Abstract
Innovations in electronic health record (EHR) systems invite new patient and family engagement methods and create opportunities to reduce healthcare disparities. However, many patients and their identified support persons (ie, proxies) are unsure how to interface with the technology. This phenomenological qualitative study served as a pilot study to investigate the patient, proxy, and provider lived experiences utilizing patient-facing EHR portals. Individual interviews and focus groups were utilized to collect qualitative data from 21 patient, proxy, and healthcare provider participants across 3 time points. Colaizzi's phenomenological data analysis method was utilized to interpret the data. Four themes emerged highlighting critical benefits and obstacles for patients and support persons interfacing with a patient portal: (a) agency, (b) connection, (c) support, and (d) technology literacy. Results help highlight strategies and dispel myths essential to advancing patient and family engagement using EHR patient portal systems. The study's outcomes reflect recommendations for onboarding proxies and improving patient/family engagement and family-centered care models.
Keywords: electronic health record, patient portal, family engagement, chronic health
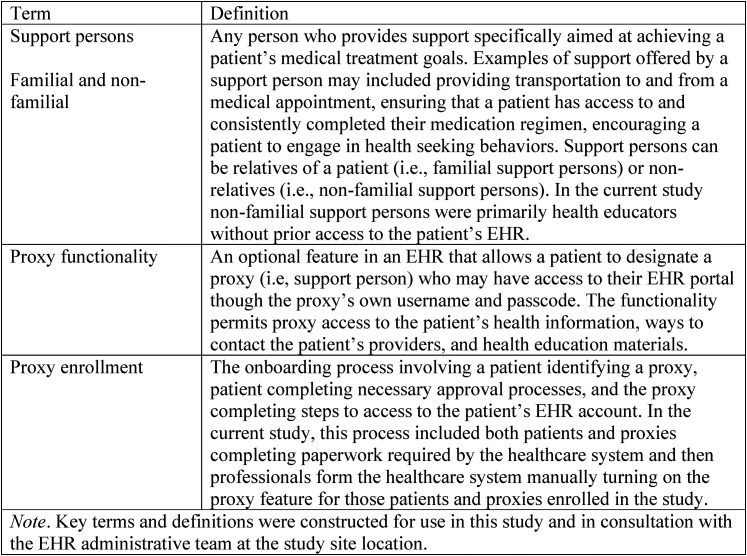
Electronic health records (EHR) were designed to safely store transactional patient information and increase communication among healthcare team members (1). Over time, patient-facing EHR portals invited patients to access their health information remotely and communicate with healthcare providers securely (2–9). A secondary analysis of the 2019 Health Information National Trends Survey found that more than 55% of patients use a portal to access their health record electronically (3). Portals demonstrated improved patient satisfaction, adherence to preventive protocols and treatment plans, better outcomes for chronic diseases, and lower healthcare costs for adult populations (10–19). Recently, researchers found health IT tools (eg, EHRs, patient portals, clinical decision support systems, telemedicine models) led to improvements in patient engagement, implementation of clinical guidelines, promotion of patient safety, and reduction of adverse outcomes among socioeconomically disadvantaged and underserved rural populations (20–22). However, despite these promising outcomes, familial and non-familial (see Figure 1 a glossary of terms) support persons frequently are left out of this engagement method (23–30).
Figure 1.
Key terms and definitions.
While support persons are interested in interacting with the portal system, there is uncertainty around how to do it safely and effectively (31–33). Support persons also report lacking a defined role in the healthcare partnership with patients and their providers (24), being unaware of patients’ specific health issues, treatment recommendations, care goals, lifestyle and medication treatment regimen adherence (34–37), and a lack of confidence in decision-making preferences (38,39). The portal may provide a bridge between what is happening inside and outside of the medical visit (40). Providers’ main source of subjective and observable data comes from the time spent with the patient during the medical visit. Patients spend majority of time interacting with systems and people outside of the medical visit who may or may not be supportive of reaching treatment goals. The portal functionality helps open up new opportunities for collecting and sharing important patient care information. However, unexplored barriers might explain its underutilization.
