Abstract
Elderly and patients with comorbid conditions have higher risk of infection and complications. Vaccination hesitancy is defined as the refusal of vaccine or the delay in accepting it despite the availability of vaccines and vaccination services. This study was aimed at assessing knowledge, perception, and acceptability of healthcare staff towards different types of COVID-19 vaccination. A multicenter hospital-based descriptive cross-sectional study was implemented to study the knowledge, perception, and acceptability of healthcare staff towards COVID-19 vaccination. Multistage sampling technique was applied. Data were collected through a self-administered questionnaire filled by the participants. 400 participants were studied. 61% of the participants were females, and the most frequent age reported was between 18 and 35 years (67%). A statistically significant association (p = 0.048) was found between knowledge about vaccination and professions. The most common vaccine type known and accepted was AstraZeneca vaccine. On assessing acceptability of COVID-19 vaccination, acceptance rate was high (63.8%) and 22.7% of the participants had already got vaccinated. The rejection rate among our staff was 27.4%. This study was conducted in April, 2021. Majority of our healthcare staff believed that vaccination is the key to combat the pandemic. One of the issues and concerns about vaccination was the safety and the risk of developing acute adverse events (p = 0.001). Encouraging factor for vaccination was the fear of getting infection themselves and their families. The present study revealed the presence of good knowledge and acceptability among medical staff towards COVID-19 vaccinations in Sudan.
1. Introduction
COVID-19 infection can cause fatal pneumonia. Elderly and patients with comorbid conditions have a higher risk of infection and complications, such as acute respiratory distress syndrome (ARDS) and cytokine storm [1–3].
There are many types of vaccines. Whole virus vaccines contain viruses whose genetic material has been destroyed by heat, chemicals, or radiation. These whole virus vaccines can be either live attenuated or inactivated. Another type of vaccine is the subunit vaccine, containing purified pieces of the virus selected specially for their ability to stimulate immune cells. Only protein subunit vaccines are being developed against the virus that causes COVID-19. Nucleic acid vaccines use the genetic materials of the pathogen to stimulate the immune response [3]. In the case of COVID-19, spike proteins of the surface of the virus interact with human cells to trigger an immune response. After the infection, the body keeps a few T-lymphocytes, called memory cells, that go into quick action upon reinfection [4–6]. Current types of COVID-19 vaccines are mRNA vaccines, protein subunit vaccines, and vector vaccines [4–6].
Vaccination is considered as one of the most effective methods for controlling infectious diseases [7]. Moreover, the vaccination programs contributed remarkably in the reduction of morbidity and mortality of many infectious diseases. Despite this, the success of vaccination faces challenges from groups and individuals who delay or refuse vaccination [8, 9]. Vaccination hesitancy is defined as the refusal of vaccine or the delay in accepting it despite the availability of vaccines and vaccination services [10]. Thus, encouragement by policy makers should be implemented to increase the vaccination willingness [11].
In Sudan, as of Jan. 2022, 13th, the number of suspected cases was 93,390 and 50,621 confirmed cases of COVID-19 reported to the Federal Ministry of Health [12]. COVID-19 detection at community level program was developed by the FMOH. This program was called “Syndromic Approach.” In this program, community volunteers detect and report COVID-19 cases, each volunteer was responsible for 150 households, and the volunteer had 50 visits per day and conducted second rounds every 3 days. Each 40-50 volunteers were supervised by a rapid response team that decides whether the infected populations need home isolation or hospital isolation. On the other hand, the vaccination status as per the reports of the Federal Ministry of Health (FMOH) was published in the official website (http://sho.gov.sd/corona/). Khartoum state was the first state to get the vaccination services. The vaccination program firstly targeted the elderly (>60 years) and the healthcare workers. Between the period of 28th of March and 5th of April, 34806 elderly populations (>60 years) were vaccinated and among healthcare workers, 23266 were vaccinated. This study was aimed at assessing knowledge, perception, and acceptability of healthcare staff towards different types of COVID-19 vaccination.
2. Methods
A multicenter hospital-based descriptive cross-sectional study was implemented to study the knowledge, perception, and acceptability of healthcare staff towards COVID-19 vaccination. The study assessed the characteristics of healthcare staff who worked at governmental hospitals in Khartoum state, as well as their acceptability to take COVID-19 vaccination. Based on the reports of the Federal Ministry of Health in Sudan (http://sho.gov.sd/corona/), vaccination centers were installed in Khartoum state targeting, at first level, the healthcare workers and elder population. Khartoum state is the capital of Sudan located at LAT 15.46414700 and LON 32.47161300. It is the most populated state in Sudan and has more advanced healthcare services than other states.
