Abstract
Introduction
Promoting older adults to self-manage their chronic conditions is a major focus of the Macao government and healthcare professionals since more than 80% of older adults have suffered chronic conditions.
Objectives
This study evaluated the effect of the Chronic Disease Self-management Program (CDSMP) on self-management behaviors, self-efficacy, health status, and healthcare services utilization among Macao older adults with chronic disease over six months, and assessed whether the intervention effect persisted for one year.
Methods
A longitudinal and quasi-experimental design was used in this study. A total number of 158 older adults with at least one chronic disease were recruited from three Macao community centers. Participants in the study group engaged in a six-session CDSMP in the community centers and participants in the control group received usual care. The Chronic Disease Self-management Questionnaire was used to assess the outcome measures for baseline, six-month and one-year assessment.
Results
The age of subjects ranged from 60 to 88, 64.6% had three or more chronic diseases. The results showed that the subjects in the study group had significant improvement in self-management behaviors, self-efficacy, and some health-related indicators at the point of six months, and these improvements were still observable at the point of one year when comparing to the control group. The results also showed that the study group had a decrease in healthcare services utilization, but there was no significant difference between the two groups.
Conclusion
This study confirmed that the community-dwelling older adults in Macao can acquire positive outcomes in self-management and health-related indicators from the CDSMP. Hence, it is worth promoting this program as a health promotion activity in community.
Keywords: older adults, self-management, chronic conditions, effectiveness
Introduction
In Macao, more than 80% of older adults have one or more chronic diseases and 17% of older adults seek medical services four or more times within three months (Kiang Wu Nursing College of Macau, 2006). Macao older adults mainly rely on public healthcare system and over 30% of users of public health services are older adults (Leong, 2012). The mean increasing rate in the use of outpatient and emergency services by the older adults was 6.0% and 11.7% per year respectively from 2009 to 2013. Owing to the increase in aging population, the medical expenditures will have increased by 2036 (Macao Statistics and Census Bureau, 2014), chronic care has thus become a greater challenge for the Macao healthcare system. Furthermore, people suffering from chronic diseases have experienced different degree of symptom distress (such as pain, fatigue and shortness of breath) and reported lower quality of life (Lam & Lauder, 2000). Since most chronic diseases cannot be cured completely, patients need to change their lifestyles and master management skills in order to reduce the impact on their daily life. The prevalence rate of chronic disease in older adults aged 60 or above was significantly higher than those aged below 60 (Research Group of “Macao Health Survey 2006,” 2008). However, previous research findings showed that the older adults in Macao have less awareness and ability to maintain their own health (Leong & Du, 2018). In addition, the current health promotion activities for the older adults in Macao mainly focus on health talks and exercise classes. Hence, it is necessary to explore the way that can promote older adults to self-manage their chronic conditions in order to reduce the usage of healthcare services by the older adults.
Evidence supported that the Stanford’s Chronic Disease Self-management Program (CDSMP) can effectively reduce the utilization of healthcare services by improving the health behaviors and health status of participants with chronic diseases (Fu et al., 2003; Hong et al., 2017; Lorig et al., 1999; McLaughlin, 2019). In addition, some studies also showed a positive outcome of the CDSMP in health behaviors and health status but have no significant difference in using healthcare services (Chan et al., 2011; Tomioka et al., 2012; Xu et al., 2017). Although most studies showed a positive outcome of the CDSMP for adults with chronic conditions, there were still some evidence gaps in related research field. First, previous studies (Chan et al., 2011; Fu et al., 2003; Hong et al., 2017) in Chinese communities mainly evaluated the short-term effect of the CDSMP after six months. Second, although some long-term follow-up studies were conducted in Western countries (Barlow et al., 2005; Lorig et al., 2001; Salvatore et al., 2015), an attrition bias may occur in uncontrolled study (Lederle & Bitzer, 2019). Third, a one-year follow-up study was conducted in Nanjing of China (Qi et al., 2019), but it was not aimed at older adults and it only evaluated the effect on quality of life. It showed that the evidence of long-term outcome and differences between short-term and long-term outcome of CDSMP for older adults in Chinese communities was still limited.
This study designed a quasi-experimental study to (1) assess the effectiveness of the CDSMP on self-management behaviors, self-efficacy, health status, and healthcare services utilization, compared to the usual care, in older adults with chronic disease over six months, and (2) determine whether the intervention effect persisted for one year.
Methods
Design and Settings
The longitudinal and quasi-experimental design was utilized in this study, and the study was performed at three community centers in Macao.
Subjects and Sample Size Calculation
Inclusion criteria: (1) Macao citizens aged 60 or above (people aged 60 or above are usually considered as older adults in Macao since those people can receive pensions provided by the Government); (2) Diagnosis with at least one chronic disease; (3) Live at home; (4) Can communicate in Chinese; (5) No severe complications.
According to previous studies, the CDSMP has a small effect on the “self-efficacy in managing disease in general” (Fu et al., 2003). Using G*Power software 3.0 with a power of 0.80, a two-sided type I error of 0.05 and number of measurements of three, the calculated total sample size for the current study would be 122. Assuming that the drop-out rate was 25%, 154 subjects were needed in this study (77 subjects in each group).
