Abstract
Initial research has indicated that college students have experienced numerous stressors as a result of the pandemic. The current investigation enrolled the largest and most diverse sample of college students to date (N = 4714) from universities in New York (NY) and New Jersey (NJ), the epicenter of the North American pandemic in Spring 2020. We described the impact on the psychological, academic, and financial health of college students who were initially most affected and examined racial/ethnic group differences. Results indicated that students’ mental health was severely affected and that students of color were disproportionately affected by academic, financial, and COVID-related stressors. Worry about COVID-19 infection, stressful living conditions, lower grades, and loneliness emerged as correlates of deteriorating mental health. COVID-19’s mental health impact on college students is alarming and highlights the need for public health interventions at the university level.
Keywords: COVID-19, college students, minorities, race, ethnicity, mental health
During the first peak of the pandemic in March 2020, universities transitioned to remote learning, and college students experienced rapid changes in living situations and daily routines. Stay-at-home directives called for social distancing and isolation. These conditions are especially difficult for college students, who, as emerging adults, are already experiencing major life transitions, such as new living situations, academic expectations, romantic relationships, and greater exploration of racial/ethnic, gender, and sexual identities (Byrd & McKinney, 2012; Syed & Azmitia, 2009). Emerging adulthood is a distinct period between adolescence and adulthood characterized by identity exploration and the acquisition of skills needed for a successful transition to attaining financial independence and becoming self-sufficient (Arnett, 2000). While not all emerging adults are college students, given the shift to a knowledge-based economy in the United States (U.S.), about 70% of emerging adults enter post-secondary education (Arnett, 2016). Despite being a time for enormous personal growth, the college years coincide with the peak onset of most psychological disorders (Kessler et al., 2007). Academic-related stressors have been shown to be a major predictor of mental health issues among college students (Beiter et al., 2015). Psychological difficulties, in turn, are associated with school dropout and poor occupational attainment (Hjorth et al., 2016; Slominski et al., 2011). Because the COVID-19 pandemic has disrupted higher education, understanding its impact specifically on college students has substantial public health implications for the future well-being of our society (Conrad et al., 2020).
Many college students experienced the transition to remote learning as a significant stressor (Kecojevic et al., 2020). Prior to the pandemic, the majority were unfamiliar with remote learning, with only 35% ever enrolled in online courses (D’Amato, 2020; National Center for Education Statistics, 2021). In addition, for many students moving home meant a loss of academic resources (e.g., computers and internet access) and an increase in competing demands and distractions (e.g., caring for siblings and providing financial support) (Clabaugh et al., 2021; Kecojevic et al., 2020; Lederer et al., 2021). Virtual learning also precluded essential opportunities such as internships, research, and travel abroad (Lederer et al., 2021). Given these restrictions, it makes sense that academic stress and uncertainty about the future is notably high among college students (Son et al., 2020). According to Clabaugh et al. (2021), 33% of students reported their academic future to be significantly at risk due to COVID-19. Compared to White students, racially and ethnically minoritized students indicated greater concern about their academic future and a higher likelihood of withdrawing from classes in Fall 2020 (Clabaugh et al., 2021).
Given pre-existing inequalities in access to quality education, racially/ethnically minoritized students may disproportionately suffer negative academic consequences related to the pandemic, such as higher rates of dropout and longer time to graduation (Velez et al., 2019). Prior to the pandemic, 6 year college graduation rates were lower for American Indian (39%), Black (40%) and Latinx (54%) students relative to Asian (74%) and White students (64%) (de Brey et al., 2019; Shapiro et al., 2017). Since the pandemic began, many institutions of higher education that primarily serve minoritized students from low-income backgrounds, such as community colleges, historically Black colleges and universities (HBCUs), Minority Serving Institutions (MSIs), and Tribal Colleges and Universities (TCUs) have seen steep declines in enrollment (U.S. Department of Education’s Office for Civil Rights [OCR], 2021). In some cases, the declines for HBCUs, MSIs, and TCUs have surpassed enrollment decreases in predominantly White peer institutions (U.S. Department of Education’s OCR, 2021). Recent National Student Clearinghouse data shows a drop in enrolled Black and Hispanic college students in Fall 2020 compared to pre-pandemic (National Student Clearinghouse Research Center, 2020). The COVID-19 pandemic has negatively impacted students’ academic outcomes, including academic performance and persistence in college, jeopardizing their future occupational prospects (Lederer et al., 2021; National Student Clearinghouse Research Center, 2020; St. Amour, 2021).
The disruption in students’ lives resulting from COVID-19 related stressors has likely exacerbated the major mental health risks college students already face. Before the pandemic, it was well documented that rates of depression, anxiety, and suicidality were rising among college students and reaching record levels (Chen et al., 2019; Liu et al., 2019). In 2017, 36% of U.S. college students reported having a lifetime mental health diagnosis compared to 22% in 2007, with past-year suicidal ideation increasing from 5.8% to 10.8% in this same 10-year period (Lipson et al., 2019). The number of students screening positive for depression has also increased steadily, from 24.8% in 2009 to 29.9% in 2017 (Lipson et al., 2019). In addition, data from large national surveys of college students’ mental health suggest that depression and suicidal ideation and attempts are more prevalent among racially/ethnically minoritized groups (Chen et al., 2019; Eisenberg et al., 2013). This surge in the frequency and severity of mental health problems among college students has outpaced the availability of mental health services on college campuses (Cornish et al., 2017; Kern et al., 2018). Untreated mental health problems can interfere with the completion of the developmental tasks of emerging adulthood, such as career preparation and sustaining friendships and romantic relationships, which can hinder future occupational and relational success (Schwartz, 2016).
Not surprisingly, both within the United States and in other countries, the prevalence of anxiety and depression among college students is on the rise since the pandemic (Cao et al., 2020; Fruehwirth et al., 2021; Huckins et al., 2020; Islam et al., 2020; Liu et al., 2020; Son et al., 2020). For instance, Fruehwirth et al. (2021) found that rates of moderate to severe anxiety symptoms increased from 18.1% pre-pandemic (October 2019-February 2020) to 25.3% mid-pandemic (June/July 2020) among first-year students attending a large public university. Similarly, the prevalence of moderate to severe depression symptoms increased from 21.5% to 31.7%, with rates increasing upwards of 90% for Black students (Fruehwirth et al., 2021). Because of these concerning trends, researchers have begun to investigate what factors may predict students’ declining mental health. With regard to academic factors, experiencing difficulty with online learning, having distractions in your current environment, and increased students’ beliefs that their academic future is at risk have been found to be associated with increased anxiety and depression (Clabaugh et al., 2021; Fruehwirth et al., 2021; Kecojevic et al., 2020).
Social isolation and loneliness have also been found to be related to worse mental health outcomes (Matthews et al., 2016). The social isolation resulting from stay-at-home orders and quarantine has led to increased feelings of loneliness among college students (Birmingham et al., 2021; Liu et al., 2020). While loneliness is a strong risk factor for depression and anxiety across the lifespan (Matthews et al., 2016; Okruszek et al., 2020), rates of loneliness are consistently found to be elevated among emerging adults relative to other developmental periods (Liu et al., 2020; Matthews et al., 2016). Thus, we would expect that isolation during the pandemic intensified these feelings among college students. For example, Hamza et al. (2020) unexpectedly found that Canadian college students without pre-existing mental health concerns were more likely to report psychological distress during the pandemic than those with previous mental health needs and that social isolation may have accounted for the worsening of their mental health. Two other studies point to the possibility that living with family or family support may be associated with better outcomes, including lower anxiety and fewer symptoms of depression and posttraumatic stress disorder (PTSD) (Liu et al., 2020; Sundarasen et al., 2020). Liu et al. (2020) also found that loneliness, worries about COVID-19, and low distress tolerance predicted clinical levels of depression, anxiety, and PTSD symptoms.
These existing studies have provided informative preliminary data about the impact of COVID-19 on emerging adults. However, study samples have been limited. Most have either been small or recruited from a single university (Kecojevic et al., 2020; Rudenstine et al., 2020), thus limiting their broader implications. Others report on students from an area of the country that had not yet experienced high COVID-19 rates in Spring 2020 (e.g., Texas and Ohio) (Lechner et al., 2020; Wang et al., 2020). Lastly, samples have lacked diversity with regard to economic status or race/ethnicity, thus limiting our understanding of COVID-19’s impact on potentially the most vulnerable university students. Due to systemic social inequality and income disparities, those of lower socioeconomic status (SES) and/or racially/ethnically minoritized backgrounds may have additional financial, structural, and health challenges that magnify COVID-19’s detrimental effects on development (Singu et al., 2020). Racially/ethnically minoritized students are disproportionately likely to suffer negative academic and mental health consequences due to the pandemic given the additional challenges they experience, such as disparities in underlying health and mental health comorbidities, lack of access to quality healthcare, and poor living and work conditions caused by structural racism (Bailey et al., 2017; Hankerson et al., 2011; Lederer et al., 2021).
The current investigation enrolled the largest and most diverse sample of college students to date (N = 4714) who were attending universities in New York (NY) and New Jersey (NJ), the North American epicenter of the pandemic in Spring of 2020. By the end of May 2020, NY and NJ ranked first and second in the number of COVID-19 cases and related deaths in America (The Atlantic Monthly Group, 2020). The evaluation was conducted from April 23 to May 31, 2020, about one month after NY and NJ issued state-wide stay-at-home mandates. The purpose of the current study was to describe the impact on the mental, academic, and financial health of college students who were initially the most affected and to examine these consequences across various racial and ethnic groups. In addition, we explored factors potentially related to changes in mental health, such as academic stressors and feelings of loneliness. Although our study was exploratory and descriptive in nature, such studies are a key first step toward understanding pandemic-related outcomes and can inform future studies that are more targeted and theory-driven. Our study aims are consistent with Holmes et al. (2020) call for researchers to measure the mental health effects of the pandemic among high-risk individuals, specifically those who are young, from racial/ethnic minorities, or of low socioeconomic status. A better understanding of the impact of the pandemic on college students and circumstances that may place individuals at increased risk can inform future public health interventions.
