Abstract
Simple Summary
We meta-analyzed prospective epidemiological studies reporting on the association between fish consumption and colorectal cancer (CRC) risk among humans and reviewed preclinical studies that examined the link between fish components and colorectal carcinogenesis in animals. By pooling results from 25 studies (encompassing over 25,000 CRC cases) published up to November 2020, we found convincing evidence that increased fish consumption may protect from CRC development among humans. The review of animal studies allowed identifying several biological mechanisms able to explain the associations that have emerged in human populations. Dietary recommendations for cancer prevention should incorporate the evidence from this literature review and meta-analysis.
Abstract
Background: Epidemiological studies on the association between fish consumption and colorectal cancer (CRC) risk have yielded inconsistent results, despite evidence from preclinical studies that long-chain ω-3 polyunsaturated fatty acids inhibit colorectal carcinogenesis. We conducted a meta-analysis of prospective epidemiological studies investigating the association between fish consumption and CRC risk among humans and reviewed studies examining the link between fish components and colorectal carcinogenesis in animal models. Methods: We included studies published until November 2020. We calculated the summary risk ratio (SRR) and 95% confidence intervals (CI) through random effects meta-analysis models in order to summarize evidence from studies among humans. Results: Twenty-five prospective epidemiological studies encompassing 25,777 CRC cases were included. Individuals in the highest (vs. lowest) category of fish consumption had a significantly reduced risk of CRC (SRR 0.94, 95%CI 0.89–0.99). In dose–response meta-analysis, a 50-g increment in the daily consumption of fish was associated with a statistically significant 4% reduction in CRC risk (SRR 0.96, 95%CI 0.92–0.99). Preclinical studies (n = 25) identified multiple mechanisms of action of fish and fish components on colorectal carcinogenesis. Conclusions: Dietary recommendations for cancer prevention should take into account the evidence from epidemiological and preclinical studies that increasing fish consumption may be effective in preventing CRC.
Keywords: fish consumption, colorectal cancer, epidemiological studies, animal studies, review, meta-analysis
1. Introduction
Colorectal cancer (CRC) is one of the most common and deadliest malignancies worldwide. According to the Global Cancer Observatory (GCO) data for 2020, it ranks third globally in terms of incidence, with an estimated 1,931,590 new cases, and second in terms of mortality, causing 935,173 deaths [1]. CRC disease burden is generally higher in high-income industrialized countries [1], clearly suggesting the importance of lifestyle factors in its etiology.
The role of diet in the pathogenesis of CRC is now established, yet uncertainty remains about some specific foods and food classes. In the latest (2018) report of the World Cancer Research Fund (WCRF) on diet, nutrition, physical activity, and CRC [2], the Expert Panel concluded there was strong evidence that red and processed meat, alcoholic drinks, and body fatness increase CRC risk, while whole grains, foods containing dietary fiber, and dairy products have a protective effect. The evidence suggesting that fish consumption reduces CRC risk was judged as still limited, albeit generally consistent.
Fish is a key component of the Mediterranean diet, and its consumption is usually actively encouraged as it contains many high-quality proteins and essential micronutrients (vitamins and minerals) and fatty acids [3]. In particular, fish represents the main dietary source of long-chain ω-3 polyunsaturated fatty acids (ω-3 PUFA), among which are eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), which possess anti-inflammatory and immunomodulatory properties [4]. Studies in animal models have consistently suggested that fish oil (FO) containing ω-3 PUFA inhibits colorectal carcinogenesis through several pathways [5,6], and a recently published meta-analysis confirmed these findings among humans by highlighting an inverse relationship between ω-3 PUFA intake, blood levels, and CRC risk [7]. Epidemiological studies on the association between fish consumption and CRC risk in human populations did not always yield consistent results [8,9,10,11], and previous meta-analyses aggregating the available evidence from prospective investigations failed to reach conclusive results, highlighting the need for further research [12].
Recently, findings from large population-based cohort studies have been published [13,14]; hence, conducting an updated meta-analysis seems appropriate and timely. Moreover, we believe that coupling the evidence from epidemiological studies with that from preclinical studies may greatly help to jointly evaluate the robustness and plausibility of the hypothesis under study. Therefore, we conducted an up-to-date meta-analysis of prospective studies on the association between fish consumption and CRC risk among humans and a review of the available evidence on the link between the intake of fish and fish components and colorectal carcinogenesis in animal models.
2. Materials and Methods
2.1. Fish Consumption and Colorectal Cancer Risk among Humans
2.1.1. Literature Search and Inclusion Criteria
The literature search and statistical analysis were conducted according to the MOOSE guidelines for the meta-analyses of observational studies [15] and the protocol was registered in the Prospective Register of Systematic Reviews (PROSPERO CRD42022299629). On 23 November 2020, we searched PUBMED/MEDLINE and EMBASE using the following search string: (fish OR seafood* OR shellfish) AND (colon OR rectal OR rectum OR colorectal) AND (cancer OR carcinoma OR tumour OR tumor OR malignancy). After removing duplicates, papers were initially screened based on their title and abstract; those that were considered as potentially of interest for the present meta-analysis were then obtained and read in full text to decide on their eligibility. Additional papers were searched by the backward citation chaining of eligible papers and previously published literature reviews and meta-analysis. Papers were eligible if they had a prospective study design (cohort, nested case-control studies (NCC), and randomized clinical trials (RCT)) and reported a measure of relative risk (RR) (e.g., hazard ratio or odds ratio), a corresponding 95% confidence intervals (CI), or a different measure of statistical uncertainty (e.g., standard errors, variance, or exact p-value) for the association between the consumption of fish and the risk of colon, rectal, or colorectal cancer. Retrospective case–control studies were not considered, as well as ecological studies, case reports, editorials/letters that did not present original data, and studies with any design in which the outcome of interest was cancer mortality instead of cancer risk. In the case of non-independent studies (with total overlap, e.g., two or more reports from the same cohort, or with partial overlap, e.g., one study reporting from a cohort consortium and a different study presenting results for a cohort that is part of it), the older/smaller study was discarded unless it provided RR estimates that were not available in a more recent/larger study. Two researchers independently decided on the inclusion of each paper and any disagreement was resolved by consensus.
As illustrated in more detail below (see Results), the type of food studied in relation to CRC risk varied across articles in that it could be limited to fish (sometimes left unspecified) or encompass a varying combination of fish and other seafoods including crustaceans and mollusks/shellfish. For the sake of brevity, the generic term “fish” will be used henceforth to refer to the area of interest.
2.1.2. Data Extraction and Statistical Analysis
The following information was extracted from all eligible papers: first author and year of publication; country in which the study was conducted; study design; source; sex and age distribution of the whole study population and number of cancer cases (for cohort studies and RCT), or of cancer cases and controls (for NCC); details of matching, if any, for NCC; methods for data collection on food consumption; mean/median and maximum duration of follow-up and total number of person–years accrued; distribution of cancer cases by site (colon further split into proximal and distal colon, rectum, or other, and overlapping sites); adjusted (whenever available) or unadjusted RRs and their 95% CI, alongside the number of cases and non-cases/controls and the total number of person–years in each category of exposure (e.g., each quantile of fish consumption); details on the statistical methods and the variables used for adjustment.
RR estimates and corresponding 95% confidence intervals were transformed into log relative risk (logRR) and corresponding variance as proposed by Greenland [16]. We then conducted highest versus lowest and linear and non-linear dose–response random effects meta-analyses to summarize the evidence on the association between fish consumption and CRC risk. For linear dose–response meta-analysis, we followed the method described by Greenland and Longnecker [17] to compute a trend from RRs and 95% CI calculated across categories (e.g., quantiles) of exposure, when this was not directly provided in the paper. The non-linear dose–response meta-analysis was conducted using 3-knots restricted cubic splines (5th, 50th, and 95th percentiles of the distribution). Between studies, the heterogeneity of RR estimates was quantified using the I2 statistics, which is a measure of the total variation of effects across studies that can be attributed to actual heterogeneity rather than chance [18]. When I2 was above 50% (which denotes large heterogeneity) and the sample size allowed, we conducted subgroup analyses and fitted meta-regression models (for categorical and continuous variables, respectively) to determine what study characteristics could explain a significant share of the observed heterogeneity. Analyses stratified by sex, cancer site (colon vs. rectum), and country were, however, planned a priori and conducted regardless of whether or not there was substantial heterogeneity. Publication bias was assessed by visually inspecting the funnel plot and applying the Egger’s test [19]. Finally, the methodological quality and proneness to bias of all included studies was rated using the Newcastle–Ottawa Scale (NOS) [20].
Statistical analyses were conducted using Stata (version 14, command metan, for highest versus lowest meta-analysis) and R (version 4.0.0, command dosresmeta [21] for dose–response meta-analysis) software.
2.2. Fish and Fish-Oil Intake and Colorectal Carcinogenesis in Animal Models
The literature search for preclinical studies focusing on the relationship between the intake of fish, FO intake, and colon carcinogenesis in animal models was conducted in PUBMED/MEDLINE using the following search string: (chemoprevention OR omega3 OR “omega 3” OR omega-3 OR diet OR fish) AND (OR colon OR colorectal OR crc OR intestinal OR bowel) AND (cancer* OR carcinogenesis) AND (rodent* OR rat* OR mouse OR mice). The search was conducted on 3 May 2021, and it extends, therefore, to all the articles that were published until April 2021. To be included in the final review, an article needed to report original data and examine the effect of fish and/or fish oil intake in the process of colorectal carcinogenesis and metastasis in rodent models. The article selection was conducted according to the same procedures described above; no formal meta-analysis was conducted because of the great diversity across studies in terms of several characteristics (see Section 3).
