Abstract
Background.
The Adolescent Brain Cognitive Development ™ Study (ABCD StudyⓇ) is an open-science, multi-site, prospective, longitudinal study following over 11,800 9- and 10-year-old youth into early adulthood. The ABCD Study aims to prospectively examine the impact of substance use (SU) on neurocognitive and health outcomes. Although SU initiation typically occurs during teen years, relatively little is known about patterns of SU in children younger than 12.
Methods.
This study aims to report the detailed ABCD StudyⓇSU patterns at baseline (n=11,875) in order to inform the greater scientific community about cohort’s early SU. Along with a detailed description of SU, we ran mixed effects regression models to examine the association between early caffeine and alcohol sipping with demographic factors, externalizing symptoms and parental history of alcohol and substance use disorders (AUD/SUD).
Primary Results.
At baseline, the majority of youth had used caffeine (67.6%) and 22.5% reported sipping alcohol (22.5%). There was little to no reported use of other drug categories (0.2% full alcohol drink, 0.7% used nicotine, 0.1% used cannabis, <0.02% used any other drug of abuse). Analyses revealed that total caffeine use and early alcohol sipping were associated with demographic variables (p’s<.05), externalizing symptoms (caffeine p=0002; sipping p=.0003), and parental history of AUD (sipping p=.03).
Conclusions.
ABCD Study participants aged 9–10 years old reported caffeine use and alcohol sipping experimentation, but very rare other SU. Variables linked with early childhood alcohol sipping and caffeine use should be examined as contributing factors in future longitudinal analyses examining escalating trajectories of SU in the ABCD Study cohort.
Keywords: ABCD Study, alcohol, Cannabis, Nicotine, caffeine, externalizing behaviors, alcohol sipping, children
1. BACKGROUND
The Adolescent Brain Cognitive Development ™ Study (ABCD StudyⓇ) is an epidemiologically informed prospective cohort study aimed at understanding the many factors that influence child and adolescent development (Volkow, Koob et al. 2018) (Jernigan, Brown et al. 2018). Over 11,800 youth aged 9–10 were recruited at baseline and are being followed for 10 years, in order to understand the developmental interaction between culture and environment (Zucker, Gonzalez et al. 2018), mental and physical health (Barch, Albaugh et al. 2018), substance use (SU) attitudes and exposure (Lisdahl, Sher et al. 2018), biological functioning (Uban, Horton et al. 2018), and genetics (Iacono, Heath et al. 2018) on neurocognitive development (Casey, Cannonier et al. 2018) (Luciana, Bjork et al. 2018).
The initiation of SU typically begins in adolescence, a period of ongoing neuromaturation (Casey, Giedd et al. 2000, Gardner and Steinberg 2005, Eaton, Kann et al. 2006, Casey, Getz et al. 2008) (Giedd, Snell et al. 1996, Sowell, Thompson et al. 1999, Sowell, Trauner et al. 2002, Gogtay, Giedd et al. 2004, Sowell, Thompson et al. 2004, Lenroot and Giedd 2006, Somerville, Jones et al. 2010, Houston, Herting et al. 2014, Mills, Goddings et al. 2014, Schmitt, Neale et al. 2014). In the United States, the national Monitoring the Future (MTF) Study identified an appreciable proportion of SU among eighth graders in 2019, including alcohol (24.5%), cannabis (aka marijuana) (15.2%), vaping including electronic nicotine delivery systems (ENDS, 20.3%; 18.9% JUUL), cigarettes (10.0%), inhalants (9.5%), smokeless tobacco (7.1%), and misuse of prescription amphetamines (6.8%), while a small percentage reported other illicit drug use (2.4% hallucinogens, 1.7% ecstasy, 1.2% cocaine, 0.9% methamphetamine, 0.7% heroin) (Johnston 2020). It is notable that published national data for SU among youth as young as 9 or 10 years old (the baseline age of the ABCD Study cohort) are uncommon, as the youngest age assessed in American national surveys is 12 years old [e.g., the National Survey on Drug Use and Health (Quality. 2014) begins at age 12, MTF Study starts at age 13 (Johnston 2020)]. Data on school-aged children are primarily available at the state level (Donovan 2007) (Donovan 2013) for caffeine usage (Ahluwalia, Herrick et al. 2014, Ahluwalia and Herrick 2015) or early alcohol sipping (Donovan 2013) (Donovan and Molina 2014) (Jackson, Barnett et al. 2015). One of the larger state surveys available on 4th-6th graders is the Texas School Survey on Drug and Alcohol Use (Institute 2012); this self-report survey found that 12.7% of 4th graders had already used any alcohol, 11.1% used inhalants, 2.8% used nicotine products, and a small fraction used cannabis (0.8%). Given the goals of prospectively studying the impact of SU on neurocognitive and health outcomes, it is important to fully characterize any SU reported by ABCD Study youth at baseline.
Few longitudinal or epidemiological studies focused on adolescent SU have assessed caffeine use and its influence on health outcomes, although addiction scientists have raised concerns over potential effects of caffeine use on decision-making and addiction risk (Budney and Emond 2014) (Temple, Bernard et al. 2017) (Temple 2009) (Curran and Marczinski 2017). Caffeine use is common (73.9%), even in elementary school-aged children (6–11-year olds) (Ahluwalia, Herrick et al. 2014, Ahluwalia and Herrick 2015); accordingly, the ABCD Study SU Module integrated caffeine use measures in its protocol (Lisdahl, Sher et al. 2018). After caffeine, alcohol remains the most commonly used substance of abuse in adolescents (Miech 2018). Initiation of alcohol often starts with sipping, defined as taking a sip of alcohol without consuming a full standard drink (Donovan 2007) (Donovan and Molina 2008). The typical age of alcohol sipping initiation is between 9 and 14 years old (Jackson, Barnett et al. 2015) (Jackson, Ennett et al. 2013, Wadolowski, Hutchinson et al. 2015) (Wadolowski, Bruno et al. 2015). However, Donovan and colleagues observed that 35% of 8-year-olds engaged in alcohol sipping in a sample of 452 children in Pennsylvania (Donovan and Molina 2008). In a prospective web-based community study on alcohol initiation in 561 students, Jackson and colleagues (Jackson, Barnett et al. 2015) found that the prevalence of sipping alcohol by fall of sixth grade was 29.5%. Of concern, sipping by sixth grade predicted greater odds of full alcohol drink consumption, getting “drunk,” heavy drinking by ninth grade (Jackson, Barnett et al. 2015), and early adolescent drinking is associated with greater risk of developing an alcohol use disorder (AUD) (Grant and Dawson 1997). Thus, carefully measuring early alcohol sipping patterns and understanding risk factors for sipping initiation may facilitate development of prevention campaigns to reduce risky adolescent drinking.
In sum, SU initiation can begin in early adolescence; however, few studies have reported SU patterns in a large cohort of elementary school-aged children. Further, no studies to date examined whether common factors linked with later SU (e.g., sex at birth, individual and household demographics, family history of substance use disorder (SUD), or youth externalizing symptoms) are associated with childhood caffeine and alcohol use patterns. Most notably, the ABCD Study was designed to assess the complex environmental, biological, psychiatric and health factors prior to the onset of regular substance exposure in order to characterize the timing and impact of escalating SU on neurocognitive and mental health outcomes (Lisdahl, Sher et al. 2018). Thus, the current study aims to provide a detailed description of the baseline SU patterns in youth enrolled in the ABCD Study. Further, we reported whether individual and household demographic variables (Garavan, Bartsch et al. 2018), parental history of AUD and SUD, and youth externalizing behaviors (variables utilized to recruit and stratify the sample based on SU risk (Loeber, Clark et al. 2018)) are associated with early caffeine and alcohol sipping use at baseline in youth enrolled in the study. This information can help guide the scientific community in considering factors that must be considered in relation to very early substance use experimentation in the ABCD Study cohort.
2. METHODS
A. Participants and Procedures
Participants in the current study included 11,857 youth who enrolled in the ABCD Study and completed the baseline session. The ABCD Study is a multi-site longitudinal study that enrolled 11,880 9- and 10-year-old racially/ethnically diverse youth (47.8% female) at baseline at 21 U.S. research sites between 2016–2018, and is following the youth and parents/guardians annually for ten years into early adulthood (Jernigan, Brown et al. 2018, Volkow, Koob et al. 2018). Baseline recruitment used a stratified probability sample of eligible schools (selected for sex at birth, race/ethnicity, socioeconomic status, urbanicity) to match the demographic profile of the American Community Survey 3rd and 4th grade enrollment statistics within research catchment areas (for details, see (Garavan, Bartsch et al. 2018)). All study procedures were approved by the centralized institutional review board (IRB) at the University of California San Diego and by the local site IRBs. Potential participants were excluded for the following reasons: child not fluent in English, magnetic resonance imaging (MRI) contraindication, major neurological disorder, gestational age less than 28 weeks or birth weight less than 1,200 grams, birth complications that resulted in hospitalization for more than one month, uncorrected vision, or current diagnosis of schizophrenia, autism spectrum disorder (moderate, severe), intellectual disability, or alcohol/substance use disorder (note: although this was exclusionary at baseline, no youth were excluded for SUD/DUD). Informed consent was obtained from parents/caregivers and assent from youth.