Method
Participants
An online survey assessing the academic, financial, social, and mental health impact of COVID-19 on college students was conducted in Spring 2020. The initial sample was 4808 students with 94 removed due to not responding to any mental health questions. Thus, the final sample consisted of 4714 college students attending a university in NY or NJ. There were no significant differences in demographics between removed participants and the remaining sample. Students from 55 universities responded to the survey with the vast majority (n = 4225; 88%) enrolled at Montclair State University, State University of New York at Buffalo, Brooklyn College, Rutgers University, New York University, and Fordham University.
Detailed demographic characteristics are displayed in Table 1. Participants were 76.1% female with a mean age of 21.29 (SD = 3.86). Ninety-seven percent were between the ages of 18 and 30 years. The sample was diverse with 43.9% of college students self-identifying as Non-Latinx White (White), 22.6% as Latinx/Hispanic (Latinx), 18.4% as Non-Latinx Asian or Pacific Islander (Asian), 8.3% as Non-Latinx Black (Black), 0.1% as American Indian or Alaska Native, 3.0% Mixed Race, and 1.8% as Other. Year in college was equally distributed from freshman to senior year, with a minority in their fifth year or more. Over 75% of participants were enrolled in a public university. The majority reported living with at least one parent (83.0%), having their own room (76.9%), and having access to a computer with internet in their home during the pandemic (97.9%). Approximately one-third (36.8%) of the sample were first-generation college students (i.e., parents did not attend college) and over half were receiving federal or state tuition assistance.
Table 1.
Sample Demographic Characteristics (N = 4714).
| Demographic Characteristics | N (%) |
|---|---|
| Age | |
| Mean ± SD | 21.3 ± 3.9 |
| Median, Range | 21, 18–50 |
| Sex (Assigned at Birth) | |
| Female | 3586 (76.1) |
| Male | 1107 (23.5) |
| Other or Prefer Not to Disclose | 21 (0.4) |
| Race/Ethnicity | |
| Black | 392 (8.3) |
| White | 2070 (43.9) |
| Latinx/Hispanic | 1064 (22.6) |
| Asian or Pacific Islander | 868 (18.4) |
| American Indian or Alaska Native | 6 (0.1) |
| Mixed Race | 142 (3.0) |
| Other | 83 (1.8) |
| Prefer Not to Disclose | 89 (1.9) |
| Class Year as of Spring 2020 | |
| First (Freshmen) | 927 (19.7) |
| Second (Sophomore) | 1015 (21.5) |
| Third (Junior) | 1283 (27.2) |
| Fourth (Senior) | 1175 (24.9) |
| Fifth Year or More | 247 (5.2) |
| Prefer Not to Disclose | 66 (1.4) |
| First-Generation College Student | |
| No | 2918 (61.9) |
| Yes | 1734 (36.8) |
| Prefer Not to Disclose | 57 (1.2) |
| Public or Private University | |
| Public | 3714 (78.8) |
| Private | 983 (20.9) |
| Prefer Not to Disclose | 17 (0.4) |
| Currently Receiving Financial Assistance | |
| No | 1912 (40.6) |
| Yes | 2620 (55.6) |
| Prefer Not to Disclose | 182 (3.9) |
| Has Health Insurance (Including Medicaid or Other Government Provided Insurance) | |
| No | 198 (4.2) |
| Yes | 4341 (92.1) |
| Prefer Not to Disclose | 175 (3.7) |
| Currently Living with Parent(s) | |
| Yes | 3912 (83.0) |
| Moved From Dorms to Family Home | 2005 (42.5) |
| Has Their Own Room | |
| No | 1047 (22.2) |
| Yes | 3623 (76.9) |
| Prefer Not to Disclose | 44 (0.9) |
| Currently Has a Computer with Internet Access | |
| No | 74 (1.6) |
| Yes | 4615 (97.9) |
| Prefer Not to Disclose | 25 (0.5) |
Procedure
The Institutional Review Board at the first author’s university approved study procedures, and informed consent was obtained electronically. The online survey was conducted from April 23, 2020 to May 31, 2020, about one month after NY and NJ issued state-wide stay-at-home mandates and before each state entered Phase 2 of reopening. Students who were 18 years of age or older and enrolled in a college or university in NY or NJ were eligible to participate. Participants across universities were either recruited online via university email listservs to undergraduate students or through psychology department research subject pools for class credit. In addition, the survey link was posted on social media (e.g., Facebook and Twitter). Participants were asked to complete an online Qualtrics survey about their financial, academic, social, and psychological experiences during the pandemic. At the end of the survey, participants were provided with a list of financial and mental health resources. As an incentive, participants were given the opportunity to enter a drawing to win one of four $100 gift cards.
Measures
The survey questions were developed by a group of faculty members across NY and NJ universities, referred to as COVID-19 College Workgroup (study authors Masia Warner et al., 2020). The survey spanned several topics including demographic characteristics, COVID-related stressors, changes in socialization and social media use, and financial, academic, and mental health changes related to the pandemic.
COVID-Related Stress (four items)
Participants reported stress associated with changes in living situation ranging from much less to much more stressful (i.e., how stressful are your current living arrangements compared to how they were before the COVID-19 outbreak?) and whether they or someone they lived with had COVID-19 (Yes or No). Using a 5-point Likert-type scale from Never to All the time, students reported how often they worry about them or their family members contracting COVID-19. The final item queried how many people close to them had died from COVID-19, ranging from none to more than three.
Socialization, Social Media Use, and Loneliness (three questions)
Two questions asked participants about how their socializing and social media use had changed since the COVID-19 outbreak with options ranging from A lot less to A lot more. In addition, participants reported the degree of change in loneliness from A lot less to A lot more.
Financial Impact (three items)
Using a 5-point Likert-type scale ranging from Not at all to Extremely, students reported how much their finances had been impacted by COVID-19 and how concerned they were about being able to afford food. Additionally, students were asked about whether changes occurred to their employment due to the pandemic, including reduced work hours or job loss.
Academic Impact (five items)
Students were first asked whether they expected to finish their Spring coursework successfully (i.e., get credits for all classes) (Yes or No). On a 5-point Likert-type scale from Not at all to Extremely, students also indicated to what degree the COVID-19 pandemic: 1) interfered with their ability to graduate on time and 2) negatively impacted their grades, as well as 3) how likely financial difficulties would prevent them from returning to college, and 4) their degree of worry related to obtaining jobs in their desired fields after graduation.
Mental Health (eight items)
To examine changes in mental health, on a 5-point Likert-type scale from Not at all to Extremely, students were asked how much their mental health had been affected by the COVID-19 outbreak and how hopeful they were that things will soon improve. In addition, from A lot less to A lot more, students indicated the degree of change in the following six symptoms: feeling down or depressed; feeling hopeless; feeling nervous, anxious, or on edge; not being able to stop worrying; frustration or boredom; and sleep problems. The depression and anxiety symptoms were derived from the Patient Health Questionnaire-4 (PHQ-4; Kroenke et al., 2009).
Data Analysis
All analyses were conducted using IBM SPSS Version 26. Descriptive statistics and frequencies were calculated for all survey items in each category, namely COVID-related stressors, financial impact, academic impact, changes in socialization and social media use, and mental health. For the frequencies and the chi-square analyses, questions that assessed degree of change were collapsed into less, no change, or more, and Likert-type scale anchors of Very much and Extremely were combined. Given our diverse sample and the disproportionate impact of COVID-19 on racial and ethnic minorities (Kantamneni, 2020; Webb Hooper et al., 2020), item responses are presented overall and separately by the sample’s four main racial/ethnic groups: Black, White, Latinx, and Asian. Racial/ethnic groups that were less than 5% of the total sample (e.g., American Indian or Alaska Native) were not reported on separately. Chi-Square Tests of Independence were conducted to examine racial/ethnic differences across the survey items. Bonferroni corrections were used to correct alpha levels for each domain (e.g., academic and financial) such that .05 was divided by the number of items within a category. In addition, given the large sample size and its impact on measures of statistical significance, we used Cramer’s V (Ferguson, 2009) to determine the strength of the association between study measures and race/ethnicity. Variables with a Cramer’s V value of 0.10 or higher were considered to have more meaningful and practical racial/ethnic differences in item responses (Cohen, 1988). To determine which specific racial/ethnic groups differed, we used a column proportions z-test with Bonferroni corrections, which assessed whether the proportion of cases for each item response significantly differed between groups.
To identify which factors were associated with worsening mental health due to the pandemic, we took several steps. First, we used a 4-item composite score (Depression/Anxiety Score) largely based on the PHQ-4 (Kroenke et al., 2009) to assess depression and anxiety symptoms (feeling down or depressed; feeling hopeless; feeling nervous, anxious, or on edge; and not being able to stop worrying). Pearson correlations between these mental health symptoms revealed strong inter-item correlations of greater than .50. The four items were averaged to create a mean composite Depression/Anxiety Score, which was used as a criterion variable in the regression model. The internal consistency for this composite score was 0.82. The second criterion variable was the item that assessed the degree to which students’ mental health had been affected by COVID-19 (referred to as mental health impact). Bivariate correlations were then computed between each survey item and each of these two criterion variables. Due to potential racial/ethnic differences in predictors, we computed all correlations for the entire sample and each racial/ethnic group. Six items showed at least moderate bivariate correlations with either criterion variable (approximately 0.30 or higher), and thus were used as the predictors in two multiple linear regressions to help best identify the factors with significant unique relationships with the mental health criterion variables.
