Abstract
This scoping review focuses on evidence gaps regarding the effects on health, social participation and life contexts of older people at the beginning of the COVID-19 pandemic. It is based on a systematic search strategy of the international literature covering a period between December 2019 and June 2020. The review is supplemented by a search of the websites of selected organisations in Germany (cut-off date: 29 June 2020). Search hits were differentiated by types of publication (empirical study, review, discussion paper). The contents were summarised in tabular form according to topic. The publications mainly discussed the high risks of suffering severe courses of COVID-19 faced by older people, specifically those belonging to certain subgroups. In addition, further main topics were the pandemic’s indirect impacts on physical and mental health, physical and cognitive functions and participation in society. Social isolation, loneliness, reduced levels of physical activity and difficulties in maintaining care were discussed as major health risks. Ageism was an issue that was addressed across all of the identified topics. The publications highlighted the need, but also the opportunity, for raising public awareness of the needs of older people in various life contexts. Publications pointed to the urgent need for research into the biological and social causes of older peoples’ high infection risk and how measures could be adapted in a differentiated manner (infection prevention and control measures, social support, medical and nursing care).
Keywords: COVID-19, PANDEMIC, SARS-COV-2, OLDER PEOPLE, SCOPING REVIEW
1. Introduction
People aged 60 years and older and, in particular, men aged 80 years and older or with pre-existing medical conditions are considered the main risk groups for a severe or fatal Coronavirus Disease 2019 (COVID-19); men are generally considered to be at greater risk than women [1–4]. As a vaccine and effective medication to treat COVID-19 were not available when the pandemic broke out, non-pharmaceutical interventions were key to containing the spread of SARS-CoV-2 and preventing the health system from becoming overwhelmed. As early as March 2020, a number of measures to limit physical contact between people were implemented, first in Italy and later across all European countries, including recommendations or regulations instructing those with respiratory symptoms to self-isolate, closure of schools, kindergartens and care facilities, and wide-ranging restrictions on movement and travel, even involving the enforcement of curfews [5]. To protect their elderly populations, Germany and other countries issued recommendations for visits to and contact with residents of long-term care facilities [6]. In addition, the pandemic made it increasingly difficult to maintain regular outpatient medical care as well as nursing care in the community and in long-term care facilities [7–10].
Against this background, it is to be expected that the COVID-19 pandemic has and will have a variety of consequences for the health and well-being of older people. This publication aims to offer a systematic overview of the situation facing older people during the first six months of the COVID-19 pandemic. The conceptual framework for this analysis is a scientific concept for public health monitoring in the population aged 65 and over [11, 12]. Based on the World Health Organization (WHO) Action Plan on Ageing and Health, three central fields of action and related topics were identified through a structured consensus process. These are: personal factors (physical and mental health, physical and cognitive functioning, health behaviour), activities/participation and environmental factors (health care, nursing care, physical and social environment) [11]. This article considers the effects of the COVID-19 pandemic during its initial phase on the three fields of action mentioned above [11–14]. On this basis, we also aim to identify the areas where obvious evidence gaps exist and to highlight issues that will require more in-depth analysis in the future.
2. Methodology
To gain a broad overview, a ‘scoping review’ was conducted based on the framework by Arksey and O’Malley [15] including the following steps: searching for and identifying relevant studies, study selection, charting the data, collating, summarising and reporting the results.
Identification of relevant studies and study selection
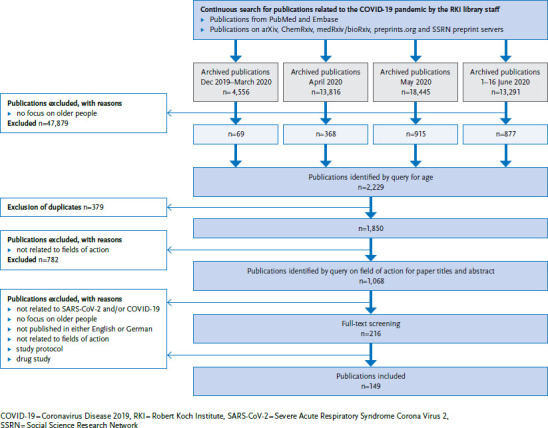
Since January 2020, the library team at the Robert Koch Institute (RKI) has conducted a continuous search of the international literature on the COVID-19 pandemic in the PubMed and Embase databases. For the database searches, two complexes of search terms were created and linked to identify relevant literature. New terms were continuously added to both complexes as needed (for example, ‘SARS-CoV-2’ was added to the complex of terms related to the virus when the initially nameless virus was named ‘Severe Acute Respiratory Syndrome Coronavirus 2’). Annex Table 1 shows the two complexes. In addition, the team also searched the following preprint servers: arXiv, ChemRxiv, medRxiv/bioRxiv, preprints.org and Social Science Research Network (SSRN). Annex Table 2 shows the search terms used here. All publications identified since 1 December 2019 are archived together with their citations in the reference manager EndNote and have been made available to all RKI staff (Figure 1).
Figure 1.
Flow chart for systematic publication selection
Source: Own diagram
The systematic search for this scoping review was based on publications identified up to 16 June 2020. At this time, four separate literature archives with the identified publications for different time periods were available (Figure 1), which, due to the size of these files, could not initially be transferred to a single database. Therefore, by means of a search in EndNote (keywords ‘aged’ or text words ‘aged’, ‘elder*’ or ‘older adult*’ in title/abstract), all citations focusing on the target group of older people were identified within the four separate archives. The authors then transferred hits from the four archives into a single literature database in EndNote and removed duplicates using an automatic procedure. In this literature database, separate searches were carried out for the three fields of action (personal factors, activities/social participation and environmental factors) (Annex Table 3). All citations identified in this way were screened independently by two persons per field: first, the title and abstract were checked, followed by the full text of the remaining relevant hits. Disagreements on whether to include a publication were resolved through discussion or by involving other members of the review team. For this two-stage review, the following exclusion criteria had been defined in advance: (1) unrelated to SARS-CoV-2 or COVID-19, (2) no focus on older people, (3) not published in English or German, (4) unrelated to one of the three fields of action mentioned above, (5) study protocol and (6) drug study.
In addition, the websites of preselected German organisations (e.g. professional societies, self-help organisations or research networks) were searched for publications related to the health of older people in connection with COVID-19 released up to and including 29 June 2020. A total of 14 organisations were selected due to their specific connection to the health of older people or to the health effects of the COVID-19 pandemic. Annex Table 4 contains a list of these organisations. Here too, relevant publications were selected independently by two persons taking into account the six predefined exclusion criteria.
Collating, summarising and reporting the results
The collated and summarised results were presented in tabular form. The results of the literature search in international databases (Table 1) and the results of the internet search on the websites of selected organisations in Germany were analysed separately (Table 2). To increase readability and avoid redundancies with the result table, the summary of the results is presented below without references.
Table 1.
Identified literature by field of action or health domain with classification of document types into specific reference areas: discussion papers [16–110], reviews [111–114] and empirical studies [115–164]
Source: Own Table
| Field of action or health domain | Content of included publications | Number of publications | Number of empirical studies [source] |
|---|---|---|---|
| Personal factors | |||
| Physical health | COVID-19 mortality of older people [93, 137, 138], older men [148, 154], hip fracture patients [150], people in nursing homes [115] | 7 | 6 [115, 137, 138, 148, 150, 154] |
| Heightened SARS-CoV-2 infection risk for people who live in care homes [134], who maintain family ties [97], or who do not receive information on current hygiene measures due to sensory limitations [22, 23] | 4 | 1 [134] | |
| Approaches to explain the high risk older people face when infected with SARS-CoV-2; role played by genetic, hormonal and immunological factors, as well as pre-existing conditions [26, 86, 90, 148, 154] | 52 | [148, 15] | |
| Scores to map biological age as a relevant COVID-19 mortality risk factor seem more appropriate than chronological age or sex [26, 113] | 2 | 0 | |
| Symptoms of older people with COVID-19 [82, 113, 151, 157, 163] | 5 | 3 [151, 157, 163] | |
| Effectiveness of vaccination [86] | 1 | 0 | |
| Medication as a risk factor for a severe COVID-19: antihypertensives [87], potential adverse interaction of long-term drug therapy for chronic diseases with hydroxychloroquine as a candidate for drug therapy to treat COVID-19 [156] | 2 | 1 [156] | |
| Worsening health behaviour as a risk for a deterioration of health [28], worsening of conditions especially due to physical inactivity [92], increase in the number of new cases of diabetes mellitus [136] | 3 | 1 [136] | |
| Health issues due to non-use of health care (e.g. follow-up appointments, emergency care) [125, 132] or limited access to health care [92] | 3 | 1 [132] | |
| Health issues due to social isolation or loneliness [65, 98, 113] or due to persistent feelings of fear and being at risk [92]: chronic stress triggered by this weakens the immune system [22, 65] | 4 | 0 | |
| Changes in the health of people with pre-existing conditions: neurodegenerative diseases [60], cardiovascular diseases [89], osteoporosis [99], stroke [102], Parkinson’s disease [25], cardiometabolic risk factors [90] | 6 | 0 | |
| Patients admitted as inpatients with fractures (broken bones) during the pandemic [131, 133], importance of prophylactic measures to prevent fractures during lockdown [164] | 3 | 3 [131, 133, 164] | |
| Deteriorated oral health with negative consequences for physical health [69, 73] | 2 | 0 | |
| Mental health | Incidence of various mental disorders or symptoms such as depression, anxiety disorders, post-traumatic stress disorders, adjustment disorders, sleep disorders, eating disorders, paranoid disorders and suicide due to loneliness and social isolation [22, 23, 28, 37, 38, 42, 63, 65, 98, 101, 103, 105, 112, 113, 145] | 15 | 1 [145] |
| Incidence of somatoform disorders, paranoid disorders, anxiety, distrust in the health system due to media reports (i.e. ‘information overload’) [22, 23, 101, 145, 155] | 5 | 2 [145, 155] | |
| Groups particularly at risk of mental health deterioration: nursing home residents, hospital patients (e.g. visiting bans), people living alone (e.g. with little social support), people with pre-existing mental health conditions and dementia patients [37, 38, 63, 65, 71, 101, 105, 124, 125, 145, 155] | 11 | 4 [124, 125, 145, 155] | |
| Underdiagnosis and inadequate treatment of mental (pre-)conditions due to limited health care and discrimination (‘ageism’) and its consequences [22, 23, 37, 38, 70, 71, 101, 105], e.g. worsening of pre-existing mental conditions | 8 | 0 | |
| Difficult implementation or non-compliance with hygiene measures due to mental illness [23] or due to overreactions caused by fear and anxiety [22] | 2 | 0 | |
| Majority report no feelings of depression, anxiety or stress [129, 147, 158, 159]; prevalence figures vary and are difficult to compare, highest rates of 37% for anxiety or depression symptoms according to PHQ-9 or GAD-7 instruments [147] | 4 | 4 [129, 147, 158, 159] | |
| Lower rates of depression and anxiety symptoms compared to younger adults [118, 129, 149], in people without vs. with chronic pre-existing conditions [129], men vs. women [129] | 3 | 3 [118, 129, 149] | |
| Higher levels of stress felt than younger people [129] or the general population [70] | 2 | 1 [129] | |
| Positive correlation between loneliness and psychological symptoms such as anxiety, depression or peritraumatic stress [158] | 1 | 1 [158] | |
| ‘Well-being’ as a factor granting resilience against the negative effects of the pandemic [140] | 1 | 1 [140] | |
| Physical functioning | Deterioration of physical functioning due to physical inactivity (especially in case of hospitalisation or in nursing home residents) [20] and loneliness [65, 113] | 3 | 0 |
| Association between frailty status and severe COVID-19 [81, 122, 161]; e.g. association with mortality [122, 161] | 3 | 2 [122, 161] | |
| Cognitive functioning | Deterioration of cognitive function (dementia) due to loneliness, isolation, less support and activation [22, 28, 30, 37, 38, 65, 103, 113] or poor mental health [65, 105] | 9 | 0 |
| Groups at particular risk of cognitive function deterioration: dementia patients, hospital patients (with or without COVID-19) and people after SARS-CoV-2 infection [32, 63, 124] | 3 | 1 [124] | |
| Cognitive impairment (dementia) causes misinformation and makes implementing hygiene measures difficult (e.g. social isolation) [22, 23, 38, 66, 84, 112], thus increasing the risk of a SARS-CoV-2 infection (especially in nursing homes) [84] | 6 | 0 | |
| Unclear link between dementia and the COVID-19 mortality risk [121, 122] | 2 | 2 [121, 122] | |
| Health behaviour | Pandemic could negatively impact health behaviour (e.g. less physical activity, unhealthy diet, more tobacco and alcohol consumption, unfavourable sleep patterns) [28, 65] | 2 | 0 |
| Lockdown measures lead to a decrease in physical activity [31, 92, 116, 127] | 4 | 2 [116, 127] | |
| For dietary habits, gender differences are evident, with women more likely to buy extra food and pay more attention to buying products for a balanced diet compared to men [117]; however, (online) shopping presents challenges, which could potentially lead to changes in eating habits [92, 153] | 3 | 2 [117, 153] | |
| It is assumed that the consumption of alcohol is increasing [91], yet one study found no such evidence [142] | 2 | 1 [142] | |
| Vaccination: people vaccinated against flu seem to be less likely to contract COVID-19 [141] | 1 | 1 [141] | |
| Following recommendations to contain the pandemic: older people make an effort to follow recommendations to avoid infection [119], but there are differences by age and education [117, 120] | 3 | 3 [117, 119, 120] | |
| Social participation and activities | |||
| Social distancing measures lead to a reduction in physical activity [20, 88, 100, 103, 104, 111, 116, 127, 152], e.g. reduced participation in activity programmes [127] | 9 | 3 [116, 127, 152] | |
| Development of video-based interventions to promote physical activity of older people at home [116] | 1 | 1 [116] | |
| Increased social isolation and/or loneliness due to restricted contact in nursing homes and in own home [21, 24, 31, 36, 45, 85, 98, 100, 103, 104, 111, 127, 152, 162] | 14 | 3 [127, 152, 162] | |
| Use of information technologies to reduce social isolation and loneliness or to maintain mental health [36, 57, 83, 104, 110, 111, 128], with so far unclear benefits [114, 152, 162] | 9 | 3 [128, 152, 162] | |
| Challenges and opportunities of the COVID-19 pandemic for older people [78], e.g. concerns about an exacerbation of social inequality (especially in rural areas) due to an unequal distribution of resources and access to new information technologies [61] or societal awareness of the concerns of older people [78] | 2 | 0 | |
| Increased age discrimination or exclusion of older people [46, 54, 98] | 3 | 0 | |
| Environmental factors | |||
| Health care | Care of patients with pain [94], with glioblastoma [160], with osteoporotic fractures [99], with hip fractures in hospital (surgical and non-operative, with/without COVID-19) [150], with head and neck tumours [95]; oral health and oral health care [69, 73], psychiatric care in the community [105] | 8 | 2 [150, 160] |
| Therapy for patients with breathing difficulties, lung function outcomes. Patient reported outcomes [139] | 1 | 1 [139] | |
| Criteria-based allocation of treatment (‘triage pathway’) for people with type 2 diabetes presenting foot ulcers [146] | 1 | 1 [146] | |
