Abstract
Simple Summary
Hyperthermia (HT) is a promising therapeutic option for multiple cancer entities as it has the potential to increase the cytotoxicity of radiotherapy (RT) and chemotherapy (CT). Thermometric parameters of HT are considered to have potential as predictive factors of treatment response. So far, only limited data about the prognostic and predictive role of thermometric parameters are available. In this review, we investigate the existing clinical evidence regarding the correlation of thermometric parameters and cancer response in clinical studies in which patients were treated with HT in combination with RT and/or CT. Some studies show that thermometric parameters correlate with treatment response, indicating their potential significance for treatment guidance. Thus, the establishment of specific thermometric parameters might pave the way towards a better standardization of HT treatment protocols.
Abstract
Hyperthermia (HT) is a cancer treatment modality which targets malignant tissues by heating to 40–43 °C. In addition to its direct antitumor effects, HT potently sensitizes the tumor to radiotherapy (RT) and chemotherapy (CT), thereby enabling complete eradication of some tumor entities as shown in randomized clinical trials. Despite the proven efficacy of HT in combination with classic cancer treatments, there are limited international standards for the delivery of HT in the clinical setting. Consequently, there is a large variability in reported data on thermometric parameters, including the temperature obtained from multiple reference points, heating duration, thermal dose, time interval, and sequence between HT and other treatment modalities. Evidence from some clinical trials indicates that thermal dose, which correlates with heating time and temperature achieved, could be used as a predictive marker for treatment efficacy in future studies. Similarly, other thermometric parameters when chosen optimally are associated with increased antitumor efficacy. This review summarizes the existing clinical evidence for the prognostic and predictive role of the most important thermometric parameters to guide the combined treatment of RT and CT with HT. In conclusion, we call for the standardization of thermometric parameters and stress the importance for their validation in future prospective clinical studies.
Keywords: hyperthermia, thermometric parameters, preclinical data, clinical evidence
1. Introduction
Hyperthermia (HT) is a clinical treatment for cancer which extraneously and intrinsically heats malignant cells to a temperature of 40–43 °C for a suitable period of time [1,2]. Heat delivered to tumor tissues can act as a cytotoxic or sensitizing agent to enhance their remission or at least regression by utilizing several biological mechanisms and pleiotropic effects when combined with other conventional cancer treatment techniques, such as radiotherapy (RT) and/or chemotherapy (CT).
The biological effects of HT, which all favor its use in combination with RT and CT, include direct cytotoxicity, radiosensitization, chemosensitization, and immune modulation. HT-induced cell lethality is predominantly a result of conformational changes and the destabilization of macromolecule structures including the disruptions in cell metabolism, inhibition of DNA repair, and triggering of cellular apoptotic pathways [3,4,5,6]. The direct HT-induced cell lethality is known to be intrinsically tumor-selective for hypoxic cells [7]. During heating, enhanced blood perfusion in tumor tissues influences the radiosensitizing and chemosensitizing effects of HT by increasing the tumor oxygenation level and local concentration of CT drugs respectively [4,8,9]. Radiosensitization and chemosensitization effects, as well as the inhibition of DNA synthesis and repair, on the molecular level depend on the aggregation of proteins produced by HT-induced denaturation [10]. Moreover, protein unfolding and the intracellular accumulation of proteins trigger molecular chaperones including the heat shock proteins (HSPs) [11]. The release of HSPs and other “immune activating signals” underly the inflammatory and immunogenic responses to HT in combination with RT and/or CT and can promote anti-tumor immunity [12,13,14]. Exploiting molecular and physiological mechanisms evoked by HT can improve the efficacy of RT and CT. Therefore, HT in cancer treatment is used mainly within the framework of multimodal treatment strategies [3,8].
Multiple preclinical studies have been designed to unravel the relationship between biological mechanisms induced by HT and thermometric parameters as predictors of tumor response [15,16,17,18,19,20]. The parameters investigated in these studies include the temperature achieved during HT [6,15], heating duration, thermal dose [21], time interval between HT and the other treatment modality [15,22,23], the number of HT sessions [24], and the sequence of treatment modality [15,25,26]. All of these parameters were shown to influence the extent to which HT enhances the effect of RT or CT using cellular assays and in vivo models. In addition to thermometric parameters, the treatment parameters of RT and CT, such as total radiation dose, number of RT fractions, type of chemotherapeutic drug and the number of CT cycles, prescribed for a specific clinical indication, also play a significant role in attaining a therapeutic window with synergistic effects when combined with HT [25,27,28].
The effectiveness of HT combined with RT and/or CT has been investigated in many clinical studies with different tumor types. Unfortunately, to date, there is no consensus on HT delivery when combined with these cancer treatment modalities, resulting in substantial heterogeneity of the HT treatment protocols applied. Any comparison of these studies in terms of outcome should be made with caution in view of this heterogeneity in HT protocols. A good understanding of thermometric parameters and their interpretation is mandatory in this regard. However, there is inconclusive clinical evidence about the relationship of thermometric parameters with both tumor and normal tissue responses to HT in combination with RT and/or CT. The reason for this is that thermometric parameters are inconsistently reported or analyzed in prospective clinical studies and the retrospective analyses are conflicting. For instance, minimum tumor temperature was identified as a prognostic factor in a few studies [29,30,31]. However, another study showed that different metrics such as temperature achieved in 90% (T90), 50% (T50), and 10% (T10) in the target volume were more strongly correlated with cancer response than minimum achieved temperature [32]. Furthermore, a short time interval between HT and RT was shown to significantly predict treatment outcome in retrospective analyses of cervical cancer patients [22]. However, conflicting results have been also reported [33] which may be attributed to differences in time interval and tumor temperature achieved, and in patient population [34]. Thermal dose has been successfully tested in several clinical trials as a predictor of tumor response to combined RT and HT treatment [35,36,37,38,39,40,41,42]. These did not result in established thresholds for thermal dose for treating different cancer sites, even though European Society for Hyperthermic Oncology (ESHO) guidelines recommend superficial HT maintains T50 ≥ 41 °C and T90 ≥ 40 °C [43]. The concept of a relationship between thermometric parameters with treatment outcome is highly attractive because it could improve the understanding of tumor-specific mechanisms of interaction between HT and RT and/or CT. Defining thermometric parameters is therefore important for a meaningful clinical evaluation of HT treatment outcomes when combined with RT and/or CT.
A limited amount of clinical information is available about the effect of thermometric parameters on treatment response. Increasing awareness of the importance of such parameters on the efficacy of HT combined with other cancer treatments is important, and thus these parameters should be evaluated and reported routinely. Achieving the defined thermometric parameters during HT treatment would further increase the effectiveness of biological mechanisms when combined with RT and/or CT. Future prospective clinical studies should include description of all relevant thermometric parameters to pave the way towards the proper analysis and standardization of thermometric parameters for each clinical indication treated with HT in combination with RT and/or CT.
This work summarizes the evidence underlying thermometric parameters as predictors of treatment outcomes as reported in clinical studies using HT in combination with RT and/or CT for treating different cancer types and emphasizes the need for reference thermometric parameters to improve HT efficacy. For completeness, the findings pertaining to thermometric parameters from preclinical studies are also discussed, to provide comprehensive information about their significance and underlying mechanisms.
2. Materials and Methods
2.1. Data Sources and Search Strategies
The literature search included databases of clinicaltrials.gov and pubmed.ncbi.nlm.nih.gov from March to September 2021 and randomized prospective and retrospective clinical studies with specific criteria were identified. The search terms were hyperthermia, cancer treatment, randomized clinical studies, prospective clinical studies, and retrospective clinical studies. Those terms were used mainly to search for the title and abstract. We also found articles which were recommended, suggested, or sent to us on the internet. Additionally, we handsearched the reference lists of the most relevant clinical studies and review articles.
2.2. Inclusion and Exclusion Criteria of Clinical Studies
This non-systematic review included randomized, prospective, and retrospective clinical studies that recruited patients with cancer who were treated with HT and RT and/or CT. The data from randomized trials are only from the patient group which received HT in combination with either RT and/or CT. Data from the non-HT arm were not extracted.
The main inclusion criteria was the use of either electromagnetic, radiative, or capacitive HT systems, independent of cancer type. Another criterion was more than 10 patients recruited in prospective and retrospective studies. Retrospective studies were only included if analysis of thermometric parameters for HT in combination with RT had been performed.
Clinical studies which used the thermal ablation technique, interstitial-based/modulated electro HT techniques, interstitial RT techniques, high intensity focused ultrasound (HIFU) HT, whole body HT, and studies in pediatric patients were not included in this review. Pilot and feasibility studies were also excluded.
2.3. Data Extraction and List of Variables Included
The data extracted from the clinical studies contained the following information:
First author of the study
Study design: prospective or retrospective
RT treatment data: total dose, number of fractionations
CT treatment data: drug and concentration prescribed, number of cycles
Thermometric parameters
Reported clinical endpoints
Reported relationship between thermometric parameters and clinical endpoint
2.4. A Summary of HT Techniques
The clinical studies included in this review administered HT using externally applied power with electromagnetic–based techniques, such as radiofrequency, microwave, or infrared. These techniques differ with regard to their application to treat superficial or deep-seated tumors, as summarized elsewhere [44].
For superficial tumors, the electromagnetic radiative and capacitive systems are the those used in the clinical trials included in this review. The superficial HT techniques and their application are explained in detail elsewhere [43]. The radiative and capacitive systems differ in the way they are applied in the clinic. A study showed that for superficial cancers, the radiative HT system performs better than capacitive systems in terms of temperature distribution [45]. The commercially available radiative superficial systems are the BSD-500 device (Pyrexar Medical, Salt Lake, UT, USA), the ALBA ON4000 (Alba Hyperthermia, Rome, Italy) and contact flexible microwave applicators (SRPC Istok, Fryazino, Moscow region, Russia). Thermotron RF8 (Yamamoto Vinita Co, Osaka, Japan), Oncotherm (Oncotherm Kft., Budapest, Hungary) and Celsius TCS (Celsius42 GmbH, Cologne, Germany) are examples of commercial capacitive systems used for superficial tumors.
Different HT techniques with unique specifications, characteristics, and limitations are used to treat deep-seated tumors [46]. The ESHO guidelines provide information as to how and when a specific particular HT device should be used to treat deep-seated tumors [46,47]. The radiative HT systems for deep-seated tumors used in clinical trials are the BSD-2000 device (Pyrexar Medical, Salt Lake, UT, USA), the ALBA 4D (Alba Hyperthermia, Rome, Italy), and the Synergo RITE (Medical Enterprises Europe B.V., Amstelveen, The Netherlands), and capacitive systems are Oncotherm (Oncotherm Kft., Budapest, Hungary), Celsius TCS (Celsius 42 GmbH, Cologne, Germany), and Thermotron RF8 (Yamamoto Vinita Co, Osaka, Japan). Another simulation study showed a difference in heating patterns between radiative and capacitive HT for deep-seated tumors [48]. The radiative technique yields more favorable simulated temperature distributions for deep-seated tumors than the capacitive technique.
2.5. Definition of Thermometric Parameters
In this work, the thermometric parameters were extracted from the selected perspective and retrospective clinical studies. The definitions of these parameters are listed in Table 1.
Table 1.
Definition of thermometric parameters.
| Thermometric Parameters |
Definitions |
|---|---|
| Heating Temperature | |
| Tmin | Minimum temperature achieved in target volume (°C). |
| Tmax | Maximum temperature achieved in target volume (°C). |
| Tavg | Average temperature achieved in target volume (°C). |
| T10 | Temperature achieved in 10% of the target volume (°C). |
| T20 | Temperature achieved in 20% of the target volume (°C). |
| T50 | Temperature achieved in 50% of the target volume (°C). |
| T80 | Temperature achieved in 80% of the target volume (°C). |
| T90 | Temperature achieved in 90% of the target volume (°C). |
| Heating duration | |
| tpre | Warm-up period is the time required to achieve the desired treatment temperature and therapeutic time (min). |
| ttreat | Treatment period is the time during which a constant temperature in the tumor (≥41 °C) is maintained (min). |
| Thermal Dose | |
| CEM43°CT90 | Cumulative equivalent minutes at 43 °C when the measured temperature is T90 (min). |
| CEM43°CT50 | Cumulative equivalent minutes at 43 °C when the measured temperature is T50 (min). |
| CEM43°CT10 | Cumulative equivalent minutes at 43 °C when the measured temperature is T10 (min). |
| TRISE | T50 values above 37 °C multiplied by the duration of all heating sessions normalized to a duration of 450 min (°C) [36]. |
| AUC | Actual time-temperature plots by computing the area under the curve (AUC) for T > 37 °C and T ≥ 39 °C (°C-min) [49]. |
| HT sessions | |
| Nweek | Number of HT sessions per week. |
| Ntotal | Total number of HT sessions during the treatment course. |
| Time interval | |
| tint | The time interval between HT and RT and/or CT. |
| Sequencing | The scheduling order of HT with RT and/or CT. |
Temperature measurements in the target volume or surrounding tissue are crucial for assessing treatment quality and are represented by temperature metrics. During a HT session, the temperature is usually monitored and recorded using high resistance thermistor probes, fiber optic temperature probes or thermocouples by invasively placing the probes in the target volume or in the vicinity of the target volume [43,46,50]. The ESHO guidelines recommend that after the definition of the tumor volume as a planning target volume, a target point should be defined where the probe is positioned intraluminally or intratumorally [46]. In addition, the guidelines strongly suggest keeping a record of thermometry measurement points within or close to the tumor sites [43]. After completion of the HT session, recorded temperature data during ttreat are evaluated by computing temperature metrics. For instance, Tmax is calculated as the maximum temperature value recorded in the target volume (Table 1). T10, another maximum temperature metric, is computed as the temperature value received by 10% of the target volume [32]. Similarly, the other temperature metrics listed in Table 1 are computed. In current practice, the thermometric parameters and thermal dose are computed by software integrated in the HT systems or using thermal analysis tools such as RHyThM [51].
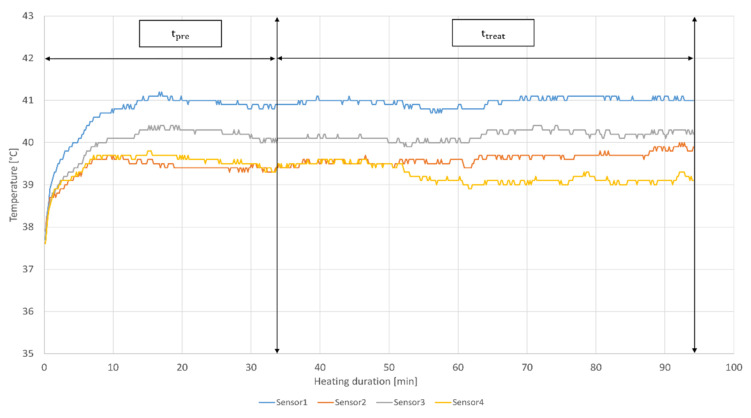
To illustrate how temperature, tpre and ttreat terms are measured in clinical practice, Figure 1 shows the temperature and heating duration parameters of a patient treated with HT in the radiation oncology center at Cantonal Hospital Aarau (KSA) using BSD-500 system (BSD Medical Corporation, Salt Lake City, UT, USA).
Figure 1.
Recorded treatment data of a single HT session for a breast cancer patient. Temperature in °C and heating duration in minutes are measured non-invasively using four sensors located in close proximity to the tumor tissue. tpre and ttreat of 33 and 60 min respectively according to the KSA clinical protocol are indicated.
The temperature metrics and thermal doses can be also computed by using the data from Figure 1. A decade ago, a new thermal dose entitled “TRISE” was proposed by Franckena et al. [36]. However, this parameter has not yet been evaluated in experimental studies. Another newly proposed thermal dose parameter is the area under the curve (AUC) [49]. In contrast to CEM43°C and TRISE, AUC is computed without any prior assumptions by summating AUC for the entire treatment session, including tpre and ttreat. Similarly to TRISE, AUC has not yet been investigated in preclinical studies. Another parameter related to HT used in this review is thermal enhancement ratio (TER), defined as ‘the ratio between RT dose required to achieve a specific endpoint and RT dose to achieve the same endpoint in combination with HT’ [52].
3. Evidence for Predictive Values of Thermometric Parameters in Preclinical Studies
3.1. Heating Temperature
The responsiveness of a tumor to HT is determined by different heat-induced mechanisms at the cellular level. The oxygenation rate is affected by temperature, as a higher rate was reported at 41–41.5 °C in comparison to higher temperature (at 43 °C) in rodent tumors, human tumor xenografts, canine, and human tumors [53]. Heating at 40 °C potentiated the cytotoxicity of CT drugs in human maxillary carcinoma cells [28], and the cytotoxicity was further increased on heating to 43.5–44 °C [54]. In contrast, another preclinical study showed no such dependency at 41–43.5 °C [55]. An in vitro study showed that apoptosis in human keratinocytes occurred at temperatures of 39 °C and above [56]. However, the majority of studies show synergistic actions of HT with RT and CT at temperatures above 41 °C [5,57], leading to the inhibition of DNA repair and chromosomal aberrations, induction of DNA breaks by RT and CT, and protein damage as an underlying molecular event of heat treatment [5,58,59]. To benefit from additive and synergistic effects of HT when combined with RT and/or CT, uniform temperature in the target volume should be delivered during the whole treatment course.
The temperature metrics are used to present the heating temperature achieved during treatment, not only in the target volume, which encompasses the tumor, but also for adjacent healthy tissue. T90, T80, T50, T20, and T10 are considered to be less sensitive than Tmin, Tavg and Tmax, due to the number and arbitrary positioning of sensors in the tissue. Such temperature metrics can be used to understand the response to heat of various cancer types for a specific duration and, at the same time, the heat-induced effects on surrounding normal tissues. However, except for Tmin and Tmax, most descriptive metrics of temperature have no specific reference values yet (Table 2).
Table 2.
Reference temperature metrics.
| Temperature Metrics | Reference Value (°C) |
|---|---|
| Tmin | 39 |
| Tmax | 44 |
| Tavg | Undefined |
| T10 | Undefined |
| T20 | Undefined |
| T50 | ≥41 * |
| T80 | Undefined |
| T90 | ≥40 * |
* According to ESHO guidelines for superficial HT [43].
T50 and T90 reference values are defined according to ESHO guidelines for treatment with superficial HT, but not for the deep HT technique. No reference values for temperature metrics are based on experimental data (Table 2), even though temperature distributions can be better controlled in preclinical than in clinical studies. In an in vivo study, no temperature variations were observed in tumors as they were recorded intratumorally [15]. Temperature at a reference value with minor variations (±0.05 °C) was reported in a vitro study [60]. In contrast, the temperature data recorded in patients are limited for various reasons. For example, thermistor probes inserted in deep-seated tumors in patients have the potential to cause complications or sometimes are impractical to insert intraluminally or intratumorally [61]. The value of the lowest temperature achieved during HT treatment is shown to have a prognostic role in describing the biological effects of HT. According to an in vivo study, T90 was a predictive parameter of reoxygenation and radiosensitization effects [62]. An in vitro experiment which investigated the difference in thermal sensitivity between hypoxic and oxic cells demonstrated that direct cytotoxicity induced by HT is more selective to the hypoxic cells [7]. Thus, temperatures required to achieve comparable thermal enhancement effect of HT vary depending on tissue type and characteristics.