A multistage sampling technique was applied to select the participants. At first level, 8 tertiary governmental hospitals in Khartoum state were randomly included in the study. All were multispecialty hospitals located in Khartoum state. Ibn Sina Hospital, Ibrahim Malik Hospital, Khartoum Hospital, Soba University Hospital, Haj Elmardi Mohieldin Teaching Hospital, Bashair University Hospital, Alturkey Hospital, and Alribat University Hospital were included in the study. At second level, stratified random sampling technique was used to select healthcare staff working in the governmental hospitals based on the size of each hospital; the selection from the different hospitals corresponded to the percentage contributed by the hospital to the population using the formula of sample size estimation for each stratum (hospital) was n = N/1 + Nd2, where n is the estimated sample size, N is the total number of patients records, and d is the degree of accuracy set at 0.05. The total sample size collected from all 8 hospitals with respect to the size of each hospital was 400 healthcare workers of different professions. Data were collected through a self-administered questionnaire filled by the participants on-site after getting their approval through informed consents. This tool was developed by two co-authors and validated by a research specialist prior to data collection. The response rate to this self-administered questionnaire was 100% with no dropouts, yet some of the questions were not answered by all participants (detailed in the tables). All the questions were closed questions, either straight forward questions (for the demographic characteristics) or check list (for knowledge and perception). The Statistical Package for Social Sciences (SPSS version 23) was used to describe and analyze the data. Chi-square test was done to assess the differences between variables; it was considered statistically significant when p ≤ 0.05. Confidentiality of participants was assured through the use of an anonymous research tool with no identifiers. Ethical approval from the Ministry of Health was granted firstly; then, approval from each hospital administration was granted. The collected data were used strictly for the purpose of the study objectives. This study was conducted in April, 2021. The data were collected in a 2-month period covering all the study area and population. This study was done in Khartoum state because at the time of the study, Khartoum state was the first state that started the vaccination services. Other states had started after this state.
3. Results
3.1. Characteristics of the Study Participants
Four hundred participants from different governmental hospitals were assessed in our study; all healthcare workers in the facility were included. 61% of the participants were females, and the most frequent age reported was between 18 and 35 years (67%); only 2% were aged above 55 years. Regarding their professions, physicians and nurses were the majority (31% and 28%, respectively), 15% were pharmacists, while other professions are mentioned in Table 1. Chronic conditions of the participants are described in Table 1. 84.5% had no chronic condition. With regard to their general vaccination status, 30% of our participants had received vaccination of any type during the year of 2020.
Table 1.
Characteristics of the study participants (n = 400).
| Characteristics | n | % | Characteristics | n | % |
|---|---|---|---|---|---|
| Gender | Chronic conditions | ||||
| Male | 156 | 39 | None | 338 | 84.5 |
| Female | 244 | 61 | Cardiovascular conditions (HTN, heart disease) | 14 | 3.5 |
| Age | Diabetes mellitus | 18 | 4.5 | ||
| 18-35 years | 268 | 67 | Asthma, COPD | 10 | 2.5 |
| 36-55 years | 124 | 31 | Others | 20 | 5 |
| >55 years | 8 | 2 | Any vaccination taken last year | ||
| Professions | Yes | 120 | 30 | ||
| Physician | 124 | 31 | No | 280 | 70 |
| Pharmacist | 60 | 15 | |||
| Nurse | 112 | 28 | |||
| Lab technician | 71 | 17.8 | |||
| Administrator | 19 | 4.8 | |||
| Others | 14 | 3.5 |
3.2. Assessment of Knowledge of Participants about COVID-19 Vaccination Based on Their Professions
Based on the different professions of the participants, their knowledge was assessed based on their professions. 365 participants have reported their knowledge about COVID-19 vaccines. From the participants who were aware of COVID-19 vaccination, 47.7% were nurses and technicians, while doctors were 35.7%, and pharmacists were only 16.5%. A statistically significant association (p = 0.048) was found between knowledge about vaccination and professions.
Regarding knowledge of participants about vaccination safety and number of vaccine shots, 359 and 367 participants have replied. No statistically significant difference in knowledge was found among the different professions (p = 0.404 and 0.152, respectively). Table 2 illustrates the details.
Table 2.
Assessment of knowledge of participants about COVID-19 vaccination based on their professions.
| Professions | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Knowledge | Doctors | % | Pharmacists | % | Nurses/technicians | % | Total | % | p value |
| Are you aware of COVID-19 vaccines | |||||||||
| Yes | 119 | 35.7 | 55 | 16.5 | 159 | 47.7 | 333 | 91.2 | 0.048∗ |
| No | 5 | 15.6 | 5 | 15.6 | 22 | 68.8 | 32 | 8.8 | |
| Total | 124 | 34.0 | 60 | 16.4 | 181 | 49.6 | 365 | 100.0 | |
| COVID-19 vaccines safety | |||||||||
| Not safe | 71 | 37.0 | 28 | 14.6 | 93 | 48.4 | 192 | 53.5 | 0.404 |
| Safe | 52 | 31.1 | 31 | 18.6 | 84 | 50.3 | 167 | 46.5 | |
| Total | 123 | 34.3 | 59 | 16.4 | 177 | 49.3 | 359 | 100.0 | |
| Number of vaccines shots | |||||||||
| One shot | 12 | 31.6 | 6 | 15.8 | 20 | 52.6 | 38 | 10.4 | 0.152 |
| Two shots | 104 | 35.3 | 52 | 17.6 | 139 | 47.1 | 295 | 80.4 | |
| More than two shots | 7 | 25.9 | 2 | 7.4 | 18 | 66.7 | 27 | 7.4 | |
| Do not know | 1 | 14.3 | 0 | 0.0 | 6 | 85.7 | 7 | 1.9 | |
| Total | 124 | 33.8 | 93 | 25.3 | 183 | 49.9 | 367 | 100.0 | |
∗Statistically significant.
3.3. Sources of Information about COVID-19 Vaccination as Reported by Participants
Participants were asked to report the sources of their knowledge about COVID-19 vaccination. The most frequently reported sources of information were the social media and the hospital announcement, reported by 47.5% and 45.3% of the participants, respectively, followed by the national media as TV and radio (42.3%). 33.8% of the participants had their knowledge from scientific websites, while 17.5% of the participants had their knowledge from official statements and press release (Figure 1).
Figure 1.
