ABSTRACT.
Epstein–Barr virus (EBV) is the most common cause of infectious mononucleosis (IM) and IM is a clinical syndrome typically characterized by fever, pharyngitis, and cervical lymph node enlargement. We describe the case of a 19-year-old man with IM complicated by splenic infarction. The patient visited our hospital because of upper abdominal pain without a fever and sore throat. Abdominal computed tomography revealed a low-density area in the spleen, which indicated splenic infarction. The next day, he developed a fever. After diminishing abdominal pain and fever, he developed pharyngitis accompanied by fever. Acute EBV infection was confirmed by serological tests. The patient was successfully managed with no specific therapy. Splenic infarction is a rare complication of IM and this case showed that splenic infarction can precede a fever and pharyngitis.
INTRODUCTION
IM is a common condition that mostly affects young individuals all over the world. The most frequent cause of IM is acute Epstein–Barr virus (EBV) infection. In the developing countries, people are often infected in early childhood, however, the age at which EBV infection is acquired is increasing.1 The typical clinical manifestations of IM are fever, pharyngitis, and cervical lymph node enlargement.2 The involvement of the reticuloendothelial system, such as the spleen, associated with IM has also been observed. Splenomegaly is seen in approximately 60% of cases3 and usually begins to recede by the third week of the disease. Splenic rupture can potentially be a life-threatening complication and is estimated to occur in 0.1–0.5% of cases.4 Splenic infarction has also been described as a complication of IM,5–9 but it is rare, and its incidence is unknown.
Herein, we describe the case of a 19-year-old man with IM due to acute EBV infection complicated by splenic infarction, which preceded a fever and pharyngitis.
CASE REPORT
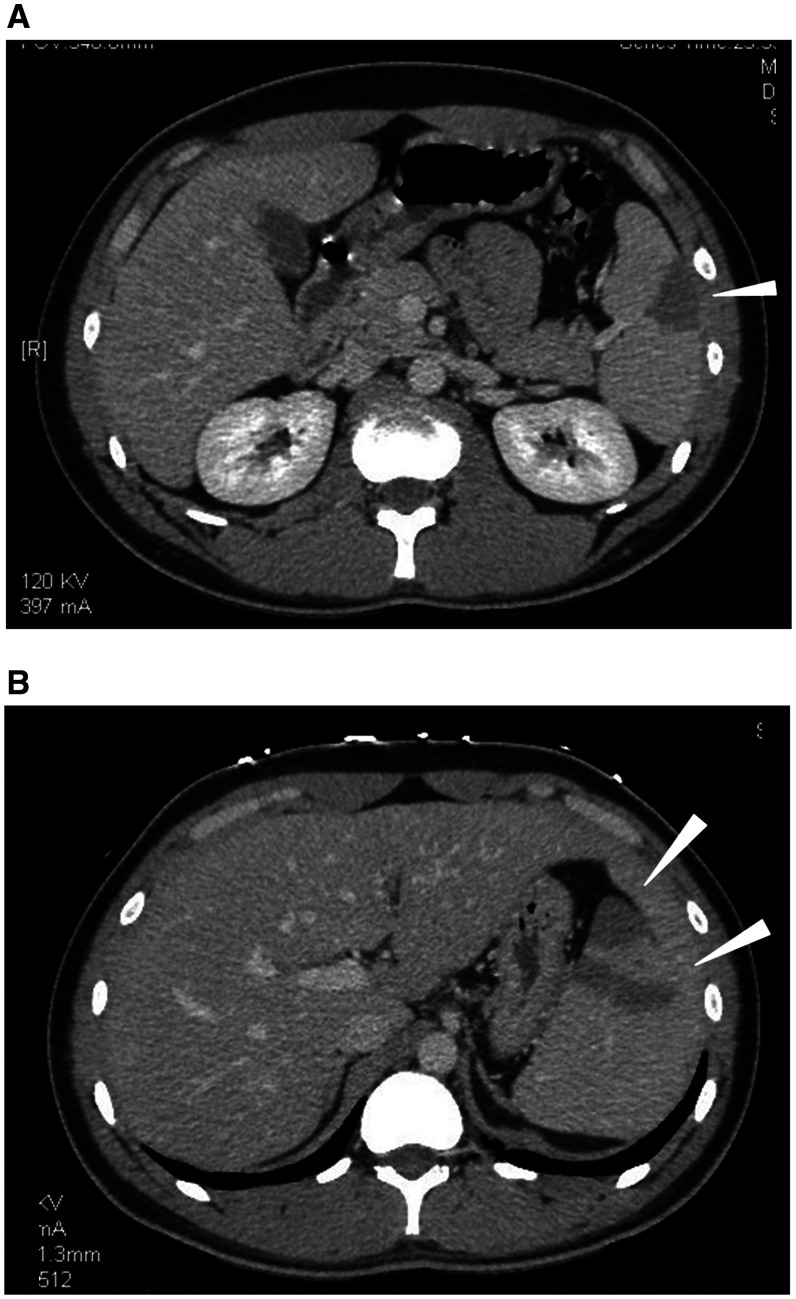
A 19-year-old Japanese man presented to our emergency room in the evening due to a persistent abdominal pain in the epigastric region and left upper quadrant, which developed after lunch. He did not have a fever, sore throat, nausea, or diarrhea. Abdominal contrast-enhanced computed tomography (CT) revealed a low-density area in the spleen, which indicated splenic infarction (Figure 1A). The etiology was unknown, and detailed examinations at the outpatient department within a few days were planned. However, the next evening, he visited us again due to the development of fever and exacerbation of abdominal pain. Abdominal CT revealed new multiple low-density areas in the spleen (Figure 1B). His medical history was unremarkable and he did not take any medication.