At baseline, youth and at least one parent or guardian participated in 1–2 in-person sessions, during which they completed a comprehensive battery of behavioral and biological assessment modules that were outlined in detail elsewhere: mental and physical health (Barch, Albaugh et al. 2018), SU (Lisdahl, Sher et al. 2018), peer, family, culture, and environment (Zucker, Gonzalez et al. 2018), biological functioning (Uban, Horton et al. 2018), genetics (Iacono, Heath et al. 2018), and neuropsychological and magnetic resonance imaging brain scans (Casey, Cannonier et al. 2018, Luciana, Bjork et al. 2018). For the vast majority of modules, all questionnaires were converted for electronic data capture via REDCap (Harris, Taylor et al. 2009) that were harmonized across sites (Auchter, Hernandez Mejia et al. 2018) (Casey, Cannonier et al. 2018) and administered on an iPad. Youth were interviewed separately from parents in a private space. The current study primarily utilized data from the SU, demographic, and mental health modules (see (Barch, Albaugh et al. 2018), (Lisdahl, Sher et al. 2018) for details).
During the SU module, rules regarding confidentiality and privacy were reiterated to the youth and they were asked if they had “heard of” a list of substances (including caffeine, alcohol, nicotine products, cannabis products, prescription or OTC drugs, inhalants, and “any other drug”‘; for the latter, the youth listed off those drugs and the RA indicated their endorsement on a drop-down menu with all drug categories) (Lisdahl, Sher et al. 2018). The remainder of the interview utilized gating, in that youth were not asked direct questions about substances that they had never heard of, or follow-up questions about substances they had never used. If a youth had not “heard of” a drug category, then their reported use of the drug at that time-point was coded as zero.
B. Measures
Demographic Factors.
Identity and household demographic factors were included in the multivariable analyses as covariates; these included age at time of assessment, sex assigned at birth, race/ethnicity [NDA 2.01 release coded variable including primary ethnic/racial categories (non-Hispanic White, Hispanic, Black, Asian, Other/Multi-ethnic)], highest parental/guardian education, parental/guardian marital status, and parental/guardian combined household income (see (Barch, Albaugh et al. 2018)).
Alcohol, Tobacco, and Cannabis Low-Level/First Use.
If youth heard of alcohol, they completed the iSay Sipping Inventory (Jackson, Barnett et al. 2015, Jackson, Colby et al. 2015), an 8-item measure of recent alcohol sipping that also characterized their first alcohol sipping experience. Participants reported whether they ever had a sip of alcohol, number of times had a sip of alcohol in lifetime, whether they sipped alcohol outside of a religious occasion (yes/no), total times had a sip of alcohol (outside of a religious setting), the age of first sip (outside of a religious context), whether they finished their first alcoholic drink, what type of alcohol was tried the first time they sipped, to whom the drink belonged, whether the sip was offered or taken without permission, and whether the youth remembered trying the alcohol or if she/he was told about it later. First use of nicotine or cannabis products was also assessed, including number of times used, age of first use, where/from whom they obtained the substance, and whether it led to further use (Lisdahl, Sher et al. 2018). For cannabis, whether they remembered or were told about their first use and subjective experience of feeling “high” during the first use were also measured.
Lifetime & Past 6-Month SU Patterns.
Youth were asked if they used each major drug category ever in their lifetime; multiple formal and informal names (including popular “street” names) of each substance were used (e.g., “alcohol such as beer, wine, or liquor – such as rum, vodka, gin, whiskey” for further details for each drug category see: (Lisdahl, Sher et al. 2018)). If a youth endorsed using the substance in the past six months, a detailed web-based Timeline Follow-Back (TLFB) interview (Sobell and Sobell 1996) (Robinson, Sobell et al. 2014) was administered (for details see (Lisdahl, Sher et al. 2018)). The TLFB uses a calendar-based interviewer-administered retrospective report of detailed quantity/frequency SU patterns during the past 6 months at baseline; for follow-up years, the entire period between sessions is assessed. Substances assessed for the lifetime SU and TLFB interviews included alcohol, nicotine products (cigarettes, electronic nicotine delivery systems (ENDS)1, smokeless tobacco, cigars, hookah, pipe, and nicotine replacement products), cannabis products (smoked/vaped flower, smoked blunts, edibles, smoked/vaped concentrates, oral tinctures, and cannabis-infused alcohol drinks, synthetic cannabinoids), cocaine, cathinones, methamphetamine, ecstasy/MDMA, ketamine, gamma-hydroxybutyrate (GHB), heroin, psilocybin, salvia, other hallucinogens (LSD, PCP, synthetic hallucinogens), anabolic steroids, inhalants, prescription stimulants, sedatives, and opioid pain relievers, and over the counter (OTC) cough/cold medicine (Lisdahl, Sher et al. 2018).
Caffeine Use.
The average weekly number of total standard doses of caffeine beverages (8 oz cup for coffee or tea, espresso shot, 12 oz soda, or 8 oz energy drink) consumed over the past six months were measured at baseline (see (Lisdahl, Sher et al. 2018)).
Externalizing Scale.
Parents rated their child’s externalizing (Rule-breaking Behavior, Aggressive Behavior) behaviors on the Child Behavior Checklist (CBCL; (TM 2009)).
Parental History of Alcohol and Drug Use Disorder.
We calculated a dummy-coded variable representing biological parental history of AUD and other drug use disorder (DUD) (no history/at least one parent with history/two parents having history) taken from the Family History Assessment Module Screener, which was filled out by the youth’s participating parent or guardian (FHAM-S; (Rice, Reich et al. 1995)).
C. Statistical Analysis.
Analyses were conducted in R (v3.6.1) utilizing published ABCD Data Release 2.01 (https://data-archive.nimh.nih.gov/abcd; DOI: 10.15154/1504041, July 2019). First, we computed descriptive statistics for variables (data were examined for non-normality and outliers prior to analysis; no trimming or corrections were applied). Next, considering the cohort was balanced for sex and sex differences have been repeatedly reported in SU patterns, especially in adolescents (Johnston 2020) (Windle 2020) (Wilkinson, Halpern et al. 2016), we examined sex differences [chi-square (Yate’s correction was employed if a cell is <5) or t-test analyses] for all analyses. Finally, in order to describe baseline relationships between demographic factors, externalizing behaviors, and parental history of AUD/SUD (Loeber, Clark et al. 2018), we ran Generalized Linear Mixed Effect (LME) (Laird and Ware 1982) models for multivariable regression analyses utilizing the appropriate distribution of the outcome (i.e., Gaussian for continuous data, and Poisson for skewed count data) examining whether age at baseline, sex at birth, race/ethnicity, highest parental education, marital status, combined parental household income, CBCL externalizing T-score, and parental history of AUD and DUD were associated with total caffeine dose and alcohol sipping (total times had alcohol sips, total times had alcohol sips in non-religious context) outcomes after accounting for covariates (random effects for site and family ID (e.g., twin/triplet/sibling status)). Results were considered significant if they were at the p<.05 level; appropriate effect sizes (Cramer’s V (denoted as ϕc), Cohen’s d, and beta weights) were included for interpretation.
3. RESULTS
A. Demographic Variables.
Of the total baseline sample, 11,857 (99.8%) completed the SU assessment module. For overall sample demographics of the baseline ABCD participants, see Table 1.
Table 1:
Demographic Characteristics, CBCL Externalizing Symptoms T-Score, and Parental Family History of AUD and DUD in Baseline ABCD Study Participants (who completed the SU Module)
| ABCD Participants (n=11,857) Mean (SD) or %; Range |
|
|---|---|
|
| |
| Age | 9.9 (0.6); 9.0–10.9 |
|
| |
| Female | 47.8% (n=5,678) |
|
| |
| Twin/Singleton Status | |
| Singleton | 68.6% |
| Siblings | 13.4% |
| Twin | 17.7% |
| Triplet | 0.3% |
|
| |
| Race/Ethnicity | |
| Caucasian | 52.0% |
| Black | 15.0% |
| Asian-American | 2.1% |
| Hispanic | 20.3% |
| Others and >1 category) | 10.1% |
| Unknown | 0.5% |
|
| |
| Parental Household Income | |
| <50,000 | 27.1% |
| 50,000–100,000 | 25.9% |
| >100,000 | 38.4% |
| Unknown | 8.6% |
|
| |
| Parental Highest Education | |
| Post Graduate Degree | 34.0% |
| Bachelor’s Degree | 25.4% |
| Some College | 26.0% |
| High School Diploma/GED | 9.5% |
| <High School Diploma | 5.0% |
| Unknown | 0.1% |
|
| |
| Parental Marital Status | |
|
| |
| CBCL Externalizing T-Score | 45.7 (10.3); 33–84 |
|
| |
| Parental History of AUD | |
| No Parents | 85.4% |
| 1 Parent | 12.7% |
| 2 Parents | 1.9% |
|
| |
| Parental History of SUD | |
| No Parents | 89.3% |
| 1 Parent | 8.6% |
| 2 Parents | 2.1% |
Notes: Parent demographic variables include either parent or guardian/primary caregiver. CBCL= Child Behavior Checklist. Parental history of alcohol use disorder (AUD) and substance use disorder (SUD) was dummy-coded as density of biological parents meeting criteria for at least one symptom of AUD or SUD (0=no parents met criteria, 1= one parent met criteria, 2=both parents met criteria) based on the FHAM-S.
B. “Heard Of” Results
“Heard of” Descriptives.