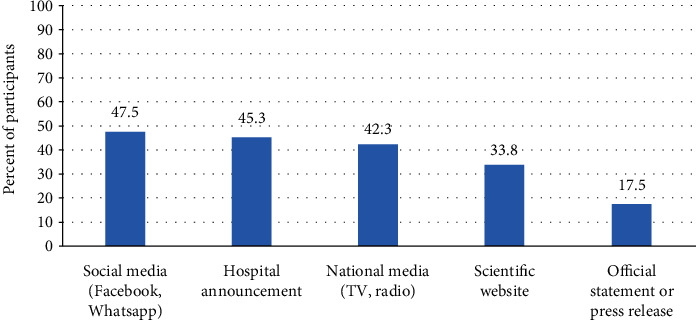
Sources of information about COVID-19 vaccines as reported by participants (n = 400).
3.4. Knowledge of Participants about the Types of COVID-19 Vaccines
Different types of COVID-19 vaccination were reported by the participants, through a closed checklist question answered by each participant, selecting each known vaccine to them. The most common vaccine type known by the participants was AstraZeneca, known by 80% of the participants, followed by Pfizer vaccine (43%). Other types of vaccines and the percent of participants who knew them are detailed in Figure 2.
Figure 2.
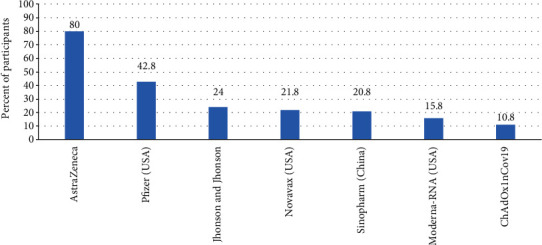
Knowledge of participants about types of COVID-19 vaccines (n = 400).
3.5. Assessment of the Perception of Participants about COVID-19 Vaccination Based on Their Professions
From the participants who believe that vaccination is the key to stop the pandemic, 50.6% were nurses and technicians, while 32.8% were doctors, and 16.6% were pharmacists. No statistically significant difference was found between the perception of participants about vaccination as a key to stop the pandemic and different professions of participants (p = 0.716).
Regarding the opinion of participants about vaccination for either COVID-19 recovered or infected people, no statistically significant difference was found between the perception of participants and their professions (p > 0.05) (Table 3).
Table 3.
Assessment of perception of participants about COVID-19 vaccination based on their professions.
| Professions | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Perception | Doctors | % | Pharmacists | % | Nurses/technicians | % | Total | % | p value |
| Is vaccination the key to stop the pandemic | |||||||||
| Yes | 87 | 32.8 | 44 | 16.6 | 134 | 50.6 | 265 | 72.8 | 0.716 |
| No | 37 | 37.4 | 15 | 15.2 | 47 | 47.5 | 99 | 27.2 | |
| Total | 124 | 34.1 | 59 | 16.2 | 181 | 49.7 | 364 | 100.0 | |
| Vaccination for recovered people from COVID-19 | |||||||||
| Yes | 81 | 36.0 | 36 | 16.0 | 108 | 48.0 | 225 | 61.3 | 0.801 |
| No | 23 | 28.8 | 13 | 16.3 | 44 | 55.0 | 80 | 21.8 | |
| Do not know | 20 | 32.3 | 11 | 17.7 | 31 | 50.0 | 62 | 16.9 | |
| Total | 124 | 33.8 | 60 | 16.3 | 183 | 49.9 | 367 | 100.0 | |
| Vaccination for COVID-19 infected people | |||||||||
| Yes | 46 | 29.9 | 30 | 19.5 | 78 | 50.6 | 154 | 42.0 | 0.389 |
| No | 57 | 39.0 | 19 | 13.0 | 70 | 47.9 | 146 | 39.8 | |
| Do not know | 21 | 31.3 | 11 | 16.4 | 35 | 52.2 | 67 | 18.3 | |
| Total | 124 | 33.8 | 60 | 16.3 | 183 | 49.9 | 367 | 100.0 | |
3.6. Perception of Participants about Criteria of Population That Should Get COVID-19 Vaccination
83% of our study population reported that healthcare workers were the group of population that should get vaccinated, followed by elderly population and people with chronic conditions (39% and 35%, respectively). Other categories are detailed in Figure 3.
Figure 3.
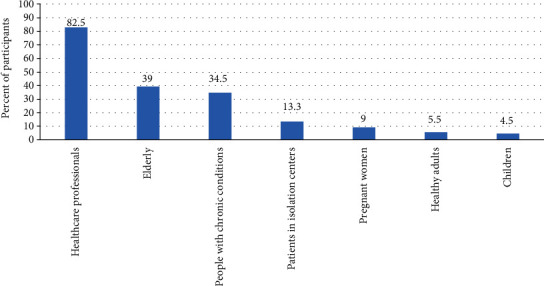
Perception of participants about criteria for vaccination (n = 400).
3.7. Acceptability of the Participants regarding COVID-19 Vaccination Based on Their Professions
Acceptability of COVID-19 vaccination was assessed among different professions of our study population. Of the participants who accepted COVID-19 vaccination, 45.1% were nurses and technicians, while 38.2% were doctors, and 16.7% were pharmacists. A statistically significant association was found (p = 0.032) between vaccine acceptability and professions. Regarding encouraging family members, no statistically significant association was found between encouraging family and professions (p > 0.05).
