Abstract
Simple Summary
Brain imaging, specifically magnetic resonance imaging (MRI), plays a key role in the clinical and research aspects of neuro-oncology. Novel neuroimaging techniques enable the transformation of a brain MRI into a so-called average brain. This allows projects using already acquired brain MRIs to perform group analyses and draw conclusions. Once the data are in this average brain, several types of analyses can be performed. For example, determining the most vulnerable locations for certain tumor types or perhaps even the underlying circuitry and gene expression that might cause predisposition to tumor growth. This information may further our understanding of tumor behavior, leading to better patient counseling, surgery timing, and treatment monitoring.
Abstract
Neuro-oncology research is broad and includes several branches, one of which is neuroimaging. Magnetic resonance imaging (MRI) is instrumental for the diagnosis and treatment monitoring of patients with brain tumors. Most commonly, structural and perfusion MRI sequences are acquired to characterize tumors and understand their behaviors. Thanks to technological advances, structural brain MRI can now be transformed into a so-called average brain accounting for individual morphological differences, which enables retrospective group analysis. These normative analyses are uncommonly used in neuro-oncology research. Once the data have been normalized, voxel-wise analyses and spatial mapping can be performed. Additionally, investigations of underlying connectomics can be performed using functional and structural templates. Additionally, a recently available template of spatial transcriptomics has enabled the assessment of associated gene expression. The few published normative analyses have shown relationships between tumor characteristics and spatial localization, as well as insights into the circuitry associated with epileptogenic tumors and depression after cingulate tumor resection. The wide breadth of possibilities with normative analyses remain largely unexplored, specifically in terms of connectomics and imaging transcriptomics. We provide a framework for performing normative analyses in oncology while also highlighting their limitations. Normative analyses are an opportunity to address neuro-oncology questions from a different perspective.
Keywords: neuro-oncology, neuroimaging, MRI, normative analysis, connectomics, imaging transcriptomics
1. Introduction
Neuroimaging plays a crucial role in neuro-oncology research. At present, magnetic resonance imaging (MRI) is a key tool for the diagnosis and treatment monitoring of brain tumors. Most commonly, high spatial resolution structural images, such as T1 and T2-weighted sequences with and without gadolinium contrast agents, are acquired [1]. Perfusion imaging has also become a mainstay of neuro-oncology imaging protocols in the past decade, in which it has been used for brain tumor characterization as well as for the evaluation of treatment response and disease progression [2]. Generally, neuro-oncology-based analyses investigate tumors and their treatment in terms of signal characteristics across patients. Thanks to recent technological advances, group analyses can be performed in a so-called average brain [3,4]. However, while they have demonstrated their usefulness in other research fields, these analyses are uncommonly used in neuro-oncology.
Neuroimaging advances have enabled precise transformation of a patient’s brain onto an average brain template. Sophisticated computer algorithms use non-rigid methods to transform an individual brain to the brain template while accounting for anatomical differences [3,4]. Within the template, each voxel has a distinct address, which allows comparisons across subjects with varied brain morphologies, also referred to as analysis in normative space. Subsequently, voxel-based group statistics, functional and structural connectomics, and imaging transcriptomics analyses can be performed [5,6]. Importantly, these analyses only require high spatial resolution structural MRI, which are routinely acquired in clinical neuro-oncology.
Brain lesions, including tumors, can have local and distant clinical and histopathological effects that can be caused, for example, by local mass effects and invasion as well as connectomal diaschisis, respectively. In this perspective, we aim to provide an overview of normative voxel-based, connectomics, and imaging transcriptomics group analyses, which are currently uncommonly used in neuro-oncology research. We will first provide a technical summary to explain these methods. Then, we will discuss the few published neuro-oncology examples, as well as several potential avenues for these techniques. We will end by providing a practical framework to use these methods while also highlighting their limitations.
2. Advanced Neuroimaging Analyses Using Normative Brain Templates
There is considerable variability between individual human brains. This variability poses a challenge when comparing and communicating findings related to normal and altered brain anatomy and function. To overcome this limitation, a brain reference space, based on many individual brains, has been proposed: the Montreal Neurological Institute (MNI) template [4,7,8,9]. This common space was widely adapted in the late 1990s [10]. It serves as the standard reference space for the analysis and reporting of results. A multitude of multimodal publicly available atlases have been accurately registered in this standard space.
To be able to use the tools and atlases available, individual brains have to be projected onto the template space. This normalization step transforms a brain to match the template brain and typically first involves rotation, translation, scaling, and shearing. These are linear operations applied to all voxels and this is usually referred to as linear registration/transformation. In the next step, voxels are non-uniformly locally warped to better match the template brain anatomy. This non-linear registration maximizes anatomical correspondence between the individual brain and the template [11]. Once all brains have been transformed into common space, one can now compare and make statistical inferences about local anatomical differences [12] or map spatial characteristics of tumors and their clinical attributes [13] (Figure 1). At this point, voxel-based analyses can be performed.
