Abstract
Background:
Healthcare workers (HCWs) during the COVID-19 pandemic report high levels of psychological distress. We examined whether concerns regarding transmission of COVID-19 to loved ones and social distancing from loved ones were associated with HCWs’ distress. We tested whether living with others modified these associations.
Methods:
HCWs at a New York City academic medical center (N = 767; 80.7% female, 58.5% white) enrolled in the COVID-19 Healthcare Provider Study and completed a web-based survey between April 9, 2020 and May 11, 2020.
Results:
Controlling for demographics, distress regarding potential transmission to loved ones and social distancing from loved ones were each significantly associated with higher odds of a positive screen for acute stress, depression, and anxiety (ORs = 1.29 – 1.59, all ps < .01). Living with others was associated with lower odds of a positive screen for depression and anxiety, though the protective effect for anxiety was evident only for HCWs with no distress regarding transmission concerns.
Conclusions:
Transmission concerns and social distancing from loved ones were associated with greater odds of psychological distress, whereas living with others was associated with lower odds of distress. Interventions should consider ways to facilitate the ability of HCWs to receive social support from loved ones, while simultaneously protecting their family’s health.
Keywords: COVID-19, coronavirus, healthcare workers, psychological distress, social support
Healthcare workers (HCWs) working during the COVID-19 pandemic exhibit high levels of psychological distress (Lai et al., 2020; Li et al., 2020; Montemurro, 2020; Shechter et al., 2020; Simione & Gnagnarella, 2020). These HCWs are at substantial risk for infection (Zhu et al., 2020) and are exposed to numerous traumas associated with treating COVID-19 patients (Brooks, Dunn, Amlôt, Rubin, & Greenberg, 2017; Thoits, 1995). Furthermore, policies to combat the spread of COVID-19 disrupted access to support from friends and family outside the home.
Although cohabiting family members may serve as an important source of social support to HCWs working in COVID-19 settings (Brooks et al., 2017; Thoits, 1995), HCWs may be distressed about infecting their loved ones (Lin, 2020; Simione & Gnagnarella, 2020; Zhu et al., 2020). Precautionary measures such as social distancing may impede family support, with the unintended consequence of worsening psychological wellbeing. This pattern has been found during prior infectious disease outbreaks, such as severe acute respiratory syndrome (Brooks, Dunn, Amlôt, Rubin, & Greenberg, 2018).
The present study tested the hypothesis that concerns over transmitting COVID-19 to loved ones and maintaining social distance from loved ones would be positively associated with psychological distress. We hypothesized that concerns about transmitting and social distancing would be even more distressing for those living with more people in their home.
Methods
Participants
Participants were HCWs at a large New York City (NYC) academic medical center enrolled in the COVID-19 Healthcare Provider Study (Shechter et al., 2020).
Procedure
HCWs were invited to complete a baseline survey via a standardized recruitment email and Qualtrics link, sent to listservs for HCWs at the medical center during a peak of the NYC COVID-19 outbreak, April 9 – May 11, 2020 (Campo-Flores, 2020; Dong, Du, & Gardner, 2020; Ellison, 2020). Of the 7,117 individuals who received an invitation by email (physicians, nurse practitioners, physician assistants, n = 1,870; interns, residents, fellows, n = 974; nurses, n = 4,273), 1,246 enrolled and began the survey (17.5% response rate), 917 completed the survey within the specified timeframe (73.6% completion). All procedures were approved by the Columbia University Irving Medical Center Institutional Review Board, and all participants provided electronic informed consent.
Measures
Psychological distress was assessed using validated questionnaires to screen for symptoms of acute stress (Primary Care Post-Traumatic Stress Disorder screen; Prins et al., 2004), depression (Patient Health Questionnaire-2; Kroenke, Spitzer, & Williams, 2003), and anxiety (2-item Generalized Anxiety Disorder scale; Kroenke, Spitzer, Williams, Monahan, & Lowe, 2007). For each measure, scores ≥ 3 indicated a positive screen.