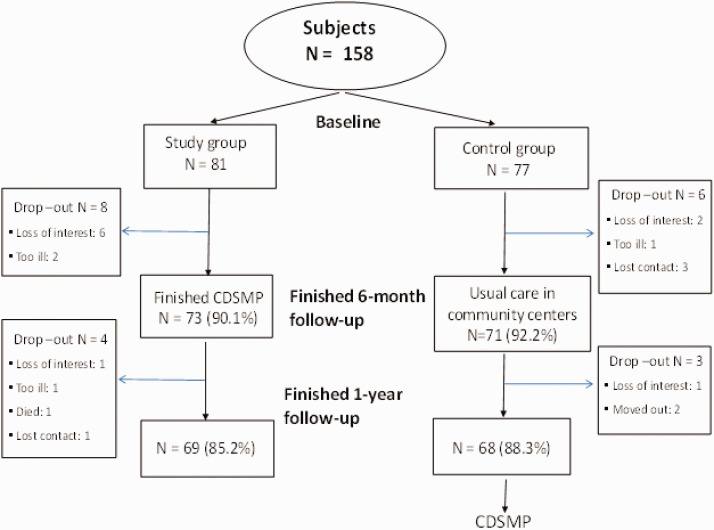
A total number of 158 older adults were recruited in this study (81 subjects in study group and 77 subjects in control group). There was no randomized allocation in the two groups since the training sessions could only be arranged in the fixed activity schedule of community centers. Subjects who could participate in the scheduled CDSMP classes were assigned to the study group, whereas the other subjects were assigned to the control group. Recruitment commenced in September 2012 and the final follow-up assessment was conducted in June 2014. Figure 1 shows the flow chart of participants.
Figure 1.
Flow Chart of Subjects.
Outcome Measurements
The outcome measurements were assessed for all subjects at baseline (before the intervention), at the point of six months and one year. In order to reduce the bias, four trained outcome assessors were blinded to perform the assessments.
The use of the Chronic Disease Self-management Questionnaire (Hong Kong Chinese Version) (Woo et al., 2009) was permitted by the author for outcome measurements in this study. The questionnaire was valid and suitable to be used in Chinese population (Fu et al., 2003; Woo et al., 2009). The content of questionnaire included: (1) Demographic data: age, gender, marital status, years of education, disease profile. (2) Self-management behaviors: exercise time per week, frequency of cognitive symptom management and communication with physician. (3) Self-efficacy: confidence in managing disease in general and managing symptoms. (4) Health status: disability, social activities limitations, energy, psychological well-being, depressive symptom, health distress, pain and discomfort, fatigue, shortness of breath, self-rated health. (5) Healthcare services utilization: number of times of general practitioner visits, other health service visits, emergency room visits, number of days in hospital.
Intervention
Subjects in the study group engaged in a six-session CDSMP held by trained leaders who did not perform any follow-up assessments, one session per week and each session lasted for 2.5 hours. All leaders had completed a four-day leader training course before leading the program. The leaders delivered the program following a standardized manual. Each program was conducted in group of 10–15 participants in the community centers. The CDSMP was developed by Dr. Lorig and colleagues of Stanford Patient Education Research Center (Lorig et al., 1999). It is a constructive program and widely used in Western countries. The Chinese version was modified and adapted for older adults by the Salvation Army (Hong Kong). Table 1 shows the content of the six weeks CDSMP (Chan et al., 2011; The Salvation Army, 2008). Educational talk, sharing, group discussion, action planning and peer support were accomplished in each session.
Table 1.
The Content of the Six Sessions CDSMP.
| Session | Content |
|---|---|
| 1 | Self introduction of participants and program overview |
| Differences between acute and chronic disease | |
| Identifying common problems among participants with chronic disease | |
| The self-management skills (include cognitive symptom management and distraction) | |
| Introduction to action plan and making an action plan according to their own goals | |
| 2 | Feedback and problem solving |
| Community resources | |
| Dealing with negative emotions | |
| Introduction to physical activity and exercise | |
| Making an action plan | |
| 3 | Feedback and problem solving |
| Better breathing, muscle relaxation, pain and fatigue management | |
| Exercises for improving flexibility, muscle strength and endurance | |
| Making an action plan | |
| 4 | Feedback and problem solving |
| Having a balanced diet | |
| Communication skills | |
| Planning for the future | |
| Making an action plan | |
| 5 | Feedback and problem solving |
| Use of medication | |
| Positive thinking, guided imagery and depression management | |
| Making informed treatment decisions | |
| Making an action plan | |
| 6 | Feedback and problem solving |
| Working with healthcare professionals and self-care actively | |
| Review and looking forward |
Usual Care
All subjects in the control and study group attended the regular activities (such as health talk, exercise classes and other recreational activities) in the community centers during the study period. In addition, all subjects could access regular follow-up consultation in the public healthcare centers.
