Abstract
The 2017 National Inpatient Sample database was utilized to investigate the association between cannabis legalization in the United States and hospitalizations for psychosis associated with cannabis use. We compared the odds of hospital discharges for psychosis associated with cannabis use in adults between the Pacific census division (where most states legalized recreational cannabis use) and other divisions using multivariable logistic regression, adjusting for confounders. We calculated a score for each census division representing cannabis legality as the population-weighted sum of state scores: 1=illegal or cannabidiol/low potency cannabis; 2= medical marijuana; and 3=recreational and medical marijuana legalized. Pearson’s correlation coefficients (r) quantified the relationship between scores and the proportion of hospitalizations with psychosis associated with cannabis. In 2017, there were an estimated 129,070 hospital discharges for psychosis associated with cannabis use. The Pacific census division had significantly higher odds of discharges than other divisions (adjusted odds ratio 1.55; 95% confidence interval 1.25 – 1.93). There was a significant correlation between the cannabis legality score and proportion of hospital discharges for psychosis associated with cannabis use (r=0.67, p<0.05). In conclusion, we observed a higher proportion of hospital discharges for psychosis associated with cannabis use in areas with more liberal cannabis legalization laws.
Keywords: cannabis, marijuana, legalization, psychosis, schizophrenia
1. INTRODUCTION
Cannabis is the most prevalent illicit substance in the United States (Substance Abuse and Mental Health Services Administration, 2018). As more states are legalizing cannabis for recreational and/or medical purposes in the US, the prevalence of cannabis use has increased. Among persons aged 18 years or older, the prevalence of current users in the past month increased from 6.0% in 2002 to 9.9% in 2017 (Center for Behavioral Health Statistics and Quality, 2018). Approximately 20–30% of individuals who use cannabis meet criteria for a cannabis use disorder (Hasin, 2018). As of November 2020, thirty-six states and the District of Columbia (D.C.) legalized medical marijuana use, with fifteen states and D.C. also legalizing recreational use in adults 21 years and older (Marijuana Policy Project website, 2021). Prior studies found increased marijuana use and cannabis use disorders among adults residing in states that have implemented medical and recreational marijuana laws compared to states without legalization (Cerdá et al., 2020; Hasin et al., 2017). Benefits of cannabis include improvement of chronic non-cancer pain and pain associated with cancer, multiple sclerosis, arthritis and human immunodeficiency virus (HIV)-associated neuropathy (Claflin et al., 2018; Johal et al., 2020; Phillips et al., 2010; Zajicek et al., 2012). Although the evidence for the use of medical cannabis is growing (Haffajee, 2021; Hesketh et al., 2017; Zajicek et al., 2012), so is the concern for the association between cannabis use and psychotic disorders (Andréasson et al., 1987; Henquet et al., 2005; van Os, 2002). There is currently a paucity of research on the impact of cannabis legalization on the risk of psychosis.
Psychotic disorders typically start in adolescence or young adulthood, with a substantial proportion of patients having difficulty completing education, maintaining employment and living independently as well as an increased risk of suicide and homelessness (Chong et al., 2009; Folsom et al., 2005; Marwaha and Johnson, 2004; Palmer et al., 2005; Ramsay et al., 2012). Increased cannabis use could lead to a higher rate of hospitalizations for psychosis by increasing the risk of developing an initial episode of psychosis, precipitating acute toxic reactions with psychotic symptoms, or increasing the likelihood of hospitalization for those with pre-existing psychotic disorders. There is nearly a four-fold risk increase in risk of developing schizophrenia or other psychotic disorders among heavy users of cannabis compared to non-users (Marconi et al., 2016). Daily use and higher potency cannabis with greater levels of tetrahydrocannabinol (THC) confers the highest risk of developing a psychotic disorder (Di Forti et al., 2009). Randomized controlled studies reveal that acute administration of THC in healthy individuals is associated with induction of psychotic symptoms (D’Souza et al., 2004). Finally, existing research shows that patients with schizophrenia who use cannabis are more likely to experience relapses requiring hospitalization (van Dijk et al., 2012).
We conducted a cross-sectional nationwide study to examine the association between geographical variation in hospitalizations for psychosis associated with cannabis use and cannabis legalization policies in 2017. We hypothesized that census divisions with more liberal cannabis legalization policies would have a greater rate of hospitalizations for psychosis with cannabis use. If our hypothesis is confirmed, this initial study will justify the need for follow-up studies using longitudinal state-level data to examine impact of state policies on trends in psychosis associated with cannabis use.
2. METHODS
2.1. Data Source and Study Population
This cross-sectional study used hospital discharge data from the 2017 National Inpatient Sample (NIS), Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality (Agency for Healthcare Research and Quality, 2017). The NIS utilizes a complex sampling design that samples 20% of hospital discharges from state hospital discharge databases in 47 states and D.C. Hospital discharges are stratified by census division, hospital location (urban or rural), teaching status, ownership and bed size. The complex sampling design allows for national estimates, as the sampling frame covers 96% of hospital discharges and more than 97% of the U.S. population. Billing data submitted by hospitals provide International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis codes for each hospitalization. The study population includes hospital discharges for adults between the ages of 18 and 64 years. This research is exempt from Institutional Review Board approval as it is minimal risk and limited to use of previously collected de-identified information.