3. Results
3.1. Fish Consumption and Colorectal Cancer Risk among Humans
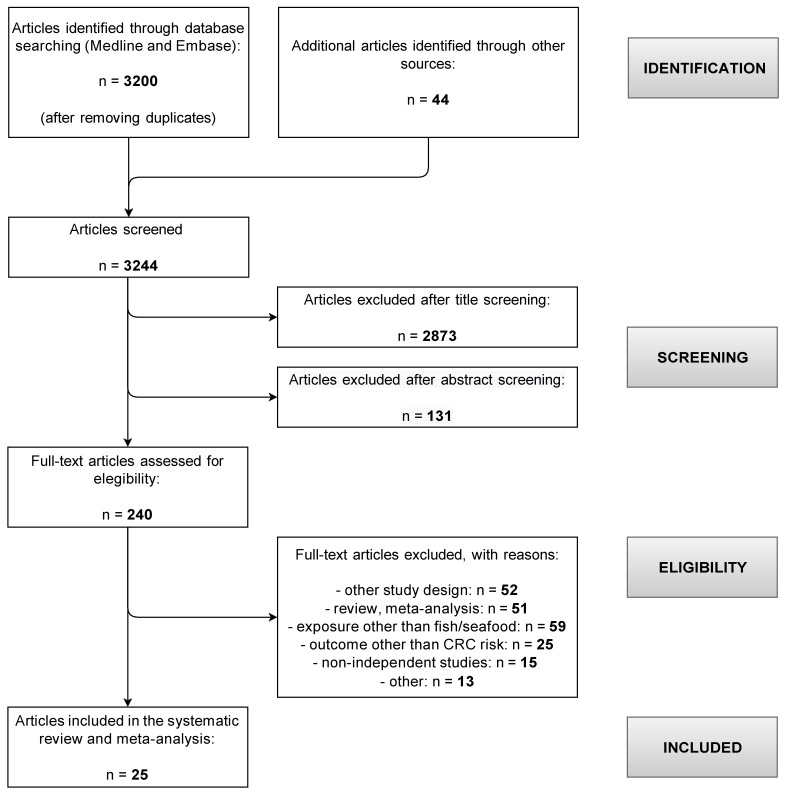
The literature search returned 3200 non-duplicate entries, and 44 were added via backward reference searching (Figure 1).
Figure 1.
Flow-chart for the selection of articles included in the systematic review and meta-analysis on the association between fish consumption and colorectal cancer risk.
A total of 2873 and 131 papers were screened out based on their titles and abstract, and the remaining 240 papers were read in full copy. Finally, 25 articles reporting on the association between fish consumption and CRC risk met the inclusion criteria for the present meta-analysis [8,9,10,11,13,14,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40] The papers by Bamia et al. [22] and Engeset et al. [23] were totally and partially overlapping, respectively, with the larger and more recent paper by Aglago et al. [13], which reported from the large, multi-country European Prospective Investigation into Cancer and Nutrition (EPIC) cohort study. Likewise, the two papers by Murff et al. [24] and Lee et al. [11] were based on the same prospective cohort (Shanghai Women’s Health Study). The study by Spencer et al. [25], a case–control study nested within a consortium of UK-based dietary cohorts including the EPIC-Norfolk and the EPIC-Oxford cohorts, had only a limited overlap with that by Aglago et al. [13], to which the two English cohorts contributed around 15.5% of the total size. Since the overlap between the two papers was limited, and in order not to discard valuable information, both papers were included in the meta-analysis and treated as if they were completely independent.
The main characteristics of included papers are summarized in Table 1.
Table 1.
Main characteristics of articles included in the systematic review and meta-analysis on the association between fish consumption and colorectal cancer risk.
| First Author, Year | Country | Study Name | Study Size (a) | Men (%) | Age Range (at Cohort Inception) | Study Length | Follow-Up Time (Years) | Fish Consumption Assessment (b) | No. Cases | Anatomic Site Distribution of Colorectal Cancers | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Colon | Rectal | Ns or Other | ||||||||||
| Aglago, 2020 [13] (c) | Europe | European Prospective Investigation into Cancer and Nutrition (EPIC) | 476,160 | 29.9% | 25–70 | 1992–ns | median 14.9 | intake + frequency | 6291 | 66.7% | 33.3% | 0.0% |
| Bradbury, 2020 [14] | UK | UK biobank study | 475,581 | 46.0% | 40–69 | 2006–2014 | mean 5.7 | intake + frequency | 2609 | 66.8% | 33.2% | 0.0% |
| Kantor, 2014 [26] | USA | VITamins And Lifestyle cohort | 68,109 | 49.0% | 50–70 | 2001–2008 | mean 6.7 | frequency | 488 | 63.7% | 26.3% | 10.0% |
| Song, 2014 [27] | USA | Nurses’ Health Study | 76,386 | 0.0% | 30–55 | 1976–2010 | mean 14.8 | intake | 1469 | 76.9% | 21.1% | 2.0% |
| Health Professionals Follow-up Study | 47,143 | 100.0% | 40–75 | 1986–2010 | 987 | 65.2% | 21.8% | 13.0% | ||||
| Bamia, 2013 [22] (c) | Europe | European Prospective Investigation into Cancer and Nutrition | 480,308 | 30.0% | 25–70 | 1992–2010 | mean 11.6 | intake | 4355 | 63.2% | 36.8% | 0.0% |
| Daniel, 2011 [28] | USA | National Institutes of Health (NIH)-AARP Diet and Health Study | 492,186 | 59.6% | 50–71 | 1995–2006 | mean 9.1 | intake | 7143 | 71.3% | 26.4% | 2.3% |
| Spencer, 2010 [25] | UK | UK Dietary Cohort Consortium | 2575 | 45.9% | ns | 1985–2006 | ns | intake | 579 | ns | ns | 100.0% |
| Murff, 2009 [24] (d) | China | Shanghai Women’s Health Study | 73,243 | 0.0% | 40–70 | 1996–2007 | ns | intake | 396 | ns | ns | 100.0% |
| Lee, 2009 [11] (d) | China | Shanghai Women’s Health Study | 74,942 | 0.0% | 45–65 | 1997–2005 | mean 7.4 | intake | 394 | 59.9% | 40.1% | 0.0% |
| Sugawara, 2009 [29] | Japan | Ohsaki National Health Insurance Cohort Study | 39,498 | 47.7% | 40–79 | 1995–2003 | mean 7.7 | intake | 566 | 59.5% | 40.5% | 0.0% |
| Butler, 2008 [30] | Singapore | Singapore Chinese Health Study | 61,321 | ns | 45–74 | 1993–ns | mean 9.8 | intake | 961 | 61.5% | 38.5% | 0.0% |
| Hall, 2008 [10] | USA | Physicians’ Health Study | 21,406 | 100.0% | ns | 1982–2006 | ns | frequency | 500 | 77.6% | 22.4% | 0.0% |
| Engeset, 2007 [23] (c) | Norway | The Norwegian Women and Cancer | 64,168 | 0.0% | 40–71 | 1991–2004 | ns | intake | 254 | ns | ns | 100.0% |
| Siezen, 2006 [31] | The Netherlands | Monitoring Project on Cardiovascular Disease Risk Factors + Diagnostisch Onderzoek Mammacarcinoom | 160 | ns | ns | 1976–2003 | ns | frequency | 160 | ns | ns | 100.0% |
| Brink, 2005 [32] | The Netherlands | The Netherlands Cohort Study | 2948 | 48.4% | 55–69 | 1986–1993 | mean 5.0 | intake | 608 | 73.7% | 26.3% | 0.0% |
| Larsson, 2005 [33] | Sweden | The Swedish Mammography Cohort | 61,433 | 0.0% | 40–75 | 1987–2003 | mean 13.9 | frequency | 733 | 53.1% | 31.4% | 15.5% |
| English, 2004 [34] | Australia | The Melbourne Collaborative Cohort Study | 37,112 | 39.5% | 27–75 | 1990–2003 | mean 9.0 | frequency | 451 | 62.5% | 37.3% | 0.2% |
| Kobayashi, 2004 [9] | Japan | The Japan Public Health Center-based prospective study | 116,194 | 49.3% | 40–69 | 1990–1999 | ns | intake | 705 | ns | ns | 100.0% |
| Lin, 2004 [35] | USA | Women’s Health Study | 37,547 | 0.0% | 45–ns | 1993–2003 | mean 8.7 | frequency | 202 | 80.2% | 19.8% | 0.0% |
| Tiemersma, 2002 [36] | The Netherlands | Monitoring Project on Cardiovascular Disease Risk Factors | 102 | 54.9% | 20–59 | 1987–1998 | mean 8.5 | frequency | 102 | 61.8% | ns | ns |
| Knekt, 1999 [37] | Finland | Cohort assembled within the Mobile Health Clinic of the Social Insurance Institution | 9985 | 52.8% | 15–99 | 1967–1990 | ns | intake | 189 | 38.6% | ns | 61.4% |
| Pietinen, 1999 [38] | Finland | The Alpha-Tocopherol, Beta-Carotene Cancer Prevention Study | 27,111 | 100.0% | 50–69 | 1985–1995 | mean 8.0 | intake | 185 | ns | ns | ns |
| Kato, 1997 [8] | USA | New York University Women’s Health Study | 14,727 | 0.0% | 34–65 | 1985–1994 | mean 7.1 | frequency | 100 | 84.0% | 16.0% | 0.0% |
| Gaard, 1996 [39] | Norway | Cohort assembled within the Norwegian National Health Screening Service | 50,535 | 50.1% | 20–54 | 1977–ns | mean 11.4 | frequency | 143 | 100.0% | 0.0% | 0.0% |
| Bostick, 1994 [40] | USA | Iowa Women’s Health Study | 35,216 | 0.0% | 55–69 | 1986–1990 | mean 4.8 | frequency | 212 | 100.0% | 0.0% | 0.0% |
(a) Cohort size or (for nested case–control studies) number of CRC cases. (b) Food intake was ex-pressed in g/day except in Daniel et al. 2001 (g/1000 kcal/day). Frequency was expressed as times, servings, or meals per week or month depending on the study. (c) Bamia et al. [22] was based on a shorter follow-up of the EPIC study than in Aglago et al. [13]. Engeset et al. [23] was based on one of the country-specific EPIC cohorts. From the studies by Bamia et al. and Engeset et al. we con-sidered only the results not available in Aglago et al. (d) The results from Murff et al. [24] were used only when they were not available in Lee et al. [11], which was based on the same cohort.