Ethical Consideration
This study was approved by the Research Committee of Kiang Wu Nursing College of Macau with Certificate of Approval No. 2011SEP01. A written informed consent was obtained from each subject after explanation of the aim of this study. All subjects can withdraw from the study anytime. All subjects in the control group can attend the same program in accordance with their wishes after the study.
Statistical Analysis
Analyses were conducted at two-sided 0.05 significance level, using the SPSS software (Version 22.0). Intention-to-Treat method was used for analysis. The missing data of dropping out participants were replaced by using the last observation data. Demographic data and outcome measures at baseline of the subjects in the study and control group were compared using independent t-test or chi-square tests. Linear mixed-effects modeling for repeated measures over time was used to compare the outcomes at baseline, the point of six months and one year in the study and control group. The mean changes of outcome measures from baseline to 12 months of the subjects between the study and control group were compared using independent t-test.
Results
A total number of 158 older adults were recruited in this study. In total, 144 subjects finished the six-month follow-up and 137 subjects completed the one-year follow-up assessment. The drop-out rate was less than 15% in both groups. The main reasons for withdrawing from the study were too ill, lost contact, moved out to another city and loss of interest in this study.
Subjects Characteristics at Baseline
The age of subjects ranged from 60 to 88 (mean age = 72.9 ± 6.64), 123 (77.8%) of them were female, and 60 (30.0%) were widowed. Most of them (64.6%) had three or more chronic diseases. The educational level of subjects was low, only 47 (29.7%) had a primary school education or above.
No significant difference was found between the study and control group in the demographic data (Table 2) and outcome measures (Table 3) in the baseline assessment.
Table 2.
Subjects’ Characteristics at Baseline.
| Characteristics | Study (N = 81) | Control (N = 77) | t /χ2 | P-valve |
|---|---|---|---|---|
| Gender: female (%) | 81.5 | 74.0 | 1.27 | 0.259 |
| Marital status (%) | 4.96 | 0.291 | ||
| Married | 50.0 | 59.7 | ||
| Widowed | 42.5 | 33.8 | ||
| Others | 7.5 | 6.5 | ||
| Mean age (SD) | 72.8 (6.8) | 73.0 (6.6) | –0.19 | 0.851 |
| Mean number of chronic disease (SD) | 3.3 (1.8) | 3.4 (1.6) | –0.44 | 0.659 |
Table 3.
Mean Scores of Outcome Measures at Baseline.
|
Study (N = 81) |
Control (N = 77) |
|||||
|---|---|---|---|---|---|---|
| Outcome measures | Mean | SD | Mean | SD | t | P-value |
| Self-management behaviors | ||||||
| Exercises (0–20) | 6.10 | 3.27 | 5.56 | 2.86 | 1.22 | 0.271 |
| Cognitive symptom management (0–5) | 1.11 | 0.82 | 1.09 | 0.89 | 0.13 | 0.894 |
| Communication with physician (0–5) | 1.20 | 1.12 | 1.38 | 1.33 | −0.92 | 0.360 |
| Self-efficacy | ||||||
| Managing disease in general (0–10) | 6.82 | 1.98 | 6.59 | 2.10 | 0.70 | 0.487 |
| Managing symptoms (0–10) | 5.93 | 2.66 | 5.64 | 2.84 | 0.66 | 0.508 |
| Health status | ||||||
| Disability (0–3) a | 0.09 | 0.19 | 0.07 | 0.19 | 0.53 | 0.594 |
| Social/role activities limitations (0–4) a | 0.42 | 0.67 | 0.33 | 0.69 | 0.85 | 0.397 |
| Energy (0–5) | 3.36 | 1.30 | 3.44 | 1.30 | −0.42 | 0.678 |
| Psychological well-being (0–5) | 4.01 | 1.15 | 4.13 | 0.94 | −0.75 | 0.456 |
| Depressive symptom (0–5) a | 0.77 | 0.94 | 0.70 | 0.87 | 0.49 | 0.627 |
| Health distress (0–5) a | 0.87 | 1.29 | 0.92 | 1.03 | −0.26 | 0.796 |
| Pain and discomfort (0–10) a | 3.54 | 3.22 | 3.39 | 3.20 | 0.30 | 0.764 |
| Fatigue (0–10) a | 3.12 | 3.06 | 2.27 | 2.80 | 1.82 | 0.071 |
| Shortness of breath (0–10) a | 0.62 | 1.83 | 0.65 | 1.80 | −0.11 | 0.912 |
| Self-rated health (1–5) a | 3.59 | 0.92 | 3.55 | 0.91 | 0.32 | 0.747 |
| Healthcare services utilization | ||||||
| General practitioner visits b | 3.08 | 9.21 | 3.23 | 4.85 | −0.13 | 0.899 |
| Other health service visits | 3.98 | 12.29 | 2.78 | 5.15 | 0.79 | 0.431 |
| Emergency room visits | 0.62 | 1.40 | 0.47 | 1.06 | 0.79 | 0.432 |
| Number of days in hospital | 0.44 | 1.92 | 0.38 | 2.32 | 0.18 | 0.856 |
Lower score indicates better result.