The majority of youth in the sample endorsed having heard of alcohol (96.3%), caffeine (94.3%), nicotine products (93.4%), and cannabis products (55.6%), while fewer youth had heard of prescription or OTC drug misuse (34.8%) or inhalants (25.6%) (see Table 2). Only a small minority of youth had heard of “any other drug”: cocaine (5.4%), heroin (1.7%), methamphetamine (1.3%), anabolic steroids (0.9%), salvia (0.03%), psilocybin (0.2%), other hallucinogens (0.3%), cathinones (0.1%), MDMA (0.1%), GHB (0.04%), and ketamine (0.008%).
Table 2:
Substance Use Patterns in Baseline ABCD Study Participants According to Full Sample and Sex at Birth (n=11,857)
| Mean (SD) or %; Range | All (n=11,857) | Boys (n=6,179) | Girls (n=5,678) |
|---|---|---|---|
|
| |||
| Heard of = YES... | |||
| Caffeine | 94.3% | 94.4% | 94.2% |
| Alcohol | 96.3% | 96.2% | 96.4% |
| Nicotine Products* | 93.4% | 93.9% | 92.8% |
| Cannabis Products* | 55.6% | 59.8% | 51.1% |
| Inhalants* | 25.6% | 27.9% | 23.1% |
| Prescription Drug Abuse | 34.8% | 34.9% | 34.6% |
|
| |||
| Used Caffeine* | 67.6% | 70.2% | 64.7% |
|
| |||
| Sipped Alcohol* | 22.5% | 24.3% | 20.6% |
| Used Alcohol (full beverage)* | 0.18% | 0.26% | 0.09% |
|
| |||
| Tried Any Nicotine Product* | 0.68% | 0.89% | 0.37% |
| Cigarette | 0.08% | 0.10% | 0.05% |
| ENDS | 0.09% | 0.13% | 0.05% |
| Cigar | 0.08% | 0.09% | 0.07% |
| Hookah | 0.06% | 0.05% | 0.07% |
| Tobacco Pipe | 0.04% | 0.02% | 0.07% |
| Nicotine Replacement | 0.07% | 0.06% | 0.07% |
| Smokeless Tobacco | 0.10% | 0.16% | 0.04% |
|
| |||
| Tried Any Cannabis Product* | 0.10% | 0.18% | 0.02% |
| Smoked/Vaped Flower | 0.04% | 0.08% | 0% |
| Smoked Blunt | 0.008% | 0.02% | 0% |
| Edible | 0.008% | 0.02% | 0% |
| Smoked/Vaped Concentrate | 0.008% | 0.02% | 0% |
| Tincture | 0.008% | 0.02% | 0% |
| Cannabis/Alcohol Drink | 0.008% | 0.02% | 0% |
| Synthetic THC | 0% | 0% | 0% |
|
| |||
| Used Other Illicit Drug | |||
| Inhalants | 0.03% | 0.05% | 0% |
| Rx Stimulants | 0.02% | 0% | 0.04% |
| Rx Opioids | 0.008% | 0.02% | 0% |
| Rx Sedatives | 0.02% | 0.03% | 0% |
| OTC Cough Medicine | 0.03% | 0.03% | 0.04% |
| Cocaine | 0% | 0% | 0% |
| Cathinone | 0.008% | 0.02% | 0% |
| Methamphetamine | 0% | 0% | 0% |
| Ecstasy/MDMA | 0% | 0% | 0% |
| Ketamine | 0% | 0% | 0% |
| GHB | 0% | 0% | 0% |
| Heroin/Opium | 0% | 0% | 0% |
| Hallucinogens | 0% | 0% | 0% |
| Psilocybin | 0% | 0% | 0% |
| Salvia | 0% | 0% | 0% |
| Anabolic Steroids | 0% | 0% | 0% |
Notes:
= chi-square or t-test analyses revealed significant difference by sex.
Sex Differences: “Heard of” Items.
Males were significantly more likely than females to report having heard of nicotine (χ2(1)=6.1, p=0.013, ϕc=0.02), cannabis (χ2(1)=91.9, p=2.2e-16, ϕc=0.09), and inhalants (χ2(1)=36.5, p=1.208e-08, ϕc=0.05), no differences were seen in hearing of alcohol, caffeine, prescription/OTC drugs, or inhalants; see Table 2.
C. Substance Use Patterns
Caffeine Use.
The majority (67.6%) of youth reported consuming at least one type of caffeinated beverage during the past six months and the most popular beverage was soda (57.8%; see Table 2). A small minority of youth (7.4%) reported ingesting at least one standard dose of caffeine per week on average; see Table 3 & Figure 1 for details by beverage type.
Table 3:
Caffeine Use Patterns in Baseline ABCD Study Participants
| Caffeine Users (n=8,018) [% or Mean (SD)] | |
|---|---|
|
| |
| % Used Caffeine Beverage | 67.6% |
| Soda | 57.8% |
| Tea | 28.9% |
| Coffee | 14.7% |
| Espresso | 7.7% |
| Energy Drink | 2.3% |
|
| |
| Average Standard Dose* Per Week | 1.95 |
| Soda | 1.18 (4.56) |
| Tea | 0.56 (2.81) |
| Coffee | 0.15 (1.56) |
| Espresso | 0.04 (0.38) |
| Energy Drink | 0.02 (0.36) |
|
| |
| % Used Caffeine Daily | 7.4% |
| Soda | 4.2% |
| Tea | 2.4% |
| Coffee | 0.4% |
| Espresso | 0.05% |
| Energy Drink | 0.08% |
Dose= 1 8 oz cup for coffee or tea, 1 shot espresso, 12 oz soda, or 8 oz energy drink.
Figure 1:
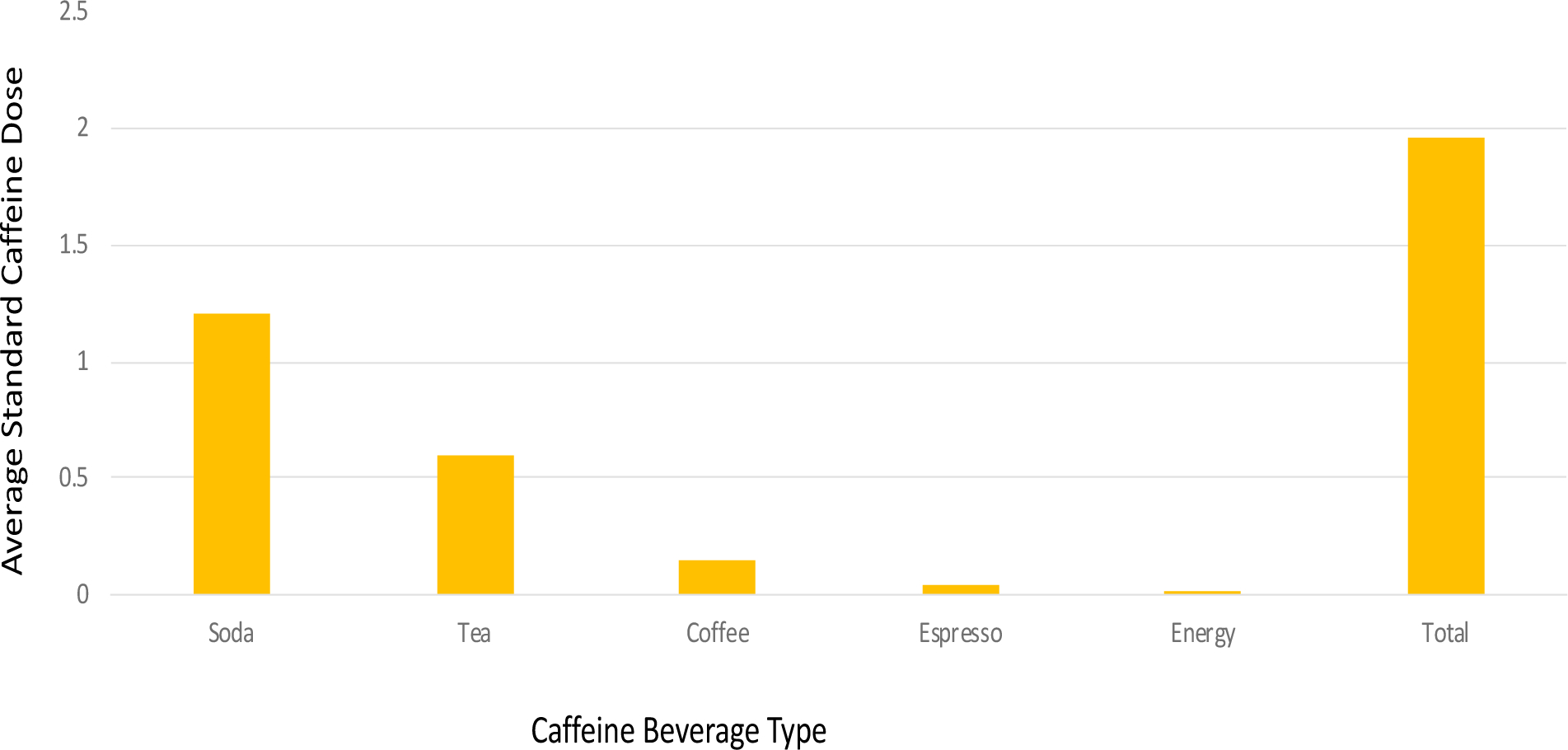
Average Caffeine Standard Dose per Week (Past 6 Months) for Soda, Tea, Coffee, Espresso, Energy Drinks, and Total Combined Dose in Baseline ABCD Study Participants. Dose= 8 oz cup for coffee or tea (532 mL), 1 shot espresso (30mL), 12 oz soda (355 mL), or 8 oz (236mL) energy drink.
