Abstract
Background:
Previous clinical studies have shown that psychological factors have significant effects on an athlete’s readiness to return to sport after anterior cruciate ligament (ACL) reconstruction (ACLR).
Hypothesis:
We hypothesized that patients who underwent bridge-enhanced ACL restoration (BEAR) would have higher levels of psychological readiness to return to sport compared with patients who underwent ACLR.
Study Design:
Randomized controlled trial; Level of evidence, 1.
Methods:
A total of 100 patients (median age, 17 years; median preoperative Marx activity score, 16) with complete midsubstance ACL injuries were randomized to either the BEAR procedure (n = 65) or autograft ACLR (n = 35 [33 hamstring and 2 bone--patellar tendon—bone]) and underwent surgery within 45 days of injury. Objective, functional, and patient-reported outcomes, including the ACL--Return to Sport after Injury (ACL-RSI) scale, were assessed at 6, 12, and 24 months postoperatively.
Results:
Patients who underwent the BEAR procedure had significantly higher ACL-RSI scores at 6 months compared with those who underwent ACLR (71.1 vs 58.2; P = .008); scores were similar at 12 and 24 months. Baseline factors independently predictive of higher ACL-RSI scores at 6 months were having a BEAR procedure and participating in level 1 sports prior to injury, explaining 15% of the variability in the scores. Regression analysis of baseline and 6-month outcomes as predictors indicated that the International Knee Documentation Committee (IKDC) score at 6 months explained 45% of the 6-month ACL-RSI variance. Subsequent analysis with IKDC excluded from the model indicated that decreased pain, increased hamstring and quadriceps strength in the surgical limb, and decreased side-to-side difference in anteroposterior knee laxity were significant predictors of a higher ACL-RSI score at 6 months, explaining 34% of the variability in scores. Higher ACL-RSI score at 6 months was associated with earlier clearance to return to sports.
Conclusion:
Patients who underwent the BEAR procedure had higher ACL-RSI scores at 6 months postoperatively. Better ACL-RSI scores at 6 months were related most strongly to higher IKDC scores at 6 months and were also associated with lower pain levels, better muscle recovery, and less knee laxity at 6 months.
Registration:
NCT02664545 (ClinicalTrials.gov identifier).
Keywords: ACL reconstruction, anterior cruciate ligament, ACL-RSI, BEAR, bridge-enhanced ACL restoration, psychological readiness, return to sport
Return to preinjury level of activity after anterior cruciate ligament (ACL) reconstruction (ACLR) has been studied extensively, as it is widely considered a primary outcome for athletes. However, up to two-thirds of patients are unable to return to their preinjury level of sports participation by 1 year after surgery, even if they have achieved satisfactory functional outcomes. 2 This discrepancy has led to the investigation of other factors influencing return to activity, including psychological factors.
Over the past decade, studies have shown that psychological factors have a significant effect on an athlete’s readiness to return to sports after ACLR. 1 –3,9,10,13,18,20,21 Psychological factors commonly reported include lack of confidence in the knee, fear of a reinjury, loss of self-esteem, and suboptimal locus of control. 1,3,8,10,13,18,20,21 The ACL—Return to Sport after Injury (ACL-RSI) scale was developed as a patient-reported outcome measure of psychological readiness to return to sports, and it has been validated in patients with ACL injury. 38 This scale assesses psychological readiness by evaluating emotions, confidence in performance, and risk appraisal.
ACLR in young athletes typically incorporates harvest of either 2 of the ipsilateral hamstring tendons or part of the extensor mechanism. 22 Patients may experience postoperative pain and weakness of the musculature associated with the harvest site as a result. 28 –30 Bridge-enhanced ACL restoration (BEAR) is a new ACL restorative technique in which graft harvest is not necessary, thus eliminating donor-site morbidity. 29,30 The BEAR procedure utilizes a collagen scaffold to aid in direct repair of the ACL. The 2-year primary results of the BEAR II prospective randomized clinical trial were published recently 28 and indicated that the BEAR technique was not inferior to an autograft ACLR when considering International Knee Documentation Committee (IKDC) subjective scores and side-to-side differences in anteroposterior (AP) knee laxity. 16,28 An important finding in a follow-up study was that patients with BEAR demonstrated superior hamstring strength across all postoperative assessments (3, 6, 12, and 24 months) and greater hip adductor strength overall compared with patients with ACLR, most of whom underwent hamstring graft harvest. 4 Given the faster physical recovery with regard to strength in patients with BEAR, we suspected these patients may also recover faster from a psychological perspective.
The primary purpose of this secondary analysis was to compare the postoperative psychological readiness of patients who were randomized to receive the BEAR procedure versus patients who were randomized to receive autograft ACLR in the previously referenced BEAR II trial. 28 Our primary hypothesis was that patients in the BEAR group would achieve higher levels of psychological readiness to return to sports compared with the ACLR group at 6, 12, and 24 months postoperatively and that the 2 groups would demonstrate different temporal trends in psychological readiness over time. Our secondary hypothesis was that baseline patient characteristics (level of sports played, age, sex, body mass index [BMI], etc) as well as level of function at 6 months postoperatively (pain scores, patient-reported outcomes, and strength and functional measurements) would correlate with the degree of psychological readiness in patients, regardless of the type of ACL surgical procedure. Finally, we hypothesized that patients with higher psychological readiness would be cleared to return to sports sooner in their postoperative course.
Methods
The methods of this randomized controlled BEAR trial have been reported previously. 28 The trial (BEAR II Trial; ClinicalTrials.gov identifier: NCT02664545) consisted of 100 patients undergoing surgery for an acute ACL injury (surgery within 45 days of injury). Institutional review board (IRB) approval (IRB-P00021470) and US Food and Drug Administration approval (IDE G150268) were obtained before the start of the BEAR II Trial, and all patients provided informed consent.
Patients
Between May 2016 and June 2017, a total of 100 patients were randomized in an approximate 2:1 ratio to undergo either the implant-enhanced ACL restoration procedure (BEAR group; 65 patients) or autograft ACLR (ACLR group; 35 patients) (Figure 1). Randomization was stratified by the surgeon’s preference for autograft source (hamstring or bone--patellar tendon—bone) and administered by the research coordinators using sealed envelopes from the statistician. Eligible patients were aged 13 to 35 years and had a complete ACL tear, were <45 days from injury, had closed physes, and had a tibial stump that spanned at least 50% of the distance from the tibial to the femoral insertion site of the ACL as measured on a sagittal view on the preoperative magnetic resonance imaging scan. Patients were excluded if they had a history of previous ipsilateral knee surgery, previous knee infection, or risk factors that could adversely affect ligament healing (nicotine/tobacco use, corticosteroids in the past 6 months, chemotherapy, diabetes, inflammatory arthritis). Patients were also excluded if they had a displaced bucket-handle tear of the meniscus requiring repair; patients with all other meniscal injuries were included. Finally, patients were excluded if they had a full-thickness chondral injury, a grade 3 medial collateral ligament injury, a concurrent complete patellar dislocation, or an operative posterolateral corner injury. All patients were enrolled at Boston Children’s Hospital, and patient recruitment was completed over 12 months.