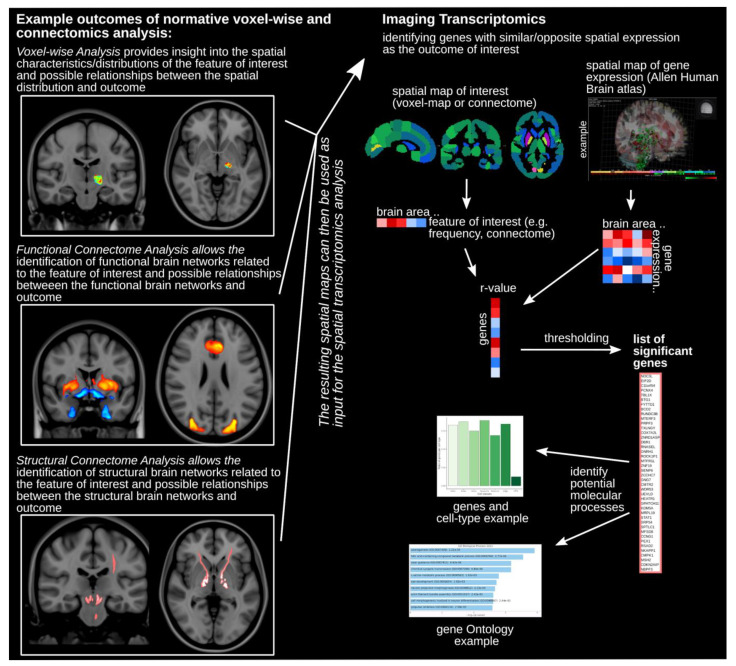
Figure 1.
Normative voxel-based, connectomics, and imaging transcriptomics analyses. Examples of outcome maps depicting voxel-based analysis (top), functional connectomic analysis (middle), and structural connectomic analysis (bottom) are shown on the left side of the figure. The resulting spatial maps of those analyses can then be used as input for the spatial transcriptomics analysis outlined on the right side of the figure. Atlas segmentation is used to calculate the correlation of spatial gene expression and imaging results across all brain areas. The thresholded subset of the list identifies the significantly implicated genes. This list can then be further investigated using, for example, gene ontology analysis.
2.1. Connectomics
The brain is a complex system of a multitude of distinct areas that are interconnected [14,15,16,17,18]. The networks formed by these groups of brain elements, as well as the interaction within and between each network, form the basis of behaviors. The connectome is key for understanding how the brain works. Over the last years, multiple studies have demonstrated that neurological and psychiatric symptoms can be mapped to a common distributed brain network [19,20,21,22,23,24,25,26,27,28,29,30]. The brain connectome can be assessed using different MRI acquisitions: (1) diffusion-weighted MRI (dMRI) to estimate the structural connectivity using the directionality of water diffusion to evaluate tracts and projections [31]; (2) resting state functional MRI (rsfMRI) to estimate functional connectivity making use of the low-frequency blood oxygen level-dependent (BOLD) fluctuations found in brain regions that are functionally related to each other [32]. The functional (i.e., rsfMRI) and structural (i.e., dMRI tractography) connectomes can be studied using normative, atlas-based connectome data assembled using high-quality acquisitions from a large number of subjects [5,26,33]. The use of these normative connectomes allows the investigation of brain-wide circuits implicated in clinical symptoms in the absence of patient-specific rsfMRI or dMRI acquisitions [24,29,34,35,36] (Figure 1). For example, if tumors are found to cause a specific cognitive impairment, one could use the normative functional connectome to map the key implicated regions and optimize patient counseling and surgical timing of subsequent tumors with similar characteristics.
2.2. Imaging Transcriptomics
These normative functional and structural connectomes have been highly valuable resources for studying normal and abnormal brain processes. Spatially resolved gene expression data provide yet another unique avenue to investigate the relationship between brain circuits implicated in various behaviors and diseases, and cell organization and underlying molecular characteristics [6,37]. The Allen Human Brain atlas provides spatially resolved gene expression in a standardized template space [38,39,40]. It is an online open access atlas of whole-brain microarray gene expression data (https://help.brain-map.org/display/humanbrain/Documentation, accessed on 1 December 2021). Using post-mortem tissue samples from six donors (age range 24–57 years, 1 female), over 20,000 genes were sampled across 3702 distinct sites creating an anatomically comprehensive spatial gene expression assay of the human brain [40]. This normative gene expression atlas allows one to investigate the molecular and cellular mechanisms associated with a spatial pattern or brain location identified in an independent neuroimaging analysis (Figure 1). For example, a study by Zheng and colleagues used normative connectomics and transcriptomics to investigate determinants of disease propagation in Parkinson’s disease [41] and recent work by Mandal and colleagues demonstrated that the spatial distribution of gliomas is related to the local normative expression of genes associated with chromatin organization and synaptic signaling [41,42].
3. Neuro-Oncology Applications
The neuro-oncology literature contains a few examples of normative analyses; however, several potential applications remain unexplored, specifically connectomics and imaging transcriptomics.
The majority of publications have used normative voxel-wise mapping to investigate spatial patterns of tumors. Spatial mapping has shown that glioblastomas tend to occur in different locations according to their molecular subtypes [43]. Similar analyses identified brain areas favored by lung cancer metastases, as well as a relationship between their spatial distribution and epidermal growth factor receptor mutation status [44,45]. Pediatric post-surgical cerebellar lesion mapping was used to identify structures most strongly associated with cognitive affective syndrome [46].