Participants self-reported past-week COVID-19-related levels of distress (Chen et al., 2020; Lai et al., 2020) regarding “Potential transmission of COVID-19 from you to your family or loved ones?” and “Maintaining social distance from loved ones as a precautionary measure?” using a 5-point Likert scale (1, no distress; 5, extreme distress).
Data Analysis Strategy
Binary logistic regression models were estimated testing concerns over transmission of COVID-19 to loved ones and social distancing from loved ones as predictors of a positive screen for acute stress, depression, and anxiety. Necessary statistical assumptions for binary logistic regression were met. Covariates included self-reported number of others in the home, age, race, ethnicity, gender, and provider type (resident, fellow, physician, primary care provider v. nurse practitioner, registered nurse, physician assistant, other). We tested effect modification by number of others in the home (0, 1, 2, or 3+). We conducted sensitivity analyses contrasting participants living alone vs. with 1+ others (0 or 1+).
Results
A total of 767 HCWs provided data for the present analysis. Participants were most often ages of 25 – 34 (47.7%), female (80.7%), white (58.5%), and lived with at least one other person (82.7%). Distress regarding transmission concerns and social distancing from loved ones was high, as was psychological distress, with positive screens (scores ≥ 3) for acute stress, depression, and anxiety being 59.1%, 33.9%, and 48.5%, respectively (see Table 1).
Table 1.
Demographics (N = 767)
| M (SD), Median [IQR], or N (%) | ||
|---|---|---|
| Age group | 18-24 | 21 (2.7%) |
| 25-34 | 366 (47.7%) | |
| 35-44 | 181 (23.6%) | |
| 45-54 | 117 (15.3%) | |
| 55-64 | 76 (9.9%) | |
| 65-74 | 4 (0.7%) | |
| ≥75 | 1 (0.1%) | |
| Gender | Female | 624 (80.7%) |
| MDa | 247 (33.5%) | |
| Race | White | 449 (58.5%) |
| Black | 62 (8.1%) | |
| Asian | 127 (16.6%) | |
| American Indian/Native American | 3 (0.4%) | |
| Hawaiian/Pacific Islander | 3 (0.4%) | |
| More than one | 46 (6.0%) | |
| Other/Unknown | 77 (10.0) | |
| Ethnicity | Hispanic or Latinx | 93 (12.1%) |
| Not Hispanic or Latinx | 633 (82.5%) | |
| Prefer not to say | 41 (5.3%) | |
| Number of others in the home | Alone | 133 (17.3%) |
| 1 | 277 (36.1%) | |
| 2 | 131 (17.1%) | |
| ≥ 3 | 226 (29.5%) | |
| Transmission concerns (potential transmission of COVID-19 to loved ones)b | 4.13 (1.12) | |
| Maintaining social distance from loved ones as a precautionary measureb | 3.88 (1.18) | |
| Acute stress symptoms | 3.00 [2.00, 4.00] | |
| Positive screen (score ≥ 3) | 453 (59.1%) | |
| Depressive symptoms | 2.00 [1.00, 3.00] | |
| Positive screen (score ≥ 3) | 260 (33.9%) | |
| Anxiety symptoms | 2.00 [1.00, 4.00] | |
| Positive screen (score ≥ 3) | 372 (48.5%) |
Resident, fellow, physician, or primary care provider (reference group: nurse practitioner, registered nurse, physician assistant, other)
Assessed on a 5-point Likert scale ranging from 1, no distress, to 5, extreme distress.