Figure 1.
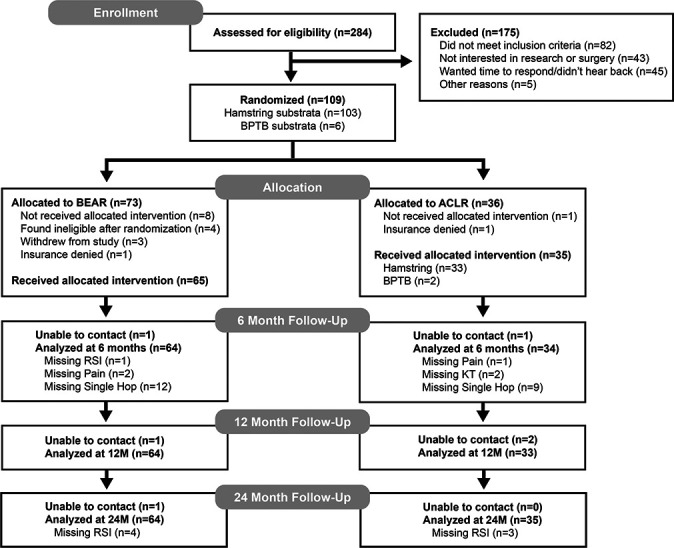
CONSORT (Consolidated Standards of Reporting Trials) diagram detailing patient flow through the study. ACL, anterior cruciate ligament; ACLR, ACL reconstruction; BEAR, bridge-enhanced ACL restoration; BPTB, bone--patellar tendon–bone; KT, KT-1000 arthrometer testing; M, months; RSI, ACL--Return to Sport after Injury.
Surgical Procedures and Postoperative Rehabilitation
The BEAR group underwent a BEAR procedure as previously described. 31 In brief, a whipstitch (Vicryl; Ethicon) was placed in the tibial stump and combined with a polyester suture stent (Ethibond; Ethicon) and the BEAR implant (Boston Children’s Hospital) to repair the ACL. The ACLR group underwent a standard ACLR, also as previously described, 28 using a quadrupled hamstring autograft (n = 33; 94.3%) or central-third bone--patellar tendon--bone autograft (n = 2; 5.7%) per surgeon preference. In the ACLR group, femoral fixation was accomplished via a continuous loop cortical button, and tibial-sided fixation was performed using a bioabsorbable interference screw.
An identical physical therapy protocol, adapted from that of the Multicenter Orthopaedic Outcomes Network, 40,41 was provided to all patients. The physical therapists were not informed of the treatment assignment. For all patients, a locking hinged brace (TScope; Breg) was applied postoperatively to limit joint range of motion to between 0° and 50° of knee flexion for 2 weeks and from 0° to 90° for the next 4 weeks, unless they had a concomitant meniscal repair, in which case the brace range was restricted to 0° to 40° for the first 4 weeks postoperatively before increasing to 0° to 90° of flexion. All patients were provided with a cold therapy unit. Both groups were partial weightbearing for 2 weeks then weightbearing as tolerated with crutches until 4 weeks. Use of a functional ACL brace was recommended from 6 to 12 weeks and then for cutting and pivoting sports for 24 months after surgery.
Baseline Characteristics
Patient characteristics, injury characteristics, sports participation, and intraoperative findings were collected for all patients. Contact injuries were defined as a direct contact to the knee or other body part resulting in the patient’s ACL tear. Level of sports participation was categorized by the study team based on a combination of previously published literature. 11,14,15,36 Level 1 sports involved jumping, pivoting, and hard cutting and included football, soccer, basketball, field hockey, rugby, volleyball, lacrosse, and ultimate Frisbee. Level 2 sports involved heavy manual work and lateral motion but less jumping or hard cutting than did level 1 sports and included skiing and snowboarding, tennis, baseball and softball, racquet sports, gymnastics, aerobics, boxing, cheerleading, dance, ice hockey, and wrestling. Level 3 sports involved light manual work or other sports, including running, swimming, cross-country skiing, weight lifting, and biking.
Outcome Measures
All patients were assessed postoperatively in a standardized fashion with physical examination, objective and subjective measures of knee function, and pain. Study visits were at 1 to 2 weeks, 6 weeks, 3 months, 6 months, 12 months, and 24 months after surgery.
Patient-Reported Outcomes
The ACL-RSI scale was used to measure a patient’s psychological readiness to return to sports at 6, 12, and 24 months after surgery. 38 The ACL-RSI scale ranges from 0 to 100, with higher scores indicating a greater psychological readiness to return to sports. The IKDC Subjective Knee Score was used per the published instructions 16 and administered at the same time points. The Marx activity scale was recorded at baseline and at 12 months and 24 months after surgery. 23
Functional Outcomes
Hamstring and quadriceps muscle isometric strengths were measured using a hand-held dynamometer (Microfet 2; Hoggan Scientific) starting at the 3-month time point. 26 The hamstring strength was measured with the patient prone, the knee at 90° of flexion, and the dynamometer placed proximal to the ankle. The quadriceps strength was measured with the knee at 90° of flexion with the dynamometer at the distal tibia. Starting at 6 months, patients also performed a single hop, triple hop, 6-m timed hop, and crossover hop tests. 32 Hop testing was also completed at 12 and 24 months. All measures were performed in duplicate on each side, and the duplicate measurements were averaged for further analysis. Results were normalized by expressing the injured knee result as a percentage of the uninjured contralateral knee result for all strength and hop-testing measures.
Instrumented AP Knee Laxity
Arthrometer testing (KT-1000; MEDMetric) was used to measure the anterior displacement of the tibia with respect to the femur under 130 N of applied anterior force and was performed in duplicate on each leg at 6, 12, and 24 months after surgery. The results were reported as a side-to-side difference between limbs (average of the surgical knee minus the average on the contralateral knee).
Pain
Self-reported pain scores were recorded using a visual analog scale at baseline and at 2 weeks, 6 weeks, 3 months, 6 months, 12 months, and 24 months after both the BEAR and ACLR procedures. Patients made a handwritten mark on a linear scale indicating their level of pain from “no pain” to “worst pain.” Scores were reported as a proportion, ranging from 0 to 1.0, computed by measuring the length to the handwritten mark and dividing it by the total length of the scale (7.6 cm). Patients reported their level of pain at the respective clinical visit as well as worst level of pain since the last clinical visit.