2.2. Exposure
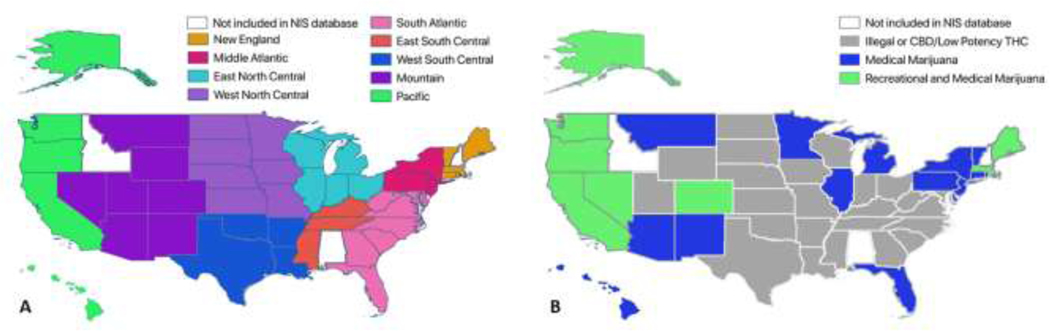
The NIS provides geographical data on census divisions but lacks information on individual states. The United States is composed of nine census divisions defined by the U.S. Census Bureau: New England, Mid-Atlantic, East North Central, West North Central, South Atlantic, East South Central, West South Central, Mountain and Pacific (Figure 1A). Exposure was categorized as hospital discharges in the Pacific census division compared to the reference group of all other census divisions. The Pacific census division was the only division where most states legalized recreational and marijuana use by 2017 (Figure 1B). The Pacific division is comprised of five states including four states that have legalized recreational use in adults 21 years and older as well as medical marijuana use (California, Oregon, Washington and Alaska) and one state (Hawaii) that has legalized medical marijuana only.
Figure 1:
A. Nine hospital census divisions represented in the National Inpatient Sample (NIS). B. Status of implementation of cannabis legalization laws in the United States in 2017 by state: illegal or cannabidiol (CBD)/low potency cannabis; standard medical marijuana, recreational and medical marijuana.
2.3. Cannabis Legalization
The status of implementation of cannabis legalization in each state by 2017 was determined by review of the National Conferences of State Legislature website on medical marijuana laws, individual state statutes and the Marijuana Policy Project’s state information websites (Marijuana Policy Project, 2021; National Conference of State Legislatures, 2021). We categorized each state based on implementation of legalization into three groups: 1) cannabis was illegal or medical cannabis programs restricted to cannabidiol (CBD)/low potency cannabis, 2) standard medical marijuana legalized (no potency restrictions), and 3) recreational and marijuana use was legalized. States where laws allowed personal cultivation were considered to have implemented cannabis legalization. For states restricting access to dispensaries, if dispensaries were open by 2017, they were considered to have implemented cannabis legalization. We grouped states that only legalized CBD/low potency cannabis with illegal states as these states generally restricted access to a small group of patients with refractory seizure disorders that failed conventional therapies. Cannabis legalization status established by this methodology is consistent with prior publications on medical and recreational cannabis legalization covering 2017 time period (Borodovsky et al., 2017; Shi and Liang, 2020). A detailed table of 2017 legalization status for each state can be found in Supplementary Table 1.
2.4. Outcome
The outcome of interest was the proportion of hospitalizations for psychosis associated with cannabis use out of all hospital discharges in individuals aged 18 to 64 years. We defined psychosis associated with cannabis use with ICD-10-CM diagnosis codes for cannabis-induced psychotic disorder (F12.15x, F12.25x, F12.95x) OR a combination of cannabis use disorder/poisoning (F12.x, T40.7x) and psychosis. Psychosis was defined as unspecified psychosis (F28, F29), brief psychotic disorder (F23), delusional disorder (F22), schizophrenia spectrum disorders (F20), schizoaffective disorder (F25), hallucinations (R44.0–3) and major depressive disorder or bipolar disorder with psychotic features (F32.3, F33.3, F30.2, F31.2, F31.5, F31.64).
2.5. Potential Confounders
Covariates included age, sex, race, and hospital location (rural, urban non-teaching or urban teaching), socioeconomic status (income quartile based on median household income for patient’s ZIP code) derived from NIS variables. We included binary variables denoting presence or absence of disorders based on ICD-10-CM codes for substance use and psychiatric disorders: alcohol use disorder, other substance use disorder, nicotine use disorder, depression or anxiety, post-traumatic stress disorder (PTSD) and other psychiatric illness. We also included covariates for illnesses consistently identified in medical marijuana laws as debilitating conditions that are prerequisites for treatment: arthritis, cancer, HIV or acquired immunodeficiency syndrome (AIDS), multiple sclerosis, Parkinson’s disease, epilepsy, cachexia, nausea/vomiting, inflammatory bowel disorders (Crohn’s disease or ulcerative colitis) and chronic pain. ICD-10-CM codes used to define these covariates can be found in Supplementary Table 2.