| Critical discussion of age as a triage criterion [33, 35] | 2 | 0 | |
| Care concepts under pandemic conditions: geriatric [34, 75, 113], geriatric-oncological [43, 55, 80] | 6 | 0 | |
| Barriers to stopping or reducing medication in a planned process (‘deprescribing’) and overcoming these barriers during the pandemic [47] | 1 | 0 | |
| Challenges with emergency care in hospitals under pandemic conditions [96] | 1 | 0 | |
| Recommendations for action on palliative care in nursing homes and at home [50, 68] | 2 | 0 | |
| Infection control practices in long-term care [16, 72, 106] | 3 | 0 | |
| Transmission and appropriateness of symptom-based screening in nursing homes [115, 130, 135, 143, 144] and assisted living [157] | 6 | 6 [115, 130, 135, 143, 144, 157] | |
| Specifics of testing strategies in older people [113] | 1 | 0 | |
| Contributions from different disciplines on how to manage the pandemic: geriatric research [83], dementia research [27], exclusion from therapy research [113], demography in the planning of non-pharmaceutical interventions in the pandemic in local and national contexts [44], forensics: post-mortem investigations to clarify unknown conditions of older people [40] | 5 | 0 | |
| Multifactorial interventions to strengthen the social and health system with the aim of ensuring well-being, prevention and access to health care [64] | 1 | 0 | |
| Rationing of limited health care resources: advance care planning, prioritisation, prognostic scoring systems, triage [51, 52, 74] | 3 | 0 | |
| Conditions of the health care system (e.g. number of hospital beds, staffing) play a decisive role in the mortality of COVID-19 patients, in addition to other factors (such as the proportion of > 65-year-olds) [126] | 1 | 1 [126] | |
| Establishment, implementation and evaluation of post-acute care centres for COVID-19 patients from hospitals, emergency departments, homes and nursing homes [67] | 1 | 0 | |
| Pandemic-related reconfiguration of family medicine [58] | 1 | 0 | |
| Adapted care concepts for older people [39, 76, 77], target group-specific education based on needs [79] | 4 | 0 | |
| Nursing care | High vulnerability of nursing home residents and spread of infections in nursing homes [17, 29, 41] | 3 | 0 |
| Public health activities of various cooperating actors to ensure appropriate care for older people [53] | 1 | 0 | |
| Problems in the care of people with psychiatric disorders or cognitive impairment (dementia): implementation of hygiene measures (work overload), ethics (patients’ rights), occupational safety for staff and others (infection control) [37, 66, 84, 112, 123], e.g. consent to SARS-CoV-2 testing, motor agitation, isolation measures, application of physical restraints and sedation | 5 | 1 [123] | |
| Task of health care providers: developing methods for identifying and taking action to overcome social isolation and loneliness [103] | 1 | 0 | |
| Implications of the pandemic for various settings in which older people are cared for [107] | 1 | 0 | |
| Physical environment | Lack of equipment and preparation for assisted living, lack of infection control, staffing [16] | 1 | 0 |
| Nursing home setting with particularly high risk, which requires intensive testing and infection control measures, adequate staffing and supervision to prevent neglect and violence as there is no social control by the family [56] | 1 | 0 | |
| Need to optimise communication channels between relatives and nursing homes during the pandemic [59] | 1 | 0 | |
| Vulnerability of older people in rural areas as access to social and health services is more difficult under pandemic conditions [61] | 1 | 0 | |
| Take into account assisted living settings in the planning of strategies to counter the pandemic [109] | 1 | 0 | |
| Social environment | Vulnerable social networks and social protection of older people under pandemic conditions [19] | 1 | 0 |
| Responsibility in social care in the UK in light of the pandemic [48] | 1 | 0 | |
| Senior-friendly service provision in the pandemic in all settings [62] and in the community [18], with a special focus on prevention from becoming a victim [49] | 3 | 0 | |
| Changed social environment and daily life, i.e. less social contact and support, due to social distancing measures [31, 65, 98], incl. approaches to overcoming these challenges [31, 65] | 3 | 0 | |
| Laws and decrees under pandemic conditions with positive effects for older people [108] | 1 | 0 | |
| Stereotypes and disparagement of the value of older people’s lives and proposals against age discrimination (‘ageism’) [46, 98] | 2 | 0 | |
COVID-19 = Coronavirus disease 2019, PHQ-9 = Nine-item Patient Health Questionnaire, GAD-7 = Generalised Anxiety Disorder Scale-7, SARS-CoV-2 = Severe Acute Respiratory Syndrome Corona-Virus 2
Table 2.
Contributions by national level organisations
Source: Own Table
| Organisation | Title [source] | Published | Topic |
|---|---|---|---|
| German National Association of Senior Citizens’ Organisations e.V. (BAGSO) | Protecting human lives – strengthening cohesion. BAGSO recommendations regarding the spread of the coronavirus [165] | 24.03.2020 | Equipment and support for people with recognised care needs in nursing homes and at home |
| Coronavirus epidemic in Germany: do not abandon people in care! BAGSO statement on the Day of the Older Generation on 1 April 2020 [169] | 30.03.2020 | Prevention of and services for older people experiencing social isolation | |
| End the social isolation of people in nursing homes! BAGSO’s urgent recommendations to politicians [170] | 27.04.2020 | Relaxation and harmonisation of social distancing restrictions | |
| Improve support for family caregivers during the coronavirus pandemic! BAGSO’s urgent recommendations to politicians [171] | 04.05.2020 | Support for family caregivers | |
| Visits to nursing homes: facilities need clear guidelines and more support. BAGSO issues call to the federal states – for the attention of the Federal Government [166] | 25.05.2020 | Uniform rules for social distancing restrictions in nursing homes and sufficient provision of protective equipment | |
| Visits to nursing homes: some federal states urgently need to make improvements. An interim assessment by BAGSO four weeks after the federal-state decision to allow such visits again [168] | 03.06.2020 | Relaxation and harmonisation of social distancing restrictions | |
| Ensure basic digital services in old people’s and nursing homes. BAGSO’s five demands [167] | 18.06.2020 | Better digital equipment for nursing homes | |
| Bundesinteressenvertretung für alte und pflegebetroffene Menschen e. V. (BIVA) | Coronavirus – effects on people with recognised care needs [173] | 12.03.2020 | Information for relatives on the rules at the beginning of the pandemic |
| Visiting restrictions in nursing homes due to the coronavirus crisis. BIVA position paper [172] | 26.03.2020 | Adequateness of social distancing restrictions for nursing home residents | |
| Coronavirus: increase the protection for nursing home residents! [175] | 31.03.2020 | Prevent the spread of COVID-19 infections in nursing homes through better equipment (e.g. protective gear) and regular testing for nursing staff | |
| Coronavirus crisis and the ‘real everyday practice of care’ in inpatient facilities for the elderly. Guest commentary by BIVA member Claus Völker [174] | 03.04.2020 | Opinion piece on the situation in nursing homes during the pandemic | |
| Nursing home residents still at risk – family caregivers are systemically relevant [176] | 12.05.2020 | Improve access to nursing homes for relatives | |
| Relaxation of bans on visits to old people’s and nursing homes insufficiently implemented [177] | 22.05.2020 | Reduction of social distancing restrictions in nursing homes | |
| Sobering survey result: insufficient options to visit nursing homes and the consequences of social isolation are severe [179] | 29.05.2020 | Reduction of social distancing restrictions in nursing homes, resume audits by medical services and home supervisors | |
| Visiting arrangements in retirement homes: making conflicts preventable [178] | 12.06.2020 | Implementation of the amended social distancing restrictions in nursing homes | |
| German Society for Gerontology (DGG) | Coronavirus: how older people can protect themselves or ‘no kiss for grandma’ [186] | 13.03.2020 | Prevention of COVID-19 infections among older people |
| COVID-19 and the elderly: geriatricians present measures to protect and care for the elderly [187] | 20.03.2020 | Protective measures and better care for older people | |
| Care bottleneck: geriatricians call for crisis concept for coronavirus risk group [188] | 20.03.2020 | Protect caregivers against infection in the context of COVID-19 | |
| Supplementary recommendations for geriatric patients in home care to the ‘Decisions on the allocation of resources in emergency and intensive care medicine in the context of the COVID 19 pandemic’ by the DIVI, DGINA, DGAI, DGIIN, DGP1, DGP 2, AEM [210] | 22.04.2020 | Allocation of resources in emergency and intensive care medicine in the context of the COVID-19 pandemic | |
| After the partial lifting of coronavirus restrictions, geriatricians recommend further protection of the elderly: ‘SARS-CoV-2 has not disappeared yet!’ [189] | 08.05.2020 | Relaxation of social distancing and application of same rules across Germany | |
| German Society of Gerontology and Geriatrics e.V. (DGGG) | Statement by the DGGG: facilitate psychotherapy via phone for elderly and vulnerable female patients during the coronavirus pandemic [191] | 18.03.2020 | Access to video appointments for elderly and vulnerable patients with mental illnesses |
| Statement by the German Society of Gerontology and Geriatrics on the COVID-19 pandemic [190] | 31.03.2020 | Targeted measures according to individual risks, not exclusively according to age | |
| Public communication and reporting on ‘Coronavirus & Age’: recommendations of the German Society of Gerontology and Geriatrics (DGGG), Section III (Social and Behavioural Gerontology) [197] | 01.04.2020 | Recommendations for public communication on age and COVID-19 | |
| Social hardship of older people in the wake of the COVID-19 pandemic: recommendation for the establishment, support and promotion of local emergency initiatives [199] | 07.04.2020 | Comprehensive establishment of local emergency aid programmes by municipalities | |
| Joint statement by the sections for Geriatric Medicine (II), Social and Behavioural Gerontology (III), Social Gerontology and Assistance for the Elderly (IV) of the German Society of Gerontology and Geriatrics (DGGG e.V.): enabling participation and a social life for older people despite the coronavirus pandemic [198] | 24.04.2020 | Promoting the self-determination, participation and social inclusion of older people | |
| Joint statement by the Social and Behavioural Gerontology (III) and Social Gerontology and Assistance for the Elderly (IV) Sections of the DGGG: participation and care for people with care needs during the coronavirus crisis and beyond [195] | 10.05.2020 | Participation and care for people with recognised care needs in the context of COVID-19 | |
| German Centre of Gerontology (DZA) | Old people are different, including in the coronavirus crisis [209] | 06.04.2020 | Providing a differentiated image of age, using non-age discriminating language |
| Age discrimination and images of age in the coronavirus crisis [208] | 07.04.2020 | Promoting the physical activity of older people | |
| Older people and their use of the internet. Implications for the coronavirus crisis [194] | 08.04.2020 | Minimising the negative effects of social distancing measures for older people | |
| Risks of bans on social contact, social support and voluntary work by and for older people [196] | 08.04.2020 | Improving the digital involvement of older people | |
| Physical activity of older people during the coronavirus crisis [211] | 08.04.2020 | Stronger orientation towards concrete risks in restrictions and support services | |
| German Alzheimer’s Association (DAlzG) | Coronavirus: considerations of the unique situation facing family members caring for dementia patients [180] | 13.03.2020 | Increasing support for family carers |
| Coronavirus crisis: regulations for visits to nursing homes [181] | 18.03.2020 | Information on social distancing in nursing homes | |
| Coronavirus: the German Alzheimer’s Association calls on politicians to take action [182] | 25.03.2020 | Support for family carers and people with dementia in their own homes | |
| Protect dementia patients! German Alzheimer’s Association calls for the easing of visiting bans to nursing homes as early as possible [183] | 05.05.2020 | Relaxation of visiting bans in nursing homes | |
| Visits to nursing homes: German Alzheimer’s Association calls for binding regulations for all facilities [185] | 12.06.2020 | Uniform visiting rules in nursing homes | |
| Closed day care facilities – are family caregivers funding the coronavirus bailout? [184] | 17.06.2020 | Support for family caregivers | |
| German Network for Evidence-based Medicine (EbM Network) | COVID-19 pandemic: there is no need to move that fast! No experiments with the elderly and chronically ill population without scientific monitoring [192] | 27.03.2020 | Systematic documentation and care research in the context of social isolation and visit bans |
| Coronavirus in German nursing homes – an evidence-free drama in three acts [193] | 28.04.2020 | Clinical-epidemiological database on COVID-19 through systematic testing in nursing homes, establishment of a registry | |
| Kuratorium Deutsche Altershilfe e.V. (KDA) | The COVID-19 pandemic and the situation of older people in Germany. A statement by the Kuratorium Deutsche Altershilfe (KDA) [200] | 07.04.2020 | Maintain and enable protection, participation and self-determination of older people and people in need of care |
| Social policy perils and missteps during the coronavirus pandemic. On the affirmative reception of coronavirus in the culture, spirit and soul of ‘Policies for the Elderly’ [205] | 14.05.2020 | Ensure self-determination and participation for older people despite COVID-19 social distancing measures | |
| Competence Network Public Health COVID-19 | Should older employees have to stay away from the workplace? Results of a systematic literature search (rapid scoping review) [206] | 24.04.2020 | Measures to protect older workers in the workplace |
| Social isolation as a mortality risk for older people: results of a systematic literature review (rapid scoping review) supplemented by a qualitative survey [207] | 18.05.2020 | Consequences of social isolation and loneliness for health in nursing homes and the lifting of social distancing measures | |
| Pflegeethik Initiative | Not allowed to live, not allowed to die [203] | 26.03.2020 | Proportionality of social distancing measures, positions taken by different professions on the topic of dying |
| General bans on visits to homes are inhumane!!!! [204] | 17.03.2020 | General bans on visits to nursing homes and their effects | |
| Wrong priorities set and ethical principles violated [202] | 15.04.2020 | Social distancing as compulsory care measures and the consequences for older people | |
| Urgent coronavirus statement: visiting bans in nursing homes are inhumane and disproportionate. Lift them immediately! [201] | 03.05.2020 | Social distancing measures are not proportionate, demand for immediate removal |
BAGSO = German National Association of Senior Citizens’ Organisations e.V., BIVA = Bundesinteressenvertretung für alte und pflegebetroffene Menschen e.V., DAlzG = German Alzheimer’s Association e.V., DGG = German Society for Gerontology e.V, DGGG = German Society of Gerontology and Geriatrics e.V., DZA = German Centre of Gerontology, EbM-Netzwerk = German Network for Evidence-Based Medicine e.V., KDA = Kuratorium Deutsche Altershilfe e.V., Pflegeethik Initiative = Pflegeethik Initiative Deutschland e.V., DIVI = Deutsche Interdisziplinäre Vereinigung für Intensiv- und Notfallmedizin e.V., DGINA = Deutsche Gesellschaft Interdisziplinäre Notfall- und Akutmedizin e.V., DGAI = Deutsche Gesellschaft für Anästhesiologie und Intensivmedizin e.V., DGIIN = German Society for Internal Intensive Care and Emergency Medicine e.V., DGP1 = German Society for Pneumology and Respiratory Medicine e.V., DGP 2 = German Society for Palliative Medicine e.V., AEM = Academy for Ethics in Medicine e.V., COVID-19 = coronavirus disease 2019, SARS-CoV-2 = Severe Acute Respiratory Syndrome Corona-Virus 2
Results from the international systematic literature search were sorted based on topic, methodology and main results. In addition, all included publications were categorised according to publication type (discussion paper, review or empirical study) and the publication’s country of origin or the first author documented.