Clearance for Return to Full Activity Without Restriction
Clearance for return to full activity without restriction was first considered by surgeons at 6 months after surgery in both groups. Patients were cleared for return to sport at the operating surgeon’s discretion based on subjective knee stability, stable ligamentous examination, and return of near full muscle strength on standardized functional testing. Strength and functional test results were used at the surgeon’s discretion in the decision to return to sports, but psychological readiness scores, as assessed using the ACL-RSI, were not provided to patients’ surgeons during the course of the trial and, thus, were not utilized in decisions regarding clearance for return to sport. Time to clearance was recorded as the number of days between surgery and the visit with the surgeon where the patient was cleared for return to cutting and pivoting sports for each patient.
Methods Used to Minimize Potential, Actual, or Perceived Bias of the Study
Patient recruitment and consent, as well as data collection and statistical analyses, were performed by investigators with no financial stake or compensation from any commercial interest that stood to gain from the results of this study. All physical examination and functional measurements were taken by examiners who were blinded to the procedure and surgical limb, using bilateral knee sleeves placed by the research coordinators prior to the examiner meeting with the patient. This study was overseen by a data safety monitoring board, with the members approved by both the IRB and the Boston Children’s Hospital Conflict of Interest Committee. An independent clinical research manager and a study monitor were appointed by the Clinical Research Center at Boston Children’s Hospital to monitor the study.
Statistical Methods
Participants randomized to BEAR and ACLR surgical groups were compared on baseline patient and surgical characteristics using t test and Wilcoxon rank sum test for continuous measures and chi-square or Fisher exact test for categorical variables. We also used t tests to compare BEAR and ACLR groups on selected 6-month outcomes; some results have been reported in a previous study. 4 Mixed-model repeated-measures analyses based on restricted maximum likelihood were used to compare temporal changes between BEAR and ACLR groups on ACL-RSI scores across postsurgical assessments. The model included 3 fixed factors (group [BEAR, ACLR], time [6, 12 and 24 months], and sex [male, female]), along with their interactions. If significant interactions were detected, simple effects (eg, group comparisons at each follow-up time point) were examined using partial F tests. All mean values represent least-squares means that were derived from the mixed-model repeated-measures analysis, which accounts for missing data due to incomplete follow-up. Power was estimated to be 80% to detect a mean difference of 12 points in ACL-RSI scores between groups at each time point.
The ability of baseline characteristics, surgical measures, and 6-month outcomes to predict psychological readiness to return to sports (ACL-RSI) at the 6-month assessment was examined. These analyses were conducted in a sequential fashion in a combined sample of BEAR and ACLR groups because of the limited sample size within each group. Surgical group (BEAR vs ACLR) was considered a predictor. First, correlations (Pearson r) were computed for each of the baseline characteristics and surgical measures to examine their bivariate association with 6-month ACL-RSI score. Next, a multiple regression model was constructed based on a backward elimination procedure using the criterion P < .05 for inclusion to determine the set of independent predictors of 6-month ACL-RSI score. In order to limit the number of potential predictors, only variables with P < .20 for their bivariate relationship with ACL-RSI were considered as candidates for the multiple regression model. This procedure was repeated with the addition of selected 6-month variables as potential predictors. This latter set of analyses was performed with and without the subjective IKDC, as both the IKDC and ACL-RSI are self-reported instruments.
Because listwise deletion of cases has the potential to adversely affect the sample size used for multiple regression models, even when missing values are sparse among candidate variables, multiple imputation procedures were used (n = 10 iterations) to allow for the use of all cases in regression analyses. Power was estimated to be >80% to detect variables explaining at least 10% of the variability in ACL-RSI scores at 6 months. Last, a log-rank test was used to compare time to clearance distributions based on dichotomizing 6-month ACL-RSI scores (<65, ≥65). This cutpoint has been shown to correspond to high specificity for predicting subsequent return to sports. 19,35,37 Power was estimated to be 80% to detect a hazard ratio associated with clearance of 1.75 between high and low ACL-RSI groups. All analyses were conducted using SAS Statistical Software (Version 9.4; SAS Institute) with statistical significance based on P < .05.
Results
Baseline Characteristics and Intraoperative Findings
The BEAR and ACLR groups were similar in age, sex, race, BMI, and baseline IKDC subjective scores as previously reported (Table 1). 28 Most injuries were noncontact, and all but 1 occurred during sports participation. The median times from injury to surgery were similar between groups. The percentages of patients with concomitant meniscal tears as well as the percentages of patients with a grade 3 pivot shift on their preoperative evaluation were similar between groups.
TABLE 1.
Baseline Characteristics of the BEAR and ACLR Groups a
| Characteristic | BEAR (n = 65) | ACLR (n = 35) |
|---|---|---|
| Demographics | ||
| Female | 37 (57) | 19 (54) |
| White, non-Hispanic | 55 (86) b | 26 (74) |
| Age, y, median (IQR) | 17 (16-20) | 17 (15-23) |
| BMI, mean ± SD | 24.7 ± 3.8 | 23.3 ± 4.5 |
| Contact injury | 17 (26) | 6 (17) |
| Level 1 sport | 49 (75) | 26 (74) |
| Baseline PROs | ||
| IKDC subjective score (mean ± SD) | 50.0 ± 16.7 b | 45.5 ± 14.6 |
| Marx score, median (IQR) | 16 (13-16) b | 16 (13-16) b |
| Surgery | ||
| Injury to surgery, d, median (IQR) | 36 (29-42) | 39 (33-43) |
| Preoperative pivot-shift grade 3 | 11 (17) | 4 (11) |
| Repair of medial meniscus | 3 (5) | 5 (14) |
| Repair of lateral meniscus | 14 (22) | 12 (34) |
a Data are presented as n (%) unless otherwise specified. ACL, anterior cruciate ligament; ACLR, ACL reconstruction; BEAR, bridge-enhanced ACL restoration; BMI, body mass index; IKDC, International Knee Documentation Committee; IQR, interquartile range; PROs, patient-reported outcomes.
b Missing data for 1 patient.
Psychological Readiness in BEAR vs ACLR Groups
Mixed-model repeated-measures analyses of ACL-RSI scores across the 6-, 12-, and 24-month postoperative assessments indicated that differences between BEAR and ACLR groups were time dependent (group × time interaction; P = .007) (Table 2 and Figure 2). Participants randomized to the BEAR group had significantly higher ACL-RSI scores compared with those randomized to the ACLR group at the 6-month assessment (71.1 ± 2.9 vs 58.2 ± 3.9; P = .008). No significant group differences were observed at either 12 months (P = .31) or 24 months (P = .62). In addition, there was no evidence that group differences or temporal patterns in ACL-RSI scores were different between male and female patients (sex × group, P = .52; sex × time, P = .43; sex × group × time, P = .26).