2.6. Statistical Analysis
Survey techniques were used for all analyses to account for the complex survey design. Sampling weights for discharges were provided by the NIS to obtain national estimates with unbiased standard errors. Analyses were performed with STATA version 15.1. Missing indicators were used to handle missing data from three variables: sex (0.01%), race (3.75%), and income quartile (1.89%).
2.6.1. Primary Analysis:
Demographic factors and characteristics of the hospital discharges from the Pacific and other census divisions were compared. For the primary analysis, odds ratios (OR) and 95% confidence intervals (CI) were computed using logistic regression to compare the odds of hospital discharges for psychosis associated with cannabis use in the Pacific versus other census divisions. Univariable and multivariable models that include covariates specified above were used to provide unadjusted and adjusted estimates, respectively.
2.6.2. Secondary Analysis:
For each census division, we calculated a Census Division Cannabis Legality Score as the population-weighted sum of state legality scores for each state within a division. State population and census division population for individuals age 18 – 64 years were obtained from U.S. Census data for 2017 (U.S. Census Bureau, 2017). Each state was assigned a cannabis legality score of 1 = illegal or CBD/low potency cannabis only, 2 = standard medical marijuana (no potency restrictions) and 3 = recreational and medical use. The Census Division Cannabis Legality Score was calculated as
where k = number of states within a census division. The possible range of values for the Census Division Cannabis Legality Score is 1 to 3, where 1 represents all states within a division have not implemented legalization of cannabis or are restricted to CBD/low potency cannabis, and 3 represents all states within a division have implemented legalization of recreational and medical cannabis use. Scores for each state and census division are provided in Supplementary Table 1. Pearson’s correlation coefficients were calculated to estimate the relationship between the proportion of hospitalizations within each census division with diagnosis of psychosis associated with cannabis use (model adjusted) and the Census Division Cannabis Legality Score. This analysis is considered exploratory; due to the complex sampling design, the proportion of hospitalizations in a census division from a given state may not precisely reflect state’s proportion of hospitalizations.
To validate the Census Division Cannabis Legality Score, we used state-wide estimates of cannabis measures obtained from the National Survey on Drug Use and Health (NSDUH) estimates for 2017–2018 (Substance Abuse and Mental Health Services Administration, 2019). For each census division, we used these estimates to calculate the proportion of adults in each census division reporting past month use of cannabis, initial cannabis use, and perception of great harm from past month use of cannabis (see Supplementary Material for details). Pearson correlation coefficients were performed to estimate relationship between the Census Division Cannabis Legality Score and each of these measures.
2.6.3. Subgroup Analyses:
Additional analyses included interaction terms for age and exposure (Pacific vs. other census divisions) and sex and exposure. Subgroup analyses were performed by age and sex. We divided age into categories by decade with additional division of younger patients into 18 – 20 and 21 – 29 years of age as recreational marijuana legalization is limited to adults 21 years and older.
2.6.4. Sensitivity Analyses: Modified Exposure/Outcome Definitions:
As a sensitivity analysis, we defined the exposure as a categorical variable with each census division compared to the reference East South Central division, where all states only legalized CBD or low potency cannabis with limited THC content limited to patients with refractory seizures. Univariable and multivariable logistic regression models using the pre-specified covariates were used to estimate odds ratios comparing the odds of risk of psychosis associated with cannabis use for each census divisions compared to the reference East South Central division.
As prior literature demonstrates a relationship between cannabis use and development of non-affective psychotic disorders (Løberg et al., 2014), we repeated the primary analysis excluding diagnoses for affective psychosis or hallucinations from the outcome definition (i.e., excluded F32.3, F33.3, F30.2, F31.2, F31.5, F31.64, R44.0–3). In addition, cannabis use may be inconsistently coded when individuals are hospitalized for psychosis. We compared the odds of psychosis and non-affective psychosis between the Pacific versus other census divisions overall, regardless of whether a cannabis use disorder/poisoning diagnosis was present.
3. RESULTS
3.1. Study Population
The sample included 25,814 discharges for psychosis associated with cannabis use, yielding a national estimate of 129,070 hospital discharges for psychosis associated with cannabis use in the year 2017 alone. Demographic and clinical characteristics associated with hospital discharges in the Pacific and other census divisions are presented in Table 1. There were 479,071 hospital discharges (13.9%) within the Pacific census division, compared to 2,979,171 in other census divisions. Age distribution and gender were comparable between the two groups. Rates of alcohol use disorder were similar at 7.9% and 8.3% in the Pacific and other census divisions, respectively. Hospital discharges from the Pacific census division were more likely to occur in an urban location, involve patients of Hispanic or Asian/Pacific Islander race and of higher income quartile, were less likely to involve patients of Black race and more commonly had diagnosis codes for smoking or depression/anxiety. Rates for conditions for which medical cannabis is indicated including arthritis, cancer, HIV/AIDS, multiple sclerosis, and nausea/vomiting were largely comparable between the Pacific and other census divisions.