Study group n = 77; control group n = 77.
Comparison Between Three Time Points in the Study and Control Group
The results of the six-month assessment showed that the subjects in the study group had significant improvement in self-management behaviors (increase in exercise time, cognitive symptom management and communication with physician), self-efficacy (increase in managing disease in general and managing symptom), and health status (increase in energy and psychological well-being, decrease in depressive symptom, health distress and fatigue). These improvements were still observable at the point of one year. The results also showed that the study group had a decrease in outpatient service utilization, but there was no significant difference between the three different time points (Table 4).
Table 4.
Comparisons of Outcome Measures between Three Time Points in the Study Group.
|
Baseline |
6 months |
12 months |
Change from baseline to 6 month |
Change from baseline to 12 month |
|||
|---|---|---|---|---|---|---|---|
| Outcome measures (range of score) | Mean (SD) | Mean (SD) | Mean (SD) | Mean | P | Mean | P |
| Self-management behaviors | |||||||
| Exercises (0–20) | 6.10 (3.27) | 7.43 (3.15) | 7.57 (3.67) | 1.33 | 0.001 | 1.47 | 0.002 |
| Cognitive symptom management (0–5) | 1.10 (0.82) | 1.79 (0.95) | 1.52 (0.86) | 0.69 | 0.000 | 0.42 | 0.001 |
| Communication with physician (0–5) | 1.26 (1.16) | 1.77 (1.46) | 1.64 (1.31) | 0.51 | 0.000 | 0.38 | 0.007 |
| Self-efficacy | |||||||
| Managing disease in general (0–10) | 6.85 (1.98) | 7.27 (1.50) | 7.47 (1.73) | 0.42 | 0.025 | 0.62 | 0.013 |
| Managing symptoms (0–10) | 6.00 (2.63) | 6.65 (1.90) | 7.16 (1.81) | 0.65 | 0.031 | 1.16 | 0.000 |
| Health status | |||||||
| Disability (0–3)a | 0.09 (0.19) | 0.12 (0.23) | 0.11 (0.22) | 0.03 | 0.078 | 0.02 | 0.203 |
| Social/role activities limitations (0–4)a | 0.42 (0.67) | 0.28 (0.63) | 0.29 (0.59) | −0.15 | 0.049 | −0.13 | 0.092 |
| Energy (0–5) | 3.35 (1.30) | 3.65 (1.17) | 3.76 (1.02) | 0.30 | 0.006 | 0.41 | 0.000 |
| Psychological well-being (0–5) | 4.00 (1.14) | 4.24 (0.93) | 4.34 (0.87) | 0.24 | 0.008 | 0.34 | 0.000 |
| Depressive symptom (0–5)a | 0.77 (0.94) | 0.59 (0.71) | 0.48 (0.71) | −0.18 | 0.004 | −0.30 | 0.000 |
| Health distress (0–5)a | 0.88 (1.29) | 0.68 (0.94) | 0.56 (0.78) | −0.20 | 0.022 | −0.32 | 0.004 |
| Pain and discomfort (0–10)a | 3.58 (3.22) | 3.42 (3.05) | 3.20 (2.65) | −0.16 | 0.639 | −0.38 | 0.269 |
| Fatigue (0–10)a | 3.15 (3.05) | 2.58 (2.96) | 2.38 (2.72) | −0.57 | 0.045 | −0.77 | 0.012 |
| Shortness of breath (0–10)a | 0.62 (1.83) | 0.83 (1.95) | 0.64 (1.66) | 0.21 | 0.398 | 0.02 | 0.902 |
| Self-rated health (1–5)a | 3.59 (0.92) | 3.42 (1.07) | 3.49 (0.90) | −0.17 | 0.099 | −0.10 | 0.328 |
| Health care services utilization | |||||||
| General practitioner visits | 3.06 (9.27) | 2.86 (4.48) | 2.01 (3.27) | −0.21 | 0.845 | −1.05 | 0.282 |
| Other health service visits | 4.12 (12.32) | 3.24 (14.01) | 3.09 (8.87) | −0.89 | 0.668 | −1.04 | 0.521 |
| Emergency room visits | 0.61 (1.40) | 0.61 (1.75) | 0.47 (1.29) | 0.00 | 1.000 | −0.14 | 0.157 |
| Number of days in hospital | 0.44 (1.92) | 0.49 (2.26) | 0.53 (2.31) | 0.05 | 0.850 | 0.09 | 0.727 |
Notes: P value in italics mean P <0.05; aLower score indicates better result.
The results showed that there was no significant difference in most outcome measures in the control group between the three different time points. However, subjects in the control group experienced worsening disability in the six-month and one-year assessment and declined self-rated health in the one-year assessment (Table 5).
Table 5.