Figure 1.
(A) On day 0, a contrast-enhanced computed tomography (CT) of the abdomen shows wedge-shaped, low-density defect in the peripheral area of the spleen (white arrowhead) in favor of splenic infarction. (B) On day 1, a contrast-enhanced CT of the abdomen reveals new multiple low-density defects in the spleen (white arrowheads).
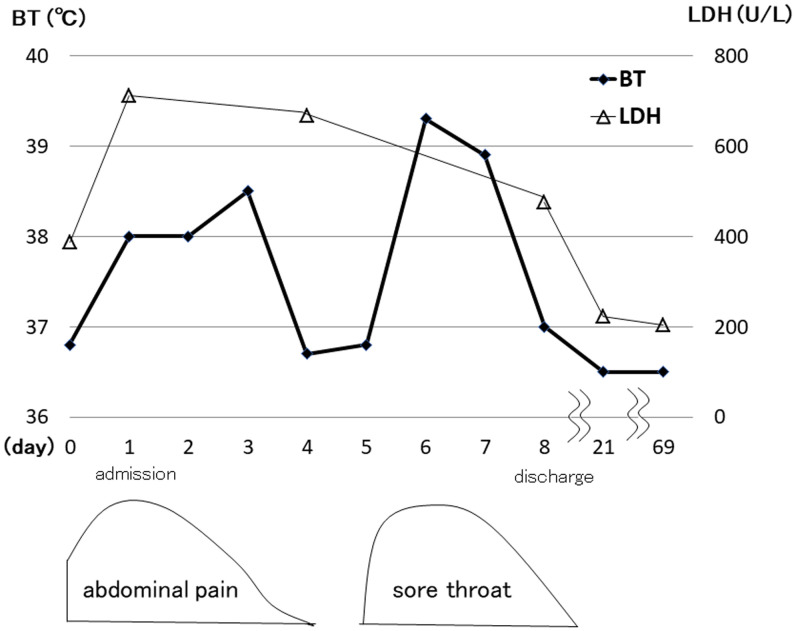
Physical examination revealed a blood pressure of 132/72 mm of Hg, heart rate of 85 beats/min, respiratory rate of 18 breaths/min, and body temperature of 38.9°C. He was alert and conscious. His tonsils were neither swollen nor red along with no observed white patches. The left posterior cervical lymph nodes were palpable and tender. His epigastric region and left upper quadrant were tender. The liver and spleen were not palpable. Laboratory findings showed a white blood cell count of 6,000/μL (neutrophils, 46%; atypical lymphocytes, 32%), hemoglobin level of 15.7 g/dL, platelet count of 14.9 × 104/μL, aspartate aminotransferase level of 365 IU/L, alanine aminotransferase level of 402 IU/L, lactate dehydrogenase (LDH) level of 711 IU/L, and C-reactive protein level of 1.2 mg/dL. Results of coagulation tests, including prothrombin time, activated partial thromboplastin time, fibrinogen, antithrombin III, D-dimer, protein C activity, and protein S activity, were normal. Tests for antinuclear antibody, lupus anticoagulant, and antiphospholipid IgM and IgG tests were negative. Serological tests revealed that EBV–viral capsid antigen IgM and IgG were positive, and the EB nuclear antigen IgG was negative. Serologies for cytomegalovirus, hepatitis B and C, and HIV were unremarkable. Electrocardiogram showed normal sinus rhythm, and a Holter electrocardiogram did not detect arrhythmia. The patient was diagnosed with IM due to an acute EBV infection complicated by splenic infarction. We prescribed acetaminophen as an antipyretic analgesic and took care of him without specific intervention. On day 4 after admission, his fever and abdominal pain subsided. However, on day 5, he complained of a sore throat. His tonsils were red and swollen with white patches. The next day, he developed a fever again. On day 8, his symptoms spontaneously improved, and he was discharged from the hospital (Figure 2). Two weeks later, the patient was followed up in the outpatient department. He completely recovered without any sequelae, and liver function tests and LDH returned to normal levels. Two months later, abdominal CT revealed a remarkable diminishment of splenic infarction.
Figure 2.
Clinical course. BT = body temperature; LDH = lactate dehydrogenase.