Innovative approaches are needed to understand portal utilization challenges better (41). Barriers identified in the literature include: (a) enrollment and technological support, (b) user's limited experience with or access to technology, (c) language difficulties, and (d) literacy challenges. Removing these barriers helps form stronger partnerships with healthcare professionals (42), engages patients in care (18), and aids support persons who may need to serve as decision makers (25,43–45). However, no known peer-reviewed literature has examined EHR utilization experiences simultaneously from patient, support person (ie, proxy), and provider perspectives. Therefore, the purpose of this study was to gather the lived experiences of patients, healthcare team members, and proxies utilizing patient-facing EHR portals to understand what barriers inhibit its utilization.
Method
A combined phenomenological and focus group design (46) was used to study participants’ lived experiences interacting with the proxy functionality of an EHR system. Data collection from patients, proxies (ie, familial or non-familial support persons designated by patients), and healthcare providers helped triangulate findings across participant groups. All participants were recruited from the same primary care clinic to ensure that the data reflected the same EHR patient portal system and enrollment procedures. Patient, proxy, and provider data was collected individually and over the phone at 3 different time points: (a) before proxy enrollment, (b) 1 month after proxy enrollment or after the last proxy enrollment for providers, and (c) 3 months after proxy enrollment or after all patient and proxy interviews for providers. IRB approval was obtained before patient recruitment.
Participants
A purposive sampling strategy was used to recruit and enroll participants, age 18 or older, who met the following inclusion criteria: (a) a patient of the selected primary care clinic, (b) a patient-identified proxy (familial or non-familial), or (c) a primary healthcare provider of a participating patient. In addition, patient participants had to have 1 or more chronic health conditions. Exclusion criteria were: (a) patients or proxies who were employees of the primary care clinic, (b) patient participants without a proxy enrolled, (c) patient participants who did not wish to enroll in the EHR patient portal system, (d) demonstration of mental confusion or illness (eg, dementia, psychosis, mania) that would compromise the participant's ability to provide consent, (e) healthcare providers who did not have a patient enrolled in the study, and (f) not fluent in spoken or written English.
Patient participants were informed of their voluntary opportunity to participate in the study during their office visit. If patients expressed interest in participating, a research team member contacted them, and an office staff member helped enroll the patient in the patient portal. If they declined to participate in the study, office staff still supported registration in the patient portal.
Twenty patients expressed interest in participating during the 1-month recruitment period, but 8 did not complete the study. Those declining citied a cumbersome proxy onboarding process. Twelve patients, 7 proxies, and 3 providers were enrolled in the study (Table 1). The number of patients and support persons interviewed was determined using theoretical saturation. Patients who agreed to participate were asked to invite a proxy to participate. Patients provided the name and contact information of their chosen support person (ie, proxy) to the research team. It is important to note that the patient was solely responsible for granting proxy access to their EHR portal and permission to view patient health information, which prevented this study from threatening patient confidentiality or privacy. Once the patient provided contact information for the proxy, the researcher contacted the potential proxy participant to explain the study, emailed them the REDCap link to the informed consent and demographic survey, and scheduled them for an individual interview. If any patient or proxy participant struggled with completing the paperwork for proxy access, a member of the research team was available to meet with them in person at the clinic to assist. Since the paperwork was not available electronically, this was a barrier that the research team needed to address. Interestingly, 5 patient participants identified the same non-familial proxy. This proxy was an off-site healthcare professional (diabetes educator) who did not have EHR access. Three provider participants enrolled in the study, but only 2 completed all 3 focus groups due to 1 provider not having any patients enrolled in the study.
Table 1.