Comparisons of Outcome Measures between Three Time Points in the Control Group.
|
Baseline |
6 months |
12 months |
Change from baseline to 6 months |
Change from baseline to 12 months |
|||
|---|---|---|---|---|---|---|---|
| Outcome measures (range of score) | Mean (SD) | Mean (SD) | Mean (SD) | Mean | P | Mean | P |
| Self-management behaviors | |||||||
| Exercises (0–20) | 5.56 (2.86) | 6.13 (2.97) | 6.05 (2.60) | 0.57 | 0.105 | 0.49 | 0.080 |
| Cognitive symptom management (0–5) | 1.10 (0.89) | 0.84 (0.72) | 0.90 (0.63) | −0.26 | 0.012 | −0.20 | 0.011 |
| Communication with physician (0–5) | 1.32 (1.29) | 1.25 (1.16) | 1.44 (1.10) | −0.08 | 0.557 | 0.12 | 0.313 |
| Self-efficacy | |||||||
| Managing disease in general (0–10) | 6.56 (2.10) | 6.57 (2.14) | 6.90 (1.79) | −0.01 | 0.972 | 0.34 | 0.124 |
| Managing symptoms (0–10) | 5.56 (2.85) | 5.65 (2.50) | 5.83 (2.49) | 0.10 | 0.753 | 0.27 | 0.409 |
| Health status | |||||||
| Disability (0–3)a | 0.07 (0.19) | 0.15 (0.26) | 0.11 (0.23) | 0.07 | 0.000 | 0.04 | 0.013 |
| Social/role activities limitations (0–4)a | 0.33 (0.69) | 0.40 (0.86) | 0.35 (0.73) | 0.07 | 0.178 | 0.02 | 0.702 |
| Energy (0–5) | 3.45 (1.30) | 3.41 (1.20) | 3.47 (1.19) | −0.04 | 0.737 | 0.02 | 0.864 |
| Psychological well-being (0–5) | 4.14 (0.94) | 4.13 (0.96) | 4.23 (0.96) | −0.01 | 0.952 | 0.09 | 0.339 |
| Depressive symptom (0–5)a | 0.70 (0.87) | 0.64 (0.82) | 0.64 (0.90) | −0.06 | 0.426 | −0.05 | 0.504 |
| Health distress (0–5)a | 0.90 (1.04) | 0.70 (0.83) | 0.84 (1.06) | −0.20 | 0.058 | −0.06 | 0.622 |
| Pain and discomfort (0–10)a | 3.55 (3.19) | 3.55 (3.01) | 3.51 (3.00) | 0.20 | 0.555 | 0.16 | 0.636 |
| Fatigue (0–10)a | 2.25 (2.81) | 2.52 (2.47) | 2.35 (2.80) | 0.27 | 0.326 | 0.10 | 0.751 |
| Shortness of breath (0–10)a | 0.65 (1.80) | 0.79 (2.07) | 0.71 (1.83) | 0.14 | 0.446 | 0.07 | 0.652 |
| Self-rated health (1–5)a | 3.55 (0.91) | 3.64 (0.89) | 3.75 (0.78) | 0.09 | 0.330 | 0.21 | 0.009 |
| Health care services utilization | |||||||
| General practitioner visits | 3.25 (4.85) | 4.01 (11.29) | 3.96 (5.45) | 0.76 | 0.564 | 0.71 | 0.275 |
| Other health service visits | 2.62 (5.05) | 2.41 (5.35) | 2.31 (4.86) | −0.21 | 0.714 | −0.31 | 0.595 |
| Emergency room visits | 0.48 (1.06) | 0.72 (2.44) | 0.69 (1.67) | 0.24 | 0.374 | 0.21 | 0.279 |
| Number of days in hospital | 0.38 (2.32) | 0.84 (3.93) | 0.97 (5.18) | 0.47 | 0.302 | 0.60 | 0.292 |
Notes: P value in italics mean P <0.05;a Lower score indicates better result.
Between-Group Comparison of the Changes of Outcome Measures From Baseline to 12 Months
The results of the one-year assessment showed that the subjects in the study group had significant improvement in cognitive symptom management, self-efficacy in managing symptoms, energy, psychological well-being, depressive symptom and self-rated health when compared with those in the control group. The results also showed that the study group had a decrease in healthcare services utilization, but there was no significant difference between the two groups (Table 6).
Table 6.
Comparisons of Mean Changes of Outcome Measures Between Groups at 12 Months.
