Abstract
Introduction
This paper describes the findings of a pilot implementation project that explored the potential of virtual reality (VR) technology in recreational programming to support the well-being of older adults in long-term care (LTC) homes.
Methods
32 Adults in four LTC homes participated in a pilot implementation project where they viewed VR experiences of popular locations in Canada created especially for this project. Data in this paper are based on multiple viewing experiences (n = 102) over a two-week period.
Results
VR appeared to be an effective distraction from pain for the participants. Participants of this study found the VR experiences to be enjoyable and were relaxed and happy while viewing them. Most participants were attentive or focused while viewing the VR experiences, and the experiences were found to be a source of reminiscence for some of the participants. Participants related well to others around them during a majority of the experiences and the VR experiences were a point of conversation between the staff and the participants.
Conclusion
The findings from this pilot implementation reveal that VR shows potential to enhance the physical, emotional, cognitive, and social well-being of older adults living in LTC, including those living with cognitive impairment.
Keywords: Aging, older adults, virtual reality, well-being, long-term care homes
Introduction
Canada, like many other countries, has a rapidly aging population. 1 Older adults are living longer than ever before, making those aged 65+ the fastest growing age group all over the world. 2 The World Health Organization has stated that the number of individuals aged 65 years and older is predicted to reach 1.5 billion by the middle of the 21st century. 3 By 2030, it is anticipated that one in four Canadians will be over 65 years old. 4 This large-scale change necessitates an in-depth look at the well-being and quality of life of older adults, and the development of novel solutions to address the needs of this rapidly growing population.
According to the 2016 Canadian census, 6.8% of Canadians 65 years and older, and 30% of Canadians 86 years and older, lived in long-term care (LTC) homes or senior’s residences. 5 In Ontario in 2019, 90% of residents in LTC were living with cognitive impairment and 64% had a diagnosis of dementia. 6 Individuals living in these settings may experience high levels of loneliness, social isolation, depression, and anxiety, as well as a lower overall sense of belonging.2,7 As such, it is important to consider innovative programming that can help increase well-being in older adults—including those living with cognitive impairment. Recently, there has been increasing interest in understanding how technology, specifically virtual reality (VR), can be utilized to contribute to the well-being of older adults.7,8 VR consists of technology that replaces our true physical environment and sensory intake, or what one may call their “lived reality,” with an alternative digital “reality.” 9
Despite popular misconceptions surrounding older adults and their aversion to technology, VR studies with older adults have shown high engagement levels when utilizing these systems.10–12 VR has been shown to be an effective intervention with the potential to make positive changes in the overall well-being and quality of life of older adults. More specifically, recent studies have suggested that there are potential benefits of VR interventions for pain management with diverse populations,13–15 to combat social isolation, 7 and to improve balance, strength, 16 and cognition.17–19
Virtual reality and well-being
Well-being has been regarded as a highly multi-faceted concept having no single agreed upon universal definition. 20 From a philosophical standpoint, the literature proposes two different types of well-being: hedonic and eudemonic. 20 Hedonic well-being ties into an individual’s level of happiness and pleasure, while eudemonic well-being focuses on one’s personal growth and fulfillment.21,22 It has been suggested that a life that has high levels of both hedonic and eudemonic well-being has the highest overall well-being. The term used when both concepts are integrated together is “flourishing.” 20
However, well-being is most often perceived more practically. The Centers for Disease Control and Prevention 23 state that a commonplace understanding of well-being includes “the presence of positive emotions and moods (e.g., contentment and happiness), the absence of negative emotions (e.g., depression and anxiety), satisfaction with life, fulfillment, and positive functioning” (p.1). Individuals believe that they achieve high levels of well-being when they observe that their lives are going well and they simultaneously “feel good.” 23 Well-being can also be further understood in terms of its various components: physical well-being, emotional well-being, social well-being, psychological well-being, development/activity well-being, life satisfaction, and engaging activities and work. 23 Well-being is fluid and changes with age. The well-being of older adults is related to their ability to positively cope with various physical and social changes that come about with age. 20 These changes, understandably, impact their well-being at a higher rate than for younger adults. 24
The literature on the potential of VR in relation to the well-being of various populations, including older adults, is promising and has applications in terms of pain management, ahderence to physical activity, improving physical, mental and cognitivehealth, and potentially reducing social isolation. These benefits are reviewed below.
Physical health
One in three Canadian older adults lives with chronic pain. 25 Pain experienced by older adults can lead to an overall lack of engagement in daily activities. 13
VR experiences in the form of games and virtual travel, have been found to provide an enjoyable and engrossing experience, creating a distraction from pain, possibly leading to a reduction in pain experienced by older adults. 13
A review of literature on the potential of VR in the treatment of pain suggests that VR technology is a promising intervention in the management of acute pain by serving as a distraction that drives attention away from acute pain. 26
VR has also been studied for the management of pain in younger populations. In their study of female patients with breast cancer, intervention group participants chose one of two VR experiences via CD-ROM: sitting at a beach or a deep sea dive. 14 The study found that VR in addition to morphine reduced pain and anxiety more so than morphine alone. VR immersed these patients into another “world,” thereby drawing attention away, or distracting them, from their pain. 14 Similarly, a systematic review of the effectiveness of VR technology on reducing pain and anxiety in burn victims 15 found VR to be successful in reducing the pain and anxiety experienced by burn victims when dressings were being changed. Another systematic review 27 identified VR as an effective mechanism to alleviate cancer patients’ discomfort while they undergo chemotherapy.