TABLE 2.
Mean ACL-RSI Values for the BEAR and ACLR Groups at 6, 12, and 24 Months Postoperatively a
| BEAR | ACLR | ||||
|---|---|---|---|---|---|
| Postoperative Assessment | n | Mean ± SEM | n | Mean ± SEM | P Value |
| 6 mo | 63 | 71.1 ± 2.9 | 34 | 58.2 ± 3.9 | .008 |
| 12 mo | 64 | 69.7 ± 2.9 | 33 | 64.8 ± 3.9 | .31 |
| 24 mo | 60 | 68.8 ± 2.9 | 32 | 71.2 ± 3.9 | .62 |
a Bolded P value indicates statistically significant difference between groups (P < .05). ACL, anterior cruciate ligament; ACL-RSI, ACL--Return to Sport after Injury; ACLR, ACL reconstruction; BEAR, bridge-enhanced ACL restoration.
Figure 2.
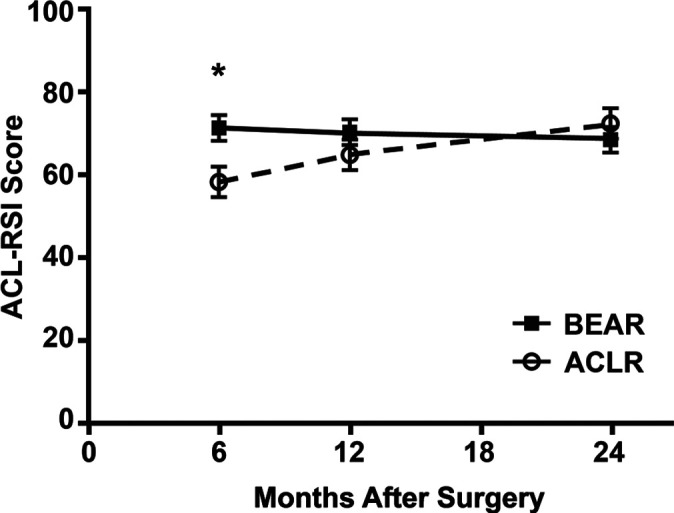
Mean ACL-RSI scores for BEAR and ACLR groups at 6, 12, and 24 months postoperatively. *P < .05. ACL, anterior cruciate ligament; ACLR, ACL reconstruction; BEAR, bridge-enhanced ACL restoration; ACL-RSI, ACL--Return to Sport after Injury.
Predictors of Psychological Readiness at 6 Months After Surgery
Bivariate Correlations Between Baseline Variables and 6-Month ACL-RSI Score
The ability of baseline patient and injury characteristics and surgical details to account for the variability in patients’ psychological readiness at 6 months was examined using bivariate correlations (Table 3). Higher ACL-RSI scores at 6 months were associated with patients who had the BEAR surgical procedure, younger patients, those with contact injuries, and patients who participated in a level 1 sport prior to their injury.
TABLE 3.
Bivariate Correlations Between Baseline Variables and 6-Month ACL-RSI Score a
| Baseline Variable | n | r | P Value |
|---|---|---|---|
| Demographics | |||
| Female sex | 97 | 0.12 | .25 |
| White, non-Hispanic | 96 | 0.19 | .06 |
| Age | 97 | -0.23 | .02 |
| BMI | 97 | 0.11 | .24 |
| Contact injury | 97 | 0.25 | .01 |
| Level 1 sport | 97 | 0.27 | .007 |
| Baseline PROs | |||
| IKDC subjective score | 96 | 0.12 | .24 |
| Marx score | 95 | 0.14 | .16 |
| Surgery | |||
| BEAR procedure | 97 | 0.28 | .005 |
| Injury to surgery time | 97 | -0.19 | .053 |
| Preoperative pivot-shift grade 3 | 97 | -0.08 | .54 |
| Repair of medial meniscus | 97 | -0.10 | .42 |
| Repair of lateral meniscus | 97 | 0.02 | .89 |
a Bolded P values indicate statistical significance (P < .05). ACL, anterior cruciate ligament; ACL-RSI, ACL--Return to Sport after Injury; BEAR, bridge-enhanced ACL restoration; BMI, body mass index; IKDC, International Knee Documentation Committee; PRO, patient-reported outcome.
Multivariable Analysis of Baseline Variables
Stepwise regression analysis resulted in 2 baseline variables meeting criteria for the final model, treatment group and sports level, which combined to explain 15% of the total variability in 6-month ACL-RSI scores. The BEAR surgical procedure was associated with an estimated 12.9-point increase in ACL-RSI score at 6 months while participation in level 1 sports corresponded to an additional 13.3-point increase.
Outcomes at 6 Months and Their Association With 6-Month ACL-RSI
The 6-month IKDC, dynamometer, instrumented AP laxity, and hop testing outcomes have been reported previously 4 and are shown in Table 4. Patients randomized to the BEAR procedure had significantly higher IKDC subjective scores at 6 months compared with patients with ACLR (P = .014) and superior functional outcomes for hamstring (P < .001) and hamstring to quadriceps ratio (P < .001). Pain level on the day of the assessment was significantly lower for the BEAR group, but levels were low for both groups on the pain scale, which ranged from 0 to 1. Hop measures were similar for BEAR and ACLR groups.
TABLE 4.
Patient-Reported and Functional Outcomes at 6 Months Postoperatively a
| BEAR | ACLR | ||||
|---|---|---|---|---|---|
| Outcome | n | Mean ± SEM | n | Mean ± SEM | P Value |
| PROs | |||||
| IKDC subjective score | 64 | 85.8 ± 1.4 | 34 | 77.7 ± 2.0 | .014 |
| Worst pain level (3 mo to 6 mo) | 62 | 0.16 ± 0.02 | 33 | 0.21 ± 0.04 | .23 |
| Today’s pain level (at 6 mo) | 62 | 0.03 ± 0.01 | 33 | 0.08 ± 0.02 | .03 |
| Functional outcomes | |||||
| Strength: dynamometer (surgical limb) b | |||||
| Hamstring | 64 | 93.1 ± 3.0 | 34 | 58.9 ± 3.6 | <.001 |
| Quadriceps | 64 | 94.1 ± 2.0 | 34 | 90.6 ± 2.4 | .29 |
| Hamstring to quadriceps ratio | 64 | 0.46 ± 0.02 | 34 | 0.30 ± 0.02 | <.001 |
| AP laxity difference, mm | 64 | 2.7 ± 0.4 | 33 | 2.2 ± 0.5 | .39 |
| Hop testing b | |||||
| Single hop | 52 | 85.9 ± 2.4 | 25 | 84.4 ± 4.0 | .73 |
| Triple hop | 47 | 91.0 ± 1.1 | 23 | 89.8 ± 2.7 | .68 |
| 6-m timed hop | 50 | 107.1 ± 2.4 | 22 | 106.8 ± 2.7 | .94 |
| Crossover hop | 44 | 92.3 ± 1.2 | 19 | 94.9 ± 2.6 | .38 |
a Bolded P values indicate statistically significant difference between groups (P < .05). ACL, anterior cruciate ligament; ACLR, ACL reconstruction; AP, anteroposterior; BEAR, bridge-enhanced ACL restoration; IKDC, International Knee Documentation Committee; PRO, patient-reported outcome.
b Strength and hop test results are presented as percentage of the contralateral side.