| Study group | Control group | |||
|---|---|---|---|---|
| Outcome measures (range of score) | Mean change (SD) | Mean change (SD) | t | P-value |
| Self-management behaviors | ||||
| Exercises (0–20) | 1.47 (4.21) | 0.49 (2.44) | 1.79 | 0.075 |
| Cognitive symptom management (0–5) | 0.42 (1.06) | −0.20 (0.67) | 4.40 | 0.000 |
| Communication with physician (0–5) | 0.38 (1.23) | 0.12 (1.01) | 1.48 | 0.141 |
| Self-efficacy | ||||
| Managing disease in general (0–10) | 0.62 (2.19) | 0.34 (1.90) | 0.85 | 0.395 |
| Managing symptoms (0–10) | 1.16 (2.67) | 0.27 (2.84) | 2.03 | 0.044 |
| Health status | ||||
| Disability (0–3)a | 0.02 (0.13) | 0.04 (0.13) | −0.97 | 0.333 |
| Social/role activities limitations (0–4)a | −0.13 (0.68) | 0.02 (0.52) | −1.58 | 0.116 |
| Energy (0–5) | 0.41 (0.99) | 0.02 (1.06) | 2.37 | 0.019 |
| Psychological well-being (0–5) | 0.34 (0.81) | 0.09 (0.78) | 2.03 | 0.044 |
| Depressive symptom (0–5)a | −0.30 (0.68) | −0.05 (0.71) | −2.20 | 0.030 |
| Health distress (0–5)a | −0.32 (0.98) | −0.06 (1.09) | −1.56 | 0.122 |
| Pain and discomfort (0–10)a | −0.38 (3.10) | 0.16 (2.88) | −1.13 | 0.260 |
| Fatigue (0–10)a | −0.77 (2.69) | 0.10 (2.86) | −1.97 | 0.051 |
| Shortness of breath (0–10)a | 0.02 (1.80) | 0.06 (1.26) | −0.16 | 0.871 |
| Self-rated health (1–5)a | −0.10 (0.90) | 0.21 (0.68) | –2.41 | 0.017 |
| Health care services utilization | ||||
| General practitioner visits | −1.05 (8.53) | 0.71 (5.70) | −1.51 | 0.133 |
| Other health service visits | −1.04 (14.50) | −0.31 (5.12) | −0.42 | 0.679 |
| Emergency room visits | −0.14 (0.90) | 0.21 (1.67) | −1.65 | 0.101 |
| Number of days in hospital | 0.09 (2.38) | 0.60 (4.94) | −0.83 | 0.411 |
Notes: Mean change = mean score at 12-month – mean score at baseline; P value in italics mean P <0.05;a Lower score indicates better result.
Discussions
This study demonstrated that subjects who participated in this six-session CDSMP had a significant improvement in self-management behaviors, self-efficacy and some aspects of health status at the point of six months. These findings were similar to previous studies (Chan et al., 2011; Fu et al., 2003; Lorig et al., 1999; McLaughlin, 2019) and supported that older adults with lower educational level could also benefit from the CDSMP in Macao. The improvement in outcome measures in subjects in the study group can be maintained for one year, which was similar to previous studies (Barlow et al., 2005; Lorig et al., 2001; Salvatore et al., 2015). The findings of this longitudinal and quasi-experimental study supported that Chinese older adults with chronic disease could have long-term benefits from the CDSMP when comparing to the subjects who received usual care in the control group. This study provided important evidence for caring people with chronic disease.
The improvement in energy and psychological well-being of older adults in this study was much more obvious than other studies (Chan et al., 2011; Fu et al., 2003; Lorig et al., 2001). It was consistent with a recent study that participants had a significant increase in the psychological component of the Short Form Health Survey after the CDSMP (Qi et al., 2019). The participants of this study expressed that they have learnt from the program the skill of handling negative emotions and they have gained peer support from other older adults.
There was no decrease in disability and no improvement in self-rated health in subjects in the study group. Regarding the subjects in the control group, there was an increase in disability in the six-month and one-year assessment and a decline in self-rated health in the one-year assessment. The results of between-group comparison showed that the subjects in the study group had better self-rated health than those in the control group. These findings supported that subjects in the study group could maintain their physical condition after the CDSMP, but the general health conditions of older adults will worsen with age. The possible reason was that the subjects have improved their self-efficacy by continuing to practice self-management behaviors (such as exercises and cognitive symptom management) after the CDSMP to face their chronic health condition. It was supported by a previous study that high efficacy was associated with good self-rated health in older adults of Macao (Leong, 2014).
The effectiveness of the CDSMP in healthcare services utilization was inconsistent in various studies. There was a significant reduction in healthcare services utilization in the six-month (Fu et al., 2003; Hong et al., 2017; Lorig et al., 1999), one-year and two-year assessment (Lorig et al., 2001), but there were no significant changes in some other studies (Chan et al., 2011; Jaglal et al., 2014). The present study showed that there was a decreased trend but there was no significant difference in healthcare services utilization, and which was consistent with a similar study conducted in Hong Kong SAR for older adults (Chan et al., 2011). One possible reason was that the participants of this study were much older and most of them had three or more chronic diseases. The other reason was that due to the free healthcare system, older adults could access public healthcare services in Macao. A previous study (Leong, 2012) found that older adults were the main users of public health services in Macao. They had regular body checkup and primary care service in healthcare centers and they could have access to specialists by physicians’ referral, hence there was no effect on healthcare utilization. A meta-analysis study (Lederle & Bitzer, 2019) showed that there was a small effect of the CDSMP on healthcare utilization and there was only a reduction in unscheduled visits.