Alcohol Use.
The next most commonly used substance was alcohol, with 22.5% (n=2,673) of youth reporting having a sip of alcohol in their lifetime. In contrast, only 21 youth reported having using a full drink of alcohol (0.18%). Of those 22.5% who reported sipping alcohol, youth reported sipping alcohol an average of 4.7 total times in their lifetime2. 17.1% of the total sample reported non-religious alcohol sipping3; the median age of first non-religious sipping was 8 years old. Although several of the non-religious sippers (45.5%) reported taking more than one sip, most youth did not finish the drink after consuming their first alcohol sip (98.4%). The vast majority of youth remembered taking their first sip of alcohol versus being told about the event (93.2%). See Table 4 for additional details.
Table 4:
Low-Level/First-Use Alcohol, Nicotine and Cannabis Use Patterns in Baseline ABCD Study Participants
| Mean (SD) or %; Range | |
|---|---|
|
| |
| Sipped Alcohol (non-religious; full sample) | 17.1% |
| Total Sipping Occasions (full sample) | 4.7 (19.2); 0–520 |
| Total Sipping Occasions (non-religious)± | 2.8 (7.67); 0–198 |
| > 1 Sip (non-religious) ± | 45.5% |
| Did Not Complete First Drink± | 98.4% |
| Age of First Sip Onset (years) ± | 7.32 (1.9); 1–11 |
|
| |
| Type of First Alcohol Sipped:± | |
| Beer | 41.3% |
| Wine/Champagne | 30.3% |
| Wine Cooler/Beer Substitute | 5.1% |
| Liquor Mixed Drink | 3.9% |
| Shots Liquor | 2.3% |
| Liqueur/Cordial | 0.6% |
| Malt Liquor | 0.2% |
| Fortified Wine | 0.05% |
| Other | 0.8% |
| Don’t Know | 15.4% |
|
| |
| First Sipped Alcohol Belonged To:± | |
| Dad | 42.1% |
| Mom | 37.0% |
| Other Guardian | 2.2% |
| Other Adult Family Member | 5.7% |
| Aunt or Uncle | 3.9% |
| Another Adult (Non-Family) | 2.2% |
| Underage (<21 yrs old) Sibling | 2.9% |
| Sibling 21 or Older | 2.9% |
| Friend | 0.2% |
| Person <20 yrs old (Non-Friend) | 0.2% |
| Stranger | 0.2% |
| Don’t Know | 5.2% |
|
| |
| How Received First Alcohol: ± | |
| Offered Sip | 72.8% |
| Accidently Took Sip | 21.9% |
| Intentionally Took Sip | 1.2% |
|
| |
| First Used Nicotine Product (n=75) Type: | |
| Cigarette | 38.7% |
| ENDS | 57.3% |
| Cigar | 4.3% |
| Hookah | 4.3% |
| Tobacco Pipe | 4.3% |
| Nicotine Replacement | 0% |
| Age of First Nicotine Puff (years) | 7.5 (1.9); 3–10 |
| Did Not Continue After First Puff | 85% |
| Nicotine Product Flavoring: | |
| Menthol or Mint | 10.7% |
| Other Flavoring | 36.0% |
| No Flavoring | 53.3% |
|
| |
| Tried Smokeless Tobacco (n=12) | 0.1% |
| Age of First Use (years) | 6.9 (1.7); |
| Did Not Continue After First Try | 100% |
| First Smokeless Tobacco Contained Flavoring: | |
| Menthol or Mint | 16.7% |
| Other Flavoring | 8.3% |
| No Flavoring | 75% |
|
| |
| Tried Cannabis Product (n=12) Type: | 0.1% |
| Smoked/Vaped Flower | 75% |
| Smoked/Vaped Strong/Potent Flower | 8.3% |
| Edible | 8.3% |
| Smoked/Vaped Concentrate or Oil | 8.3% |
| Tincture | 0% |
| Infused Alcohol Drink | 0% |
| Synthetic THC | 0% |
| Total Cannabis Puffs/Tastes | 7.4 (12.3); 1–40 |
| Age of First Cannabis Use (years) ± | 8.5 (1.7); 4–10 |
| Did Not Continue After First Try | 83% |
|
| |
| First Cannabis Product Provided By: | |
| Dad | 8.3% |
| Mom | 25.0% |
| Other Guardian | 0% |
| Other Adult Family Member | 8.3% |
| Aunt or Uncle | 16.7% |
| Another Adult (Non-Family) | 8.3% |
| Younger (<21 yrs old) Sibling | 16.7% |
| Sibling 21yrs or Older | 0% |
| Friend | 8.3% |
| Person <20 yrs old (Non-Friend) | 0% |
| Stranger | 0% |
| Don’t Know | 8.3% |
|
| |
| How Received First Cannabis Product: | |
| Offered | 50.0% |
| Accidently Took | 16.7% |
| Intentionally Took | 33.3% |
Notes:
Alcohol data only includes youth who endorsed non-religious alcohol sipping (n=2,034). Low-level (aka, first use) nicotine and cannabis data only include youth who endorsed trying a nicotine (n=75; n=12) or cannabis product (n=12).
Nicotine Use.
The next most commonly tried substance at baseline were nicotine products, as 81 (0.68%) youth reported having a “puff” or taste of a tobacco product or ENDS in their lifetime. Of the 81 youth who reported any nicotine use, 75 (0.6% of study participants) reported trying a puff of a tobacco product outside of a religious context. Twelve (0.1%) youth reported trying smokeless tobacco. (See Table 4 for more details characterizing their first nicotine use, including type of product, age of first use, and use of flavoring.) Nine youth reported having more than just a puff of a tobacco cigarette; 11 reported using ENDS (more than a puff) (.09%), 10 youth used a cigar (0.08%), 7 youth smoked hookah tobacco (0.06%), 5 youth reported using tobacco in a pipe (0.04%), and 8 reported using a nicotine replacement product (0.07%). Twelve (0.1%) youth in the sample used smokeless tobacco. See Table 2 for details.
Cannabis Use.
Twelve youth reported trying a “puff” or taste of a cannabis product (0.1%). On average, at baseline those youth had 7.4 puffs or tastes (median=1.5). For their first cannabis use, the majority smoked or vaped cannabis flower (75%; n=9). On average, during their first use, they reported that they felt “buzzed” (M=2.5, range 0–10 on a scale of 1–10). The vast majority (92%) remembered their first time using (versus being told about it). (See Table 4 for more details regarding the youth’s first cannabis use.) Five youth reported smoking or vaping more than a puff of cannabis flower, 1 youth smoked a blunt, 1 consumed a cannabis edible product, 1 used cannabis concentrate (e.g., vape pen, dabs), 1 used a cannabis tincture, 1 consumed a cannabis alcohol drink, and 0 used synthetic THC (see Table 2 for cannabis use details).
Other Illicit SU.
A very small subset (<0.02% for each drug category) of youth reported use of any other illicit drugs [inhalants (n=3), cathinones (n=1); prescription stimulant (n=2), opioid (n=1), sedative (n=2) and OTC cough medicine (n=4) misuse] (see Table 2 for use according to the whole cohort and by sex).
Sex Differences in SU Patterns4.
Males were significantly more likely than females to report using caffeine (χ2(1)=40.8, p=1.7e-10, ϕc=0.06), sipping alcohol (χ2(1)=22.8, p=0.000002, ϕc=0.04), having a full alcohol drink (χ2(1)=3.96, p=0.05, ϕc=0.02), puffing/trying a tobacco product (χ2(1)=7.5, p=0.006, ϕc=0.03), and puffing or trying a cannabis product (χ2(1)=6.02, p=0.01, ϕc=0.03). Males also reported significantly greater caffeine total dose (t(11,264)=−2.6, p=0.02, d=0.04) and greater total non-religious alcohol sips (t(11,747)=−2.47, p=0.01, d=0.05). There were no sex differences for any of the other SU outcomes (notably, there was very little use reported for other substances); see Table 2 for use rates according to sex at birth.
D. Multivariable Predictors of Caffeine & Alcohol
Total Caffeine Use.