Distress regarding transmission concerns for family and loved ones and social distancing from loved ones were positively related to a positive screen for acute stress (transmission concerns, OR = 1.29, 95% CI [1.10, 1.52], p = .002; social distancing, OR = 1.54, 95% CI [1.32, 1.80], p < .001), depression (transmission concerns, OR = 1.31, 95% CI [1.09, 1.57], p = .004; social distancing, OR = 1.59, 95% CI [1.33, 1.90], p < .001), and anxiety (transmission concerns, OR = 1.46, 95% CI [1.23, 1.73], p < .001; social distancing, OR = 1.39, 95% CI [1.19, 1.62], p < .001). There was no association between number of others in the home and screening positive for acute stress, p = .066, but number others in the home was significantly associated with lower odds of a positive screen for depression, OR = 0.77, 95% CI [0.66, 0.91], p < .001, and anxiety, OR = 0.80, 95% CI [0.69, 0.93], p = .004 (see Table 2).
Table 2.
Results of binary logistic regression analyses predicting a positive screen for acute stress, depression, and anxiety.
| Acute Stress | Depression | Anxiety | |
|---|---|---|---|
|
|
|||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Age | 0.90 (0.77, 1.04) | 1.05 (0.90, 1.22) | 0.89 (0.77, 1.04) |
| Male | 0.61 (0.41, 0.93)* | 0.82 (0.52, 1.29) | 0.71 (0.47, 1.08) |
| White | 1.08 (0.78, 1.50) | 0.99 (0.71, 1.37) | 1.00 (0.73, 1.38) |
| Hispanic or Latinx | 1.41 (0.85, 2.32) | 1.42 (0.89, 2.28) | 1.45 (0.91, 2.32) |
| MDa | 0.87 (0.61, 1.26) | 084 (0.57, 1.24) | 0.95 (0.66, 1.37) |
| Number of others in the home | 0.87 (0.74, 1.01)+ | 0.77 (0.66, 0.91)** | 0.80 (0.69, 0.93)** |
| Transmission concerns | 1.29 (1.10, 1.52)** | 1.31 (1.09, 1.57)** | 1.46 (1.23 1.73)** |
| Social distance | 1.54 (1.32, 1.80)** | 1.59 (1.33, 1.90)** | 1.39 (1.19, 1.62)** |
Resident, fellow, or attending physician
p < .10,
p < .05,
p < .01
The only statistically significant interaction was between transmission concerns and number of others in the home when predicting a positive screen for anxiety (p = .042). For participants living alone, transmission concerns were only marginally associated with anxiety, OR = 1.25, 95% CI [0.99, 1.56], p = .057. For those living with 3+ others, transmission concerns were positively associated with anxiety, OR = 2.01, 95% CI [1.41, 2.88], p < .001. Viewed differently, the association between living with others and anxiety was negligible for those self-reporting extreme distress regarding transmission concerns, OR = 0.96, 95% CI [0.51, 1.81], p = .90, whereas there was a negative association between number of others in the home and anxiety for those self-reporting no distress, OR = 0.51, 95% CI [0.27, 0.94], p = .032 (see Figure 1).
Figure 1.
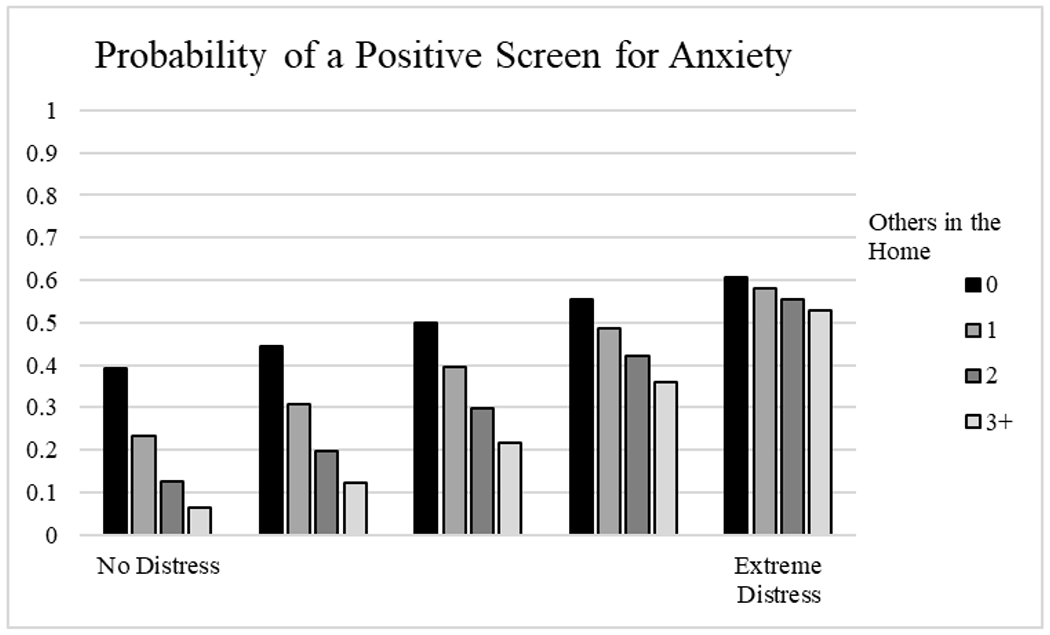
Interaction of others in the home with transmission concerns predicting a positive screen for anxiety.