3.2. Heating Duration
Temperature fluctuations, such as a decrease by 0.5 °C, have been shown to have a strong effect on the extent of cell kill, which was compensated by doubling the heating duration [6,63]. Therapeutic ratio, defined as the ratio of thermosensitive liposomal doxorubicin delivered to the heated tumor increased from 1.9-fold with 10 min heating to 4.4-fold with 40 min heating [64]. In an in vivo study, TER for mouse mammary adenocarcinoma (C3H) increased with respect to heating exposure longer than 30 min at 41.5 °C [15]. A study used mouse leukemia, human cervical carcinoma (HeLa), and Chinese hamster ovary (CHO) cells to demonstrate that the time required to kill 90% of the cells at 43 °C varied according to type [65]. The survival data from different tissues were analyzed using the Arrhenius equation to understand the effect of ttreat for different cell types [66]. These analyses showed that the reference ttreat value is set at 60 min when heating constantly at reference temperature (Table 3).
Table 3.
Reference heating duration parameters for HT.
| Heating Duration Parameters | Reference Value (min) |
| tpre | undefined |
| ttreat | 60 1 |
1 According to the Arrhenius plot [66].
Heating for longer than 60 min is restricted by thermotolerance, which was observed after 20 min while heating at 43.5 °C [67]. In addition, the surviving fraction of asynchronous CHO cells heated to 41.5 °C was decreased with increasing ttreat, until the thermotolerance effect appeared [21]. Thermotolerance is activated by different forms of stress including heat exposure for a specific time [68], which depends on the temperature and the amount of HT damage induced [69]. In an experimental study, the effect of thermotolerance was observed using the human tumor cell line (HTB-66) and CHO cells after 4 h of heating at 42.5 °C and 3 h of heating at either 42.5 or 43 °C [70]. The degree of thermotolerance is determined by cell type, heating temperature, and time of heating including the interval between successive heat treatments [71].
3.3. Thermal Dose
The relationship between temperature and ttreat was demonstrated experimentally in two preclinical studies, which showed that the same thermal enhancement of ionizing radiation in cells lines was achieved by heating for 7–11 min at 45 °C or for 120 min at 42 °C [26,72]. It was also shown that different survival rates were obtained when heating asynchronous CHO cells to different temperatures for varying ttreat [66]. These preclinical data showed that heating temperature and ttreat influence thermal damage. The relationship of temperature and ttreat to the biological effects induced by HT is described using the Arrhenius equation, which models the relationship of the inactivation rate in a biological system [21]. This led to the discovery that the relationship between temperature and ttreat depends on the activation energy required to induce a particular HT-induced biological event, such as protein denaturation [59,66]. The thermal dose concept, CEM43°C, was established to account for the biological effects induced by HT in terms of both temperature and ttreat [21]. More specifically, CEM43°C calculates the equivalent time of a HT treatment session by correlating temperature, ttreat and inactivation rate of a biological effect induced by heat based on the Arrhenius equation. The reference temperature of 43 °C was shown as a breakpoint in the Arrhenius plot with a steeper slope between 41.5 and 43 °C in comparison to 43–57 °C [66]. The threshold values of CEM43°C for tissue damage differ for specific tissues as identified in in vivo studies and are reviewed elsewhere [70,73,74]. In addition, these data underline that CEM43°C is an important parameter that has biological validity to assess the thermal damage in tissues. CEM43°CT90 is one of the most frequently used thermal dose descriptors at T90, not only in clinical, but also in experimental settings. In an in vivo study, Thrall et al. [75] showed a relationship between CEM43°CT90 and local control in canine sarcomas, but not with CEM43°CT50 and CEM43°CT10. Another in vivo study using breast (MDA-MB-231) and pancreatic cancer (BxPC-3) xenografts showed that at relatively low values of CEM43°CT90, tumor volumes could be reduced by exposure to heat alone [76]. However, none of the preclinical studies proposed reference values for clinical validation, as shown in Table 4.
Table 4.
Reference thermal dose parameters for HT.
| Thermal Dose Parameters | Reference Value |
|---|---|
| CEM43°CT10 | Undefined (min) |
| CEM43°CT50 | Undefined (min) |
| CEM43°CT90 | Undefined (min) |
| TRISE | Undefined (°C) |
| AUC | Undefined (°C-min) |
Although there is no reference threshold value for the CEM43°C, its efficacy to predict tumor response and local control has been experimentally proven [75,77]. CEM43°C is considered as a thermal dose parameter with few weaknesses which have been discussed elsewhere [78].
3.4. Number of HT Sessions
Thermotolerance is an undesirable side effect of HT which renders tumor cells insensitive to heat treatment for 48 to 72 h [79]. Thermotolerance consists of an induction phase, a development phase, and a decay phase. Each of these components may have its own temperature dependence as well as dependence on other factors, such as pH and presence of nutrients [80]. Thermotolerance plays an important role on how HT sessions are scheduled during the treatment course. An in vivo study using C3H mouse mammary carcinoma confirmed that preheating for 30 min at 43.5 °C induced thermotolerance for the next heating session [81]. Twice weekly heating to 43 °C for 60 min in combination with RT at 3 Gray (Gy) per fraction for 4 weeks was shown to result in a steady state decline in oxygenation level suggesting vascular thermotolerance [82]. In comparison, Nah et al. reported that heating at 42.5 °C for 60 min could render the tumor blood vessels resistant to the next heating session after an interval of 72 h [83]. It has also been shown that when HT was delivered daily with RT 5 days a week, no significant thermal enhancement could be detected in comparison to one single HT session, even when heat was delivered simultaneously or sequentially [84]. With the agreement of these findings, Nweek is defined as 1 or 2 sessions separated by at least 72 h (Table 5).
Table 5.
Reference HT treatment session parameters. N: positive constant value.
| Heating Session Parameter | Reference Value (N) |
|---|---|
| Ntotal | Defined 1 |
| Nweek | 1–2 2 |
1 Depending on RT and CT schedules; 2 Depending on cancer site.
In summary, HT should be delivered once or twice weekly, taking into account the type of cancer, RT fractionation and CT drug scheduling. Due to logistical reasons, the Ntotal usually depends on, the treatment plan for different cancer sites, number of RT fractions or number of CT cycles (Table 5).
3.5. Time Interval Parameter between HT and RT and/or CT
The tint between HT and RT and/or CT treatment is another parameter that affects sensitization due to time-dependent biological effects and its contribution to thermotolerance.
Recently, an in vitro study of human papillomavirus (HPV)-positive (HPV16+, HPV18+) and HPV-negative cell lines that were treated with HT either 0, 2 and 4 h before and after RT showed that the shortest tint resulted in lower cell survival fractions and decreased DNA damage repair [85]. The influence of tint has been investigated in an in vivo study, which reported that TER is greatest when heat and radiation are delivered simultaneously [15]. Unfortunately, simultaneous delivery is currently technically impossible in clinical routine and therefore heat and radiation are usually delivered sequentially. A very short tint of approximately five min is considered as an almost simultaneous application [86]. Dewey et al. concluded that HT should be applied simultaneously or within 5–10 min either side of radiation to benefit maximally from the radiosensitizating effect of heat [6]. TER is decreased faster for the normal cells than for cancerous cells when tint ≤ 4 h between HT and RT [15]. Thus, it can be argued that a slightly longer tint could ensure the sparing of normal tissue from radiosensitization before or after RT. A tint longer than 4 h, no sensitization effects induced by HT were observed [15,85]. The wide range of acceptable tint values reported in experimental studies is from 0 (when CT is delivered during HT) to 4 h (Table 6).
Table 6.
Reference tint parameter for HT in combination with RT or CT.
| Time Interval Parameter | Reference Value (min) |
|---|---|
| tint | 0–240 |
In contrast to RT, CT can be given simultaneously or immediately after or before HT [87]. A preclinical study, in which cisplatin and heat were used to treat C3H xenografts, showed that a higher additive effect can be obtained when cisplatin was given 15 min before HT in comparison with an interval longer than 4 h [55].
Furthermore, HT has been shown to sensitize the effects of gemcitabine at 43 °C when the drug was given 24 h after heating [88], whereas another study showed an optimal effect when the drug was given 24–48 h before heating [89]. The type of CT agent and its interaction with heat are factors which determine the tint between HT and CT (Table 6).
3.6. Sequencing of HT in Combination with and RT and/or CT
An additional predictive parameter for the effectiveness of radiosensitization and chemosensitization is the sequencing of heat prior to or after the application of RT or CT. Usually, HT and RT are delivered sequentially but there is no consensus as to the optimal sequence. An in vivo study by Overgaard investigated the impact of sequence and interval between the two modalities on local tumor control and normal tissue damage in a murine breast cancer model and found that the sequence did not have any significant effect on the thermal enhancement in tumor tissues [15]. However, an experimental study using Chinese hamster ovary (HA-1) and mouse mammary sarcoma (EMT-6) cell lines showed that sequencing of radiation and heat altered radiosensitivity for these two cancer cell types [90]. HT before RT showed more thermal enhancement in synchronous HA-1 cell lines and the opposite sequence increased the thermal enhancement in EMT-6 cell lines. Other experimental studies reported no impact of the sequence of RT and HT in V79 cells on thermal enhancement [26,72]. In line with these results, an experimental study with HPV cell lines showed no difference in radiosensitization or cell death when heat was delivered prior or after radiation [85]. Due to conflicting results with regard to the treatment sequencing of HT and RT, additional preclinical mechanistic studies on different cell types are required.
An in vivo study where heat was combined with cisplatin CT showed that simultaneous application of both treatments resulted in prolonged tumor growth delay in comparison with administration of cisplatin after HT [55]. Another study found that simultaneous exposure of human colorectal cancer (HCT116) cells to HT and doxorubicin was more effective than sequential administration because of higher intercellular drug concentrations at 42 °C [91]. In conclusion, better insight into the interaction of various CT drugs with HT and RT is required to define the optimal sequencing of specific drugs and RT dose.
4. Evidence for the Predictive Values of Thermometric Parameters in Clinical Studies Combining HT with RT
Numerous prospective and retrospective clinical studies have been conducted to assess the efficacy of HT in combination with RT for treating superficial and deep-seated tumors. The design of most clinical studies was based on the translation of experimental findings aiming to reproduce benefit of HT when combined with RT.
Table 7 and Table 8 show the results of the most important clinical studies. The prospective clinical studies in Table 7 reported improved clinical results, apart from the study by Mitsumori et al. which did not show a significant difference in the primary clinical endpoint of local tumor control between two treatment arms [92]. The underlying reason could have been differences in RT dose prescriptions and missing patient treatment data. Although the study showed a significant difference in progression free survival, this was judged to be not a substantial benefit. The authors stressed the need for internationally standardized treatment protocols for the combination of HT and RT.
Table 7.
Prospective clinical studies using RT in combination with HT.
| Author(s) | Cancer Site, n | RT Dose (Gy) /Fractions |
Temperature Metrics (°C) |
HT Session |
ttreat
(min) |
Thermal Dose (min) |
tint
(min) |
Sequence | Clinical Outcome (Comment) |
|---|---|---|---|---|---|---|---|---|---|
| Chi et al. [96] |
Bone metastases, n = 29 | 30.0/10 | Tmax
†: 41.9 ± 1.2 |
Ntotal: 4 Nweek: 2 |
40 | n.r. | 120 | HT after RT |
|
| Valdagni et al. [103] | Head & neck, n = 18 |
64.0–70.0 /32–35 |
Tmax
†: 43.3 ± 0.2 Tmin †: 40.4 ± 0.2 T50: 41.8 ± 0.2 T90: 39.8 ± 0.02 |
Ntotal: 6 Nweek: 2 |
n.r. | max CEM42.5°C 5: 83.84 ± 9.4 min CEM42.5°C: 12.8–2.1 |
20–25 | HT after RT |
|
| Jones et al. [35] | Superficial cancers, n = 56 |
30.0–66.0 /15–33 when previously unirradiated 60.0–70.0 /30–35 |
n.r. | Ntotal: 4–10 Nweek: 2 |
60 min | CEM43°CT90
†: 14.3 (0.57–36.21) |
n.r. | n.r. |
|
| van der Zee et al. [104] |
Locally advanced pelvic tumors, n = 182 |
Bladder: 66.0–70.0 /33–35 Cervix: 40.0–50.0 /23–28 with HDR-IRT 23 (192 Ir): 14.0 or LDR-IRT 24 (192 Ir): 20.0–30.0 Rectum: 46.0–50.0 /20–22 |
n.r. | Ntotal: 5 Nweek: 1 |
60 | n.r. | 60–240 | HT after RT |
|
| Harima et al. [105] | Cervix cancer, n = 20 |
52.2/29 with HDR-IRT (192 Ir): 30.0/4 |
Tmax
†: 41.8 ± 1.1 Tavg †: 40.6 ± 1.0 Tmin †: 39.6 ± 0.9 |
Ntotal: 3 Nweek: 1 |
60 | n.r. | 30 | HT after RT |
|
| Mitsumori et al. [92] | Locally advanced non-small cell lung cancers, n = 40 |
66.0–70.0 /33–38 |
Tmax
†: 41.3 (37.7–44.0) Tmin †: 39.5 (35.5–41.7) Tavg †: 40.3 (37.0–42.7) |
Ntotal: 7 Nweek: 1 |
60 | n.r. | n.r. | n.r. |
|
| Masunaga et al. [100] | Urinary bladder cancer, n = 28 |
24.0/6 | Tavg
†: 41.5 ± 1.1 (39–44) |
Ntotal: 4 Nweek: 2 |
15–40 | n.r. | n.r. | HT after RT |
|
| Berdov et al. [106] | Advanced rectal cancer, n = 56 |
40.0/10 | n.r. | Ntotal: 4–5 Nweek: n.r. |
60 | n.r. | 10 | HT before RT |
|
| Maluta et al. [107] | Locally advanced high risk prostate cancer, n = 144 | 70.0–76.0 /35–38 |
Rectum Tmax †: 42.7 T90 †: 40.2 (38.4–42.0) Bladder T90 †: 41.3 (39.5–42.3) |
Ntotal: 4 Nweek: 1 |
n.r. | CEM40 °CT90
†: 24.4 (14.4–34.4) |
15–30 | HT before RT |
|
| Leopold et al. [40] | Superficial cancers, n = 111 |
24.0–70.0 /7–28 |
n.r. | Ntotal
†:4.5(1–6) for Nweek=1 and 7 (2–13) for Nweek=2 Nweek: 1–2 |
60 | n.r. | 30–90 | HT after RT |
|
| Nishimura et al. [97] | Colorectal cancer, n = 33 | 40.0–70.0 /25–35 |
Abdominal wall & hip: Tmax †: 44.2 ± 2.1 Tavg †: 42.6 ± 1.3 Tmin †: 40.5 ± 0.7 Perineum: Tmax †: 43.1 ± 1.7 Tavg †: 42.2 ± 1.2 Tmin †: 40.5 ± 1.1 Pelvis: Tmax †: 42.1 ± 1.5 Tavg †: 41.2 ± 1.5 Tmin †: 40.1 ± 1.1 |
Ntotal: 2–14 Nweek: 1–2 |
40–60 | n.r. | 10–30 | HT after RT |
|
| Anscher et al. [108] | Prostate cancer, n = 21 |
65–70 /32–35 |
Intraprostate median T90 †: 39.3 ± 0.9 T50 †: 40.4 ± 0.8 |
Ntotal: 5–10 Nweek: 1–2 |
60 | CEM43°CT90
†: 2.34 ± 3.23 |
60–154 | HT after RT |
|
| Gabriele et al. [109] | Inoperable or recurrent parotid carcinoma, n = 13 |
Inoperable: 70.0/35 Recurrent: 30.0/15 |
Tmin
†: 40.28 ± 0.83 Tmax †: 42.83 ± 1.32 |
Ntotal: 4–10 Nweek: 2 |
30–45 | n.r. | n.r. | n.r. |
|
| Maguire et al. [110] | Soft tissue sarcomas, n = 35 | 50.0/25–27 | n.r. | Ntotal: 10 Nweek: 2 |
60 | CEM43°CT90
‡: 38 (0.1–601) |
n.r. | n.r. |
|
| Tilly et al. [99] | Recurrent or locally advanced prostate cancer, n = 22 |
68.4/38 | Primary cancer: T90 †: 40.7 ± 0.3 Tmax †: 41.4 ± 0.4 Recurrent cancer: T90 †: 40.6 ± 0.8 Tmax †: 41.0 ± 0.7 |
Ntotal: 5–6 Nweek: 1 |
0–30 | n.r. | 30 | HT before RT or HT after RT |
|
| Lutgens et al. [111] | Locally advanced cervical cancer, n = 42 |
50.0/25 with HDR-IRT (192 Ir): 21.0/3 weekly or LDR: 32.0/1–2 or MDR: 29.0/1–2 |
n.r. | Ntotal: 5 Nweek: 1 |
60 | n.r. | 60–240 | HT after RT |
|
| Hurwitz et al. [112] | Locally advanced prostate cancer, n = 37 |
66.60–70.0 /33–37 |
Tmin
†: 40.1 (37.5–41.8) Tmax †: 42.5 (40.5–45.9) Tavg †: 41.2 (39.2–42.8) |
Ntotal: 2 Nweek: 1 |
60 | CEM43°CT90
†: 8.4 |
60 | HT before RT |
|
| Vernon et al. [113] | Localized superficial breast cancer, n = 306 |
DHG 17 (p): 32.0/16 DHG (r): 40.5–50.0/25 + boost: 10.0–20.0 MRC 18 BrR (p): 28.8/8 MRC BrI(r) + MRC BrR(r): 50.0/25 + boost: 15.0/5 ESHO 19: 32.0/8 PMH 20(p): 32.0/18 PMH(r): 50.0/25 |
DHG: T90 †: 39.0 T50 †: 40.7 Tmax †: 43.5 MRC BrR: T90 †: 40.7 T50 †: 42.5 Tmax †: 45.6 MRC BrI: T90 †: 40.4 T50 †: 42.3 Tmax †: 45.1 ESHO: T90 †: 39.5 T50 †: 41.1 Tmax †: 43.3 PMH: T90 †: 40.7 T50 †: 42.2 Tmax †: 44.6 |
n.r. | DHG: 60 (55–61) MRC BrR: 60 (30–60) MRC BrI: 60 (17–65) ESHO: 60 (60–60) PMH: 60 |
DGH: maximum of CEM42 °C †: 0(0–69.5) CEM43°C †: 3.95 (0–122) MRC: maximum of CEM42 °C †: 9 (0–60) CEM43°C †: 7.5 (0.1–87.7) ESHO: maximum of CEM42 °C †: 5 (0–59) CEM43°C †: 8.4 (0.2–74) PMH: maximum of CEM42 °C †: 0 (0–32.8) CEM43°C †: 1.5 (0–25) data from Sherar et al. [39] |
n.r. | n.r. |
|
| Datta et al. [114] | Head & neck cancer, n = 33 |
50.0 /25 |
n.r. | Ntotal: 8–10 Nweek: 2 |
n.r. | n.r. | n.r. | HT before RT |
|
| Overgaard et al. [115] | Recurrent or metastatic malignant melanoma, n = 63 |
24.0–27.0 /3 |
n.r. | Ntotal: 3 Nweek: 1 |
60 | CEM43°C †: 9 (0–219) data from Overgaard et al. [116] |
30 | HT after RT |
|
| Dinges et al. [41] | Uterine cervix carcinomas, n = 18 |
50.4/28 with HDR-IRT (192 Ir): 20.0/4 |
T20
†: 41.7 (40.3–43.2) T50 †: 41.1 (39.2–42.5) T90 †: 39.9 (37.7–41.9) |
Ntotal: 4 Nweek: 2 |
60 | CEM43°CT20
†: 48.2 (5.9–600.5) CEM43°CT50†: 15.2 (0.6–54.0) CEM43°CT90 †: 6.8 (0.4–23.0) |
n.r. | n.r. |
|
| Kim et al. [117] |
Inoperable hepatoma, n = 30 |
30.6/17 | n.r. | Ntotal: 6 Nweek: 2 |
30–60 | n.r. | 30 | n.r. |
|
| Engin et al. [98] | Superficial tumors, n = 50 | 60.0–70.0 /30–35 when previouslyirradiated: 40.0/10 |
Group A: Tmin †: 39.6 ± 0.2 Group B: Tmin †: 39.3 ± 0.2 |
Group A: Ntotal: 4 Nweek: 1 Group A: Ntotal: 8 Nweek: 2 |
60 | Group A: CEM 43°C †: 12.1 ± 3.9 Group B: CEM43°C †: 15.0 ± 5.1 |
15–30 | HT after RT |
|
n: number of patients assigned to be treated with HT in combination with RT; †: mean value (±standard deviation) or mean value (range); ‡: median (range); n.r.: not reported; 1 CR: complete response; 2 PR: partial response; 3 PD: progressive disease; 4 LC: local control; 5 CEM42.5 °C: cumulative equivalent minutes at reference temperature 42.5 °C; 6 OS:overall survival, 7 NC: no change; 8 LRFS: local relapse-free survival; 9 DFS: disease free survival; 10 RR: responserate; 11 LR: local response; 12 pCR: pathological CR; 13 LF: local failure; 14 DM: distant metastasis; 15 RrR: recurrence rate; 16 PSA: prostate specific antigen; 17 DHG: Daniel den Hoed Cancer Center in Rotterdam; 18 MRC: Medical Research Council at the Hammersmith Hospital; 19 ESHO: European Society of Hyperthermic Oncology; 20 PMH: Princess Margaret Hospital/Ontario Cancer Institute; 21 NR: no response; 22 DSS: disease specific survival; 23 HDR-IRT: high dose rate interventional radiotherapy; 24 LDR-IRT: low dose rate interventional radiotherapy.