Based on the above steps and considerations, two regression models were conducted, one for each criterion variable: Depression/Anxiety Score and mental health impact. Race/ethnicity (for the four racial/ethnic main groups) was entered as a covariate in both regression models to adjust for any unique relationship with the criterion variables. One item (i.e., worry that you or a family member will contract COVID-19) demonstrated the largest discrepancy in correlational strength across racial/ethnic groups. As a result, we performed additional moderation analyses to test whether racial/ethnic group interacted with worry about COVID-19 in predicting the mental health outcomes. However, none of the interaction terms reached statistical significance. We also screened for univariate and multivariate outliers in the non-binary regression variables. For multivariate outliers, Mahalanobis distance was used to identify any potential outliers. Eight participants had Mahalanobis distance values significant at the p < .001 level. We performed the two regression models with these eight participants removed. Patterns of results were unchanged from the results reported below. Finally, we conducted multi-level analyses to evaluate whether accounting for the nested nature of the data within colleges/universities (school) impacted the conclusions of the two regression analyses. We included a random intercept in the multi-level models with school acting as the clustering variable. Intraclass correlation coefficients (ICC) were less than .05 in all models, suggesting little variance in the criterion variables existed at the school level. Moreover, patterns of significance in the fixed effects predictors were similar across single- and multi-level models. All supplementary analyses and results mentioned above can be found on the Open Science Framework (https://osf.io/yzuqr/).
Results
COVID-Related Stressors
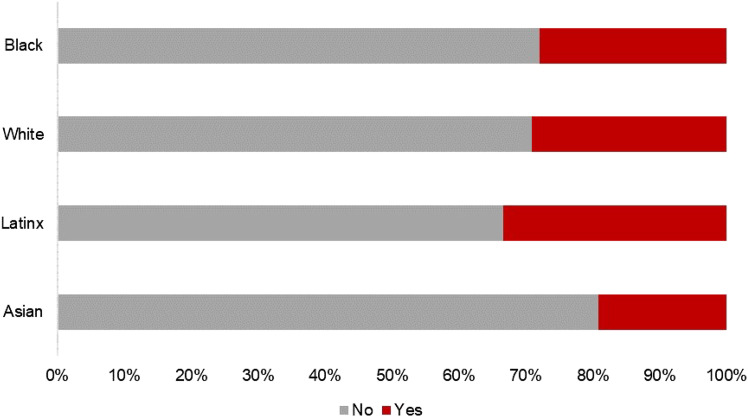
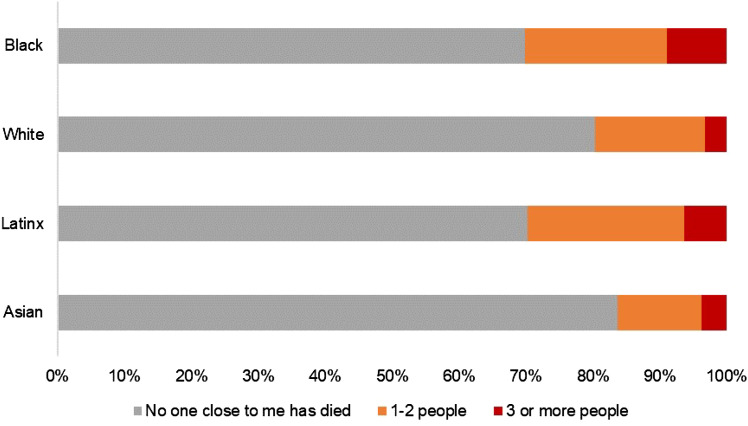
As shown in Table 2, almost half (48%) of the sample reported increased stress as a result of their current living arrangements compared to before the pandemic. About 29% either had COVID-19 or lived with someone who had the virus, and more than half (58%) indicated consistent (Often/All the Time) worry about their own risk or their family’s risk of becoming infected. Nearly one-quarter (23%) of students reported losing someone close to them due to COVID-19. Racial/ethnic differences were found for COVID-19 incidence and associated death. Specifically, Asian college students and their families (19%) were less likely to have contracted COVID-19 than Black (28%), White (29%), and Latinx students (33%) who had similar rates (see Figure 1). Black (30%) and Latinx students (30%) were more likely than White (20%) and Asian students (16%) to experience the death of a loved one due to COVID-19 (see Figure 2).
Table 2.
Impact of COVID-Related Stressors for the Overall Sample and by Racial/Ethnic Group.
| Overall N (%) |
Black N (%) |
White N (%) |
Latinx N (%) |
Asian N (%) |
χ2 | Cramer’s V | |
|---|---|---|---|---|---|---|---|
| Stress of current living | |||||||
| Less stressful | 522 (11.3) | 45 (11.9) | 229 (11.2) | 101 (9.7) | 114 (13.4) | 11.57 | .04 |
| Same amount of stress | 1863 (40.4) | 161 (42.7) | 830 (40.7) | 444 (42.8) | 313 (36.8) | ||
| More stressful | 2223 (48.2) | 171 (45.4) | 97 (48.0) | 492 (47.4) | 424 (49.8) | ||
| You or someone you live with had COVID-19 | |||||||
| No | 3292 (71.5) | 276a (72.1) | 1439a (70.9) | 689a (66.6) | 683b (80.8) | 51.03* | .11+ |
| Yes | 1312 (28.5) | 107a (27.9) | 590a (29.1) | 346a (33.4) | 162b (19.2) | ||
| Worry that you or a family member will get COVID-19 | |||||||
| Never | 157 (3.4) | 18 (4.7) | 68 (3.3) | 27 (2.5) | 30 (3.5) | 27.21* | .05 |
| Rarely | 439 (9.4) | 39 (10.1) | 214 (10.4) | 78 (7.4) | 86 (9.9) | ||
| Sometimes | 1354 (18.9) | 120 (31.0) | 615 (29.9) | 272 (25.6) | 265 (30.6) | ||
| Often or All the Time | 2736 (58.4) | 210 (54.3) | 1163 (56.5) | 684 (64.5) | 484 (56.0) | ||
| People close to you who have died from COVID-19 | |||||||
| 0 people | 3556 (77.3) | 266a (69.8) | 1626b (80.3) | 730a (70.3) | 708b (83.7) | 83.36* | .10+ |
| 1–2 people | 822 (17.9) | 81a,b (21.3) | 331b,c (16.4) | 243a (23.4) | 106c (12.5) | ||
| 3 or more people | 222 (4.8) | 34a (8.9) | 67b (3.3) | 66a,c (6.4) | 32b,c (3.8) | ||
Note. Since four chi-square tests were conducted for this category, we used Bonferroni corrections to adjust our alpha level to .013.
*p < .013.
a, b, c Racial/ethnic groups with the same letter subscripts had column proportions that did not differ significantly from each other according to column proportion z-tests with Bonferroni corrections. Column proportion z-tests were only performed on items that demonstrated at least a small effect size using Cramer’s V.
+small effect size.
Figure 1.
Have you or someone you live with had COVID-19?
Figure 2.
How many people close to you who have died from COVID-19?
Financial Stress
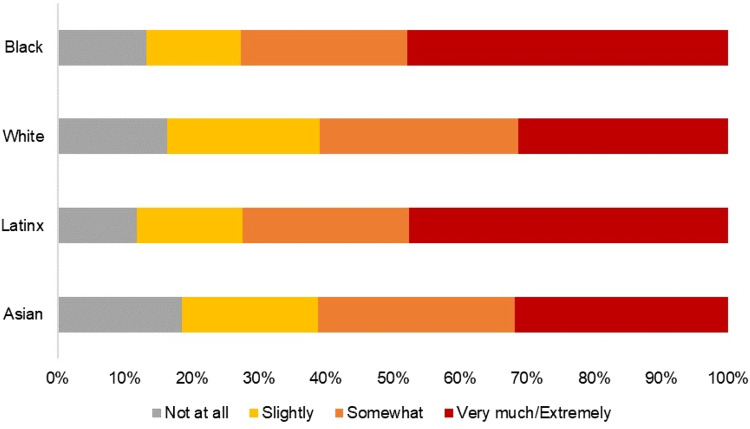
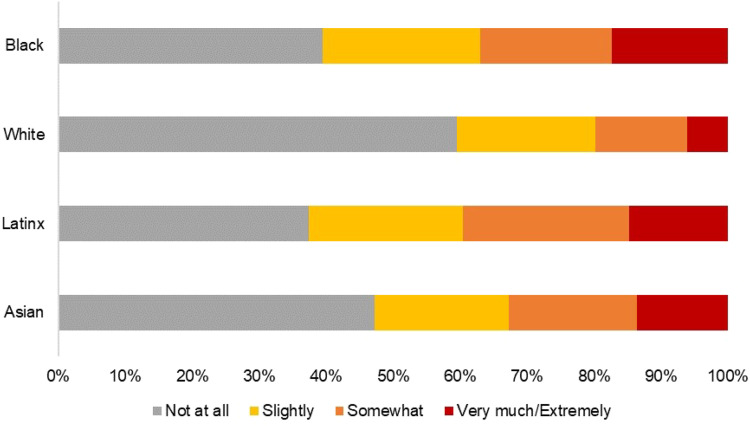
About half (49%) of our sample reported either losing their employment or having their hours reduced. In addition, 37% reported marked financial impact (Very much/Extremely), with nearly one-third (29%) of students reporting they were at least somewhat concerned about being able to afford food. Regarding racial/ethnic differences, Black (48%) and Latinx (48%) students were more likely than White (31%) and Asian (32%) students to report severe (Very much/Extremely) financial impact due to the pandemic (see Figure 3), and Black (17%), Latinx (15%), and Asian (14%) students reported greater severe concern than White (6%) students about affording food (see Table 3 and Figure 4).
Figure 3.
How much have your finances been impacted by the COVID-19 outbreak?
Table 3.