There is a paucity of neuro-oncology studies that have explored the normative functional connectome. One study found that the underlying normative circuitry of a group of spatially distinct mass lesions could explain the development of medically refractory epilepsy [36]. Following further validation, this approach could be used for patient counseling and optimizing surgical timing for lesions in locations involving epileptogenic networks. This type of analysis could also assess other tumor characteristics, such as preferential localization to specific functional networks based on tumor histology and genetics. There is also a case report of post-operative depression after cingulate low-grade glioma resection, in which functional connectomics suggests that the surgical corridor, rather than the tumor resection bed, had greater overlap with depression-related networks [47]. Furthermore, functional connectomics has been used to investigate the key functional networks underlying cognitive affective syndrome after cerebellar lesion resection [46]. Normative functional connectomic analyses are most appropriate when investigating distinct neurological manifestations from lesions in anatomically disparate locations. This analysis can be used to correlate symptoms and lesions, and may be a valuable tool for pre-operative patient counseling and selecting the optimal surgical approach.
There are very few publications taking advantage of normative structural connectomics and imaging transcriptomics. There is evidence that certain types of tumors exhibit preferential growth along white matter fiber directions [48,49]. Tumor growth patterns could be further assessed with large-scale data using normative structural connectomics. Two recently published reviews also suggest the application of brain connectomics for glioma surgery [50,51]. Similarly, understanding tumor behaviors and associated symptoms might require a whole-brain approach [52]. Rather than considering tumors with traditional lesion mapping, disconnectivity analysis may further our understanding of how white matter disconnections may predict tumor growth and recurrence patterns, as well as pre- and post-operative symptoms. Disconnectivity analysis could also inform surgical planning. The Allen Human Brain atlas [53], which integrates gene expression data and neuroanatomical information, has not yet been applied to neuro-oncology. This could potentially represent a powerful tool to investigate normative gene expression for various tumor types. Hypothetically, the results may show the vulnerability of certain brain areas to tumor growth and, possibly, highlight new genetic therapeutic targets. Similarly, sites of recurrence after resection could be assessed based on the normative gene expression of the adjacent brain; once again, these may reveal a pattern of vulnerability of certain brain areas. This could help understand and predict recurrences, as well as optimize surgical timing.
4. Practical Framework for Normative Brain Analyses
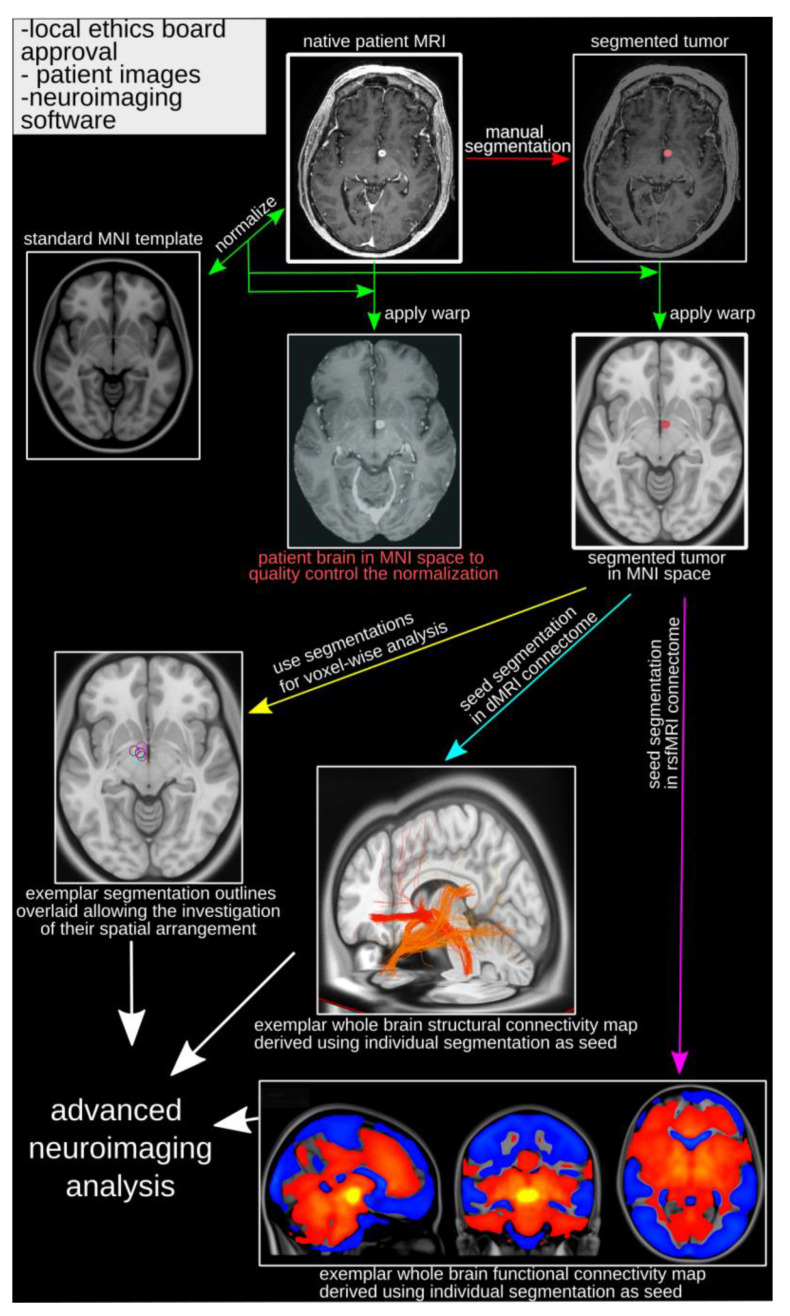
The use of these advanced normative brain atlases enables the analysis of retrospective patient data using MRI routinely acquired with clinical scans. Two items are necessary to begin: (1) approval from the local ethics board allowing chart review and data consolidation; (2) high spatial resolution MRI (typically a T1 or T2-weighted whole-brain image) allowing the localization of the relevant features (e.g., a tumor) and transformation of the patient data into template brain space (Figure 2). The next step is the identification/segmentation of the feature of interest using the native brain (Figure 2). Most commonly, the images have to be converted from DICOM (i.e., most common output format from MRI scanners) to nifti format [53,54]. There are many publicly available toolboxes that can easily be installed and used to perform these operations, for example SPM (https://www.fil.ion.ucl.ac.uk/spm/, accessed on 1 December 2021), FSL (https://fsl.fmrib.ox.ac.uk/fsl/fslwiki, accessed on 1 December 2021), ANTs (http://picsl.upenn.edu/software/ants/, accessed on 1 December 2021), or MINCtools (https://bic-mni.github.io/, accessed on 1 December 2021). To normalize the images containing the identified/segmented feature of interest (e.g., brain tumor), one would derive linear and non-linear transformations using the native structural MRI and apply these to the image capturing the feature of interest (Figure 2) [11,55,56]. This has to be performed for each individual subject/patient. Once transformed, the first question that can be investigated is whether or not the feature of interest shows a distinct spatial pattern, for example voxels or regions more or less likely to have tumor occurrence (Figure 2).