In sensitivity analyses, as above, living with 1+ others modified the association between transmission concerns and a positive screen for anxiety, p = .021. In addition, living with 1+ others also modified the association of transmission concerns with a positive screen for acute stress, p = .013, and depression, p = .035. Transmission concerns were not associated with positive screens for psychological distress in those living alone (acute stress, OR = 0.98, 95% CI [0.73, 1.32], p = .91; depression, OR = 1.05, 95% CI [0.79, 1.39], p = .72), but these associations were positive and significant for those living with 1+ others (acute stress, OR = 1.58, 95% CI [1.27, 1.95], p < .001; depression, OR = 1.59, 95% CI [1.23, 2.06], p < .001).
Discussion
In a large sample of HCWs working at an academic medical center in NYC during the peak of the COVID-19 outbreak, distress regarding the potential to transmit COVID-19 to loved ones and keeping social distance from loved ones were associated with positive screens for psychological distress. The association between transmission concerns and screening positive for anxiety (and for acute stress and depression in sensitivity analyses), was only significant for individuals living with others. The number of others in the home was protective against positive screens for depression overall, and for anxiety in HCWs self-reporting no distress over transmission concerns.
Results underscore the paradoxical nature of social relationships during the COVID-19 pandemic. For HCWs, living with others may buffer the development of significant psychological distress. Concomitantly, fears associated with transmission and the need for social distancing increase psychological distress. To better support HCWs during the pandemic, it is critical to implement safeguards that reduce infection concerns in the home. Increasing access to personal protective equipment, frequent and rapid COVID-19 testing, telehealth implementation, and provision of free housing when working high-risk shifts could help to address these issues, as could problem-solving or stress reduction interventions. Strict workplace protective measures for HCWs during the Middle East respiratory syndrome (MERS) outbreak helped to alleviate distress (Khalid, Khalid, Qabajah, Barnard, & Qushmaq, 2016), and the ability to reduce infection risk to families mitigated concerns about exposing loved ones to pandemic influenza (Ives et al., 2009). Healthcare systems must protect HCWs in the workplace, and also help them to protect their family and maintain social support (Brooks et al., 2017; Thoits, 1995).
Limitations include lack of generalizability to non-urban settings, a largely female sample, and the cross-sectional nature of the data. Psychological distress symptoms were measured using brief screening questionnaires, limiting conclusions about symptom burden or psychiatric diagnosis. Data regarding workplace exposures and living arrangements (e.g., size of the living space, health status of cohabiting others) were unavailable. Future studies should explore nuances of the living situation that might exacerbate or ameliorate these associations, with the goal of creating safety in the home so that HCWs can reap the benefits of having support from loved ones and those they live with during rare, but severe public health crises such as the COVID-19 pandemic.
Acknowledgements
We thank our colleagues for their time and invaluable contributions to this study. We also wish to acknowledge the dedication and commitment of the staff, personnel, and healthcare workers at our institution for their care of patients, families, and our community during the NYC COVID-19 pandemic.