Table 1:
Baseline characteristics of hospital discharges by census division
| Pacific Census Division N = 479,071 |
Other Census Divisions N = 2,979,171 |
|
|---|---|---|
| Age, n (%) | ||
| 18 – 20 years | 16,031 (3.4) | 102,232 (3.4) |
| 21 – 29 years | 90,194 (18.8) | 540,128 (18.1) |
| 30 – 39 years | 111,962 (23.3) | 604,979 (20.3) |
| 40 – 49 years | 73,964 (15.4) | 477,670 (16.0) |
| 50 – 59 years | 115,634 (24.1) | 778,788 (26.1) |
| 60 – 64 years | 71,286 (14.9) | 475,374 (16.0) |
| Female sex, n (%) | 293,599 (61.3) | 1,795,345 (60.3) |
| Race, n (%) | ||
| White | 221,464 (46.2) | 1,764,239 (59.2) |
| Black | 44,045 (9.2) | 586,004 (19.7) |
| Hispanic | 139,579 (29.1) | 327,467 (11.0) |
| Asian/Pacific Islander | 45,339 (9.5) | 55,605 (1.9) |
| Other | 20,870 (4.4) | 124,087 (4.2) |
| Income level, n (%) | ||
| 0–25th percentile | 95,934 (20.0) | 1,017,201 (34.1) |
| 26–50th percentile | 110,583 (23.1) | 782,419 (26.3) |
| 51–75th percentile | 128,247 (26.8) | 642,765 (21.6) |
| 76–100th percentile | 124,952 (26.1) | 490,647 (16.5) |
| Location of hospital, n (%) | ||
| Rural | 14,398 (3.0) | 268,578 (9.0) |
| Urban (non-teaching) | 144,580 (30.2) | 607,256 (20.4) |
| Urban (teaching) | 320,093 (66.8) | 2,103,337 (70.6) |
| Alcohol use disorder, n (%) | 37,735 (7.9) | 247,929 (8.3) |
| Other substance use disorder, n (%) | 44,928 (9.4) | 234,912 (7.9) |
| Smoking, n (%) | 76,397 (16.0) | 686,336 (23.0) |
| Depression/Anxiety, n (%) | 84,954 (17.7) | 704,686 (23.7) |
| PTSD, n (%) | 10,835 (2.3) | 90,279 (3.0) |
| Other psychiatric disorder, n (%) | 2,570 (0.5) | 18,737 (0.6) |
| Debilitating conditions required for medical cannabis use | ||
| Arthritis, n (%) | 28,935 (6.0) | 231,609 (7.8) |
| Cancer, n (%) | 23,707 (5.0) | 146,841 (4.9) |
| HIV/AIDS, n (%) | 2,709 (0.6) | 19,808 (0.7) |
| Multiple sclerosis, n (%) | 2,164 (0.5) | 18,973 (0.6) |
| Parkinson’s Disease, n (%) | 1,076 (0.2) | 6,658 (0.2) |
| Epilepsy, n (%) | 17,820 (3.7) | 125,476 (4.2) |
| Nausea and vomiting, n (%) | 9,194 (1.9) | 66,581 (2.2) |
| Cachexia, n (%) | 2,840 (0.6) | 17,001 (0.6) |
| Glaucoma, n (%) | 2,134 (0.5) | 14,788 (0.5) |
| Inflammatory bowel disease, n (%) | 4,865 (1.0) | 38,381 (1.3) |
| Chronic pain, n (%) | 37,417 (7.8) | 237,036 (8.0) |
PTSD = post-traumatic stress disorder. n is the study sample size with weighted %.
3.2. Primary Analysis
Hospitalizations for psychosis associated with cannabis use were more likely to occur in the Pacific division than other census divisions with an unadjusted OR of 1.32 (95% CI 1.01 – 1.72) and adjusted OR of 1.55 (95% CI 1.25 – 1.93), after adjusting for demographics, hospital characteristics and presence of other disorders (Table 2).