Motivation/adherence to physical activity
Physical activity in older adults is a crucial component in the prevention of disease and disability. 28 Incorporating VR into physical activity training is a new method to enhance the fun and enjoyment of daily physical activity. 29 Delivering exercises and activities through VR has the potential to increase motivation and, in turn, lead to higher adherence. 3 Virtual reality has the ability to motivate individuals to partake in an enjoyable way of exercising, with the additional benefit of being able to do so in their own homes. 28
Emotional and psychological well-being
VR has been used in interventions to improve different aspects of psychological well-being. In their study in residential aged care facilities, Baker et al. 7 comment that VR may be an effective tool in entertainment provision and can improve the mood of older adults in these settings. Older adults face challenges with no longer being able to participate in activities they love, and VR may have the ability to expand the daily worlds of individuals living in LTC homes. 7
Cognitive health
Reminiscence therapy has been found useful in alleviating depressive symptoms and improving psychological well-being among older adults with dementia. 30 VR shows promise as a tool to enhance cognitive function and for rehabilitation/memory exercises for individuals with dementia. 17 Optale et al., (2010) implemented a VR intervention consisting of audio-visual experiences with path finding with elderly residents and found that the experimental group of older adults in their study showed significant improvements in memory tests, particularly in long-term recall. The researchers suggest that virtual reality memory training can be an effective tool to help improve memory function in elderly adults. 18
A recent longitudinal one-month-long pilot study 31 examined the effectiveness of a music and reminiscence cognitive stimulation interactive platform Musiquence for people living with dementia. The authors found that persons with dementia showed improvements in “general cognition, mood, quality of life, and verbal fluency while using Musiquence.” (p.9). They also found that respondents relied more on music-based feedback during the task performance of virtual reality activities. This implies that music-based cues may help people living with dementia navigate and use virtual reality platforms.
Finally, a study of older adults in Hong Kong with possible dementia 19 suggests that VR can offer self-paced learning and a less threatening method of training so that individuals may easily “pick-up” new memory strategies.
Dietrichkeit et al. 32 conducted a study using VR to explore memory biases and cognitive insight in individuals with and without psychosis. They highlight that treatments that include VR environments may correct cognitive bias and reduce psychotic symptoms in individuals with psychosis. 32 Słyk and colleagues 33 completed a review of VR systems’ effectiveness of diagnosing and rehabilitating neurological patients with cognitive disorders. This review showed that VR is a promising tool in screening for earlier signs of mild cognitive impairment and Alzheimer’s disease, although there is need for more research in this area, as it is understudied. 33
Reduction in social isolation
A challenge many older adults living in LTC communities experience is that of social isolation and loneliness. 7 Previous research on the benefits of technology have focused on its positive impact on the social well-being of older adults, particularly its potential to increase social interaction and improve a sense of accomplishment and mood. 34 In their exploratory study with residents of LTC homes, Baker and colleagues 7 found that interactive and stimulating features of the Oculus Rift VR technology used in the study increases engagement among individuals who frequently self-isolate, by providing topics of conversation for residents to engage with their families and friends. 7
In this paper we present the findings of a mixed methods pilot implementation study that describes the potential of VR technology in supporting the well-being of older adults, including those living with cognitive impairment, in LTC homes.
Methods
This applied research project was conducted by the Sheridan Centre for Elder Research in collaboration with a national provider of retirement and LTC homes. The partner organization was interested in understanding the potential of VR experiences developed in consultation with residents and staff, for the well-being of its resident population and tasked the Centre for Elder Research with the creation of VR experiences and the pilot implementation of the same. Ethics approval was received from the Sheridan College Research Ethics Board (SREB Approval: N° 2017-03-001-005). The VR experiences used in this study were created in consultation with 18 staff and 38 residents of five LTC homes in Southwestern Ontario (as per Hayden et al. in this journal issue).
Recruitment
The staff comprised of recreation team members and the residents opted to participate in the initial consultation. Focus groups were held with these staff and participants to generate ideas about the kinds of VR experiences might be most meaningful for the residents in the homes. Basic demographic information was collected from the residents who participated in these focus group consultations to understand the diversity of the group that was providing input into the program. This information included age, gender, and self reported cognitive impairment. This feedback was to be used in the creation of meaningful VR experiences that could be incorporated into the recreational programing of the homes. Written letters of consent were collected from all participants or from persons authorized to consent for the residents.
Participants
Participants were recruited using purposive sampling. Staff played a key role in identifying participants for the initial focus groups consultations, and additional residents for the VR viewing experiences. They chose residents who did not regularly attend most recreational programming and they thought might benefit from novel approaches to recreational programming. Many participants who took part in the initial consultation also became involved as participants for the implementation.
Our participant data is described in Table 1. Thirty-two participants (x age = 77, s = 10.64; 47% female) took part in the implementation of the VR experiences. 63% (n = 20) used some form of assistive devices including glasses (n = 4), walkers (n = 3), wheelchairs (n = 9) or multiple assistive devices (n = 4). Only 14% of the participants (n = 5) had viewed a VR experience prior to participating in the study. Based on the initial demographic information collected from the focus group participants who also participated in the pilot implementation, at least 22% percent of participants had self-reported cognitive impairments. As information about self-reported cognitive impairment was not collected during implementation, it is possible the number of participants with cognitive impairment was even higher given that long-term care residents typically have high rates of cognitive impairment. Data in this paper are based on 102 VR viewing experiences collected from 32 older adults in four of the five LTC home sites that had participated in the initial focus groups. The fifth site had an outbreak during the pilot testing phase and could not be included in this pilot implementation study. Each participant engaged in between 1 and 6 VR viewing experiences over the data collection period over a 2-week period (Mean number of experiences = 4.9). Each VR viewing experience lasted between 8 and 10 min. Location and participant names were removed for confidentiality and replaced with an identifying number for each participant from the four different locations.