Funding:
Dr. Abdalla receives support through 18AMFDP34380732 from the American Heart Association and the NIH/NHLBI (K23HL141682-01A1and R01HL146636-01A1. Dr. Shechter receives support from NIH/NHLBI (R01HL141494 and R01HL146911). Dr. Cornelius receives support from NIH/NCATS (KL2 TR001874). Dr. Edmondson receives support from NIH from NIA U24AG052175 and P30AG064198, and NHLBI R01HL132347.
References
- Brooks SK, Dunn R, Amlôt R, Rubin GJ, & Greenberg N (2017). Social and occupational factors associated with psychological wellbeing among occupational groups affected by disaster: a systematic review. Journal of mental health, 26(4), 373–384. [DOI] [PubMed] [Google Scholar]
- Brooks SK, Dunn R, Amlôt R, Rubin GJ, & Greenberg N (2018). A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. Journal of occupational and environmental medicine, 60(3), 248–257. [DOI] [PubMed] [Google Scholar]
- Campo-Flores A (2020). What Does a Coronavirus Peak in New York Mean? The Wall Street Journal. Retrieved from https://www.wsj.com/articles/what-does-a-coronavirus-peak-in-new-york-mean-11586338201 [Google Scholar]
- Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, … Zhang Z (2020). Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry, 7(4), e15–e16. doi: 10.1016/S2215-0366(20)30078-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong E, Du H, & Gardner L (2020). An interactive web-based dashboard to track COVID-19 in real time. The Lancet infectious diseases. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellison A (2020). COVID-19 peak dates: Updated projections for each state. Retrieved from COVID-19 peak dates: Updated projections for each state [Google Scholar]
- Ives J, Greenfield S, Parry JM, Draper H, Gratus C, Petts JI, … Wilson S (2009). Healthcare workers’ attitudes to working during pandemic influenza: a qualitative study. BMC Public Health, 9(1), 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalid I, Khalid TJ, Qabajah MR, Barnard AG, & Qushmaq IA (2016). Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clinical medicine & research, 14(1), 7–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2003). The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care, 41(11), 1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB, Monahan PO, & Lowe B (2007). Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med, 146(5), 317–325. doi: 10.7326/0003-4819-146-5-200703060-00004 [DOI] [PubMed] [Google Scholar]
- Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, … Li R (2020). Factors associated with mental health outcomes among health care workers exposed to Coronavirus disease 2019. JAMA network open, 3(3), e203976–e203976. Retrieved from https://jamanetwork.com/journals/jamanetworkopen/articlepdf/2763229/lai_2020_oi_200192.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z, Ge J, Yang M, Feng J, Qiao M, Jiang R, … Wang L (2020). Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain, behavior, and immunity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C-Y (2020). Social reaction toward the 2019 novel coronavirus (COVID-19). Social Health and Behavior, 3(1), 1. [Google Scholar]
- Montemurro N (2020). The emotional impact of COVID-19: from medical staff to common people. Brain, behavior, and immunity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A, Ouimette P, Kimerling R, R.P C, D.S H, Shaw-Hegwer J … Sheikh J (2004). The primary care PTSD screen (PC-PTSD): Development and operating characteristics. International Journal of Psychiatry in Clinical Practice, 9, 9–14. doi: 10.1185/135525703125002360 [DOI] [Google Scholar]
- Shechter A, Diaz F, Moise N, Anstey DE, Ye S, Agarwal S, … Chang B (2020). Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. General hospital psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simione L, & Gnagnarella C (2020). Differences between health workers and general population in risk perception, behaviors, and psychological distress related to COVID-19 spread in Italy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoits PA (1995). Stress, coping, and social support processes: Where are we? What next? Journal of health and social behavior, 53–79. [PubMed] [Google Scholar]
- Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, … Lu R (2020). A novel coronavirus from patients with pneumonia in China, 2019. New England Journal of Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]