Demographic Characteristics of Patients, Proxies, and Providers.
| Characteristic | Patients (n = 12) | Proxies (n = 7) | Providers (n = 2) |
|---|---|---|---|
| Race | |||
| Non-Hispanic White | 5 (41%) | 4 (57%) | 2 (100%) |
| Black, Afro-Caribbean, African American | 5 (41%) | 2 (28%) | |
| Native American, Alaskan Native | 1 (8%) | 1 (8%) | |
| Latino, Hispanic American | 1 (8%) | ||
| Gender | |||
| Male | 6 (50%) | 1 (50%) | |
| Female | 6 (50%) | 7 (100%) | 1 (50%) |
| Non-binary | |||
| Other | |||
| Age in years | 26–68 | 25–64 | 41 |
| (M = 51.6; SD = 10.5) | (M = 48.1; SD = 11.4) | ||
Data Collection
Patient, proxy, and provider participants virtually provided their informed consent and completed an online demographic questionnaire through REDCap, a HIPAA compliant data collection tool (47). Participants were given pseudonyms to protect their confidentiality. Semi-structured individual and focus group interviews were used to obtain a detailed description of each participant's lived experience. The demographic tool and questionnaire used for the study are available by contacting the corresponding author. Focus groups were used for provider-level data as the study was about their overall experience. One investigator conducted all the interviews, and the same 3 investigators analyzed the data. Patient and proxy interviews were conducted over the phone and provider focus groups were conducted in person to help reduce barriers in participation. Many patients and proxies did not live close to the clinic so conducting the interviews in person was not realistic. Providers were interviewed in person. A pre-study meeting with clinic administration and providers confirmed that this format was more conducive. Participants who completed all 3 study phases were presented with a $25 online gift card as an incentive.
Analysis
A modified 7-step method for phenomenological qualitative data analysis was used in this study (48). The analysis process consists of (a) reading each transcript, (b) identifying significant statements, (c) forming meaning statements from the significant statements, (d) clustering themes from the meaning statements and forming emerging themes, and (e) creating an exhaustive description. Investigators each maintained and referenced their reflexive journals and audit trails while collecting and analyzing the data to increase the trustworthiness of the findings. They also completed bias statements documenting their beliefs and biases about what the investigation may yield and revisited those at each data analysis stage.
A third-party transcription service transcribed interviews. Each transcript was checked for accuracy by the investigator who conducted the interview. During data analysis, investigators extracted meaningful statements of each transcript independently and then compared results. When they encountered coding differences, they would discuss until an agreement was reached. In 2% of instances, a third researcher (ie, peer debriefer) was brought in to help reach an agreement. Interrater agreement was 100% after this process.
Results
Analysis of qualitative data collected from patients, proxies, and provider participants yielded 4 salient themes: (a) agency, (b) connection, (c) support, and (d) technology literacy. A final exhaustive description and statement of identification were formulated from these 4 thematic areas. A table of themes and example quotes demonstrate how the findings are grounded in the actual data (Table 2).
Table 2.
Experiences of Patients, Proxies, and Providers Utilizing the Patient Portal Feature.
| Key themes and subthemes | Sample quotes |
|---|---|
| Agency | “I giveth and taketh away [proxy access]”—Patient |
| “I think the benefits [of proxy access] are numerous … having the patient becoming more engaged with their own disease process and having the support person help hold a patient accountable.”—Provider | |
| “I really want my folks [parents]to be self-managers, so I really encourage … them to go look for their [medical information] on their [MyChart].”—Proxy | |
| Connection | “I think the objective of having everybody on the same page and seeing the same health information. I think is the most beneficial [part of proxy access].”—Patient |
| “So when we walk in [to the patient's appointment] we’re doing a bit of that trying to gauge. Are [the patient and the support person in the room with the patient] really working together for the patient's condition.”—Provider | |
| “I mean it's been nice to have access without having to use [patient's] login information because I know that's not really the right thing to do. This makes me feel like [the patient] gave me permission to [access patient's EHR].”—Proxy | |
| Support | “Without my [proxy] I don't know where I’d be.”—Patient |
| “But a lot of times, even if the patient with diabetes is very knowledgeable about what [medications] they are taking, it can still be overwhelming. Having the support person … to help comfort [the patient].”—Provider | |
| “I think that's very good to have somebody you know because diabetes is like a roller coaster … it is hard to manage … So it's important to take your medicines as direct and keep your appointments regularly but it's also important to have good support.”—Provider | |
| “There's not really been, anything that I felt like I needed [from the patient's EHR].”—Proxy | |
| Technology literacy | |
| Comfortability | “Anything dealing with a computer is not for me.”—Patient |
| “I use the Patient Portal a huge amount! I think we [providers] all do.”—Provider | |
| “I’m not the fastest that the computer but I am getting it.”—Proxy | |
| Utilization | “Even if an elderly [patient] never uses it, if you just get [EHR and proxy access] set up and get the proxy going, somebody can keep up with [the patient's records].”—Provider |
Agency
Across all 3 interview phases, participants discussed proxy access in relation to patient agency (ie, retention of patient voices and control over their health information). While some providers voiced initial concerns that patients would feel undermined by sharing their medical records with their proxies, patients reported the opposite. Patients said that proxy access resulted in an increased sense of agency and no concerns disclosing their medical information. Patients liked being able to select their proxies rather than leaving it to providers to decide with whom they disclosed patient information. Proxies described making a conscious effort to respect the patient's agency and only accessed relevant medical information as needed. As a result, several patients explained that having a proxy increased their sense of control (ie, selecting and taking take away proxy access if required) and desire to engage more in their care.