Figure 2.
Framework for normative brain analyses. Following typical research project prerequisites (upper left side of the image), the analysis begins with the native patient MRI. The feature of interest (e.g., tumor) is manually segmented (red arrow) using the native patient image. The native patient brain is then normalized (transformed) to MNI space and the estimated transforms applied to the native patient brain (for quality control) and the segmented feature (green arrows). The segmented feature (e.g., tumor) in MNI space is the main input for further processing, such as voxel-based group analysis (yellow arrow), and is used as seeds in normative structural (turquoise arrow) and functional (purple arrow) connectome analyses to derive brain-wide connectivity patterns. dMRI = diffusion-weighted MRI; MNI = Montreal Neurological Institute; MRI = Magnetic resonance imaging; rsfMRI = resting state functional MRI.
Using the segmented feature in the template space as the input in the normative functional and structural connectomes, one can then identify the brain-wide network of functionally and structurally connected areas (Figure 2). This allows identification of networks involved in clinical symptoms or disease processes (Figure 1) [22,25,26,27,46]. For example, tumor growth might preferentially move along a specific fiber tract or metastasis might be more likely to appear in brain areas functionally connected.
The spatial pattern of either the segmented feature (i.e., voxel-based analysis) and connectomics analyses can then be related to the spatial pattern of gene expression, which enables investigating the relationship of brain patterns and cell types or molecular processes [53,54,55]. One can use, for example, the regional Allen Gene Expression data (https://human.brain-map.org/, accessed on 1 December 2021) or tools, such as the abagen toolbox [54], to derive gene expression patterns and correlate these with the connectome or tumor occurrence pattern (Figure 1). This allows the identification of the gene set showing similar or opposite expression patterns. Moreover, gene ontology analysis (http://geneontology.org/, accessed on 1 December 2021) can assess processes associated with that gene set. If investigating tumor occurrences, this process could identify biological or molecular processes that make tumor occurrences more or less likely (Figure 1 and Figure 3).
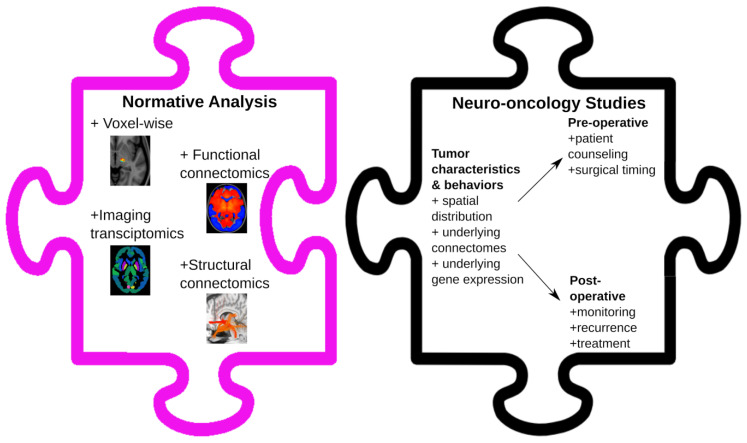
Figure 3.
Neuro-oncology applications of normative analyses. Voxel-based, connectomics, and imaging transcriptomics are various tools that can be used when performing normative analyses. Their applications to neuro-oncology are broad and include the assessment of tumor characteristics and behaviors, leading to potential pre- and post-operative improvements for patients.
5. Limitations of Normative Analyses
While normative analyses could have broad applications to the field of neuro-oncology, it is important to acknowledge their weaknesses. The major limitation of normative datasets is that the templates do not contain information about the brains of the individual patients to which they are applied [5,55]. This means that normative connectomes are not sensitive to intrinsic interindividual differences at a more granular level. Similarly, they may omit certain idiosyncrasies of pathology-specific brain characteristics. Therefore, it is imperative to ask appropriate scientific questions when using normative analyses. The normalization process represents another limitation. Although this has been highly optimized for non-linearly registering subcortical elements with submillimeter precision, normalization remains an imperfect process, particularly when marked morphological changes are present [3]. Of note, certain techniques, including masking specific brain areas or emphasizing certain brain structures during this process, can be used to improve the normalization of specific datasets. Finally, direct electrical stimulation during surgery may still provide more immediate and accurate information for surgical planning than functional and structural imaging, even at the patient level [56]. The unfamiliarity of the neuro-oncology field with these neuroimaging analyses combined with the novelty and requisite expertise to apply these techniques likely accounts for the paucity of neuro-oncology publications taking advantage of normative connectomics and transcriptomics.