DISCUSSION
The clinical course of this patient raises two important issues. First, splenic infarction can develop in IM due to EBV infection and can precede a fever and pharyngitis. Second, splenic infarction in IM can be managed conservatively.
Splenic infarction is a rare complication of IM and its incidence is unknown. A total of 26 cases of splenic infarction due to EBV infection have been reported in the medical literature published between 1961 and 2018.5–9 Splenic infarction usually causes left upper quadrant pain. None of the previously reported cases have mentioned that abdominal pain preceded a fever and pharyngitis. However, our patient clearly showed that abdominal pain due to splenic infarction occurred before a fever and pharyngitis developed. This suggests that IM can develop presenting abdominal pain as an initial and sole symptom.
The mechanism of splenic infarction in IM is yet to be elucidated, however, several mechanisms have been proposed. A few cases have been reported to have an underlying hematologic disorder, including hereditary spherocytosis,10 hereditary spherocytosis, and protein C activity deficiency,11 and sickle cell anemia traits.12 Nevertheless, most patients did not have any obvious underlying diseases, as in our case. Arterial blood supply may be insufficient for the increased demand of the enlarged spleen during the acute stage of IM, leading to local infarction. The presence of a transient hypercoagurable state during IM, resulting in low perfusion to the spleen, has been proposed. Transient elevated antiphospholipid antibodies,13 lupus anticoagulant,5 and factor VIII14 have been documented during the acute stage of IM in cases of splenic infarction. These transient prothrombotic factors may initiate autoimmune-mediated infarction via thrombosis.15 An increased level of circulating immune complexes due to B cell proliferation, which promotes leukocyte aggregation and adhesiveness, has been proposed to be associated with splenic infarction with EBV.16 Unfortunately, we did not know the mechanism of splenic infarction in our case.
One study summarized the outcomes of 19 cases of splenic infarction in IM.6 Splenectomy was performed in five cases (26%), although the reason for the surgery was unknown, and 14 cases (74%) experienced improvement through medical treatment. There were no deaths. A few patients received anticoagulant or corticosteroid therapy, but their effectiveness was unclear. In other reports, patients were successfully managed without surgery. In most cases, splenic infarction in IM can be managed conservatively with no specific therapy under close observation, as in our case.