The papers were published between 1994 and 2020 and reported on studies conducted in Europe (n = 12), the USA (n = 7), Asia (n = 5), and Australia (n = 1). In terms of design, all were prospective cohort studies, except for Spencer et al. [25], Siezen et al. [31], and Tiemersma et al. [36], which were nested case–control studies, and Pietinen et al., whose study population consisted of subjects previously enrolled in a randomized controlled trial testing the effect of alpha-tocopherol and beta-carotene supplementation on lung cancer risk among male smokers [38]. The 25 studies included 2,228,377 individuals altogether, aged between 15 and 99 years at cohort inception, among which a total of 25,777 CRC cases were diagnosed during an average follow-up that varied between 4.8 and 14.9 across the studies. Seven and two studies included only women and men, respectively; the proportion of women ranged between 40.3% and 70.1% in the remaining sixteen papers. The breakdown of CRC cases into subsites was fully specified in seventeen studies; the studies by Gaard et al. and Bostick et al. included only colon cancer cases [39,40]. Information on food consumption was collected using food-frequency questionnaires in all studies except in Spencer et al. where 4-to-7-day diet diaries were used [25]. All included studies were of fair to very good quality, with the scores (assigned according to the NOS tool) ranging from the maximum allowed of 9 (for nine articles) to a minimum of 6 (for two articles) (Table S1).
The studies varied widely both in the way the exposure of interest was defined (e.g., (total) fish, fish and shellfish, (fish and) seafoods, etc.) and in the availability of risk estimates for specific subtypes of fish (e.g., fatty vs. lean, oily vs. non-oily, marine vs. fresh water, etc.) (Table S2). Dietary consumptions were reported by using as a unit of measure either the daily intake (mostly g/day) or the frequency of consumption (e.g., times or servings per week or month) (Table 1).
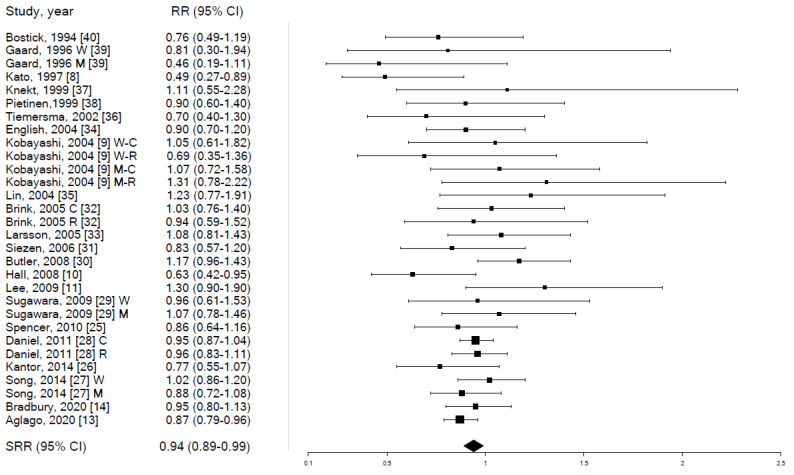
In meta-analysis, individuals in the highest (vs. lowest) category of fish consumption had a mild yet statistically significant reduction in CRC risk (SRR 0.94, 95% CI 0.89–0.99, p-value 0.023), based on data from 22 independent studies, with negligible heterogeneity (I2 = 11.7%) and no evidence of publication bias (Egger’s test p-value = 0.955) (Table 2 and Table S3 and Figure 2).
Table 2.
Meta-analysis of studies for the association between fish consumption (highest vs. lowest category of consumption) and colorectal cancer risk, overall and stratified by tumor site and sex.
| N Studies | SRR | Lower 95% CI | Upper 95% CI | p-Value | I2 | |
|---|---|---|---|---|---|---|
| Colorectal cancer | 22 | 0.94 | 0.89 | 0.99 | 0.023 | 11.7% |
| women | 13 | 0.95 | 0.87 | 1.05 | 0.310 | 13.9% |
| men | 10 | 0.91 | 0.82 | 1.01 | 0.088 | 27.2% |
| Colon cancer | 15 | 0.94 | 0.88 | 1.01 | 0.089 | 12.9% |
| women | 7 | 1.02 | 0.88 | 1.19 | 0.763 | 12.5% |
| men | 4 | 1.02 | 0.85 | 1.22 | 0.866 | 0.0% |
| Rectal cancer | 13 | 0.94 | 0.87 | 1.03 | 0.173 | 0.0% |
| women | 5 | 0.99 | 0.79 | 1.26 | 0.966 | 0.0% |
| men | 3 | 0.90 | 0.57 | 1.43 | 0.663 | 63.2% |
SRR: summary relative risk. CI: confidence intervals.
Figure 2.
Forest plot for the association between fish consumption (highest vs. lowest category of consumption) and colorectal cancer risk. RR: relative risk. SRR: summary relative risk. CI: confidence intervals. W: RR among women. M: RR among men. C: RR for colon cancer. R: RR for rectal cancer.
A comparable (in direction and strength) association emerged in stratified analyses (expect sex-stratified SRR for colon cancer risk, which was 1.02 among both women and men) but statistical significance was not achieved because of the lower number of available risk estimates (Table 2). In detail, the reduction in CRC risk for those in the highest category of fish consumption was slightly more evident among men (SRR 0.91) than women (SRR 0.95), while not differing by cancer site (SRR 0.94 for both colon and rectum) (Tables S4–S11) (Figures S1–S8). The association differed significantly (p-value 0.007) by country, as the SRR was 0.91 (95% CI 0.82–1.00) for studies conducted in North America, (n = 7), 0.90 (95% CI 0.84–0.97) for studies conducted in Europe (n = 10), and 1.12 (95% CI 0.98–1.27) in Asian studies (n = 4).
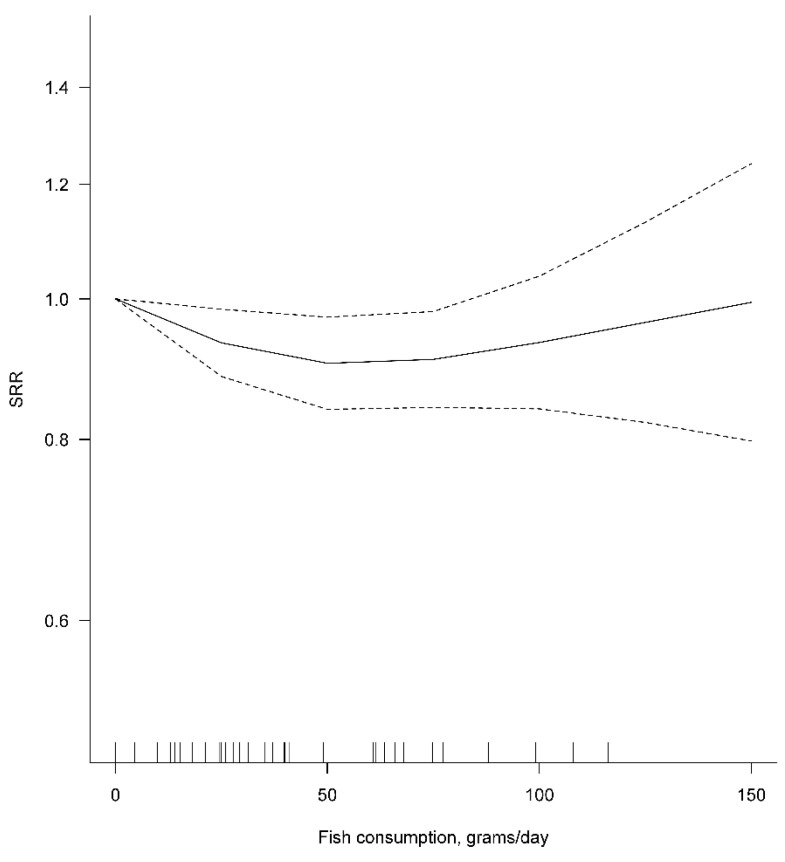
In dose–response meta-analysis, a 50-g increment in the daily consumption of fish was associated with a statistically significant 4% reduction in CRC risk (SRR 0.96, 95% CI 0.92–0.99, p-value 0.021), based on data from seven independent studies, with no evidence of heterogeneity between studies (I2 = 0.0%) (Table 3).
Table 3.
Dose–response meta-analysis of studies for the association between fish consumption (linear increment by 50 g/day) and colorectal cancer risk, overall and stratified by tumor site and sex.
| N Studies | SRR (for an Increase by 50 g/day) | Lower 95% CI | Upper 95% CI | p-Value | I2 | p-Value for Non-Linearity | |
|---|---|---|---|---|---|---|---|
| Colorectal cancer | 7 | 0.96 | 0.92 | 0.99 | 0.021 | 0.0% | 0.071 |
| women | 5 | 0.95 | 0.90 | 1.01 | 0.078 | 0.0% | 0.880 |
| men | 6 | 0.97 | 0.92 | 1.02 | 0.188 | 0.0% | 0.280 |
| Colon cancer | 6 | 0.96 | 0.92 | 1.01 | 0.140 | 0.0% | 0.991 |
| Rectal cancer | 6 | 0.95 | 0.89 | 1.02 | 0.174 | 0.0% | 0.248 |
SRR: summary relative risk. CI: confidence intervals.