Table 2:
Psychosis Associated with Cannabis Use and Pacific vs. Other Census Divisions in the 2017 National (Nationwide) Inpatient Sample
| Study Sample | National Estimates | |||||
|---|---|---|---|---|---|---|
| Pacific Census Division N=479,071 |
Other Census Divisions N=2,979,171 |
Pacific Census Division N=2,395,348 |
Other Census Divisions N=14,895,853 |
Unadjusted OR (95% CI) | Adjusted OR* (95% CI) | |
| Psychosis associated with Cannabis Use Hospitalizations, n (%) | 4,502 (0.94) |
21,312 (0.72) |
22,510 (0.94) |
106,560 (0.72) |
1.32 (1.01, 1.72) |
1.55 (1.25, 1.93) |
| Other Hospitalizations (Not psychosis associated with cannabis use), n (%) | 474,569 (99.1) |
2,957,859 (99.3) |
2,372,838 (99.1) |
14,789,293 (99.3) |
- | - |
OR = odds ratio, CI = confidence interval.
Adjusted for age, sex, race, income quartile, hospital location, alcohol use disorders, other substance use disorders, smoking, depression/anxiety, post-traumatic stress disorder, other psychiatric disorders, arthritis, cancer, HIV/AIDS, multiple sclerosis, Parkinson’s disease, epilepsy, nausea/vomiting, cachexia, glaucoma, inflammatory bowel disease and chronic pain. Survey methods were used to derive weighted percentages and standard errors.
3.3. Census Division Cannabis Legality Score
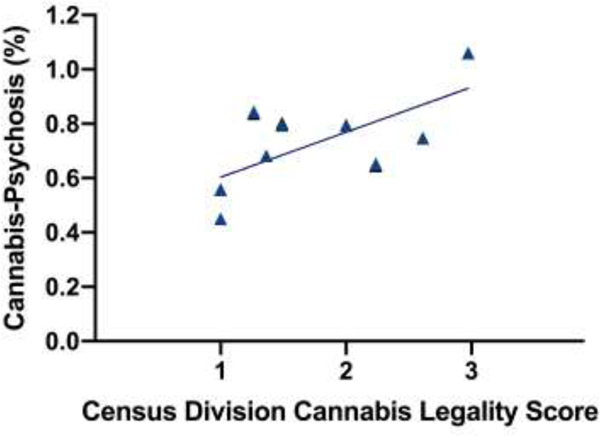
The division with the highest Census Division Cannabis Legality Score was the Pacific division (2.97) while the divisions with the lowest scores were East South Central and West South Central (1.00) (Supplementary Table 1). We found a significant correlation between the proportion of hospitalizations for psychosis associated with cannabis use and the Census Division Cannabis Legality Score (Figure 2; r=0.67, p<0.05).
Figure 2:
Correlation between percentage of hospitalizations with diagnosis of psychosis associated with cannabis use (adjusted for covariates) in each census division and Census Division Cannabis Legality Score (r=0.67, p<0.05). The Census Division Legality Score was calculated as sum of state legality scores weighted by proportion of state population in census division. State legality scores were defined as: 1 = illegal or cannabidiol/low potency cannabis, 2 = standard medical marijuana and 3 = recreational and medical marijuana. Census Division Cannabis Legality Scores ranged from 1 – 3.
There were significant positive correlations between the Census Division Cannabis Legality Score and NSDUH estimates of the proportion of individuals with past month cannabis use (r=0.90, p=0.0008) and initial use of cannabis (r=0.80, p=0.01) (Supplementary Figure 1). We also observed a trend between the Census Division Cannabis Legality Score and perception of great harm from past month use of cannabis (r=−0.61, p=0.08), where divisions with more liberal cannabis legalization had a lower perception of harm. These findings from NSDUH estimates support the validity of the Census Division Cannabis Legality Score.
3.4. Subgroup Analyses
We identified a significant interaction between age and exposure (Pacific vs. other census divisions; p=0.02). Subgroup analyses by age category are presented in Supplementary Table 3 and indicated a greater association between census division and psychosis associated with cannabis use as age increased. Interestingly, hospital discharges from the Pacific census division had a significantly greater odds of having diagnosis of psychosis in all age groups except for age 18 – 20 years (OR 1.22, 95% CI 0.98 – 1.53). There was no significant interaction between exposure and sex (p=0.47) with similar adjusted OR for females and males (OR 1.60, 95% CI 1.27 – 2.02 for females; OR 1.52, 95% CI 1.22 – 1.89 for males).
3.5. Sensitivity Analyses
Hospitalizations for psychosis associated with cannabis use were significantly more likely to occur in all census divisions compared to East South Central, with the notable exception of West South Central (Table 3). Of note, East and West South Central are the only two census divisions where all states had not implemented legalization of medical or recreational cannabis or restricted medical use to CBD/low potency cannabis.
Table 3:
Psychosis Associated with Cannabis Use and Census Division vs. East South Central in the 2017 National Inpatient Sample
| Census Division | Unadjusted OR (95% CI) | Adjusted OR (95% CI)* |
|---|---|---|
| Pacific | 2.03 (1.33, 3.10) | 2.46 (1.75, 2.09) |
| New England | 1.55 (1.06, 2.27) | 1.70 (1.24, 2.32) |
| Mid-Atlantic | 1.86 (1.30, 2.66) | 1.81 (1.35, 2.44) |
| East North Central | 1.78 (1.24, 2.58) | 1.83 (1.36, 2.47) |
| West North Central | 1.92 (1.32, 2.80) | 1.92 (1.42, 2.58) |
| South Atlantic | 1.62 (1.13, 2.33) | 1.54 (1.15, 2.07) |
| Mountain | 1.28 (0.83, 1.98) | 1.45 (1.01, 2.09) |
| West South Central | 0.98 (0.67, 1.45) | 1.25 (0.91, 1.71) |
| East South Central | - | - |
OR = odds ratio, CI = confidence interval.