Examination of all patients (BEAR and ACLR groups combined), utilizing bivariate correlations between the ACL-RSI score at 6 months and these outcomes measured at that same timepoint, found that higher ACL-RSI scores were associated with higher 6-month IKDC scores, lower pain levels, greater hamstring and quadriceps strength in the surgical limb, and longer distances for single hop testing (Table 5).
TABLE 5.
Bivariate Correlations Between Other Outcomes and ACL-RSI Score at 6 Months Postoperatively a
| 6-Mo Outcomes | n | r | P Value |
|---|---|---|---|
| PROs | |||
| IKDC subjective score | 97 | 0.68 | <.001 |
| Worst pain level (3 mo to 6 mo) | 96 | -0.36 | <.001 |
| Today’s pain level (at 6 mo) | 96 | -0.40 | <.001 |
| Functional outcomes | |||
| Strength: dynamometer (surgical limb) b | |||
| Hamstring | 97 | 0.42 | <.001 |
| Quadriceps | 97 | 0.34 | <.001 |
| Hamstring to quadriceps ratio | 97 | 0.11 | .30 |
| AP laxity difference | 96 | -0.17 | .10 |
| Hop testing b | |||
| Single hop | 77 | 0.23 | .04 |
| Triple hop | 70 | -0.02 | .89 |
| 6-m timed hop | 72 | -0.12 | .30 |
| Crossover hop | 63 | 0.07 | .54 |
a Bolded P values indicate statistical significance (P < .05). ACL, anterior cruciate ligament; ACL-RSI, ACL--Return to Sport after Injury; AP, anteroposterior; IKDC, International Knee Documentation Committee; PRO, patient-reported outcome.
b Strength and hop test results are presented as percentage of the contralateral side.
Multivariable Analysis of Baseline and 6-Month Variables
Regression analysis based on a backward elimination procedure was performed to determine the best set of independent predictors of 6-month ACL-RSI score. Candidate variables were all baseline and 6-month variables with P < .20 for their bivariate relationship with ACL-RSI. The backward elimination procedure resulted in a single predictor, subjective IKDC score at 6-months, which explained 45% of the variability in patients’ ACL-RSI scores. Each 10-unit increase in IKDC score was associated with an estimated 12.4-point increase in ACL-RSI score. The modeling process was repeated excluding IKDC as a candidate because, similar to the ACL-RSI, it is also a validated patient-reported outcome instrument. This subsequent analysis resulted in 4 significant predictors of 6-month ACL-RSI score that explained, on average, 34% of the variability in ACL-RSI scores across the 10 imputations. Increased pain level at the 6-month visit was associated with decreased ACL-RSI score (-5.4 per 0.10 increase on the 0-1 scale). Hamstring and quadriceps strength in surgical limb were associated with increased ACL-RSI score, with a 10% increase in hamstring strength (expressed as percentage of contralateral) associated with a 2.5-point increase in ACL-RSI score (P = .001) while a 10% increase in quadriceps strength resulted in an estimated increase of 3.7 points in ACL-RSI score (P = .004). In addition, increased side-to-side differences in AP knee laxity (KT-1000 difference) corresponded to decreased ACL-RSI scores (-2.0 per mm; P = .007).
Psychological Readiness and Time to Clearance for Return to Sport
Although patients’ ACL-RSI scores were not used by physicians to determine clearance for return to sport, patients’ ACL-RSI scores at 6 months were predictive of when patients were subsequently cleared by their surgeons. Figure 3 compares the time to clearance for all patients using a 6-month ACL-RSI score cutpoint of 65, which has been used in previous publications. 19,35,37 Patients with higher ACL-RSI scores were cleared earlier, on average, than were those who had lower scores on the ACL-RSI at 6 months (median time to clearance, 246 vs 294 days; log-rank test, P = .024).
Figure 3.
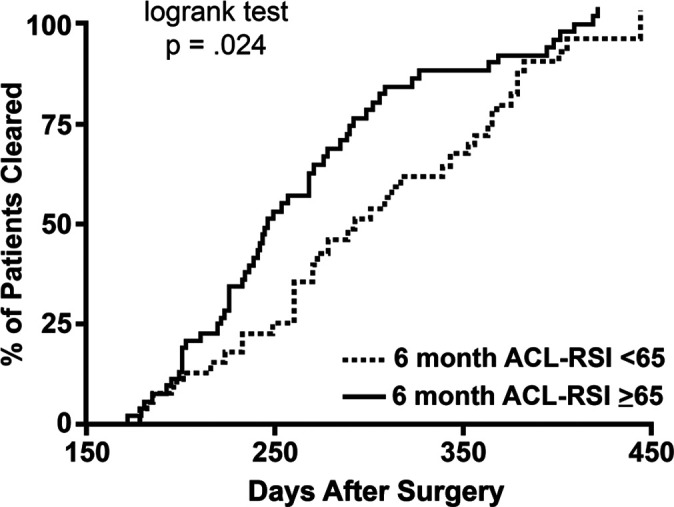
Plot for time to clearance for return to sports based on a cutoff ACL-RSI score of 65 at 6 months after surgery. ACL, anterior cruciate ligament; ACL-RSI, ACL--Return to Sport after Injury.
Discussion
Many patients are unable to return to preinjury level of sports participation by 12 months post-ACLR, in spite of satisfactory objective and functional outcomes, which has led to further investigation of how psychological factors play a role in an athlete’s readiness to return to sport. 1 –3,9,10,13,18,20,21 In the present study, we found that the mean ACL-RSI score in the BEAR group was 12.9 points higher than that in the ACLR group at 6 months after surgery, with the ACLR group catching up to similar levels of psychological readiness to the BEAR group by 12 months after surgery. The baseline factors associated with higher ACL-RSI scores at 6 months were having a BEAR procedure, younger age, a contact injury, and participating in level 1 sports prior to injury. At 6 months postoperatively, a bivariate analysis of all patients (BEAR and ACLR groups combined) suggested the predictors of a higher ACL-RSI score were the 6-month IKDC score, lower levels of pain experienced at the 6-month visit and between the 3-month and 6-month visits, higher hamstring and quadriceps strength, and better performance on the single hop test. However, multivariable regression analysis indicated that the IKDC score itself explained 45% of the ACL-RSI variance. If the IKDC was excluded from the analysis, as the IKDC and ACL-RSI are both self-reported measures, then decreased pain, increased hamstring and quadriceps strength in the surgical limb, and decreased side-to-side difference in AP knee laxity were significant predictors of a higher ACL-RSI score. In addition, patients with higher ACL-RSI scores at 6 months were cleared earlier in their postoperative course.