Recently, a study indicated that self-management of multiple chronic conditions by older adults was a complex process that required the alignment of many factors, such as acquiring health education, using financial resources, continuing engagement in health system and disease monitoring (Garnett et al., 2018). It was evident that the CDSMP provided an interactive learning opportunity for older adults to acquire health-related knowledge and practice the skills of utilizing social support, community health resources for problem solving and managing their chronic conditions. Older adults’ self-efficacy would have increased when they gained successful experiences by adopting action plan to solve their health problems. Subsequently, a virtuous circle would be established that older adults practicing more self-management behaviors would have their health status improved. Therefore, the older adults could benefit from the CDSMP.
Strengths and Limitations
This was the first controlled longitudinal study aimed to evaluate the effectiveness in health outcome and healthcare service utilization of the CDSMP in older adults in Chinese communities. Furthermore, this study provided the changes in pattern of measurement indicators over time by using linear mixed-effects modeling for repeated measures. The findings of the present study provided important evidence for chronic care of older adults.
There was no randomized allocation in the two groups. Subjects in the study group may be more willing to change their lifestyle since they were more motivated than those in the control group. Some positive outcomes may occur in the study group due to this bias. In addition, the study has been completed for a few years and the reproducibility of the study may be affected. Nevertheless, the results of this study are still of reference value for the chronic care due to limited related research in Chinese communities and the chronic care for older adults is still a big challenge for the Macao healthcare system.
Implications for Practice
Since the aging population has increased rapidly and most of the older adults are suffering from chronic illness, it is important to foster older adults to acquire self-management skills in order to increase their quality of life by overcoming their chronic conditions. The CDSMP was found to be effective to improve older adults’ self-management behaviors and health-related indicators for a longer period of time. The effect of the CDSMP on maintaining self-rated health of older adults is worth mentioning since self-rated health is an independent predictor of mortality rate in older adults (Ford et al., 2008; Giltay et al., 2012). Although the CDSMP cannot substitute for the healthcare service, it can be launched as a health promotion activity in community. A previous study indicated that the CDSMP is very cost-effective (Ahn et al., 2013) and the low drop-out rate of this study demonstrated that the CDSMP is suitable and worth adopting in Chinese communities. It is suggested that the CDSMP can be launched regularly in community centers or primary care settings and a referral mechanism by primary healthcare professionals should be established in the healthcare system in order to facilitate older adults with chronic disease to participate in this program.
Conclusions
This study confirmed that the community-dwelling older adults in Macao can acquire positive outcomes in self-management and health-related indicators from the CDSMP. The effect occurred at the point of six months and lasted for at least one year. It is suggested that the participants may apply the learnt skills to face their chronic conditions in their daily life. Hence, it is worth promoting this program in community.
Acknowledgments
The authors acknowledge The Salvation Army (Hong Kong) for its professional support to launch the CDSMP in Macao. We are grateful to Caritas de Macau, The Women’s General Association of Macau, General Union of Neighborhood Associations of Macao for their assistance in recruiting participants and providing venues for the delivery of the program. We also thank our students Hoi Tong LEI, Weng Ian LEI, Mei Ian CHAN, Mei I LAO for their assistance in data collection and Ms Kuan Ieong MAK for her efforts to proofread this article. Last but not least, we would like to express special thanks to the subjects who participated in this study.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Macao Foundation (3041/DSDSC/2011).
ORCID iD
Sok Man Leong https://orcid.org/0000-0002-4674-5521
References
- Ahn S. N., Basu R., Smith M. L., Jiang L., Lorig K., Whitelaw N., Ory M. G. (2013). The impact of chronic disease self-management programs: Healthcare savings through a community-based intervention. BMC Public Health, 13, 1141. 10.1186/1471-2458-13-1141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow J. H., Wright C. C., Turner A. P., Bancroft G. V. (2005). A 12-month follow-up study of self-management training for people with chronic disease: Are changes maintained over time? British Journal of Health Psychology, 10, 589–599. 10.1348/135910705X26317 [DOI] [PubMed] [Google Scholar]
- Chan, W. L. S., Hui, E., Chan, C., Cheung, D., Wong, S. K., Wong, R. P., Li, S. F., & Woo, J. (2011). Evaluation of chronic disease self-management programme (CDSMP) for older adults in Hong Kong. The Journal of Nutrition, Health & Aging, 15(3), 209–214. 10.1007/s12603-010-0257-9 [DOI] [PubMed] [Google Scholar]
- Ford J., Spallek M., Dobson A. (2008). Self-rated health and a healthy lifestyle are the most important predictors of survival in elderly women. Age and Ageing, 37, 194–200. 10.1093/ageing/afm171 [DOI] [PubMed] [Google Scholar]
- Fu, D., Fu, H., McGowan, P., Shen, Y., Zhu, L., Yang., H., Mao, J., Zhu, S., Ding, Y., & Wei, Z. (2003). Implementation and quantitative evaluation of chronic disease self-management programme in Shanghai, China: Randomized controlled trial. Bulletin of the World Health Organization, 81(3), 174–182. [PMC free article] [PubMed] [Google Scholar]
- Garnett A., Ploeg J., Markle-Reid M., Strachan P. H. (2018). Self-management of multiple chronic conditions by community-dwelling older adults: A concept analysis. SAGE Open Nursing, 4, 1–16. 10.1177/2377960817752471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giltay E. J., Vollaard A. M., Kromhout D. (2012). Self-rated health and physician-rated health as independent predictors of mortality in elderly men. Age and Ageing, 41, 165–171. 10.1093/ageing/afr161 [DOI] [PubMed] [Google Scholar]
- Hong, X., Wang, C. C., Qi, S. X., Qin, Z. Z., Chen, X. P., Zhou, H. R., Wang, Z. Y., & Xu, F. (2017). Effectiveness evaluation on chronic disease self-management program among patients with chronic disease in Nanjing community. Chinese Journal of Health Education, 33(9), 825–827. 10.16168/j.cnki.issn [DOI] [Google Scholar]
- Jaglal S. B., Guilcher S. J. T., Hawker G., Lou W., Salbach N. M., Manno M. M., Zwarenstein M. (2014). Impact of a chronic disease self-management program on health care utilization in rural communities: A retrospective cohort study using linked administrative data. BMC Health Services Research, 14, 198. 10.1186/1472-6963-14-198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiang Wu Nursing College of Macau. (2006). Research on the long-term care needs of the elderly in Macao.