Adjusted for age, sex, race, income quartile, hospital location, alcohol use disorders, other substance use disorders, smoking, depression/anxiety, post-traumatic stress disorder, other psychiatric disorders, arthritis, cancer, HIV/AIDS, multiple sclerosis, Parkinson’s disease, epilepsy, nausea/vomiting, cachexia, glaucoma, inflammatory bowel disease and chronic pain.
Hospitalizations for non-affective psychosis associated with cannabis use were also more likely to occur in the Pacific division than other census divisions with an unadjusted OR of 1.47 (95% CI 1.10 – 1.97) and adjusted OR of 1.75 (95% CI 1.38 – 2.22). Hospitalizations for psychosis and non-affective psychosis, regardless of whether cannabis use diagnosis was present, were also more likely to occur in the Pacific division compared to other census divisions [psychosis overall: adjusted OR 1.32 (95% CI 1.12 – 1.57); non-affective psychosis: adjusted OR 1.45 (95% CI 1.21 – 1.73)].
4. DISCUSSION
This nationwide study identified a greater proportion of hospital discharges for psychosis associated with cannabis use in the Pacific census division, the area with the most liberal cannabis legalization policies in the United States. We found a significant correlation between the proportion of hospitalizations for psychosis associated with cannabis use within each division and the Census Division Cannabis Legality Score, a novel score that we developed and validated to represent the status of cannabis legalization within each census division, suggesting that areas that implemented more liberal cannabis legalization policies were more likely to have a greater proportion of discharges for psychosis associated with cannabis use. Consistent with our hypothesis, each census division had a greater proportion of hospitalizations for psychosis associated with cannabis use compared to the East South Central division, the region with the most restrictive laws, except for the West South Central division. The West South Central division was the only other census division where all states only legalized CBD/low potency cannabis use or cannabis use was fully illegal.
Our findings are consistent with studies identifying an increase in cannabis use and cannabis use disorders in states that have legalized medical and/or recreational marijuana (Cerdá et al., 2020; Haffajee, 2021; Hasin et al., 2017), as well as studies finding an increased risk of poisoning following commercialization of recreational cannabis use and increased hospitalizations associated with cannabis legalization (Davis et al., 2016; Shi and Liang, 2020). However, this is the first study to specifically examine the association between cannabis legalization and hospital discharges for psychosis associated with cannabis use. Increased hospitalizations for psychosis in areas experiencing an increase in cannabis use or cannabis use disorders associated with legalization could be due to multiple reasons. First, multiple cohort studies have found that individuals who are daily users of cannabis have an increased risk of psychosis and schizophrenia (Andréasson et al., 1987; Henquet et al., 2005; van Os, 2002). A case control study identified an increased risk of heavy cannabis use in those with first episode psychosis, with a greater association in those who used cannabis with high levels of THC (Di Forti et al., 2009). In a study of European cities, the incidence of psychosis in various cities was correlated with local prevalence of daily cannabis use and high potency cannabis use (Di Forti et al., 2019). Secondly, patients without pre-existing history of psychosis may experience an acute self-limited toxic reaction to cannabis with psychotic symptoms, consistent with studies showing that acute administration of THC in healthy individuals leads to an increase in psychotic-like symptoms (D’Souza et al., 2004). Finally, patients with pre-existing psychotic disorders such as schizophrenia have been shown to be more likely to experience a relapse requiring hospitalization if they are using cannabis (van Dijk et al., 2012). By studying hospitalizations, this study focuses on serious cases of psychosis with diagnosis codes that link psychosis to cannabis use.
Multiple studies have consistently shown that legalization of medical marijuana and recreational marijuana are associated with an increase in cannabis use and cannabis use disorders in adults (Cerdá et al., 2020; Haffajee, 2021; Hasin et al., 2017), but not adolescents (Sarvet et al., 2018). In our study, the proportion of hospitalization discharges for psychosis associated with cannabis use was significantly higher in the Pacific Division than other census divisions in all age groups except for those 18 – 20 years of age. Since legalization of recreational use is limited to adults 21 years and older, this finding is suggestive of a possible association between hospitalizations for psychosis and recreational legalization more so than medical marijuana legalization. A previous study of the impact of recreational legalization on cannabis use did not find any changes in cannabis use or use disorders in adults 18 – 25 years but did not divide this group of adults into those legally impacted (21 years and older) (Cerdá et al., 2020). This same study found no increase in use or frequent use in the past month in adolescents age 12–17 years after recreational legalization with a slight increase in cannabis use disorders, which the authors acknowledged may have been due to time-varying confounding. In contrast, in adults 26 years and older, legalization of recreational marijuana was associated with an increase in past month use, past-month frequent use, and cannabis use disorders. This constellation of findings suggest that recreational legalization increases cannabis use and adverse consequences of cannabis use in adults who are legally impacted by laws.