Financial Impact of COVID-19 for Overall Sample and by Racial/Ethnic Group.
| Overall N (%) |
Black N (%) |
White N (%) |
Latinx N (%) |
Asian N (%) |
χ2 | Cramer’s V | |
|---|---|---|---|---|---|---|---|
| Change in your employment status | |||||||
| Reduced hours or lost job | 2267 (49.1) | 193 (50.1) | 1012 (49.5) | 562 (54.1) | 355 (42.2) | 40.67* | .07 |
| No change | 2052 (44.4) | 164 (42.6) | 893 (43.7) | 404 (38.9) | 447 (53.1) | ||
| Increased hours or started job | 302 (6.5) | 28 (7.3) | 139 (6.8) | 73 (7.0) | 40 (4.8) | ||
| Finances impacted by COVID-19 | |||||||
| Not at all | 707 (15.3) | 51a,b,c (13.3) | 332c (16.3) | 123b (11.8) | 156a,c (18.5) | 115.84* | .10+ |
| Slightly | 914 (19.8) | 54a (14.1) | 463b (22.8) | 164a,c (15.8) | 172b,c (20.4) | ||
| Somewhat | 1286 (27.9) | 95a,b (24.7) | 602b (29.6) | 258a (24.8) | 247a,b (29.3) | ||
| Very much or Extremely | 1707 (37.0) | 184a (47.9) | 638b (31.4) | 496a (47.6) | 269b (31.9) | ||
| Concern about affording food | |||||||
| Not at all | 2305 (49.5) | 153a, b (39.5) | 1219c (59.6) | 393b (37.4) | 405a (47.3) | 211.53* | .13+ |
| Slightly | 992 (21.3) | 91a (23.5) | 422a (20.6) | 241a (23.0) | 172a (20.1) | ||
| Somewhat | 851 (18.3) | 76a, b (19.6) | 280c (13.7) | 261b (24.9) | 164a (19.1) | ||
| Very much or Extremely | 505 (10.9) | 67a (17.3) | 126b (6.2) | 155a (14.8) | 116a (13.5) | ||
Note. Since three chi-square tests were conducted for this category, we used Bonferroni corrections to adjust our alpha level to .017.
a, b, c Racial/ethnic groups with the same letter subscripts had column proportions that did not differ significantly from each other according to column proportion z-tests with Bonferroni corrections. Column proportion z-tests were only performed on items that demonstrated at least a small effect size using Cramer’s V.
*p < .017. +small effect size.
Figure 4.
Since the COVID-19 outbreak, how concerned are you about being able to afford food?
Academic Impact
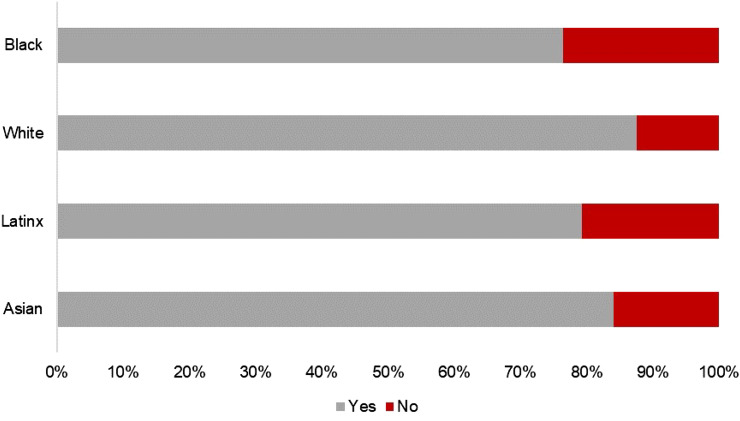
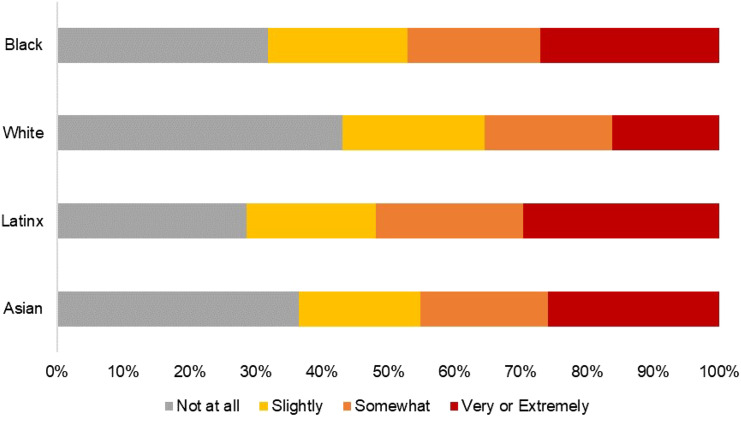
Most students (84%) expected to finish their Spring coursework successfully, and the majority (66%) did not report that COVID-19 interfered with their ability to graduate on time. About a quarter of students believed that COVID-19 had a severe (Very much/Extremely) impact on their grades (26%) and finances affecting their ability to return to college in the Fall (23%). Finally, about 41% reported severe (Very/Extremely) worry about finding a job in their desired field following graduation (see Table 4). Compared to White (88%) and Asian (84%) students, Black (77%) and Latinx (79%) students reported a significantly lower likelihood of expecting to complete the Spring semester (see Figure 5). In addition, Black (27%), Latinx (30%), and Asian (26%) students were more likely to express serious concern (Very much/Extremely), relative to White (16%) individuals, about being able to return to college due to financial difficulties (see Figure 6).
Table 4.
Academic Impact of COVID-19 for Overall Sample and by Racial/Ethnic Group.
| Overall N (%) |
Black N (%) |
White N (%) |
Latinx N (%) |
Asian N (%) |
χ2 | Cramer’s V | |
|---|---|---|---|---|---|---|---|
| Complete Spring coursework | |||||||
| Yes | 3879 (83.7) | 293a (76.5) | 1795b (87.6) | 828a (79.2) | 710b (84.0) | 52.65* | .11+ |
| No | 756 (16.3) | 90a (23.5) | 255b (12.4) | 217a (20.8) | 135b (16.0) | ||
| Interfered with graduating on time | |||||||
| Not at all | 3067 (66.0) | 249 (64.7) | 1446 (70.8) | 669 (63.6) | 507 (59.2) | 54.82* | .07 |
| Slightly | 733 (15.8) | 53 (13.8) | 310 (15.2) | 174 (16.5) | 152 (17.7) | ||
| Somewhat | 524 (11.3) | 47 (12.2) | 180 (8.8) | 131 (12.5) | 122 (14.2) | ||
| Very or Extremely | 320 (6.9) | 36 (9.4) | 106 (5.2) | 78 (7.4) | 76 (8.9) | ||
| Negative impact on grades | |||||||
| Not at all | 1123 (24.0) | 103 (26.4) | 539 (26.2) | 224 (21.2) | 191 (22.2) | 45.73* | .06 |
| Slightly | 1094 (23.4) | 73 (18.7) | 518 (25.2) | 227 (21.5) | 196 (22.7) | ||
| Somewhat | 1256 (26.8) | 89 (22.8) | 550 (26.7) | 295 (27.9) | 246 (28.5) | ||
| Very or Extremely | 1207 (25.8) | 125 (32.1) | 450 (21.9) | 312 (29.5) | 229 (26.6) | ||
| Worry finances will impact return to school in Fall 2020 | |||||||
| Not at all | 1647 (36.7) | 119a,b (31.8) | 848c (43.1) | 290b (28.6) | 303a (36.5) | 113.34* | .10+ |
| Slightly | 914 (20.4) | 79a (21.1) | 422a (21.5) | 198a (19.5) | 152a (18.3) | ||
| Somewhat | 904 (20.1) | 75a (20.1) | 378a (19.2) | 225a (22.2) | 160a (19.3) | ||
| Very or Extremely | 1023 (22.8) | 101a (27.0) | 319b (16.2) | 300a (29.6) | 215a (25.9) | ||
| Worry about difficulty finding a job in desired field | |||||||
| Not at all | 1086 (23.4) | 117 (30.6) | 505 (24.7) | 252 (24.1) | 160 (18.4) | 31.36* | .05 |
| Slightly | 748 (16.1) | 59 (15.4) | 321 (15.7) | 181 (17.3) | 131 (15.3) | ||
| Somewhat | 914 (19.7) | 80 (20.9) | 384 (18.8) | 200 (19.1) | 187 (21.8) | ||
| Very or Extremely | 1896 (40.8) | 126 (33.0) | 833 (40.8) | 414 (39.5) | 381 (44.4) | ||
Note. Since five chi-square tests were conducted for this category, we used Bonferroni corrections to adjust our alpha level to .01.
*p < .01. +small effect size
a, b, c Racial/ethnic groups with the same letter subscripts had column proportions that did not differ significantly from each other according to column proportion z-tests with Bonferroni corrections. Column proportion z-tests were only performed on items that demonstrated at least a small effect size using Cramer’s V.
Figure 5.
Do you expect to be able to finish your Spring 2020 coursework successfully?
Figure 6.
How likely are you to have financial difficulties due to COVID-19 that will impact you returning to college in Fall 2020?
Changes in Socialization, Social Media Use, and Loneliness
The vast majority of students reported connecting to family and friends less frequently (73%) and using more social media (75%) compared to before the COVID-19 pandemic. In addition, 68% indicated increased loneliness. As seen in Table 5, two of three items reached statistical significance between racial/ethnic groups at the adjusted alpha level of .017, but none reached a Cramer’s V of 0.10.
Table 5.