Results were similar in analyses stratified by sex or cancer site (Table 3). The results of the dose–response meta-analysis were heavily influenced by the single study of Aglago et al. [13], whose percentage study weight was 66.5% in the main analysis and ranged between 59.5% and 73.4% in stratified analysis. The p-value for deviation from linearity of the dose–response association was nearly significant (0.071) only for the main analysis. The visual inspection of the graph obtained by fitting a non-linear dose–response meta-analysis revealed that the decrease in CRC risk was observed only for the daily consumption of fish increasing up to 50 g/day and appeared to level off (albeit confidence intervals became increasingly wide because of limited data availability) above this value (Figure 3).
Figure 3.
Non-linear dose–response meta-analysis for the association between fish consumption (g/day) and colorectal cancer risk. SRR: summary relative risk.
3.2. Fish and Fish-Oil Intake and Colorectal Carcinogenesis in Animal Models
The literature search resulted in 281 entries altogether: upon removing duplicates and checking inclusion criteria, a total of 25 articles were finally included in the review. The majority of preclinical experiments with rodents dealt with the effects of FO or pure ω-3 polyunsaturated fatty acids (PUFA) on colorectal carcinogenesis, while only a few studies were conducted by administering fish meat to the animals.
In 1986, Reddy and Maruyama, using an experimental model in which colorectal carcinogenesis was chemically induced (with 1,2-dimethylhydrazine (DMH) or its metabolite azoxymethane (AOM)), first documented in rats that a diet containing FO as a source of fat (Menhaden oil) reduces colon tumorigenesis when compared with a diet containing the same amount of fat as corn oil (CO) which is rich in ω-6 PUFA [41] (Table 4 and Table S11).
Table 4.
Effects of fish or its components on different animal models of colorectal cancer.
| Experimental Model | Dietary Intervention and Duration of Treatment | Effects on Carcinogenesis | Reference |
|---|---|---|---|
| AOM-induced rats | Diets containing Menhaden or Corn oils | Reduction in CRC in rats fed Menhaden Oil. | Reddy, 1986 [41] |
| -+AOM-induced rats | Different levels of FO or CO in the diet. | Reduction in CRC in rats fed high FO. | Reddy, 1988 [42] |
| AOM-induced rats | Diets containing EPA or LA | Reduction in colon carcinogenesis in the EPA group. | Minoura, 1988 [43] |
| AOM-induced mice | Commercial preparations of FO or CO. | Reduction in dysplastic areas and carcinogenesis in the FO group. | Deschner, 1990 [44] |
| AOM-induced rats | Diets containing FO and/or CO. | Reduction in colon carcinogenesis in rats fed high FO. | Reddy, 1991 [45] |
| DMH-induced rats | DHA (0.7 mL by gavage) 5 times a wk. | Reduction in ACF. | Takahashi, 1993 [46] |
| AOM-induced rats | DHA (0.7 mL of by gavage) twice a wk. | Slight non-significant reduction of CRC. | Takahashi, 1994 [47] |
| Significant reduction in ACF. | |||
| AOM-induced rats | DHA (1 mL by gavage) 5 times a wk. | Significant reduction in ACF and in CRC. | Takahashi, 1997a [48] |
| 2-amino-1-methyl-6-phenylimidazo [4,5-b]pyridine (PhIP)-induced rats | DHA (1 mL by gavage) 5 times a wk. | Reduction in ACF. | Takahashi, 1997b [49] |
| AOM-induced rats | Diet supplemented with FO or CO; cellulose or pectin also tested. | FO reduced CRC. | Chang, 1998 [50] |
| AOM-induced rats | FO vs. HFML. | Reduction in carcinogenesis and ACF in rats fed FO. | Rao, 2001 [51] |
| Apc∆716 mice of both sexes | Diet with 3% DHA for 7 wks. | Reduction in SI polyps, only in female mice fed DHA. | Oshima, 1995 [52] |
| Min mice mutated in Apc | Diet containing a commercial FO preparation. | Reduction in SI tumors in treated mice. | Paulsen, 1997 [53] |
| Min mice mutated in Apc | Diets containing EPA (1.5%) or different PUFA for 8 wks. | Reduction in SI tumors in the EPA group. | Petrik, 2000 [54] |
| Min mice mutated in Apc | EPA-FFA fed for 12 wks. | Reduction in polyp number in SI and colon. | Fini, 2011 [55] |
| Mice treated with AOM/DSS to induce CAC | EPA-FFA in the diet tested in the initiation and post-initiation phases. | Reduction in tumorigenesis | Piazzi, 2014 [56] |
| A/J Min/+ mice of both sexes | Salmon compared with beef or chicken muscles fed from weaning for 10 wks. | Salmon muscle decreased tumor load and size in the SI. | Steppler, 2017 [57] |
| Mice treated with AOM-DSS to induce CAC | Tuna muscle extract rich in Selenoeine fed for 14 wks. | Reduction in carcinogenesis. | Masuda, 2018 [58] |
The same authors found that diets containing high levels of FO and low levels of CO were associated with fewer AOM-induced colon cancers compared with diets containing only CO [42]. Later investigations confirmed that Menhaden oil is effective in reducing both the initiation and post-initiation stages of carcinogenesis when compared to ω-6 PUFA-rich CO [44,45]. Studies were conducted in parallel in which pure ω-3 PUFA was administered instead of not-purified FO. Minoura et al. found that rats fed with eicosapentaenoic acid (EPA) had lower colon carcinogenesis and lower prostaglandin E2 (PGE2) levels than rats on a linoleic acid (LA) diet [43]. Takahashi et al. reported fewer DMH-induced microscopic preneoplastic lesions (aberrant crypt foci (ACF)) and protection against AOM-induced carcinogenesis among rats fed with pure docosahexaenoic acid (DHA) [46,47,48,49]. Subsequent studies confirmed the role of FO in preventing AOM-induced colon carcinogenesis through enhanced cell differentiation and apoptosis [50], particularly when compared to diets containing a mixture of lipids simulating the Western diet (lipids derived from saturated fats, peanut and corn oils) [51] and suggested that the effect could be mediated via reduced cyclooxygenase-2 (COX-2) activity and prostaglandin production.
A beneficial effect of DHA was also observed in genetic models of intestinal carcinogenesis (Apc∆716 mice) [52] (Table 4 and Table S11). Likewise, an ω-3 PUFA ethyl ester-enriched fish oil concentrate was shown to oppose tumor growth in the small intestine (but not in the colon) in Apc-Min mice [53], and subsequent studies suggested that the protective effect could be mediated via antagonism with the production of arachidonic acid (a precursor of eicosanoids such as PGE2) [54]. More recently, highly purified EPA as free fatty acid (EPA-FFA) was observed to reduce COX-2 expression and cell proliferation and, eventually, prevent intestinal carcinogenesis in Apc-Min mice [55]. The potential of EPA-FFA in preventing colon carcinogenesis was later confirmed in a preclinical model mimicking CRC arising in the setting of inflammatory bowel disease (colitis-associated colorectal cancer (CAC)) [56].
Regarding colon cancer metastasis, Menhaden oil, in 1989, was first shown to be able to suppress the growth of a transplanted colon cancer cell line (CT-26 cells) and inhibit pulmonary colonization [59] (Table 5 and Table S13).
Table 5.
Effects of fish or its components on different animal models of colorectal cancer metastasis.
| Experimental Model | Dietary Intervention and Duration of Treatment | Effects on Colon Cancer and Metastasis | Reference |
|---|---|---|---|
| Mice inoculated with CT-26 tumor cells | Diets containing fish or safflower oils fed for 30 days before and after CT-26 transplantation. | Fish oil (FO) reduced tumor growth and pulmonary colonization. | Cannizzo, 1989 [59] |
| Mice s.c. implanted with Co 26 Lu tumor cells | Diets containing EPA and DHA during and after cancer cell transplantation. | Inhibition of tumor growth and decrease in lung metastatic nodules. | Iigo, 1997 [60] |
| Mice s.c. implanted with Co 26 Lu tumor cells | Diets containing EPA, DHA, LA, or oleic acid (OA) from day 5 for a total of 3 wks after cell implantation. | EPA, DHA, and OA reduced metastasis. Tumor cells treated with DHA showed a very low potential for lung colony formation when injected i.v. | Suzuki, 1997 [61] |
| Rats inoculated with ACL-15 tumor cells | Diets containing EPA, LA, or PA. ACL-15 tumor cells inoculated at 6 wks and rats sacrificed at 9 wks. | EPA reduced metastatic foci in liver. EPA and PA diet groups had smaller liver metastatic foci. |
Iwamoto,1998 [62] |
| Rats injected (via portal vein) with CC531 tumor cells | Diets containing FO or safflower oil for 3 wks before CC531 inoculation until sacrifice after 1 or 3 wks. | FO increased metastasis (number and size) at 1 wk after implantation; both FO and the safflower oil diets increased metastasis 3 wks after implantation. | Griffini, 1998 [63] |
| Rats injected (into the spleen) with CC531 tumor cells | Diets containing PUFA or coconut oil in the diet 3 days before and 28 days after CC 531 injection. | Reduction in tumor growth in the PUFA group. | Gutt, 2007 [64] |
| Mice injected (into the spleen) with MC-26 tumor cells | Diet containing EPA-FFA. Feeding 2 wks before and after cell injection. | EPA-FFA administration caused a reduced MC-26 liver tumor burden. | Hawcroft, 2012 [65] |
Similar results were seen in mice transplanted with a highly metastatic murine colon carcinoma cell line (Co 26 Lu) and fed with EPA and DHA [60], which were also effective in decreasing the number of lung metastasis via reduced metalloproteinase-2 and -9 activity [61]. Furthermore, EPA was also reported to inhibit the formation of liver metastatic foci of previously injected ACL-15 rat colon cancer cells by decreasing tumor cell proliferation and adhesion to the capillary bed [62]. Despite initial findings documenting adverse effects [63], ω-3 PUFA were reported to be able to prevent the development of colon cancer metastases in the liver of Wag-Rij rats transplanted with an established colon cancer cell line [64]. Subsequent experiments using EPA-FFA in the diet reported largely consistent results [65] and identified, among the possible mechanisms of action, a shift from PGE2 to PGE3 in tumor cells, as well as a reduced ERK signaling at the invasive edge of tumors.