The finding that the ACL-RSI score in the BEAR group (mean, 71) was 12.9 points higher than that in the ACLR group (mean, 58) at 6 months was a new finding. To our knowledge, this was also the first study exploring psychological readiness predictors in a randomized controlled trial. We focused on 6-month factors because the patients’ surgeons were willing to consider medical clearance at this time point. Research continues to examine the clinical relevance of ACL-RSI scores; however, recent studies have suggested that cutoff scores of 60 and 62 are predictive of a patient’s return to preinjury level of sports. 34,35 The mean score for the ACLR group failed to meet these cutoffs at the 6-month postoperative timepoint, while the mean score for the BEAR group was approximately 15% higher than these suggested cutoffs. Furthermore, Webster and Feller 37 considered an ACL-RSI score of at least 65 at 6 months an indicator of satisfactory recovery because receiver operating characteristic statistics determined that this score corresponded to 80% specificity for return to sport at 12 months. Once again, the mean score for the ACLR group failed to meet this 65 cutpoint value until at least 12 months postsurgery, whereas the mean score for the BEAR group was 71 at 6 months postoperatively. The majority of patients with ACLR (94.3%) had quadrupled hamstring tendon autograft, while a smaller number had bone--patellar tendon--bone autograft (5.7%). With the lack of donor-site morbidity from graft harvest in the BEAR group and, theoretically, faster muscle recovery, patients may have been more confident earlier in their postoperative course, which was associated with higher psychological readiness scores at 6 months. Our results did in fact demonstrate that higher hamstring and quadriceps strength at 6 months correlated with higher psychological readiness scores, which further supports the idea of a mind-body connection during recovery. While this difference in psychological readiness was present at 6 months postoperatively, by 12 months, the ACLR group had achieved similar levels to the BEAR group, suggesting this was only a delay of psychological readiness in the ACLR group and not a permanent concern. The 12-month ACL-RSI scores for both groups are consistent with those in previous literature. 24,39
Baseline patient factors can be useful for counseling patients preoperatively and during their recovery as to timing of return to sport. In addition to surgical procedure correlating with readiness to return, younger age, a contact injury, and participating in level 1 sports prior to injury were also correlated with a higher ACL-RSI at 6 months. Interestingly, sex was not significantly associated with ACL-RSI scores in this study as previous research has suggested for other surgical procedures. 17 When considering only baseline factors in multivariable regression analysis, we found the strongest predictor of psychological readiness was participation in level 1 sports at the time of the index injury, which corresponded to a 13.3-point increase in 6-month ACL-RSI score. Level 1 sports were considered to involve jumping; pivoting; and hard cutting, such as football, soccer, basketball, rugby, and lacrosse. Patients involved in highly competitive sports may be more motivated and driven to return to sports earlier. In addition, these athletes may have stronger athletic identities, driving them to a stricter commitment to rehabilitation. 5 –7
When accounting for baseline and 6-month factors, we found the ACL-RSI score was most strongly predicted by another patient-reported outcome measure: the IKDC subjective score. Subjective knee scores, such as the IKDC, have previously been reported to be significantly higher in patients who returned to sports than those who had not after ACLR. 2,20,27 In addition, the IKDC has been shown to correlate positively with psychological readiness in patients with ACLR, while also having a significant association with self-esteem. 9,12,39 This finding suggests that psychological readiness matched the patient’s perceived knee function.
We were also interested in examining other factors that predicted 6-month ACL-RSI scores, outside of expected patient-reported outcome associations, for our full cohort (BEAR and ACLR). Decreased pain level, increased hamstring and quadriceps strength, and decreased side-to-side differences in AP knee laxity at 6 months combined to explain 34% of the variance in psychological readiness. It is important to note that pain was significantly lower and hamstring strength was significantly higher in the BEAR group compared with the ACLR group, while there were no statistical differences in quadriceps strength or AP knee laxity between the groups. Knee symptoms, especially pain, have been shown previously to be associated with return to sport and, thus, may have an effect on psychological readiness. 10,13,20 It is evident in the literature that hamstring strength and quadriceps strength have effects on return to sport after ACLR while also showing associations with ACL-RSI scores. 20,25,27,33 Although the BEAR surgical procedure was a significant predictor when only baseline factors were considered, it did not meet criteria for inclusion in the regression model that included 6-month factors as candidates. The BEAR group had increased hamstring strength and decreased pain relative to the ACLR group, and thus, these outcomes may have acted as mediators influencing 6-month ACL-RSI. Previous research has shown no significant differences in AP knee laxity between BEAR and ACLR, 28 indicating knee laxity is likely not a mediator but still explains patient-to-patient variability in ACL-RSI scores after ACL surgery. These results again support the existence of a mind-body connection that is important after BEAR or ACLR surgery; perceptions of psychological readiness may be reflective of how the knee feels with respect to pain, strength, and laxity.
The 6-month ACL-RSI scores were independently predictive of when patients were subsequently cleared by their surgeons. In this study, surgeons were able to clear patients at their discretion and did so based on their overall perception of how patients reported feeling about their knee, their strength testing results, and the amount of activity they reported prior to the visit. As stated previously, our results are consistent with previous research, which has shown that early, higher ACL-RSI scores are predictive of return to sport at 12 months. 34,35,37
The results of this study should be interpreted with several limitations in mind. The ACL-RSI is a self-reported measure and could be subject to recall and self-report bias. While the follow-up rate of the BEAR II Trial at 2 years was excellent at 96%, we did not have 100% follow-up represented. 28 Our ACLR group (35 patients) had 33 hamstring autografts, and thus, our findings may not be generalized to other autograft reconstructions. Further studies to assess ACL-RSI after the BEAR procedure in comparison with these other graft types would be of interest. In addition, surgeon clearance for return to sport did not necessarily equate with their patients’ date for return to sports, as some patients may have been reluctant to return to sports even after surgeon clearance. In addition, while our study focused on associations between patient and surgical variables and outcomes, these interactions should not be interpreted as causative relationships. Statistically, multiple imputations were used to account for missing values. Furthermore, the current report focused on analyses of multiple secondary outcomes, which increased the probability of a type I error. Last, our study was not powered to determine the effect of ACL-RSI on the risk of a secondary ACL injury, and future studies with a larger number of patients should be conducted to answer that important question.