Socialization, Social Media Use, and Loneliness for Overall Sample and by Racial/Ethnic Group.
| Overall N (%) |
Black N (%) |
White N (%) |
Latinx N (%) |
Asian N (%) |
χ2 | Cramer’s V | |
|---|---|---|---|---|---|---|---|
| Change in socialization with family/friends | |||||||
| Connect less | 3430 (73.4) | 231 (59.8) | 1610 (78.3) | 738 (70.2) | 622 (72.4) | 74.66* | .09 |
| Not changed | 517 (11.1) | 70 (18.1) | 198 (9.6) | 113 (10.7) | 95 (11.1) | ||
| Connect more | 724 (15.5) | 85 (22.0) | 249 (12.1) | 201 (19.1) | 142 (16.5) | ||
| Change in social media use | |||||||
| Less than usual | 336 (7.2) | 34 (8.7) | 121 (5.9) | 83 (7.8) | 71 (8.2) | 13.82 | .04 |
| No change | 790 (18.1) | 83 (21.3) | 374 (18.1) | 193 (18.2) | 141 (16.3) | ||
| More than usual | 3503 (74.6) | 272 (69.9) | 1569 (76.0) | 786 (74.0) | 653 (75.5) | ||
| Change in loneliness | |||||||
| Less than usual | 321 (6.9) | 38 (9.9) | 111 (5.4) | 89 (8.4) | 59 (6.9) | 33.00* | .06 |
| No change | 1186 (25.4) | 119 (30.9) | 480 (23.4) | 282 (26.7) | 224 (26.2) | ||
| More than usual | 3157 (67.7) | 228 (59.2) | 1460 (71.2) | 685 (64.9) | 573 (66.9) | ||
Note. Since three chi-square tests were conducted for this category, we used Bonferroni corrections to adjust our alpha level to .017.
*p < .017.
Mental Health
Across the board, college students reported detrimental effects on their psychological functioning. More than 40% of students indicated that their mental health had been markedly affected by COVID-19 (Very much/Extremely). Most students reported feeling more down or depressed (74%), feeling more anxious (76%), and experiencing more frustration or boredom (83%). A sizable proportion of students also reported uncontrollable worry (65%), sleep problems (68%), and feeling hopeless (60%). Finally, students were split on whether they believed the pandemic would soon improve; about half (53%) reported being at least feeling Somewhat hopeful. As seen in Table 6, three items were statistically significant for racial/ethnic differences at the adjusted alpha level of .006, but none reached a Cramer’s V of 0.10.
Table 6.
Impact of COVID-19 on Mental Health for Overall Sample and by Racial/Ethnic Group.
| Overall N (%) |
Black N (%) |
White N (%) |
Latinx N (%) |
Asian N (%) |
χ2 | Cramer’s V | |
|---|---|---|---|---|---|---|---|
| Impact on Mental Health Quality | |||||||
| Not at all | 399 (8.5) | 43 (11.1) | 159 (7.7) | 87 (8.2) | 85 (9.8) | 25.91 | .04 |
| Slightly | 935 (19.9) | 76 (19.6) | 420 (20.4) | 191 (18.0) | 183 (21.2) | ||
| Somewhat | 1397 (29.8) | 107 (27.6) | 639 (31.0) | 291 (27.4) | 279 (32.3) | ||
| Very much or Extremely | 1962 (41.8) | 162 (41.8) | 842 (40.9) | 494 (46.5) | 318 (36.8) | ||
| Hopeful pandemic will improve | |||||||
| Not at all | 876 (18.8) | 63 (16.7) | 403 (19.7) | 188 (17.9) | 148 (17.2) | 36.04 | .05 |
| Slightly | 1317 (28.3) | 96 (25.5) | 581 (28.4) | 288 (27.4) | 265 (30.9) | ||
| Somewhat | 1582 (34.0) | 115 (30.5) | 717 (35.0) | 348 (33.0) | 306 (35.7) | ||
| Very much or Extremely | 873 (18.8) | 103 (27.3) | 345 (16.9) | 229 (21.7) | 139 (16.2) | ||
| Feeling down or depressed | |||||||
| Less than usual | 260 (5.6) | 32 (8.2) | 91 (4.4) | 63 (6.0) | 55 (6.4) | 16.14 | .04 |
| No change | 976 (20.9) | 93 (23.9) | 419 (20.4) | 212 (20.2) | 180 (21.0) | ||
| More than usual | 3434 (73.5) | 264 (67.9) | 1548 (75.2) | 775 (73.8) | 621 (72.5) | ||
| Feeling hopeless | |||||||
| Less than usual | 269 (5.8) | 40 (10.3) | 85 (4.1) | 74 (7.0) | 51 (6.0) | 34.25 | .06 |
| No change | 1611 (34.6) | 143 (37.0) | 729 (35.5) | 367 (35.0) | 272 (31.8) | ||
| More than usual | 2782 (59.7) | 204 (52.7) | 1239 (60.4) | 609 (58.0) | 532 (62.2) | ||
| Feeling nervous or anxious | |||||||
| Less than usual | 267 (5.7) | 32 (8.2) | 96 (4.7) | 62 (5.9) | 56 (6.5) | 40.40 | .07 |
| No change | 848 (18.1) | 100 (25.8) | 346 (16.8) | 162 (15.3) | 177 (20.6) | ||
| More than usual | 3563 (76.2) | 256 (66.0) | 1614 (78.5) | 833 (78.8) | 625 (72.8) | ||
| Unable to stop worrying | |||||||
| Less than usual | 277 (5.9) | 38 (9.8) | 107 (5.2) | 66 (6.2) | 51 (5.9) | 15.94 | .04 |
| No change | 1372 (29.3) | 116 (30.1) | 617 (30.0) | 286 (27.0) | 249 (29.0) | ||
| More than usual | 3031 (64.8) | 232 (60.1) | 1335 (64.8) | 706 (66.7) | 559 (65.1) | ||
| Frustration or boredom | |||||||
| Less than usual | 179 (3.8) | 17 (4.4) | 64 (3.1) | 53 (5.0) | 32 (3.7) | 8.34 | .03 |
| No change | 614 (13.1) | 56 (14.4) | 261 (12.7) | 135 (12.8) | 111 (12.9) | ||
| More than usual | 3886 (83.1) | 316 (81.2) | 1732 (84.2) | 868 (82.2) | 716 (83.4) | ||
| Sleep problems | |||||||
| Less than usual | 281 (6.0) | 29 (7.5) | 109 (5.3) | 64 (6.1) | 57 (6.6) | 17.32 | .05 |
| No change | 1198 (25.6) | 86 (22.3) | 569 (27.7) | 232 (22.0) | 226 (26.3) | ||
| More than usual | 3192 (68.3) | 270 (70.1) | 1377 (67.0) | 759 (71.9) | 576 (67.1) | ||
Note. Since eight chi-square tests were conducted for this category, we used Bonferroni corrections to adjust our alpha level to .006.
*p < .006.
Predictors of Worsening Mental Health
Two multiple regressions were conducted: one with Depression/Anxiety as the outcome variable and the other with the degree of mental health impact (see Tables 7 and 8). The overall model predicting Depression/Anxiety was significant, R2 and adjusted R2 = .37, F (9, 4003) = 264.19, p <.001, indicating that the predictor variables in the model accounted for 37% of the variance in worsening anxiety and depression. The overall model predicting the degree of mental health impact was also significant, R2 and adjusted R2 = .33, F (9, 4001) = 220.02, p <.001, indicating that the predictors in the model accounted for 33% of the variance in COVID-19 impact on mental health. In the first multiple regression model, four of the six predictors were unique correlates of Depression/Anxiety, including loneliness (β = 0.46), feeling your grades had been negatively impacted due to the pandemic (β = 0.12), stressful living circumstances (β = 0.14), and worry about yourself or your family contracting COVID-19 (β = 0.18). Black students also had significantly lower Depression/Anxiety scores than White Students (β = −0.03). For the second multiple regression model, all six predictor variables were unique correlates of mental health impact, namely loneliness (β = 0.29), feeling your grades had been negatively impacted due to the pandemic (β = 0.21), stressful living circumstances (β = 0.16), worry about yourself or your family contracting COVID-19 (β = 0.16), finances being impacted by COVID-19 (β = 0.08), and financial difficulties that will impact return to college in Fall 2020 (β = 0.06). Asian students reported significantly less mental health impact than White students (β = −0.04).
Table 7.
Linear Regression Predicting Mean Depression/Anxiety Symptom Score.
| B (SE) | β | p-value | |
|---|---|---|---|
| Race/Ethnicity+ | |||
| Black | −0.08 (0.04) | −0.03 | .034 |
| Latinx | −0.02 (0.03) | −0.01 | .440 |
| Asian | −0.05 (0.03) | −0.02 | .089 |
| Finances been impacted by COVID-19 | <0.01 (0.01) | 0.01 | .677 |
| Change in loneliness | 0.36 (0.01) | 0.46 | <.001 |
| Grades negatively impacted | 0.07 (0.01) | 0.12 | <.001 |
| Financial difficulties that will impact return to college in Fall 2020 | 0.02 (0.01) | 0.03 | .092 |
| Stressful current living arrangements compared to before COVID-19 | 0.13 (0.01) | 0.14 | <.001 |
| Worry that you or a family member will get COVID-19 | 0.13 (0.01) | 0.18 | <.001 |
Note. Multicollinearity was not considered an issue in the regression model as the variance inflation factor (VIF) was less than 1.5 for all predictors. +The reference group for race/ethnicity was White.
Table 8.
Linear Regression Predicting Mental Health Impact.
| B (SE) | β | p-value | |
|---|---|---|---|
| Race/Ethnicity+ | |||
| Black | −0.03 (0.06) | −0.01 | .570 |
| Latinx | 0.04 (0.04) | 0.01 | .325 |
| Asian | −0.11 (0.04) | −0.04 | .008 |
| Finances been impacted by COVID-19 | 0.08 (0.01) | 0.08 | <.001 |
| Change in loneliness | 0.35 (0.02) | 0.29 | <.001 |
| Grades negatively impacted | 0.20 (0.01) | 0.21 | <.001 |
| Financial difficulties that will impact return to college in Fall 2020 | 0.05 (0.01) | 0.06 | <.001 |
| Stressful current living arrangements compared before COVID-19 | 0.21 (0.02) | 0.16 | <.001 |
| Worry that you or a family member will get COVID-19 | 0.18 (0.02) | 0.16 | <.001 |
Note. Multicollinearity was deemed to not be an issue in the regression model as the variance inflation factor (VIF) was less than 1.5 for all predictors. +The reference group for race/ethnicity was White.