A strength of this study is the large sample size that facilitates detection of rare events. The complex sampling design allows for national estimates, with an estimated 129,070 hospitalizations for psychosis associated with cannabis use in the year 2017 alone. Our findings are strengthened by consistency of results from primary, secondary and sensitivity analyses even after adjusting for covariates reflecting demographic factors, hospital characteristics and presence of other disorders associated with psychosis or cannabis use. We constructed a novel Census Division Cannabis Legality Score and found a significant correlation between these scores and the proportion of hospital discharges for psychosis associated with cannabis use within census divisions. This score was validated by correlations with NSDUH estimates of cannabis use measures. If confirmed, the finding of increased psychosis with cannabis legalization is an important consideration when weighing the risks and benefits of such policies, with appropriate education of the public of such risk and strengthening of support programs for psychosis associated with cannabis use when laws are enacted.
This study has several limitations including the cross-sectional design and restriction to one year of hospital data. The database of hospital discharges does not have subject-level data, such that a patient hospitalized more than once in 2017 will be represented as multiple hospital discharges. Diagnoses were limited to ICD-10-CM billing data, and hospital discharges for psychosis may have under-reporting of cannabis use or other medical comorbidities. NIS data has no information on the potency of cannabis used by patients, and strains of cannabis differ in terms of the quantity of THC and CBD (ElSohly et al., 2016). This study is also limited by the lack of state-specific data, as there is heterogeneity in state cannabis policies within census divisions. Any association between legalization policies and hospitalizations for psychosis associated with cannabis use may be due to other factors such as increased potency of cannabis over time (National Academies of Sciences, Engineering, and Medicine et al., 2017) or increases in perceived safety of cannabis (Compton et al., 2016; Pacek et al., 2015). It is possible that other unmeasured factors may be responsible for our findings; for example, California, the largest state in the Pacific census division, has a high rate of homelessness, with 1.9 times the national rate (The Council of Economic Advisers, 2019). Individuals who are homeless are disproportionately afflicted with substance use disorders and serious mental illnesses such as schizophrenia (Fischer and Breakey, 1991; Folsom and Jeste, 2002). Future studies employing a longitudinal design using state data to examine trends in psychosis over time associated with cannabis use and legalization are required.
In summary, this is the first cross-sectional population-based study of hospital discharges that revealed there is geographic variation in hospitalizations for psychosis associated with cannabis use that was associated with implementation of cannabis legalization policies. Given the rapid changes in legislative landscape, there is a need for further longitudinal research to better understand the nature of the relationship between cannabis legalization and the risk of psychosis.
Supplementary Material
HIGHLIGHTS:
Hospitalizations for psychosis/cannabis use more likely in areas where cannabis legalized.
Recreational cannabis legalization associated with greater rate of hospitalization.
Findings warrant future longitudinal studies to evaluate psychosis in U.S. states.
Acknowledgments:
The authors would like to thank Dr. Ellen McCarthy and Aaron Fleishman, MPH for input on study design and statistical analyses.
Funding: This research was supported by grants from the National Institute of Mental Health (K23MH110564, R01MH122427 to Lauren Moran) and by the Laboratory for Early Psychosis (LEAP) center (P50 MH115846 to Dost Ongur and John Hsu; pilot grant to Lauren Moran).
Footnotes
CRedit Author Statement: Lauren V. Moran: Conceptualization, Software, Data Curation, Formal Analysis, Writing – Original Draft; Erica S. Tsang: Conceptualization, Software, Data Curation, Formal Analysis, Writing – Review & Editing; Dost Ongur: Supervision, Writing – Review & Editing; John Hsu: Supervision, Writing – Review & Editing; May Y. Choi: Conceptualization, Software, Data Curation, Formal Analysis, Writing – Review & Editing.
All authors edited and approved the final manuscript.