Table 8.
Retrospective clinical studies using RT in combination with HT.
| Author(s) | Cancer Site, n | RT Dose (Gy) /Fractions |
Temperature Metrics (°C) |
HT Session |
ttreat
(min) |
Thermal Dose (min) |
tint
(min) |
Sequence | Clinical Outcome (Comment) |
|---|---|---|---|---|---|---|---|---|---|
| Franckena et al. [36] | Locally advanced cervix cancer, n = 420 |
46.0–50.4 /23–28 with HDR-IRT 11 (192 Ir): 17.0/2 weekly or LDR-IRT 12: 18.0/3 weekly or LDR: 30 Gy in 60 h |
n.r. | Ntotal: 5 Nweek: 1 |
60 | CEM43°CT90
†: 5.05 ± 4.18 min |
n.r. | n.r. |
|
| Kroesen et al. [33] | Locally advanced cervix cancer, n = 400 |
46.0 -50.4 /23–28 with HDR-IRT (192 Ir): 17.0/2 or MRI-IRT 7.0/3–4 |
n.r. | Ntotal: 5 Nweek: 1 |
60 | CEM43°CT90
†: 3.40 (1.89–5.83) TRISE †: 3.46 (2.93–3.86) |
30–230 | HT after RT |
|
| van Leeuwen et al. [22] | Locally advanced cervix cancer, n = 58 |
46.0–50.4 /23–28 with PDR: 24 |
n.r. | Ntotal: 4–5 Nweek: 1 |
60 | n.r. | 33.8–125.2 † | HT after RT |
|
| Franckena et al. [120] | Locally advanced cervix cancer, n = 378 |
46.0–50.4 /23–28 with HDR-IRT (192 Ir): 17.0/2 or 18.0–21.0/3 or 20.0–24.0/1 or HDR: 30.0/1 |
Tavg †: 40.6 | Ntotal: 5 Nweek: 1 |
60 | n.r. | 30–240 | HT after RT |
|
| Oldenborg et al. [121] | Recurrent breast cancer, n = 78 |
32.0/8 | T90
†: 41.1 (37.7–42.4) T50 †: 42.2 (39.0–43.4) T10 †: 43.2 (41.0–44.5) |
Ntotal: 4 Nweek: 1 |
60 | CEM43°CT90
†: 22.3 (1.5–107.7) CEM43°CT50 †: 37.3 (3.3–96.0) |
60 | HT after RT |
|
| Datta et al. [49] | Muscle invasive bladder cancer, n = 18 |
unifocal cancer: 48.0/16 multifocal cancer: 50.0/20 |
Tavg
†: 40.5 ± 0.5 Tmin †: 36.7 ± 0.3 Tmax †: 42.0 ± 0.6 |
Ntotal: 4 Nweek: 1 |
60 | CEM43°C: 59.8 ± 45.6 |
15–20 | HT before RT |
|
| Leopold et al. [32] | Soft tissue sarcoma, n = 45 | 50.0–50.4 /25–28 |
T90
‡: 39.5 T50 ‡: 41.6 T10 ‡: 43.0 Tmin ‡: 37.7 Tmax ‡: 44.0 |
Group A: Ntotal: 5 Nweek: 1 Group B: Ntotal: 10 Nweek: 2 |
60 | n.r. | 30–60 | HT after RT |
|
| Ohguri et al. [94] | Non-small cell lung cancer, n = 35 |
45.0–80.0 /23–30 |
Tmax
‡: 43.2 (38.9–48.1) Tavg ‡: 42.6 (38.8–47.0) Tmin ‡: 41.7 (38.6–45.6) |
Ntotal
‡: 11 (3–17) Nweek: 1–2 |
40–70 | n.r. | 15 | HT after RT |
|
n: number of patients assigned to be treated with HT in combination with RT; †: mean value (±standard deviation) or mean value (range); ‡: median (range); n.r.: not reported; 1 CR: complete response; 2 PR: partial response; 3 SD: stable disease; 4 PD: progressive disease; 5 PTC: pelvic tumor control; 6 DSS: disease specific survival; 7 DFS: disease free survival; 8 OS:overall survival; 9 IFR: in-field recurrence; 10 NC: no change; 11 HDR-IRT: high dose rate interventional radiotherapy; 12 LDR-IRT: low dose rate interventional radiotherapy.
In reality, temperature and thermal dose are usually reported as post-treatment data recordings (Table 2 and Table 4) to account for temperature homogeneity or sensitivity. Even though temperature cannot always be measured invasively, depending on the location of the tumor, a strong correlation was reported between intratumoral and intraluminal temperatures, suggesting that intraluminal temperature measurements are a good surrogate for pelvic tumor measurements [50,93]. In addition, retrospective studies showed that a higher intra-esophageal temperature (>41 °C) predicts longer overall survival, improved local control and metastasis-free rate [94,95]. The difficulty of performing invasive measurements was illustrated by a randomized phase III study by Chi et al. [96] in which only 3 out of 29 patients with bone metastases had directly measured intratumoral temperature. In the study by Nishimura et al. [97], the HT session was defined as effective if an intratumoral temperature exceeded 42 °C for more than 20 min. However, according to the Arrhenius relationship, this is not considered long enough to induce a significant biological effect [21].
Another obstacle during HT is the non-standardized methodology for describing the temporal and spatial variance of temperature fields. Several groups have investigated the correlation between various temperature metrics. The study by Oleson et al. showed that Tmin, tumor volume, radiation dose, and heating technique play significant roles in predicting treatment response for patients treated with RT in combination with HT [29]. In contrast, Leopold et al. reported that the more robust parameters T90, T50, and T10 are better temperature descriptors and predictors of histopathologic outcome than Tmin and Tmax [32]. The median Tmin, Tmin during the first heat treatment and tumor volume were reported to be factors predictive for the duration of cancer response (Table 7) [98], even though it is considered that skin surface temperature is not representative for superficial tumors and cannot be associated with clinical outcomes [42]. For deep-seated tumors, Tilly et al. reported that Tmax was a predictive treatment parameter for prostate-specific antigen (PSA) control [99]. The relationship of high (Tavg ≥ 41.5 °C) and low (Tavg < 41.5 °C) tumor temperature with clinical response has been analyzed in a study by Masunaga et al. [100]. They showed that heating the tumor to temperatures of Tavg ≥ 41.5 °C for a duration of 15–40 min achieved better tumor down-staging and better tumor degeneration rates [100]. This finding supports the concept that direct cytotoxic effects of HT are enhanced at temperatures higher than 41 °C, as suggested in preclinical studies [5,57]. A higher response rate was also reported when tumors were heated with Tavg > 42 °C for 3–5 HT sessions [97]. In contrast, a study showed no difference in clinical outcome when patients were treated with mean Tmin = 40.2 °C, Tmax = 44.8 °C or Tavg = 42.5 °C for Ntotal of 2 or 6 [24]. Other studies also reported no impact of Ntotal and Nweek on clinical outcome [40,101]. The contradictory results derived from clinical studies with regard to the predictive power of temperature descriptors and Ntotal are why we did not list reference values for these descriptors in Table 5.
The predictive role of thermal dose has been investigated in both prospective and retrospective clinical studies (Table 7 and Table 8). However, there is still no conclusion about the values for thermal dose that should be obtained during HT treatment for maximal enhancement effect. In prospective studies (Table 7), the correlation between thermal dose and treatment outcome is rarely reported. Retrospective studies reported that thermal dose, CEM43°C, is an adequate predictor of treatment response and its best prognostic descriptor is CEM43°CT90 [32,33,36,37,38,102].
In a phase III study of the International Collaborative Hyperthermia Group, led by Vernon et al. [113], thermal dose was associated with complete response (CR) in patients treated for superficial recurrences of breast cancer [39]. Another randomized study showed that the best tumor control probability was dependent on thermal dose [106]. Further, retrospective analyses indicate that thermal dose is a significant predictor of different clinical endpoints (Table 8) [33,36]. A few studies did not find such significant relationships between clinical endpoints and thermal dose [103,109,110]. For example, in the prospective study of Maguire et al., a total CEM43°CT90 with a threshold above 10 min did not show a significant effect on CR [110]. However, the association of CEM43°CT90 with CR was later reported for patients treated with superficial malignant cancers [35]. Similar to the study by Maguire et al., the minimum effective thermal dose was set as 10 CEM43°CT90. In addition, a test HT session was performed to verify if the tumor was heatable, and a thermal dose of higher than 0.5 CEM43°CT90 could be achieved [35,110]. The objective of the study by Hurwitz et al. was to achieve a CEM 43 °CT90 of 10 min, yet the resulting mean of thermal dose for all 37 patients was only 8.4 min [112]. The cumulative minutes T90 > 40.5 °C, defined as ‘the time in minutes with T90 > 40.5 °C for the whole Ntotal’, with a mean of 179 ± 92 min, together with T90 and Tmax were reported to correlate with toxicity and prostate specific antigen clinical endpoints [99]. Similarly, Leopold et al. showed that cumulative minutes of T90 > 40 °C is a predictor of treatment endpoints [40]. In retrospective studies, TRISE thermal dose concepts [36] were shown to have a predictive role in treatment response. These retrospective analyses showed that TRISE had a significant effect on local control for a cohort of patients with cervical cancer [33].
The effect of the tint parameter has been only analyzed with respect to treatment endpoints in retrospective studies. The study by van Leeuwen et al. reported that a tint less than 79.2 min between RT and reaching 41 °C during HT was associated with a lower risk of in-field recurrences (IFR) and a better overall survival (OS) in comparison to a longer tint [22]. In contrast, another retrospective study showed that neither a shorter tint of 30–74 min nor a longer tint of 75–220 min between RT and the start of HT were significant predictors of local control (LC), disease free survival (DFS), disease specific survival (DSS) or OS [33]. Thus, the optimal tint between HT and RT to achieve a maximal effect on the tumor remains unknown.
Apart from heat-related parameters, the total dose of ionizing radiation and its fractionation in combination with HT has an impact on clinical treatment response [118,119]. Valdagni et al. [103] reported that increasing the total dose of RT appeared to improve clinical response as 71% (5/7) and 90% (9/10) CR rates were observed for patients with nodal metastases of head and neck cancers who received total doses of 64–66 Gy or 66.1–70 Gy, respectively. In addition, it was reported that previously irradiated tumors, which are typically more resistant to ionizing radiation, achieved higher CR rates when treated with combined RT and HT in comparison with RT alone [35].
Furthermore, RT technique has been reported to have a beneficial effect on combined RT and HT treatment outcomes [29]. For example, technological advance such as MRI-guided brachytherapy were shown to improve the treatment outcome when RT is combined with HT [36].
The weak, and in part contradictory, evidence from clinical studies clearly shows that further analyses of thermometric parameters are required to define reference values for clinical use. The reported values for thermometric parameters from prospective and retrospective clinical studies (Table 7 and Table 8) can be translated into standard references after being tested and validated in prospective clinical trials.
5. Evidence for Predictive Values of Thermometric Parameters in Clinical Studies Combining HT and CT
The added value of combining CT with HT has been established, not only in in vitro and in vivo studies, but also in clinical studies. Randomized clinical studies, which demonstrate that the combination of CT and HT results in improved clinical outcome in comparison with single modality treatment [122,123,124,125], confirm the preclinical findings [126]. The positive prospective and retrospective clinical studies are summarized in Table 9 and Table 10 respectively, with a focus on thermometric parameters.
Table 9.
Prospective clinical studies using CT in combination with HT.
| Author(s) | Cancer Site, n |
CT Drug(s) (mg/m2) × Cycles |
Temperature Metrics (°C) |
HT Session |
ttreat
(min) |
Thermal Dose |
tint
(min) |
Sequence | Clinical Outcome (Comment) |
|---|---|---|---|---|---|---|---|---|---|
| Issels et al. [123] | Localised high-risk soft-tissue sarcoma, n = 104 |
125 etoposide twice weekly × 4 1500 ifosfamide four times weekly × 4 50 doxorubicin once weekly × 4 |
Tmax
‡: 41.8 (IQR: 41.1–43.2) T20 ‡: 40.8 (IQR: 40.1–42.3) T50 ‡: 40.3 (IQR: 39.5–41.0) T90 ‡: 39.2 (IQR: 38.5–39.8) |
Ntotal: 8 Nweek: 2 |
60 | n.r. | n.r. | n.r. |
|
| Alvarez Secord et al. [136] | Refractory ovarian cancer, n = 30 | 40 doxil once weekly × 6 |
T90
†: 39.78 ± 0.59 T50 †:40.47 ± 0.56 |
Ntotal: 6 |
60 | CEM43°CT90
†: 5.84 ± 5.66 CEM43°CT50 †: 13.00 ± 11.25 |
0–60 | HT after CT |
|
| Fiegl et al. [134] |
Advanced soft tissue sarcoma, n = 20 |
1500 ifosfamide four times weekly × 7 100 carboplatin four times weekly × 7 150 etoposide four times weekly × 7 |
Tmax
†: 40.6 (39.1–42.2) |
Ntotal: 8 Nweek: 2 |
60 | n.r. | n.r. | n.r. |
|
| Rietbroek et al. [133] | Irradiated recurrent cervical cancer, n = 23 | 50 cisplatin once weekly × 12 |
T20
†: 41.9 ± 0.9 °C T50 †: 41.3 ± 0.8 °C T90 †: 40.5 ± 0.7 °C |
Ntotal: 12 Nweek: 1 |
60 | n.r. | 30 | HT after CT |
|
| Zagar et al. [127] | Recurrent breast cancer, ntrial 1 = 18 ntrial 2 = 11 |
Trial A: 20–60 LTDL 13 every 21–35 days × 6 Trial B: 40–50 LTDL every 21–35 days × 6 |
max T90: 42.6 min T90: 36.0 |
Ntotal: 6 |
60 min | n.r. | 30–60 | HT after CT |
|
| Ishikawa et al. [139] | Locally advanced or metastatic pancreatic cancer, n = 18 |
1000 gemcitabine once weekly × 12 |
n.r. | Ntotal: 20 Nweek: 1 |
40 | n.r. | 0–1440 | HT before CT |
|
| Vujaskovic et al. [138] | Locally advanced breast cancer, n = 43 |
30–75 LTDL × 4 100–175 paclitaxel × 4 |
T90 †: 39.7(37.7–41.8) | Ntotal: 4 Nweek: 2 |
60 | CEM43°CT90
†: 11.5 (1.5–159.3) |
60 | HT after CT |
|
| de Wit et al. [135] | Recurrent uterine cervical carcinoma, n = 19 |
60, 70, 80 cisplatin once weekly × 6 |
Tmax
†: 41.6 ± 0.7 (39.7–43.6) |
Ntotal: 6 Nweek: 1 |
60 | n.r. | 0 | HT after CT |
|
| Sugimach et al. [124] | Oesophageal >carcinoma, n = 20 | 30 * bleomycin twice weekly × 3 50 * cisplatin once weekly × 3 |
n.r. | Ntotal: 6 Nweek: 2 |
30 | n.r. | n.r. | HT after CT |
|
n: number of patients assigned to be treated with HT in combination withCT; †: mean value (±standard deviation) or mean value (range); ‡: median (range); n.r.: not reported; *: in mg unit only; 1 LPFS: local progressionfree survival; 2 OS: overall survival; 3 CR: complete response; 4 PR: partial response; 5 SD: stable disease; 6 PD: progressive disease; 7 PFS: progression free survival; 8 PFR: progression free rate; 9 RR: response rate; 10 DFS: disease free survival; 11 QoL: quality of life; 12 NC: no change; 13 LTDL: low temperature liposomal doxorubicin.