Table 1.
Profile of the participants.
| Participant location and code | Age | Gender | Self-reported cognitive impairment |
|---|---|---|---|
| L1_1 | 88 | Female | No |
| L1_10 | 80 | Female | Unknown 1 |
| L1_3 | 100 | Female | Yes |
| L1_4 | 96 | Male | Yes |
| L1_5 | 84 | Male | Yes |
| L1_6 | 60 | Male | No |
| L1_7 | 79 | Female | Yes |
| L1_8 | 66 | Male | Yes |
| L1_9 | 81 | Female | Unknown |
| L2_1 | 73 | Male | No |
| L2_2 | 81 | Male | Unknown |
| L2_4 | 72 | Female | No |
| L2_6 | 71 | Male | No |
| L2_1 | 75 | Male | No |
| L3_10 | 71 | Female | Unknown |
| L3_2 | 79 | Female | Yes |
| L3_5 | 80 | Male | Yes |
| L3_6 | 61 | Male | No |
| L3_8 | 50 | Female | No |
| L3_9 | 71 | Female | No |
| L4_1 | 67 | Female | No |
| L4_10 | 65 | Male | Unknown |
| L4_11 | 82 | Male | Unknown |
| L4_12 | 91 | Male | Unknown |
| L4_2 | 85 | Female | No |
| L4_3 | 78 | Female | No |
| L4_4 | 69 | Male | No |
| L4_5 | 73 | Male | No |
| L4_6 | 86 | Male | Unknown |
| L4_7 | 71 | Female | Unknown |
| L4_8 | 88 | Male | Unknown |
| L4_9 | 78 | Female | Unknown |
Virtual reality experiences
Ten unique VR experiences (immersive video clips) were created especially for this study. As shown in Table 2, each VR experience profiled popular locations in Western Canada and Ontario. The experiences allowed for the person using the VR technology to get a sense of being in, standing and/or moving along at the location in the experience. The 10 VR experiences were user-tested by older adults (n = 3, ages, 65–75 years) living with dementia in the community and who attended a day care program. By testing with persons who had dementia, the pilot test allowed the team to create VR experiences and implementation processes that were inclusive and took into account persons with varied cognitive status. In data not reported here, the adult day program, that is, co-located with the Centre for Elder Research and was the site of the pilot test, was much more involved and in that context, they were an appropriate site to work out any issues with the VR technology.
Table 2.
Virtual reality experiences created based on focus group findings.
| 1 | Docks in Victoria, BC |
| 2 | Butchart Gardens, Brentwood Bay, BC |
| 3 | Stanley Park and Granville Market, Vancouver, BC |
| 4 | Capilano Suspension Bridge Park, North Vancouver, BC |
| 5 | Canadian Pacific Railway Last Spike, Craigellachie, BC |
| 6 | Lake Louise, Banff National Park, Alberta |
| 7 | Banff, Alberta |
| 8 | Brant Street Pier, Burlington, Ontario |
| 9 | Hendrie Park |
| 10 | Niagara Falls Canada, Ontario |
These allowed for valuable feedback on the experiences and use of the VR headsets, which was used to improve the VR experience. Based on this feedback, the following changes were made to the final experiences used in the current study: the time limit for each experience was limited to 8–10 min and relaxing music and narration were added to each experience. Table 3 provides a transcription of the narration in one of the VR experiences and showcases the manner in which narration both oriented the viewer and encouraged them to engage with the experience.
Table 3.
Transcription of narration for experience 1: docks in Victoria, BC.
| Hello! You are joining us on a warm summer day on a ferry to Victoria, BC. |
| We are now in Victoria, standing near the empress |
| At the docks, the sun is starting to set. Visitors are enjoying a walk by the water |
| We are standing by the ticket center to catch a ride on the water taxis. We will be taking a ride very soon |
| On the water taxi, we get to experience the neighborhood. Can you see the other boats on the water? |
| What a great view! Can you see the buildings in the distance? |
| We have arrived at the docks. Take a look around to explore the restaurants and shops nearby |
| Thank you for joining us in Victoria. We hope you had a great virtual reality experience! |
Measures
Data for this study were collected using both quantitative and qualitative data collection approaches.
Quantitative
The researchers collected observational information on the participants’ discomfort and pain during the VR experiences using a Pain Assessment in Advanced Dementia tool (PAINAD). 35 The tool allowed the researcher to rate on a scale from 0 to 2 the participant’s breathing, negative vocalization, facial expression, and body language to assess any pain the participant might be experiencing while engaging in the VR experience. This tool, which includes an observational sheet, was considered suitable for the study as it allowed for the inclusion of participants who may or may not be able to vocalize their pain. The researchers also collected observational data on how participants were expressing themselves during the VR experience using the using the Interact Short tool 7 which assesses the resident’s emotional expression (whether tearful/sad; confused; relaxed; fearful/anxious; and happy/content), interest toward tasks (did things out of own initiative; attentive/focused; bored/inactive; enjoying self; and active or alert), and behaviors to environments (related well to other staff/people; wandering, restless; or aggressive) on a score from 1 (“not at all”) to 5 (“nearly all of the time”).
Qualitative
A semi structured interview guide was used to ask participants what they thought of the experience they had watched, whether they typically experience pain in the normal course of the day, and whether they had experienced pain while engaged in the VR experience. Research staff also filled out a technological implementation observation guide created using a RE-AIM framework. 36 The acronym RE-AIM stands for the Reach, Effectiveness, Adoption, Implementation, and Maintenance of any implementation. Research staff used these qualitative and quantitative instruments for the resident VR experiences they observed during their initial visit and during their follow-up visit after 2 weeks.