The time which the participants were intending to get vaccinated was assessed among different professions of the participants. Of those who already took COVID-19 vaccine, 50% were doctors, 34.1% were nurses and technicians, while 15.9% were pharmacists. Among the participants who intended to get COVID-19 vaccination as soon as possible, 50% were nurses, 33.9% were doctors, and 16.1% were pharmacists. Of those who are not intending to get vaccinated at all, 65.7% were nurses, 20.2% were doctors, and 14.1% were pharmacists. A statistically significant association (p = 0.001) was found between intention of getting vaccination and professions of participants (Table 4).
Table 4.
Acceptability of the participants regarding COVID-19 vaccination based on their professions.
| Professions | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Acceptability | Doctors | % | Pharmacists | % | Nurses/technicians | % | Total | % | p value |
| Accepting to get vaccinated | |||||||||
| Yes | 89 | 38.2 | 39 | 16.7 | 105 | 45.1 | 233 | 63.8 | 0.032∗ |
| No | 34 | 25.8 | 21 | 15.9 | 77 | 58.3 | 132 | 36.2 | |
| Total | 123 | 33.7 | 60 | 16.4 | 182 | 49.9 | 365 | 100.0 | |
| Encourage family to take COVID-19 vaccine | |||||||||
| Yes | 94 | 38.2 | 39 | 15.9 | 113 | 45.9 | 246 | 68.1 | 0.135 |
| No | 30 | 26.8 | 17 | 15.2 | 65 | 58.0 | 112 | 31.0 | |
| Do not know | 0 | 0.0 | 1 | 33.3 | 2 | 66.7 | 3 | 0.8 | |
| Total | 124 | 34.3 | 57 | 15.8 | 180 | 49.9 | 361 | 100.0 | |
| When are you going to get vaccinated | |||||||||
| Already did | 41 | 50.0 | 13 | 15.9 | 28 | 34.1 | 82 | 22.7 | 0.001∗ |
| As soon as possible | 42 | 33.9 | 20 | 16.1 | 62 | 50.0 | 124 | 34.3 | |
| After few months | 20 | 35.7 | 12 | 21.4 | 24 | 42.9 | 56 | 15.5 | |
| Never | 20 | 20.2 | 14 | 14.1 | 65 | 65.7 | 99 | 27.4 | |
| Total | 123 | 34.1 | 59 | 16.3 | 179 | 49.6 | 361 | 100.0 | |
∗Statistically significant.
3.8. Association between Acceptability of COVID-19 Vaccination and the Characteristics of the Participants
Based on characteristics of participants, acceptability of COVID-19 vaccination was assessed. No statistically significant association was found between the characteristics of participants, as gender, age, chronic conditions, any vaccination before, and their acceptability of COVID-19 vaccination (p > 0.05). However, there was a statistically significant association between the safety of vaccination and the acceptance of participants to get it (p = 0.001). Table 5 illustrates the associations between characteristic of the participants and their acceptability of COVID-19 vaccination.
Table 5.
Association between acceptability of COVID-19 vaccination and the characteristics of the participants.
| Accepting to get vaccinated | |||||||
|---|---|---|---|---|---|---|---|
| Characteristics | Yes | % | No | % | Total | % | p value |
| Gender | |||||||
| Male | 102 | 65.8 | 53 | 34.2 | 155 | 39.0 | 0.544 |
| Female | 152 | 62.8 | 90 | 37.2 | 242 | 61.0 | |
| Total | 254 | 64.0 | 143 | 36.0 | 397 | 100.0 | |
| Age | |||||||
| 18-35 years | 163 | 61.0 | 104 | 39.0 | 267 | 67.3 | 0.13 |
| 36-55 years | 85 | 69.1 | 38 | 30.9 | 123 | 31.0 | |
| >55 years | 6 | 85.7 | 1 | 14.3 | 7 | 1.8 | |
| Total | 254 | 64.0 | 143 | 36.0 | 397 | 100.0 | |
| Professions | |||||||
| Physician | 89 | 72.4 | 34 | 27.6 | 123 | 31.0 | |
| Pharmacist | 39 | 65.0 | 21 | 35.0 | 60 | 15.1 | 0.127 |
| Nurse | 67 | 60.4 | 44 | 39.6 | 111 | 28.0 | |
| Lab technician | 38 | 53.5 | 33 | 46.5 | 71 | 17.9 | |
| Administrator | 13 | 72.2 | 5 | 27.8 | 18 | 4.5 | |
| Others | 8 | 57.1 | 6 | 42.9 | 14 | 3.5 | |
| Total | 254 | 64.0 | 143 | 36.0 | 397 | 100.0 | |
| Chronic conditions | |||||||
| Yes | 40 | 66.67 | 20 | 33.33 | 60 | 15.11 | 0.638 |
| No | 214 | 63.5 | 123 | 36.5 | 337 | 84.89 | |
| Total | 254 | 63.98 | 143 | 36.02 | 397 | 100 | |
| Received any vaccination last year | |||||||
| Yes | 79 | 69.3 | 35 | 30.7 | 114 | 29.1 | 0.207 |
| No | 174 | 62.6 | 104 | 37.4 | 278 | 70.9 | |
| Total | 253 | 64.5 | 139 | 35.5 | 392 | 100.0 | |
| COVID-19 vaccine safety | 0.001∗ | ||||||
| Not safe | 120 | 57.4 | 89 | 42.6 | 209 | 54.0 | |
| Safe | 131 | 73.6 | 47 | 26.4 | 178 | 46.0 | |
| Total | 251 | 64.9 | 136 | 35.1 | 387 | 100.0 | |
∗Statistically significant.