Table 10.
Retrospective clinical trial studies using CT in combination with HT.
| Author(s) | Cancer Site, n | CT Drug(s) (mg/m2) × Cycles |
Temperature Metrics (°C) |
HT Session |
ttreat
(min) |
Thermal Dose |
tint
(min) |
Sequence | Clinical Outcome (Comment) |
|---|---|---|---|---|---|---|---|---|---|
| Yang et al. [140] | Advanced non-small cell lung cancer, n = 48 |
1000 gemcitabine twice weekly × 6 75 cisplatin twice weekly × 6 |
n.r. | Ntotal: 8 Nweek: 2 |
40–60 | n.r. | n.r. | HT after CT or HT before CT |
|
| Tschoep-Lechner et al. [141] | Advanced pancreatic cancer, n = 23 |
1000 gemcitabine once weekly × 8 25 cisplatin twice weekly × 8 |
Tmax
†: 42.1 (40.9–44.1) |
Nweek: 2 Ntotal ‡: 8 |
60 | n.r. | 0 | simultaneously |
|
| Stahl et al. [137] | Soft tissue sarcomas, n = 46 |
250 etoposide × 4 6000 ifosfamide × 4 50 adriamycin × 4 |
T90
†: 39.90 ± 0.74 (good responders) and T90 †: 39.42 ± 1.78 (bad responders) |
Nweek: 2 Ntotal ‡: 8 |
60 | CEM43°CT90†: 17.96 ± 7.16 (good responders) CEM43°CT90†: 11.07 ± 5.58 (good responders) |
0 | simultaneously |
|
n: number of patients assigned to be treated with HT in combination withCT; †: mean value (±standard deviation) or mean value (range); ‡: median (range); 1 CR: complete response; 2 PR: partial response; 3 SD: stable disease; 4 PD: progression disease; 5 ORR: objective response rate; 6 DCR: disease control rate; 7 OS: overall survival; 8 RECIST: Response Evaluation Criteria in Solid Tumors; 9 WHO: world health organization.
The effectiveness of CT drugs has been enhanced by HT in a variety of clinical situations, such as localized, irradiated, recurrent, and advanced cancers, but only few indications are really promising. Long term outcome data, e.g., regarding the combination of CT with HT for bladder cancer, underline the clinical efficacy of this treatment strategy [125]. Chemosensitization by HT is induced by specifics biological interactions between CT drugs and heat. The increased blood flow and the increased fluidity of the cytoplasmic membrane of the cells induced by HT increase the concentration of CT drugs within malignant tissues. Interestingly, Zagar et al. performed a joint analysis of two different clinical trials and reported no significant correlation between drug concentration and combined treatment effect of CT and HT [127]. However, only a few CT drugs with specific properties (Table 9 and Table 10) are good candidates to use with HT. Alkylating agents, nitrosureas, platinum drugs, and some antibiotic classes show synergism with HT, whereas only additive effects are reported with pyrimidine antagonists and vinca alkaloids [59]. For example, heat increases the cytotoxicity of cisplatin, as shown by in vitro and in vivo studies [28,55]. Cisplatin concentration increases linearly with temperatures above 38 °C when applied simultaneously [28,128]. Synergy between HT and CT could be obtained at temperatures below 43.5 °C in a preclinical study [55]. Similarly, enhanced toxicity has been demonstrated for bleomycin [126,129], liposomal doxorubicin [130], and mitomycin-C [131]. Based on the summary of preclinical data, van Rhoon et al. suggested a CEM43°C of 1–15 min from heating to 40–42 °C for 30–60 min for any free CT drug, including thermos-sensitive liposomal drugs [132].
Lower temperatures might increase the therapeutic window by differential chemosensitization of cancer and normal tissues. In the prospective study of Rietbroek et al. [133] in patients with recurrent cervical cancer treated with weekly cisplatin and HT, three temperature descriptors, T20, T50, and T90, including the time in minutes in which 50% of the measured tumor sites were above 41 °C, indicated a significant difference in these parameters between patients who did and who did not exhibit a CR after treatment. However, there was neither a difference in Tmax between responders and non-responders in a cohort of patients with recurrent soft tissue sarcomas treated with CT and HT [134], nor in a cohort of patients with recurrent cervical cancer [135].
In a prospective study of patients treated with CT and HT for recurrent ovarian cancer, no significant relationship of T90 and T50 and CEM43°CT90 and CEM43°CT50 with clinical outcome was found [136]. Similarly, the independency of T90 and CEM43°CT90 was also demonstrated in a retrospective study in soft tissue sarcoma [137]. Although a relationship of thermal dose with treatment response has been reported by Vujaskovic et al. [138], the parameters CEM43°CT50 and CEM43°CT90 were not statistically different between patients who did or did not respond to the treatment. The low mean value of T90 =39.7 (33.5–39.8) °C reported in this study might be the reason for the non-significant relationship of thermal dose with the clinical endpoint in addition to other factors such as hypoxia and vascularization level of the tumor. The first randomized phase III study that assessed the safety and efficacy of CT in combination with HT also recorded a low (≤40 °C) mean value of T90 = 39.2 °C (38.5–39.8 °C). However, the thermometric data were not analyzed or reported in correlation with treatment response [123]. Further investigations are required to understand which temperature is needed to achieve a maximum therapeutic effect, according to the type of CT drug and its concentration.
Based on preclinical studies, the delivery of simultaneous CT and HT is recommended to achieve the greatest chemosensitization effect by HT [55,142]. However, in contrast to experimental results [20,55], most of the prospective studies listed in Table 9 were designed to deliver heat sequentially, and in most studies the CT drugs were administered prior to HT. Despite the fact that a considerable supra-additive or synergistic effect can be achieved by the simultaneous delivery of CT and RT, the sequential application of CT and HT may protect normal tissues from chemosensitization. The cell killing of hypoxic and oxygenated tumor cells can still be obtained with sequential delivery of CT drugs and HT [54]. In clinical studies, the tint between modalities is usually kept under an hour [122,127,133,136,138]. Of note, the study of Ishikawa et al. showed a different scheduling of gemcitabine and HT for the treatment of locally advanced or metastatic pancreatic cancer [139]. Patients enrolled in this clinical study were treated with HT prior to CT with a tint of 0–24 h. This unique flexible relationship of gemcitabine cytotoxicity with the tint and sequence was revealed in an in vitro study [143]. The specific properties of CT drugs are main factors in determining the most efficient treatment sequence between CT and HT for each class of drugs.
That treatment protocols might require individualized standards for HT thermometric parameters as has recently been illustrated by an interim analysis of cisplatin and etoposide given concurrently with HT for treatment of patients with esophageal carcinoma. This analysis showed a relationship between tumor location and temperature reporting, i.e., higher temperatures were achieved in distal tumors [144]. Similar treatment site-dependent analysis of thermometric parameters should be performed in future trials. Although the biology underlying the interaction between CT drugs and heat in cancer and normal tissues is largely unknown, thermometric parameters have been shown to predict outcome when HT is combined with CT. Therefore, as discussed above, no definitive conclusions can be drawn regarding the optimal thermometric parameters for an enhanced effect of HT with CT.
6. Evidence for Predictive Values of Thermometric Parameters in Clinical Studies Using RT and CT in Combination with HT
Clinical malignancies, in particular advanced and inoperable tumors, can be treated using triplet therapy consisting of CT, RT and HT as a maximal treatment approach. The number of prospective and retrospective clinical studies investigating this approach is limited, the most important of which are listed in Table 11 and Table 12, respectively. These studies have already reported the feasibility of this trimodal approach for cervical cancer, rectal cancer, and pancreatic cancer.
Table 11.
Prospective clinical studies using RT and CT in combination with HT.
| Author(s) | Cancer site, n | CT Drug(s) (mg/m2) × Cycles |
RT Dose (Gy) /Fractions |
Temperature Metrics (°C) |
Session | ttreat
(min) |
Thermal Dose (min) |
tint (min) | Sequence | Clinical Outcome (Comment) |
|---|---|---|---|---|---|---|---|---|---|---|
| Amichetti et al. [152] | Locally advanced head & neck cancer, n = 18 |
20 cisplatin once weekly × 7 |
70.0/35 | Tmax
†: 43.2 (41.5–44.5) Tmin †: 40.1 (37–42) T90 †: 40.4 (38.7–42.2) |
Ntotal: 2 Nweek: 2 |
30 | CEM42.5 °C Tmin †: 4.36 (0–27) CEM42.5 °C Tmax †: 88 (31.8–174) |
20 | HT after RT & CT |
|
| Maluta et al. [156] | Primary or recurrent locally advanced pancreatic cancer, n = 40 |
1000 gemcitabine × 1–2 30 cisplatin × |
30.0–66.0 /10–33 |
T90
†: 40.5 (95% CI: 39.8–41) Tmax †: 41.1 (95% CI: 40.2–42.5) |
Ntotal: 3–10 Nweek: 2 |
60 | n.r. | n.r. | CT before HT & RT |
|
| Asao et al. [151] | Locally advanced rectal cancer, n = 29 |
250 5-fluorouracil for 5 days × 2 25 for 5 days × 2 |
40.0–50.0 /20–25 |
Tmax
†: 40.3 ± 0.89 (38.6–41.9) |
Ntotal: 3 Nweek: 1 |
60 | n.r. | n.r. | HT after RT during CT |
|
| Westermann et al. [150] | Cervix cancer, n = 68 |
40 cisplatin once weekly × 35 |
45.0–50.4 /25–28 with LDR- IRT 7 and HDR-IRT 7 (192 Ir) |
T90
†: 39.4 T50 †: 40.7 |
Ntotal: 8–10 Nweek: 1 |
60 | n.r. | n.r. | HT & CT after/before RT |
|
| Harima et al. [149] | Locally advanced cervical cancer, n = 51 |
30–40 cisplatin once weekly × 3–5 |
30.0–50.0 /15–25 with LDR- IRT7 (192 Ir): 5.0–6.0 /3–5 |
Tmax
†: 42.2 (40.1–44.6) Tavg†: 41.1 (39.6–42.5) Data from Ohguri et al. [155] T90 ‡: 38.9 (37.7–42.2) T50 ‡: 39.9 (38.4–42.4) |
Ntotal: 4–6 Nweek: 1 |
60 | CEM43°CT90
†: 3.8 (0.1–46.6) |
20 | HT after RT&CT |
|
| Kouloulias et al. [153] | Recurrent breast cancer, n = 15 |
40–60 liposomal doxorubicin once monthly × 6 |
30.6/17 | Tmax
†: 43.2 (41.5–44.5) Tmin †: 45.0 (44.2–45.7) |
Ntotal: 6 Nmonthly: 1 |
60 | n.r. | 180–240 | HT after CT&RT |
|
| Herman et al. [146] | Locally advanced malignancies, n = 24 |
20–50 cisplatin once weekly × 6 |
60.0–66.0 /30–33 or 24.0- 36.0 /12–18 |
Tmax
†: 43.7 ± 2.6 Tmin †: 38.2 ± 2.0 Tavg †: 40.8 ± 1.9 |
Ntotal: 6 Nweek: 1 |
60 | CEM42 °CT90
†: 11.2 ± 21.3 CEM43°CT90 †: 3.1 ± 5.4 |
n.r. | HT before CT&RT |
|
| Barsukov et al. [157] | Locally advanced rectal cancer, n = 68 |
650 capecitabine on days 1–22 × 6–8 50 oxaliplatin on days 3, 10 and 17 after × 6–8 10 metronidazole on days 8 and 15 |
40.0/10 | n.r. | Ntotal: 4 Nweek: 2 |
60 | n.r. | 60 | n.r. |
|
| Ott et al. [158] | Locally advanced or recurrent rectal cancer, n = 105 |
250 5-fluorouracil on days 1–14 and 22–35 or 1650 capecitabine on days 1–14 and 22–35 50 oxaliplatin × 4 |
LARC 50.4/28 LCC 45/25 |
n.r. | Ntotal
‡: 10 Nweek: 2 |
60 | LARC 19 CEM43°C †: 6.4 ± 5.2 LCC 20 CEM43°C †: 6.4 ± 4.9 |
n.r. | HT before RT |
|
| Gani et al. [154] | Locally advanced rectal cancer, n = 78 |
1000 5-fluorouracil × 4 |
50.4/28 | T90
‡: 39.5 (IQR: 39.1–39.9) |
Ntotal: 8 Nweek: 2 |
60 | CEM43°C ‡: 4.5 (IQR: 2.2–8.2) |
n.r. | n.r. |
|
| Rau et al. [159] | Locally advanced rectal cancer, n = 37 |
300–350 5-fluorouracil 50 * mg leucovorin 5 times weekly × 2 |
45.0–50.0 /25 |
Data from Rau et al. [160]: T90 †: 40.2 ± 1.2 Tmax †: 41.4 ± 0.6 |
Ntotal
‡: 5 Nweek: 1 |
60 | Data from Rau et al. [160] CEM43°CT90 †: 7.7 ± 5.6 CEM43°CTmax †: 33.1 ± 28.0 |
n.r. | RT after concurrent HT&CT |
|
| Wittlinger et al. [161] | Bladder cancer, n = 45 |
20 cisplatin 5 times weekly × 2 600 5-fluorouracil 5 times weekly × 2 |
50.4–55.8/ 28–31 |
Tavg
†: 40.8 (95%CI: 40.5–41.6) |
Ntotal: 5–7 Nweek: 1 |
60 | CEM43°C †:57 (95%CI: 40.5–41.6) |
60 | RT after concurrent CT&HT |
|
| Milani et al. [162] | Recurrent rectal cancer, n = 24 |
350 5-fluorouracil 5 times weekly × 4 (continuous infusion) |
30.0–45.0/ 16–25 |
T90
†: 41.4 T50 †: 42.9 T20 †: 43.5 |
Ntotal
‡: 8 Nweek: 2 |
60 | n.r. | 60 | HT after concurrent RT&CT |
|
n: number of patients assigned to be treated with HT in combination with RT and CT; †: mean value (±standard deviation) or mean value (range); ‡: median (range); 1 CR: complete response; 2 PR: partial response; 3 NC: no change; 4 OS: overall survival, 5 DFS: disease free survival; 6 LPFS: local progression free survival; 7 DFILR: disease-free interval to local relapse; 8 DLT: dose limiting toxicities; 9 FR: feasibility rate; 10 CTR: complete tumor regression; 11 LC: local control; 12 EORTC-QLQ: European Organization for research and treatment of cancer-quality of life questionnaire; 13 ORR: objective response rate; 14 RR: response rate; 15 DFSR: disease-free survival rate; 16 MFS: metastasis-free survival; 17 DMFS: distant metastases-free survival; 18 LPFR: local progression-free survival; 19 LARC: locally advanced rectal cancer; 20 LCC: recurrent rectal cancer.
Table 12.
Retrospective clinical studies using RT and CT in combination with HT.
| Author(s) | Cancer Site, n | CT Drug (s)(mg/m2) × Cycles |
RT Dose (Gy) /Fractions |
Temperature Metrics (°C) |
Session | ttreat (min) |
Thermal Dose (min) |
tint (min) | Sequence | Clinical Outcome (Comment) |
|---|---|---|---|---|---|---|---|---|---|---|
| Zhu et al. [163] | Locally advanced esophageal cancer, n = 78 |
450 5-fluorouracil five times weekly × 4–6 25 cisplatin five times weekly × 4–6 6 |
60.0–66.0 /30–33 |
n.r. | Ntotal: 6–12 Nweek: 2 |
60 | n.r. | 120 | n.r. |
|
| Ohguri et al. [148] | Locally advanced pancreatic cancer, n = 20 |
Group A: 40–50 gemcitabine twice weekly × 4 Group B: 200–500 gemcitabine once weekly × 3 |
50.4–64.8 /28–36 |
n.r. | Ntotal: 6 Nweek: 1 |
n.r. | n.r. | Group A:Instant Group B: 60–180 |
HT after CT&RT |
|
| Gani et al. [164] | Locally advanced rectal cancer, n = 60 |
1000 5-fluorouracil × 4 |
50.4/28 | T90 ‡: 39.3 (37.1–40.6) | Ntotal
‡: 4 Nweek: 1–2 |
60 | CEM43°C ‡: 1.1 (0.0–9.2) |
n.r. | n.r. |
|
| Merten et al. [165] | Bladder cancer, n = 79 |
20 cisplatin 5 times weekly × 2 600 5-fluorouracil 5 times weekly × 2 |
50.4–55.8/ 28–31 |
n.r. | Ntotal: 5–7 Nweek: 1 |
60 | n.r. | 0–60 | RT after concurrent CT&HT |
|
| van Haaren et al. [166] | Esophageal cancer, n = 29 |
50 paclitaxelonce weekly × 5 and carboplatin (AUC=2) once weekly × 5 |
41.4/23 | T90
†: 38.6 ± 0.5 T50 †: 39.2 ± 0.6 T10 †: 40.1 ± 0.8 |
Ntotal: 5 Nweek: 1 |
60 | n.r. | 0–60 | HT after CT & RT |
|
n: number of patients assigned to be treated with HT in combination with RT; †: mean value (±standard deviation) or mean value (range); ‡: median (range); 1 CR: complete response; 2 PR: partial response; 3 SD: stable disease; 4 LRC:locoregional control, 5 DMFS: distant metastasis-free survival; 6 OS: overall survival; 7 NC: no change; 8 DM: distant metastases; 9 LF: local failure; 10 DPFS: disease progression-free survival; 11 DFS:disease free survival; 12 mPR: partial remission with only residual microscopic tumor foci.
The optimal combination of CT, RT, and HT in a single framework is complex, be-cause so many biological processes underly the interactions between the three modalities. In addition, clinical factors often influence the optimal combination of RT and CT. A template with fundamental specifications for designing a clinical study with the trimodal treatment is proposed by Herman et al. [145].
Even though there is no consensus as to the optimal scheduling of trimodal treatment, clinical studies to date integrate HT in combination with daily RT and CT drugs based on the concept that CT should interact with both RT and HT. Scheduling CT weekly is most feasible in terms of maintaining an optimal tint between HT sessions, drug administration, and RT fraction [145].