As already mentioned, only a few studies documented the effect of edible parts of fish on colon carcinogenesis (Table 4). The effect of salmon muscle was tested by Steppler et al. in A/J Min/+ mice, Apc mutated animals showing tumorigenesis not only in the small intestine but also in the colon [66]. Salmon-fed animals showed a slightly lower intestinal carcinogenesis when compared to a standard diet and to diets containing meat from terrestrial animals [57]. More recently, dietary supplementation with tuna muscle extract rich in selenoeine (an Se-protein with antioxidant activity present in the blood and muscle of tuna) was reported to decrease colon carcinogenesis in a colitis-associated model of CRC in mice [58].
4. Discussion
We conducted an up-to-date meta-analysis aiming to summarize the most recent available evidence about the association between fish consumption and CRC risk among humans. Twenty-five studies were included that encompassed a total of over 25,000 CRC cases arising from over 2.2 million individuals. The most important finding was the mild yet statistically significant reduction in CRC risk for individuals in the highest (vs. lowest) category of fish consumption, a finding that was made particularly trustworthy by the fair consistency of risk estimates across the studies and by the lack of evidence of publication bias. Analyses stratified by subsite showed that the effect was similar for colon and rectal cancer, the lower number of available studies for subsite-specific analyses being, therefore, the most likely explanation for the failure to achieve full statistical significance. Analyses stratified by sex also yielded comparable results to the main analysis in terms of both the direction and strength of the association, while geographical variability existed, whereby significant results emerged only in studies conducted in Europe and North America. The latter finding may partly be due to chance (only four of the included studies were conducted in Asia), but geographical diversity in terms of the genetic background and cooking methods of populations may also play a role; therefore, more research on the topic would be desirable to disentangle the importance of the different factors potentially at play. Finally, while based on only seven independent studies, the dose–response analysis showed a 4% decrease in CRC risk associated with a 50-g daily increase in fish consumption.
We then carried out a review of preclinical studies that reported on the link between the intake of fish and fish oil and colon carcinogenesis in animal models. While the diversity across the studies in terms of experimental methods advised against applying a formal meta-analytical approach to summarize the results, the reviewed studies were fairly consistent in suggesting a beneficial effect of fish- and fish oil-based diets against colorectal carcinogenesis and dissemination in rodents and identified several biological mechanisms potentially able to underlie this effect.
The preventive effect of fish consumption on CRC risk observed in epidemiological studies can recognize several possible explanations. Partly, the association may be attributable to a replacement effect since those who eat more fish generally eat less red meat, whose causal link with colorectal carcinogenesis is well-known. Additionally, preferring fish instead of meat may be part of a generally healthier lifestyle encompassing other habits effective in preventing cancer [67,68]. However, prospective epidemiological studies are fairly consistent in detecting a reduction in CRC risk associated with fish consumption, which is, therefore, difficult to dismiss as mostly due to bias. In this regard, preclinical studies using animal models have been instrumental in helping to understanding the process of colorectal carcinogenesis and to give insights on how this may be affected by intrinsic and external factors such as diet, thus, providing support to the evidence stemming from epidemiological studies. Among animal models, both chemically-induced carcinogenesis and genetic models (the latter, mostly based on Apc mutations in mice and rats [69]) have been used to test the effect of dietary treatments, which are typically administered to the animals after the chemical induction of tumorigenesis or, in genetic models, starting from weaning. Depending on the duration of dietary treatment, either precursor lesions or straightforward tumors were used as a primary end-point of treatment efficacy. As stated before, the majority of animal experiments were carried out testing the effect of FO or its pure components (e.g., EPA and DHA) on colon carcinogenesis, while fish muscle consumption has not been thoroughly tested. This underlies the need to conduct studies in which animals are fed with fish, possibly using as a control group animals fed the same number of proteins and fat deriving from other animal muscles (i.e., beef or chicken) to resemble an actual human diet more closely. Notably, the majority of preclinical data documented a beneficial effect of FO and its pure compounds when compared with fats more common in the Western diet (like ω-6 or saturated fats), which emerged when focusing on CRC, its early phases (ACF or polyps), and even metastasis (although with some exceptions, e.g., Griffini et al.).
The reviewed studies highlighted some of the several biological mechanisms that may account for the protective effect of fish and FO against colorectal carcinogenesis. A detailed overview is beyond the scope of the present paper (interested readers may refer to existing reviews [5,6,70,71]), but some data deserve to be briefly described here. ω-3 PUFAs affect eicosanoids metabolism by inhibiting PGE2 production, EPA can function as a substrate for COXs to synthesize unique 3-series prostaglandin compounds (e.g., PGE3) less endowed with inflammatory action compared to 2-series prostaglandin compounds [72]. EPA and DHA produce lipid mediators endowed with pro-resolving, immunomodulatory, and anti-inflammatory properties (which may also explain their effect in preventing cardiovascular diseases) [6]. The molecular basis for the health benefits of ω-3 PUFA was also ascribed to the incorporation of these fatty acids into membrane phospholipids. Moreover, ω-3 PUFA do not enhance the luminal concentration of secondary bile acids (unlike saturated fats and ω-6 PUFA) and lower colon and liver activity of ornithine decarboxylase (ODC) and tyrosine-specific protein kinase (TPK), all of which are implicated in colon carcinogenesis [70]. Positive epigenetic effects have also been described together with interaction of ω-3 PUFA with nuclear receptors and transcription factors, thus, altering the proliferation, lipid metabolism, and apoptosis of cancer cells [5]. More recently, ω-3 PUFA was reported to be associated with higher intestinal microbial diversity, thus, improving host immune function and eventually halting the development of CRC [71,73].
ω-3 PUFA is also the nutrient contained in fish that was most extensively investigated in relation to CRC risk among humans, including in several prospective studies that mostly yielded results consistent with preclinical studies. In 2020, Kim et al. published a meta-analysis of twenty prospective studies which encompassed a total of 18,102 cases and over 1.3 million participants and found that ω-3 PUFA intake (from fish or FO supplements) was inversely associated with CRC risk [7]. In particular, linear increments by 0.1 g/day in the intake of EPA and DHA were associated with statistically significant 5% and 3% reductions, respectively, in CRC risk. Similar reviews for fish components other than ω-3 PUFA are warranted to reach a clearer understanding of the mechanisms underlying the observed protective effect of fish consumption against CRC risk. Like for every food, however, it is important to emphasize that the nutritional value of fish, and its association with human disease, is better evaluated on the basis of its consumption as a whole rather than as the effect of any single nutrient therein, both because the different nutrients may interact between one another in complex ways once they have entered the body, and because the food matrix affects how the food is digested and absorbed [3,74]. The finding of Kim et al.’s meta-analysis deserves attention, however, because it is consistent with data from animal models and confirms the role of ω-3 PUFA intake as an important (although not exclusive) mediator of the protective effect of fish consumption against CRC risk.
The main strength of this paper lies in our having reviewed the available evidence from both preclinical and epidemiological studies with the aim of giving as broad an overview as possible on the role of fish in the prevention of CRC and on the possible mechanisms underlying this effect. The meta-analysis of prospective human studies takes advantage of a very large size and of a remarkable consistency of results across time and space: the studies were conducted in the USA, Europe, Australia, and Asia, and participants were followed up from as early as 1967 until as late as 2014. Results from highest-versus-lowest and dose–response analyses were consistent, heterogeneity among studies was low-to-negligible, and there was no evidence of publication bias, which further contributed to the reliability of our findings. Articles included in the review of preclinical studies were published over a period of more than three decades (1986–2018): in spite of the inevitable differences in study methods, the data were considerably consistent and provided valuable support to those originating from epidemiological studies, as well as many insights into underlying causal mechanisms. Our work also has some weaknesses that are important to acknowledge. A few papers may have been missed for having limited the search to only two databases (PUBMED/MEDLINE and EMBASE): however, the meticulous citation chaining of the papers included, the previously published reviews, the meta-analysis, and the lack of evidence for publication bias in meta-analysis suggest that the number of missed papers is unlikely to be high and their impact on the summary results minimal. Regarding the epidemiological studies, we merged results from studies that varied in terms of how the exposure of interest (“fish”) was defined (crustaceans and shellfish were included only in some studies, and a clear definition was sometimes missing) and measured (g/day or frequency of consumption). Moreover, the categories of fish consumption used to conduct the highest-versus-lowest analysis differed across studies, which is, however, usual in meta-analysis in the field of nutritional epidemiology. Furthermore, only a limited subset of studies (7 out of 25) contributed to the dose–response meta-analysis and summary results were heavily affected by a single study [13] which contributed around two-thirds of the statistical power of that analysis. Our meta-analysis does not suggest that any major disparity by sex exists in the association between fish consumption and CRC risk; however, only around half of the studies provided separate risk estimates for men and women, which may have curbed our ability to detect small differences in the strength of the association. With regard to studies on animal models, in addition to the aforementioned very large variability in study design, materials and methods, and to the use of fish meat (instead of fish oil) in only a very limited subset of studies, an important limitation is the fact that some of the potential biological mechanisms (e.g., modification of COX-2 activity, prostaglandins production, and others) were investigated in only a few studies; therefore, confirmation is needed to corroborate and extend current knowledge.
5. Conclusions
In conclusion, by jointly reviewing epidemiological studies among human populations and preclinical studies in animal models we found evidence that increasing fish consumption may effectively help inhibit colorectal carcinogenesis. CRC is a disease characterized by high incidence and mortality rates worldwide, so even a moderate reduction in its risk at the individual level (such as that achievable by increasing the consumption of fish, according to our findings) may lead to a major reduction in its disease burden at the population level. The consistent evidence from epidemiological and preclinical studies that fish consumption may be effective in preventing CRC should be taken into account when making dietary recommendations for cancer prevention.