3.9. Types of COVID-19 Vaccines Accepted to Be Taken by the Participants
Different types of vaccines that were accepted to be taken by the participants are reported in Figure 4. The most accepted type of vaccine was AstraZeneca, accepted by 50% of the participants, followed by Pfizer vaccine, accepted by 20% of the participants. Sinopharm (China) vaccine was accepted by 8%. Other types of vaccines accepted by the participants are mentioned in Figure 4.
Figure 4.

Types of vaccines accepted to be taken by the participants.
3.10. Factors Affecting the Choice of COVID-19 Vaccines as Reported by the Participants
These types of vaccines chosen above were preferred by the participants based on various factors. The most frequently reported factor affecting the choice of vaccine type was the availability of the vaccine in Sudan (reported by 33% of the participants), followed by the reliability of the vaccine in preventing COVID-19 infection (24%). The manufacturing country was the third frequently reported factor (14%). Less side effects were the factor affected the choice of 11% of the participants. Other factors are mentioned in Figure 5.
Figure 5.
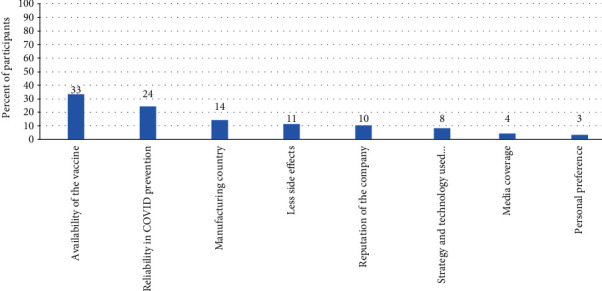
Factors affecting the choice of COVID-19 vaccines as reported by the participants.
3.11. Reasons for Either Taking COVID-19 Vaccine or Not as Reported by the Participants
The reasons reported by the participants for weather taking the vaccine or not were detailed below, and their frequency was detailed.
3.12. Reasons behind Accepting Taking COVID-19 Vaccines Available in Sudan
The most common reasons reported by the participants behind accepting to get COVID-19 vaccination were the worry about getting infected or a family member getting infected. These two reasons were reported by 39% and 36% of the participants, respectively. Other reasons for accepting vaccination were the social responsibility (17.8%) and worry about COVID-19 complications (15.8%). On the other hand, 4% of the participants had no intention to get COVID-19 vaccine (Figure 6).
Figure 6.
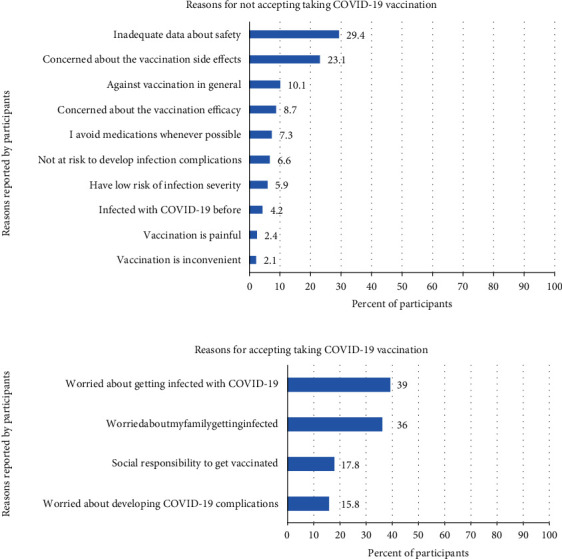
Reasons behind not taking COVID-19 vaccines as reported by participants (n = 400).
3.13. Reasons for Not Taking COVID-19 Vaccines as Reported by the Participants
On the other hand, the reasons for rejecting COVID-19 vaccines were recorded. The most frequently reported reasons were the inadequate data about safety and the concern about side effects. These reasons were reported by 29.4% and 23.1% of the participants who rejected the vaccination. Other reasons are detailed in Figure 6.
4. Discussion
Most of the healthcare staff in this study were young (67%) and aged between 18 and 35 years. This percent was slightly higher than that of the medical staff in United Arab Emirates (50.8%) and lower than the percentage of young staff in Saudi Arabia (72.1%) [13, 14], while in other studies, less than 30% of their staff were aged below 30 years [14–17]. No statistically significant difference was found (p = 0.13) between the age of our participants and their acceptability of COVID-19 vaccination, contrary to the Turkish and Chinese community members (p = 0.001) with older ages being more willing to get COVID-19 vaccines [18, 19].
Females comprised 61% of the healthcare workers in our study, similar studies [20–22] and contrary to the Emirati staff who had more males (64.9%) than females [13]. However, in other studies [14–17, 23, 24], percentages of males and females were almost equal. There was no statistically significant difference in vaccine acceptability between males and females in our study (p = 0.544) as in the study of Saied et al. in Egypt (p = 0.263) [21]. However, in a Turkish study, males were more willing to get COVID-19 vaccination than females (p = 0.02) [18].
Having chronic conditions had no statistically significant association (p = 0.638) to vaccine acceptability as in Turkey (p = 0.397) [18].
Lab technicians and pharmacists were the minority of the medical staff (17.8% and 15%, respectively) compared to doctors and nurses (31% and 28%, respectively).
In Sudan, the medical staff had higher awareness about COVID-19 vaccines (91.2% of the staff) compared to published literature (65.7% and 65.8%) [14, 22], with a statistically significant difference (p = 0.048) among different professions, with doctors being the most aware population.
Sources of information play an important role in vaccination knowledge and acceptability [25]. Our staff reported that the primary source of information about COVID-19 vaccination was the social media as Facebook and WhatsApp (47.5%). This was a preferred source among Egyptian health students [21]. However, in another study, the primary source of information was the government website (46%) and the social media was the source for only (17%) of their staff [13].