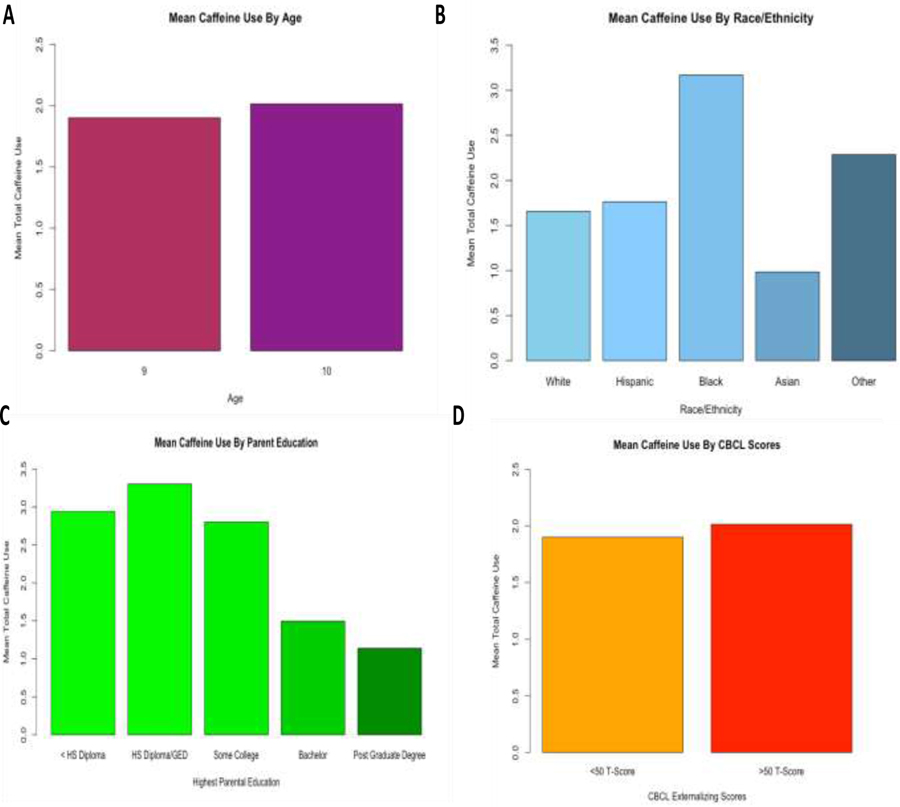
After statistically controlling for other demographics variables (sex, parental marital status, household income, parental history of AUD/ DUD) and accounting for site and twin/sibling status, we found that 10-year-olds (vs. 9-year-olds; b=.02, t=2.2, p=0.03), Hispanic youth (vs. Caucasian; b=−.40, t=−2.1, p=0.03), youth from families with lower parental education (less than high school (HS) diploma vs. Bachelor degree, b=−1.2, t=3.4, p=0.0007; less than HS diploma vs. postgraduate degree, b=−1.53, t=−4.3, p=0.00002), and youth with greater CBCL externalizing behaviors (b=.02, t=3.7, p=0.0002) reported significantly greater total average caffeine dosage per week (see Figure 3).
Figure 3:
Mean Caffeine Dose Per Week (Past Six Months) in Baseline ABCD Study Participants According to (A) Age, (B) Race/Ethnicity, (C) Highest Parental Education, and (D) CBCL Externalizing Behavior Scores.
Total Times Had Sip of Alcohol.
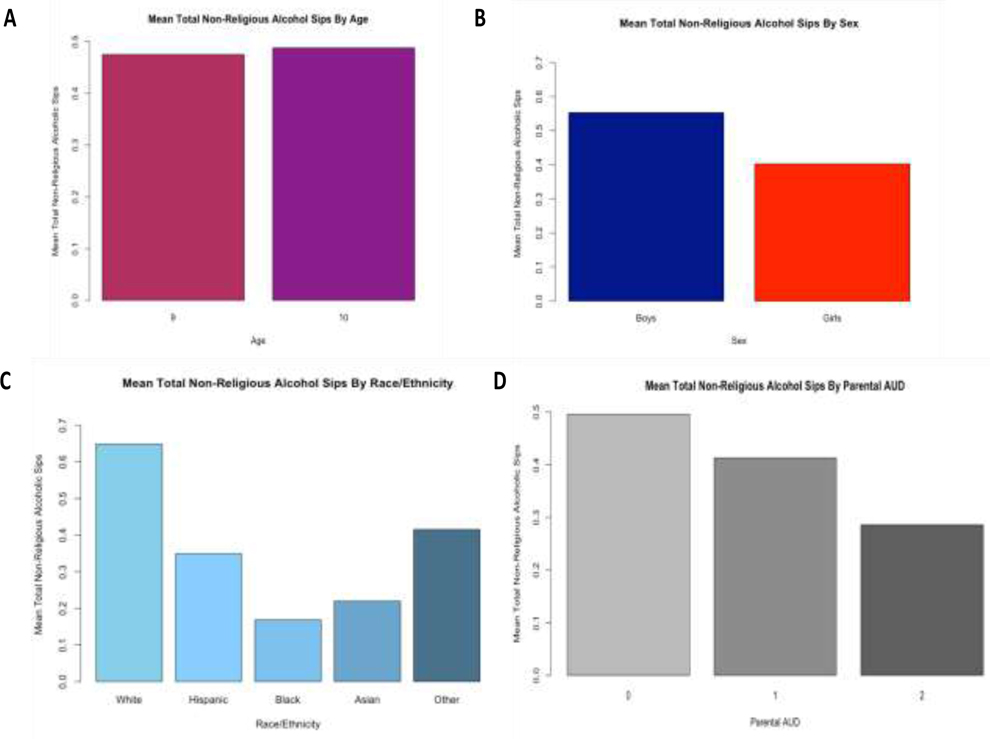
After controlling for the other demographic variables, site and twin/sibling status, 10-year-olds (vs. 9-year-olds; b=.02, t=6.1, p=1.4e-09), Caucasian youth (vs. African-American youth; b=−.21, t=−2.0, p=0.05), youth from married households (vs. unmarried households; b=.16, t=2.3, p=0.02), and youth with greater CBCL externalizing behaviors (b=.008, t=3.7, p=0.0003) reported greater total number times they had a sip of alcohol. Total Times Had Sip Alcohol (Non-Religious Context). We also found that 10-year-olds (vs. 9-year-olds; b=−.01, t=9.0, p=2e-16), boys (vs. girls; b=−.15, t=−3.1; p=0.002), Caucasian youth (vs. Asian-American youth; b=−.40, t=−2.0, p=0.05), and youth with a negative history of parental AUD (vs. positive parental history; b=−.15, t=−2.1, p=0.03) reported greater total number of times they had a sip of alcohol (non-religious context) (see Figure 4).
Figure 4:
Mean Total Times Sipped Alcohol (Non-Religious) in ABCD Study Participants at Baseline According to (A) Age, (B) Sex at Birth, (C) Race/Ethnicity, and (D) Parental AUD History Density.
4. DISCUSSION
The ABCD Study is the largest prospective study to date to examine the impact of various SU patterns on neurocognitive, health and affective outcomes. The sample is particularly unique in that it is large, geographically and demographically diverse, and provides detailed yearly assessments of individual/biological, neurocognitive, peer, family, cultural, and environment factors that can be harnessed to prospectively examine the onset, trajectories, and sequala of SU in adolescents (Jernigan, Brown et al. 2018, Volkow, Koob et al. 2018). Before scientists begin to examine predictors of SU initiation and trajectories in longitudinal analyses, full characterizing of the baseline SU patterns is needed. Here, we found that the most common early SU behavior was consuming caffeinated beverages (67.6%). Second to that was sipping alcohol (22.5%). Most notably, aside from caffeine use and sipping alcohol, SU was very low at baseline (0.7% for trying a nicotine product, 0.1% trying a cannabis product, and <0.02% for trying any other drug of abuse). Although very minimal SU initiation was reported, boys demonstrated an overall pattern of greater early use compared to girls. Further, demographics including age, ethnicity/race, parental education, marital status, parental history of AUD and youth externalizing behaviors were linked with early caffeine or alcohol sipping behavior, although effect sizes were generally small.
Given the common use of caffeinated beverages in children and teens (Ahluwalia and Herrick 2015), and the growing concerns over health effects and addiction risk associated with excessive caffeine use (Budney and Emond 2014) (Temple, Bernard et al. 2017) (Temple 2009), examining caffeine effects on health and neurodevelopment in youth is of increasing importance. The majority of the 9- and 10-year-olds in the ABCD cohort already initiated some low-level caffeine use at baseline, although they on average only consumed around two standard doses of caffeine per week (most commonly soda). Still, a notable 7.4% reported daily caffeine usage and a small group of youth (2.3%) reported consumption of energy drinks- which can contain higher doses of caffeine. Older youth, youth from families with lower parental education, Hispanic youth (vs. Caucasian), and youth with higher externalizing scores reported greater weekly caffeine use; the effect sizes for all relationships were small, with the exception of parental education, which demonstrated a large effect at baseline. These factors will need to be examined longitudinally in the ABCD cohort to determine whether they represent long-term risk factors for problematic caffeine consumption (>400 mg per day), development of a caffeine use disorder (Evatt, Juliano et al. 2016), and to examine the links between caffeine use and health and neurocognitive outcomes during adolescence.