- Lam C. L. K., Lauder I. J. (2000). The impact of chronic diseases on the health-related quality of life (HRQOL) of Chinese patients in primary care. Family Practice, 17(2), 159–166. 10.1093/fampra/17.2.159 [DOI] [PubMed] [Google Scholar]
- Lederle M., Bitzer E. (2019). A close look at lay-led self-management programs for chronic diseases and health care utilization: A systematic review and meta-analysis. GMS German Medical Science, 17, Doc03. 10.3205/000269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leong S. M. (2012). The health status and utilization of health care services of elderly people in Macau. Macau Journal of Nursing, 11(2), 23–24. [Google Scholar]
- Leong S. M. (2014). Relationship between social support, self-efficacy and self-rated health of community elderly in Macau. Macau Journal of Nursing, 13(2), 18–21. [Google Scholar]
- Leong S. M., Du P. (2018). The health-promoting lifestyle and its related factors of older adults in Macao. Chinese Journal of Gerontology, 38(23), 5851–5854. 10.3969/j.issn.1005-9202.2018.23.084 [DOI] [Google Scholar]
- Lorig, K. R., Ritter, P., Stewart, A. L., Sobel, D. S., Brown, B. W., Bandura, A., Gonzalez, V. M., Laurent, D. D., & Holman, H. R. (2001). Chronic disease self-management programme: 2 year health status and health care utilization outcomes. Medical Care, 39(11), 1217–1223. 10.1097/00005650-200111000-00008 [DOI] [PubMed] [Google Scholar]
- Lorig, K. R., Sobel, D. S., Stewart, A. L., Brown, B. W., Bandura, A., Ritter, P., Gonzalez, V. M., Laurent, D. D., & Holman, H. R. (1999). Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: A randomized trial. Medical Care, 37(1), 5–14. 10.1097/00005650-199901000-00003 [DOI] [PubMed] [Google Scholar]
- Macao Statistics and Census Bureau. (2014). Trends and challenges of aging population. [Google Scholar]
- McLaughlin R. (2019). The effects of a self-management programme (Stanford model) on adults in County Donegal with long term health conditions. International Journal of Integrated Care, 19(S1): A513. 10.5334/ijic.s3513 [DOI] [Google Scholar]
- Qi S. X., Wang C. C., Zhou H. R, Qin Z. Z., Chen X. P., Hong X. (2019). Effectiveness of chronic disease self-management on quality of life among patients with chronic disease. Chinese Journal of Health Education, 35(10), 885–889. 10.16168/j.cnki.issn.1002-9982.2019.10.005 [DOI] [Google Scholar]
- Research Group of “Macao Health Survey 2006”. (2008). Macao Health Survey 2006. Macao: Health Bureau of Macao SAR. [Google Scholar]
- Salvatore A. L., Ahn S. N., Jiang L., Lorig K., Ory M. G. (2015). National study of chronic disease self-management: 6-month and 12-month findings among cancer survivors and non-cancer survivors. Psycho-Oncology, 24, 1714–1722. 10.1002/pon.3783 [DOI] [PubMed] [Google Scholar]
- The Salvation Army. (2008). Chronic disease self-management programme: Leader’s manual.
- Tomioka M., Braun K. L., Compton M., Tanoue L. (2012). Adapting Stanford’s chronic disease self-management program to Hawaii’s multicultural population. The Gerontologist, 52(1), 121–132. 10.1093/geront/gnr054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo J., Hui E., Chan W., Cheung D., Chan C., Hui F. Y. (2009). Evaluation of chronic disease self-management programme for older adults in Hong Kong. Hong Kong: The Hong Kong Jockey Club. [DOI] [PubMed] [Google Scholar]
- Xu M. R., Qiang D. R., Zhou Y. H., Shi S. Y., Qin J. (2017). Evaluation of self-management on chronic diseases patients, Wujin District. Modern Preventive Medicine, 44(3), 462–465. [Google Scholar]