The reason why cisplatin is most frequently used in trimodality regimens is less based on a specific interaction with heat, but rather on extensive evidence from phase III randomized trials showing that cisplatin potently improves the antitumor efficacy of radiotherapy, albeit at the cost of increased toxicity. Drug concentration has been shown to affect treatment response [146], as proven experimentally [147]. A phase I-II study reported that a higher cisplatin dose (50 mg/m2) in comparison with a lower dose (20–40 mg/m2) combined with RT and HT was positively correlated with CR [146]. Interestingly, overall survival between patients treated with two different CT regimes in combination with RT and HT did not differ [148]. However, the study was limited by the small size of the patient cohort. With reference to Table 11, clinical studies using trimodality treatment usually used conventional fractionation schemes with 1.8–2.0 Gy per fractions, leaving it largely unknown whether other schedules such as hypofractionation (>10 Gy per week or large single fractions) might be biologically more favorable. The total dose varied according to cancer type. In the case of cervical cancer, brachytherapy at high dose rate (HDR) or low dose rate (LDR) was applied to deliver the boost dose [149,150]. Furthermore, high or low total RT dose was reported to have an influence on CR rate when combined with 5-FU, leucovorin and HT [151]. In contrast to CT and RT treatment parameters, HT treatment parameters were frequently not reported. Thermometric parameters, such as temperature and thermal dose including tint, are reported but not set as fixed treatment requirements as there are no accepted reference values.
Disregarding the Arrhenius relationship of heating temperature and ttreat, Amichetti et al. [152] reported a short ttreat of 30 min with mean temperature range values of Tmax = 43.2 °C (41.5–44.5 °C) and Tmin = 40.1 °C (37–42 °C). This might explain why this study did not result in a higher CR rate in comparison to the previous study by Valdagni et al. [103]. A correlation of achieved temperature with treatment response such as disease-free interval to local relapse (DFILR) was reported in the study by Kouloulias et al. [153]. This study showed that the DFILR rate was greater in patients who achieved heating temperature T90 > 44 °C for longer than 16 min during HT treatment. No significant correlation of DFILR with mean values of temperature descriptor Tmin was confirmed. Referring to the last row in Table 7, Table 8, Table 9, Table 10, Table 11 and Table 12, the clinical endpoints among studies differ, which adds another level of complexity to generalizing the thermometric parameter correlations reported in studies.
Thermal dose was reported less frequently than temperature measurements, hence there is a lack of information about its predictive role for treatment response. In one study, thermal dose was directly and proportionally associated with CR, as patients who exhibited CR after treatment with a measured CEM43°CT90 of 4.6 min in comparison with patients with a PR and a CEM43°CT90 of only 2.0 min [146]. Recently, a prospective phase II study investigating neoadjuvant triplet therapy in patients with rectal cancer showed that patients achieving good local tumor regression had received a high thermal dose [154]. However, no threshold, only the mean of CEM 43 °C, was reported. The retrospective analysis of thermometric parameters of the prospective study by Harima et al. [149] showed that >1 min CEM43°CT90 is the threshold value which significantly correlates with treatment response (CR and disease-free survival rates). It also confirmed that CEM43°CT90 below 1 min are insufficient to achieve enhancement of RT and CT [155]. Unfortunately, no further analyses of the relationship between HT treatment parameters with clinical outcomes in studies using triplet therapy were reported.
Furthermore, the optimal interval between heat, radiation and anticancer drugs is still unclear. With reference to preclinical and clinical outcomes, tint affects the thermal enhancement effect of HT on both ionizing radiation and CT drugs. A particular interaction between HT and CT in terms of tint was reported according to properties of the CT drugs. A short tint between sequential HT and doxorubicin resulted in more rapid treatment response [153]. However, it is not clear whether the CT drug interacts primarily with RT only when administered on the same day or also during an extended time period. In the first scenario, CT and HT could typically be administered within a range of 1–6 h prior to RT to optimally exploit the biological interaction.
Moreover, the Ntotal was shown to be a prognostic factor for OS for bladder cancer patients treated with combined CT, RT, and HT followed by surgery [161]. In contrast, Gani et al. [164] reported that the number of HT sessions was not predictive for OS, DFS, LC, or distant metastasis-free survival. Neither did the sequencing of CT, HT, and RT in clinical reports follow a specific pattern. Preclinical studies are required to better understand the interaction of CT, RT, and heat and how they should be combined in future clinical trials.
7. Future Prospects
The main limitations of HT as a cancer treatment in current clinical practice are the need for better standardization of treatment protocols, up-to-date quality assurance guidelines that are widely applicable and dedicated planning systems to generate patient treatment plans. The wide variation of thermometric parameters derived from clinical studies indicate that HT treatment is currently delivered according to individual clinical center guidelines. Consequently, the comparison of clinical study outcomes is substantially hampered by the large degree of variation in treatment parameters. Regarding the data summarized in Table 6, Table 7, Table 8, Table 9, Table 10 and Table 11, apart from thermal dose and temperature measured during treatment, other thermometric parameters reported often include only ttreat, tint, or Nweek.
Monitoring and measuring temperature is one of the main challenges in routine clinical practice and has hindered the clinical expansion of HT. The future of HT in combination with RT and CT requires novel technical developments for the delivery and measurement of homogenous heating of the malignant tissues. Not all studies (Table 7, Table 8, Table 9, Table 10, Table 11 and Table 12) recorded temperatures in the region of the tumor. The process of inserting temperature probes to monitor and record the HT is considered invasive and uncomfortable, and sometimes the tumor site is inaccessible for the temperature probe. For example, Milani et al. [162] reported that even though the tumors were not deep-seated, intratumoral temperature measurements were only feasible in one of 24 patients, so no representative thermal doses could be reported. One of the non-invasive approaches currently under clinical evaluation is magnetic resonance thermometry (MRT) that provides 3-D temperature measurements. Hybrid MR/HT devices are currently installed in five European clinical centers.
Temperature measurements in anthropomorphic phantoms with MRT are accurate in comparison with thermistor probes [167], but clinical measurements are currently inaccurate in most pelvic and abdominal tumors [168]. The physiological changes in tissue microenvironment, patient movements, magnetic field drift over time, limited sensitivity in fatty tissues, and respiratory motion, including cardiac activity in regions of the pelvis and abdomen, hamper the accurate temperature measurement by MRT [168]. The temperature images from MRT systems contain image distortion, artifacts, and noise, leading to inaccurate temperature measurement, low temporal resolution, and low imaging to signal-to-noise ratio (SNR) [169]. The sources and solutions of image artifacts as a result of additional frequencies were described by Gellermann et al. [170]. Proton-resonance frequency shift (PRFS), apparent diffusion coefficient (ADC), longitudinal relaxation time (T1), transversal relaxation time (T2), and equilibrium magnetization (M0) are the imaging techniques used to exploit temperature-dependent parameters [170,171,172,173]. The PRFS technique is the most frequently used MRT method, even though it was shown that when there is a poor magnetic field homogeneity, ADC or T1 techniques are preferable [174]. However, the accuracy of temperature measurements was in the range of ±0.4 to ±0.5 °C between PRFS method and thermistor probe using a heterogeneous phantom [175]. A stronger correlation between MRT and thermistor probes was found in patients with soft tissue sarcomas of lower extremities and pelvis [176] in comparison with recurrent rectal carcinoma [177]. The successful implementation of MRT in clinical centers, as automated temperature feedback during the HT session, might have a considerable impact on clinical outcomes to deliver the desired heating and conform the heat distribution to spare healthy surrounding tissues. This could substantially help to standardize data collection and the analysis of thermometric parameters. Another experimental approach to monitoring treatment temperature during HT sessions is electrical impedance tomography (EIT) as recently reported in a simulation study by Poni et al. [178]. EIT captures the electrical conductivity of tissues depends on temperature elevation. For example, the multifrequency EIT technique detects the changes in conductivity due to perfusion increase induced by the change in temperature [179]. The accuracy of EIT for temperature measurements was reported to range from 1.5 °C to 5 °C [180]. The potential of EIT to monitor temperature in the cardiac thermal ablation field is being investigated [181]. This technique also holds promise for HT treatment. Both MRT and EIT may allow for improvement of the spatial homogeneity of heat to the cancer tissues.
The technological advances and standardization of international treatment protocols for different cancer types will improve the effectiveness and synergy of HT in combination with RT and/or CT. In line with this, there is a need for clinically accepted processes for the recording and reporting of thermometric data. This will allow for the inclusion of specific thermometric parameters in future clinical studies combining HT with RT and/or CT. For any future prospective study, it should be mandatory that thermometric parameters are recorded and some recommendations are available in the current guidelines [43,46]. The integration of thermometric parameters is one of the objectives of the HYPERBOOST (“Hyperthermia boosting the effect of Radiotherapy”) international consortium within the European Horizon 2020 Program MSCA-ITN. The HYPERBOOST network aims to create a novel treatment planning system, including the standardization of thermometric parameters derived from retrospective and prospective clinical trials.
8. Conclusions
In this review, we provide an extensive overview of thermometric parameters reported in prospective and retrospective clinical studies which applied HT in combination with RT and/or CT and their correlation with clinical outcome. It is recognized that there is a wide variety in the practice of HT between clinical centers, and we aimed to elucidate the use and reporting of thermometric parameters in different clinical settings. It emerged that the sequencing of HT and RT varies more than the sequencing of HT and CT. Only a few standards seem to exist with regard to the sequence of HT with RT and CT in a triplet for specific CT drug, RT fractionation and thermal dose. According to the evaluated studies, tint is a critical parameter in clinical routine, but no clinical reference values have been established. Of note, a constant ttreat of 60 min throughout the HT treatment course was described in most clinical studies. The most important parameter seems to be temperature itself, which correlates with thermal dose. Revealing the relationship between thermal dose and treatment response for different cancer entities in future clinical studies will lead to the improved application of heat to promote the synergistic actions of HT with RT and CT. We suggest that it become mandatory for new clinical study protocols to include the extensive recording and analysis of thermometric parameters for their validation and overall standardization of HT. This would allow for the definition of thermometric parameters, in particular of thresholds for temperature descriptors and thermal dose.
Author Contributions
Conceptualization, O.R. and P.G.; writing, A.A. and O.R.; writing— review and editing, A.A., O.R., D.P.V., P.G., D.M., H.C., E.O., O.J.O., S.R., P.W., R.A.H., E.P., S.B. and R.F.; visualization, A.A. and O.R.; supervision, H.C., R.F., O.R. and P.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research has received support from the European Union’s Horizon 2020 research and innovation programme under the Marie Skłodowska-Curie (MSCA-ITN) grant “Hyperboost” project, no. 955625.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wust P., Hildebrandt B., Sreenivasa G., Rau B., Gellermann J., Riess H., Felix R., Schlag P.M. Hyperthermia in combined treatment of cancer. Lancet Oncol. 2002;3:487–497. doi: 10.1016/S1470-2045(02)00818-5. [DOI] [PubMed] [Google Scholar]
- 2.Van der Zee J. Heating the patient: A promising approach? Ann. Oncol. 2002;13:1173–1184. doi: 10.1093/annonc/mdf280. [DOI] [PubMed] [Google Scholar]
- 3.Horsman M.R., Overgaard J. Hyperthermia: A potent enhancer of radiotherapy. Clin. Oncol. (R Coll. Radiol.) 2007;19:418–426. doi: 10.1016/j.clon.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 4.Engin K. Biological rationale and clinical experience with hyperthermia. Control Clin. Trials. 1996;17:316–342. doi: 10.1016/0197-2456(95)00078-X. [DOI] [PubMed] [Google Scholar]
- 5.Oei A.L., Vriend L.E., Crezee J., Franken N.A., Krawczyk P.M. Effects of hyperthermia on DNA repair pathways: One treatment to inhibit them all. Radiat. Oncol. 2015;10:165. doi: 10.1186/s13014-015-0462-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dewey W.C., Hopwood L.E., Sapareto S.A., Gerweck L.E. Cellular responses to combinations of hyperthermia and radiation. Radiology. 1977;123:463–474. doi: 10.1148/123.2.463. [DOI] [PubMed] [Google Scholar]
- 7.Overgaard J. Effect of hyperthermia on the hypoxic fraction in an experimental mammary carcinoma in vivo. Br. J. Radiol. 1981;54:245–249. doi: 10.1259/0007-1285-54-639-245. [DOI] [PubMed] [Google Scholar]
- 8.Oei A.L., Kok H.P., Oei S.B., Horsman M.R., Stalpers L.J.A., Franken N.A.P., Crezee J. Molecular and biological rationale of hyperthermia as radio- and chemosensitizer. Adv. Drug Deliv. Rev. 2020;163–164:84–97. doi: 10.1016/j.addr.2020.01.003. [DOI] [PubMed] [Google Scholar]
- 9.Dewhirst M.W., Vujaskovic Z., Jones E., Thrall D. Re-setting the biologic rationale for thermal therapy. Int. J. Hyperthermia. 2005;21:779–790. doi: 10.1080/02656730500271668. [DOI] [PubMed] [Google Scholar]
- 10.Lepock J.R. Role of nuclear protein denaturation and aggregation in thermal radiosensitization. Int. J. Hyperthermia. 2004;20:115–130. doi: 10.1080/02656730310001637334. [DOI] [PubMed] [Google Scholar]
- 11.Calderwood S.K., Theriault J.R., Gong J. How is the immune response affected by hyperthermia and heat shock proteins? Int. J. Hyperthermia. 2005;21:713–716. doi: 10.1080/02656730500340794. [DOI] [PubMed] [Google Scholar]
- 12.Repasky E.A., Evans S.S., Dewhirst M.W. Temperature matters! And why it should matter to tumor immunologists. Cancer Immunol. Res. 2013;1:210–216. doi: 10.1158/2326-6066.CIR-13-0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mukhopadhaya A., Mendecki J., Dong X., Liu L., Kalnicki S., Garg M., Alfieri A., Guha C. Localized hyperthermia combined with intratumoral dendritic cells induces systemic antitumor immunity. Cancer Res. 2007;67:7798–7806. doi: 10.1158/0008-5472.CAN-07-0203. [DOI] [PubMed] [Google Scholar]
- 14.Frey B., Weiss E.M., Rubner Y., Wunderlich R., Ott O.J., Sauer R., Fietkau R., Gaipl U.S. Old and new facts about hyperthermia-induced modulations of the immune system. Int. J. Hyperthermia. 2012;28:528–542. doi: 10.3109/02656736.2012.677933. [DOI] [PubMed] [Google Scholar]
- 15.Overgaard J. Simultaneous and sequential hyperthermia and radiation treatment of an experimental tumor and its surrounding normal tissue in vivo. Int. J. Radiat. Oncol. Biol. Phys. 1980;6:1507–1517. doi: 10.1016/0360-3016(80)90008-5. [DOI] [PubMed] [Google Scholar]
- 16.Henle K.J., Leeper D.B. Interaction of hyperthermia and radiation in CHO cells: Recovery kinetics. Radiat. Res. 1976;66:505–518. doi: 10.2307/3574455. [DOI] [PubMed] [Google Scholar]
- 17.Overgaard J., Suit H.D. Time-temperature relationship th hyperthermic treatment of malignant and normal tissue in vivo. Cancer Res. 1979;39:3248–3253. [PubMed] [Google Scholar]
