patients. Stakeholders also expressed concern about the level of technological skill and knowledge needed for effective consultation. Levels of technological literacy and internet connectivity are not equivalent in all populations, and patients will not benefit from systems they cannot properly access. There are also cultural implications wherein the sharing of intimate medical images may be considered taboo. It will be the responsibility of government and healthcare providers to adapt and implement policies that provide satisfactory and long-lasting solutions to these issues.
Understanding and predicting a population's response to the implementation of telemedicine relies on the identification of participants with prior training or cognizance of the associated technologies. A study conducted in Turkey in 2020 found that 79.4% of respondents had sound prior knowledge of teledermatology. 4 These results are in stark contrast with a study conducted in the same country in 2014 wherein 50% of participants reported having little to no knowledge of teledermatology approaches. 12 In this study, all the participants stated that they were not using teledermatology before the COVID-19 pandemic. However, the questionnaire was not designed to include leading questions aimed at evaluating the level of understanding of teledermatology before the pandemic.
To the best of the author's knowledge, this is the only study on teledermatology that has been conducted digitally using social media platforms, which has accepted respondent feedback from all over the world. These data reflect the real-world perspectives and experiences of private healthcare practitioners and staff from a broad range of countries, including India, the United Arab Emirates, and countries from Europe and South America. Previous studies of this nature account for the experiences in major academic institutions where in-house telemedical systems are capable of performing live interactive video consultations. 13 Additionally, data from the current study derive from medical practices operating outside of the telemedicine triage wherein a dermatology advisory panel was employed to determine the need for a face-to-face consultation on a case-by-case basis. 13 In fact, the use of the telemedicine triage was a novel concept to the author and respondents alike, and no respondents reported having encountered this practice in their daily activities. Potentially, this approach is favored in large academic institutions and is underrepresented in global clinical practice. However, the author believes that the triage approach may be instrumental in the continuation of teledermatology as an established practice.
In addition to common ailments, such as acne and eczema, this study identified infections as the most common dermatological diagnosis made using teledermatology among the cohort of respondents. In contrast, academic institutional research only reported common dermatological diagnoses and did not report diagnoses of infection, possibly because of local epidemiology. 13 Considerations of patient cost and the inability to perform physical examinations in many cases were identical in both studies. In summary, lessons learned from academic institutions may help develop and guide policies in other institutions, allowing them to replicate the success of teledermatology through the implementation of patient screening procedures and incorporation of telemedical software in electronic medical record-keeping systems.
Conclusion
Between March and June 2020, when the COVID-19 pandemic was at its initial peak, teledermatology became common practice, and the effects are ongoing as the world continues to deal with emerging COVID-19 variants. Therefore, it is vital that the relevant stakeholders invest in teledermatology and work together to develop the technology such that it will benefit all parties in the e-health sector. Teledermatology has allowed practitioners to improve their personal work–life balance and allowed patients full access to immediate, quality dermatological care. The advancement and development of teledermatology would be of benefit to the global population.
Acknowledgments
I would like to thank all respondents who were part of this study.
Footnotes
Data availability: All raw data are available upon request.
Declaration of conflicting interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Participant consent was obtained as part of the survey process. The study was conducted in compliance with the declaration of Helsinki.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Participant consent was obtained as part of the survey process. The study was conducted in compliance with the declaration of Helsinki.
ORCID iD: Piyu Parth Naik https://orcid.org/0000-0002-6499-4062
Trial registration: Not applicable, because this article does not contain any clinical trials.
References
- 1.World Health Organization. Advice for the public: Coronavirus disease (COVID-19), https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (2021, accessed 23 November 2021).
- 2.Kwatra SG, Sweren RJ, Grossberg AL. Dermatology practices as vectors for COVID-19 transmission: A call for the immediate cessation of nonemergent dermatology visits. J Am Acad Dermatol 2020; 82: e179–e180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang RH, Barbieri JS, Nguyen HP, et al. Clinical effectiveness and cost-effectiveness of teledermatology: Where are we now, and what are the barriers to adoption? J Am Acad Dermatol 2020; 83: 299–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Altunisik N, Turkmen D, Calikoglu E, et al. Views and experiences of dermatologists in Turkey about teledermatology during the COVID-19 pandemic. J Cosmet Dermatol 2020; 19: 2460–2463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee KJ, Finnane A, Soyer HP. Recent trends in teledermatology and teledermoscopy. Dermatol Pract Concept 2018; 8: 214–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Temiz SA, Dursun R, Daye M, et al. Evaluation of dermatology consultations in the era of COVID-19. Dermatol Ther 2020; 33: e13642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Trettel A, Eissing L, Augustin M. Telemedicine in dermatology: Findings and experiences worldwide—a systematic literature review. J Eur Acad Dermatol Venereol 2018; 32: 215–224. [DOI] [PubMed] [Google Scholar]
- 8.Sharma A, Jindal V, Singla P, et al. Will teledermatology be the silver lining during and after COVID-19? Dermatol Ther 2020; 33: e13643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eber EL, Janda M, Arzberger E, et al. Survey on the status of teledermatology in Austria. J Dtsch Dermatol Ges 2019; 17: 25–31. [DOI] [PubMed] [Google Scholar]
- 10.Eedy D, Wootton R. Teledermatology: A review. Br J Dermatol 2001; 144: 696–707. [DOI] [PubMed] [Google Scholar]
- 11.Asabor EN, Bunick CG, Cohen JM, et al. Patient and physician perspectives on teledermatology at an academic dermatology department amid the COVID-19 pandemic. J Am Acad Dermatol 2021; 84: 158–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yildiz H, Özlem KA, Bilgili ME. The use of teledermatology in daily practices among dermatologists in Turkey (in Turkish). Turk Dermatoloji Dergisi 2014; 8: 7–11. [Google Scholar]
- 13.Perkins S, Cohen JM, Nelson CA, et al. Teledermatology in the era of COVID-19: experience of an academic department of dermatology. J Am Acad Dermatol 2020; 83: e43–e44. [DOI] [PMC free article] [PubMed] [Google Scholar]