Conclusion
The study results indicated that patients who underwent the BEAR procedure had higher psychological readiness at 6 months postoperatively compared with patients who underwent an ACLR, with this difference dissipating by 12 months after surgery. The baseline variables that most strongly predicted a higher ACL-RSI score were having a BEAR procedure, a younger age, a contact injury, and participation in a level 1 sport at the time of injury. The IKDC at 6 months was the single strongest predictor of ACL-RSI score. Outside of validated patient-reported outcome measures, at 6 months, a lower pain level, better hamstring and quadriceps strength, and lower side-to-side difference in AP knee laxity were also significant predictors of a higher 6-month ACL-RSI score. Last, patients with higher psychological readiness at 6 months were medically cleared earlier for return to sport. These results suggest that the psychological readiness to return to sport after ACL surgery may be influenced by the surgical procedure performed, as well as baseline patient characteristics, return of muscle strength, and knee stability at 6 months after surgery.
Authors
Members of the BEAR Trial Team: Benedikt Proffen, MD (Division of Sports Medicine, Department of Orthopaedic Surgery, Boston Children’s Hospital, Boston, Massachusetts, USA); Nicholas Sant, BS (Division of Sports Medicine, Department of Orthopaedic Surgery, Boston Children’s Hospital, Boston, Massachusetts, USA); Samuel Barnett, MD (Division of Sports Medicine, Department of Orthopaedic Surgery, Boston Children’s Hospital, Boston, Massachusetts, USA); Braden C. Fleming, PhD (Department of Orthopaedics, Warren Alpert Medical School of Brown University/Rhode Island Hospital, Providence, Rhode Island, USA); Dennis E. Kramer, MD (Division of Sports Medicine, Department of Orthopaedic Surgery, Boston Children’s Hospital, Boston, Massachusetts, USA); and Lyle J. Micheli, MD (Division of Sports Medicine, Department of Orthopaedic Surgery, Boston Children’s Hospital, Boston, Massachusetts, USA).
Acknowledgment
The authors acknowledge the significant contributions of the clinical trial team, including Bethany Trainor, Rachael Henderson, Christina Freiberger, Gabriela Portilla, Elizabeth Carew, Brett Flutie, Laura Thurber, and Shanika Coney. The authors also acknowledge the contributions of our medical safety monitoring team of Joseph DeAngelis, Peter Nigrovic, and Carolyn Hettrich; our data monitors Maggie Malsch, Megan Fitzgerald, and Erica Denhoff; and the members of the Division of Sports Medicine at Boston Children’s Hospital for their clinical care of the patients in this trial. Finally, the authors are especially grateful to the patients and their families who participated in this study.
Footnotes
Final revision submitted August 31, 2021; accepted October 7, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study received funding support from the Translational Research Program at Boston Children’s Hospital, the Children’s Hospital Orthopaedic Surgery Foundation, the Children’s Hospital Sports Medicine Foundation, the Football Players Health Study at Harvard University, the National Institutes of Health, and the National Institute of Arthritis and Musculoskeletal and Skin Diseases through grants R01-AR065462 and R01-AR056834. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Medical School, Harvard University or its affiliated academic health care centers, the National Football League Players Association, Boston Children’s Hospital, or the National Institutes of Health. Y.-M.Y. has received education payments from Kairos Surgical and consulting fees from Smith & Nephew. M.M.M. is a founder, paid consultant, and equity holder in Miach Orthopaedics, which was formed to work on upscaling production of the BEAR scaffold. M.M.M. has also received honoraria from Musculoskeletal Transplant Foundation. M.A.C. has received hospitality payments from Smith & Nephew. B.P. has received consulting fees and has stock/stock options in Miach Orthopaedics. N.S. has received consulting fees from Miach Orthopaedics. B.C.F. is a paid associate editor for The American Journal of Sports Medicine and is the spouse of M.M.M. with inherently the same conflicts. D.E.K. has received education payments from Kairos Surgical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Boston’s Children Hospital (protocol No. IRB-P00021470).
References
- 1. Ardern CL, Österberg A, Tagesson S, Gauffin H, Webster KE, Kvist J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br J Sports Med. 2014;48(22):1613–1619. [DOI] [PubMed] [Google Scholar]
- 2. Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2013;41(7):1549–1558. [DOI] [PubMed] [Google Scholar]
- 3. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596–606. [DOI] [PubMed] [Google Scholar]
- 4. Barnett S, Murray MM, Badger GJ; et al. BEAR Trial Team. Earlier resolution of symptoms and return of function after bridge-enhanced anterior cruciate ligament repair as compared with anterior cruciate ligament reconstruction. Orthop J Sports Med. 2021;9(11):23259671211052530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brewer BW, Cornelius AE, Van Raalte JL, et al. Age-related differences in predictors of adherence to rehabilitation after anterior cruciate ligament reconstruction. J Athl Train. 2003;38(2):158. [PMC free article] [PubMed] [Google Scholar]
- 6. Brewer BW, Cornelius AE, Van Raalte JL, et al. Rehabilitation adherence and anterior cruciate ligament reconstruction outcome. Psychol Health Med. 2004;9(2):163–175. [Google Scholar]
- 7. Brewer BW, Cornelius AE, Van Raalte JL, Tennen H, Armeli S. Predictors of adherence to home rehabilitation exercises following anterior cruciate ligament reconstruction. Rehabil Psychol. 2013;58(1):64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Christino MA, Fantry AJ, Vopat BG. Psychological aspects of recovery following anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2015;23(8):501–509. [DOI] [PubMed] [Google Scholar]
- 9. Christino MA, Fleming BC, Machan JT, Shalvoy RM. Psychological factors associated with anterior cruciate ligament reconstruction recovery. Orthop J Sports Med. 2016;4(3):2325967116638341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Czuppon S, Racette BA, Klein SE, Harris-Hayes M. Variables associated with return to sport following anterior cruciate ligament reconstruction: a systematic review. Br J Sports Med. 2014;48(5):356–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient: a prospective outcome study. Am J Sports Med. 1994;22(5):632–644. [DOI] [PubMed] [Google Scholar]
- 12. Ellis HB, Sabatino M, Nwelue E, Wagner KJ III, Force E, Wilson P. The use of psychological patient reported outcome measures to identify adolescent athletes at risk for prolonged recovery following an ACL reconstruction. J Pediatr Orthop. 2020;40(9):e844–e852. [DOI] [PubMed] [Google Scholar]