- 18.Nielsen O.S., Overgaard J., Kamura T. Influence of thermotolerance on the interaction between hyperthermia and radiation in a solid tumour in vivo. Br. J. Radiol. 1983;56:267–273. doi: 10.1259/0007-1285-56-664-267. [DOI] [PubMed] [Google Scholar]
- 19.Roizin-Towle L., Pirro J.P. The response of human and rodent cells to hyperthermia. Int. J. Radiat. Oncol. Biol. Phys. 1991;20:751–756. doi: 10.1016/0360-3016(91)90018-Y. [DOI] [PubMed] [Google Scholar]
- 20.Dahl O., Mella O. Effect of timing and sequence of hyperthermia and cyclophosphamide on a neurogenic rat tumor (BT4A) in vivo. Cancer. 1983;52:983–987. doi: 10.1002/1097-0142(19830915)52:6<983::AID-CNCR2820520609>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 21.Sapareto S.A., Dewey W.C. Thermal dose determination in cancer therapy. Int. J. Radiat. Oncol. Biol. Phys. 1984;10:787–800. doi: 10.1016/0360-3016(84)90379-1. [DOI] [PubMed] [Google Scholar]
- 22.Van Leeuwen C.M., Oei A.L., Chin K., Crezee J., Bel A., Westermann A.M., Buist M.R., Franken N.A.P., Stalpers L.J.A., Kok H.P. A short time interval between radiotherapy and hyperthermia reduces in-field recurrence and mortality in women with advanced cervical cancer. Radiat. Oncol. 2017;12:75. doi: 10.1186/s13014-017-0813-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Overgaard J. Influence of sequence and interval on the biological response to combined hyperthermia and radiation. Natl. Cancer Inst. Monogr. 1982;61:325–332. [PubMed] [Google Scholar]
- 24.Kapp D.S., Petersen I.A., Cox R.S., Hahn G.M., Fessenden P., Prionas S.D., Lee E.R., Meyer J.L., Samulski T.V., Bagshaw M.A. Two or six hyperthermia treatments as an adjunct to radiation therapy yield similar tumor responses: Results of a randomized trial. Int. J. Radiat. Oncol. Biol. Phys. 1990;19:1481–1495. doi: 10.1016/0360-3016(90)90361-M. [DOI] [PubMed] [Google Scholar]
- 25.Arcangeli G., Nervi C., Cividalli A., Lovisolo G.A. Problem of sequence and fractionation in the clinical application of combined heat and radiation. Cancer Res. 1984;44:4857s–4863s. [PubMed] [Google Scholar]
- 26.Gerweck L.E., Gillette E.L., Dewey W.C. Effect of heat and radiation on synchronous Chinese hamster cells: Killing and repair. Radiat. Res. 1975;64:611–623. doi: 10.2307/3574251. [DOI] [PubMed] [Google Scholar]
- 27.Pauwels B., Korst A.E., Lardon F., Vermorken J.B. Combined modality therapy of gemcitabine and radiation. Oncologist. 2005;10:34–51. doi: 10.1634/theoncologist.10-1-34. [DOI] [PubMed] [Google Scholar]
- 28.Ohtsubo T., Saito H., Tanaka N., Matsumoto H., Sugimoto C., Saito T., Hayashi S., Kano E. Enhancement of cisplatin sensitivity and platinum uptake by 40 degrees C hyperthermia in resistant cells. Cancer Lett. 1997;119:47–52. doi: 10.1016/S0304-3835(97)00250-4. [DOI] [PubMed] [Google Scholar]
- 29.Oleson J.R., Sim D.A., Manning M.R. Analysis of prognostic variables in hyperthermia treatment of 161 patients. Int. J. Radiat. Oncol. Biol. Phys. 1984;10:2231–2239. doi: 10.1016/0360-3016(84)90228-1. [DOI] [PubMed] [Google Scholar]
- 30.Cox R.S., Kapp D.S. Correlation of thermal parameters with outcome in combined radiation therapy-hyperthermia trials. Int. J. Hyperthermia. 1992;8:719–732. doi: 10.3109/02656739209005020. [DOI] [PubMed] [Google Scholar]
- 31.Dewhirst M.W., Sim D.A. The utility of thermal dose as a predictor of tumor and normal tissue responses to combined radiation and hyperthermia. Cancer Res. 1984;44:4772s–4780s. [PubMed] [Google Scholar]
- 32.Leopold K.A., Dewhirst M., Samulski T., Harrelson J., Tucker J.A., George S.L., Dodge R.K., Grant W., Clegg S., Prosnitz L.R., et al. Relationships among tumor temperature, treatment time, and histopathological outcome using preoperative hyperthermia with radiation in soft tissue sarcomas. Int. J. Radiat. Oncol. Biol. Phys. 1992;22:989–998. doi: 10.1016/0360-3016(92)90798-M. [DOI] [PubMed] [Google Scholar]
- 33.Kroesen M., Mulder H.T., van Holthe J.M.L., Aangeenbrug A.A., Mens J.W.M., van Doorn H.C., Paulides M.M., Oomen-de Hoop E., Vernhout R.M., Lutgens L.C., et al. The Effect of the Time Interval Between Radiation and Hyperthermia on Clinical Outcome in 400 Locally Advanced Cervical Carcinoma Patients. Front. Oncol. 2019;9:134. doi: 10.3389/fonc.2019.00134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crezee J., Oei A.L., Franken N.A.P., Stalpers L.J.A., Kok H.P. Response: Commentary: The Impact of the Time Interval Between Radiation and Hyperthermia on Clinical Outcome in Patients With Locally Advanced Cervical Cancer. Front. Oncol. 2020;10:528. doi: 10.3389/fonc.2020.00528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jones E.L., Oleson J.R., Prosnitz L.R., Samulski T.V., Vujaskovic Z., Yu D., Sanders L.L., Dewhirst M.W. Randomized trial of hyperthermia and radiation for superficial tumors. J. Clin. Oncol. 2005;23:3079–3085. doi: 10.1200/JCO.2005.05.520. [DOI] [PubMed] [Google Scholar]
- 36.Franckena M., Fatehi D., de Bruijne M., Canters R.A., van Norden Y., Mens J.W., van Rhoon G.C., van der Zee J. Hyperthermia dose-effect relationship in 420 patients with cervical cancer treated with combined radiotherapy and hyperthermia. Eur. J. Cancer. 2009;45:1969–1978. doi: 10.1016/j.ejca.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 37.Kapp D.S., Cox R.S. Thermal treatment parameters are most predictive of outcome in patients with single tumor nodules per treatment field in recurrent adenocarcinoma of the breast. Int. J. Radiat. Oncol. Biol. Phys. 1995;33:887–899. doi: 10.1016/0360-3016(95)00212-4. [DOI] [PubMed] [Google Scholar]
- 38.Oleson J.R., Samulski T.V., Leopold K.A., Clegg S.T., Dewhirst M.W., Dodge R.K., George S.L. Sensitivity of hyperthermia trial outcomes to temperature and time: Implications for thermal goals of treatment. Int. J. Radiat. Oncol. Biol. Phys. 1993;25:289–297. doi: 10.1016/0360-3016(93)90351-U. [DOI] [PubMed] [Google Scholar]
- 39.Sherar M., Liu F.F., Pintilie M., Levin W., Hunt J., Hill R., Hand J., Vernon C., van Rhoon G., van der Zee J., et al. Relationship between thermal dose and outcome in thermoradiotherapy treatments for superficial recurrences of breast cancer: Data from a phase III trial. Int. J. Radiat. Oncol. Biol. Phys. 1997;39:371–380. doi: 10.1016/S0360-3016(97)00333-7. [DOI] [PubMed] [Google Scholar]
- 40.Leopold K.A., Dewhirst M.W., Samulski T.V., Dodge R.K., George S.L., Blivin J.L., Prosnitz L.R., Oleson J.R. Cumulative minutes with T90 greater than Tempindex is predictive of response of superficial malignancies to hyperthermia and radiation. Int. J. Radiat. Oncol. Biol. Phys. 1993;25:841–847. doi: 10.1016/0360-3016(93)90314-L. [DOI] [PubMed] [Google Scholar]
- 41.Dinges S., Harder C., Wurm R., Buchali A., Blohmer J., Gellermann J., Wust P., Randow H., Budach V. Combined treatment of inoperable carcinomas of the uterine cervix with radiotherapy and regional hyperthermia. Results of a phase II trial. Strahlenther. Onkol. 1998;174:517–521. doi: 10.1007/BF03038984. [DOI] [PubMed] [Google Scholar]
- 42.Bakker A., van der Zee J., van Tienhoven G., Kok H.P., Rasch C.R.N., Crezee H. Temperature and thermal dose during radiotherapy and hyperthermia for recurrent breast cancer are related to clinical outcome and thermal toxicity: A systematic review. Int. J. Hyperthermia. 2019;36:1024–1039. doi: 10.1080/02656736.2019.1665718. [DOI] [PubMed] [Google Scholar]
- 43.Trefná H.D., Crezee H., Schmidt M., Marder D., Lamprecht U., Ehmann M., Hartmann J., Nadobny J., Gellermann J., van Holthe N., et al. Quality assurance guidelines for superficial hyperthermia clinical trials: I. Clinical requirements. Int. J. Hyperthermia. 2017;33:471–482. doi: 10.1080/02656736.2016.1277791. [DOI] [PubMed] [Google Scholar]
- 44.Paulides M.M., Dobsicek Trefna H., Curto S., Rodrigues D.B. Recent technological advancements in radiofrequency- and microwave-mediated hyperthermia for enhancing drug delivery. Adv. Drug Deliv. Rev. 2020;163–164:3–18. doi: 10.1016/j.addr.2020.03.004. [DOI] [PubMed] [Google Scholar]
- 45.Kok H.P., Crezee J. A comparison of the heating characteristics of capacitive and radiative superficial hyperthermia. Int. J. Hyperthermia. 2017;33:378–386. doi: 10.1080/02656736.2016.1268726. [DOI] [PubMed] [Google Scholar]
- 46.Bruggmoser G., Bauchowitz S., Canters R., Crezee H., Ehmann M., Gellermann J., Lamprecht U., Lomax N., Messmer M.B., Ott O., et al. Guideline for the clinical application, documentation and analysis of clinical studies for regional deep hyperthermia: Quality management in regional deep hyperthermia. Strahlenther. Onkol. 2012;188((Suppl. 2)):198–211. doi: 10.1007/s00066-012-0176-2. [DOI] [PubMed] [Google Scholar]
- 47.Dobšíček Trefná H., Crezee J., Schmidt M., Marder D., Lamprecht U., Ehmann M., Nadobny J., Hartmann J., Lomax N., Abdel-Rahman S., et al. Quality assurance guidelines for superficial hyperthermia clinical trials: II. Technical requirements for heating devices. Strahlenther. Onkol. 2017;193:351–366. doi: 10.1007/s00066-017-1106-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kroeze H., Kokubo M., Kamer J.B.V.D., Leeuw A.A.C.D., Kikuchi M., Hiraoka M., Lagendijk J.J.W. Comparison of a Capacitive and a Cavity Slot Radiative Applicator for Regional Hyperthermia. Therm. Med. (Jpn. J. Hyperthermic Oncol.) 2002;18:75–91. doi: 10.3191/thermalmedicine.18.75. [DOI] [Google Scholar]
- 49.Datta N.R., Marder D., Datta S., Meister A., Puric E., Stutz E., Rogers S., Eberle B., Timm O., Staruch M., et al. Quantification of thermal dose in moderate clinical hyperthermia with radiotherapy: A relook using temperature-time area under the curve (AUC) Int. J. Hyperthermia. 2021;38:296–307. doi: 10.1080/02656736.2021.1875060. [DOI] [PubMed] [Google Scholar]
- 50.Fatehi D., van der Zee J., Notenboom A., van Rhoon G.C. Comparison of intratumor and intraluminal temperatures during locoregional deep hyperthermia of pelvic tumors. Strahlenther. Onkol. 2007;183:479–486. doi: 10.1007/s00066-007-1768-0. [DOI] [PubMed] [Google Scholar]
- 51.Fatehi D., de Bruijne M., van der Zee J., van Rhoon G.C. RHyThM, a tool for analysis of PDOS formatted hyperthermia treatment data generated by the BSD2000/3D system. Int. J. Hyperthermia. 2006;22:173–184. doi: 10.1080/02656730600597459. [DOI] [PubMed] [Google Scholar]
- 52.Overgaard J. Formula to estimate the thermal enhancement ratio of a single simultaneous hyperthermia and radiation treatment. Acta Radiol. Oncol. 1984;23:135–139. doi: 10.3109/02841868409136001. [DOI] [PubMed] [Google Scholar]
- 53.Song C.W., Park H., Griffin R.J. Improvement of tumor oxygenation by mild hyperthermia. Radiat. Res. 2001;155:515–528. doi: 10.1667/0033-7587(2001)155[0515:IOTOBM]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 54.Overgaard J., Radacic M.M., Grau C. Interaction of hyperthermia and cis-diamminedichloroplatinum(II) alone or combined with radiation in a C3H mammary carcinoma in vivo. Cancer Res. 1991;51:707–711. [PubMed] [Google Scholar]
- 55.Lindegaard J.C., Radacic M., Khalil A.A., Horsman M.R., Overgaard J. Cisplatin and hyperthermia treatment of a C3H mammary carcinoma in vivo. Importance of sequence, interval, drug dose, and temperature. Acta Oncol. 1992;31:347–351. doi: 10.3109/02841869209108184. [DOI] [PubMed] [Google Scholar]
- 56.Hintzsche H., Riese T., Stopper H. Hyperthermia-induced micronucleus formation in a human keratinocyte cell line. Mutat. Res. 2012;738–739:71–74. doi: 10.1016/j.mrfmmm.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 57.Urano M., Ling C.C. Thermal enhancement of melphalan and oxaliplatin cytotoxicity in vitro. Int. J. Hyperthermia. 2002;18:307–315. doi: 10.1080/02656730210123534. [DOI] [PubMed] [Google Scholar]
- 58.Kampinga H.H., Dynlacht J.R., Dikomey E. Mechanism of radiosensitization by hyperthermia (> or = 43 degrees C) as derived from studies with DNA repair defective mutant cell lines. Int. J. Hyperthermia. 2004;20:131–139. doi: 10.1080/02656730310001627713. [DOI] [PubMed] [Google Scholar]
- 59.Kampinga H.H. Cell biological effects of hyperthermia alone or combined with radiation or drugs: A short introduction to newcomers in the field. Int. J. Hyperthermia. 2006;22:191–196. doi: 10.1080/02656730500532028. [DOI] [PubMed] [Google Scholar]
- 60.Ohtsubo T., Chang S.W., Tsuji K., Picha P., Saito H., Kano E. Effects of cis-diamminedichloroplatinum (CDDP) and cis-diammine (1,1-cyclobutanedicarboxylate) platinum (CBDCA) on thermotolerance development and thermosensitivity of the thermotolerant cells. Int. J. Hyperthermia. 1990;6:1031–1039. doi: 10.3109/02656739009140986. [DOI] [PubMed] [Google Scholar]
- 61.Van der Zee J., Peer-Valstar J.N., Rietveld P.J., de Graaf-Strukowska L., van Rhoon G.C. Practical limitations of interstitial thermometry during deep hyperthermia. Int. J. Radiat. Oncol. Biol. Phys. 1998;40:1205–1212. doi: 10.1016/S0360-3016(98)00008-X. [DOI] [PubMed] [Google Scholar]
- 62.Oleson J.R. Eugene Robertson Special Lecture. Hyperthermia from the clinic to the laboratory: A hypothesis. Int. J. Hyperthermia. 1995;11:315–322. doi: 10.3109/02656739509022467. [DOI] [PubMed] [Google Scholar]
- 63.Sapareto S.A., Hopwood L.E., Dewey W.C., Raju M.R., Gray J.W. Effects of hyperthermia on survival and progression of Chinese hamster ovary cells. Cancer Res. 1978;38:393–400. [PubMed] [Google Scholar]
- 64.Bing C., Patel P., Staruch R.M., Shaikh S., Nofiele J., Wodzak Staruch M., Szczepanski D., Williams N.S., Laetsch T., Chopra R. Longer heating duration increases localized doxorubicin deposition and therapeutic index in Vx2 tumors using MR-HIFU mild hyperthermia and thermosensitive liposomal doxorubicin. Int. J. Hyperthermia. 2019;36:196–203. doi: 10.1080/02656736.2018.1550815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bhuyan B.K., Day K.J., Edgerton C.E., Ogunbase O. Sensitivity of different cell lines and of different phases in the cell cycle to hyperthermia. Cancer Res. 1977;37:3780–3784. [PubMed] [Google Scholar]
- 66.Dewey W.C. Arrhenius relationships from the molecule and cell to the clinic. Int. J. Hyperthermia. 2009;25:3–20. doi: 10.1080/02656730902747919. [DOI] [PubMed] [Google Scholar]
- 67.Law M.P. Induced thermal resistance in the mouse ear: The relationship between heating time and temperature. Int. J. Radiat. Biol. Relat. Stud. Phys. Chem. Med. 1979;35:481–485. doi: 10.1080/09553007914550581. [DOI] [PubMed] [Google Scholar]
- 68.Li G.C., Mivechi N.F., Weitzel G. Heat shock proteins, thermotolerance, and their relevance to clinical hyperthermia. Int. J. Hyperthermia. 1995;11:459–488. doi: 10.3109/02656739509022483. [DOI] [PubMed] [Google Scholar]
- 69.Field S.B., Morris C.C. The relationship between heating time and temperature: Its relevance to clinical hyperthermia. Radiother. Oncol. 1983;1:179–186. doi: 10.1016/S0167-8140(83)80020-6. [DOI] [PubMed] [Google Scholar]
- 70.Dewhirst M.W., Viglianti B.L., Lora-Michiels M., Hanson M., Hoopes P.J. Basic principles of thermal dosimetry and thermal thresholds for tissue damage from hyperthermia. Int. J. Hyperthermia. 2003;19:267–294. doi: 10.1080/0265673031000119006. [DOI] [PubMed] [Google Scholar]
- 71.Nielsen O.S. Fractionated hyperthermia and thermotolerance. Experimental studies on heat-induced resistance in tumour cells treated with hyperthermia alone or in combination with radiotherapy. Dan. Med. Bull. 1984;31:376–390. [PubMed] [Google Scholar]
- 72.Ben-Hur E., Elkind M.M., Bronk B.V. Thermally enhanced radioresponse of cultured Chinese hamster cells: Inhibition of repair of sublethal damage and enhancement of lethal damage. Radiat. Res. 1974;58:38–51. doi: 10.2307/3573947. [DOI] [PubMed] [Google Scholar]
- 73.Van Rhoon G.C., Samaras T., Yarmolenko P.S., Dewhirst M.W., Neufeld E., Kuster N. CEM43°C thermal dose thresholds: A potential guide for magnetic resonance radiofrequency exposure levels? Eur. Radiol. 2013;23:2215–2227. doi: 10.1007/s00330-013-2825-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yarmolenko P.S., Moon E.J., Landon C., Manzoor A., Hochman D.W., Viglianti B.L., Dewhirst M.W. Thresholds for thermal damage to normal tissues: An update. Int. J. Hyperthermia. 2011;27:320–343. doi: 10.3109/02656736.2010.534527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Thrall D.E., LaRue S.M., Yu D., Samulski T., Sanders L., Case B., Rosner G., Azuma C., Poulson J., Pruitt A.F., et al. Thermal dose is related to duration of local control in canine sarcomas treated with thermoradiotherapy. Clin. Cancer Res. 2005;11:5206–5214. doi: 10.1158/1078-0432.CCR-05-0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kossatz S., Ludwig R., Dähring H., Ettelt V., Rimkus G., Marciello M., Salas G., Patel V., Teran F.J., Hilger I. High therapeutic efficiency of magnetic hyperthermia in xenograft models achieved with moderate temperature dosages in the tumor area. Pharm. Res. 2014;31:3274–3288. doi: 10.1007/s11095-014-1417-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dewhirst M.W., Sim D.A., Sapareto S., Connor W.G. Importance of minimum tumor temperature in determining early and long-term responses of spontaneous canine and feline tumors to heat and radiation. Cancer Res. 1984;44:43–50. [PubMed] [Google Scholar]