The second most commonly used substance was alcohol, with 22.5% of youth reporting sipping alcohol (17.1% outside of a religious occasion). In the users, the average number of times they sipped alcohol (non-religious context) was relatively low (2.8 times) and the vast majority of the youth (98.4%) did not continue to finish a full alcoholic drink after their first sip. Interestingly, for their first sip, the majority were offered the alcoholic beverage (72.8%) by a parent or guardian (81.3%). Risk-factors related to increased total times youth sipped alcohol included being older (10- vs. 9-years-old), Caucasian (vs. African-American), living in a married household (vs. unmarried household), and having greater CBCL externalizing behaviors. Further, older youth, boys (vs. girls), Caucasian youth (compared to Asian youth), and youth without a history of parental AUD also reported greater total times sipped alcohol outside of a religious context. Notably, all statistical effect sizes were considered to be in the small range, demonstrating subtle relationships at baseline. These findings are consistent with prior research demonstrating that sipping at this age (prior to high-school) generally occurs within a family context (Donovan and Molina 2008) and alcohol beverages are being offered primarily by parents (Jackson, Barnett et al. 2015). Our findings are also consistent with prior smaller regional studies reporting increased risk of early sipping linked with increased age (Donovan 2007), being Caucasian (vs. African-American) (Donovan and Molina 2008) and male (Donovan 2007). Uniquely, we found that youth from married households reported greater sipping occasions compared to unmarried households, which is partially discrepant with one prior study that reported an earlier age of onset of sipping in single-mother headed households (Donovan and Molina 2011); however, it is notable that this effect size was small and our study did not specifically categorize whether the household was considered a single-mother headed household. Positive parental history of AUD was linked with fewer sipping occasions, a finding partially discrepant with regional studies finding parental drinking history to be positively associated with early adolescent sipping (Donovan and Molina 2008) (Donovan and Molina 2011). Examining the influence of parental AUD history on other influential factors such as parental monitoring, household alcohol rules, availability, alcohol expectancies and alcohol trajectories in the ABCD Study cohort will be an important future direction (Lisdahl et al., 2018). Consistent with the prior literature linking externalizing behaviors with development of SUD (e.g., (Grant and Dawson 1997) (Dawson, Goldstein et al. 2008) (Loeber, Clark et al. 2018)), here we found early associations between externalizing behaviors and total alcohol sipping occasions, although effect sizes were generally small. These early risk factors will need to be considered when prospectively examining the impact of early alcohol use on risk for problematic alcohol use trajectories in the ABCD Cohort as they age. Given that prior research links early alcohol sipping with risky adolescent drinking patterns and AUD development (Jackson, Barnett et al. 2015) (Grant and Dawson 1997), even when the alcohol is provided by parents (Kaynak, Winters et al. 2014), it is recommended that healthcare providers discuss household alcohol rules and sipping behavior with parents and youth as young as seven to eight years old.
Recently ENDS use has grown in popularity in adolescents as young as 13–14 years old (Miech 2019) (Johnston 2020), although reports in younger cohorts are unavailable. In the current sample, few of the 9–10-year-olds reported any nicotine product use. Only 81 youth (0.68%) reported trying a “puff” of a tobacco product such as ENDS or cigarettes. Consistent with the MTF Study reports (Miech 2019), the most commonly first-used nicotine product was ENDS (57.3%). The majority of youth did not continue to use the product after their first try (85%), and the median age of first use was 7.5 years old. Thus, the ABCD cohort can be considered generally naïve to nicotine usage at baseline, although low-level early experimentation is starting as young as 6–7 years old, supporting prevention campaigns aimed at elementary-aged youth.
Notably, other SU (including cannabis use), was very rare in the 9- and 10-year-olds. Twelve youth (0.1%) reported trying a cannabis product, most commonly smoking or vaping cannabis flower, although at least one youth reported trying other products (including blunts, cannabis edibles, cannabis concentrate or oil). The latter supports prior studies suggesting that measuring multiple routes of administration (e.g., vaping, smoking, ingestion) and types of cannabis product (e.g., flower, edibles, concentrates) (Streck, Hughes et al. 2019) is important, even in young cohorts. We also found that only a small fraction (<0.03%) of youth reporting use of any other drugs of abuse. Findings support the ABCD Study aims to prospectively determine the impact of cannabis and other illicit drug use onset on neurocognitive and health outcomes, as the baseline cohort can be considered naïve to cannabis and other illicit-drugs.
Across several indices, males showed a riskier early substance experimentation pattern. They were significantly more likely to hear of nicotine, cannabis, and inhalant products. Despite being the same age, boys were more likely to use caffeine, consume a greater caffeine dose, sip alcohol, have greater non-religious alcohol sipping occasions, drink a full drink of alcohol, and try a nicotine or cannabis product compared to girls. Notably, effect sizes for these findings were generally small at this time-point, meaning sex differences at baseline may be considered subtle. Further, sex differences in caffeine use and alcohol sipping occasions were no longer significant in the multivariable analysis after accounting for other demographics, externalizing behaviors, and parental AUD or SUD. Still, these findings support prior studies showing increased risk of alcohol sipping in boys (Donovan 2007) and suggest that future longitudinal SU analyses with the ABCD cohort need to carefully consider sex differences.
Potential limitations of the current study should be considered. Substance use was based on self-report and the current study did not discuss toxicology findings primarily due to low availability at baseline; toxicology collection is increased at follow-up time-points and will be integrated into NDA 3.0/4.0 data releases. For this analysis, the aims were to provide a detailed description of the SU patterns reported by youth enrolled in the ABCD Study at the baseline session to inform the broad scientific community as they plan their longitudinal analyses; therefore, demographic corrections were not employed. Several other potential risk and protective factors were not analyzed here; more thorough examination of broad risk factors linked with early caffeine use and alcohol sipping are future directions (e.g., for a recent analysis examining personality factors associated with sipping, see (Watts, Wood et al. 2020). Finally, although the ABCD Study is a national, diverse study, it cannot be considered fully nationally-representative (Compton, Dowling et al. 2019).
In conclusion, youth who participated at the baseline time-point of the ABCD Study can be considered relatively substance-naïve with low-levels of caffeine use and alcohol sipping experimentation. Ongoing longitudinal assessment of these domains over a period of ten years in a socio-demographically diverse, nationwide sample of youth presents an unprecedented opportunity to examine the risk and protective factors influencing the onset, trajectories and sequela of SU, the impact of SU on neurocognitive and brain development, health and psychosocial outcomes, and to further understand the timing and interactive relationship between SU and psychopathology in youth that live in the United States.
Figure 2:
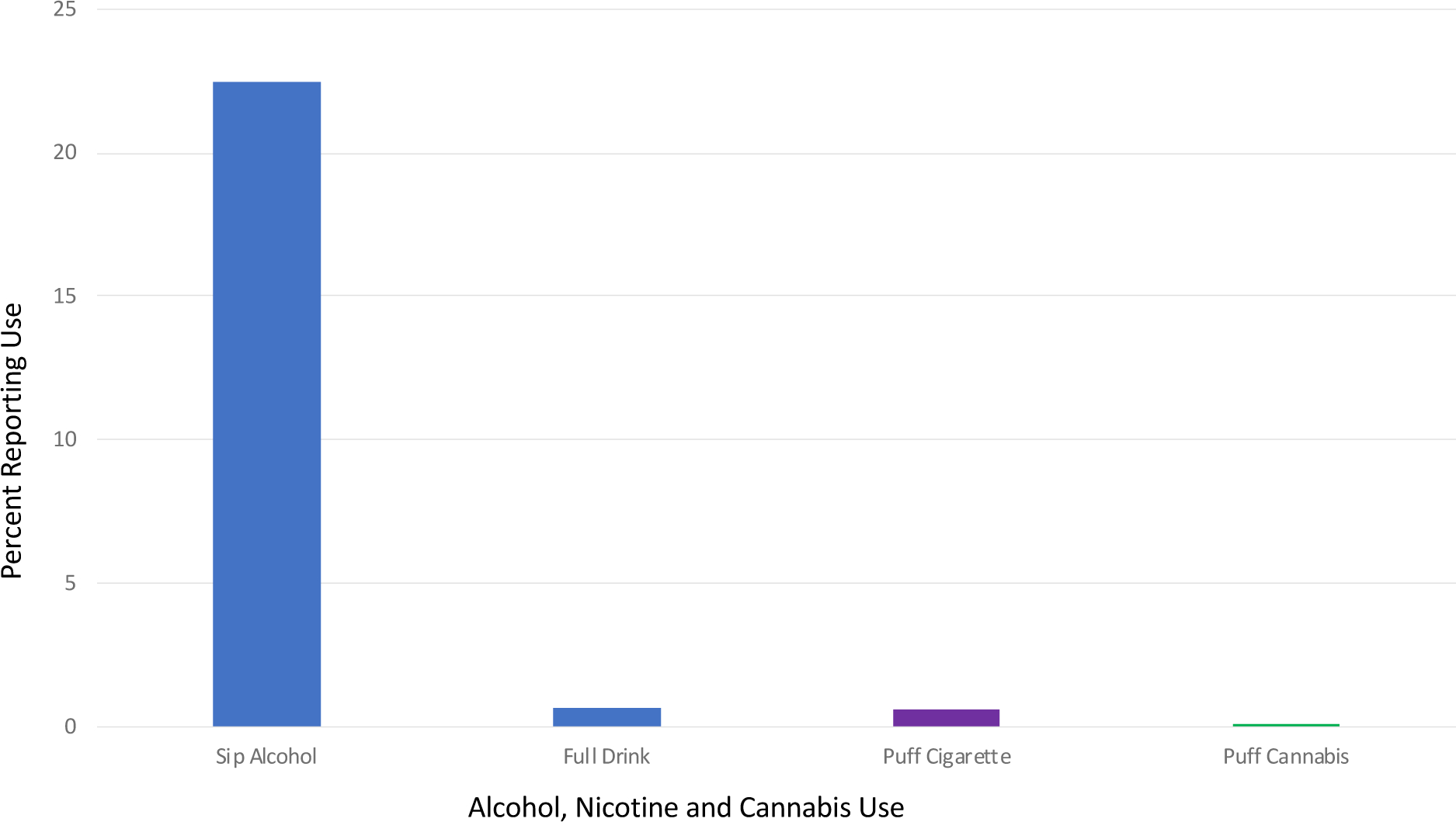
Percentage of ABCD Participants Reporting Alcohol (Sip, Full Alcohol Drink), Nicotine (Puff/Taste), and Cannabis (Puff/Taste) Use at Baseline.
Highlights.
The Adolescent Brain Cognitive Development ™ Study (ABCD StudyⓇ) is an open-science, multi-site, prospective, longitudinal study following over 11,800 9- and 10-year-old youth into early adulthood.