Discussion
This study examined the financial, academic, and mental health impact of COVID-19 on college students enrolled in NY and NJ universities at a time when both states were at the North American epicenter of the pandemic. Consistent with previous research, we saw alarming trends in these college students. Across the sample, the vast majority of youth were experiencing an increase in depressed mood, anxiety and worry, and frustration or boredom. In addition, 68% reported sleep problems, and 60% feeling more hopeless. This worsening in anxiety and depressive symptoms coupled with most reporting decreased connection with family and friends and increased loneliness likely places many of these emerging adults at heightened risk for mood disorders and suicidal thoughts and behaviors (Macrynikola et al., 2018; Mushtaq et al., 2014). Overall, the detrimental impact on mental health was pervasive and seemed to similarly affect students of various racial/ethnic groups.
More notable differences across racial and ethnic groups arose when examining COVID-related stressors as well as financial and academic consequences. Specifically, relative to White and Asian students, Black and Latinx students were more likely to be personally affected by COVID-19, particularly by the loss of loved ones due to the virus. In addition, Black and Latinx students reported the most consistent financial and academic consequences of the pandemic, reporting uncertainty about being able to complete current coursework and concerns about affording food and college. Our findings support what has been repeatedly reported across news outlets and by the Centers for Disease Control and Prevention, specifically that individuals from communities of color have been disproportionately affected by the pandemic with increased risk of contracting and dying from COVID-19 (American Public Media [APM] Research Lab, 2020; Centers for Disease Control and Prevention [CDC], 2020; Kantamneni, 2020; Webb Hooper et al., 2020). COVID-19 has further exposed long-standing racial and ethnic disparities in health care access and quality. Due to social determinants of health (Braveman et al., 2011), racially/ethnically minoritized people have higher rates of underlying health conditions, such as diabetes, asthma, and obesity (National Center for Health Statistics, 2016), tend to live in more crowded households and lower SES neighborhoods (Ogedegbe et al., 2020), and comprise the majority of essential workers (e.g., grocery stores and public transportation) who do not have the luxury of working from home, receiving paid sick days, or social distancing (Maxwell, 2020; Rogers et al., 2020; Yancy, 2020).
Possibly more specific to this sample of college students were the racial/ethnic group differences in academic-related outcomes, and the substantial rates of Black and Latinx students reporting that they were unable to successfully complete their coursework (about 20%) and were markedly worried that they would be unable to afford to return to college (about 30%). Unfortunately, in the United States, race and ethnicity intertwine with many societal and economic disadvantages. Thus, socioeconomic status (SES) may partly explain the inequitable impact of the pandemic. As our survey did not include direct measurement of SES, we were not able to test this hypothesis explicitly. However, we did include two proxy SES variables, first-generation college status (58% Latinx, 45% Black, 39% Asian, and 23% White) and receiving financial aid (72% Black, 67% Latinx, 53% Asian, and 47% White) with noticeable racial/ethnic differences. Additionally, racially/ethnically minoritized individuals experience discrimination, implicit bias, and structural racism that increase risk of poor health and academic outcomes (Bailey et al., 2017; Hall et al., 2015; Logan & Burdick-Will, 2016). The pandemic seems to have disproportionately impacted those that were already most vulnerable to systemic inequities and has the potential to further widen disparities in education, income, and social mobility for generations to come.
There were surprisingly few racial/ethnic group differences with regard to changes in mental health symptoms, with all groups doing poorly overall. The only significant difference was that Black students had lower mean Depression/Anxiety scores than White students. Although higher for Black and Latinx participants, White and Asian students also reported considerable and concerning levels of financial stress and loss of loved ones due to COVID-19. The pandemic has clearly been a time of adversity for all college students with implications for their immediate mental health. Additionally, it is likely that we have not yet seen the full extent of the aftermath of the COVID-19 pandemic for Asian students. Although Asians were equivalent to Whites regarding COVID-19 related stressors and degree of financial impact, they indicated more worry about affording food and being able to return to college. There has also been an alarming rise in discrimination and assaults directed at Asian individuals and businesses in the current pandemic (Chen et al., 2020). The majority of anti-Asian incidents have occurred in grocery stores, local businesses, and public places (Jeung & Nham, 2020), likely escalating Asian individuals’ fear and uncertainty about their well-being and future. Future long-term research in Asian populations on discrimination and its relation to employment, academic outcomes, and mental health will be crucial.
For the entire sample, four variables emerged as significant unique correlates of deteriorating mental health across both criterion variables in our regression models. They were current stressful living arrangements, grades being negatively impacted, worry about self or family getting COVID-19, and loneliness. Although this is an emerging area of research, the level of consistency between ours and previous results is striking. Liu et al. (2020) also found loneliness and worries about COVID-19 to be predictive of clinical levels of depression, anxiety, and PTSD symptoms, and Hamza et al. (2020) highlighted the importance of social isolation. These findings suggest that interventions aimed at decreasing loneliness while practicing social distancing, such as key personnel at universities regularly checking in with students, having university virtual events, or possibly providing safe ways to connect in-person in small groups, may be essential. In addition, education about COVID-19 and recommended and reasonable precautions to prevent infection as well as addressing overly exaggerated or catastrophic predictions about the disease may help lessen anxiety and worry. Of note, current financial difficulties (finances impacted by COVID-19, financial difficulties affecting return to college) were associated with general mental health status but not self-reported depression/anxiety, despite a large number of students worried about current and future financial prospects.
Regarding living situations, most students (83%) reported currently living with parents, which was a change from independent living for about 43%. Prior studies have indicated that family support may protect against internalizing symptoms (Liu et al., 2020; Sundarasen et al., 2020), and conversely, our finding suggests that stressful family environments may contribute to deteriorating mental health. The adjustment surrounding moving from living independently back into a parental home may have added stress to the situation. However, we did not specifically evaluate the quality of the family environment or perceived parental support. Research has shown an increase in family violence and volatile situations during the pandemic (Peterman et al., 2020; van Gelder et al., 2020), which can be heightened by other stressors including economic challenges and social isolation (Usher et al., 2020). Given that these are central features of the current pandemic, this area certainly warrants further attention.
Finally, the more COVID-19 negatively impacted students’ grades the more likely they were to report worsening mental health symptoms. College students faced many challenges during the NY and NJ stay-at-home orders including relocating, lack of social connection, loneliness, as well as loss of employment, COVID-19 infection, and death of loved ones. Most colleges quickly transitioned to virtual platforms with minimal preparation or training of instructors. Students had limited face time with professors and grading options were uncertain. Such factors may have negatively affected some students’ performance and added to the overwhelming nature of the situation. It will be important to continue to examine the impact of COVID-19 on students’ grades and the link between grades and mental health symptoms as the pandemic progresses and post-pandemic. Most colleges and universities in the U.S. continued online instruction in the Fall with presumably more rigorous online and hybrid courses to help facilitate student learning and academic success.
Given the unprecedented circumstances created by the pandemic, the hallmark transitions of emerging adulthood may have been altered or slowed for some students. In line with a risk and resilience perspective (Garmezy et al., 1984), it will be essential to understand what factors promote positive adaptation in the face of this adversity (Masten et al., 1990). Cultural protective factors, such as familism, extended family and kinship networks, religious support, and spirituality, have been shown to buffer against the impact of stress (e.g., discrimination and acculturation) on mental health outcomes among Black and Latinx populations (Boyd-Franklin, 2013; Corona et al., 2017; Hope et al., 2017; Valdivieso-Mora et al., 2016). These protective factors and others (e.g., relationship with parents and siblings) may be particularly potent and relevant in supporting recovery following the pandemic and should be studied further.
Limitations
Although this study has several strengths including the diversity of the sample and its region and timing of assessment, it is cross-sectional, based solely on self-report, and descriptive in nature. The cross-sectional design limits our ability to make inferences regarding causality or the temporal ordering of variables. For instance, changes in depression and anxiety may have preceded exposure to the predictor variables examined. It will be important to assess these relationships across time. The use of self-report assessment is also limited in that participants may have misinterpreted questions or responded in a socially desirable manner. We developed the survey for the purpose of the study questions; it is not a validated measure with known psychometric properties and we did not use standardized mental health assessments. In addition, common method bias in survey items may inflate observed relationships, and thus, it will be important for future research to employ multi-method assessment. For instance, future research could investigate the degree of the relationships between reported stressors in college students and mental health assessments made by trained clinicians. This line of research would strengthen the current findings as well test their generalizability. Given that Indigenous individuals have also been disproportionately impacted by COVID-infection and death (APM Research Group, 2020; Maxwell, 2020), it is a limitation that they are not better represented in our sample. The majority of participants were female, possibly limiting generalizability to males. Finally, most participants were attending four year institutions, and thus results may not generalize to students at community colleges.