Connection
Patients, proxies, and providers reported that connection was an essential benefit of proxy access. It created a vehicle for patients and proxies to access the same information instead of patient recall or interpretation. Eliminating the “middleman” resulted in more efficient provider-to-proxy and patient-to-proxy communication. Proxies and patients also explained that proxy access resulted in more honest communication between patients and proxies about the patients’ current health status. Several patients explained that before proxy access, patients might have provided a vague response about a specific lab result to avoid the subject. However, proxies’ access to lab test results eliminated the avoidant behavior and led to more honest and open communication.
While the level of proxy support varied across the second and third data collection time points, proxy access allowed them to engage at a level tailored to the individual patient and proxy's needs. For example, some proxies accessed the portal multiple times a week, whereas others reported only checking it every few months or after a medical appointment. Regardless of the level of support provided, proxies reported EHR access allowed them to provide better support. Before being granted access, proxies reported trying to support patients by logging into the EHR through the patient's account. Many proxies expressed feeling uncomfortable with this process and preferred having their own access for a more transparent and open connection.
Providers explained that having patients identify a proxy reduced diagnostic and treatment ambiguity and invited better engagement. Providers described wanting to engage support persons in patient care but were unsure who to contact and who would best fit this role in the patients’ lives. They also reported that they were unsure how much health information the patient would want the support person to know before the proxy process. By having patients identify a specific proxy person, providers could better engage the proxy, leading to an increased sense of connection between patients, proxies, and providers. Furthermore, providers also explained that the increased connection was beneficial for office workflow (ie, reducing phone calls, no-shows, and cancellations) and building connections with proxies to benefit patient care.
Support
Patients, proxies, and providers placed a high value around patient support through proxy engagement. This was especially true for patients who experienced a chronic illness, as providers noted that chronic illnesses often create unique long-term support needs for patients and sometimes proxies. Providers explained that patients benefit from proxy support at every point throughout care, from receiving a diagnosis to management of daily healthcare tasks. Additionally, providers described the importance of forming “partnerships” with proxies to reach the patients’ targeted health goals.
Patients and proxies described feeling as though proxy access also provided “peace of mind” by allowing access to the patients’ medical records (eg, up-to-date medication list) in case of an emergency. They highlighted how proxy access assisted with: (a) communicating with the healthcare team, (b) reviewing lab results, (c) scheduling appointments, and (d) filling and picking up mediation refills. Patients also explained that having another person, outside of their provider, connected to their health information through a formal process (ie, proxy access) motivated them to achieve their health goals.
Technology Literacy
Interacting with the patient portal technology was a common barrier among patients and familial proxies. Interestingly, patients and proxies who did not consent to participate also cited it as a reason for not enrolling in the study. The analysis yielded 2 sub-themes connected to technology literacy: (a) comfortability and (b) utilization.