Abbreviations
ACF: Aberrant Crypt Foci. AOM: Azoxymethane. AOM/DSS: Azoxymethane/Dextran Sodium Sulfate. APC: Adenomatous Polyposis Coli. CAC: Colitis-Associated Colorectal cancer. CI: Confidence Intervals. CO: Corn Oil. COX-2: Cyclossigenase-2. CRC: Colorectal Cancer. DHA: Docosahexaenoic Acid. DMH: 1,2-Dimethylhydrazine. EPA: Eicosapentaenoic acid. EPA-FFA: Eicosapentaenoic Acid as Free Fatty Acid. EPIC: European Prospective Investigation into Cancer and Nutrition. ERK: Extracellular Signal-Regulated Kinase. FFA: Free Fatty Acid. FO: Fish Oil. GCO: Global Cancer Observatory. HFML: High-Fat diet containing Mixed Lipids. LA: Linoleic Acid. LogRR: Log Relative Risk. MOOSE: Guidelines for Meta-Analyses and Systematic Reviews of Observational Studies. NCC: Nested Case–Control studies. NOS: Newcastle–Ottawa Scale. OA: Oleic Acid. ODC: Ornithine Decarboxylase. PA: Palmitic Acid. PGE2: Prostaglandin E2. PGE3: Prostaglandin E3. PhIP: 2-amino-1-methyl-6-phenylimidazo [4,5-b]pyridine. PUFA (ω-3): Long chain ω-3 Polyunsturated Fatty Acids. RCT: Randomized Clinical Trials. RR: Relative Risk. SI: Small Intestine. SRR: Summary Risk Ratio. TPK: Tyrosine-specific Protein Kinase. WCRF: World Cancer Research Fund.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cancers14030640/s1, Figure S1: Forest plot for the association between fish consumption (highest vs. lowest category of consumption) and colorectal cancer risk among women; Figure S2: Forest plot for the association between fish consumption (highest vs. lowest category of consumption) and colorectal cancer risk among men; Figure S3: Forest plot for the association between fish consumption (highest vs. lowest category of consumption) and colon cancer risk; Figure S4: Forest plot for the association between fish consumption (highest vs. lowest category of consumption) and colon cancer risk among women; Figure S5: Forest plot for the association between fish consumption (highest vs. lowest category of consumption) and colon cancer risk among men; Figure S6: Forest plot for the association between fish consumption (highest vs. lowest category of consumption) and rectal cancer risk; Figure S7: Forest plot for the association between fish consumption (highest vs. lowest category of consumption) and rectal cancer risk among women; Figure S8: Forest plot for the association between fish consumption (highest vs. lowest category of consumption) and rectal cancer risk among men; Table S1: Quality assessment (using the Newcastle–Ottawa Scale tool) of the articles included in the meta-analysis; Table S2: Exact definition (as reported in the paper text) of the exposures that were studied in relation to colorectal, colon, or rectal cancer risk in each included study. Risk estimates entered in meta-analysis models were those marked with the asterisk (*); Table S3: Studies and corresponding relative risk estimates included in the meta-analysis of the association between fish consumption (highest vs. lowest category of consumption) and colorectal cancer risk; Table S4: Studies and corresponding relative risk estimates included in the meta-analysis of the association between fish consumption (highest vs. lowest category of consumption) and colon cancer risk; Table S5: Studies and corresponding relative risk estimates included in the meta-analysis of the association between fish consumption (highest vs. lowest category of consumption) and rectal cancer risk; Table S6: Studies and corresponding relative risk estimates included in the meta-analysis of the association between fish consumption (highest vs. lowest category of consumption) and colorectal cancer risk among women; Table S7: Studies and corresponding relative risk estimates included in the meta-analysis of the association between fish consumption (highest vs. lowest category of consumption) and colon cancer risk among women; Table S8: Studies and corresponding relative risk estimates included in the meta-analysis of the association between fish consumption (highest vs. lowest category of consumption) and rectal cancer risk among women; Table S9: Studies and corresponding relative risk estimates included in the meta-analysis of the association between fish consumption (highest vs. lowest category of consumption) and colorectal cancer risk among men; Table S10: Studies and corresponding relative risk estimates included in the meta-analysis of the association between fish consumption (highest vs. lowest category of consumption) and colon cancer risk among men; Table S11: Studies and corresponding relative risk estimates included in the meta-analysis of the association between fish consumption (highest vs. lowest category of consumption) and rectal cancer risk among men; Table S12: Experiments with fish and its components on animal models of colorectal cancer; Table S13: Experiments with fish or its components on different animal models of colorectal cancer metastasis.
Author Contributions
Conceptualization, S.C. (Saverio Caini), G.C. and G.M.; methodology, S.C. (Saverio Caini), S.C. (Sofia Chioccioli) and G.C.; software, S.C. (Saverio Caini); validation, E.P., M.F. and K.T.; formal analysis, S.C. (Saverio Caini); investigation, all authors; resources, G.C. and G.M.; data curation, S.C. (Saverio Caini), S.C. (Sofia Chioccioli), E.P., M.F. and K.T.; writing—original draft preparation, S.C. (Saverio Caini), S.C. (Sofia Chioccioli), E.P., M.F. and K.T.; writing—review and editing, G.C. and G.M.; visualization, S.C. (Saverio Caini); supervision, S.C. (Saverio Caini), G.C. and G.M.; project administration, G.C. and G.M.; funding acquisition, not applicable. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Global Cancer Observatory (GCO) Colorectal Cancer Factsheet 2020. [(accessed on 31 August 2021)]. Available online: https://gco.iarc.fr/today/data/factsheets/cancers/10_8_9-Colorectum-fact-sheet.pdf.
- 2.World Cancer Research Fund/American Institute for Cancer Research Diet, Nutrition, Physical Activity, and Cancer: A Global Perspective. Continuous Update Project (CUP): Colorectal Cancer. [(accessed on 31 August 2021)]. Available online: https://www.wcrf.org/dietandcancer/colorectal-cancer/
- 3.Institute of Food Research, Norwich, UK Nutrient Analysis of Fish and Fish Products. [(accessed on 13 October 2021)];2013 Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/167923/Nutrient_analysis_of_fish_and_fish_products_-_Analytical_Report.pdf.
- 4.Saedisomeolia A., Wood L.G., Garg M.L., Gibson P.G., Wark P.A. Anti-inflammatory effects of long-chain n-3 PUFA in rhinovirus-infected cultured airway epithelial cells. Br. J. Nutr. 2009;101:533–540. doi: 10.1017/S0007114508025798. [DOI] [PubMed] [Google Scholar]
- 5.Hou T.Y., Davidson L.A., Kim E., Fan Y.Y., Fuentes N.R., Triff K., Chapkin R.S. Nutrient-Gene Interaction in Colon Cancer, from the Membrane to Cellular Physiology. Annu. Rev. Nutr. 2016;36:543–570. doi: 10.1146/annurev-nutr-071715-051039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Irún P., Lanas A., Piazuelo E. Omega-3 Polyunsaturated Fatty Acids and Their Bioactive Metabolites in Gastrointestinal Malignancies Related to Unresolved Inflammation. A Review. Front. Pharmacol. 2019;10:852. doi: 10.3389/fphar.2019.00852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim Y., Kim J. Intake or Blood Levels of n-3 Polyunsaturated Fatty Acids and Risk of Colorectal Cancer: A Systematic Review and Meta-analysis of Prospective Studies. Cancer Epidemiol. Biomark. Prev. 2020;29:288–299. doi: 10.1158/1055-9965.EPI-19-0931. [DOI] [PubMed] [Google Scholar]
- 8.Kato I., Akhmedkhanov A., Koenig K., Toniolo P.G., Shore R.E., Riboli E. Prospective study of diet and female colorectal cancer: The New York University Women’s Health Study. Nutr. Cancer. 1997;28:276–281. doi: 10.1080/01635589709514588. [DOI] [PubMed] [Google Scholar]
- 9.Kobayashi M., Tsubono Y., Otani T., Hanaoka T., Sobue T., Tsugane S., JPHC Study Group Fish, long-chain n-3 polyunsaturated fatty acids, and risk of colorectal cancer in middle-aged Japanese: The JPHC study. Nutr. Cancer. 2004;49:32–40. doi: 10.1207/s15327914nc4901_5. [DOI] [PubMed] [Google Scholar]
- 10.Hall M.N., Chavarro J.E., Lee I.M., Willett W.C., Ma J. A 22-year prospective study of fish, n-3 fatty acid intake, and colorectal cancer risk in men. Cancer Epidemiol. Biomark. Prev. 2008;17:1136–1143. doi: 10.1158/1055-9965.EPI-07-2803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee S.A., Shu X.O., Yang G., Li H., Gao Y.T., Zheng W. Animal origin foods and colorectal cancer risk: A report from the Shanghai Women’s Health Study. Nutr. Cancer. 2009;61:194–205. doi: 10.1080/01635580802419780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vieira A.R., Abar L., Chan D.S.M., Vingeliene S., Polemiti E., Stevens C., Greenwood D., Norat T. Foods and beverages and colorectal cancer risk: A systematic review and meta-analysis of cohort studies, an update of the evidence of the WCRF-AICR Continuous Update Project. Ann. Oncol. 2017;28:1788–1802. doi: 10.1093/annonc/mdx171. [DOI] [PubMed] [Google Scholar]
- 13.Aglago E.K., Huybrechts I., Murphy N., Casagrande C., Nicolas G., Pischon T., Fedirko V., Severi G., Boutron-Ruault M.C., Fournier A., et al. Consumption of fish and long-chain n-3 polyunsaturated fatty acids is associated with reduced risk of colorectal cancer in a large European cohort. Clin. Gastroenterol. Hepatol. 2020;18:654–666.e6. doi: 10.1016/j.cgh.2019.06.031. [DOI] [PubMed] [Google Scholar]
- 14.Bradbury K.E., Murphy N., Key T.J. Diet and colorectal cancer in UK Biobank: A prospective study. Int. J. Epidemiol. 2020;49:246–258. doi: 10.1093/ije/dyz064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stroup D.F., Berlin J.A., Morton S.C., Olkin I., Williamson G.D., Rennie D., Moher D., Becker B.J., Sipe T.A., Thacker S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 16.Greenland S. Quantitative methods in the review of epidemiologic literature. Epidemiol. Rev. 1987;9:1–30. doi: 10.1093/oxfordjournals.epirev.a036298. [DOI] [PubMed] [Google Scholar]
- 17.Greenland S., Longnecker M.P. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am. J. Epidemiol. 1992;135:1301–1309. doi: 10.1093/oxfordjournals.aje.a116237. [DOI] [PubMed] [Google Scholar]
- 18.Higgins J.P., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 19.Egger M., Davey Smith G., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analysis. 2020. [(accessed on 2 July 2021)]. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 21.The Comprehensive R Archive Network (CRAN) Package Dosresmeta. [(accessed on 9 June 2021)]. Available online: https://cran.r-project.org/web/packages/dosresmeta/dosresmeta.pdf.