Conclusions
Despite these limitations, the current study clearly documents the considerable mental health impact of the pandemic on a large sample of diverse, Northeastern college students. Emerging adulthood is a critical time to acquire the skills needed for a successful transition to adulthood. The increase in depression and anxiety symptoms due to COVID-19 may interfere with college students’ ability to meet important developmental milestones, such as completing post-secondary education and obtaining employment, as well as elevating risk of developing more serious mental illness and suicidal thoughts and behavior. COVID-19’s mental health impact on college students is alarming and highlights the need for public health interventions at the university level. Similar to findings in adults regarding the disproportionate impact of COVID-19 on racial and ethnic minorities (CDC, 2020; Rogers et al., 2020; Yancy, 2020), our study demonstrated parallel results in college students. Black and Latinx students experienced greater COVID-related, financial, and academic hardships likely stemming from systemic inequities that existed before the pandemic. It will be crucial for universities to develop programs and interventions to protect their most vulnerable students and prevent the pandemic from further increasing racial and ethnic differences in social and economic disparities.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Carrie Masia Warner https://orcid.org/0000-0002-1920-6557
Emily A. Kline https://orcid.org/0000-0002-6633-1916
Erum Nadeem https://orcid.org/0000-0001-9133-9955
References
- American Public Media [APM] Research Lab (2020). The color of coronavirus: COVID-19 deaths by race and ethnicity in the U.S. https://www.apmresearchlab.org/covid/deaths-by-race [Google Scholar]
- Arnett J. J. (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist, 55(5), 469–480. 10.1037/0003-066X.55.5.469. [DOI] [PubMed] [Google Scholar]
- Arnett J. J. (2016). College students as emerging adults: The developmental implications of the college context. Emerging Adulthood, 4(3), 219–222. 10.1177/2167696815587422 [DOI] [Google Scholar]
- Bailey Z. D., Krieger N., Agénor M., Graves J., Linos N., Bassett M. T. (2017). Structural racism and health inequities in the USA: evidence and interventions. The Lancet, 389(10077), 1453–1463. 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- Beiter R., Nash R., McCrady M., Rhoades D., Linscomb M., Clarahan M., Sammut S. (2015). The prevalence and correlates of depression, anxiety, and stress in a sample of college students. Journal of Affective Disorders, 173, 90-96. 10.1016/j.jad.2014.10.054. [DOI] [PubMed] [Google Scholar]
- Birmingham W. C., Wadsworth L. L., Lassetter J. H., Graff T. C., Lauren E., Hung M. (2021). COVID-19 lockdown: Impact on college students’ lives. Journal of American College Health. Advance online publication 10.1080/07448481.2021.1909041 [DOI] [PubMed]
- Boyd-Franklin N. (2013). Black families in therapy: Understanding the African American experience. Guilford Publications. [Google Scholar]
- Braveman P., Egerter S., Williams D. R. (2011). The social determinants of health: Coming of age. Annual Review of Public Health, 32(1), 381–398. 10.1146/annurev-publhealth-031210-101218 [DOI] [PubMed] [Google Scholar]
- Byrd D. R., McKinney K. J. (2012). Individual, interpersonal, and institutional level factors associated with the mental health of college students. Journal of American College Health, 60(3), 185–193. 10.1080/07448481.2011.584334 [DOI] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. (2020). The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research, 287, 112934. 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [CDC] (2020). COVID-19 Hospitalization and Death by race/ethnicity. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html#footnote03 [Google Scholar]
- Chen J. A., Stevens C., Wong S. H. M., Liu C. H. (2019). Psychiatric symptoms and diagnoses among US college students: A comparison by race and ethnicity. Psychiatric Services, 70(6), 442–449. 10.1176/appi.ps.201800388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J. A., Zhang E., Liu C. H. (2020). Potential impact of COVID-19-related racial discrimination on the health of Asian Americans. American Journal of Public Health, 110(11), 1624–1627. 10.2105/AJPH.2020.305858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clabaugh A., Duque J. F., Fields L. J. (2021). Academic stress and emotional well-being in united states college students following onset of the COVID-19 pandemic. Frontiers in Psychology, 12, 628787. 10.3389/fpsyg.2021.628787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. (1988). Statistical power analysis for the behavioural sciences (2nd edn). L. Erlbaum Associates. [Google Scholar]
- Conrad R., Rayala H., Menon M., Vora K. (2020). Universities’ response to supporting mental health of college students during the COVID-19 pandemic. Psychiatric Times. https://www.psychiatrictimes.com/view/universities-response-supporting-mental-health-college-students-during-covid-19-pandemic [Google Scholar]
- Cornish P. A., Berry G., Benton S., Barros-Gomes P., Johnson D., Ginsburg R., Whelan B., Fawcett E., Romano V. (2017). Meeting the mental health needs of today’s college student: Reinventing services through Stepped Care 2.0. Psychological Services, 14(4), 428-442. 10.1037/ser0000158. [DOI] [PubMed] [Google Scholar]
- Corona R., Rodríguez V. M., McDonald S. E., Velazquez E., Rodríguez A., Fuentes V. E. (2017). Associations between cultural stressors, cultural values, and Latina/o college students’ mental health. Journal of Youth and Adolescence, 46(1), 63–77. 10.1007/s10964-016-0600-5 [DOI] [PubMed] [Google Scholar]
- D’Amato P. (2020). Coronavirus accelerates higher education’s trend toward distance learning. The Hechinger Report. https://hechingerreport.org/coronavirus-accelerates-higher-educations-trend-toward-distance-learning/
- de Brey C., Musu L., McFarland J., Wilkinson-Flicker S., Diliberti M., Zhang A., Branstetter C., Wang X. (2019). Status and Trends in the Education of Racial and Ethnic Groups 2018 (NCES 2019-038). Washington DC: National Center for Education Statistics: U.S. Department of Education. https://nces.ed.gov/pubsearch/. [Google Scholar]
- Eisenberg D., Hunt J., Speer N. (2013). Mental health in American colleges and universities: Variation across student subgroups and across campuses. The Journal of Nervous and Mental Disease, 201(1), 60–67. 10.1097/NMD.0b013e31827ab077 [DOI] [PubMed] [Google Scholar]
- Ferguson C. J. (2009). An effect size primer: a guide for clinicians and researchers. Professional Psychology: Research and Practice, 40(5), 532–538. 10.1037/a0015808 [DOI] [Google Scholar]
- Fruehwirth J. C., Biswas S., Perreira K. M. (2021). The Covid-19 pandemic and mental health of first-year college students: Examining the effect of Covid-19 stressors using longitudinal data. Plos One, 16(3), e0247999. 10.1371/journal.pone.0247999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garmezy N., Masten A. S., Tellegen A. (1984). The study of stress and competence in children: A building block for developmental psychopathology. Child Development, 55(1), 97–111. 10.2307/1129837 [DOI] [PubMed] [Google Scholar]
- Hall W. J., Chapman M. V., Lee K. M., Merino Y. M., Thomas T. W., Payne B. K., Eng E., Day S. H., Coyne-Beasley T. (2015). Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: A systematic review. American Journal of Public Health, 105(12), e60–e76. 10.2105/AJPH.2015.302903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamza C. A., Ewing L., Heath N. L., Goldstein A. L. (2020). When social isolation is nothing new: A longitudinal study psychological distress during COVID-19 among university students with and without preexisting mental health concerns. Canadian Psychology/Psychologie Canadienne, 62(1), 20–30. 10.1037/cap0000255 [DOI] [Google Scholar]
- Hankerson S. H., Fenton M. C., Geier T. J., Keyes K. M., Weissman M. M., Hasin D. S. (2011). Racial differences in symptoms, comorbidity, and treatment for major depressive disorder among black and white adults. Journal of the National Medical Association, 103(7), 576–584. 10.1016/s0027-9684(15)30383-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjorth C. F., Bilgrav L., Frandsen L. S., Overgaard C., Torp-Pedersen C., Nielsen B., Bøggild H. (2016). Mental health and school dropout across educational levels and genders: A 4.8-year follow-up study. BMC Public Health, 16, 976. 10.1186/s12889-016-3622-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E. A., O'Connor R. C., Perry V. H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A. K., Shafran R., Sweeney A., Bullmore E. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hope M. O., Assari S., Cole-Lewis Y. C., Caldwell C. H. (2017). Religious social support, discrimination, and psychiatric disorders among Black adolescents. Race and Social Problems, 9(2), 102-114. 10.1007/s12552-016-9192-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huckins J. F., daSilva A. W., Wang W., Hedlund E., Rogers C., Nepal S. K., Wu J., Obuchi M., Murphy E. I., Meyer M. L., Wagner D. D., Holtzheimer P. E., Campbell A. T. (2020). Mental health and behavior of college students during the early phases of the COVID-19 pandemic: Longitudinal smartphone and ecological momentary assessment study. Journal of Medical Internet Research, 22(6), e20185. 10.2196/20185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam M. A., Barna S. D., Raihan H., Khan M. N. A., Hossain M. T. (2020). Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: A web-based cross-sectional survey. Plos One, 15(8), e0238162. 10.1371/journal.pone.0238162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeung R., Nham K. (2020). Incidents of coronavirus-related discrimination. Asian Pacific Policy and Planning Council. http://www.asianpacificpolicyandplanningcouncil.org/wp-content/uploads/STOP_AAPI_HATE_MONTHLY_REPORT_4_23_20.pdf. [Google Scholar]
- Kantamneni N. (2020). The impact of the COVID-19 pandemic on marginalized populations in the United States: A research agenda. Journal of Vocational Behavior, 119, 103439. 10.1016/j.jvb.2020.103439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kecojevic A., Basch C. H., Sullivan M., Davi N. K. (2020). The impact of the COVID-19 epidemic on mental health of undergraduate students in New Jersey, cross-sectional study. Plos One, 15(9), e0239696. 10.1371/journal.pone.0239696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kern A., Hong V., Song J., Lipson S. K., Eisenberg D. (2018). Mental health apps in a college setting: Openness, usage, and attitudes. Mhealth, 4, 20. 10.21037/mhealth.2018.06.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R. C., Angermeyer M., Anthony J. C., De Graaf R., Demyttenaere K., Gasquet I., DE Girolamo G., Gluzman S., Gureje O., Haro J. M., Kawakami N., Karam A., Levinson D., Medina Mora M. E., Oakley Browne M. A., Posada-Villa J., Stein D. J., Adley Tsang C. H., Aguilar-Gaxiola S., Ustün T. B. (2007). Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization's World Mental Health Survey Initiative. World Psychiatry, 6(3), 168–176. [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R. L., Williams J. B., Löwe B. (2009). An ultra-brief screening scale for anxiety and depression: The PHQ–4. Psychosomatics, 50(6), 613–621. 10.1016/S0033-3182(09)70864-3 [DOI] [PubMed] [Google Scholar]
- Lechner W. V., Laurene K. R., Patel S., Anderson M., Grega C., Kenne D. R. (2020). Changes in alcohol use as a function of psychological distress and social support following COVID-19 related university closings. Addictive Behaviors, 110, 106527. 10.1016/j.addbeh.2020.106527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lederer A. M., Hoban M. T., Lipson S. K., Zhou S., Eisenberg D. (2021). More than inconvenienced: the unique needs of US college students during the CoViD-19 pandemic. Health Education & Behavior, 48(1), 14–19. 10.1177/1090198120969372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipson S. K., Lattie E. G., Eisenberg D. (2019). Increased rates of mental health service utilization by US college students: 10-year population-level trends (2007–2017). Psychiatric Services, 70(1), 60–63. 10.1176/appi.ps.201800332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C. H., Stevens C., Wong S. H. M., Yasui M., Chen J. A. (2019). The prevalence and predictors of mental health diagnoses and suicide among US college students: Implications for addressing disparities in service use. Depression and Anxiety, 36(1), 8–17. 10.1002/da.22830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C. H., Zhang E., Wong G. T. F., Hyun S., Hahm H. C. (2020). Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Research, 290, 113172. 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan J. R., Burdick-Will J. (2016). School segregation, charter schools, and access to quality education. Journal of Urban Affairs, 38(3), 323–343. 10.1111/juaf.12246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macrynikola N., Miranda R., Soffer A. (2018). Social connectedness, stressful life events, and self-injurious thoughts and behaviors among young adults. Comprehensive Psychiatry, 80, 140-149. 10.1016/j.comppsych.2017.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masia Warner C., Reyes-Portillo J. A., Chu B., Miranda R., Nadeem E., Nickerson A., Ortin Peralta A., Reigada L., Rizvi S. L., Roy A. K., Shatkin J. (2020). COVID-19 Impact College Workshop Survey (available from Carrie Masia Warner, masiac@montclair.edu, and Jazmin Reyes-Portillo, reyesportilj@montclair.edu).