At baseline, the majority of the ABCD Study youth reported recently using caffeine (67.6%) and 22.5% reported sipping alcohol.
Beyond caffeine consumption and alcohol sipping, the ABCD Study cohort reported little to no use of drugs of abuse (0.2% full alcohol drink, 0.7% used nicotine, 0.1% used cannabis, <0.02% used any other drug of abuse) at baseline.
Results revealed that total caffeine use and early alcohol sipping were linked with demographic variables (sex, age, ethnicity/race, parental education, parental marital status), externalizing behaviors, and parental history of AUD. These factors will need to be considered in longitudinal analyses.
Aside from caffeine use and early alcohol sipping, the baseline ABCD Study cohort can be considered relatively substance-naïve; this supports the aims of the ABCD Study to prospectively examine the impact of escalating SU trajectories on neurocognitive, psychopathology and health outcomes.
Acknowledgements
Data used in the preparation of this article were obtained from the Adolescent Brain Cognitive DevelopmentSM (ABCD) Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA). This is a multisite, longitudinal study designed to recruit more than 10,000 children age 9–10 and follow them over 10 years into early adulthood. The ABCD Study® is supported by the National Institutes of Health and additional federal partners under award numbers U01DA041048, U01DA050989, U01DA051016, U01DA041022, U01DA051018, U01DA051037, U01DA050987, U01DA041174, U01DA041106, U01DA041117, U01DA041028, U01DA041134, U01DA050988, U01DA051039, U01DA041156, U01DA041025, U01DA041120, U01DA051038, U01DA041148, U01DA041093, U01DA041089, U24DA041123, U24DA041147. A full list of supporters is available at https://abcdstudy.org/federal-partners.html. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/consortium_members/. ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in analysis or writing of this report. This manuscript reflects the views of the authors and may not reflect the opinions or views of the NIH or ABCD consortium investigators. The ABCD data repository grows and changes over time. The ABCD data used in this report came from the ABCD Data Release 2.0 (DOI: 10.15154/1503209, March 2019) and ABCD Fix Release 2.0.1 (DOI: 10.15154/1504041, July 2019).
Disclosure Statement
Martin Paulus is an adviser to Spring Care (New York City, NY, USA), a behavioral health startup. He has received royalties for an article about methamphetamine in UpToDate (Wolters Kluwer; Waltham, MA, USA).
Andrew Nencka receives research funding from GE Healthcare.
Kevin M. Gray provided consultation for Pfizer, Inc.
Susan R.B. Weiss and her husband own stock in Merck and GE, respectively.
Marilyn A. Huestis is a consultant for PinneyAssociates, Canopy Health Innovations, and AlgometRx.
Damien A. Fair and Nico U.F. Dosenbach are patent holders on the Framewise Integrated Real-Time Motion Monitoring (FIRMM) software and co-founders of Nous Imaging Inc. The nature of this financial interest and the design of the study have been reviewed by two committees at Oregon Health and Science University and Washington University School of Medicine. They have put in place plans to help ensure that this research study is not affected by the financial interests.
Anders M. Dale reports that he is a Founder of and holds equity in CorTechs Labs, Inc., and serves on its Scientific Advisory Board. He is a member of the Scientific Advisory Board of Human Longevity, Inc., and receives funding through research grants with General Electric Healthcare. The terms of these arrangements have been reviewed by and approved by the University of California, San Diego in accordance with its conflict of interest policies.
All other authors report no potential conflicts of interest.
Footnotes
At baseline, ENDS use is described as including “electronic cigarettes, vape pens, or e-hookah” and may include products that contain only flavoring. Whether the ENDS contains nicotine is asked as a follow-up question.
The iSay Sip inventory was missing for 4 participants who initially endorsed lifetime sipping.
Due to an initial gating error in RedCap, follow-up questions in the iSay Sip inventory were only collected on 2,016 of the 2,034 youth who reported non-religious sipping.
n=3 participants with substance use data had sex missing or reported response other than male or female for sex; due to low sample size they were excluded from this analysis.
Publisher's Disclaimer: This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ahluwalia N and Herrick K (2015). “Caffeine intake from food and beverage sources and trends among children and adolescents in the United States: review of national quantitative studies from 1999 to 2011.” Adv Nutr 6(1): 102–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahluwalia N, Herrick K, Moshfegh A and Rybak M (2014). “Caffeine intake in children in the United States and 10-y trends: 2001–2010.” Am J Clin Nutr 100(4): 1124–1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auchter AM, Hernandez Mejia M, Heyser CJ, Shilling PD, Jernigan TL, Brown SA, Tapert SF and Dowling GJ (2018). “A description of the ABCD organizational structure and communication framework.” Dev Cogn Neurosci 32: 8–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barch DM, Albaugh MD, Avenevoli S, Chang L, Clark DB, Glantz MD, Hudziak JJ, Jernigan TL, Tapert SF, Yurgelun-Todd D, Alia-Klein N, Potter AS, Paulus MP, Prouty D, Zucker RA and Sher KJ (2018). “Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: Rationale and description.” Dev Cogn Neurosci 32: 55–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budney AJ and Emond JA (2014). “Caffeine addiction? Caffeine for youth? Time to act!” Addiction 109(11): 1771–1772. [DOI] [PubMed] [Google Scholar]
- Casey BJ, Cannonier T, Conley MI, Cohen AO, Barch DM, Heitzeg MM, Soules ME, Teslovich T, Dellarco DV, Garavan H, Orr CA, Wager TD, Banich MT, Speer NK, Sutherland MT, Riedel MC, Dick AS, Bjork JM, Thomas KM, Chaarani B, Mejia MH, Hagler DJ, Daniela Cornejo M, Sicat CS, Harms MP, Dosenbach NUF, Rosenberg M, Earl E, Bartsch H, Watts R, Polimeni JR, Kuperman JM, Fair DA, Dale AM and Workgroup AIA (2018). “The Adolescent Brain Cognitive Development (ABCD) study: Imaging acquisition across 21 sites.” Dev Cogn Neurosci 32: 43–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey BJ, Getz S and Galvan A (2008). “The adolescent brain.” Dev Rev 28(1): 62–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey BJ, Giedd JN and Thomas KM (2000). “Structural and functional brain development and its relation to cognitive development.” Biol Psychol 54(1–3): 241–257. [DOI] [PubMed] [Google Scholar]
- Compton WM, Dowling GJ and Garavan H (2019). “Ensuring the Best Use of Data: The Adolescent Brain Cognitive Development Study.” JAMA Pediatr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran CP and Marczinski CA (2017). “Taurine, caffeine, and energy drinks: Reviewing the risks to the adolescent brain.” Birth Defects Res 109(20): 1640–1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Chou SP, Ruan WJ and Grant BF (2008). “Age at first drink and the first incidence of adult-onset DSM-IV alcohol use disorders.” Alcohol Clin Exp Res 32(12): 2149–2160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan JE (2007). “Really underage drinkers: the epidemiology of children’s alcohol use in the United States.” Prev Sci 8(3): 192–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan JE (2013). “The burden of alcohol use: focus on children and preadolescents.” Alcohol Res 35(2): 186–192. [PMC free article] [PubMed] [Google Scholar]
- Donovan JE and Molina BS (2008). “Children’s introduction to alcohol use: sips and tastes.” Alcohol Clin Exp Res 32(1): 108–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan JE and Molina BS (2011). “Childhood risk factors for early-onset drinking.” J Stud Alcohol Drugs 72(5): 741–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan JE and Molina BS (2014). “Antecedent predictors of children’s initiation of sipping/tasting alcohol.” Alcohol Clin Exp Res 38(9): 2488–2495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Ross J, Hawkins J, Harris WA, Lowry R, McManus T, Chyen D, Shanklin S, Lim C, Grunbaum JA and Wechsler H (2006). “Youth risk behavior surveillance--United States, 2005.” MMWR Surveill Summ 55(5): 1–108. [PubMed] [Google Scholar]
- Evatt DP, Juliano LM and Griffiths RR (2016). “A brief manualized treatment for problematic caffeine use: A randomized control trial.” J Consult Clin Psychol 84(2): 113–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garavan H, Bartsch H, Conway K, Decastro A, Goldstein RZ, Heeringa S, Jernigan T, Potter A, Thompson W and Zahs D (2018). “Recruiting the ABCD sample: Design considerations and procedures.” Dev Cogn Neurosci 32: 16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner M and Steinberg L (2005). “Peer influence on risk taking, risk preference, and risky decision making in adolescence and adulthood: an experimental study.” Dev Psychol 41(4): 625–635. [DOI] [PubMed] [Google Scholar]
- Giedd JN, Snell JW, Lange N, Rajapakse JC, Casey BJ, Kozuch PL, Vaituzis AC, Vauss YC, Hamburger SD, Kaysen D and Rapoport JL (1996). “Quantitative magnetic resonance imaging of human brain development: ages 4–18.” Cereb Cortex 6(4): 551–560. [DOI] [PubMed] [Google Scholar]