- 78.Van Rhoon G.C. Is CEM43 still a relevant thermal dose parameter for hyperthermia treatment monitoring? Int. J. Hyperthermia. 2016;32:50–62. doi: 10.3109/02656736.2015.1114153. [DOI] [PubMed] [Google Scholar]
- 79.Gerner E.W., Boone R., Connor W.G., Hicks J.A., Boone M.L. A transient thermotolerant survival response produced by single thermal doses in HeLa cells. Cancer Res. 1976;36:1035–1040. [PubMed] [Google Scholar]
- 80.Li Z., Sun Q., Huang X., Zhang J., Hao J., Li Y., Zhang S. The Efficacy of Radiofrequency Hyperthermia Combined with Chemotherapy in the Treatment of Advanced Ovarian Cancer. Open Med. 2018;13:83–89. doi: 10.1515/med-2018-0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kamura T., Nielsen O.S., Overgaard J., Andersen A.H. Development of thermotolerance during fractionated hyperthermia in a solid tumor in vivo. Cancer Res. 1982;42:1744–1748. [PubMed] [Google Scholar]
- 82.Zywietz F., Reeker W., Kochs E. Changes in tumor oxygenation during a combined treatment with fractionated irradiation and hyperthermia: An experimental study. Int. J. Radiat. Oncol. Biol. Phys. 1997;37:155–162. doi: 10.1016/S0360-3016(96)00465-8. [DOI] [PubMed] [Google Scholar]
- 83.Nah B.S., Choi I.B., Oh W.Y., Osborn J.L., Song C.W. Vascular thermal adaptation in tumors and normal tissue in rats. Int. J. Radiat. Oncol. Biol. Phys. 1996;35:95–101. doi: 10.1016/S0360-3016(96)85016-4. [DOI] [PubMed] [Google Scholar]
- 84.Overgaard J., Nielsen O.S. The importance of thermotolerance for the clinical treatment with hyperthermia. Radiother. Oncol. 1983;1:167–178. doi: 10.1016/S0167-8140(83)80019-X. [DOI] [PubMed] [Google Scholar]
- 85.Mei X., Ten Cate R., van Leeuwen C.M., Rodermond H.M., de Leeuw L., Dimitrakopoulou D., Stalpers L.J.A., Crezee J., Kok H.P., Franken N.A.P., et al. Radiosensitization by Hyperthermia: The Effects of Temperature, Sequence, and Time Interval in Cervical Cell Lines. Cancers. 2020;12:582. doi: 10.3390/cancers12030582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Notter M., Piazena H., Vaupel P. Hypofractionated re-irradiation of large-sized recurrent breast cancer with thermography-controlled, contact-free water-filtered infra-red-A hyperthermia: A retrospective study of 73 patients. Int. J. Hyperthermia. 2017;33:227–236. doi: 10.1080/02656736.2016.1235731. [DOI] [PubMed] [Google Scholar]
- 87.Hurwitz M., Stauffer P. Hyperthermia, radiation and chemotherapy: The role of heat in multidisciplinary cancer care. Semin. Oncol. 2014;41:714–729. doi: 10.1053/j.seminoncol.2014.09.014. [DOI] [PubMed] [Google Scholar]
- 88.Joschko M.A., Webster L.K., Groves J., Yuen K., Palatsides M., Ball D.L., Millward M.J. Enhancement of radiation-induced regrowth delay by gemcitabine in a human tumor xenograft model. Radiat. Oncol. Investig. 1997;5:62–71. doi: 10.1002/(SICI)1520-6823(1997)5:2<62::AID-ROI4>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 89.Van Bree C., Beumer C., Rodermond H.M., Haveman J., Bakker P.J. Effectiveness of 2’,2’difluorodeoxycytidine (Gemcitabine) combined with hyperthermia in rat R-1 rhabdomyosarcoma in vitro and in vivo. Int. J. Hyperthermia. 1999;15:549–556. doi: 10.1080/026567399285530. [DOI] [PubMed] [Google Scholar]
- 90.Li G.C., Kal H.B. Effect of hyperthermia on the radiation response of two mammalian cell lines. Eur. J. Cancer. 1977;13:65–69. doi: 10.1016/0014-2964(77)90231-6. [DOI] [PubMed] [Google Scholar]
- 91.Chen H., Ma G., Wang X., Zhou W., Wang S. Time interval after heat stress plays an important role in the combination therapy of hyperthermia and cancer chemotherapy agents. Int. J. Hyperthermia. 2020;37:254–255. doi: 10.1080/02656736.2020.1736343. [DOI] [PubMed] [Google Scholar]
- 92.Mitsumori M., Zeng Z.F., Oliynychenko P., Park J.H., Choi I.B., Tatsuzaki H., Tanaka Y., Hiraoka M. Regional hyperthermia combined with radiotherapy for locally advanced non-small cell lung cancers: A multi-institutional prospective randomized trial of the International Atomic Energy Agency. Int. J. Clin. Oncol. 2007;12:192–198. doi: 10.1007/s10147-006-0647-5. [DOI] [PubMed] [Google Scholar]
- 93.Wust P., Gellermann J., Harder C., Tilly W., Rau B., Dinges S., Schlag P., Budach V., Felix R. Rationale for using invasive thermometry for regional hyperthermia of pelvic tumors. Int. J. Radiat. Oncol. Biol. Phys. 1998;41:1129–1137. doi: 10.1016/S0360-3016(98)00165-5. [DOI] [PubMed] [Google Scholar]
- 94.Ohguri T., Imada H., Yahara K., Morioka T., Nakano K., Terashima H., Korogi Y. Radiotherapy with 8-MHz radiofrequency-capacitive regional hyperthermia for stage III non-small-cell lung cancer: The radiofrequency-output power correlates with the intraesophageal temperature and clinical outcomes. Int. J. Radiat. Oncol. Biol. Phys. 2009;73:128–135. doi: 10.1016/j.ijrobp.2008.03.059. [DOI] [PubMed] [Google Scholar]
- 95.Ohguri T., Yahara K., Moon S.D., Yamaguchi S., Imada H., Terashima H., Korogi Y. Deep regional hyperthermia for the whole thoracic region using 8 MHz radiofrequency-capacitive heating device: Relationship between the radiofrequency-output power and the intra-oesophageal temperature and predictive factors for a good heating in 59 patients. Int. J. Hyperthermia. 2011;27:20–26. doi: 10.3109/02656736.2010.500644. [DOI] [PubMed] [Google Scholar]
- 96.Chi M.S., Yang K.L., Chang Y.C., Ko H.L., Lin Y.H., Huang S.C., Huang Y.Y., Liao K.W., Kondo M., Chi K.H. Comparing the Effectiveness of Combined External Beam Radiation and Hyperthermia Versus External Beam Radiation Alone in Treating Patients With Painful Bony Metastases: A Phase 3 Prospective, Randomized, Controlled Trial. Int. J. Radiat. Oncol. Biol. Phys. 2018;100:78–87. doi: 10.1016/j.ijrobp.2017.09.030. [DOI] [PubMed] [Google Scholar]
- 97.Nishimura Y., Hiraoka M., Akuta K., Jo S., Nagata Y., Masunaga S., Takahashi M., Abe M. Hyperthermia combined with radiation therapy for primarily unresectable and recurrent colorectal cancer. Int. J. Radiat. Oncol. Biol. Phys. 1992;23:759–768. doi: 10.1016/0360-3016(92)90649-3. [DOI] [PubMed] [Google Scholar]
- 98.Engin K., Tupchong L., Moylan D.J., Alexander G.A., Waterman F.M., Komarnicky L., Nerlinger R.E., Leeper D.B. Randomized trial of one versus two adjuvant hyperthermia treatments per week in patients with superficial tumours. Int. J. Hyperthermia. 1993;9:327–340. doi: 10.3109/02656739309005034. [DOI] [PubMed] [Google Scholar]
- 99.Tilly W., Gellermann J., Graf R., Hildebrandt B., Weissbach L., Budach V., Felix R., Wust P. Regional hyperthermia in conjunction with definitive radiotherapy against recurrent or locally advanced prostate cancer T3 pN0 M0. Strahlenther. Onkol. 2005;181:35–41. doi: 10.1007/s00066-005-1296-8. [DOI] [PubMed] [Google Scholar]
- 100.Masunaga S.I., Hiraoka M., Akuta K., Nishimura Y., Nagata Y., Jo S., Takahashi M., Abe M., Terachi T., Oishi K., et al. Phase I/II trial of preoperative thermoradiotherapy in the treatment of urinary bladder cancer. Int. J. Hyperthermia. 1994;10:31–40. doi: 10.3109/02656739409009329. [DOI] [PubMed] [Google Scholar]
- 101.Valdagni R., Liu F.F., Kapp D.S. Important prognostic factors influencing outcome of combined radiation and hyperthermia. Int. J. Radiat. Oncol. Biol. Phys. 1988;15:959–972. doi: 10.1016/0360-3016(88)90133-2. [DOI] [PubMed] [Google Scholar]
- 102.Kroesen M., Mulder H.T., van Holthe J.M.L., Aangeenbrug A.A., Mens J.W.M., van Doorn H.C., Paulides M.M., Oomen-de Hoop E., Vernhout R.M., Lutgens L.C., et al. Confirmation of thermal dose as a predictor of local control in cervical carcinoma patients treated with state-of-the-art radiation therapy and hyperthermia. Radiother. Oncol. 2019;140:150–158. doi: 10.1016/j.radonc.2019.06.021. [DOI] [PubMed] [Google Scholar]
- 103.Valdagni R., Amichetti M. Report of long-term follow-up in a randomized trial comparing radiation therapy and radiation therapy plus hyperthermia to metastatic lymph nodes in stage IV head and neck patients. Int. J. Radiat. Oncol. Biol. Phys. 1994;28:163–169. doi: 10.1016/0360-3016(94)90154-6. [DOI] [PubMed] [Google Scholar]
- 104.Van der Zee J., González González D., van Rhoon G.C., van Dijk J.D., van Putten W.L., Hart A.A., Dutch Deep Hyperthermia Group Comparison of radiotherapy alone with radiotherapy plus hyperthermia in locally advanced pelvic tumours: A prospective, randomised, multicentre trial. Lancet. 2000;355:1119–1125. doi: 10.1016/S0140-6736(00)02059-6. [DOI] [PubMed] [Google Scholar]
- 105.Harima Y., Nagata K., Harima K., Ostapenko V.V., Tanaka Y., Sawada S. A randomized clinical trial of radiation therapy versus thermoradiotherapy in stage IIIB cervical carcinoma. Int. J. Hyperthermia. 2001;17:97–105. doi: 10.1080/02656730903092018. [DOI] [PubMed] [Google Scholar]
- 106.Berdov B.A., Menteshashvili G.Z. Thermoradiotherapy of patients with locally advanced carcinoma of the rectum. Int. J. Hyperthermia. 1990;6:881–890. doi: 10.3109/02656739009140970. [DOI] [PubMed] [Google Scholar]
- 107.Maluta S., Dall’Oglio S., Romano M., Marciai N., Pioli F., Giri M.G., Benecchi P.L., Comunale L., Porcaro A.B. Conformal radiotherapy plus local hyperthermia in patients affected by locally advanced high risk prostate cancer: Preliminary results of a prospective phase II study. Int. J. Hyperthermia. 2007;23:451–456. doi: 10.1080/02656730701553260. [DOI] [PubMed] [Google Scholar]
- 108.Anscher M.S., Samulski T.V., Dodge R., Prosnitz L.R., Dewhirst M.W. Combined external beam irradiation and external regional hyperthermia for locally advanced adenocarcinoma of the prostate. Int. J. Radiat. Oncol. Biol. Phys. 1997;37:1059–1065. doi: 10.1016/S0360-3016(97)00109-0. [DOI] [PubMed] [Google Scholar]
- 109.Gabriele P., Amichetti M., Orecchia R., Valdagni R. Hyperthermia and radiation therapy for inoperable or recurrent parotid carcinoma. A phase I/II study. Cancer. 1995;75:908–913. doi: 10.1002/1097-0142(19950215)75:4<908::AID-CNCR2820750403>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 110.Maguire P.D., Samulski T.V., Prosnitz L.R., Jones E.L., Rosner G.L., Powers B., Layfield L.W., Brizel D.M., Scully S.P., Harrelson J.M., et al. A phase II trial testing the thermal dose parameter CEM43 degrees T90 as a predictor of response in soft tissue sarcomas treated with pre-operative thermoradiotherapy. Int. J. Hyperthermia. 2001;17:283–290. doi: 10.1080/02656730110039449. [DOI] [PubMed] [Google Scholar]
- 111.Lutgens L.C., Koper P.C., Jobsen J.J., van der Steen-Banasik E.M., Creutzberg C.L., van den Berg H.A., Ottevanger P.B., van Rhoon G.C., van Doorn H.C., Houben R., et al. Radiation therapy combined with hyperthermia versus cisplatin for locally advanced cervical cancer: Results of the randomized RADCHOC trial. Radiother. Oncol. 2016;120:378–382. doi: 10.1016/j.radonc.2016.02.010. [DOI] [PubMed] [Google Scholar]
- 112.Hurwitz M.D., Hansen J.L., Prokopios-Davos S., Manola J., Wang Q., Bornstein B.A., Hynynen K., Kaplan I.D. Hyperthermia combined with radiation for the treatment of locally advanced prostate cancer: Long-term results from Dana-Farber Cancer Institute study 94-153. Cancer. 2011;117:510–516. doi: 10.1002/cncr.25619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Vernon C.C., Hand J.W., Field S.B., Machin D., Whaley J.B., van der Zee J., van Putten W.L., van Rhoon G.C., van Dijk J.D., González González D., et al. Radiotherapy with or without hyperthermia in the treatment of superficial localized breast cancer: Results from five randomized controlled trials. International Collaborative Hyperthermia Group. Int. J. Radiat. Oncol. Biol. Phys. 1996;35:731–744. doi: 10.1016/0360-3016(96)00154-x. [DOI] [PubMed] [Google Scholar]
- 114.Datta N.R., Bose A.K., Kapoor H.K., Gupta S. Head and neck cancers: Results of thermoradiotherapy versus radiotherapy. Int. J. Hyperthermia. 1990;6:479–486. doi: 10.3109/02656739009140944. [DOI] [PubMed] [Google Scholar]
- 115.Overgaard J., Gonzalez Gonzalez D., Hulshof M.C., Arcangeli G., Dahl O., Mella O., Bentzen S.M. Randomised trial of hyperthermia as adjuvant to radiotherapy for recurrent or metastatic malignant melanoma. European Society for Hyperthermic Oncology. Lancet. 1995;345:540–543. doi: 10.1016/S0140-6736(95)90463-8. [DOI] [PubMed] [Google Scholar]
- 116.Overgaard J., Gonzalez Gonzalez D., Hulshof M.C., Arcangeli G., Dahl O., Mella O., Bentzen S.M. Hyperthermia as an adjuvant to radiation therapy of recurrent or metastatic malignant melanoma. A multicentre randomized trial by the European Society for Hyperthermic Oncology. Int. J. Hyperthermia. 1996;12:3–20. doi: 10.3109/02656739609023685. [DOI] [PubMed] [Google Scholar]
- 117.Kim B.S., Chung H.C., Seong J.S., Suh C.O., Kim G.E. Phase II trial for combined external radiotherapy and hyperthermia for unresectable hepatoma. Cancer Chemother. Pharmacol. 1992;31:S119–S127. doi: 10.1007/BF00687121. [DOI] [PubMed] [Google Scholar]
- 118.Overgaard J., Overgaard M., Hansen P.V., von der Maase H. Some factors of importance in the radiation treatment of malignant melanoma. Radiother. Oncol. 1986;5:183–192. doi: 10.1016/S0167-8140(86)80048-2. [DOI] [PubMed] [Google Scholar]
- 119.Emami B., Perez C.A., Konefal J., Pilepich M.V., Leybovich L., Straube W., VonGerichten D., Hederman M.A. Thermoradiotherapy of malignant melanoma. Int. J. Hyperthermia. 1988;4:373–381. doi: 10.3109/02656738809016491. [DOI] [PubMed] [Google Scholar]
- 120.Franckena M., Lutgens L.C., Koper P.C., Kleynen C.E., van der Steen-Banasik E.M., Jobsen J.J., Leer J.W., Creutzberg C.L., Dielwart M.F., van Norden Y., et al. Radiotherapy and hyperthermia for treatment of primary locally advanced cervix cancer: Results in 378 patients. Int. J. Radiat. Oncol. Biol. Phys. 2009;73:242–250. doi: 10.1016/j.ijrobp.2008.03.072. [DOI] [PubMed] [Google Scholar]
- 121.Oldenborg S., Van Os R.M., Van rij C.M., Crezee J., Van de Kamer J.B., Rutgers E.J., Geijsen E.D., Zum vörde sive vörding P.J., Koning C.C., Van tienhoven G. Elective re-irradiation and hyperthermia following resection of persistent locoregional recurrent breast cancer: A retrospective study. Int. J. Hyperthermia. 2010;26:136–144. doi: 10.3109/02656730903341340. [DOI] [PubMed] [Google Scholar]
- 122.Shen H., Li X.D., Wu C.P., Yin Y.M., Wang R.S., Shu Y.Q. The regimen of gemcitabine and cisplatin combined with radio frequency hyperthermia for advanced non-small cell lung cancer: A phase II study. Int. J. Hyperthermia. 2011;27:27–32. doi: 10.3109/02656736.2010.500645. [DOI] [PubMed] [Google Scholar]
- 123.Issels R.D., Lindner L.H., Verweij J., Wust P., Reichardt P., Schem B.C., Abdel-Rahman S., Daugaard S., Salat C., Wendtner C.M., et al. Neo-adjuvant chemotherapy alone or with regional hyperthermia for localised high-risk soft-tissue sarcoma: A randomised phase 3 multicentre study. Lancet Oncol. 2010;11:561–570. doi: 10.1016/S1470-2045(10)70071-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Sugimachi K., Kuwano H., Ide H., Toge T., Saku M., Oshiumi Y. Chemotherapy combined with or without hyperthermia for patients with oesophageal carcinoma: A prospective randomized trial. Int. J. Hyperthermia. 1994;10:485–493. doi: 10.3109/02656739409009352. [DOI] [PubMed] [Google Scholar]
- 125.Colombo R., Salonia A., Leib Z., Pavone-Macaluso M., Engelstein D. Long-term outcomes of a randomized controlled trial comparing thermochemotherapy with mitomycin-C alone as adjuvant treatment for non-muscle-invasive bladder cancer (NMIBC) BJU Int. 2011;107:912–918. doi: 10.1111/j.1464-410X.2010.09654.x. [DOI] [PubMed] [Google Scholar]
- 126.Braun J., Hahn G.M. Enhanced cell killing by bleomycin and 43 degrees hyperthermia and the inhibition of recovery from potentially lethal damage. Cancer Res. 1975;35:2921–2927. [PubMed] [Google Scholar]
- 127.Zagar T.M., Vujaskovic Z., Formenti S., Rugo H., Muggia F., O’Connor B., Myerson R., Stauffer P., Hsu I.C., Diederich C., et al. Two phase I dose-escalation/pharmacokinetics studies of low temperature liposomal doxorubicin (LTLD) and mild local hyperthermia in heavily pretreated patients with local regionally recurrent breast cancer. Int. J. Hyperthermia. 2014;30:285–294. doi: 10.3109/02656736.2014.936049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Wallner K.E., DeGregorio M.W., Li G.C. Hyperthermic potentiation of cis-diamminedichloroplatinum(II) cytotoxicity in Chinese hamster ovary cells resistant to the drug. Cancer Res. 1986;46:6242–6245. [PubMed] [Google Scholar]
- 129.Magin R.L., Sikic B.I., Cysyk R.L. Enhancement of bleomycin activity against Lewis lung tumors in mice by local hyperthermia. Cancer Res. 1979;39:3792–3795. [PubMed] [Google Scholar]
- 130.Kong G., Anyarambhatla G., Petros W.P., Braun R.D., Colvin O.M., Needham D., Dewhirst M.W. Efficacy of liposomes and hyperthermia in a human tumor xenograft model: Importance of triggered drug release. Cancer Res. 2000;60:6950–6957. [PubMed] [Google Scholar]