Since the scoping review aimed to provide a summary of existing scientific knowledge, the next step was to categorise the main content described in the individual publications and assign them to the corresponding topic areas within the fields of action in accordance with the underlying scientific framework concept [11, 12]. For the field of action ‘participation and activities’, for example, nine papers discussed ‘Physical activities in the context of contact and movement restrictions’ and the results of the papers (or the line of argument in discussion papers) all referred to a reduction in physical activity levels following the implementation of social distancing measures. The tabulated summary of the results provides the publications sorted by content category. Likewise, the total number of publications and the proportion of empirical publications are shown by content category, health domain and field of action (Table 1).
Statements retrieved from selected German organisations were listed separately (Table 2) with title, reference and responsible organisation; the central topic was described using key words.
3. Results
Search result
By 16 June 2020, a total of 50,108 publications on SARS-CoV-2 infections or COVID-19 had been archived in four separate literature databases at the RKI (Figure 1). Of these, 47,879 publications were excluded via search query in EndNote as they were not focused on older people. Of the remaining 2,229 publications, 379 duplicates were excluded using an automated procedure. The remaining 1,850 publications formed the basis of the systematic research. The initial search for the fields of action in the literature database using EndNote resulted in a total of 1,068 hits (for all fields of action). The first review (title and abstract) led to the exclusion of 852 publications; the full texts of 216 publications were checked for inclusion.
A total of 149 publications were included for this paper. Of these, 95 were discussion papers [16–110], four reviews [111–114] and 50 empirical studies [115–164]. A total of 77 publications were identified for the field of action ‘personal factors’, 71 for ‘environmental factors’ and 26 for ‘participation and activity’. Some publications were relevant for several fields of action and their results have therefore been included under several fields of action.
The 149 publications came from the following 26 countries: 52 from the USA [16, 18, 24, 30, 31, 39, 42, 49, 51, 52, 56, 57, 59–62, 73, 77–80, 83, 85, 91–93, 95–98, 100, 103, 104, 107–112, 115, 117–119, 123, 135, 143, 144, 149, 152, 157, 160, 162], 13 from China [36, 72, 102, 105, 120, 137–139, 147, 153, 154, 163, 164], 13 from Italy [26, 33, 34, 40, 41, 43, 55, 58, 121, 131, 141, 146, 148], ten from the United Kingdom [21, 29, 44, 48, 63, 89, 113, 130, 136, 161], eight from Canada [17, 20, 45, 47, 54, 66, 94, 156], seven from Spain [67, 74, 90, 128, 129, 140, 150], six from India [22, 23, 35, 99, 145, 155], five from Germany [46, 53, 86, 124, 132], five from Switzerland [32, 68, 76, 81, 82], four from Australia [38, 101, 142, 159], four from Brazil [71, 87, 88, 125], two from Bangladesh [64, 75], two from Belgium [122, 133], two from France [37, 127], two from Ireland [84, 114], two from Israel [70, 158], two from Norway [50, 151], two from Taiwan [65, 106] and one publication each from Chile [69], Ghana [19], Japan [116], the Philippines [28], Thailand [25], Turkey [27], Hungary [134] and Vietnam [126].
The narrative synthesis revealed different topics for the different fields of action, which are listed in Table 1 together with the associated literature. The aim of this scoping review was not providing a detailed analysis of the results.
Field of action ‘Personal factors’
There were 77 hits for the ‘personal factors’ field of action. These included 37 discussion papers [20, 22, 23, 25, 26, 28, 30–32, 37, 38, 42, 60, 63, 65, 66, 69–71, 73, 81, 82, 84, 86, 87, 89–93, 97–99, 101–103, 105], two reviews [112, 113] and 38 empirical studies [115–122, 124, 125, 127, 129, 131–134, 136–138, 140–142, 145, 147–151, 153–159, 161, 163, 164].
For physical health, some papers described specific subgroups at particularly high risk of suffering a severe or fatal COVID-19 and highlighted that biological rather than chronological age should be used to assess a person’s risk of suffering severe illness as a result of contracting COVID-19. Reviews discussed the genetic, hormonal and immunological factors potentially contributing to the higher risks faced by older people following an infection with SARS-CoV-2. Publications emphasized the need for further research to better understand age-specific changes to the immune system, also regarding the effectiveness of vaccinating older people against COVID-19. Case studies show that older persons may develop atypical symptoms of COVID-19 (i.e. other symptoms may be present). Reduced levels of physical activity, social isolation and loneliness, as well as changes to overall medical care brought about by the COVID-19 pandemic are expected to lead to a deterioration in the physical health of older people. This risk is believed to be particularly great for older people suffering from cancers, Parkinson’s disease, dementia, cardiovascular diseases or osteoporosis. The oral health of older people could also deteriorate. A modelling study concluded that continued physical inactivity in otherwise active, prediabetic older people could lead to an increased incidence of diabetes. An empirical study on emergency neurological care to older people during the COVID-19 pandemic indicated worsened prognoses due to older people delaying seeking medical care.
For the ‘mental health’ domain, some publications expressed the fear that pandemic-related loneliness and social isolation could have serious effects. An increase in the incidence of various psychological disorders and symptoms is expected, especially in patients with pre-existing mental illnesses or dementia, and those living in nursing homes or who are admitted to hospital. Limited access to the health care system as well as intensive media coverage of the pandemic that, at times, features negative images of old age could amplify this. On the other hand, a majority of older people reported good mental health, especially compared to younger adults, in the early stages of the COVID-19 pandemic. However, those older people who suffer more pronounced feelings of loneliness reported more symptoms of anxiety and depression; this was also the case for those with chronic conditions.
In the ‘physical functioning’ domain, it is assumed that physical inactivity due to frequent sitting or lying down as well as loneliness will lead to a deterioration in physical functioning. Frailty is considered a risk factor for more severe and even fatal outcomes of a SARS-CoV-2 infection.
Loneliness, isolation, as well as less support and activation are expected to lead to a deterioration in ‘cognitive functioning’, especially in dementia sufferers, hospitalised patients and those who become infected with SARS-CoV-2. People suffering cognitive impairments often find it difficult to understand and implement the recommended hygiene measures, putting them at an increased risk of contracting SARS-CoV-2 (especially nursing home residents). Based on the available study data, it cannot be determined to what extent dementia increases the COVID-19 mortality risk.
For the ‘health behaviour’ domain, there are discussions about how social distancing reduces physical activity, promoting the loss of muscle and endurance and the increase of frailty. With regard to nutrition, older people were described as having difficulty obtaining sufficient healthy food. With regard to alcohol consumption, there is concern that the pandemic could lead to an increase in abuse. However, compared to younger people, older people were less likely to have increased their alcohol consumption during the pandemic. An ecological study found a negative correlation at the regional level between COVID-19 morbidity rates and flu vaccination take-up among older people in the previous year. Therefore, low COVID-19 rates were found in places where many people had received a flu vaccination and vice versa. It was also found that older people with low education levels were less likely to follow infection prevention measures than those with a higher education; likewise, men were less likely than women to follow these measures.
Field of action ‘Participation and activity’
A total of 26 publications were assigned to the field of action ‘participation and activity’. Of these, 19 were discussion papers [20, 21, 24, 31, 36, 45, 46, 54, 57, 61, 78, 83, 85, 88, 98, 100, 103, 104, 110], two reviews [111, 114] and five empirical studies [116, 127, 128, 152, 162].
These studies were focused on the health consequences of containment measures related to the COVID-19 pandemic, specifically social distancing and movement restrictions, for older people. The majority of the papers in this field highlighted a potentially increased risk of social isolation and loneliness for older people – both in nursing homes as well as those living in their own homes – as a result of social distancing measures. Against this backdrop, some papers discussed the role of different professional groups (for example, social workers and health professionals) and public health care, as well as the potential benefits of information technologies. In order to avoid the social isolation of older people, two studies analysed programmes providing telephone contact. The results showed a high level of satisfaction with the service. In contrast, a Cochrane Rapid Review found no evidence that video calls with older people can reduce social isolation, loneliness or symptoms of depression, but the number of studies and the reliability of the evidence were low.
Generally, the pandemic was described as a challenge for older people. Some publications dealt with the blanket classification of older people as a risk group and described their increased stigmatisation and even discrimination as possible consequences. In addition to social isolation, other challenges of the pandemic included financial losses, temporary loss of support and increased social inequality. Individual publications also described opportunities, such as the increased use and improved handling of technology, the strengthening of family networks or increased social awareness of the concerns of the elderly.
Field of action ‘Environmental factors’
A total of 71 hits were found for the ‘environmental factors’ field of action. Of these, 57 were discussion papers [16–19, 27, 29, 31, 33–35, 37, 39–41, 43, 44, 46–53, 55, 56, 58, 59, 61, 62, 64–69, 72–77, 79, 80, 83, 84, 94–96, 98, 99, 103, 105–109], two were reviews [112, 113] and 12 empirical studies [115, 123, 126, 130, 135, 139, 143, 144, 146, 150, 157, 160].
The publications considered the settings in which older people live, receive care and how they have been altered by the pandemic. Several empirical contributions analysed infection outbreaks in nursing homes and assisted living settings. Measures of infection control in health care facilities were discussed and suggestions made for coping with social isolation, boredom, reduced contact and quarantine measures. While publications outlined that, as a group, older people have a greater need for protection and support, it remains important to prevent social isolation and ensure the provision of health care services and social support in nursing homes and home care settings. This would require models for cross-sectoral care and the follow-up care of elderly COVID-19 patients. Some publications analysed the challenges health care systems were facing due to the pandemic regarding specific conditions such as hip fractures.
Health care professionals face major challenges in terms of occupational health and safety and workload, especially when caring for people with mental illness or cognitive impairment. Issues related to limited health care resources (including triage and prioritisation), but also palliative care, stereotyping and ageism are also addressed. Issues of social care and security as well as the impact of laws and regulations on older people are also discussed.
Contributions by organisations concerning the pandemic and older people in Germany
Until 29 June 2020, contributions related to the pandemic and older people were identified on the websites of 13 of the 14 organisations selected. Of the 57 contributions identified, 47 contributions from a total of ten organisations were included in this review [165–211]. They include statements, comments and recommendations related to (1) infection protection for residents and carers in nursing homes; (2) the equipment provided to nursing homes (e.g. with protective equipment, IT infrastructure); (3) visiting bans and restrictions; (4) the situation facing family caregivers in the home; and (5) the public perception of older people in the context of the COVID-19 pandemic. Table 2 provides an overview of these hits.
The contributions on visiting restrictions addressed the changes that took place during the course of the relaxation of social distancing measures, which started later for nursing home residents compared to other groups. In the context of visiting bans, older people’s risk of social isolation and the potential negative consequences were highlighted. Many contributions criticised the vastly different rules that were applied depending on the federal state and the differences regarding the relaxation of restrictions in nursing homes. The situation for family caregivers was also addressed, for example the burdens caused by a lack of care services such as day care facilities, the difficulties for family caregivers who work and the unique burdens placed on relatives caring for people with dementia. Other topics include the demand for a differentiated picture of older people, for example with regard to the risks of SARS-CoV-2 infection, and the avoidance of ageism.
4. Discussion
This scoping review aimed to provide an overview of international and German publications on the direct and indirect effects of the COVID-19 pandemic on the health of older people during the first six months of 2020. The main aim of this evaluation was to identify gaps in the evidence concerning the initial phases of the COVID-19 pandemic and, thus, areas requiring further research. Based on a biopsychosocial understanding of health and guided by the public health framework of the WHO Action Plan on Ageing and Health, the effects of the COVID-19 pandemic on the three fields of action – personal factors, participation/activities and environmental factors – were considered [11, 12, 14].
Only a very small proportion of the extremely high number of publications found for the first six months of the COVID-19 pandemic related specifically to older people’s health. The publication hits reveal serious impacts of the COVID-19 pandemic on the health and well-being of older people in all three fields of action and the associated health domains. However, in the initial stages of the COVID-19 pandemic, discussion paper (e.g. statements, position papers) predominated overall, while literature reviews (4/149) and empirical studies (50/149) accounted for only a third of hits. The distribution of empirical studies among the fields of action was skewed, each accounting for just under 20% in the ‘environmental factors’ and ‘participation/activities’ fields of action compared to 49% in the ‘personal factors’ field of action.