- Gogtay N, Giedd JN, Lusk L, Hayashi KM, Greenstein D, Vaituzis AC, Nugent TF 3rd, Herman DH, Clasen LS, Toga AW, Rapoport JL and Thompson PM (2004). “Dynamic mapping of human cortical development during childhood through early adulthood.” Proc Natl Acad Sci U S A 101(21): 8174–8179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF and Dawson DA (1997). “Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: results from the National Longitudinal Alcohol Epidemiologic Survey.” J Subst Abuse 9: 103–110. [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N and Conde JG (2009). “Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support.” J Biomed Inform 42(2): 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houston SM, Herting MM and Sowell ER (2014). “The neurobiology of childhood structural brain development: conception through adulthood.” Curr Top Behav Neurosci 16: 3–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacono WG, Heath AC, Hewitt JK, Neale MC, Banich MT, Luciana MM, Madden PA, Barch DM and Bjork JM (2018). “The utility of twins in developmental cognitive neuroscience research: How twins strengthen the ABCD research design.” Dev Cogn Neurosci 32: 30–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute PPR (2012). Texas School Survey of Drug and Alcohol Use: 2012. State: Grades 4–6. College Station, TX, Texas A&M University: 53 pp. [Google Scholar]
- Jackson C, Ennett ST, Dickinson DM and Bowling JM (2013). “Attributes that differentiate children who sip alcohol from abstinent peers.” J Youth Adolesc 42(11): 1687–1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KM, Barnett NP, Colby SM and Rogers ML (2015). “The prospective association between sipping alcohol by the sixth grade and later substance use.” J Stud Alcohol Drugs 76(2): 212–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KM, Colby SM, Barnett NP and Abar CC (2015). “Prevalence and correlates of sipping alcohol in a prospective middle school sample.” Psychol Addict Behav 29(3): 766–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jernigan TL, Brown SA and Coordinators AC (2018). “Introduction.” Dev Cogn Neurosci 32: 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, & Patrick ME (2020). Monitoring the Future national survey results on drug use, 1975–2019: Overview, key findings on adolescent drug use. Ann Arbor, Institute for Social Research, The University of Michigan: 124. [Google Scholar]
- Kaynak Ö, Winters KC, Cacciola J, Kirby KC and Arria AM (2014). “Providing alcohol for underage youth: what messages should we be sending parents?” J Stud Alcohol Drugs 75(4): 590–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laird NM and Ware JH (1982). “Random-effects models for longitudinal data.” Biometrics 38(4): 963–974. [PubMed] [Google Scholar]
- Lenroot RK and Giedd JN (2006). “Brain development in children and adolescents: insights from anatomical magnetic resonance imaging.” Neurosci Biobehav Rev 30(6): 718–729. [DOI] [PubMed] [Google Scholar]
- Lisdahl KM, Sher KJ, Conway KP, Gonzalez R, Feldstein Ewing SW, Nixon SJ, Tapert S, Bartsch H, Goldstein RZ and Heitzeg M (2018). “Adolescent brain cognitive development (ABCD) study: Overview of substance use assessment methods.” Dev Cogn Neurosci 32: 80–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeber R, Clark DB, Ahonen L, FitzGerald D, Trucco EM and Zucker RA (2018). “A brief validated screen to identify boys and girls at risk for early marijuana use.” Dev Cogn Neurosci 32: 23–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luciana M, Bjork JM, Nagel BJ, Barch DM, Gonzalez R, Nixon SJ and Banich MT (2018). “Adolescent neurocognitive development and impacts of substance use: Overview of the adolescent brain cognitive development (ABCD) baseline neurocognition battery.” Dev Cogn Neurosci 32: 67–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech RA, Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME (2018) “Monitoring the Future national survey results on drug use, 1975–2017: Volume I, Secondary school students.”. [Google Scholar]
- Miech RA, Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, & Patrick ME (2019). Monitoring the Future national survey results on drug use, 1975–2018: Volume I, Secondary School students. Ann Arbor, Michigan., Ann Arbor: Institute for Social Research, University of Michigan.: 586 pp. [Google Scholar]
- Mills KL, Goddings AL, Clasen LS, Giedd JN and Blakemore SJ (2014). “The developmental mismatch in structural brain maturation during adolescence.” Dev Neurosci 36(3–4): 147–160. [DOI] [PubMed] [Google Scholar]
- Quality C. f. B. H. S. a. (2014). 2015 National Survey on Drug Use and Health (NSDUH): CAI Specifications for Programming (English Version). Rockville, MD., Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Rice JP, Reich T, Bucholz KK, Neuman RJ, Fishman R, Rochberg N, Hesselbrock VM, Nurnberger JI, Schuckit MA and Begleiter H (1995). “Comparison of direct interview and family history diagnoses of alcohol dependence.” Alcohol Clin Exp Res 19(4): 1018–1023. [DOI] [PubMed] [Google Scholar]
- Robinson SM, Sobell LC, Sobell MB and Leo GI (2014). “Reliability of the Timeline Followback for cocaine, cannabis, and cigarette use.” Psychol Addict Behav 28(1): 154–162. [DOI] [PubMed] [Google Scholar]
- Schmitt JE, Neale MC, Fassassi B, Perez J, Lenroot RK, Wells EM and Giedd JN (2014). “The dynamic role of genetics on cortical patterning during childhood and adolescence.” Proc Natl Acad Sci U S A 111(18): 6774–6779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC and Sobell MB (1996). Timeline FollowBack: A calendar method for assessing alcohol and drug use. User’s Guide. Toronto, Ontario, Addiction Research Foundation. [Google Scholar]
- Somerville LH, Jones RM and Casey BJ (2010). “A time of change: behavioral and neural correlates of adolescent sensitivity to appetitive and aversive environmental cues.” Brain Cogn 72(1): 124–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sowell ER, Thompson PM, Holmes CJ, Jernigan TL and Toga AW (1999). “In vivo evidence for post-adolescent brain maturation in frontal and striatal regions.” Nat Neurosci 2(10): 859–861. [DOI] [PubMed] [Google Scholar]
- Sowell ER, Thompson PM, Leonard CM, Welcome SE, Kan E and Toga AW (2004). “Longitudinal mapping of cortical thickness and brain growth in normal children.” J Neurosci 24(38): 8223–8231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sowell ER, Trauner DA, Gamst A and Jernigan TL (2002). “Development of cortical and subcortical brain structures in childhood and adolescence: a structural MRI study.” Dev Med Child Neurol 44(1): 4–16. [DOI] [PubMed] [Google Scholar]
- Streck JM, Hughes JR, Klemperer EM, Howard AB and Budney AJ (2019). “Modes of cannabis use: A secondary analysis of an intensive longitudinal natural history study.” Addict Behav 98: 106033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temple JL (2009). “Caffeine use in children: what we know, what we have left to learn, and why we should worry.” Neurosci Biobehav Rev 33(6): 793–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temple JL, Bernard C, Lipshultz SE, Czachor JD, Westphal JA and Mestre MA (2017). “The Safety of Ingested Caffeine: A Comprehensive Review.” Front Psychiatry 8: 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TM A (2009). The Achenbach System of Emprically Based Assessment (ASEBA): Development, Findings, Theory and Applications. Burlington, VT:, University of Vermont Research Center for Children, Youth, and Families. [Google Scholar]
- Uban KA, Horton MK, Jacobus J, Heyser C, Thompson WK, Tapert SF, Madden PAF, Sowell ER and Study ABCD (2018). “Biospecimens and the ABCD study: Rationale, methods of collection, measurement and early data.” Dev Cogn Neurosci 32: 97–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Koob GF, Croyle RT, Bianchi DW, Gordon JA, Koroshetz WJ, Pérez-Stable EJ, Riley WT, Bloch MH, Conway K, Deeds BG, Dowling GJ, Grant S, Howlett KD, Matochik JA, Morgan GD, Murray MM, Noronha A, Spong CY, Wargo EM, Warren KR and Weiss SRB (2018). “The conception of the ABCD study: From substance use to a broad NIH collaboration.” Dev Cogn Neurosci 32: 4–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadolowski M, Bruno R, Aiken A, Stone C, Najman J, Kypri K, Slade T, Hutchinson D, McBride N and Mattick RP (2015). “Sipping, drinking, and early adolescent alcohol consumption: a cautionary note.” Alcohol Clin Exp Res 39(2): 350–354. [DOI] [PubMed] [Google Scholar]
- Wadolowski M, Hutchinson D, Bruno R, Aiken A, Clare P, Slade T, Najman J, Kypri K, McBride N and Mattick RP (2015). “Early Adolescent Alcohol Use: Are Sipping and Drinking Distinct?” Alcohol Clin Exp Res 39(9): 1805–1813. [DOI] [PubMed] [Google Scholar]
- Watts AL, Wood PK, Jackson KM, Lisdahl KM, Heitzeg MM, Gonzalez R, Tapert SF, Barch DM and Sher KJ (2020). “Incipient alcohol use in childhood: Early alcohol sipping and its relations with psychopathology and personality.” Dev Psychopathol: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson AL, Halpern CT, Herring AH, Shanahan M, Ennett ST, Hussey JM and Harris KM (2016). “Testing Longitudinal Relationships Between Binge Drinking, Marijuana Use, and Depressive Symptoms and Moderation by Sex.” J Adolesc Health 59(6): 681–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windle M (2020). “Sex differences in substance use from adolescence to young adulthood: Tests of increases in emergent adulthood and maturing out in later young adulthood.” Drug Alcohol Depend 207: 107813. [DOI] [PubMed] [Google Scholar]
- Zucker RA, Gonzalez R, Feldstein Ewing SW, Paulus MP, Arroyo J, Fuligni A, Morris AS, Sanchez M and Wills T (2018). “Assessment of culture and environment in the Adolescent Brain and Cognitive Development Study: Rationale, description of measures, and early data.” Dev Cogn Neurosci 32: 107–120. [DOI] [PMC free article] [PubMed] [Google Scholar]