In summary, although IM due to EBV infection is a very common condition in young people, splenic infarction is a rare and an infrequent complication. Our case showed that upper abdominal pain due to splenic infarction can develop as an initial symptom of IM and can precede a fever or pharyngitis. This suggests that IM should be in the differential diagnosis for splenic infarction in young people, even if a fever or pharyngitis has not yet been observed. No specific therapy may be required for splenic infarction in IM.
REFERENCES
- 1. Balfour HH Jr Odumade OA Schmeling DO Mullan BD Knight JA Vezina HE Thomas W Hogquist KA , 2013. Behavioral, virologic, and immunologic factors associated with acquisition and severity of primary Epstein-Barr virus infection in university students. J Infect Dis 207: 80–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Luzuriaga K Sullivan JL , 2010. Infectious mononucleosis. N Engl J Med 362: 1993–2000. [DOI] [PubMed] [Google Scholar]
- 3. Ishii T Sasaki Y Maeda T Komatsu F Suzuki T Urita Y , 2019. Clinical differentiation of infectious mononucleosis that is caused by Epstein–Barr virus or cytomegalovirus: a single-center case-control study in Japan. J Infect Chemother 25: 431–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Macsween KF Crawford DH , 2003. Epstein–Barr virus-recent advances. Lancet Infect Dis 3: 131–140. [DOI] [PubMed] [Google Scholar]
- 5. Naviglio S Abate MV Chinello M Ventura A , 2016. Splenic infarction in acute infectious mononucleosis. J Emerg Med 50: e11–e13. [DOI] [PubMed] [Google Scholar]
- 6. Heo DH Baek DY Oh SM Hwang JH Lee CS Hwang JH , 2017. Splenic infarction associated with acute infectious mononucleosis due to Epstein–Barr virus infection. J Med Virol 89: 332–336. [DOI] [PubMed] [Google Scholar]
- 7. Noor M Sadough M Chan S Singh G , 2017. Splenic infarct in a patient with infectious mononucleosis: a rare presentation. J Community Hosp Intern Med Perspect 7: 248–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Li Y George A Arnaout S Wang JP Abraham GM , 2018. Splenic infarction: an under-recognized complication of infectious mononucleosis? Open Forum Infect Dis 5: ofy041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Suzuki Y Kakisaka K Kuroda H Sasaki T Takikawa Y , 2018. Splenic infarction associated with acute infectious mononucleosis. Korean J Intern Med (Korean Assoc Intern Med) 33: 451–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Suzuki Y et al. 2017. Splenic infarction after Epstein–Barr virus infection in a patient with hereditary spherocytosis. Int J Hematol 85: 380–383. [DOI] [PubMed] [Google Scholar]
- 11. Breuer C Janssen G Laws HJ Schaper J Mayatepek E Schroten H Tenenbaum T , 2008. Splenic infarction in a patient hereditary spherocytosis, protein C deficiency and acute infectious mononucleosis. Eur J Pediatr 167: 1449–1452. [DOI] [PubMed] [Google Scholar]
- 12. Symeonidis A. et al. , 2001. Non hypoxia-related splenic infarct in a patient with sickle cell trait and infectious mononucleosis. Acta Haematol 105: 53–56. [DOI] [PubMed] [Google Scholar]
- 13. van Hal S Senanayake S Hardiman R , 2005. Splenic infarction due to transient antiphospholipid antibodies induced by acute Epstein–Barr virus infection. J Clin Virol 32: 245–247. [DOI] [PubMed] [Google Scholar]
- 14. Machado C Melo Salgado J Monjardino L , 2015. The unexpected finding of a splenic infarction in a patient with infectious mononucleosis due to Epstein–Barr virus. BMJ Case Rep 2015: bcr2015212428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gang MH Kim JY , 2013. Splenic infarction in a child with primary Epstein–Barr virus infection. Pediatr Int 55: e126–e128. [DOI] [PubMed] [Google Scholar]
- 16. Gavriilaki E Sabanis N Paschou E Grigoriadis S Mainou M Gaitanaki A Skargani-Koraka M , 2013. Splenic infarction as a rare complication of infectious mononucleosis due to Epstein–Barr virus infection in a patient with no significant comorbidity: case report and review of the literature. Scand J Infect Dis 45: 888–890. [DOI] [PubMed] [Google Scholar]