Comfortability
While providers reported high literacy levels and comfortability with the EHR, patient and proxy comfort fell along a continuum from significant discomfort to highly comfortable. In the first focus group, providers anticipated that older proxies (age 65 and older) would not engage through the portal as much as younger proxies. However, this was not reported to be true in later interviews with proxies or providers. Age did not appear to be a limiting factor. Some patients self-identified as a “frequent user” of the EHR before participating in the study, while others were not (and had no intention of) using the EHR at all. Despite this variability, patients with lower technology literacy or desirability were still able to experience the benefits of the EHR by selecting a proxy who was motivated to learn the functionality of the EHR to help the patient achieve their health goals.
Utilization
After proxy access was granted, utilization varied. Some patient and proxy participants self-identified as a “frequent user,” and others had little to no use of the EHR across all 3 study periods. Patients and proxies familiar with the EHR, and those who previously used it, reported the following functions as beneficial: (a) reviewing billing, (b) accessing the medication list, (c) communicating with the healthcare team, (d) scheduling and confirming appointments, and (e) checking lab results. However, patients and proxies less familiar with the EHR reported the billing and scheduling functions as confusing and challenging to navigate. Providers reported that utilization was not a disruption to their workflow or an impediment to providing exemplary patient care. They were surprised to discover that proxy access led to more efficient communication overall.
Exhaustive Description
Patient participants expressed a desire for proxy involvement and valued proxy portal access. Granting proxy access increased patient accountability and engagement. Likewise, proxies reported an increased desire to support patients in achieving their health goals, from checking on labs to communicating with the patient's healthcare provider through the portal's email function. Age was not a factor in proxy comfort using the EHR portal. Accessing the proxy function of the patient portal enabled proxies to support the patient more efficiently and effectively in following their treatment plan. While initially apprehensive, providers were eager to support patients in activating their patient EHR accounts and establishing a proxy. They found it did not disrupt workflow and resulted in more meaningful and effective communication without redundancy. The proxy feature appeared to remove ambiguity and dispel myths for all participants about using patient portal technology. While proxies and providers worried patient agency would be taken away using this technology, all participants reported the proxy feature enhanced it through more active engagement among all stakeholders.
Discussion
This pilot study explored participants’ lived experiences interacting with the proxy functionality of an EHR system. It was the first known study to include patients’, proxies’, and providers’ experiences from the same clinical context. Determining who will be a proxy in a patient's care and the proxy's level of involvement is the patient's responsibility. As part of a patient-centered focus in healthcare, shared power and responsibility between the provider and the patient must be maintained through the decision-making period (47). In this study, patients selected the proxy that would take an active role in their care. In some cases, this was not a family member but another healthcare professional who did not document in the same EHR system. Recognizing this intentionality in choosing a support person reinforces the value of EHR communication technology (24). While agency must be granted to the patient in selecting a proxy, the healthcare team must recognize that proxy involvement is not a replacement for communication with the patient (47). This study reinforces the finding that proxy involvement in EHR communication is a means of supporting patient outcomes (26). A unique aspect of this study is how it counters the myth that age and technology literacy are the most significant barriers to patient portal usage. Alternatively, this study discovered that a cumbersome enrollment protocol and lack of a defined role for the proxy might have been the greatest barriers.
Research investigating the use of the EHR to improve collaboration between patients, proxies, and providers requires all stakeholder groups to be represented in patient portal and proxy access studies. This study takes a novel approach to involving patients and providers in understanding the use of the EHR to improve collaboration with patients’ identified support persons. It is the first known study to include this in its methodology. While involving patients in their care through patient portals has demonstrated success in improving outcomes (10–12), the involvement of a support person in care through the EHR is necessary for patients with more complex diagnoses (23). This involvement does not come without its complexities. Success in involving stakeholders outside the patient and provider relationship requires a new look at patient, proxy, and provider readiness for communication through the EHR.
Implications
This study has several implications for healthcare organizations. The design of EHR portal features that facilitate patient, proxy, and provider communication must ensure the registration process is efficient. A burdensome process for proxy registration and barriers to access (eg, restricted internet access) may prevent utilization despite the benefits of the feature. Policies that reduce disparities caused by geographic proximity issues and internet access are essential to growing patient/proxy portal usage. An additional implication is developing training for healthcare providers on using the EHR proxy feature as a tool for engaging families, reducing health disparities, and improving patient care while dispelling the myth of age as a barrier.