Procedures
The qualitative and quantitative data reported in this paper emerge from the pilot implementation of the VR experiences across four of the five LTC communities. The implementation took place over a two-week period for each community. To start off the implementation project, members of the research team visited each community and trained the staff on using the VR equipment. The researchers then demonstrated how this technology could be used with older adults for recreation purposes. The VR experiences, VR training manual, data collection sheets, and Oculus-Go VR headset were left with the care community for 2 weeks following this initial training and data collection. Over the 2-week period, the LTC staff encouraged residents who had consented to participate in the study (n = 32) to engage with the VR experiences. During the 2-week VR implementation period, LTC staff were also encouraged to use the VR with residents as much as they could, including residents who were not formally part of the research study. At each VR experience, staff noted observations about the consented participants’ attention and focus on tasks and to the participants’ interactions with the staff members and other residents during the VR experience. They also noted participant emotions expressed during the VR through the Interact Short tool. They also conducted a brief interview with each participant, asking them about their experience and the effect of the VR on any chronic pain. After the 2-week period, the research team returned to the LTC community where they collected feedback from the staff on their experiences of using VR with older adults in their community using a brief structured interview guide. The qualitative data emerged from participant responses that were captured during the observations and during the brief interview after each experience and was analyzed using grounded theory procedure . 37
Results
Physical responses to the virtual reality experiences
The PAINAD data indicated that throughout the 102 viewing experiences a minority of participants displayed occasionally labored breathing (n = 5), noisy/labored breathing (n = 1), occasional moans or groans (n = 4), sad or frightened facial expressions (n = 3), tense (n = 8) or rigid body language (n = 1). For the most part, participants did not experience observable discomfort during the experiences.
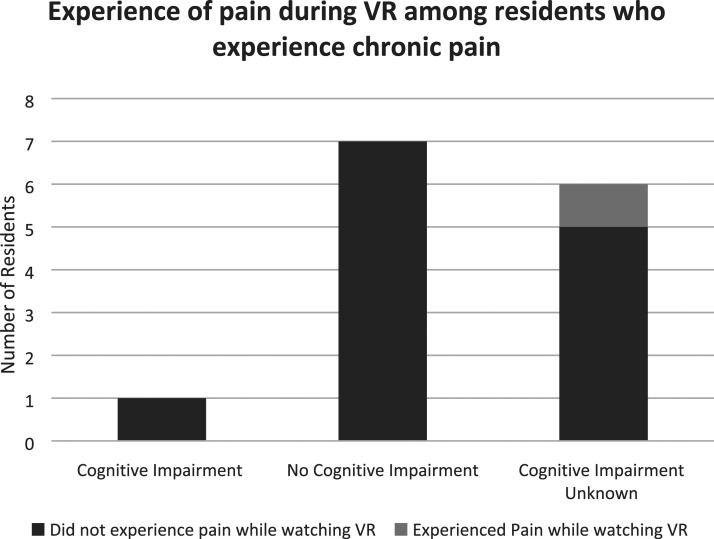
Participants were asked whether they experienced pain on a regular basis and whether they had experienced pain while immersed in the VR experience. Their responses are summarized in Figure 1. The data show that the vast majority of those who experience pain on a regular basis did not experience it during the VR sessions. Seven participants had known cognitive impairments and only one of them experienced pain on an ongoing basis, and this person reported that they did not experience any pain during the VR session. Of the 14 participants with no self-reported cognitive impairments, 50% (n = 7) experienced pain on an ongoing daily basis and all reported not experiencing it during the VR session. Of the 11 participants with unknown cognitive impairments, 55% (n = 6) experienced pain on an ongoing basis and five of the six did not experience it during the VR session.
Figure 1.
Experience of pain during virtual reality among residents who experience chronic pain.
The participants spoke of how the VR experience helped distract them from their ongoing and regular pain
“No, absolutely, I forgot about it.” (L1_1)
“No, I think it will distract” (L2_5).
“You can forget pain when you see something peaceful.” (L1_6)
In 25% of the 102 VR viewing experiences (n = 25) participants self-initiated movement all of the time and in 27% (n = 28) of the VR experiences participants self-initiated movement some of the time while engaging with the VR. This included moving their arms or legs, reaching out to try to touch objects or to point, moving their wheelchairs or standing up and moving around. In 31% of experiences (n = 32), the participant did not self-initiate movement at anytime during the VR experience. Participants were seen responding both verbally and non-verbally to the narration on the VR experiences, to the staff questions and to the experiences themselves. Non-verbal reactions that the staff/researchers noted included relaxing into the experience, smiling, and nodding. Verbal responses included answering questions on what they were observing, describing what was being observed and asking questions about what was being observed.
A staff member noted that in the case of one resident who has chronic hand tremors, the tremors reduced during the experience. In the case of another resident with cerebral palsy, a staff member noted that while it was normal for the resident to have noisy labored breathing normally, both the laboured breathing and the tremors reduced while watching the VR experience. In addition, one participant with aphasia and a physical impairment that made him favor his right side, also moved left during the VR experience, something staff noted that he rarely does.
The research team noted three instances when the participants showed physical signs of discomfort with the VR experience. In one case, the participant was restless and did not complete the entire experience. In an experience that involved standing at the edge of a drop, one participant said they felt dizzy if they looked straight down, while another wanted the wheelchair to be moved away from the “edge” to feel safer.