Many of the empirical studies were based on cross-sectional online surveys with small convenience samples without any claim to representativeness [e.g. 117, 119, 140, 149, 158, 159], case series [e.g. 132, 133, 138, 150, 154, 163, 164] or individual case studies [e.g. 151, 161]. These studies have only limited validity since other sampling strategies are needed for older and very old people with health impairments, for example, nursing home residents [212–214]. In addition, there is an urgent need for representative population-based studies of older people living at home in different living contexts (e.g. people living alone in private households with different support and care needs, people with different levels of care dependency, family caregivers) in order to assess the consequences of the pandemic for older people. Here, the evaluations of epidemiological data in Germany collected at the RKI during the course of the pandemic (e.g. GEDA 2019/2020-EHIS, COSMO60+, RKI-Corona-Monitoring, MonAge/Health 65+) can contribute to describing the well-being and health status of older people before and during the pandemic [e.g. 215, 216].
Considering the limited time period that was covered by the search (1 December 2019 to 16 June 2020), including only the initial months of the pandemic, it seems plausible that empirical data are predominantly available from countries that were heavily affected early on in the pandemic, such as China [120, 137–139, 147, 153, 154, 163, 164], Italy [121, 131, 141, 146, 148] and Spain [128, 129, 140, 150]. This is especially true for empirical studies analysing nursing homes. Only two out of the 50 empirical studies came from Germany, and both analysed medical care. A point to take into account is that continuous data collection, which is common in other countries, for example in US nursing homes with the Resident Assessment Instrument (RAI), does not take place in Germany. During the pandemic, it was either not possible to collect data in German nursing homes or only possible under difficult conditions [192]. Mandatory documentation requirements were suspended in nursing homes in Germany. In addition, visits and monitoring by the Health Insurance Medical Service (MDK) and internal supervision were drastically reduced. This also applied to visits by physicians. There was thus a lack of social control and information on the quality of care during the pandemic is limited [193]. The same applies to the frequency with which patients were sedated, measures that deprive patients of their freedom were applied, or challenging behaviour in dementia patients occurred. As of the reporting date, there were no empirical data available on the situation in home care from the perspective of those affected, care staff or family caregivers. Such studies are, however, now also available for Germany. An overview of the available evidence is being compiled by the Competence Network Public Health COVID-19. Empirical data on physical health that were identified in the research period are largely limited to the observation of the high risk for a severe COVID-19 for particularly vulnerable groups of older people, including older people in nursing homes and frail older people who have undergone emergency hospitalisation following a hip fracture. In general, the situations faced by older people in different countries are certainly similar. However, due to the differences in health care systems between countries, not all findings, especially regarding limited health care during the COVID-19 pandemic, are directly applicable to the situation in Germany.
Overall, men seem to run a higher risk than women of suffering a severe COVID-19. Very few empirical studies on the possible indirect effects of the pandemic on the physical health of older people were available during the research period. The results indicate that fears of negative health consequences due to reduced physical activity resulting from social distancing measures, but also due to a delayed access to medical care, could prove true. Initial empirical studies on the impacts of the pandemic on older people’s mental health appear not to confirm the blanket expectation of negative consequences [217, 218]. However, during the initial phases of the COVID-19 pandemic, no data on the potential longer-term consequences were yet available.
During the research period, no empirical data were available on the provision of medical care to older COVID-19 patients, nor for acute medical care or for medical and nursing follow-up care for older people recovering from COVID-19. Similarly, no empirical data were identified for assessing how the pandemic impacted the quality of outpatient and inpatient medical care for multimorbid or frail older people, or for developing quality standards. The extent of the short- and medium-term health consequences of the pandemic for older people also remains unclear. Such consequences would include a deterioration in the physical and mental health, as well as the physical and cognitive functions, of older people in nursing homes and private households. Equally unclear is how cause-specific excess mortality will develop and what changes in mortality will occur by place of death. Regarding the vaccination against COVID-19, more research is needed to determine the effectiveness of the various available vaccines, especially in frail and very old people.
A central question, which is also increasingly being discussed in international publications [e.g. 219], is how to encourage empirical research on the above-mentioned questions, in particular research requiring personal contact. There will also be a need to clarify the options for analysing the consequences of COVID-19 based on the data provided by official statistics, routine data and epidemiological studies. To meet these challenges, ideally, a publicly accessible online repository (i.e. a scientific document server) for the systematic compilation of results produced by empirical studies concerning older people will become available, such as the one set up for long-term care (Example: LTC-COVID).
Numerous publications highlighted the fact that the COVID-19 pandemic had made social tendencies towards age discrimination visible, and this issue was addressed across fields of action and health domains. Blanket risk assessments and medical triage of COVID-19 patients on the basis of chronological age were mentioned, as was the indiscriminate application of measures to restrict contact and mobility. Some contributions also warned against paternalistic attitudes indicating expectations on how older people should behave (e.g. the demand for self-isolation), potentially limiting their freedom of choice [46, 54]. There were calls for a social discourse that recognises the heterogeneity of old people as a group and adapts medical, nursing and social care structures to the largely diverse needs of older people and particularly vulnerable groups (e.g. people in need of care, those who are socially isolated or physically and cognitively impaired). Including new technologies and digital media in a process of adaptation that leads to the creation of appropriate infrastructures and services at the individual and municipal level was seen as a challenge, but also as an opportunity.
This scoping review has its strengths and limitations. The search was conducted for the period from 1 December 2019 to 16 June 2020 in literature archives prepared by the RKI and thus refers exclusively to the initial phase of the COVID-19 pandemic. The systematic search relied on the two most important medical and health science databases, PubMed and Embase, as well as several preprint servers. The search terms were broadly discussed and agreed upon by the authors and included keywords as well as free text terms. To provide findings that reflect the situation in Germany, national contributions via the websites of relevant organisations were included in addition to the literature search. For our study objective, i.e. to provide a systematic overview of the current discourse on the situation of older people during the initial stages of the COVID-19 pandemic, this search strategy seems suitable, but does not claim to be exhaustive. An important limitation of our analysis is that the quality of the studies included was not assessed. However, the aim of the review was to take account of the topics and issues being discussed and not to assess the study results. Furthermore, no quality assessment tools are available to judge the quality of discussion papers, which make up the majority of the included papers.
Conclusion
The results of this systematic literature review up to June 2020 show that a wide range of direct and indirect effects of the COVID-19 pandemic on the health and well-being of older people can already be expected even during the initial stages of the pandemic. There is an urgent need for empirical research, especially implementation and intervention research, that addresses both infection prevention and control as well as the impact of containment measures on older people in a wide range of life situations throughout the COVID-19 pandemic. Individual (intrinsic) health, functional and social resources and external contextual factors, such as living circumstances, medical and nursing care and social support services, must be taken into account. During the COVID-19 pandemic, it has become clear that continuous and systematic health reporting for the population aged 65 and older is needed; it must also be able to take into account the heterogeneity of this age group. For this purpose, a basis of data needs to be established that can be used in a low-threshold manner and enable timely analyses. The COVID-19 pandemic has shown the danger of a generalising and partly discriminatory approach regarding age. The reality of demographic change requires a differentiated and future-oriented approach to this topic in all areas of society.
Key statements
Sociodemographic factors and life contexts influence an older person’s risk of suffering a severe course of COVID-19.
Social distancing measures likely increase the risk of social isolation, loneliness and physical inactivity among older people, with negative consequences for health and functioning.
Infection prevention and control measures, social support, medical and nursing care must be adapted to the needs of older people in specific life contexts and their life situation.
The COVID-19 pandemic highlights the threat of age discrimination and the need to raise societal awareness of the fact that older people form a heterogeneous group.
There is an urgent need of research on the effects of non-pharmaceutical interventions to protect older people.
Acknowledgements
We would like to thank the staff at the RKI library for their continuous efforts to search and provide the available literature. In addition, we would like to thank Denise Ducks for her meticulous work in helping to document the systematic search, manage literature and compile the bibliography.
Annex Table 1.
Literature databases and search strings used by library staff at the Robert Koch Institute to identify publications on SARS-CoV-2 and COVID-19 (as of 16 June 2020)
Source: Own Table
| PubMed |
|
| Embase |
|
Annex Table 2.
Preprint servers and the respective search strings used by the library staff of the Robert Koch Institute to identify publications on SARS-CoV-2 and COVID-19 (as of 16 June 2020)
Source: Own Table
Annex Table 3.
Search strings used per field of action
Source: Own Table
|
‘Environmental factors’ field of action:
(“Social Environment”[MeSH] OR “Social Support”[Mesh] OR “social environment” [TIAB] OR environment*[TIAB] OR “social support”[TIAB] OR “health care”[TIAB] OR “Health Services”[MeSH] OR “health service*”[TIAB] OR “Nursing Care”[MeSH] OR “nursing care”[TIAB] OR “Residence Characteristics”[MeSH]) |
|
‘Participation’ field of action:
(“social participation”[MeSH] OR “Social Isolation”[MeSH] OR “Leisure Ac-tivities”[MAJR] OR participation[TIAB] OR participat*[TIAB] OR “Activities of Daily Living”[MeSH] OR activit*[TIAB] OR inclusion[TIAB] OR “Health Literacy” [MeSH] OR “health literacy”[TIAB] OR “Health Behavior” [MeSH] OR “Health Behavior”[TIAB] OR “Health Behaviour” [TIAB] OR “Aging in Place”[TIAB]) |
|
‘Personal factors’ field of action:
(health[MeSH] OR health*[TIAB] OR “life expectancy”[MeSH] OR life expectancy[TIAB] OR mortality[MeSH] OR mortality [TIAB] OR “mental health”[MeSH] OR “mental health”[TIAB] OR depression[MeSH] OR depress*[TIAB] OR anxiety[MeSH] OR anx*[TIAB] OR suicide[MeSH] OR suicid*[TIAB] OR frailty [MeSH] OR frail*[TIAB] OR “physical function*”[TIAB] OR functioning[TIAB] OR cognition[MeSH] OR cognit*[TIAB] OR memory[MeSH] OR memory[TIAB] OR dementia [MeSH] OR dementia[TIAB] OR “health behav-ior”[MeSH] OR “health behav*”[TIAB] OR “health-related behav*”[TIAB] OR lifestyle[TIAB] OR “alcohol drinking”[MeSH] OR alcohol [TIAB] OR smoking[MeSH] OR smok*[TIAB] OR exercise [MeSH] OR exercise[TIAB] OR “diet, healthy”[MeSH] OR “healthy diet*”[TIAB]) OR sleep[MeSH] OR sleep[TIAB]) |
Annex Table 4.
List of selected German organisations
Source: Own Table
| Federal Association of Senior Citizens’ Organisations e.V.
(www.bagso.de) Bundesinteressenvertretung für alte und pflegebetroffene Menschen e.V. (www.biva.de) German Alzheimer’s Association e.V. Self-Help Dementia (www.deutsche-alzheimer.de) German Society of Geriatrics e.V. (www.dggeriatrie.de) German Society of Gerontology and Geriatrics e.V. (www.dggg-online.de) German Society for Nursing Science e.V. (www.dg-pflegewissenschaft.de) German Society for General and Family Medicine e.V. (www.degam.de) German Society for Infectiology e.V. (www.dgi-net.de) German Society for Palliative Medicine e.V. (www.dgpalliativmedizin.de) German Network for Evidence-Based Medicine e.V. (www.ebm-netzwerk.de) German Centre of Gerontology (www.dza.de/informationsdienste.html) Competence Network Public Health COVID-19 (www.public-health-COVID19.de) Kuratorium Deutsche Altershilfe e.V. (www.kda.de) Pflegeethik Initiative Deutschland e.V. (www.pflegeethik-initiative.de) |
Funding Statement
This publication was prepared within the ‘Extension of the existing RKI monitoring by including the very old and older people with health impairments’ project (MonAge; funding code: ZMVI1-2518FSB410) that is funded from the Federal Ministry of Health (Beate Gaertner). The other authors received no additional funding for this publication.
Footnotes
The German version of the article is available at: www.rki.de/journalhealthmonitoring
Conflicts of interest
The authors declared no conflicts of interest.