- 22.Bamia C., Lagiou P., Buckland G., Grioni S., Agnoli C., Taylor A.J., Dahm C.C., Overvad K., Olsen A., Tjønneland A., et al. Mediterranean diet and colorectal cancer risk: Results from a European cohort. Eur. J. Epidemiol. 2013;28:317–328. doi: 10.1007/s10654-013-9795-x. [DOI] [PubMed] [Google Scholar]
- 23.Engeset D., Andersen V., Hjartåker A., Lund E. Consumption of fish and risk of colon cancer in the Norwegian Women and Cancer (NOWAC) study. Br. J. Nutr. 2007;98:576–582. doi: 10.1017/S0007114507721487. [DOI] [PubMed] [Google Scholar]
- 24.Murff H.J., Shu X.O., Li H., Dai Q., Kallianpur A., Yang G., Cai H., Wen W., Gao Y.T., Zheng W. A prospective study of dietary polyunsaturated fatty acids and colorectal cancer risk in Chinese women. Cancer Epidemiol. Biomark. Prev. 2009;18:2283–2291. doi: 10.1158/1055-9965.EPI-08-1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spencer E.A., Key T.J., Appleby P.N., Dahm C.C., Keogh R.H., Fentiman I.S., Akbaraly T., Brunner E.J., Burley V., Cade J.E., et al. Meat, poultry and fish and risk of colorectal cancer: Pooled analysis of data from the UK dietary cohort consortium. Cancer Causes Control. 2010;21:1417–1425. doi: 10.1007/s10552-010-9569-7. [DOI] [PubMed] [Google Scholar]
- 26.Kantor E.D., Lampe J.W., Peters U., Vaughan T.L., White E. Long-chain omega-3 polyunsaturated fatty acid intake and risk of colorectal cancer. Nutr. Cancer. 2014;66:716–727. doi: 10.1080/01635581.2013.804101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Song M., Chan A.T., Fuchs C.S., Ogino S., Hu F.B., Mozaffarian D., Ma J., Willett W.C., Giovannucci E.L., Wu K. Dietary intake of fish, ω-3 and ω-6 fatty acids and risk of colorectal cancer: A prospective study in U.S. men and women. Int. J. Cancer. 2014;135:2413–2423. doi: 10.1002/ijc.28878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Daniel C.R., Cross A.J., Graubard B.I., Hollenbeck A.R., Park Y., Sinha R. Prospective investigation of poultry and fish intake in relation to cancer risk. Cancer Prev. Res. 2011;4:1903–1911. doi: 10.1158/1940-6207.CAPR-11-0241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sugawara Y., Kuriyama S., Kakizaki M., Nagai M., Ohmori-Matsuda K., Sone T., Hozawa A., Nishino Y., Tsuji I. Fish consumption and the risk of colorectal cancer: The Ohsaki Cohort Study. Br. J. Cancer. 2009;101:849–854. doi: 10.1038/sj.bjc.6605217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Butler L.M., Wang R., Koh W.P., Yu M.C. Prospective study of dietary patterns and colorectal cancer among Singapore Chinese. Br. J. Cancer. 2008;99:1511–1516. doi: 10.1038/sj.bjc.6604678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Siezen C.L., Bueno-de-Mesquita H.B., Peeters P.H., Kram N.R., van Doeselaar M., van Kranen H.J. Polymorphisms in the genes involved in the arachidonic acid-pathway, fish consumption and the risk of colorectal cancer. Int. J. Cancer. 2006;119:297–303. doi: 10.1002/ijc.21858. [DOI] [PubMed] [Google Scholar]
- 32.Brink M., Weijenberg M.P., de Goeij A.F., Roemen G.M., Lentjes M.H., de Bruïne A.P., Goldbohm R.A., van den Brandt P.A. Meat consumption and K-ras mutations in sporadic colon and rectal cancer in The Netherlands Cohort Study. Br. J. Cancer. 2005;92:1310–1320. doi: 10.1038/sj.bjc.6602491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Larsson S.C., Rafter J., Holmberg L., Bergkvist L., Wolk A. Red meat consumption and risk of cancers of the proximal colon, distal colon and rectum: The Swedish Mammography Cohort. Int. J. Cancer. 2005;113:829–834. doi: 10.1002/ijc.20658. [DOI] [PubMed] [Google Scholar]
- 34.English D.R., MacInnis R.J., Hodge A.M., Hopper J.L., Haydon A.M., Giles G.G. Red meat, chicken, and fish consumption and risk of colorectal cancer. Cancer Epidemiol. Biomark. Prev. 2004;13:1509–1514. [PubMed] [Google Scholar]
- 35.Lin J., Zhang S.M., Cook N.R., Lee I.M., Buring J.E. Dietary fat and fatty acids and risk of colorectal cancer in women. Am. J. Epidemiol. 2004;160:1011–1022. doi: 10.1093/aje/kwh319. [DOI] [PubMed] [Google Scholar]
- 36.Tiemersma E.W., Kampman E., Bueno de Mesquita H.B., Bunschoten A., van Schothorst E.M., Kok F.J., Kromhout D. Meat consumption, cigarette smoking, and genetic susceptibility in the etiology of colorectal cancer: Results from a Dutch prospective study. Cancer Causes Control. 2002;13:383–393. doi: 10.1023/A:1015236701054. [DOI] [PubMed] [Google Scholar]
- 37.Knekt P., Järvinen R., Dich J., Hakulinen T. Risk of colorectal and other gastro-intestinal cancers after exposure to nitrate, nitrite and N-nitroso compounds: A follow-up study. Int. J. Cancer. 1999;80:852–856. doi: 10.1002/(SICI)1097-0215(19990315)80:6<852::AID-IJC9>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 38.Pietinen P., Malila N., Virtanen M., Hartman T.J., Tangrea J.A., Albanes D., Virtamo J. Diet and risk of colorectal cancer in a cohort of Finnish men. Cancer Causes Control. 1999;10:387–396. doi: 10.1023/A:1008962219408. [DOI] [PubMed] [Google Scholar]
- 39.Gaard M., Tretli S., Løken E.B. Dietary factors and risk of colon cancer: A prospective study of 50,535 young Norwegian men and women. Eur. J. Cancer Prev. 1996;5:445–454. [PubMed] [Google Scholar]
- 40.Bostick R.M., Potter J.D., Kushi L.H., Sellers T.A., Steinmetz K.A., McKenzie D.R., Gapstur S.M., Folsom A.R. Sugar, meat, and fat intake, and non-dietary risk factors for colon cancer incidence in Iowa women (United States) Cancer Causes Control. 1994;5:38–52. doi: 10.1007/BF01830725. [DOI] [PubMed] [Google Scholar]
- 41.Reddy B.S., Maruyama H. Effect of dietary fish oil on azoxymethane-induced colon carcinogenesis in male F344 rats. Cancer Res. 1986;46:3367–3370. [PubMed] [Google Scholar]
- 42.Reddy B.S., Sugie S. Effect of different levels of omega-3 and omega-6 fatty acids on azoxymethane-induced colon carcinogenesis in F344 rats. Cancer Res. 1988;48:6642–6647. [PubMed] [Google Scholar]
- 43.Minoura T., Takata T., Sakaguchi M., Takada H., Yamamura M., Hioki K., Yamamoto M. Effect of dietary eicosapentaenoic acid on azoxymethane-induced colon carcinogenesis in rats. Cancer Res. 1988;48:4790–4794. [PubMed] [Google Scholar]
- 44.Deschner E.E., Lytle J.S., Wong G., Ruperto J.F., Newmark H.L. The effect of dietary omega-3 fatty acids (fish oil) on azoxymethanol-induced focal areas of dysplasia and colon tumor incidence. Cancer. 1990;66:2350–2356. doi: 10.1002/1097-0142(19901201)66:11<2350::AID-CNCR2820661117>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 45.Reddy B.S., Burill C., Rigotty J. Effect of diets high in omega-3 and omega-6 fatty acids on initiation and postinitiation stages of colon carcinogenesis. Cancer Res. 1991;51:487–491. [PubMed] [Google Scholar]
- 46.Takahashi M., Minamoto T., Yamashita N., Yazawa K., Sugimura T., Esumi H. Reduction in formation and growth of 1,2-dimethylhydrazine-induced aberrant crypt foci in rat colon by docosahexaenoic acid. Cancer Res. 1993;53:2786–2789. [PubMed] [Google Scholar]
- 47.Takahashi M., Minamoto T., Yamashita N., Kato T., Yazawa K., Esumi H. Effect of docosahexaenoic acid on azoxymethane-induced colon carcinogenesis in rats. Cancer Lett. 1994;83:177–184. doi: 10.1016/0304-3835(94)90316-6. [DOI] [PubMed] [Google Scholar]
- 48.Takahashi M., Fukutake M., Isoi T., Fukuda K., Sato H., Yazawa K., Sugimura T., Wakabayashi K. Suppression of azoxymethane-induced rat colon carcinoma development by a fish oil component, docosahexaenoic acid (DHA) Carcinogenesis. 1997;18:1337–1342. doi: 10.1093/carcin/18.7.1337. [DOI] [PubMed] [Google Scholar]
- 49.Takahashi M., Totsuka Y., Masuda M., Fukuda K., Oguri A., Yazawa K., Sugimura T., Wakabayashi K. Reduction in formation of 2-amino-1-methyl-6-phenylimidazo [4,5-b]pyridine (PhIP)-induced aberrant crypt foci in the rat colon by docosahexaenoic acid (DHA) Carcinogenesis. 1997;18:1937–1941. doi: 10.1093/carcin/18.10.1937. [DOI] [PubMed] [Google Scholar]