Regarding perception of COVID-19 vaccination, 72.8% of our healthcare staff believed that vaccination is the key to combat the pandemic, and lower percentage (67.9%) was reported in an Egyptian study [21]. Even though 5.9% of our staff believed that they were at low risk of getting severe infection, this belief was common (22.4%) among Egyptian staff [19]. By far, the most known vaccine among our staff was AstraZeneca vaccine (80%), followed by Pfizer (43%); other vaccines were less known.
Positively, 83% of our study population reported that healthcare workers were one or the priority groups of population that should get vaccinated, followed by elderly population and people with chronic conditions (39% and 35%, respectively). This was in line with the WHO, 2020 Strategic Advisory Group of Experts [26].
On assessing acceptability of COVID-19 vaccination, acceptance rate was high (63.8%), similar to the rate in China [19] and higher than reported rates (19.6%-60%) in other studies [20, 23, 27–30]. With regard to profession, nurses and lab technicians were the most accepting group (45.1%), followed by doctors (38.2%). The least accepting group was the pharmacists (16.7%) (p = 0.032). Furthermore, in a Canadian study, acceptance of COVID-19 vaccination was the highest among physicians (95%), followed by nurses and administrative staff [20].
The most prevalent reason encouraging vaccination among our staff was the worry of getting COVID-19 infection themselves (39%) or their families (36%). These percentages were lower than reported (47%) in UAE [13]. To put in mind, the percentages depend on when the studies were done, as most countries have ongoing vaccination programs. On the other hand, worry about families was the most prevalent reason among Lebanese and Egyptian health staff (80% and 77.7%, respectively) followed by worrying about themselves (78% and 35.1%), respectively [15, 21].
At the time of the study, 22.7% of the participants had already got vaccinated, with doctors being the most vaccinated group (50%), followed by nurses and technician (34.1%). In China, 34.4% of the participants had received COVID-19 vaccination [19]. This percentage of vaccinated staff was higher than the reported percent (15%) in UAE [13]. On the other hand, pharmacists who got vaccinated were (15.9%) (p = 0.001). Additionally, the most accepted type of vaccination among our healthcare staff was AstraZeneca vaccine, accepted by 50% of the participants, followed by Pfizer vaccine (20%). In contrast to that, in Egypt, the most accepted vaccine was Pfizer (22%) followed by AstraZeneca (7.1%) [21]. Moreover, the most accepted vaccines in Brazil were USA vaccine (82%) and Oxford/England vaccine (81%). Nevertheless, China vaccine was favored by only 8% of our participant, while in Brazil, it was accepted by 67% of their participants [31]. Availability of the vaccine was the most prevalent factor affecting the choice of COVID-19 vaccines as reported by the participants (33%) followed by reliability in protection (24%) and lesser side effects (11%). The same as in Egypt, the motivations for getting COVID-19 vaccines were the effectiveness (14.2%) and the availability (11.7%) [21]. The acceptance of a particular brand of COVID-19 vaccination would depend on the availability and on the national policy of administration of vaccines as well. By the time of the study, only AstraZeneca vaccine was available in vaccination centers, but other vaccines were arriving.
One of the issues and concerns about vaccination was the safety and the risk of developing acute adverse events [19, 30, 32–34]. Fear of adverse effects was expressed by 23.1% of our participants and by 56.3% of Egyptian participants reported in a published study [21]. Vaccination safety was an issue among 53.5% of our participants; this percent was lower in some studies [17, 21, 35]. Nevertheless, these barriers were the reported barriers among Lebanese health staff with the concern about side effects being the most reported barrier (64%) [15]. Moreover, in a multinational study, acceptance of vaccines with minor adverse reactions was the reason reported with a percentage ranging from 42% to 86.4% based in the country [16]. Other reported reasons among our staff were as follows: have low risk for developing severe infection (5.9%), have natural immunity from previous infection (4.2%), and dislike of injections (2.4%). These same reasons were reported in a Canadian study with comparable percentages [20].
The rejection rate among our staff was 27.4%, similar to published studies [17, 21]. Contrary to that, the rejection rate was mush lower in other studies [19, 20, 23, 35]. Among those rejecting vaccination, 65.7% were nurses and technicians, 20.2% were doctors, and 14.1% were pharmacists (p = 0.001). Vaccination safety had a statistically significant association to the acceptability of vaccines among our staff (p = 0.001). This strong association (p < 0.001) was reported by İkiışık et al. and Saied et al. as well [18, 21].
Since majority of health staff work at public hospitals [22], our study assessed the staff in governmental hospitals to get a clear image about vaccination hesitancy. The privilege of our study is that it tangled the vaccination acceptance among different professions of healthcare staff (doctors, pharmacists, lab technicians, nurses, and administrative staff).
Our study was not without limitations; the data collected from working staff were not validated through Cronbach test of reliability. Moreover, private sector was not covered in this study. Moreover, wider studies covering all states of Sudan, as well as community-based studies, will give a clearer picture about vaccination knowledge and acceptability.
5. Conclusion
The present study revealed the presence of good knowledge and acceptability among medical staff towards COVID-19 vaccinations in Sudan. The healthcare staff in Sudan were mostly young in their age more than elsewhere. As in many other countries, concern about safety and side effects governed the vaccination acceptance. Majority of our study population had a perception that healthcare workers were the group of population that should get vaccinated first, followed by elderly population and people with chronic conditions. The mostly known and accepted COVID-19 vaccines were AstraZeneca and Pfizer. This might be dependent on the availability and on the national policy of administration of vaccines. Encouraging factor for vaccination was the fear of getting infection themselves and their families.