Disclaimer
Note: External contributions do not necessarily reflect the opinions of the Robert Koch Institute
References
- 1.Robert Koch-Institut (RKI) (2020) Informationen und Hilfestellungen für Personen mit einem höheren Risiko für einen schweren COVID-19-Krankheitsverlauf. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Risikogruppen.html (As at 13.05.2020)
- 2.Bundeszentrale für gesundheitliche Aufklärung (BZgA) (2020) Ältere Menschen und Corona. (03.04.2020). https://www.bzga.de/presse/pressemitteilungen/2020-04-03-aeltere-menschen-und-corona/ (As at 30.04.2020)
- 3.World Health Organization (WHO) (2020) Statement – Older people are at highest risk from COVID-19, but all must act to prevent community spread. https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/statements/statement-older-people-are-at-highest-risk-from-covid-19,-but-all-must-act-to-prevent-community-spread (As at 02.04.2020)
- 4.Reilev M, Kristensen KB, Pottegard A, et al. (2020) Characteristics and predictors of hospitalization and death in the first 11 122 cases with a positive RT-PCR test for SARS-CoV-2 in Denmark: a nationwide cohort. Int J Epidemiol 49(5):1468–1481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flaxman S, Mishra S, Gandy A, et al. (2020) Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature 584(7820):257–261 [DOI] [PubMed] [Google Scholar]
- 6.Die Bundesregierung (2020) Pressekonferenz von Bundeskanzlerin Merkel zu Maßnahmen der Bundesregierung im Zusammenhang mit dem Coronavirus. https://www.bundesregierung.de/breg-de/suche/pressekonferenz-von-bundeskanzlerin-merkel-zu-massnahmen-der-bundesregierung-im-zusammenhang-mit-dem-coronavirus-1731022 (As at 17.09.2020)
- 7.Blankenfeld H, Kaduszkiewicz H, Kochen MM, et al. (2020) Neues Coronavirus (SARS-CoV-2) – Informationen für die hausärztliche Praxis. DEGAM S1-Handlungsempfehlung (AWMF-Register-Nr. 053–054). Version 12. Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin e. V. (DEGAM), Ulm. https://www.awmf.org/uploads/tx_szleitlinien/054-054l_S1_Neues_CORONA_Virus_2020-06_01.pdf (As at 30.06.2020)
- 8.Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin (DEGAM), Zentralinstitut für die Kassenärztliche Versorgung in Deutschland (Zi) (2020) Anforderungen an die Organisation der ambulanten hausärztlichen Versorgung während der COVID-19-Pandemie. https://www.zi.de/fileadmin/images/content/PMs/Zi_DEGAM_Versorgungsplanung_2020-05-06_final.pdf (As at 20.06.2020)
- 9.World Health Organization (WHO) (2020) Rapid assessment of service delivery for NCDs during the COVID-19 pandemic. https://www.who.int/publications/m/item/rapid-assessment-of-service-delivery-for-ncds-during-the-covid-19-pandemic (As at 20.06.2020)
- 10.World Health Organization (WHO) (2020) Statement – Invest in the overlooked and unsung: build sustainable people-centred long-term care in the wake of COVID-19. https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/statements/statement-invest-in-the-over-looked-and-unsung-build-sustainable-people-centred-long-term-care-in-the-wake-of-covid-19 (As at 20.06.2020)
- 11.Grube M, Fuchs J, Meyer G, et al. (2017) Entwicklung eines Rahmenkonzepts für ein Public-Health-Monitoring der Bevölkerung ab 65 Jahren. Bundesgesundheitsbl 60(8):879–882 [DOI] [PubMed] [Google Scholar]
- 12.Grube MM, Möhler R, Fuchs J, et al. (2019) Indicator-based public health monitoring in old age in OECD member countries: a scoping review. BMC Public Health 19(1):1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization (WHO) (2020) International Classification of Functioning, Disability and Health (ICF). https://www.who.int/classifications/icf/en/ (As at 20.06.2020)
- 14.Beard JR, Officer A, de Carvalho IA, et al. (2016) The World report on ageing and health: a policy framework for healthy ageing. Lancet 387(10033):2145–2154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arksey H, O’Malley L. (2005) Scoping studies: towards a methodological framework. Int J Soc Res Methodol 8(1):19–32 [Google Scholar]
- 16.American Geriatrics Society (AGS) (2020) American Geriatrics Society (AGS) Policy Brief: COVID-19 and Assisted Living Facilities. J Am Geriatr Soc 68(6):1131–1135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Andrew M, Searle SD, McElhaney JE, et al. (2020) COVID-19, frailty and long-term care: Implications for policy and practice. J Infect Dev Ctries 14(5):428–432 [DOI] [PubMed] [Google Scholar]
- 18.Angel JL, Mudrazija S. (2020) Local Government Efforts to Mitigate the Novel Coronavirus Pandemic among Older Adults. J Aging Soc Policy 32(4–5):439–449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arthur-Holmes F, Agyemang-Duah W. (2020) Reaching older adults during the COVID-19 pandemic through social networks and Social Security Schemes in Ghana: Lessons for considerations. J Gerontol Soc Work 63(6–7):699–701 [DOI] [PubMed] [Google Scholar]
- 20.Aubertin-Leheudre M, Rolland Y. (2020) The Importance of Physical Activity to Care for Frail Older Adults During the COVID-19 Pandemic. J Am Med Dir Assoc 21(7):973–976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baker E, Clark LL. (2020) Biopsychopharmacosocial approach to assess impact of social distancing and isolation on mental health in older adults. Br Community Nurs 25(5):231–238 [DOI] [PubMed] [Google Scholar]
- 22.Banerjee D. (2020) ‘Age and ageism in COVID-19’: Elderly mental health-care vulnerabilities and needs. Asian J Psychiatr 51:102154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Banerjee D. (2020) The Impact of COVID-19 Pandemic on Elderly Mental Health. Int J Geriatr Psychiatry 35(12):1466–1467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berg-Weger M, Morley JE. (2020) Editorial: Loneliness and Social Isolation in Older Adults during the COVID-19 Pandemic: Implications for Gerontological Social Work. J Nutr Health Aging 24(5):456–458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bhidayasiri R, Virameteekul S, Kim JM, et al. (2020) COVID-19: An Early Review of Its Global Impact and Considerations for Parkinson’s Disease Patient Care. J Mov Disord 13(2):105–114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bonafè M, Prattichizzo F, Giuliani A, et al. (2020) Inflamm-aging: Why older men are the most susceptible to SARS-CoV-2 complicated outcomes. Cytokine Growth Factor Rev 53:33–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bostanciklioglu M, Temiz E. (2020) Severe acute respiratory syndrome coronavirus 2 is penetrating to dementia research. Curr Neurovasc Res 17(4):342–343 [DOI] [PubMed] [Google Scholar]
- 28.Buenaventura RD, Ho JB, Lapid MI. (2020) COVID-19 and Mental Health of Older Adults in the Philippines: A Perspective from a Developing Country. Int Psychogeriatr 32(10):1129–1133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Burki T. (2020) England and Wales see 20 000 excess deaths in care homes. Lancet 395(10237):1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Butler MJ, Barrientos RM. (2020) The impact of nutrition on COVID-19 susceptibility and long-term consequences. Brain Behav Immun 87:53–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Campbell AD. (2020) Practical Implications of Physical Distancing, Social Isolation, and Reduced Physicality for Older Adults in Response to COVID-19. J Gerontol Soc Work 63(6–7):668–670 [DOI] [PubMed] [Google Scholar]
- 32.Carda S, Invernizzi M, Bavikatte G, et al. (2020) COVID-19 pandemic. What should Physical and Rehabilitation Medicine specialists do? A clinician’s perspective. Eur J Phys Rehabil Med 56(4):515–524 [DOI] [PubMed] [Google Scholar]
- 33.Cesari M, Proietti M. (2020) COVID-19 in Italy: Ageism and Decision Making in a Pandemic. J Am Med Dir Assoc 21(5):576–577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cesari M, Proietti M. (2020) Geriatric Medicine in Italy in the Time of COVID-19. J Nutr Health Aging 24(5):459–460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chehrehgosha M. (2020) The Unpreparedness of the Healthcare System for the Management of COVID-19 Pandemic Leading to the Mistreatment of the Elderly: A Newly Emerging Moral Dilemma. J Nutr Health Aging 24(9):973–974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen K. (2020) Use of Gerontechnology to Assist Older Adults to Cope with the COVID-19 Pandemic. J Am Med Dir Assoc 21(7):983–984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chevance A, Gourion D, Hoertel N, et al. (2020) Ensuring mental health care during the SARS-CoV-2 epidemic in France: A narrative review. L’Encephale 46(3):193–201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chong TWH, Curran E, Ames D, et al. (2020) Mental health of older adults during the COVID-19 pandemic: lessons from history to guide our future. Int Psychogeriatr 32(10):1249–1250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cohen MA, Tavares J. (2020) Who are the Most At-Risk Older Adults in the COVID-19 Era? It’s Not Just Those in Nursing Homes. J Aging Soc Policy 32(4–5):380–386 [DOI] [PubMed] [Google Scholar]
- 40.Cordasco F, Scalise C, Sacco MA, et al. (2020) The silent deaths of the elderly in long-term care facilities during the COVID-19 pandemic: The role of forensic pathology. Med Leg J 88(2):66–68 [DOI] [PubMed] [Google Scholar]
- 41.de Leo D, Trabucchi M. (2020) COVID-19 and the Fears of Italian Senior Citizens. Int J Environ Res Public Health 17(10):3572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dell NA, Sasaki N, Stewart M, et al. (2020) Service Needs of Older Adults with Serious Mental Illness. J Gerontol Soc Work 63 (6–7):659–661 [DOI] [PubMed] [Google Scholar]
- 43.Desideri I, Pilleron S, Battisti NML, et al. (2020) Caring for older patients with cancer during the COVID-19 pandemic: A Young International Society of Geriatric Oncology (SIOG) global perspective. J Geriatr Oncol 11(7):1175–1181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dowd JB, Andriano L, Brazel DM, et al. (2020) Demographic science aids in understanding the spread and fatality rates of COVID-19. Proc Natl Acad Sci U S A 117(18):9696–9698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Eghtesadi M. (2020) Breaking Social Isolation Amidst COVID-19: A Viewpoint on Improving Access to Technology in Long-Term Care Facilities. J Am Geriatr Soc 68(5):949–950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ehni HJ, Wahl HW. (2020) Six Propositions against Ageism in the COVID-19 Pandemic. J Aging Soc Policy 32(4–5):515–525 [DOI] [PubMed] [Google Scholar]
- 47.Elbeddini A, Prabaharan T, Almasalkhi S, et al. (2021) Barriers to conducting deprescribing in the elderly population amid the COVID-19 pandemic. Res Social Adm Pharm 17(1):1942–1945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Elliott L. (2020) COVID-19: Is it time that Social Care for the elderly was part of the National Health Service in the United Kingdom? J Psychiatr Ment Health Nurs (efirst) [DOI] [PubMed] [Google Scholar]
- 49.Elman A, Breckman R, Clark S, et al. (2020) Effects of the COVID-19 Outbreak on Elder Mistreatment and Response in New York City: Initial Lessons. J Appl Gerontol 39(7):690–699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Eriksen S, Grov EK, Lichtwarck B, et al. (2020) Palliative treatment and care for dying nursing home patients with COVID-19. Tidsskr Nor Laegeforen 140(8) [DOI] [PubMed] [Google Scholar]
- 51.Farrell TW, Ferrante LE, Brown T, et al. (2020) AGS Position Statement: Resource Allocation Strategies and Age-Related Considerations in the COVID-19 Era and Beyond. J Am Geriatr Soc 68(6):1136–1142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Farrell TW, Francis L, Brown T, et al. (2020) Rationing Limited Healthcare Resources in the COVID-19 Era and Beyond: Ethical Considerations Regarding Older Adults. J Am Geriatr Soc 68(6):1143–1149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fischer F, Raiber L, Boscher C, et al. (2020) COVID-19 and the Elderly: Who Cares? Front Public Health 8:151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fraser S, Lagace M, Bongue B, et al. (2020) Ageism and COVID-19: What does our society’s response say about us? Age Ageing 49(5):692–695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fratino L, Procopio G, Di Maio M, et al. (2020) Coronavirus: Older Persons With Cancer in Italy in the COVID-19 Pandemic. Front Oncol 10:648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gardner W, States D, Bagley N. (2020) The Coronavirus and the Risks to the Elderly in Long-Term Care. J Aging Soc Policy 32(4–5):310–315 [DOI] [PubMed] [Google Scholar]
- 57.Gould CE, Hantke NC. (2020) Promoting Technology and Virtual Visits to Improve Older Adult Mental Health in the Face of COVID-19. Am J Geriatr Psychiatry 28(8):889–890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Grattagliano I, Rossi A, Cricelli I, et al. (2020) The changing face of family medicine in the covid and post-covid era. Eur J Clin Invest 50(7):e13303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hado E, Friss Feinberg L. (2020) Amid the COVID-19 Pandemic, Meaningful Communication between Family Caregivers and Residents of Long-Term Care Facilities is Imperative. J Aging Soc Policy 32(4–5):410–415 [DOI] [PubMed] [Google Scholar]
- 60.Hascup ER, Hascup KN. (2020) Does SARS-CoV-2 infection cause chronic neurological complications? Geroscience 42(4):1083–1087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Henning-Smith C. (2020) The Unique Impact of COVID-19 on Older Adults in Rural Areas. J Aging Soc Policy 32(4–5):396–402 [DOI] [PubMed] [Google Scholar]
- 62.Hoffman GJ, Webster NJ, Bynum JPW. (2020) A Framework for Aging-Friendly Services and Supports in the Age of COVID-19. J Aging Soc Policy 32(4–5):450–459 [DOI] [PubMed] [Google Scholar]