Cognitive response to the virtual reality experiences
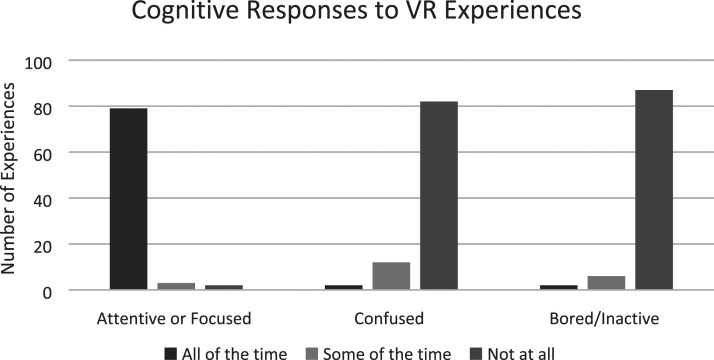
We measured cognitive response using the Interact Short form. Results of participants’ cognitive responses are described in Figure 2. In 77% of the experiences (n = 79), participants were attentive or focused throughout the viewing. Participants were confused or inattentive all of the time in only two instances each.
Figure 2.
Cognitive responses to virtual reality experiences.
Participants were excited to visit places they had been to in the past as it brought back memories and they reminisced about these.
“It’s excellent. It’s very relaxing. Lots of reminiscing about boats and fishing.” (L1_6)
“Brings back good memories with my lady…Looking for animals I've seen before.” (L4_6)
Others found the experiences a good way to visit a place they had never been to before. For others, these experiences created new memories.
“I wish I went when I was younger. It felt like I was there. It’s nice that it’s on the water because it’s so calm. I can’t imagine the price tag of the houses. Excellent, felt real, felt safe. Clear picture. Good pace.” (L1_8)
“Enjoyed it. I have never been to Lake Louise before. Now I know what it looks like.” (L4_2)
“Marvelous. You feel as though you’re there. Now I can say I’ve been to Hamilton!” (L1_3)
Emotional responses to the virtual reality experiences
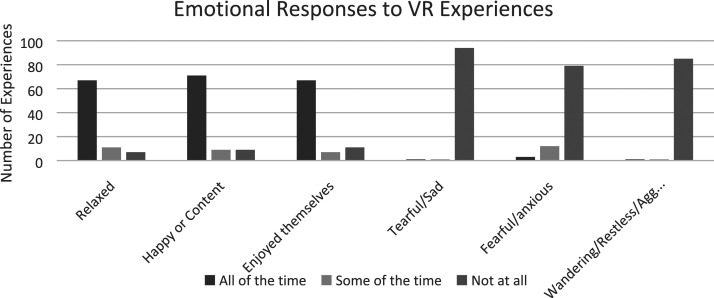
Emotional responses to the VR sessions were captured using the Interact Short form and are summarized in Figure 3. Of the 102 VR viewing experiences observed, participants were relaxed (n = 67) and enjoyed themselves (n = 67) and were happy (n = 71) throughout the experience. In few VR experiences, participants appeared tearful/sad (n = 2), confused (n = 2), fearful/anxious (n = 3), or bored/inactive (n = 2) nearly the entire time they were viewing the VR.
Figure 3.
Emotional responses to virtual reality experiences.
The participants expressed a positive verbal response during 82% of the observed experiences (n = 84). They used words such as “nice” “very nice,” “awesome,” “beautiful,” “pretty,” “amazing,” “great,” “interesting,” “very interesting,” “lovely,” “fantastic,” “relaxing,” “wonderful,” “fantastic,” and “enjoyed it” to describe the immersion experience. Some of the participants commented on how this experience felt very real and that it was a positive change from their daily routine.
“Amazing. Something different.” (L1_2)
“It’s beautiful. All those restaurants. Lord have mercy. I felt I was there. Would like to see the cedar trees up close.” (L1_10)
“Fantastic. Sharp images and audio. It felt very real. Comfortable with what was around me. Felt like I would fall into the water, but I knew I wouldn’t.” (L1_4)
For some participants, the VR immersion allowed them to enjoy experiences they could not take for granted anymore.
“Very incredible to do. We can’t go everywhere else. So very good to do.” (L4_1)
“Felt great.” “I was going to enter the restaurant.” (L4_8)
“I feel like I'm there. I get to ride the boat.” (L1_1)
“Very good” “Can see things that you couldn't see unless you go there.” (L4_5)
Few participants had recommendations on other places they would like to visit using VR.
“Peggy’s Cove next time. Neck is a bit sore. Makes me feel like I'm there” (L1_6)
“Good. I would do it again.” “I’d like to see Algonquin.” (L4_4)
Social interactions
Participants related well to the staff and to others around them all the time during 86% of the experiences (n = 88). Based on the qualitative interviews, some participants were excited to view more such experiences and to recommend the same to others. However, the percentage of respondents who said that they would like to try it again, or may like to try it again varied significantly by location and ranged from 22% at Location C to 83% at Location B. On average, 53% responded yes to either of these questions. When asked how they liked the experience, many respondents offered positive feedback.