- 13. Flanigan DC, Everhart JS, Pedroza A, Smith T, Kaeding CC. Fear of reinjury (kinesiophobia) and persistent knee symptoms are common factors for lack of return to sport after anterior cruciate ligament reconstruction. Arthroscopy. 2013;29(8):1322–1329. [DOI] [PubMed] [Google Scholar]
- 14. Grindem H, Eitzen I, Moksnes H, Snyder-Mackler L, Risberg MA. A pair-matched comparison of return to pivoting sports at 1 year in anterior cruciate ligament-injured patients after a nonoperative versus an operative treatment course. Am J Sports Med. 2012;40(11):2509–2516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hefti E, Müller W, Jakob R, Stäubli H-U. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3-4):226–234. [DOI] [PubMed] [Google Scholar]
- 16. Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2001;29(5):600–613. [DOI] [PubMed] [Google Scholar]
- 17. Kostyun RO, Burland JP, Kostyun KJ, Milewski MD, Nissen CW. Male and female adolescent athletes’ readiness to return to sport after anterior cruciate ligament injury and reconstruction. Clin J Sport Med. 2021;31(4):383–387. [DOI] [PubMed] [Google Scholar]
- 18. Kvist J, Ek A, Sporrstedt K, Good L. Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2005;13(5):393–397. [DOI] [PubMed] [Google Scholar]
- 19. Langford JL, Webster KE, Feller JA. A prospective longitudinal study to assess psychological changes following anterior cruciate ligament reconstruction surgery. Br J Sports Med. 2009;43(5):377–378. [DOI] [PubMed] [Google Scholar]
- 20. Lentz TA, Zeppieri G, Jr, George SZ, et al. Comparison of physical impairment, functional, and psychosocial measures based on fear of reinjury/lack of confidence and return-to-sport status after ACL reconstruction. Am J Sports Med. 2015;43(2):345–353. [DOI] [PubMed] [Google Scholar]
- 21. Lentz TA, Zeppieri G, Jr, Tillman SM, et al. Return to preinjury sports participation following anterior cruciate ligament reconstruction: contributions of demographic, knee impairment, and self-report measures. J Orthop Sports Phys Ther. 2012;42(11):893–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Marshall JL, Warren RF, Wickiewicz TL. Primary surgical treatment of anterior cruciate ligament lesions. Am J Sports Med. 1982;10(2):103–107. [DOI] [PubMed] [Google Scholar]
- 23. Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29(2):213–218. [DOI] [PubMed] [Google Scholar]
- 24. McPherson AL, Feller JA, Hewett TE, Webster KE. Psychological readiness to return to sport is associated with second anterior cruciate ligament injuries. Am J Sports Med. 2019;47(4):857–862. [DOI] [PubMed] [Google Scholar]
- 25. Meierbachtol A, Yungtum W, Paur E, Bottoms J, Chmielewski TL. Psychological and functional readiness for sport following advanced group training in patients with anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2018;48(11):864–872. [DOI] [PubMed] [Google Scholar]
- 26. Mentiplay BF, Perraton LG, Bower KJ, et al. Assessment of lower limb muscle strength and power using hand-held and fixed dynamometry: a reliability and validity study. PloS One. 2015;10(10):e0140822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Müller U, Krüger-Franke M, Schmidt M, Rosemeyer B. Predictive parameters for return to pre-injury level of sport 6 months following anterior cruciate ligament reconstruction surgery. Knee Surg Sports Traumatol Arthrosc. 2015;23(12):3623–3631. [DOI] [PubMed] [Google Scholar]
- 28. Murray MM, Fleming BC, Badger GJ, et al. Bridge-enhanced anterior cruciate ligament repair is not inferior to autograft anterior cruciate ligament reconstruction at 2 years: results of a prospective randomized clinical trial. Am J Sports Med. 2020;48(6):1305–1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Murray MM, Flutie BM, Kalish LA, et al. The bridge-enhanced anterior cruciate ligament repair (BEAR) procedure: an early feasibility cohort study. Orthop J Sports Med. 2016;4(11):2325967116672176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Murray MM, Kalish LA, Fleming BC, et al. Bridge-enhanced anterior cruciate ligament repair: two-year results of a first-in-human study. Orthop J Sports Med. 2019;7(3):2325967118824356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Murray MM, Kiapour AM, Kalish LA, et al. Predictors of healing ligament size and magnetic resonance signal intensity at 6 months after bridge-enhanced anterior cruciate ligament repair. Am J Sports Med. 2019;47(6):1361–1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19(5):513–518. [DOI] [PubMed] [Google Scholar]
- 33. O’Connor RF, King E, Richter C, Webster KE, Falvey ÉC. No relationship between strength and power scores and anterior cruciate ligament return to sport after injury scale 9 months after anterior cruciate ligament reconstruction. Am J Sports Med. 2020;48(1):78–84. [DOI] [PubMed] [Google Scholar]
- 34. Sadeqi M, Klouche S, Bohu Y, Herman S, Lefevre N, Gerometta A. Progression of the psychological ACL-RSI score and return to sport after anterior cruciate ligament reconstruction: a prospective 2-year follow-up study from the French Prospective Anterior Cruciate Ligament Reconstruction Cohort Study (FAST). Orthop J Sports Med. 2018;6(12):2325967118812819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Webster KE, Feller JA. Development and validation of a short version of the anterior cruciate ligament return to sport after injury (ACL-RSI) scale. Orthop J Sports Med. 2018;6(4):2325967118763763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Webster KE, Feller JA. Return to level I sports after anterior cruciate ligament reconstruction: evaluation of age, sex, and readiness to return criteria. Orthop J Sports Med. 2018;6(8):2325967118788045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Webster KE, Feller JA. Who passes return-to-sport tests, and which tests are most strongly associated with return to play after anterior cruciate ligament reconstruction? Orthop J Sports Med. 2020;8(12):2325967120969425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport. 2008;9(1):9–15. [DOI] [PubMed] [Google Scholar]
- 39. Webster KE, Nagelli CV, Hewett TE, Feller JA. Factors associated with psychological readiness to return to sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2018;46(7):1545–1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wright RW, Preston E, Fleming BC, et al. A systematic review of anterior cruciate ligament reconstruction rehabilitation---part I: continuous passive motion, early weight bearing, postoperative bracing, and home-based rehabilitation. J Knee Surg. 2008;21(3):217–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wright RW, Preston E, Fleming BC, et al. A systematic review of anterior cruciate ligament reconstruction rehabilitation---part II: open versus closed kinetic chain exercises, neuromuscular electrical stimulation, accelerated rehabilitation, and miscellaneous topics. J Knee Surg. 2008;21(3):225–234. [DOI] [PMC free article] [PubMed] [Google Scholar]