These disadvantages are partially offset by considering that normative templates are high-resolution, high-fidelity, and high-n aggregate imaging data from initiatives such as the Brain Genomics Superstruct Project [57,58,59]. This is in contrast with clinically acquired individual patient imaging, which is often limited by suboptimal acquisition parameters due to time constraints and outdated hardware [5,55].
6. Conclusions
Normative neuroimaging approaches provide an opportunity to perform large-scale retrospective data analysis with MRI commonly acquired with clinical protocols. Thus far, their usage in neuro-oncology has been limited. We discussed their potential broad novel applications, from assessing tumor characteristics to pre-operative patient counselling and from surgical planning to post-operative treatment monitoring (Figure 3). These analyses may provide different perspectives on the current knowledge base.
Abbreviations
| BOLD | blood oxygen level-dependent |
| dMRI | diffusion weighted magnetic resonance imaging |
| MNI | Montreal Neurological Institute |
| MRI | magnetic resonance imaging |
| rsfMRI | resting state functional magnetic resonance imaging |
Author Contributions
Conceptualization, J.G., G.Z., A.M., W.K., A.M.L. and A.B.; methodology, J.G. and A.B.; formal analysis, J.G. and A.B.; investigation, J.G. and A.B.; resources, J.G. and A.B.; data curation, J.G. and A.B.; writing—original draft preparation, J.G. and A.B.; writing—review and editing, J.G., G.Z., A.M., W.K., A.M.L. and A.B.; visualization, J.G.; supervision, J.G. and A.B.; project administration, J.G. and A.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
A.M.L. is Scientific Director for Functional Neuromodulation Ltd. and a consultant to Medtronic, Abbott, Boston Scientific, Insightec, and Focused Ultrasound Foundation. The remaining authors have no conflict of interest to disclose.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ellingson B.M., Bendszus M., Boxerman J., Barboriak D., Erickson B.J., Smits M., Nelson S.J., Gerstner E., Alexander B., Goldmacher G., et al. Consensus Recommendations for a Standardized Brain Tumor Imaging Protocol in Clinical Trials. Neuro. Oncol. 2015;17:1188–1198. doi: 10.1093/neuonc/nov095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boxerman J.L., Quarles C.C., Hu L.S., Erickson B.J., Gerstner E.R., Smits M., Kaufmann T.J., Barboriak D.P., Huang R.H., Wick W., et al. Consensus Recommendations for a Dynamic Susceptibility Contrast MRI Protocol for Use in High-Grade Gliomas. Neuro. Oncol. 2020;22:1262–1275. doi: 10.1093/neuonc/noaa141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Avants B.B., Tustison N.J., Song G., Cook P.A., Klein A., Gee J.C. A Reproducible Evaluation of ANTs Similarity Metric Performance in Brain Image Registration. Neuroimage. 2011;54:2033–2044. doi: 10.1016/j.neuroimage.2010.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fonov V.S., Evans A.C., McKinstry R.C., Almli C.R., Collins D.L. Unbiased Nonlinear Average Age-Appropriate Brain Templates from Birth to Adulthood. Neuroimage. 2009;47:S102. doi: 10.1016/S1053-8119(09)70884-5. [DOI] [Google Scholar]
- 5.Horn A., Fox M.D. Opportunities of Connectomic Neuromodulation. Neuroimage. 2020;221:117180. doi: 10.1016/j.neuroimage.2020.117180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ståhl P.L., Salmén F., Vickovic S., Lundmark A., Navarro J.F., Magnusson J., Giacomello S., Asp M., Westholm J.O., Huss M., et al. Visualization and Analysis of Gene Expression in Tissue Sections by Spatial Transcriptomics. Science. 2016;353:78–82. doi: 10.1126/science.aaf2403. [DOI] [PubMed] [Google Scholar]
- 7.Talairach J., Tournoux P. Co-Planar Stereotaxic Atlas of the Human Brain. 3-Dimensional Proportional System: An Approach to Imaging. Georg Thieme Verlag; New York, NY, USA: Thieme Medical Publishers, Inc.; New York, NY, USA: 1988. [Google Scholar]
- 8.Mazziotta J.C., Toga A.W., Evans A., Fox P., Lancaster J. A Probabilistic Atlas of the Human Brain: Theory and Rationale for Its Development. Neuroimage. 1995;2:89–101. doi: 10.1006/nimg.1995.1012. [DOI] [PubMed] [Google Scholar]
- 9.Mazziotta J., Toga A., Evans A., Fox P., Lancaster J., Zilles K., Woods R., Paus T., Simpson G., Pike B., et al. A Probabilistic Atlas and Reference System for the Human Brain: International Consortium for Brain Mapping (ICBM) Philos. Trans. R. Soc. Lond. B Biol. Sci. 2001;356:1293–1322. doi: 10.1098/rstb.2001.0915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brett M., Johnsrude I.S., Owen A.M. The Problem of Functional Localization in the Human Brain. Nat. Rev. Neurosci. 2002;3:243–249. doi: 10.1038/nrn756. [DOI] [PubMed] [Google Scholar]