6. Recommendations
The construction of immediate health educational programs and more accurate information should be distributed and advertised by respective health authorities for all community members. Policy makers should take steps to ensure encouragement, positive perceptions, and improved acceptability towards COVID-19 vaccinations in order to reduce the vaccine hesitancy. In Sudan, using the social media to spread the correct knowledge is an important approach as it was the primary source used by healthcare workers as shown by this study. More vaccination centers or community vaccination teams will fasten the vaccination process and provide more coverage. Moreover, more studies similar to this study are needed in other states of Sudan.
Acknowledgments
The authors are grateful to Shurouq O. H. Abdelraheem, Faculty of Engineering, University of Khartoum, for her assistance in the data entry process. The authors also acknowledge the cooperation of the departments of the hospitals during the data collection.
Abbreviations
- ARDS:
Acute respiratory distress syndrome
- FMOH:
Federal Ministry of Health
- MOH:
Ministry of Health
- mRNA:
Messenger ribonucleic acid
- WHO:
World Health Organization.
Data Availability
All supporting data are available.
Ethical Approval
The study proposal was approved by the Administration of Innovation and Scientific Research at the State Ministry of Health (MOH), Khartoum. Expedited review was conducted by the IRB of the MOH, and approval was granted. Then, approval was obtained from the medical administrations of the hospitals. Regarding participants, the data were collected through a self-administered questionnaire. Confidentiality of the participants was assured through the use of an anonymous research tool. The collected data were used strictly for the purpose of the study objectives.
Consent
Informed consents from the participants were obtained, voluntarily. No clinical details of participants that might compromise their anonymity were used in the development of this manuscript.
Conflicts of Interest
The authors declared no competing interest.
Authors' Contributions
All authors have read the final manuscript and gave their approval for publication. YEOM, FHAA, IZBY, MMMA, and IMMA contributed to the conceptualization and data collection. WSEK contributed to the data collection and writing—review and editing. AGOH contributed to the cosupervision, formal analysis, and writing—original draft. MMYS contributed to the supervision, conceptualization, and writing—review and editing.
Supplementary Materials
Table S1: knowledge of participants about COVID-19 vaccination. Table S2: perception of participants about COVID-19 vaccination. Table S3: acceptability of participants for COVID-19 vaccination. Table S4: reasons behind accepting taking COVID-19 vaccines available in Sudan. Table S5: reasons behind not taking COVID-19 vaccines as reported by participants.
References
- 1.Abdelhafiz A. S., Mohammed Z., Ibrahim M. E., et al. Knowledge, perceptions, and attitude of Egyptians towards the novel coronavirus disease (COVID-19) Journal of Community Health . 2020;45(5):881–890. doi: 10.1007/s10900-020-00827-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang J., Peng Y., Xu H., Cui Z., Williams R. O. The COVID-19 vaccine race: challenges and opportunities in vaccine formulation. AAPS PharmSciTech . 2020;21(6):p. 225. doi: 10.1208/s12249-020-01744-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhong B. L., Luo W., Li H. M., et al. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. International Journal of Biological Sciences . 2020;16(10):1745–1752. doi: 10.7150/ijbs.45221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers of Disease Control and Prevention. How vaccines work . 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/how-they-work.html .
- 5.Centers of Disease Control and Prevention. Understanding mRNA COVID-19 vaccines . 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/mrna.html .
- 6.World Health Organization. How do vaccines work? 2020. https://www.who.int/news-room/feature-stories/detail/how-do-vaccines-work .
- 7.Karlsson L. C., Lewandowsky S., Antfolk J., et al. The association between vaccination confidence, vaccination behavior, and willingness to recommend vaccines among Finnish healthcare workers. PLoS One . 2019;14(10):p. e0224330. doi: 10.1371/journal.pone.0224330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paterson P., Meurice F., Stanberry L. R., Glismann S., Rosenthal S. L., Larson H. J. Vaccine hesitancy and healthcare providers. Vaccine . 2016;34(52):6700–6706. doi: 10.1016/j.vaccine.2016.10.042. [DOI] [PubMed] [Google Scholar]
- 9.Dubé E., Laberge C., Guay M., Bramadat P., Roy R., Bettinger J. Vaccine hesitancy: an overview. Human Vaccines & Immunotherapeutics . 2013;9(8):1763–1773. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mac Donald N. E. SAGE working group on vaccine hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine . 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 11.Caserotti M., Girardi P., Rubaltelli E., Tasso A., Lotto L., Gavaruzzi T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Social Science & Medicine . 2021;272, article 113688 doi: 10.1016/j.socscimed.2021.113688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization. Federal Ministry of Health. SUDAN Outbreaks Dashboard . 2022. https://fmoh.shinyapps.io/Outbreaks/