“Truly beautiful! Absolutely fantastic. Phenomenal. Can not tell you how fantastic this is. The view is absolutely breath taking. I would recommend this to everyone.” (L4_2)
Discussion
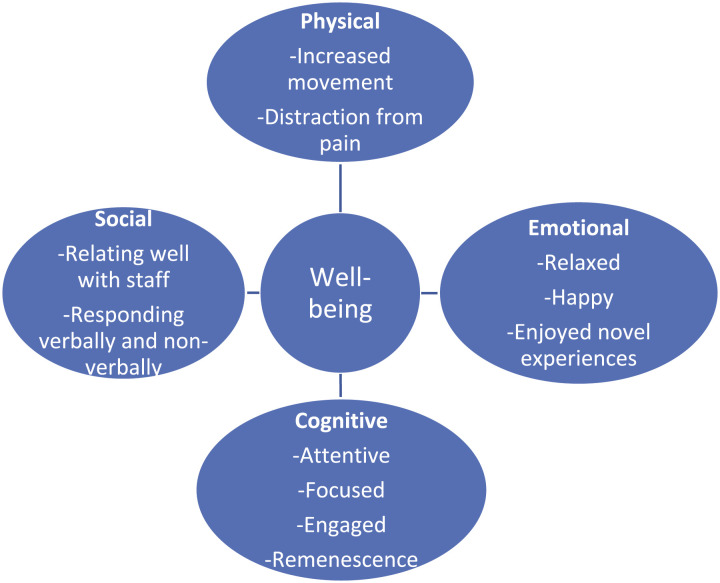
The findings of this paper demonstrate the potential of VR experiences to contribute to the physical, emotional, cognitive, and social well-being of older adults. Figure 4 below provides a summary overview of the various ways in which the VR experiences were related to the participants’ well-being in four domains: Physical, Emotional, Cognitive and Social.
Figure 4.
Overview of virtual reality experiences contribution to participants’ well-being.
Physical well-being
Residents in LTC homes typically have lower levels of physical activity and movement than community-dwelling older adults 29 and VR is a promising intervention to increase physical movement among such residents. In this pilot implementation, participants initiated many physical movements in response to the VR activity such as moving their limbs, reaching out and moving around. The participants also responded verbally and non-verbally to the narration in the VR or to staff questions in relation to the VR experiences.
Past research has identified the role that VR experiences can play in distraction from pain.14,26 Participants in this research also identified that the VR experience distracted them from the chronic pain they experience in their day to day lives. Moreover, an important finding of this pilot implementation study was the indication that VR appeared to be an effective distraction from pain for residents irrespective of cognitive status. Our study noted anecdotal findings of modified physical behaviors during the VR experience, including reduced tremors, reduced coughing, and increased movement on the neglected side.
Emotional well-being
Similar to the other studies with VR and older adults,7,13 the participants in the current study found the VR experiences to be enjoyable. For the most part, participants in this study were relaxed during the VR experience and felt happy or content while viewing it. Participants noted the positive change the VR experience was from the daily routine and the way in which the VR allowed them to enjoy experiences they could no longer take for granted. The participants’ verbal responses to the experiences captured in this paper reflect the joy the VR experiences brought to the participants, when they were able to visit/revisit a place they could likely not physically travel to themselves given their current situations.
Participants in this study expressed an interest in the sites they had visited and had suggestions for sites they would want to visit virtually in future. The creation of VR experiences based on initial feedback and recommendations seemed to have enhanced the enjoyment of the viewing.
Cognitive well-being
Most of the participants were observed to be attentive and focused throughout the VR experiences. Our study also found that the VR experiences were a source of reminiscence for the participants. The VR experience allowed participants to share stories of times they had visited the sites in person with loved ones and to think back to the sights, sounds and experiences of the moment. The findings suggest that VR can be an important tool in the use of Reminiscence Therapy which in turn can help improve mood and cognitive abilities for older adults with dementia. 38
Social well-being
Participants related well to the staff and to others around them during a majority of the experiences. The VR experiences engaged the staff and the participants in conversations that otherwise would not have happened. Over half of the participants were excited to view more such experiences and to recommend the same to others. This highlights the potential for VR to be a source of conversation and engagement between the older adults, other residents, and staff in LTC homes. Similar to the study by Baker et al., 7 our study highlighted the potential of VR to increase engagement between older adults and those around them. Most VR programs for older adults described in the literature, like our study, have focused on experiences for individuals. Future research should focus on the potential for multi-player, immersive VR social games to enhance social interaction.
Implications for practice and research
VR has applications in recreation for older adults, and our data from this pilot study suggest that VR also shows promise as a therapeutic intervention. VR technology can offer clinicians another avenue of exploration of how to treat patients. If patients are comfortable with VR, they may be more likely to adopt therapeutic interventions designed using VR and/or consider augmented reality (AR) as a related approach. VR techniques could be used to support physical therapy/rehabilitation, reminiscence and socialization, among other domains. Further research should continue to establish best practices in relation to the use of VR with older adults. Some of the learnings from this study that could inform such a development include: providing iconic scenes as sites for the visit; adding narration and music to the scenes to engage the older adult; providing a range of immersive scenario options; noting whether particular experiences are inappropriate for those with particular phobias; providing hygiene instructions to prevent disease transfer during the use of VR headsets; and the ways to integrate VR into other recreational programming to maximize the potential to improve well-being.
Limitations
As this was an applied research project, the partner organization’s needs and interests structured the study. The purpose of the research partnership was to test VR as a proof of concept—the process of creating and implementing VR technology and staff and resident engagement—as opposed to the demonstration of clinical outcomes.
The data for this study were based on convenience sampling and may be prone to bias. The implementation sites were picked by the partner organization who was invested in implementing a successful VR program. The staff at the four sites selected participants for the study based on whom the staff felt would benefit most or would be eager to participate. In addition, our partners determined which sites the technology would be piloted at. As such, they are not a random sample and prone to bias. The findings, thus, cannot be generalized to a larger population.
The VR experiences were piloted with a smaller group of older adults with a diagnosis of dementia that participated in an adult day program while the implementation was carried out with older adults, some of whom had self reported cognitive impairment, residing in LTC. No cognitive screening was carried out for the older adults who participated in this study.
Last, the kind of experiences crafted for the implementation were limited by access to spaces that could be filmed and to the use of English language. This limited the ability to cater to all participants in terms of reminiscence needs.