- 11.Klein A., Andersson J., Ardekani B.A., Ashburner J., Avants B., Chiang M.-C., Christensen G.E., Collins D.L., Gee J., Hellier P., et al. Evaluation of 14 Nonlinear Deformation Algorithms Applied to Human Brain MRI Registration. Neuroimage. 2009;46:786–802. doi: 10.1016/j.neuroimage.2008.12.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Almairac F., Duffau H., Herbet G. Contralesional Macrostructural Plasticity of the Insular Cortex in Patients with Glioma. Neurology. 2018;91:e1902–e1908. doi: 10.1212/WNL.0000000000006517. [DOI] [PubMed] [Google Scholar]
- 13.Sagberg L.M., Iversen D.H., Fyllingen E.H., Jakola A.S., Reinertsen I., Solheim O. Brain Atlas for Assessing the Impact of Tumor Location on Perioperative Quality of Life in Patients with High-Grade Glioma: A Prospective Population-Based Cohort Study. NeuroImage Clin. 2019;21:101658. doi: 10.1016/j.nicl.2019.101658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leergaard T.B., Hilgetag C.C., Sporns O. Mapping the Connectome: Multi-Level Analysis of Brain Connectivity. Front. Neuroinform. 2012;6 doi: 10.3389/fninf.2012.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hagmann P. From Diffusion MRI to Brain Connectomics. EPFL; Lausanne, Switzerland: 2005. [Google Scholar]
- 16.Sporns O. Structure and Function of Complex Brain Networks. Dialogues Clin. Neurosci. 2013;15:247–262. doi: 10.31887/DCNS.2013.15.3/osporns. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sporns O. The Human Connectome: A Complex Network. Ann. N. Y. Acad. Sci. 2011;1224:109–125. doi: 10.1111/j.1749-6632.2010.05888.x. [DOI] [PubMed] [Google Scholar]
- 18.Sporns O., Tononi G., Kötter R. The Human Connectome: A Structural Description of the Human Brain. PLoS Comput. Biol. 2005;1:0245–0251. doi: 10.1371/journal.pcbi.0010042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elias G.J.B., Germann J., Boutet A., Pancholi A., Beyn M.E., Bhatia K., Neudorfer C., Loh A., Rizvi S.J., Bhat V., et al. Structuro-Functional Surrogates of Response to Subcallosal Cingulate Deep Brain Stimulation for Depression. Brain. 2021 doi: 10.1093/brain/awab284. [DOI] [PubMed] [Google Scholar]
- 20.Boutet A., Madhavan R., Elias G.J.B., Joel S.E., Gramer R., Ranjan M., Paramanandam V., Xu D., Germann J., Loh A., et al. Predicting Optimal Deep Brain Stimulation Parameters for Parkinson’s Disease Using Functional MRI and Machine Learning. Nat. Commun. 2021;12:3043. doi: 10.1038/s41467-021-23311-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neudorfer C., Elias G.J.B., Jakobs M., Boutet A., Germann J., Narang K., Loh A., Paff M., Horn A., Kucharczyk W., et al. Mapping Autonomic, Mood and Cognitive Effects of Hypothalamic Region Deep Brain Stimulation. Brain. 2021;144:2837–2851. doi: 10.1093/brain/awab170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Germann J., Elias G.J.B., Neudorfer C., Boutet A., Chow C.T., Wong E.H.Y., Parmar R., Gouveia F.V., Loh A., Giacobbe P., et al. Potential Optimization of Focused Ultrasound Capsulotomy for Obsessive Compulsive Disorder. Brain. 2021 doi: 10.1093/brain/awab232. [DOI] [PubMed] [Google Scholar]
- 23.Li N., Hollunder B., Baldermann J.C., Kibleur A., Treu S., Akram H., Al-Fatly B., Strange B.A., Barcia J.A., Zrinzo L., et al. A Unified Functional Network Target for Deep Brain Stimulation in Obsessive-Compulsive Disorder. Biol. Psychiatry. 2021 doi: 10.1016/j.biopsych.2021.04.006. [DOI] [PubMed] [Google Scholar]
- 24.Siddiqi S.H., Schaper F.L.W.V.J., Horn A., Hsu J., Padmanabhan J.L., Brodtmann A., Cash R.F.H., Corbetta M., Choi K.S., Dougherty D.D., et al. Brain Stimulation and Brain Lesions Converge on Common Causal Circuits in Neuropsychiatric Disease. Nat. Hum. Behav. 2021;5 doi: 10.1038/s41562-021-01161-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Germann J., Elias G.J.B., Boutet A., Narang K., Neudorfer C., Horn A., Loh A., Deeb W., Salvato B., Almeida L., et al. Brain Structures and Networks Responsible for Stimulation-Induced Memory Flashbacks during Forniceal Deep Brain Stimulation for Alzheimer’s Disease. Alzheimer’s Dement. 2021;17:777–787. doi: 10.1002/alz.12238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fox M.D. Mapping Symptoms to Brain Networks with the Human Connectome. N. Engl. J. Med. 2018;379:2237–2245. doi: 10.1056/NEJMra1706158. [DOI] [PubMed] [Google Scholar]