Limitations
This study does have limitations. While this study was done with a patient, proxy, and provider sample, and data collection took place over 3 time periods, it was conducted within one rural primary care clinic. Therefore, the findings may not be generalizable to all primary or specialty care settings. Studying the benefits and challenges of proxy access in a wide variety of healthcare settings may help design policies and proxy engagement protocols that best fit the context, population, and health conditions. As is the case with many research studies, patients from the current study self-selected to participate. While this is representative of the real life proxy access process (ie, patients will self-select their proxy and may choose whether or not their proxy has access to the proxy function within the EHR portal) it should be noted that there will likely be patients who would not choose to give a support person proxy access. Proxy access may not be a desirable resource for every patient. Patient agency should be honored and maintained whenever possible should a healthcare system offer the EHR proxy feature.
Conclusion
This study is the first known to collect data from patients, proxies, and providers in the same context about the benefits of using the patient portal to enhance the patient care experience. Researchers learned that using the EHR proxy feature dispelled myths that it would violate patient agency and require too much time and demonstrated important benefits to the patient–proxy and proxy–provider relationships. Researchers also learned that patients and providers experienced the proxy feature as a positive resource for building connection between the patient, support person, and healthcare providers, as well as increasing their confidence in treatment plan success. While exploratory, more studies like this one are needed to identify the ways EHR technology such as patient portals can reduce disparities and add value to the patient, proxy, and provider healthcare experience.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Jennifer Hodgson https://orcid.org/0000-0001-5363-0215
Emily Tucker https://orcid.org/0000-0002-1660-2722
References
- 1.Garrett P, Seidman J. EMR vs EHR – What is the Difference? Health IT Buzz. 2011. https://www.healthit.gov/buzz-blog/electronic-health-and-medical-records/emr-vs-ehr-difference.
- 2.Archer N, Fevrier-Thomas U, Lokker C, McKibbon KA, Straus SE, Personal health records: a scoping review. J Am Med Inform Assoc. 2011;18(4):515‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Raj M, Iott B. Evaluation of family caregivers’ use of their adult care recipient’s patient portal from the 2019 health information national trends survey: secondary analysis. JMIR Aging. 2021;4(4):e29074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ, Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13(2):121‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weingart SN, Rind D, Tofias Z, Sands DZ, Who uses the patient internet portal? The PatientSite experience. J Am Med Inform Assoc. 2006;13(1):91‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nazi KM, Woods SS. Myhealthevet PHR: a description of users and patient portal use. AMIA Annu Symp Proc. 2008:1182. [PubMed] [Google Scholar]
- 7.Kaelber D, Pan EC. The value of personal health record (PHR) systems. AMIA Annu Symp Proc. 2008:343‐7. [PMC free article] [PubMed] [Google Scholar]
- 8.Detmer D, Bloomrosen M, Raymond B, Tang P, Integrated personal health records: transformative tools for consumer-centric care. BMC Med Inform Decis Mak. 2008;8(1):45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ralston JD, Hereford J, Carrell D. Use and satisfaction of a patient Web portal with a shared medical record between patients and providers. AMIA Annu Symp Proc. 2006:1070. [PMC free article] [PubMed] [Google Scholar]