- 63.Holmes EA, O’Connor RC, Perry VH, et al. (2020) Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 7(6):547–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hossain MM, Mazumder H, Tasnim S, et al. (2020) Geriatric Health in Bangladesh during COVID-19: Challenges and Recommendations. J Gerontol Soc Work 63(6–7):724–727 [DOI] [PubMed] [Google Scholar]
- 65.Hwang TJ, Rabheru K, Peisah C, et al. (2020) Loneliness and Social Isolation during the COVID-19 Pandemic. Int Psychogeriatr 32(10):1217–1220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Iaboni A, Cockburn A, Marcil M, et al. (2020) Achieving Safe, Effective, and Compassionate Quarantine or Isolation of Older Adults With Dementia in Nursing Homes. Am J Geriatr Psychiatry 28(8):835–838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Inzitari M, Udina C, Len O, et al. (2020) How a Barcelona post-acute facility became a referral center for comprehensive management of subacute patients with COVID-19. J Am Med Dir Assoc 21(7):954–957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kunz R, Minder M. (2020) COVID-19 pandemic: palliative care for elderly and frail patients at home and in residential and nursing homes. Swiss Med Wkly 150:w20235. [DOI] [PubMed] [Google Scholar]
- 69.Leon S, Giacaman RA. (2020) COVID-19 and Inequities in Oral Health Care for Older People: An Opportunity for Emerging Paradigms. JDR Clin Trans Res 5(4):290–292 [DOI] [PubMed] [Google Scholar]
- 70.Levi-Belz Y, Aisenberg D. (2020) Together we stand: Suicide risk and suicide prevention among Israeli older adults during and after the COVID-19 world crisis. Psychol Trauma 12(S1):S123–S125 [DOI] [PubMed] [Google Scholar]
- 71.Lima CKT, Carvalho PMM, Lima I, et al. (2020) The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease). Psychiatry research 287:112915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lum T, Shi C, Wong G, et al. (2020) COVID-19 and Long-Term Care Policy for Older People in Hong Kong. J Aging Soc Policy 32(4–5):373–379 [DOI] [PubMed] [Google Scholar]
- 73.Marchini L, Ettinger RL. (2020) COVID-19 pandemics and oral health care for older adults. Spec Care Dentist 40(3):329–331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Martínez-Sellés D, Martínez-Sellés H, Martinez-Sellés M. (2020) Ethical Issues in Decision-making Regarding the Elderly Affected by Coronavirus Disease 2019: An Expert Opinion. Eur Cardiol 15:e48–e48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mazumder H, Hossain MM, Das A. (2020) Geriatric Care during Public Health Emergencies: Lessons Learned from Novel Corona Virus Disease (COVID-19) Pandemic. J Gerontol Soc Work 63(4):257–258 [DOI] [PubMed] [Google Scholar]
- 76.Mesa Vieira C, Franco OH, Gómez Restrepo C, et al. (2020) COVID-19: The forgotten priorities of the pandemic. Maturitas 136:38–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mills JP, Kaye KS, Mody L. (2020) COVID-19 in older adults: clinical, psychosocial, and public health considerations. JCI Insight 5(10):e139292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Morrow-Howell N, Galucia N, Swinford E. (2020) Recovering from the COVID-19 Pandemic: A Focus on Older Adults. J Aging Soc Policy 32(4–5):526–535 [DOI] [PubMed] [Google Scholar]
- 79.Naylor MD, Hirschman KB, McCauley K. (2020) Meeting the Transitional Care Needs of Older Adults with COVID-19. J Aging Soc Policy 32(4–5):387–395 [DOI] [PubMed] [Google Scholar]
- 80.Nguyen NP, Vinh-Hung V, Baumert B, et al. (2020) Older Cancer Patients during the COVID-19 Epidemic: Practice Proposal of the International Geriatric Radiotherapy Group. Cancers 12(5):1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Nickel CH, Rueegg M, Pargger H, et al. (2020) Age, comorbidity, frailty status: effects on disposition and resource allocation during the COVID-19 pandemic. Swiss Med Wkly 150:w20269. [DOI] [PubMed] [Google Scholar]
- 82.Nickel Christian H, Bingisser R. (2020) Mimics and chameleons of COVID-19. Swiss Med Wkly 150(13–14) [DOI] [PubMed] [Google Scholar]
- 83.Nicol GE, Piccirillo JF, Mulsant BH, et al. (2020) Action at a Distance: Geriatric Research during a Pandemic. J Am Geriatr Soc 68(5):922–925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.O’Shea E. (2020) Remembering people with dementia during the COVID-19 crisis. HRB open research 3:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Patel SS, Clark-Ginsberg A. (2020) Incorporating issues of Elderly Loneliness into the COVID-19 Public Health Response. Disaster Med Public Health Prep 14(3):e13–e14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Pawelec G, Weng NP. (2020) Can an effective sars-cov-2 vaccine be developed for the older population? Immun Ageing 17(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Peron JPS, Nakaya H. (2020) Susceptibility of the Elderly to SARS-CoV-2 Infection: ACE-2 Overexpression, Shedding, and Antibody-dependent Enhancement (ADE). Clinics (Sao Paulo) 75:e1912–e1912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Roschel H, Artioli GG, Gualano B. (2020) Risk of Increased Physical Inactivity During COVID-19 Outbreak in Elderly People: A Call for Actions. J Am Geriatr Soc 68(6):1126–1128 [DOI] [PubMed] [Google Scholar]
- 89.Rowland B, Kunadian V. (2020) Challenges in the management of older patients with acute coronary syndromes in the COVID-19 pandemic. Heart 106(17):1296–1301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Saban-Ruiz J, Ly-Pen D. (2020) COVID-19: A Personalized Cardiometabolic Approach for Reducing Complications and Costs. The Role of Aging beyond Topics. J Nutr Health Aging 24(6):550–559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Satre DD, Hirschtritt ME, Silverberg MJ, et al. (2020) Addressing problems with alcohol and other substances among older adults during the COVID-19 pandemic. Am J Geriatr Psychiatry 28(7):780–783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Schrack JA, Wanigatunga AA, Juraschek SP. (2020) After the COVID-19 Pandemic: The Next Wave of Health Challenges for Older Adults. J Gerontol A Biol Sci Med Sci 75(9):e121–e122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Shahid Z, Kalayanamitra R, McClafferty B, et al. (2020) COVID-19 and Older Adults: What We Know. J Am Geriatr Soc 68(5):926–929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Shanthanna H, Strand NH, Provenzano DA, et al. (2020) Caring for patients with pain during the COVID-19 pandemic: consensus recommendations from an international expert panel. Anaesthesia 75(7):935–944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sharma A, Crosby DL. (2020) Special considerations for elderly patients with head and neck cancer during the COVID-19 pandemic. Head Neck 42(6):1147–1149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sonis JD, Kennedy M, Aaronson EL, et al. (2020) Humanism in the Age of COVID-19: Renewing Focus on Communication and Compassion. West J Emerg Med 21(3):499–502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Stokes JE, Patterson SE. (2020) Intergenerational Relationships, Family Caregiving Policy, and COVID-19 in the United States. J Aging Soc Policy 32(4–5):416–424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tyrrell CJ, Williams KN. (2020) The paradox of social distancing: Implications for older adults in the context of COVID-19. Psychol Trauma 12(S1):S214–S216 [DOI] [PubMed] [Google Scholar]
- 99.Upadhyaya GK, Iyengar K, Jain VK, et al. (2020) Challenges and strategies in management of osteoporosis and fragility fracture care during COVID-19 pandemic. J Orthop 21:287–290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Van Orden KA, Bower E, Lutz J, et al. (2020) Strategies to Promote Social Connections Among Older Adults During ‘Social Distancing’ Restrictions. Am J Geriatr Psychiatry (efirst) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wand APF, Zhong BL, Chiu HFK, et al. (2020) COVID-19: The implications for suicide in older adults. Int Psychogeriatr 32(10):1225–1230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wang H, Tang X, Fan H, et al. (2020) Potential mechanisms of hemorrhagic stroke in elderly COVID-19 patients. Aging 12(11):10022–10034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Wu B. (2020) Social isolation and loneliness among older adults in the context of COVID-19: a global challenge. Glob Health Res Policy 5:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Xie B, Charness N, Fingerman K, et al. (2020) When Going Digital Becomes a Necessity: Ensuring Older Adults’ Needs for Information, Services, and Social Inclusion During COVID-19. J Aging Soc Policy 32(4–5):460–470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Yang Y, Li W, Zhang Q, et al. (2020) Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry 7(4):e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Yen MY, Schwartz J, King CC, et al. (2020) Recommendations for protecting against and mitigating the COVID-19 pandemic in long-term care facilities. J Microbiol Immunol Infect 53(3):447–453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Young HM, Fick DM. (2020) Public Health and Ethics Intersect at New Levels With Gerontological Nursing in COVID-19 Pandemic. J Gerontol Nurs 46(5):4–7 [DOI] [PubMed] [Google Scholar]
- 108.Young HM, Quinn W, Brassard A, et al. (2020) COVID-19 Pandemic Spurs Policy Changes Benefiting Older Adults. J Gerontol Nurs 46(6):19–23 [DOI] [PubMed] [Google Scholar]
- 109.Zimmerman S, Sloane PD, Katz PR, et al. (2020) The Need to Include Assisted Living in Responding to the COVID-19 Pandemic. J Am Med Dir Assoc 21(5):572–575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zubatsky M, Berg-Weger M, Morley J. (2020) Using Telehealth Groups to Combat Loneliness in Older Adults through COVID-19. J Am Geriatr Soc 68(8):1678–1679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Banskota S, Healy M, Goldberg EM. (2020) 15 Smartphone Apps for Older Adults to Use While in Isolation During the COVID-19 Pandemic. West J Emerg Med 21(3):514–525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Cabrera MA, Karamsetty L, Simpson SA. (2020) Coronavirus and its implications for psychiatry: a rapid review of the early literature. Psychosomatics 61(6):607–615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Lithander FE, Neumann S, Tenison E, et al. (2020) COVID-19 in Older People: A Rapid Clinical Review. Age Ageing 49(4):501–515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Noone C, McSharry J, Smalle M, et al. (2020) Video calls for reducing social isolation and loneliness in older people: a rapid review. Cochrane Database Syst Rev 5:Cd013632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Arons MM, Hatfield KM, Reddy SC, et al. (2020) Presymptomatic SARS-CoV-2 Infections and Transmission in a Skilled Nursing Facility. N Engl J Med 382(22):2081–2090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Aung MN, Yuasa M, Koyanagi Y, et al. (2020) Sustainable health promotion for the seniors during COVID-19 outbreak: a lesson from Tokyo. J Infect Dev Ctries 14(4):328–331 [DOI] [PubMed] [Google Scholar]
- 117.Barber SJ, Kim H. (2021) COVID-19 Worries and Behavior Changes in Older and Younger Men and Women. J Gerontol B Psychol Sci Soc Sci 76(2):e17–e23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Bruine de Bruin W. (2021) Age Differences in COVID-19 Risk Perceptions and Mental Health: Evidence From a National U.S. Survey Conducted in March 2020. J Gerontol B Psychol Sci Soc Sci 76(2):e24–e29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Canning D, Karra M, Dayalu R, et al. (2020) The association between age, COVID-19 symptoms, and social distancing behavior in the United States. medRxiv: 10.1101/2020.04.19.20065219 (As at 18.04.2020) [DOI]
- 120.Chan EYY, Huang Z, Lo ESK, et al. (2020) Sociodemographic Predictors of Health Risk Perception, Attitude and Behavior Practices Associated with Health-Emergency Disaster Risk Management for Biological Hazards: The Case of COVID-19 Pandemic in Hong Kong, SAR China. Int J Environ Res Public Health 17(11):3869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Covino M, De Matteis G, Santoro M, et al. (2020) Clinical characteristics and prognostic factors in COVID-19 patients aged >/=80 years. Geriatr Gerontol Int 20(7):704–708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.De Smet R, Mellaerts B, Vandewinckele H, et al. (2020) Frailty and mortality in hospitalized older adults with COVID-19: retrospective observational study. medRxiv: 10.1101/2020.05.26.20113480 (As at 27.05.2020) [DOI] [PMC free article] [PubMed]
- 123.Fahed M, Barron GC, Steffens DC. (2020) Ethical and Logistical Considerations of Caring for Older Adults on Inpatient Psychiatry During the COVID-19 Pandemic. Am J Geriatr Psychiatry 28(8):829–834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Fatke B, Holzle P, Frank A, et al. (2020) Psychische Probleme in der Pandemie – Beobachtungen während der COVID-19-Krise. Dtsch Med Wochenschr 145(10):675–681 [DOI] [PubMed] [Google Scholar]
- 125.Forlenza OV, Stella F. (2020) Impact of SARS-CoV-2 pandemic on mental health in the elderly: perspective from a psychogeriatric clinic at a tertiary hospital in Sao Paulo, Brazil. Int Psychogeriatr 32(10):1147–1151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Giang TL, Vo DT, Vuong QH. (2020) COVID-19: A Relook at Healthcare Systems and Aged Populations. Sustainability 12(10):4200 [Google Scholar]