- 27.Fox M.D., Buckner R.L., Liu H., Chakravarty M.M., Lozano A.M., Pascual-Leone A. Resting-State Networks Link Invasive and Noninvasive Brain Stimulation across Diverse Psychiatric and Neurological Diseases. Proc. Natl. Acad. Sci. USA. 2014;111 doi: 10.1073/pnas.1405003111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cohen A.L., Ferguson M.A., Fox M.D. Lesion Network Mapping Predicts Post-Stroke Behavioural Deficits, and Improves Localization. Brain. 2021;144 doi: 10.1093/brain/awab002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Darby R.R., Joutsa J., Fox M.D. Network Localization of Heterogeneous Neuroimaging Findings. Brain. 2019;142:70–79. doi: 10.1093/brain/awy292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Corp D.T., Joutsa J., Darby R.R., Delnooz C.C.S., van de Warrenburg B.P.C., Cooke D., Prudente C.N., Ren J., Reich M.M., Batla A., et al. Network Localization of Cervical Dystonia Based on Causal Brain Lesions. Brain. 2019;142:1660–1674. doi: 10.1093/brain/awz112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jbabdi S., Sotiropoulos S.N., Haber S.N., Van Essen D.C., Behrens T.E. Measuring Macroscopic Brain Connections in Vivo. Nat. Neurosci. 2015;18:1546–1555. doi: 10.1038/nn.4134. [DOI] [PubMed] [Google Scholar]
- 32.Biswal B.B., Mennes M., Zuo X.-N., Gohel S., Kelly C., Smith S.M., Beckmann C.F., Adelstein J.S., Buckner R.L., Colcombe S., et al. Toward Discovery Science of Human Brain Function. Proc. Natl. Acad. Sci. USA. 2010;107:4734–4739. doi: 10.1073/pnas.0911855107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Elias G.J.B., Germann J., Loh A., Boutet A., Taha A., Wong E.H.Y., Parmar R., Lozano A.M. Connectomic Deep Brain Stimulation. Academic Press; Cambridge, MA, USA: 2022. Normative connectomes and their use in DBS; pp. 245–274. [Google Scholar]
- 34.Mithani K., Boutet A., Germann J., Elias G.J.B., Weil A.G., Shah A., Guillen M., Bernal B., Achua J.K., Ragheb J., et al. Lesion Network Localization of Seizure Freedom Following MR-Guided Laser Interstitial Thermal Ablation. Sci. Rep. 2019;9:1–11. doi: 10.1038/s41598-019-55015-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Elias G.J.B., De Vloo P., Germann J., Boutet A., Gramer R.M., Joel S.E., Morlion B., Nuttin B., Lozano A.M. Mapping the Network Underpinnings of Central Poststroke Pain and Analgesic Neuromodulation. Pain. 2020;161:2805–2819. doi: 10.1097/j.pain.0000000000001998. [DOI] [PubMed] [Google Scholar]
- 36.Mansouri A.M., Germann J., Boutet A., Elias G.J.B., Mithani K., Chow C.T., Karmur B., Ibrahim G.M., McAndrews M.P., Lozano A.M., et al. Identification of Neural Networks Preferentially Engaged by Epileptogenic Mass Lesions through Lesion Network Mapping Analysis. Sci. Rep. 2020;10:1–11. doi: 10.1038/s41598-020-67626-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rodriques S.G., Stickels R.R., Goeva A., Martin C.A., Murray E., Vanderburg C.R., Welch J., Chen L.M., Chen F., Macosko E.Z. Slide-Seq: A Scalable Technology for Measuring Genome-Wide Expression at High Spatial Resolution. Science. 2019;363:1463–1467. doi: 10.1126/science.aaw1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shen E.H., Overly C.C., Jones A.R. The Allen Human Brain Atlas: Comprehensive Gene Expression Mapping of the Human Brain. Trends Neurosci. 2012;35:711–714. doi: 10.1016/j.tins.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 39.Jones A.R., Overly C.C., Sunkin S.M. The Allen Brain Atlas: 5 Years and beyond. Nat. Rev. Neurosci. 2009;10:821–828. doi: 10.1038/nrn2722. [DOI] [PubMed] [Google Scholar]
- 40.Hawrylycz M.J., Lein E.S., Guillozet-Bongaarts A.L., Shen E.H., Ng L., Miller J.A., van de Lagemaat L.N., Smith K.A., Ebbert A., Riley Z.L., et al. An Anatomically Comprehensive Atlas of the Adult Human Brain Transcriptome. Nature. 2012;489:391–399. doi: 10.1038/nature11405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zheng Y.-Q., Zhang Y., Yau Y., Zeighami Y., Larcher K., Misic B., Dagher A. Local Vulnerability and Global Connectivity Jointly Shape Neurodegenerative Disease Propagation. PLoS Biol. 2019;17:e3000495. doi: 10.1371/journal.pbio.3000495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mandal A.S., Romero-Garcia R., Hart M.G., Suckling J. Genetic, Cellular, and Connectomic Characterization of the Brain Regions Commonly Plagued by Glioma. Brain. 2020;143:3294–3307. doi: 10.1093/brain/awaa277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bilello M., Akbari H., Da X., Pisapia J.M., Mohan S., Wolf R.L., O’Rourke D.M., Martinez-Lage M., Davatzikos C. Population-Based MRI Atlases of Spatial Distribution Are Specific to Patient and Tumor Characteristics in Glioblastoma. Neuroimage Clin. 2016;12:34–40. doi: 10.1016/j.nicl.2016.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang Y., Xia W., Liu B., Zhou L., Ni M., Zhang R., Shen J., Bai Y., Weng G., Yuan S., et al. Exploration of Spatial Distribution of Brain Metastasis from Small Cell Lung Cancer and Identification of Metastatic Risk Level of Brain Regions: A Multicenter, Retrospective Study. Cancer Imaging. 