- 10.Lin CT, Wittevrongel L, Moore L, Beaty BL, Ross SE, An internet-based patient-provider communication system: randomized controlled trial. J Med Internet Res. 2005;7(4):e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krist AH, Woolf SH, Rothemich SF, Johnson RE, Peele JE, Cunningham TD, et al. Interactive preventive health record to enhance delivery of recommended care: a randomized trial. Ann Fam Med. 2012;10(4):312‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wright A, Poon EG, Wald J, Feblowitz J, Pang JE, Schnipper JL, et al. Randomized controlled trial of health maintenance reminders provided directly to patients through an electronic PHR. J Gen Intern Med. 2012;27(1):85‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Green BB, Cook AJ, Ralston JD, Fishman PA, Catz SL, Carlson J, et al. Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. 2009;302(18):1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ralston JD, Hirsch IB, Hoath J, Mullen M, Cheadle A, Goldberg HI, Goldberg HI, Web-based collaborative care for type 2 diabetes: a pilot randomized trial. Diabetes Care. 2009;32(2):234‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tang PC, Overhage JM, Chan AS, Brown NL, Aghighi B, Entwistle MP, et al. Online disease management of diabetes: engaging and motivating patients online with enhanced resources-diabetes (EMPOWER-D), a randomized controlled trial. J Am Med Inform Assoc. 2013;20(3):526‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Simon GE, Ralston JD, Savarino J, Pabiniak C, Wentzel C, Operskalski BH, Randomized trial of depression follow-up care by online messaging. J Gen Intern Med. 2011;26(7):698‐704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goldzweig CL, Orshansky G, Paige NM, Towfigh AA, Haggstrom DA, Miake-Lye I, et al. Electronic patient portals: evidence on health outcomes, satisfaction, efficiency, and attitudes: a systematic review. Ann Intern Med. 2013;159(10):677‐87. [DOI] [PubMed] [Google Scholar]
- 18.de Lusignan S, Mold F, Sheikh A, Majeed A, Wyatt JC, Quinn T, et al. Patients’ online access to their electronic health records and linked online services: a systematic interpretative review. BMJ Open. 2014;4(9):e006021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Forbat L, Cayless S, Knighting K, Cornwell J, Kearney N, Engaging patients in health care: an empirical study of the role of engagement on attitudes and action. Patient Educ Couns. 2009;74(1):84‐90. [DOI] [PubMed] [Google Scholar]
- 20.Perez-Stable EJ, Jean-Francois B, Aklin CF. Leveraging advances in technology to promote health equity. Med Care. 2019;6(S2):S101‐3. Crossref, Google Scholar. [DOI] [PubMed] [Google Scholar]
- 21.Institute of Medicine. Health IT and patient safety: Building safer systems for better care, 2012. Accessed January 8, 2018. https://pubmed.ncbi.nlm.nih.gov/24600741/. Google Scholar
- 22.National Academy of Medicine. Optimizing Strategies for Clinical Decision Support: Summary of a Meeting Series. Washington, DC: National Academy of Medicine; 2017. Accessed January 8, 2018. https://nam.edu/optimizing-strategies-clinical-decision-support/. Google Scholar [PubMed] [Google Scholar]
- 23.Cené CW, Johnson BH, Wells N, Baker B, Davis R, Turchi R, A narrative review of patient and family engagement: the “foundation” of the medical home”. Med Care. 2016;54(7):697‐705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vick JB, Amjad H, Smith KC, Boyd CM, Gitlin LR, Roth DL, “Let him speak:” a descriptive qualitative study of the roles and behaviors of family companions in primary care visits among older adults with cognitive impairment. Int J Geriatr Psychiatry. 2018;33(1):e103‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aikens JE, Trivedi R, Heapy A, Pfeiffer PN, Piette JD, Potential impact of incorporating a patient-selected support person into mHealth for depression. J Gen Intern Med. 2015;30(6):797‐803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Piette JD, Striplin D, Marinec N, Chen J, Trivedi RB, Aron DC, et al. A mobile health intervention supporting heart failure patients and their informal caregivers: a randomized comparative effectiveness trial. J Med Internet Res. 2015;17(6):e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wolff JL, Berger A, Clarke D, Green JA, Stametz R, Yule C, Patients, care partners, and shared access to the patient portal: online practices at an integrated health system. J Am Med Inform Assoc. 2016;23(6):1150‐8. [DOI] [PubMed] [Google Scholar]