Conclusion
Past research on VR implementation with older adults is largely in lab-like settings. There is limited literature on the use of VR technology with older adults in LTC. To the best of our knowledge, no other study has described the potential of VR technology in supporting older adults’ well-being in Canadian LTC, and this study makes a valuable addition to an emerging body of literature. Our study describes how residents and staff can be engaged in the creation and implementation of meaningful VR experiences that can be relatively cost effective and have the potential to benefit individuals in LTC.
This study joins an emerging literature on the use of VR among older adults. The study piloted the use of unique VR immersive experiences based on the recommendations collected from residents in LTC homes. The findings of this study highlight the ways in which carefully crafted VR experiences can contribute to the well-being of older adults in LTC homes. These findings are particularly relevant during the ongoing COVID pandemic where VR provides an opportunity for the residents to stay indoors and safe, while still engaging in meaningful and enjoyable activities.
Notes
Self-reported cognitive status was asked of those who participated in the focus group. Many (but not all) of those people also participated in the VR implementation. However, some additional people were recruited in the implementation of the VR, and self-reported cognitive status was not collected from those individuals.
Footnotes
Author contributions: FC took leadership in conceptualizing the manuscript and writing up the findings and discussion, in addition to assisting with data collection. LH provided contributed to the writing of the manuscript and to the shaping of the findings and discussions and assisted with data collection. AA contributed to the introduction and literature review with support from AK and DB. YK assisted with developing the VR experiences. MD assisted with the focus group transcription and analysis. JD assisted with implementation data entry and management. AJ and CR assisted with data collection and initial literature review. LT was the principal investigator on the study and was involved in protocol development and gaining ethical approval. KWN provided assistance with the VR manual design and development. KD provided methodological input. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded through a Natural Sciences and Engineering Research Council (NSERC)- College and Community Social Innovation Fund grant (NSERC CCSIF grant 520081–17).
Guarantor: FC
ORCID iDs
Ferzana Chaze https://orcid.org/0000-0002-5335-9346
Leigh Hayden https://orcid.org/0000-0002-3345-7686
Ashwin Kamath https://orcid.org/0000-0003-3130-9222
References
- 1.Statistics Canada . Canada year book 2010 @BULLET catalogueno. 11-402-X, https://www150.statcan.gc.ca/n1/pub/11-402-x/11-402-x2010000-eng.htm?wbdisable=true (2016, accessed 20 January 2020). [Google Scholar]
- 2.Chesler J, McLaren S, Klein B, et al. The effects of playing nintendo wii on depression, sense of belonging and social support in Australian aged care residents: a protocol study of a mixed methods intervention trial. BMC Geriatr 2015; 15: 106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arlati S, Colombo V, Spoladore D, et al. A social virtual reality-based application for the physical and cognitive training of the elderly at home. Sensors (Basel) 2019; 19: 261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Canadaof G. Action for seniors report, https://www.canada.ca/en/employment-social-development/programs/seniors-action-report.html#tc2a (2014). [Google Scholar]
- 5.Garner R, Tanuseputro P, Manuel DG, et al. Transitions to long-term and residential care among older Canadians. Health Rep 2018; 29(5): 13–23. [PubMed] [Google Scholar]
- 6.Ontario Long Term Care Association . Facts and figures. Toronto, Canada: OLTCA. https://www.oltca.com/oltca/OLTCA/Public/LongTermCare/FactsFigures.aspx (2019, accessed 10 January 2020). [Google Scholar]
- 7.Baker S, Waycott J, Robertson E, et al. Evaluating the use of interactive virtual reality technology with older adults living in residential aged care. Inf Process Manag 2019; 57(3): 102105. [Google Scholar]
- 8.Hughes S, Warren-Norton K, Spadafora P, et al. Supporting optimal aging through the innovative use of virtual reality technology. Multimodal Technol Interact 2017; 1(4): 23. DOI: 10.3390/mti1040023. [DOI] [Google Scholar]
- 9.Fox J, Arena D, Bailenson JN. Virtual reality: a survival guide for the social scientist. J Media Psychol 2009; 21(3): 95–113. DOI: 10.1027/1864-1105.21.3.95. [DOI] [Google Scholar]
- 10.Appel L, Appel E, Bogler O, et al. Older adults with cognitive and/or physical impairments can benefit from immersive virtual reality experiences: a feasibility study. Front Med; 6: 329. DOI: 10.3389/fmed.2019.00329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chesham A, Wyss P, Müri RM, et al. What older people like to play: genre preferences and acceptance of casual games. JMIR Serious Games 2017; 5: e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim A, Darakjian N, Finley JM. Walking in fully immersive virtual environments: an evaluation of potential adverse effects in older adults and individuals with parkinson’s disease. J Neuroeng Rehabil 2017; 14: 16. DOI: 10.1186/s12984-017-0225-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Benham S, Kang M, Grampurohit N. Immersive virtual reality for the management of pain in community-dwelling older adults. OTJR (Thorofare N J) 2019; 39: 90–96. [DOI] [PubMed] [Google Scholar]