- 127.Goethals L, Barth N, Guyot J, et al. (2020) Impact of home quarantine on physical activity for older adults living at home during the COVID-19 pandemic: Qualitative interview study. JMIR Aging 3(1):e19007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Goodman-Casanova JM, Dura-Perez E, Guzman-Parra J, et al. (2020) Telehealth Home Support During COVID-19 Confinement for Community-Dwelling Older Adults With Mild Cognitive Impairment or Mild Dementia: Survey Study. J Med Internet Res 22(5):e19434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Gorrochategi MP, Munitis AE, Santamaria MD, et al. (2020) Stress, anxiety, and depression in people aged over 60 in the COVID-19 outbreak in a sample collected in Northern Spain. Am J Geriatr Psychiatry 28(9):993–998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Graham NSN, Junghans C, Downes R, et al. (2020) SARS-CoV-2 infection, clinical features and outcome of COVID-19 in United Kingdom nursing homes. J Infect 81(3):411–419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Gumina S, Proietti R, Polizzotti G, et al. (2020) The impact of COVID-19 on shoulder and elbow trauma: an Italian survey. J Shoulder Elbow Surg 29(9):1737–1742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Hecht N, Wessels L, Werft FO, et al. (2020) Need for ensuring care for neuro-emergencies-lessons learned from the COVID-19 pandemic. Acta Neurochir (Wien) 162(8):1795–1801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Hernigou J, Morel X, Callewier A, et al. (2020) Staying home during “COVID-19” decreased fractures, but trauma did not quarantine in one hundred and twelve adults and twenty eight children and the “tsunami of recommendations” could not lockdown twelve elective operations. Int Orthop 44(8):1473–1480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kemenesi G, Kornya L, Tóth GE, et al. (2020) Nursing homes and the elderly regarding the COVID-19 pandemic: situation report from Hungary. Geroscience:1–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Kimball A, Hatfield KM, Arons M, et al. (2020) Asymptomatic and Presymptomatic SARS-CoV-2 Infections in Residents of a Long-Term Care Skilled Nursing Facility – King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep 69(13):377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kipps C, Hamer M, Hill N, et al. (2020) Enforced inactivity in the elderly and diabetes risk: initial estimates of the burden of an unintended consequence of COVID-19 lockdown. medRxiv: 10.1101/2020.06.06.20124065 (As at 08.06.2020) [DOI]
- 137.Leung C. (2020) Risk factors for predicting mortality in elderly patients with COVID-19: A review of clinical data in China. Mech Ageing Dev 188:111255–111255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Li P, Chen L, Liu Z, et al. (2020) Clinical features and short-term outcomes of elderly patients with COVID-19. Int J Infect Dis 97:245–250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Liu K, Zhang W, Yang Y, et al. (2020) Respiratory rehabilitation in elderly patients with COVID-19: A randomized controlled study. Complement Ther Clin Pract 39:101166–101166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Lopez J, Perez-Rojo G, Noriega C, et al. (2020) Psychological Well-Being among Older Adults during the COVID-19 Outbreak: A Comparative Study of the Young-Old and the Old-Old Adults. Int Psychogeriatr 32(11):1365–1370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Marin-Hernandez D, Schwartz RE, Nixon DF. (2020) Epidemiological Evidence for Association between Higher Influenza Vaccine Uptake in the Elderly and Lower COVID-19 Deaths in Italy. J Med Virol 93:64–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.McCaffery K, Dodd RH, Cvejic E, et al. (2020) Disparities in COVID-19 related knowledge, attitudes, beliefs and behaviours by health literacy. Public Health Res Pract 30(4):10.1101. [DOI] [PubMed] [Google Scholar]
- 143.McMichael TM, Clark S, Pogosjans S, et al. (2020) COVID-19 in a Long-Term Care Facility – King County, Washington, February 27-March 9, 2020. MMWR Morb Mortal Wkly Rep 69(12):339–342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.McMichael TM, Currie DW, Clark S, et al. (2020) Epidemiology of COVID-19 in a Long-Term Care Facility in King County, Washington. N Engl J Med 382(21):2005–2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Mehra A, Rani S, Sahoo S, et al. (2020) A crisis for elderly with mental disorders: Relapse of symptoms due to heightened anxiety due to COVID-19. Asian J Psychiatr 51:102114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Meloni M, Izzo V, Giurato L, et al. (2020) Management of diabetic persons with foot ulceration during COVID-19 health care emergency: Effectiveness of a new triage pathway. Diabetes Res Clin Pract 165:108245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Meng H, Xu Y, Dai J, et al. (2020) Analyze the psychological impact of COVID-19 among the elderly population in China and make corresponding suggestions. Psychiatry Research 289:112983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Michelozzi P, de’Donato F, Scortichini M, et al. (2020) Mortality impacts of the coronavirus disease (COVID-19) outbreak by sex and age: rapid mortality surveillance system, Italy, 1 February to 18 April 2020. Euro Surveill 25(19):2000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Moore RC, Lee A, Hancock JT, et al. (2020) Experience with Social Distancing Early in the COVID-19 Pandemic in the United States: Implications for Public Health Messaging. medRxiv: 10.1101/2020.04.08.20057067 (As at 11.04.2020) [DOI]
- 150.Muñoz Vives JM, Jornet-Gibert M, Cámara-Cabrera J, et al. (2020) Mortality Rates of Patients with Proximal Femoral Fracture in a Worldwide Pandemic: Preliminary Results of the Spanish HIP-COVID Observational Study. J Bone Joint Surg Am 102(13):e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Neerland BE, Dobloug A, Nore KG, et al. (2020) COVID-19 in an elderly woman with acute functional decline. Tidsskr Nor Laege-foren 140(7) [DOI] [PubMed] [Google Scholar]
- 152.Office EE, Rodenstein MS, Merchant TS, et al. (2020) Reducing Social Isolation of Seniors during COVID-19 through Medical Student Telephone Contact. J Am Med Dir Assoc 21(7):948–950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Pan SL, Cui M, Qian J. (2020) Information Resource Orchestration during the COVID-19 Pandemic: A Study of Community Lockdowns in China. Int J Inf Manage 54:102143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Qin L, Li X, Shi J, et al. (2020) Gendered effects on inflammation reaction and outcome of COVID-19 patients in Wuhan. J Med Virol 92(11):2684–2692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Rana U. (2020) Elderly Suicides in India: An Emerging Concern during COVID-19 Pandemic. Int Psychogeriatr 32(10):1251–1252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Ross SB, Wilson MG, Papillon-Ferland L, et al. (2020) COVID-SAFER: Deprescribing Guidance for Hydroxychloroquine Drug Interactions in Older Adults. J Am Geriatr Soc 68(8):1636–1646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Roxby AC, Greninger AL, Hatfield KM, et al. (2020) Detection of SARS-CoV-2 Among Residents and Staff Members of an Independent and Assisted Living Community for Older Adults – Seattle, Washington, 2020. MMWR Morb Mortal Wkly Rep 69(14):416–418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Shrira A, Hoffman Y, Bodner E, et al. (2020) COVID-19 Related Loneliness and Psychiatric Symptoms among Older Adults: The Buffering Role of Subjective Age. Am J Geriatr Psychiatry 28(11):1200–1204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Stanton R, To QG, Khalesi S, et al. (2020) Depression, Anxiety and Stress during COVID-19: Associations with Changes in Physical Activity, Sleep, Tobacco and Alcohol Use in Australian Adults. Int J Environ Res Public Health 17(11):4065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Tabrizi S, Trippa L, Cagney D, et al. (2020) A quantitative framework for modeling COVID-19 risk during adjuvant therapy using published randomized trials of glioblastoma in the elderly. Neuro Oncol 22(7):918–927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Tay HS, Harwood R. (2020) Atypical presentation of COVID-19 in a frail older person. Age Ageing 49(4):523–524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.van Dyck LI, Wilkins KM, Ouellet J, et al. (2020) Combating Heightened Social Isolation of Nursing Home Elders: The Telephone Outreach in the COVID-19 Outbreak Program. Am J Geriatr Psychiatry 28(9):989–992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Zhao M, Wang M, Zhang J, et al. (2020) Comparison of clinical characteristics and outcomes of patients with coronavirus disease 2019 at different ages. Aging 12(11):10070–10086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Zhu Y, Chen W, Xin X, et al. (2020) Epidemiologic characteristics of traumatic fractures in elderly patients during the outbreak of coronavirus disease 2019 in China. Int Orthop 44(8):1565–1570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Bundesarbeitsgemeinschaft der Seniorenorganisationen e. V. (BAGSO) (2020) Stellungnahme: Menschenleben schützen – Zusammenhalt stärken. Empfehlungen der BAGSO in Zeiten der Ausbreitung des Coronavirus. https://www.bagso.de/fileadmin/user_upload/bagso/06_Veroeffentlichungen/2020/20200325_Menschenleben_schuetzen_Zusammenhalt_staerken.pdf (As at 30.06.2020)
- 166.Bundesarbeitsgemeinschaft der Seniorenorganisationen e. V. (BAGSO) (2020) Stellungnahme: Besuche in Pflegeheimen: Einrichtungen brauchen klare Vorgaben und mehr Unterstützung. Aufruf der BAGSO an die Bundesländer – der Bundesregierung zur Kenntnis. https://www.bagso.de/fileadmin/user_upload/bagso/06_Veroeffentlichungen/2020/barrierefrei_BAGSO_4_seiter_stellungnahme_besuche_in_pflegeheimen_corona....pdf (As at 30.06.2020)
- 167.Bundesarbeitsgemeinschaft der Seniorenorganisationen e. V. (BAGSO) (2020) Stellungnahme: Digitale Grundversorgung in Alten- und Pflegeheimen sicherstellen. Fünf Forderungen der BAGSO. https://www.bagso.de/fileadmin/user_upload/bagso/06_Veroeffentlichungen/2020/Stellungnahme_Digitale_Grundversorgung_in_Pflegeheimen.pdf (As at 30.06.2020)
- 168.Bundesarbeitsgemeinschaft der Seniorenorganisationen e. V. (BAGSO) (2020) Stellungnahme: Besuche in Pflegeheimen: Einige Bundesländer müssen dringend nachbessern. Eine Zwischenbilanz der BAGSO vier Wochen nach dem Bund-Länder-Beschluss zur Wiederermöglichung solcher Besuche. https://www.bagso.de/fileadmin/user_upload/bagso/06_Veroeffentlichungen/2020/BAGSO-Stellungnahme_Besuche_in_Pflegeheimen_Zwischenbilanz.pdf (As at 30.06.2020)
- 169.BundesarbeitsgemeinschaftderSeniorenorganisationene.V.(BAGSO) (2020) Stellungnahme: Corona-Epidemie in Deutschland: Menschen in der Pflege nicht allein lassen! Stellungnahme der BAGSO zum Tag der älteren Generation am 1. April 2020. https://www.bagso.de/fileadmin/user_upload/bagso/06_Veroeffentlichungen/2020/Stellungnahme_Menschen_in_der_Pflege_nicht_allein_lassen.pdf (As at 30.06.2020)
- 170.Bundesarbeitsgemeinschaft der Seniorenorganisationen e. V. (BAGSO) (2020) Stellungnahme: Soziale Isolation von Menschen in Pflegeheimen beenden! Dringende Empfehlungen der BAGSO an die Politik. https://www.bagso.de/fileadmin/user_upload/bagso/06_Veroeffentlichungen/2020/Stellungnahme_Soziale_Isolation_Pflegeheime.pdf (As at 30.06.2020)
- 171.Bundesarbeitsgemeinschaft der Seniorenorganisationen e. V. (BAGSO) (2020) Stellungnahme: Pflegende Angehörige in der Corona-Situation besser unterstützen! Dringende Empfehlungen der BAGSO an die Politik. https://www.bagso.de/fileadmin/user_upload/bagso/06_Veroeffentlichungen/2020/Stellungnahme_pflegende_angehoerige_besser_unterstuetzen.pdf (As at 30.06.2020)
- 172.BundesinteressenvertretungfüralteundpflegebetroffeneMenschene.V.(BIVA-Pflegeschutzbund) (2020) Besuchsbeschränkungen in Pflegeheimen aufgrund der Corona-Krise. BIVA-Positionspapier. https://www.biva.de/positionspapier-besuchsbeschraenkungen-pflegeheim/ (As at 30.06.2020)
- 173.Bundesinteressenvertretung für alte und pflegebetroffene Menschen e. V. (BIVA-Pflegeschutzbund) (2020) Corona-Virus – Auswirkungen auf Pflegebedürftige. https://www.biva.de/corona-virus-auswirkungen-auf-pflegeheime/ (As at 30.06.2020)
- 174.Bundesinteressenvertretung für alte und pflegebetroffene Menschen e. V. (BIVA-Pflegeschutzbund) (2020) Corona-Krise und der ‚real existierende Pflegealltag‘ in stationären Einrichtungen der Altenhilfe. Gastkommentar von BIVA-Mitglied Claus Völker. https://www.biva.de/corona-krise-und-der-real-existierende-pflegealltag/ (As at 30.06.2020)
- 175.BundesinteressenvertretungfüralteundpflegebetroffeneMenschene.V.(BIVA-Pflegeschutzbund) (2020) Corona: Pflegeheimbewohner besser schützen! https://www.biva.de/corona-pflegeheimbewohner-besser-schuetzen/ (As at 30.06.2020)
- 176.Bundesinteressenvertretung für alte und pflegebetroffene Menschen e. V. (BIVA-Pflegeschutzbund) (2020) Pflegeheimbewohner weiterhin gefährdet – Helfende Angehörige sind systemrelevant. https://www.biva.de/pflegeheimbewohner-weiterhin-gefaehrdet/ (As at 30.06.2020)
- 177.Bundesinteressenvertretung für alte und pflegebetroffene Menschen e. V. (BIVA-Pflegeschutzbund) (2020) Lockerungen des Besuchsverbotes in Alten- und Pflegeheimen unzureichend umgesetzt. https://www.biva.de/lockerungen-des-besuchsverbotes-in-alten-und-pflegeheimen-unzureichend-umgesetzt/ (As at 30.06.2020)
- 178.Bundesinteressenvertretung für alte und pflegebetroffene Menschen e. V. (BIVA-Pflegeschutzbund) (2020) Besuchsregelungen in Altenheimen: Konflikte vermeidbar machen. https://www.biva.de/besuchsregelungen-in-altenheimen-konflikte-vermeidbar-machen/ (As at 30.06.2020)
- 179.Bundesinteressenvertretung für alte und pflegebetroffene Menschen e. V. (BIVA-Pflegeschutzbund) (2020) Ernüchterndes Umfrageergebnis: Besuchsmöglichkeiten in Pflegeheimen sind unzureichend und die Folgen der sozialen Isolation gravierend. https://www.biva.de/umfrage-besuche-im-pflegeheim-noch-unzureichend/ (As at 30.06.2020)