- 13.Ahamed F., Ganesan S., James A., Zaher W. A. Understanding perception and acceptance of Sinopharm vaccine and vaccination against COVID-19 in the UAE. BMC Public Health . 2021;21(1):p. 1602. doi: 10.1186/s12889-021-11620-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Al-Mohaithef M., Padhi B. K., Ennaceur S. Socio-demographics correlate of COVID-19 vaccine hesitancy during the second wave of COVID-19 pandemic: a cross-sectional web-based survey in Saudi Arabia. Front Public Health . 2021;9 doi: 10.3389/fpubh.2021.698106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nasr L., Saleh N., Hleyhel M., El-Outa A., Noujeim Z. Acceptance of COVID-19 vaccination and its determinants among Lebanese dentists: a cross-sectional study. BMC Oral Health . 2021;21(1):p. 484. doi: 10.1186/s12903-021-01831-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wong L. P., Alias H., Danaee M., et al. COVID-19 vaccination intention and vaccine characteristics influencing vaccination acceptance: a global survey of 17 countries. Infectious Diseases of Poverty . 2021;10(1):p. 122. doi: 10.1186/s40249-021-00900-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.El-Mohandes A., White T. M., Wyka K., et al. COVID-19 vaccine acceptance among adults in four major US metropolitan areas and nationwide. Scientific Reports . 2021;11(1):p. 21844. doi: 10.1038/s41598-021-00794-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.İkiışık H., Akif Sezerol M., Taşçı Y., Maral I. COVID-19 vaccine hesitancy: a community-based research in Turkey. International Journal of Clinical Practice . 2021;75(8, article e14336) doi: 10.1111/ijcp.14336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang C., Han B., Zhao T., et al. Vaccination willingness, vaccine hesitancy, and estimated coverage at the first round of COVID-19 vaccination in China: a national cross-sectional study. Vaccine . 2021;39(21):2833–2842. doi: 10.1016/j.vaccine.2021.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dzieciolowska S., Hamel D., Gadio S., et al. Covid-19 vaccine acceptance, hesitancy, and refusal among Canadian healthcare workers: a multicenter survey. American Journal of Infection Control . 2021;49(9):1152–1157. doi: 10.1016/j.ajic.2021.04.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saied S. M., Saied E. M., Kabbash I. A., Abdo S. A. E. Vaccine hesitancy: beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. Journal of Medical Virology . 2021;93(7):4280–4291. doi: 10.1002/jmv.26910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fakonti G., Kyprianidou M., Toumbis G., Giannakou K. Attitudes and acceptance of COVID-19 vaccination among nurses and midwives in Cyprus: a cross-sectional survey. Front Public Health . 2021;9 doi: 10.3389/fpubh.2021.656138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sherman S. M., Smith L. E., Sim J., et al. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Human Vaccines & Immunotherapeutics . 2021;17(6):1612–1621. doi: 10.1080/21645515.2020.1846397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Graeber D., Schmidt-Petri C., Schröder C. Attitudes on voluntary and mandatory vaccination against COVID-19: evidence from Germany. PLoS One . 2021;16(5, article e0248372) doi: 10.1371/journal.pone.0248372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kestenbaum L. A., Feemster K. A. Identifying and addressing vaccine hesitancy. Pediatric Annals . 2015;44(4):e71–e75. doi: 10.3928/00904481-20150410-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brüssow H. COVID-19: vaccination problems. Environmental Microbiology . 2021;23(6):2878–2890. doi: 10.1111/1462-2920.15549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marquez R. R., Gosnell E. S., Thikkurissy S., Schwartz S. B., Cully J. L. Caregiver acceptance of an anticipated COVID-19 vaccination. Journal of the American Dental Association (1939) . 2021;152(9):730–739. doi: 10.1016/j.adaj.2021.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ameerah M., Alshareef N. Q. N., Alsharqi O. Acceptability of a COVID-19 vaccine among healthcare workers in the Kingdom of Saudi Arabia . 2020. https://www.frontiersin.org/articles/10.3389/fmed.2021.644300/full . [DOI] [PMC free article] [PubMed]
- 29.Islam M. S., Siddique A. B., Akter R., et al. Knowledge, attitudes and perceptions towards COVID-19 vaccinations: a cross-sectional community survey in Bangladesh. BMC Public Health . 2021;21(1, article 1851) doi: 10.1186/s12889-021-11880-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Al-Qerem W. A., Jarab A. S. COVID-19 vaccination acceptance and its associated factors among a middle eastern population. Frontiers in Public Health . 2021;9:1–11. doi: 10.3389/fpubh.2021.632914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gramacho W. G., Turgeon M. When politics collides with public health: COVID-19 vaccine country of origin and vaccination acceptance in Brazil. Vaccine . 2021;39(19):2608–2612. doi: 10.1016/j.vaccine.2021.03.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ozawa S., Stack M. L. Public trust and vaccine acceptance--international perspectives. Human Vaccines & Immunotherapeutics . 2013;9(8):1774–1778. doi: 10.4161/hv.24961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Williams S. E. What are the factors that contribute to parental vaccine-hesitancy and what can we do about it? Human Vaccines & Immunotherapeutics . 2014;10(9):2584–2596. doi: 10.4161/hv.28596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zarobkiewicz M. K., Zimecka A., Zuzak T., Cieślak D., Roliński J., Grywalska E. Vaccination among Polish university students. Knowledge, beliefs and anti-vaccination attitudes. Human Vaccines & Immunotherapeutics . 2017;13(11):2654–2658. doi: 10.1080/21645515.2017.1365994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Day P., Strenth C., Kale N., Schneider F. D., Arnold E. M. Perspectives of primary care physicians on acceptance and barriers to COVID-19 vaccination. Family Medicine and Community Health . 2021;9(4, article e001228) doi: 10.1136/fmch-2021-001228. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1: knowledge of participants about COVID-19 vaccination. Table S2: perception of participants about COVID-19 vaccination. Table S3: acceptability of participants for COVID-19 vaccination. Table S4: reasons behind accepting taking COVID-19 vaccines available in Sudan. Table S5: reasons behind not taking COVID-19 vaccines as reported by participants.
Data Availability Statement
All supporting data are available.