- 14.Bani Mohammad E, Ahmad M. Virtual reality as a distraction technique for pain and anxiety among patients with breast cancer: a randomized control trial. Palliat Support Care 2019; 17: 29–34. [DOI] [PubMed] [Google Scholar]
- 15.Morris LD, Louw QA, Grimmer-Somers K. The effectiveness of virtual reality on reducing pain and anxiety in burn injury patients: a systematic review. Clin J Pain; 25: 815–826. DOI: 10.1097/AJP.0b013e3181aaa909. [DOI] [PubMed] [Google Scholar]
- 16.Yeşilyaprak SS, Yildirim MŞ, Tomruk M, et al. Comparison of the effects of virtual reality-based balance exercises and conventional exercises on balance and fall risk in older adults living in nursing homes in Turkey. Physiother Theory Pract 2016; 32: 191–201. [DOI] [PubMed] [Google Scholar]
- 17.Strong J. Immersive virtual reality and persons with dementia: a literature review. J Gerontol Soc Work 2020; 63: 209–226. DOI: 10.1080/01634372.2020.1733726. [DOI] [PubMed] [Google Scholar]
- 18.Optale G, Urgesi C, Busato V, et al. Controlling memory impairment in elderly adults using virtual reality memory training: a randomized controlled pilot study. Neurorehabil Neural Repair 2010; 24: 348–357. [DOI] [PubMed] [Google Scholar]
- 19.Man DWK, Chung JCC, Lee GYY. Evaluation of a virtual reality-based memory training programme for Hong Kong Chinese older adults with questionable dementia: a pilot study. Int J Geriatr Psychiatry 2012; 27: 513–520. [DOI] [PubMed] [Google Scholar]
- 20.Henderson L, Knight T. Integrating the hedonic and eudaimonic perspectives to more comprehensively understand wellbeing and pathways to wellbeing. Int J Wellbeing 2012; 2: 196–221. [Google Scholar]
- 21.Ryan RM, Deci EL. On happiness and human potentials: a review of research on hedonic and eudaimonic well-being. Annu Rev Psychol; 52: 141–166. DOI: 10.1146/annurev.psych.52.1.141. [DOI] [PubMed] [Google Scholar]
- 22.Ryff CD, Singer BH. Know thyself and become what you are: a eudaimonic approach to psychological well-being. J Happiness Stud 2008; 9: 13–39. DOI: 10.1007/s10902-006-9019-0. [DOI] [Google Scholar]
- 23.Centers for Disease Control and Prevention . Well-being concepts (HRQOL). Atlanta, GE: CDC, 2018, https://www.cdc.gov/hrqol/wellbeing.htm#three. [Google Scholar]
- 24.Segerstrom SC, Eisenlohr-Moul TA, Evans DR, et al. Repetitive thought dimensions, psychological well-being, and perceived growth in older adults: a multilevel, prospective study. Anxiety Stress Coping 2015; 28: 287–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Force CPT. No Title, 2019, https://www.canada.ca/content/dam/hc-sc/documents/corporate/about-health-canada/public-engagement/external-advisory-bodies/canadian-pain-task-force/report-2019/canadian-pain-task-force-June-2019-report-en.pdf. [Google Scholar]
- 26.Keefe FJ, Huling DA, Coggins MJ. Virtual reality for persistent pain. Pain 2013; 153: 2163–2166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chirico A, Lucidi F, De Laurentiis M, et al. Virtual reality in health system: beyond entertainment. A mini-review on the efficacy of VR during cancer treatment. J Cell Physiol; 231: 275–287. DOI: 10.1002/jcp.25117. [DOI] [PubMed] [Google Scholar]
- 28.Miller KJ, Adair BS, Pearce AJ, et al. Effectiveness and feasibility of virtual reality and gaming system use at home by older adults for enabling physical activity to improve health-related domains: a systematic review. Age Ageing 2014; 43: 188–195. [DOI] [PubMed] [Google Scholar]
- 29.Chen YM, Li YP. Motivators for physical activity among ambulatory nursing home older residents. Sci World J 2014; 2014: 329–397. DOI: 10.1155/2014/329397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gonzalez J, Mayordomo T, Torres M, et al. Reminiscence and dementia: a therapeutic intervention. Int Psychogeriatr 2015; 27: 1731–1737. [DOI] [PubMed] [Google Scholar]
- 31.Ferreira AL. Musiquence – design, implementation and validation of a customizable music and reminiscence cognitive stimulation platform for people with dementia Universidade da Madeira, https://run.unl.pt/bitstream/10362/116417/1/Ferreira_2020.pdf (2020, accessed 15 December 2021). [Google Scholar]
- 32.Dietrichkeit M, Grzella K, Nagel M, et al. Using virtual reality to explore differences in memory biases and cognitive insight in people with psychosis and healthy controls. Psychiatry Res 2020; 285: 112787. DOI: 10.1016/j.psychres.2020.112787. [DOI] [PubMed] [Google Scholar]
- 33.Słyk S, Zarzycki MZ, Kocwa-Karnaś A, et al. Virtual reality in the diagnostics and therapy of neurological diseases. Expert Rev Med Devices 2019; 16: 1035–1040. DOI: 10.1080/17434440.2019.1693892. [DOI] [PubMed] [Google Scholar]
- 34.Chao Y-Y, Scherer YK, Montgomery CA. Effects of using nintendo wiiTM exergames in older adults: a review of the literature. J Aging Health 2015; 27: 379–402. [DOI] [PubMed] [Google Scholar]
- 35.Warden V, Hurley AC, Volicer L. Development and psychometric evaluation of the pain assessment in advanced dementia (PAINAD) scale. J Am Med Dir Assoc 2003; 4(1): 9–15. DOI: 10.1097/01.JAM.0000043422.31640.F7. [DOI] [PubMed] [Google Scholar]
- 36.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 1999; 89: 1322–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Strauss A, Corbin J. Basics of qualitative research: techniques for developing grounded theory. Thousand Oaks, CA: SAGE Publications Inc., 1998. [Google Scholar]
- 38.Cotelli M, Manenti R, Zanetti O. Reminiscence therapy in dementia: a review. Maturitas 2012; 72: 203–205. DOI: 10.1016/j.maturitas.2012.04.008. [DOI] [PubMed] [Google Scholar]