- 50.Chang W.L., Chapkin R.S., Lupton J.R. Fish oil blocks azoxymethane-induced rat colon tumorigenesis by increasing cell differentiation and apoptosis rather than decreasing cell proliferation. J. Nutr. 1998;128:491–497. doi: 10.1093/jn/128.3.491. [DOI] [PubMed] [Google Scholar]
- 51.Rao C.V., Hirose Y., Indranie C., Reddy B.S. Modulation of experimental colon tumorigenesis by types and amounts of dietary fatty acids. Cancer Res. 2001;61:1927–1933. [PubMed] [Google Scholar]
- 52.Oshima M., Takahashi M., Oshima H., Tsutsumi M., Yazawa K., Sugimura T., Nishimura S., Wakabayashi K., Taketo M.M. Effects of docosahexaenoic acid (DHA) on intestinal polyp development in Apc delta 716 knockout mice. Carcinogenesis. 1995;16:2605–2607. doi: 10.1093/carcin/16.11.2605. [DOI] [PubMed] [Google Scholar]
- 53.Paulsen J.E., Elvsaas I.K., Steffensen I.L., Alexander J. A fish oil derived concentrate enriched in eicosapentaenoic and docosahexaenoic acid as ethyl ester suppresses the formation and growth of intestinal polyps in the Min mouse. Carcinogenesis. 1997;18:1905–1910. doi: 10.1093/carcin/18.10.1905. [DOI] [PubMed] [Google Scholar]
- 54.Petrik M.B., McEntee M.F., Chiu C.H., Whelan J. Antagonism of arachidonic acid is linked to the antitumorigenic effect of dietary eicosapentaenoic acid in Apc(Min/+) mice. J. Nutr. 2000;130:1153–1158. doi: 10.1093/jn/130.5.1153. [DOI] [PubMed] [Google Scholar]
- 55.Fini L., Piazzi G., Daoud Y., Selgrad M., Maegawa S., Garcia M., Fogliano V., Romano M., Graziani G., Vitaglione P., et al. Chemoprevention of intestinal polyps in ApcMin/+ mice fed with western or balanced diets by drinking annurca apple polyphenol extract. Cancer Prev. Res. 2011;4:907–915. doi: 10.1158/1940-6207.CAPR-10-0359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Piazzi G., D’Argenio G., Prossomariti A., Lembo V., Mazzone G., Candela M., Biagi E., Brigidi P., Vitaglione P., Fogliano V., et al. Eicosapentaenoic acid free fatty acid prevents and suppresses colonic neoplasia in colitis-associated colorectal cancer acting on Notch signaling and gut microbiota. Int. J. Cancer. 2014;135:2004–2013. doi: 10.1002/ijc.28853. [DOI] [PubMed] [Google Scholar]
- 57.Steppeler C., Sødring M., Egelandsdal B., Kirkhus B., Oostindjer M., Alvseike O., Gangsei L.E., Hovland E.M., Pierre F., Paulsen J.E. Effects of dietary beef, pork, chicken and salmon on intestinal carcinogenesis in A/J Min/+ mice. PLoS ONE. 2017;12:e0176001. doi: 10.1371/journal.pone.0176001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Masuda J., Umemura C., Yokozawa M., Yamauchi K., Seko T., Yamashita M., Yamashita Y. Dietary Supplementation of Selenoneine-Containing Tuna Dark Muscle Extract Effectively Reduces Pathology of Experimental Colorectal Cancers in Mice. Nutrients. 2018;10:1380. doi: 10.3390/nu10101380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cannizzo F., Jr., Broitman S.A. Postpromotional effects of dietary marine or safflower oils on large bowel or pulmonary implants of CT-26 in mice. Cancer Res. 1989;49:4289–4294. [PubMed] [Google Scholar]
- 60.Iigo M., Nakagawa T., Ishikawa C., Iwahori Y., Asamoto M., Yazawa K., Araki E., Tsuda H. Inhibitory effects of docosahexaenoic acid on colon carcinoma 26 metastasis to the lung. Br. J. Cancer. 1997;75:650–655. doi: 10.1038/bjc.1997.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Suzuki I., Iigo M., Ishikawa C., Kuhara T., Asamoto M., Kunimoto T., Moore M.A., Yazawa K., Araki E., Tsuda H. Inhibitory effects of oleic and docosahexaenoic acids on lung metastasis by colon-carcinoma-26 cells are associated with reduced matrix metalloproteinase-2 and -9 activities. Int. J. Cancer. 1997;73:607–612. doi: 10.1002/(SICI)1097-0215(19971114)73:4<607::AID-IJC24>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 62.Iwamoto S., Senzaki H., Kiyozuka Y., Ogura E., Takada H., Hioki K., Tsubura A. Effects of fatty acids on liver metastasis of ACL-15 rat colon cancer cells. Nutr. Cancer. 1998;31:143–150. doi: 10.1080/01635589809514694. [DOI] [PubMed] [Google Scholar]
- 63.Griffini P., Fehres O., Klieverik L., Vogels I.M., Tigchelaar W., Smorenburg S.M., Van Noorden C.J. Dietary omega-3 polyunsaturated fatty acids promote colon carcinoma metastasis in rat liver. Cancer Res. 1998;58:3312–3319. [PubMed] [Google Scholar]
- 64.Gutt C.N., Brinkmann L., Mehrabi A., Fonouni H., Müller-Stich B.P., Vetter G., Stein J.M., Schemmer P., Büchler M.W. Dietary omega-3-polyunsaturated fatty acids prevent the development of metastases of colon carcinoma in rat liver. Eur. J. Nutr. 2007;46:279–285. doi: 10.1007/s00394-007-0662-y. [DOI] [PubMed] [Google Scholar]
- 65.Hawcroft G., Volpato M., Marston G., Ingram N., Perry S.L., Cockbain A.J., Race A.D., Munarini A., Belluzzi A., Loadman P.M., et al. The omega-3 polyunsaturated fatty acid eicosapentaenoic acid inhibits mouse MC-26 colorectal cancer cell liver metastasis via inhibition of PGE2-dependent cell motility. Br. J. Pharmacol. 2012;166:1724–1737. doi: 10.1111/j.1476-5381.2012.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sødring M., Gunnes G., Paulsen J.E. Spontaneous initiation, promotion and progression of colorectal cancer in the novel A/J Min/+ mouse. Int. J. Cancer. 2016;138:1936–1946. doi: 10.1002/ijc.29928. [DOI] [PubMed] [Google Scholar]
- 67.Wennberg M., Tornevi A., Johansson I., Hörnell A., Norberg M., Bergdahl I.A. Diet and lifestyle factors associated with fish consumption in men and women: A study of whether gender differences can result in gender-specific confounding. Nutr. J. 2012;11:101. doi: 10.1186/1475-2891-11-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tani S., Kawauchi K., Atsumi W., Matsuo R., Ashida T., Imatake K., Suzuki Y., Yagi T., Takahashi A., Matsumoto N., et al. Association among daily fish intake, white blood cell count, and healthy lifestyle behaviors in an apparently healthy Japanese population: Implication for the anti-atherosclerotic effect of fish consumption. Heart Vessels. 2021;36:924–933. doi: 10.1007/s00380-020-01769-9. [DOI] [PubMed] [Google Scholar]
- 69.Femia A.P., Caderni G. Rodent models of colon carcinogenesis for the study of chemopreventive activity of natural products. Planta Med. 2008;74:1602–1607. doi: 10.1055/s-2008-1074577. [DOI] [PubMed] [Google Scholar]
- 70.Reddy B.S. Studies with the azoxymethane-rat preclinical model for assessing colon tumor development and chemoprevention. Environ. Mol. Mutagen. 2004;44:26–35. doi: 10.1002/em.20026. [DOI] [PubMed] [Google Scholar]
- 71.Song M., Chan A.T. Environmental Factors, Gut Microbiota, and Colorectal Cancer Prevention. Clin. Gastroenterol. Hepatol. 2019;17:275–289. doi: 10.1016/j.cgh.2018.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yang P., Jiang Y., Fischer S.M. Prostaglandin E3 metabolism and cancer. Cancer Lett. 2014;348:1–11. doi: 10.1016/j.canlet.2014.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Piazzi G., Prossomariti A., Baldassarre M., Montagna C., Vitaglione P., Fogliano V., Biagi E., Candela M., Brigidi P., Balbi T., et al. A Mediterranean Diet Mix Has Chemopreventive effects in a murine model of colorectal cancer modulating apoptosis and the gut microbiota. Front. Oncol. 2019;9:140. doi: 10.3389/fonc.2019.00140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Thorning T.K., Bertram H.C., Bonjour J.P., de Groot L., Dupont D., Feeney E., Ipsen R., Lecerf J.M., Mackie A., McKinley M.C., et al. Whole dairy matrix or single nutrients in assessment of health effects: Current evidence and knowledge gaps. Am. J. Clin. Nutr. 2017;105:1033–1045. doi: 10.3945/ajcn.116.151548. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.