- 180.Deutsche Alzheimer Gesellschaft e. V. (DAlzG) (2020) Corona-Virus: Die besondere Situation von pflegenden Angehörigen von Menschen mit Demenz berücksichtigen. https://www.deutsche-alzheimer.de/ueber-uns/presse/artikelansicht/artikel/corona-virus-die-besondere-situation-von-pflegenden-angehoerigen-von-menschen-mit-demenz-beruecksicht.html (As at 30.06.2020)
- 181.Deutsche Alzheimer Gesellschaft e. V. (DAlzG) (2020) Corona-Krise: Regelungen zu Besuchen in Pflegeheimen. https://www.deutsche-alzheimer.de/ueber-uns/presse/artikelansicht/artikel/corona-virus-die-deutsche-alzheimer-gesellschaftfordert-die-politik-zum-handeln-auf.html (As at 30.06.2020)
- 182.Deutsche Alzheimer Gesellschaft e. V. (DAlzG) (2020) Corona-Virus: Die Deutsche Alzheimer Gesellschaft fordert die Politik zum Handeln auf. https://www.deutsche-alzheimer.de/ueber-uns/presse/artikelansicht/artikel/corona-virus-die-deutsche-alzheimer-gesellschaftfordert-die-politik-zum-handeln-auf.html (As at 30.06.2020)
- 183.Deutsche Alzheimer Gesellschaft e. V. (DAlzG) (2020) Menschen mit Demenz schützen! Deutsche Alzheimer Gesellschaft fordert schnellstmögliche Lockerung der Besuchsverbote in Heimen. https://www.deutsche-alzheimer.de/ueber-uns/presse/artikelansicht/artikel/menschen-mit-demenz-schuetzen-deutsche-alzheimer-gesellschaft-fordert-schnellstmoegliche-lockerung-de.html (As at 30.06.2020)
- 184.Deutsche Alzheimer Gesellschaft e. V. (DAlzG) (2020) Geschlossene Tagespflegeeinrichtungen – finanzieren pflegende Angehörige den Corona-Rettungsschirm? https://www.deutsche-alzheimer.de/ueber-uns/presse/artikelansicht/artikel/geschlossene-tagespflegeeinrichtungen-finanzier-en-pflegende-angehoerige-den-corona-rettungsschirm.html (As at 30.06.2020)
- 185.Deutsche Alzheimer Gesellschaft e. V. (DAlzG) (2020) Besuche in Pflegeheimen: Deutsche Alzheimer Gesellschaft fordert verbind liche Regelungen für alle Einrichtungen. https://www.deutsche-alzheimer.de/ueber-uns/presse/artikelansicht/artikel/besuche-in-pflegeheimen-deutsche-alzheimer-gesellschaft-fordert-verbindliche-regelungen-fuer-alle-e.html (As at 30.06.2020)
- 186.Deutsche Gesellschaft für Geriatrie e. V. (DGG) (2020) Pressemeldung der Deutschen Gesellschaft für Geriatrie (DGG): Corona-Virus: So können sich ältere Menschen schützen oder „Kein Küsschen für Oma“. https://www.dggeriatrie.de/images/Dokumente/200313-dgg-pressemeldung-corona-wie-sich-aeltere-menschenschuetzen-koennen.pdf (As at 30.06.2020)
- 187.Deutsche Gesellschaft für Geriatrie e. V. (DGG) (2020) Pressemeldung der Deutschen Gesellschaft für Geriatrie (DGG): COVID-19 und Senioren: Geriater stellen Maßnahmen zum Schutz und zur Versorgung älterer Menschen vor. https://www.dggeriatrie.de/images/Dokumente/200320-dgg-pressemeldung-covid-19-und-senioren-schutzmassnahmen-und-versorgung.pdf (As at 30.06.2020)
- 188.Deutsche Gesellschaft für Geriatrie e. V. (DGG) (2020) Pressemeldung der Deutschen Gesellschaft für Geriatrie (DGG): Engpass Pflegeversorgung: Geriater fordern Krisen-Konzept für Corona-Risikogruppe. https://www.dggeriatrie.de/images/Dokumente/200320-dgg-pressemeldung-engpass-pflegeversorgung.pdf (As at 30.06.2020)
- 189.Deutsche Gesellschaft für Geriatrie e. V. (DGG) (2020) Pressemeldung der Deutschen Gesellschaft für Geriatrie (DGG): Nach Corona-Lockerungen empfehlen Altersmediziner weiteren Schutz älterer Menschen: „SARS-CoV-2 ist noch nicht verschwunden!“. https://www.dggeriatrie.de/images/Dokumente/200508-dgg-pressemeldung-covid-19-lockerungen-schutz-aelterer-menschen.pdf (As at 30.06.2020)
- 190.Deutsche Gesellschaft für Gerontologie und Geriatrie e. V. (DGGG) (2020) Stellungnahme der Deutschen Gesellschaft für Gerontologie und Geriatrie zur COVID-19 Pandemie. https://www.dggg-online.de/fileadmin/aktuelles/covid-19/20200331_covid-19_Praesidium-statement.pdf (As at 30.06.2020)
- 191.Deutsche Gesellschaft für Gerontologie und Geriatrie e. V. (DGGG) (2020) Statement der DGGG: Möglichkeit für telefonische Psychotherapie für alte und vulnerable Patientinnen während der Coronapandemie erleichtern. https://www.dggg-online.de/covid-19-news/telefonische-psychotherapie.html (As at 30.06.2020)
- 192.Deutsches Netzwerk Evidenzbasierte Medizin e. V. (EbM-Netzwerk) (2020) Stellungnahme: COVID-19 Pandemie: So viel Zeit muss sein! Keine Experimente mit der alten und chronisch kranken Bevölkerung ohne wissenschaftliche Begleitung. https://www.ebm-netzwerk.de/de/veroeffentlichungen/pdf/stn20200327-covid19-begleitforschung (As at 30.06.2020)
- 193.Deutsches Netzwerk Evidenzbasierte Medizin e. V. (EbM-Netzwerk) (2020) Stellungnahme: Corona-Virus in unseren Pflegeheimen – ein evidenzfreies Drama in drei Akten. https://www.ebm-netzwerk.de/de/veroeffentlichungen/nachrichten/corona-virus-in-unseren-pflegeheimen-ein-evidenzfreies-drama-in-drei-akten (As at 30.06.2020)
- 194.Endter C, Hagen C, Berner F. (2020) DZA-Fact Sheet: Ältere Menschen und ihre Nutzung des Internets. Folgerungen für die Corona-Krise. Deutsches Zentrum für Altersfragen (DZA), Berlin. https://www.dza.de/fileadmin/dza/Dokumente/Fact_Sheets/Fact_Sheet_Corona4_Digitalisierung.pdf (As at 30.06.2020) [Google Scholar]
- 195.Hämel K, Kümpers S, Olbermann E, et al. (2020) Gemeinsames Statement der Sektionen Sozial- und Verhaltenswissenschaftliche Gerontologie (III) und Soziale Gerontologie und Altenarbeit (IV) der DGGG: Teilhabe und Versorgung von Menschen mit Pflegebedarf in Zeiten von Corona und darüber hinaus. Deutsche Gesellschaft für Gerontologie und Geriatrie e. V. (DGGG), Berlin. https://www.dggg-online.de/fileadmin/aktuelles/covid-19/20200510_DGGG_Statement_Sektionen_III_IV_Menschen_mit_Pflegebedarf.pdf (As at 30.06.2020) [Google Scholar]
- 196.Huxhold O, Engstler H, Klaus D. (2020) DZA-Fact Sheet: Risiken der Kontaktsperre für soziale Kontakte, soziale Unterstützung und ehrenamtliches Engagement von und für ältere Menschen. Deutsches Zentrum für Altersfragen (DZA), Berlin. https://www.dza.de/fileadmin/dza/Dokumente/Fact_Sheets/Fact_Sheet_Corona3_Kontaktsperre.pdf (As at 30.06.2020) [Google Scholar]
- 197.Kessler EM, Gellert P. (2020) Öffentliche Kommunikation und Berichterstattung zu ‚Corona & Alter‘: Empfehlungen der Deutschen Gesellschaft für Gerontologie und Geriatrie (DGGG), Sektion III (Sozial- und Verhaltenswissenschaftliche Gerontologie). Deutsche Gesellschaft für Gerontologie und Geriatrie e. V. (DGGG), Berlin. https://www.dggg-online.de/fileadmin/aktuelles/covid-19/20200401_Paper-Kommunikation-Alter-und-Corona-SektionIII.pdf (As at 30.06.2020) [Google Scholar]
- 198.Kessler EM, Strumpen S, Kricheldorff C, et al. (2020) Gemeinsames Statement der Sektionen für Geriatrische Medizin (II), Sozial- und Verhaltenswissenschaftliche Gerontologie (III), Soziale Gerontologie und Altenhilfe (IV) der Deutschen Gesellschaft für Gerontologie und Geriatrie (DGGG e. V.): Partizipation und soziale Teilhabe älterer Menschen trotz Corona-Pandemie ermöglichen. Deutsche Gesellschaft für Gerontologie und Geriatrie e. V. (DGGG), Berlin. https://www.dggg-online.de/fileadmin/aktuelles/covid-19/20200424_DGGG_Statement_Sektionen_II_III_IV_Soziale_Teilhabe_und_Partizipation.pdf (As at 30.06.2020) [Google Scholar]
- 199.Kümpers S, Olbermann E, Strümpen S, et al. (2020) Soziale Notlagen älterer Menschen im Zuge der COVID-19 Pandemie: Empfehlung zur Einrichtung, Unterstützung und Förderung lokaler Nothilfeinitiativen. Deutsche Gesellschaft für Gerontologie und Geriatrie e. V. (DGGG), Berlin. https://www.dggg-online.de/fileadmin/aktuelles/covid-19/20200407_SektionIV-DGGG-Empfehlung-LokaleNothilfe.pdf (As at 30.06.2020) [Google Scholar]
- 200.Kuratorium Deutsche Altershilfe e. V. (KDA) (2020) Die COVID-19-Pandemie und die Situation der älteren Menschen in Deutschland. Eine Stellungnahme des Kuratoriums Deutsche Altershilfe (KDA). https://kda.de/wp-content/uploads/2020/04/Stellungnahme-KDA-Corona-kompakt.pdf (As at 30.06.2020)
- 201.Pflegeethik Initiative Deutschland e. V. (2020) CORONA-BRAND-BRIEF: Besuchsverbote in Pflegeheimen sind unmenschlich und unverhältnismäßig. Sie sind daher sofort aufzuheben! http://pflegeethik-initiative.de/wp-content/uploads/2020/05/Corona-Brandbrief.pdf (As at 30.06.2020)
- 202.Pflegeethik Initiative Deutschland e. V. (2020) Falsche Prioritäten gesetzt und ethische Prinzipien verletzt. http://pflegeethik-initiative.de/2020/04/15/corona-krise-falsche-prioritaeten-gesetzt-und-ethische-prinzipien-verletzt/ (As at 30.06.2020)
- 203.PflegeethikInitiative Deutschland e. V. (2020) Nicht Leben und nicht Sterben dürfen. http://pflegeethik-initiative.de/2020/03/26/nicht-leben-und-nicht-sterben-duerfen/ (As at 30.06.2020)
- 204.Pflegeethik Initiative Deutschland e. V. (2020) Generelle Besuchsverbote in Heimen sind unmenschlich!!! http://pflegeethik-initiative.de/2020/03/17/besuchsverbote-in-heimen-sind-unangemessen-und-unmenschlich/ (As at 30.06.2020)
- 205.Schulz-Nieswandt F. (2020) Gefahren und Abwege der Sozialpolitik im Zeichen von Corona. Zur affirmativen Rezeption von Corona in Kultur, Geist und Seele der „Altenpolitik“. Kuratorium Deutsche Altershilfe (KDA), Berlin. https://sozialpolitik.uni-koeln.de/sites/sozialpolitik/user_upload/RZ_KDA_Corona_2.pdf (As at 30.06.2020) [Google Scholar]
- 206.Seidler A, Petereit-Haack G, Riedel-Heller S, et al. (2020) Müssen ältere Beschäftigte dem Arbeitsplatz fernbleiben? Ergebnisse einer systematischen Literaturrecherche („Rapid Scoping Review“). Kompetenznetz Public Health COVID-19. https://www.ghup.de/wp-content/uploads/2020/05/2020_04_23_Fact_Sheet_Auswirkungen_auf_ltere_Beschftigte_V3.pdf (As at 30.06.2020)
- 207.Seidler A, Schubert M, Petereit-Haack G, et al. (2020) Soziale Isolation als Sterblichkeitsrisiko für ältere Menschen: Ergebnisse einer systematischen Literaturrecherche („Rapid Scoping Review“), ergänzt durch eine qualitative Erhebung. Kompetenznetz Public Health COVID-19. https://www.public-health-covid19.de/images/2020/Ergebnisse/2020_05_18_fact_sheet_soziale-isolation-als-mortalita__tsrisiko_1.pdf (As at 30.06.2020)
- 208.Spuling SM, Wettstein M, Tesch-Römer C. (2020) DZA-Fact Sheet: Altersdiskriminierung und Altersbilder in der Corona-Krise. Deutsches Zentrum für Altersfragen (DZA), Berlin. https://www.dza.de/fileadmin/dza/Dokumente/Fact_Sheets/Fact_Sheet_Corona2_Altersbilder.pdf (As at 30.06.2020) [Google Scholar]
- 209.Tesch-Römer C, Vogel C, Wettstein M, et al. (2020) DZA-Fact Sheet: Alte Menschen sind unterschiedlich, auch in der Corona-Krise. Deutsches Zentrum für Altersfragen (DZA), Berlin. https://www.dza.de/fileadmin/dza/Dokumente/Fact_Sheets/Fact_Sheet_Corona1_Ungleichheit.pdf (As at 30.06.2020) [Google Scholar]
- 210.Wedding U, Thiem U, Heppner HJ. (2020) Ergänzende Empfehlungen für die Situation heimversorgter geriatrischer Patienten zu den „Entscheidungen über die Zuteilung von Ressourcen in der Notfall- und Intensivmedizin im Kontext der COVID-19-Pandemie“ der DIVI, DGINA, DGAI, DGIIN, DGP, DGP, AEM. Deutsche Gesellschaft für Geriatrie e. V. (DGG), Berlin. https://www.dggeriatrie.de/images/Dokumente/200422-dgg-er-gaenzende-empfehlungen-fuer-heimversorgte-patienten.pdf (As at 30.06.2020) [Google Scholar]
- 211.Wettstein M, Nowossadeck S, Spuling SM, et al. (2020) DZA-Fact Sheet: Körperliche Aktivität älterer Menschen in der Corona-Krise. Deutsches Zentrum für Altersfragen (DZA), Berlin. https://www.dza.de/fileadmin/dza/Dokumente/Fact_Sheets/Fact_Sheet_Corona5_Koerperl.Aktiv.pdf (As at 30.06.2020) [Google Scholar]
- 212.Kelfve S. (2019) Underestimated Health Inequalities Among Older People-A Consequence of Excluding the Most Disabled and Disadvantaged. J Gerontol B Psychol Sci Soc Sci 74(8):e125–e134 [DOI] [PubMed] [Google Scholar]
- 213.Gaertner B, Lüdtke D, Koschollek C, et al. (2019) Effects of a sequential mixed-mode design on participation, contact and sample composition – Result of the pilot study „IMOA – Improving Health Monitoring in Old Age“ Survey Insights: Methods from the Field. https://surveyinsights.org/?p=10841 (As at 06.05.2019)
- 214.Gaertner B, Seitz I, Fuchs J, et al. (2016) Baseline participation in a health examination survey of the population 65 years and older: who is missed and why? BMC Geriatr 16:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Santos-Hövener C, Busch MA, Koschollek C, et al. (2020) Seroepidemiological study on the spread of SARS-CoV-2 in populations in especially affected areas in Germany – Study protocol of the CORONA-MONITORING lokal study. Journal of Health Monitoring 5(S5):2–16. https://edoc.rki.de/handle/176904/7490 (As at 15.02.2021) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Damerow S, Rommel A, Prütz F, et al. (2020) Developments in the health situation in Germany during the initial stage of the COVID-19 pandemic for selected indicators of GEDA 2019/2020-EHIS. Journal of Health Monitoring 5(4):3–20. https://edoc.rki.de/handle/176904/7550 (As at 15.02.2021) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Picaza Gorrochategi M, Eiguren Munitis A, Dosil Santamaria M, et al. (2020) Stress, Anxiety, and Depression in People Aged Over 60 in the COVID-19 Outbreak in a Sample Collected in Northern Spain. Am J Geriatr Psychiatry 28(9):993–998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Hamm ME, Brown PJ, Karp JF, et al. (2020) Experiences of American Older Adults with Pre-existing Depression During the Beginnings of the COVID-19 Pandemic: A Multicity, Mixed-Methods Study. Am J Geriatr Psychiatry 28(9):924–932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Richardson SJ, Carroll CB, Close J, et al. (2020) Research with older people in a world with COVID-19: identification of current and future priorities, challenges and opportunities. Age Ageing 49(6):901–906 [DOI] [PMC free article] [PubMed] [Google Scholar]