- Masten A. S., Best K. M., Garmezy N. (1990). Resilience and development: Contributions from the study of children who overcome adversity. Development and Psychopathology, 2(4), 425–444. 10.1017/S0954579400005812 [DOI] [Google Scholar]
- Matthews T., Danese A., Wertz J., Odgers C. L., Ambler A., Moffitt T. E., Arseneault L. (2016). Social isolation, loneliness and depression in young adulthood: a behavioural genetic analysis. Social Psychiatry and Psychiatric Epidemiology, 51(3), 339–348. 10.1007/s00127-016-1178-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell C. (2020). Coronavirus compounds inequality and endangers communities of color. Center for American Progress. https://www.americanprogress.org/issues/race/news/2020/03/27/482337/coronavirus-compounds-inequality-endangers-communities-color/ [Google Scholar]
- Mushtaq R., Shoib S., Shah T., Mushtaq S. (2014). Relationship between loneliness, psychiatric disorders and physical health? A review on the psychological aspects of loneliness. Journal of Clinical and Diagnostic Research, 8(9), WE01-WE04. 10.7860/JCDR/2014/10077.4828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Education Statistics (2021). Number and percentage of students enrolled in degree-granting postsecondary institutions, by distance education participation, location of student, level of enrollment, and control and level of institution: Fall 2018 and Fall 2019. https://nces.ed.gov/programs/digest/d20/tables/dt20_311.15.asp [Google Scholar]
- National Center for Health Statistics (2016). Health, United States, 2015: With special feature on racial and ethnic health disparities. National Center for Health Statistics (US). Report No.: 2016-1232. PMID: 27308685http://www.cdc.gov/nchs/hus.htm [PubMed] [Google Scholar]
- National Student Clearinghouse Research Center (2020). Term enrollment estimates: Fall 2020. https://nscresearchcenter.org/wp-content/uploads/CTEE_Report_Fall_2020.pdf [Google Scholar]
- Ogedegbe G., Ravenell J., Adhikari S., Butler M., Cook T., Francois F., Iturrate E., Jean-Louis G., Jones S. A., Onakomaiya D., Petrilli C. M., Pulgarin C., Regan S., Reynolds H., Seixas A., Volpicelli F. M., Horwitz L. I. (2020). Assessment of racial/ethnic disparities in hospitalization and mortality in patients with COVID-19 in New York city. JAMA Network Open, 3(12), e2026881. 10.1001/jamanetworkopen.2020.26881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okruszek Ł., Aniszewska-Stańczuk A., Piejka A., Wiśniewska M., Żurek K. (2020). Safe but lonely? Loneliness, anxiety, and depression symptoms and COVID-19. Frontiers in Psychology, 11, 3222. 10.3389/fpsyg.2020.579181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterman A., Potts A., O’Donnell M., Thompson K., Shah N., Oertelt-Prigione S., van Gelder N. (2020). Pandemics and violence against women and children (Working Paper No. 528). Washington DC: Center for Global Development. https://www.cgdev.org/publication/pandemics-and-violence-against-women-and-children. [Google Scholar]
- Rogers T. N., Rogers C. R., VanSant-Webb E., Gu L. Y., Yan B., Qeadan F. (2020). Racial disparities in COVID-19 mortality among essential workers in the United States. World Medical & Health Policy, 12(3), 311-327. 10.1002/wmh3.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudenstine S, McNeal K, Schulder T, Ettman CK, Hernandez M, Gvozdieva K, Galea S. (2021). Depression and anxiety during the COVID-19 pandemic in an urban, low-income public university sample. Journal of Traumatic Stress, 34(1), 12–22. 10.1002/jts.22600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz S. J. (2016). Turning point for a turning point: Advancing emerging adulthood theory and research. Emerging Adulthood, 4(5), 307–317. 10.1177/2167696815624640. [DOI] [Google Scholar]
- Shapiro D., Dundar A., Huie F., Wakhungu P., Yuan X., Nathan A, Hwang Y. A. (2017). A national view of student attainment rates by race and ethnicity – Fall 2010 cohort (signature report No. 12b). National Student Clearinghouse Research Center. https://nscresearchcenter.org/wp-content/uploads/SignatureReport12.pdf [Google Scholar]
- Singu S., Acharya A., Challagundla K., Byrareddy S. N. (2020). Impact of social determinants of health on the emerging COVID-19 pandemic in the United States. Frontiers in Public Health, 8, 406. 10.3389/fpubh.2020.00406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slominski L., Sameroff A., Rosenblum K., Kasser T. (2011). Longitudinal predictors of adult socioeconomic attainment: The roles of socioeconomic status, academic competence, and mental health. Development and Psychopathology, 23(1), 315–324. 10.1017/S0954579410000829 [DOI] [PubMed] [Google Scholar]
- Son C., Hegde S., Smith A., Wang X., Sasangohar F. (2020). Effects of COVID-19 on college students’ mental health in the United States: Interview survey study. Journal of Medical Internet Research, 22(9), e21279. 10.2196/21279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- St Amour M. (2021). Survey: Pandemic negatively affected grades this Fall. Inside Higher Ed. https://www.insidehighered.com/quicktakes/2021/01/05/survey-pandemic-negatively-affected-grades-fall. [Google Scholar]
- Sundarasen S., Chinna K., Kamaludin K., Nurunnabi M., Baloch G. M., Khoshaim H. B., Hossain S. F. A., Sukayt A. (2020). Psychological impact of COVID-19 and lockdown among university students in malaysia: implications and policy recommendations. International Journal of Environmental Research and Public Health, 17(17), 6206. 10.3390/ijerph17176206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syed M., Azmitia M. (2009). Longitudinal trajectories of ethnic identity during the college years. Journal of Research on Adolescence, 19(4), 601-624. 10.1111/j.1532-7795.2009.00609.x. [DOI] [Google Scholar]
- The Atlantic Monthly Group (2020). The COVID-19 tracking project. https://covidtracking.com/ [Google Scholar]
- U.S. Department of Education’s Office for Civil Rights [OCR] (2021). Education in a pandemic: The disparate impacts of COVID-19 on America’s students. https://www2.ed.gov/about/offices/list/ocr/docs/20210608-impacts-of-covid19.pdf [Google Scholar]
- Usher K., Bhullar N., Durkin J., Gyamfi N., Jackson D. (2020). Family violence and COVID-19: Increased vulnerability and reduced options for support. International Journal of Mental Health Nursing, 29(4), 549–552. 10.1111/inm.12735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valdivieso-Mora E., Peet C. L., Garnier-Villarreal M., Salazar-Villanea M., Johnson D. K. (2016). A systematic review of the relationship between familism and mental health outcomes in latino population. Frontiers in Psychology, 7, 1632. 10.3389/fpsyg.2016.01632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Gelder N., Peterman A., Potts A., O’Donnell M., Thompson K., Shah N., Oertelt-Prigione S. (2020). COVID-19: Reducing the risk of infection might increase the risk of intimate partner violence. EClinicalMedicine, 21, 100348. 10.1016/j.eclinm.2020.100348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velez E. D., Lew T., Thomsen E., Johnson K., Wine J., Cooney J., Socha T. (2019). Baccalaureate and Beyond (B&B:16/17): A first look at the employment and educational experiences of college graduates, 1 year later. U.S. Department of Education, National 194 Center for Education Statistics. https://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2019241
- Wang Z. H., Yang H. L., Yang Y. Q., Liu D., Li Z. H., Zhang X. R., Zhang Y. J., Shen D., Chen P. L., Song W. Q., Wang X. M., Wu X. B., Yang X. F., Mao C. (2020). Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: A large cross-sectional study. Journal of Affective Disorders, 275, 188-193. 10.1016/j.jad.2020.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb Hooper M., Nápoles A. M., Pérez-Stable E. J. (2020). COVID-19 and racial/ethnic disparities. JAMA, 323(24), 2466–2467. 10.1001/jama.2020.8598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yancy C. W. (2020). COVID-19 and African Americans. JAMA, 323(19), 1891–1892. https://doi:10.1001/jama.2020.6548 [DOI] [PubMed] [Google Scholar]