- 131.Van der Heijden A.G., Jansen C.F., Verhaegh G., O’Donnell M A., Schalken J.A., Witjes J.A. The effect of hyperthermia on mitomycin-C induced cytotoxicity in four human bladder cancer cell lines. Eur. Urol. 2004;46:670–674. doi: 10.1016/j.eururo.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 132.Van Rhoon G.C., Franckena M., Ten Hagen T.L.M. A moderate thermal dose is sufficient for effective free and TSL based thermochemotherapy. Adv. Drug Deliv. Rev. 2020;163–164:145–156. doi: 10.1016/j.addr.2020.03.006. [DOI] [PubMed] [Google Scholar]
- 133.Rietbroek R.C., Schilthuis M.S., Bakker P.J., van Dijk J.D., Postma A.J., González González D., Bakker A.J., van der Velden J., Helmerhorst T.J., Veenhof C.H. Phase II trial of weekly locoregional hyperthermia and cisplatin in patients with a previously irradiated recurrent carcinoma of the uterine cervix. Cancer. 1997;79:935–943. doi: 10.1002/(SICI)1097-0142(19970301)79:5<935::AID-CNCR10>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 134.Fiegl M., Schlemmer M., Wendtner C.M., Abdel-Rahman S., Fahn W., Issels R.D. Ifosfamide, carboplatin and etoposide (ICE) as second-line regimen alone and in combination with regional hyperthermia is active in chemo-pre-treated advanced soft tissue sarcoma of adults. Int. J. Hyperthermia. 2004;20:661–670. doi: 10.1080/02656730410001714959. [DOI] [PubMed] [Google Scholar]
- 135.De Wit R., van der Zee J., van der Burg M.E., Kruit W.H., Logmans A., van Rhoon G.C., Verweij J. A phase I/II study of combined weekly systemic cisplatin and locoregional hyperthermia in patients with previously irradiated recurrent carcinoma of the uterine cervix. Br. J. Cancer. 1999;80:1387–1391. doi: 10.1038/sj.bjc.6690533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Alvarez Secord A., Jones E.L., Hahn C.A., Petros W.P., Yu D., Havrilesky L.J., Soper J.T., Berchuck A., Spasojevic I., Clarke-Pearson D.L., et al. Phase I/II trial of intravenous Doxil and whole abdomen hyperthermia in patients with refractory ovarian cancer. Int. J. Hyperthermia. 2005;21:333–347. doi: 10.1080/02656730500110155. [DOI] [PubMed] [Google Scholar]
- 137.Stahl R., Wang T., Lindner L.H., Abdel-Rahman S., Santl M., Reiser M.F., Issels R.D. Comparison of radiological and pathohistological response to neoadjuvant chemotherapy combined with regional hyperthermia (RHT) and study of response dependence on the applied thermal parameters in patients with soft tissue sarcomas (STS) Int. J. Hyperthermia. 2009;25:289–298. doi: 10.1080/02656730902873616. [DOI] [PubMed] [Google Scholar]
- 138.Vujaskovic Z., Kim D.W., Jones E., Lan L., McCall L., Dewhirst M.W., Craciunescu O., Stauffer P., Liotcheva V., Betof A., et al. A phase I/II study of neoadjuvant liposomal doxorubicin, paclitaxel, and hyperthermia in locally advanced breast cancer. Int. J. Hyperthermia. 2010;26:514–521. doi: 10.3109/02656731003639364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Ishikawa T., Kokura S., Sakamoto N., Ando T., Imamoto E., Hattori T., Oyamada H., Yoshinami N., Sakamoto M., Kitagawa K., et al. Phase II trial of combined regional hyperthermia and gemcitabine for locally advanced or metastatic pancreatic cancer. Int. J. Hyperthermia. 2012;28:597–604. doi: 10.3109/02656736.2012.695428. [DOI] [PubMed] [Google Scholar]
- 140.Yang W.H., Xie J., Lai Z.Y., Yang M.D., Zhang G.H., Li Y., Mu J.B., Xu J. Radiofrequency deep hyperthermia combined with chemotherapy in the treatment of advanced non-small cell lung cancer. Chin. Med. J. 2019;132:922–927. doi: 10.1097/CM9.0000000000000156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Tschoep-Lechner K.E., Milani V., Berger F., Dieterle N., Abdel-Rahman S., Salat C., Issels R.D. Gemcitabine and cisplatin combined with regional hyperthermia as second-line treatment in patients with gemcitabine-refractory advanced pancreatic cancer. Int. J. Hyperthermia. 2013;29:8–16. doi: 10.3109/02656736.2012.740764. [DOI] [PubMed] [Google Scholar]
- 142.Monge O.R., Rofstad E.K., Kaalhus O. Thermochemotherapy in vivo of a C3H mouse mammary carcinoma: Single fraction heat and drug treatment. Eur. J. Cancer Clin. Oncol. 1988;24:1661–1669. doi: 10.1016/0277-5379(88)90060-0. [DOI] [PubMed] [Google Scholar]
- 143.Adachi S., Kokura S., Okayama T., Ishikawa T., Takagi T., Handa O., Naito Y., Yoshikawa T. Effect of hyperthermia combined with gemcitabine on apoptotic cell death in cultured human pancreatic cancer cell lines. Int. J. Hyperthermia. 2009;25:210–219. doi: 10.1080/02656730802657036. [DOI] [PubMed] [Google Scholar]
- 144.Albregts M., Hulshof M.C., Zum Vörde Sive Vörding P.J., van Lanschot J.J., Richel D.J., Crezee H., Fockens P., van Dijk J.D., González González D. A feasibility study in oesophageal carcinoma using deep loco-regional hyperthermia combined with concurrent chemotherapy followed by surgery. Int. J. Hyperthermia. 2004;20:647–659. doi: 10.1080/02656730410001714977. [DOI] [PubMed] [Google Scholar]
- 145.Herman T.S., Teicher B.A., Jochelson M., Clark J., Svensson G., Coleman C.N. Rationale for use of local hyperthermia with radiation therapy and selected anticancer drugs in locally advanced human malignancies. Int. J. Hyperthermia. 1988;4:143–158. doi: 10.3109/02656738809029305. [DOI] [PubMed] [Google Scholar]
- 146.Herman T.S., Jochelson M.S., Teicher B.A., Scott P.J., Hansen J., Clark J.R., Pfeffer M.R., Gelwan L.E., Molnar-Griffin B.J., Fraser S.M., et al. A phase I-II trial of cisplatin, hyperthermia and radiation in patients with locally advanced malignancies. Int. J. Radiat. Oncol. Biol. Phys. 1989;17:1273–1279. doi: 10.1016/0360-3016(89)90536-1. [DOI] [PubMed] [Google Scholar]
- 147.Herman T.S., Teicher B.A. Sequencing of trimodality therapy[cis-diamminedichloroplatinum(II)/hyperthermia/radiation] as determined by tumor growth delay and tumor cell survival in the FSaIIC fibrosarcoma. Cancer Res. 1988;48:2693–2697. [PubMed] [Google Scholar]
- 148.Ohguri T., Imada H., Yahara K., Narisada H., Morioka T., Nakano K., Korogi Y. Concurrent chemoradiotherapy with gemcitabine plus regional hyperthermia for locally advanced pancreatic carcinoma: Initial experience. Radiat. Med. 2008;26:587–596. doi: 10.1007/s11604-008-0279-y. [DOI] [PubMed] [Google Scholar]
- 149.Harima Y., Ohguri T., Imada H., Sakurai H., Ohno T., Hiraki Y., Tuji K., Tanaka M., Terashima H. A multicentre randomised clinical trial of chemoradiotherapy plus hyperthermia versus chemoradiotherapy alone in patients with locally advanced cervical cancer. Int. J. Hyperthermia. 2016;32:801–808. doi: 10.1080/02656736.2016.1213430. [DOI] [PubMed] [Google Scholar]
- 150.Westermann A.M., Jones E.L., Schem B.C., van der Steen-Banasik E.M., Koper P., Mella O., Uitterhoeve A.L., de Wit R., van der Velden J., Burger C., et al. First results of triple-modality treatment combining radiotherapy, chemotherapy, and hyperthermia for the treatment of patients with stage IIB, III, and IVA cervical carcinoma. Cancer. 2005;104:763–770. doi: 10.1002/cncr.21128. [DOI] [PubMed] [Google Scholar]
- 151.Asao T., Sakurai H., Harashima K., Yamaguchi S., Tsutsumi S., Nonaka T., Shioya M., Nakano T., Kuwano H. The synchronization of chemotherapy to circadian rhythms and irradiation in pre-operative chemoradiation therapy with hyperthermia for local advanced rectal cancer. Int. J. Hyperthermia. 2006;22:399–406. doi: 10.1080/02656730600799873. [DOI] [PubMed] [Google Scholar]
- 152.Amichetti M., Graiff C., Fellin G., Pani G., Bolner A., Maluta S., Valdagni R. Cisplatin, hyperthermia, and radiation (trimodal therapy) in patients with locally advanced head and neck tumors: A phase I-II study. Int. J. Radiat. Oncol. Biol. Phys. 1993;26:801–807. doi: 10.1016/0360-3016(93)90495-H. [DOI] [PubMed] [Google Scholar]
- 153.Kouloulias V.E., Dardoufas C.E., Kouvaris J.R., Gennatas C.S., Polyzos A.K., Gogas H.J., Sandilos P.H., Uzunoglu N.K., Malas E.G., Vlahos L.J. Liposomal doxorubicin in conjunction with reirradiation and local hyperthermia treatment in recurrent breast cancer: A phase I/II trial. Clin. Cancer Res. 2002;8:374–382. [PubMed] [Google Scholar]
- 154.Gani C., Lamprecht U., Ziegler A., Moll M., Gellermann J., Heinrich V., Wenz S., Fend F., Königsrainer A., Bitzer M., et al. Deep regional hyperthermia with preoperative radiochemotherapy in locally advanced rectal cancer, a prospective phase II trial. Radiother. Oncol. 2021;159:155–160. doi: 10.1016/j.radonc.2021.03.011. [DOI] [PubMed] [Google Scholar]
- 155.Ohguri T., Harima Y., Imada H., Sakurai H., Ohno T., Hiraki Y., Tuji K., Tanaka M., Terashima H. Relationships between thermal dose parameters and the efficacy of definitive chemoradiotherapy plus regional hyperthermia in the treatment of locally advanced cervical cancer: Data from a multicentre randomised clinical trial. Int. J. Hyperthermia. 2018;34:461–468. doi: 10.1080/02656736.2017.1352105. [DOI] [PubMed] [Google Scholar]
- 156.Maluta S., Schaffer M., Pioli F., Dall’oglio S., Pasetto S., Schaffer P.M., Weber B., Giri M.G. Regional hyperthermia combined with chemoradiotherapy in primary or recurrent locally advanced pancreatic cancer: An open-label comparative cohort trial. Strahlenther. Onkol. 2011;187:619–625. doi: 10.1007/s00066-011-2226-6. [DOI] [PubMed] [Google Scholar]
- 157.Barsukov Y.A., Gordeyev S.S., Tkachev S.I., Fedyanin M.Y., Perevoshikov A.G. Phase II study of concomitant chemoradiotherapy with local hyperthermia and metronidazole for locally advanced fixed rectal cancer. Colorectal Dis. 2013;15:1107–1114. doi: 10.1111/codi.12281. [DOI] [PubMed] [Google Scholar]
- 158.Ott O.J., Gani C., Lindner L.H., Schmidt M., Lamprecht U., Abdel-Rahman S., Hinke A., Weissmann T., Hartmann A., Issels R.D., et al. Neoadjuvant Chemoradiation Combined with Regional Hyperthermia in Locally Advanced or Recurrent Rectal Cancer. Cancers. 2021;13:1279. doi: 10.3390/cancers13061279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Rau B., Wust P., Hohenberger P., Löffel J., Hünerbein M., Below C., Gellermann J., Speidel A., Vogl T., Riess H., et al. Preoperative hyperthermia combined with radiochemotherapy in locally advanced rectal cancer: A phase II clinical trial. Ann. Surg. 1998;227:380–389. doi: 10.1097/00000658-199803000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Rau B., Wust P., Tilly W., Gellermann J., Harder C., Riess H., Budach V., Felix R., Schlag P.M. Preoperative radiochemotherapy in locally advanced or recurrent rectal cancer: Regional radiofrequency hyperthermia correlates with clinical parameters. Int. J. Radiat. Oncol. Biol. Phys. 2000;48:381–391. doi: 10.1016/S0360-3016(00)00650-7. [DOI] [PubMed] [Google Scholar]
- 161.Wittlinger M., Rödel C.M., Weiss C., Krause S.F., Kühn R., Fietkau R., Sauer R., Ott O.J. Quadrimodal treatment of high-risk T1 and T2 bladder cancer: Transurethral tumor resection followed by concurrent radiochemotherapy and regional deep hyperthermia. Radiother. Oncol. 2009;93:358–363. doi: 10.1016/j.radonc.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 162.Milani V., Pazos M., Issels R.D., Buecklein V., Rahman S., Tschoep K., Schaffer P., Wilkowski R., Duehmke E., Schaffer M. Radiochemotherapy in combination with regional hyperthermia in preirradiated patients with recurrent rectal cancer. Strahlenther. Onkol. 2008;184:163–168. doi: 10.1007/s00066-008-1731-8. [DOI] [PubMed] [Google Scholar]
- 163.Zhu H., Huo X., Chen L., Wang H., Yu H. Clinical experience with radio-, chemo- and hyperthermotherapy combined trimodality on locally advanced esophageal cancer. Mol. Clin. Oncol. 2013;1:1009–1012. doi: 10.3892/mco.2013.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Gani C., Schroeder C., Heinrich V., Spillner P., Lamprecht U., Berger B., Zips D. Long-term local control and survival after preoperative radiochemotherapy in combination with deep regional hyperthermia in locally advanced rectal cancer. Int. J. Hyperthermia. 2016;32:187–192. doi: 10.3109/02656736.2015.1117661. [DOI] [PubMed] [Google Scholar]
- 165.Merten R., Ott O., Haderlein M., Bertz S., Hartmann A., Wullich B., Keck B., Kühn R., Rödel C.M., Weiss C., et al. Long-Term Experience of Chemoradiotherapy Combined with Deep Regional Hyperthermia for Organ Preservation in High-Risk Bladder Cancer (Ta, Tis, T1, T2) Oncologist. 2019;24:e1341–e1350. doi: 10.1634/theoncologist.2018-0280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Van Haaren P.M., Hulshof M.C., Kok H.P., Oldenborg S., Geijsen E.D., Van Lanschot J.J., Crezee J. Relation between body size and temperatures during locoregional hyperthermia of oesophageal cancer patients. Int. J. Hyperthermia. 2008;24:663–674. doi: 10.1080/02656730802210448. [DOI] [PubMed] [Google Scholar]
- 167.Curto S., Aklan B., Mulder T., Mils O., Schmidt M., Lamprecht U., Peller M., Wessalowski R., Lindner L.H., Fietkau R., et al. Quantitative, Multi-institutional Evaluation of MR Thermometry Accuracy for Deep-Pelvic MR-Hyperthermia Systems Operating in Multi-vendor MR-systems Using a New Anthropomorphic Phantom. Cancers. 2019;11:1709. doi: 10.3390/cancers11111709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Winter L., Oberacker E., Paul K., Ji Y., Oezerdem C., Ghadjar P., Thieme A., Budach V., Wust P., Niendorf T. Magnetic resonance thermometry: Methodology, pitfalls and practical solutions. Int. J. Hyperthermia. 2016;32:63–75. doi: 10.3109/02656736.2015.1108462. [DOI] [PubMed] [Google Scholar]
- 169.Adibzadeh F., Sumser K., Curto S., Yeo D.T.B., Shishegar A.A., Paulides M.M. Systematic review of pre-clinical and clinical devices for magnetic resonance-guided radiofrequency hyperthermia. Int. J. Hyperthermia. 2020;37:15–27. doi: 10.1080/02656736.2019.1705404. [DOI] [PubMed] [Google Scholar]
- 170.Gellermann J., Faehling H., Mielec M., Cho C.H., Budach V., Wust P. Image artifacts during MRT hybrid hyperthermia-causes and elimination. Int. J. Hyperthermia. 2008;24:327–335. doi: 10.1080/02656730701881141. [DOI] [PubMed] [Google Scholar]
- 171.Ishihara Y., Calderon A., Watanabe H., Okamoto K., Suzuki Y., Kuroda K., Suzuki Y. A precise and fast temperature mapping using water proton chemical shift. Magn. Reson. Med. 1995;34:814–823. doi: 10.1002/mrm.1910340606. [DOI] [PubMed] [Google Scholar]
- 172.Le Bihan D., Delannoy J., Levin R.L. Temperature mapping with MR imaging of molecular diffusion: Application to hyperthermia. Radiology. 1989;171:853–857. doi: 10.1148/radiology.171.3.2717764. [DOI] [PubMed] [Google Scholar]
- 173.Gellermann J., Wlodarczyk W., Feussner A., Fähling H., Nadobny J., Hildebrandt B., Felix R., Wust P. Methods and potentials of magnetic resonance imaging for monitoring radiofrequency hyperthermia in a hybrid system. Int. J. Hyperthermia. 2005;21:497–513. doi: 10.1080/02656730500070102. [DOI] [PubMed] [Google Scholar]
- 174.Lüdemann L., Wlodarczyk W., Nadobny J., Weihrauch M., Gellermann J., Wust P. Non-invasive magnetic resonance thermography during regional hyperthermia. Int. J. Hyperthermia. 2010;26:273–282. doi: 10.3109/02656731003596242. [DOI] [PubMed] [Google Scholar]
- 175.Gellermann J., Wlodarczyk W., Ganter H., Nadobny J., Fähling H., Seebass M., Felix R., Wust P. A practical approach to thermography in a hyperthermia/magnetic resonance hybrid system: Validation in a heterogeneous phantom. Int. J. Radiat. Oncol. Biol. Phys. 2005;61:267–277. doi: 10.1016/j.ijrobp.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 176.Gellermann J., Hildebrandt B., Issels R., Ganter H., Wlodarczyk W., Budach V., Felix R., Tunn P.U., Reichardt P., Wust P. Noninvasive magnetic resonance thermography of soft tissue sarcomas during regional hyperthermia: Correlation with response and direct thermometry. Cancer. 2006;107:1373–1382. doi: 10.1002/cncr.22114. [DOI] [PubMed] [Google Scholar]
- 177.Gellermann J., Wlodarczyk W., Hildebrandt B., Ganter H., Nicolau A., Rau B., Tilly W., Fähling H., Nadobny J., Felix R., et al. Noninvasive magnetic resonance thermography of recurrent rectal carcinoma in a 1.5 Tesla hybrid system. Cancer Res. 2005;65:5872–5880. doi: 10.1158/0008-5472.CAN-04-3952. [DOI] [PubMed] [Google Scholar]
- 178.Poni R., Neufeld E., Capstick M., Bodis S., Samaras T., Kuster N. Feasibility of Temperature Control by Electrical Impedance Tomography in Hyperthermia. Cancers. 2021;13:3297. doi: 10.3390/cancers13133297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Esrick M.A., McRae D.A. The effect of hyperthermia-induced tissue conductivity changes on electrical impedance temperature mapping. Phys. Med. Biol. 1994;39:133–144. doi: 10.1088/0031-9155/39/1/008. [DOI] [PubMed] [Google Scholar]
- 180.Paulsen K.D., Moskowitz M.J., Ryan T.P., Mitchell S.E., Hoopes P.J. Initial in vivo experience with EIT as a thermal estimator during hyperthermia. Int. J. Hyperthermia. 1996;12:573–591. doi: 10.3109/02656739609027666. [DOI] [PubMed] [Google Scholar]
- 181.Nguyen D.M., Andersen T., Qian P., Barry T., McEwan A. Electrical Impedance Tomography for monitoring cardiac radiofrequency ablation: A scoping review of an emerging technology. Med. Eng. Phys. 2020;84:36–50. doi: 10.1016/j.medengphy.2020.07.025. [DOI] [PubMed] [Google Scholar]