- 28.Wolff JL, Darer JD, Larsen KL. Family caregivers and consumer health information technology. J Gen Intern Med. 2016;31(1):117‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wolff JL, Darer JD, Berger A, Clark D, Green JA, Stametz RA, et al. Inviting patients and care partners to read doctors’ notes: OpenNotes and shared access to electronic medical records. J Am Med Inform Assoc. 2017;24(e1):e166‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sarkar U, Bates DW. Care partners and online patient portals. JAMA. 2014;311(4):357‐8. [DOI] [PubMed] [Google Scholar]
- 31.Goel MS, Brown TL, Williams A, Cooper AJ, Hasnain-Wynia R, Baker DW, Patient reported barriers to enrolling in a patient portal. JAMIA. 2011;18(Suppl 1):i8‐i12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim E, Stolyar A, Lober WB, Herbaugh A, Shinstrom SE, Zierler BK, Challenges to using an electronic personal health record by a low-income elderly population. J Med Internet Res. 2009;11(12):e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Walker J, Leveille SG, Ngo L, Ross SE, Delbanco T, Ngo L, et al. Inviting patients to read their doctors’ notes: patients and doctors look ahead: patient and physician surveys. Ann Intern Med. 2011;155(12):811‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Almborg A, Ulander K, Thulin A, Berg S, Discharge planning of stroke patients: the relatives’ perceptions of participation. J Clin Nurs. 2009;18(6):857‐65. [DOI] [PubMed] [Google Scholar]
- 35.Rosland A, Heisler M, Janevic MR, Connell CM, Langa KM, Kerr EA, et al. Current and potential support for chronic disease management in the United States: the perspective of family and friends of chronically ill adults. Fam Sys Health. 2013;31(2):119‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kernisan LP, Sudore RL, Knight SJ. Information-seeking at a caregiving website: a qualitative analysis. J Med Internet Res. 2010;12:e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Forbes TH, Hodgson J, Crespo J, Jones E, Hardee S, et al. Putting the pieces together: an exploration of diabetes ketoacidosis readmissions. Contemp Fam Ther. 2020;42(4):436‐45. [Google Scholar]
- 38.Vig E, Starks H, Taylor J, Hopley E, Hopley EK, Fryer-Edwards K, et al. Surviving surrogate decision-making: what helps and hampers the experience of making medical decisions for others. JGIM. 2007;22(9):1274‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wendler D, Rid A. Systematic review: the effect on surrogates of making treatment decisions for others. Ann Intern Med. 2011;154(5):336‐46. [DOI] [PubMed] [Google Scholar]
- 40.Otte-Trojel T, de Bont A, Rundall TG, Klundert J, How outcomes are achieved through patient portals: a realist review. J Am Med Inform Assoc. 2014;21(4):751‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Manias E, Bucknall T, Wickramasinghe N, Gray K, Schaffer J, Rosenfeld E, Patient and family engagement in communicating with electronic medical records in hospitals: a systematic review. Int J Med Inform. 2020;134:104036. [DOI] [PubMed] [Google Scholar]
- 42.Mitnick S, Leffler C, Hood V. Family caregivers, patients and physicians: ethical guidance to optimize relationships. J Gen Intern Med. 2010;25(3):255‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Piette JD, Gregor MA, Share D, Dirmaier J, et al. Improving heart failure self-management support by actively engaging out-of-home caregivers: results of a feasibility study. Congest Heart Fail. 2008;14(1):12‐8. [DOI] [PubMed] [Google Scholar]
- 44.Pope TM. Legal fundamentals of surrogate decision making. Chest. 2012;141(4):1074‐81. [DOI] [PubMed] [Google Scholar]
- 45.Wittenberg-Lyles E, Oliver DP, Kruse RL, Demirls G, Gage LA, Wagner K. Family caregiver participation in hospice interdisciplinary team meetings: how does it affect the nature and content of communication? Health Commun. 2013;28(2):110‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Creswell JW. Qualitative Inquiry and Research Design: Choosing Among Five Approaches. 3rd ed. Los Angeles: Sage Publications; 2013. [Google Scholar]
- 47.Langberg EM, Dyhr L, Davidsen AS. Development of the concept of patient-centeredness: a systematic review. Patient Educ Couns. 2019;102(7):1228‐36. [DOI] [PubMed] [Google Scholar]
- 48.Colaizzi PF. Psychological research as a phenomenologist views it. In: Valle RS, King M, eds. Existential-Phenomenological Alternatives for Psychology. New York: Oxford University Press; 1978:48‐71. [Google Scholar]