2021;21:41. doi: 10.1186/s40644-021-00410-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Takano K., Kinoshita M., Takagaki M., Sakai M., Tateishi S., Achiha T., Hirayama R., Nishino K., Uchida J., Kumagai T., et al. Different Spatial Distributions of Brain Metastases from Lung Cancer by Histological Subtype and Mutation Status of Epidermal Growth Factor Receptor. Neuro. Oncol. 2016;18:716–724. doi: 10.1093/neuonc/nov266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Albazron F.M., Bruss J., Jones R.M., Yock T.I., Pulsifer M.B., Cohen A.L., Nopoulos P.C., Abrams A.N., Sato M., Boes A.D. Pediatric Postoperative Cerebellar Cognitive Affective Syndrome Follows Outflow Pathway Lesions. Neurology. 2019;93:e1561–e1571. doi: 10.1212/WNL.0000000000008326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mansouri A., Boutet A., Elias G., Germann J., Yan H., Babu H., Lozano A.M., Valiante T.A. Lesion Network Mapping Analysis Identifies Potential Cause of Postoperative Depression in a Case of Cingulate Low-Grade Glioma. World Neurosurg. 2020;133:278–282. doi: 10.1016/j.wneu.2019.10.020. [DOI] [PubMed] [Google Scholar]
- 48.Esmaeili M., Stensjøen A.L., Berntsen E.M., Solheim O., Reinertsen I. The Direction of Tumour Growth in Glioblastoma Patients. Sci. Rep. 2018;8:1199. doi: 10.1038/s41598-018-19420-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mickevicius N.J., Carle A.B., Bluemel T., Santarriaga S., Schloemer F., Shumate D., Connelly J., Schmainda K.M., LaViolette P.S. Location of Brain Tumor Intersecting White Matter Tracts Predicts Patient Prognosis. J. Neurooncol. 2015;125:393–400. doi: 10.1007/s11060-015-1928-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Duffau H. Brain Connectomics Applied to Oncological Neuroscience: From a Traditional Surgical Strategy Focusing on Glioma Topography to a Meta-Network Approach. Acta Neurochir. 2021;163:905–917. doi: 10.1007/s00701-021-04752-z. [DOI] [PubMed] [Google Scholar]
- 51.Samuel N., Vetkas A., Pancholi A., Sarica C., Loh A., Germann J., Harmsen I.E., Tasserie J., Milano V., Yamamoto K., et al. A Network-Based Approach to Glioma Surgery: Insights from Functional Neurosurgery. Cancers. 2021;13:6127. doi: 10.3390/cancers13236127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Griffis J.C., Metcalf N.V., Corbetta M., Shulman G.L. Lesion Quantification Toolkit: A MATLAB Software Tool for Estimating Grey Matter Damage and White Matter Disconnections in Patients with Focal Brain Lesions. Neuroimage Clin. 2021;30:102639. doi: 10.1016/j.nicl.2021.102639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sunkin S.M., Ng L., Lau C., Dolbeare T., Gilbert T.L., Thompson C.L., Hawrylycz M., Dang C. Allen Brain Atlas: An Integrated Spatio-Temporal Portal for Exploring the Central Nervous System. Nucleic Acids Res. 2013;41:D996–D1008. doi: 10.1093/nar/gks1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Markello R.D., Arnatkevičiūtė A., Poline J.-B., Fulcher B.D., Fornito A., Misic B. Standardizing Workflows in Imaging Transcriptomics with the Abagen Toolbox. eLife. 2021;10:e72129. doi: 10.7554/eLife.72129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang Q., Akram H., Muthuraman M., Gonzalez-Escamilla G., Sheth S.A., Oxenford S., Yeh F.-C., Groppa S., Vanegas-Arroyave N., Zrinzo L., et al. Normative vs. Patient-Specific Brain Connectivity in Deep Brain Stimulation. Neuroimage. 2021;224:117307. doi: 10.1016/j.neuroimage.2020.117307. [DOI] [PubMed] [Google Scholar]
- 56.Azad T.D., Duffau H. Limitations of Functional Neuroimaging for Patient Selection and Surgical Planning in Glioma Surgery. Neurosurg. Focus. 2020;48:E12. doi: 10.3171/2019.11.FOCUS19769. [DOI] [PubMed] [Google Scholar]
- 57.Holmes A.J., Hollinshead M.O., O’Keefe T.M., Petrov V.I., Fariello G.R., Wald L.L., Fischl B., Rosen B.R., Mair R.W., Roffman J.L., et al. Brain Genomics Superstruct Project Initial Data Release with Structural, Functional, and Behavioral Measures. Sci. Data. 2015;2:150031. doi: 10.1038/sdata.2015.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Glasser M.F., Smith S.M., Marcus D.S., Andersson J.L.R., Auerbach E.J., Behrens T.E.J., Coalson T.S., Harms M.P., Jenkinson M., Moeller S., et al. The Human Connectome Project’s Neuroimaging Approach. Nat. Neurosci. 2016;19:1175–1187. doi: 10.1038/nn.4361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Elam J.S., Glasser M.F., Harms M.P., Sotiropoulos S.N., Andersson J.L.R., Burgess G.C., Curtiss S.W., Oostenveld R., Larson-Prior L.J., Schoffelen J.-M., et al. The Human Connectome Project: A Retrospective. Neuroimage. 2021;244:118543. doi: 10.1016/j.neuroimage.2021.118543. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.