Conflict of Interest: All authors report no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Agency for Healthcare Research and Quality, 2017. HCUP National Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). https://www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp (accessed 01 October 2020). [Google Scholar]
- Andréasson S, Engström A, Allebeck P, et al. , 1987. CANNABIS AND SCHIZOPHRENIA A Longitudinal Study of Swedish Conscripts. The Lancet 330, 1483–1486. 10.1016/S0140-6736(87)92620-1 [DOI] [PubMed] [Google Scholar]
- Borodovsky JT, Lee DC, Crosier BS, et al. , 2017. U.S. cannabis legalization and use of vaping and edible products among youth. Drug Alcohol Depend. 177, 299–306. 10.1016/j.drugalcdep.2017.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2018. 2017 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration, Rockville, MD. https://www.samhsa.gov/data/report/2018-nsduh-detailed-tables (accessed 05 July 2021) [Google Scholar]
- Cerdá M, Mauro C, Hamilton A, Levy NS, et al. , 2020. Association Between Recreational Marijuana Legalization in the United States and Changes in Marijuana Use and Cannabis Use Disorder From 2008 to 2016. JAMA Psychiatry 77, 165. 10.1001/jamapsychiatry.2019.3254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong SA, Subramaniam M, Lee I-M, et al. , 2009. Academic attainment: a predictor of psychiatric disorders? Soc. Psychiatry Psychiatr. Epidemiol 44, 999–1004. 10.1007/s00127-009-0027-3 [DOI] [PubMed] [Google Scholar]
- Claflin SB, van der Mei IAF, Taylor BV, 2018. Complementary and alternative treatments of multiple sclerosis: a review of the evidence from 2001 to 2016. J. Neurol. Neurosurg. Psychiatry 89, 34–41. 10.1136/jnnp-2016-314490 [DOI] [PubMed] [Google Scholar]
- Compton WM, Han B, Jones CM, Blanco C, Hughes A, 2016. Marijuana use and use disorders in adults in the USA, 2002–14: analysis of annual cross-sectional surveys. Lancet Psychiatry 3, 954–964. 10.1016/S2215-0366(16)30208-5 [DOI] [PubMed] [Google Scholar]
- Davis JM, Mendelson B, Berkes JJ, et al. , 2016. Public Health Effects of Medical Marijuana Legalization in Colorado. Am. J. Prev. Med 50, 373–379. 10.1016/j.amepre.2015.06.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Forti M, Morgan C, Dazzan P, et al. , 2009. High-potency cannabis and the risk of psychosis. Br. J. Psychiatry J. Ment. Sci 195, 488–491. 10.1192/bjp.bp.109.064220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Forti M, Quattrone D, Freeman TP, et al. , 2019. The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU-GEI): a multicentre case-control study. Lancet Psychiatry 6, 427–436. 10.1016/S2215-0366(19)30048-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Souza DC, Perry E, MacDougall L, et al. , 2004. The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacol 29, 1558–1572. 10.1038/sj.npp.1300496 [DOI] [PubMed] [Google Scholar]
- ElSohly MA, Mehmedic Z, Foster S, et al. , 2016. Changes in Cannabis Potency Over the Last 2 Decades (1995–2014): Analysis of Current Data in the United States. Biol. Psychiatry 79, 613–619. 10.1016/j.biopsych.2016.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer PJ, Breakey WR, 1991. The epidemiology of alcohol, drug, and mental disorders among homeless persons. Am. Psychol 46, 1115–1128. 10.1037//0003-066x.46.11.1115 [DOI] [PubMed] [Google Scholar]
- Folsom D, Jeste DV, 2002. Schizophrenia in homeless persons: a systematic review of the literature: Schizophrenia in homeless persons. Acta Psychiatr. Scand 105, 404–413. 10.1034/j.1600-0447.2002.02209.x [DOI] [PubMed] [Google Scholar]
- Folsom DP, Hawthorne W, Lindamer L, et al. , 2005. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am. J. Psychiatry 162, 370–376. 10.1176/appi.ajp.162.2.370 [DOI] [PubMed] [Google Scholar]
- Haffajee R, 2021. Cannabis Legalization In The US: Population Health Impacts. Project HOPE. 10.1377/hpb20210701.500845 [DOI]
- Hasin DS, 2018. US Epidemiology of Cannabis Use and Associated Problems. Neuropsychopharmacology 43, 195–212. 10.1038/npp.2017.198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Sarvet AL, Cerdá M, et al. , 2017. US Adult Illicit Cannabis Use, Cannabis Use Disorder, and Medical Marijuana Laws: 1991–1992 to 2012–2013. JAMA Psychiatry 74, 579. 10.1001/jamapsychiatry.2017.0724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henquet C, Krabbendam L, Spauwen J, et al. , 2005. Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people. BMJ 330, 11. 10.1136/bmj.38267.664086.63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesketh PJ, Kris MG, Basch E, et al. , 2017. Antiemetics: American Society of Clinical Oncology Clinical Practice Guideline Update. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol 35, 3240–3261. 10.1200/JCO.2017.74.4789 [DOI] [PubMed] [Google Scholar]
- Johal H, Devji T, Chang Y, et al. , 2020. Cannabinoids in Chronic Non-Cancer Pain: A Systematic Review and Meta-Analysis. Clin. Med. Insights Arthritis Musculoskelet. Disord 13, 1179544120906461. 10.1177/1179544120906461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Løberg E-M, Helle S, Nygård M, et al. , 2014. The Cannabis Pathway to Non-Affective Psychosis may Reflect Less Neurobiological Vulnerability. Front. Psychiatry 5, 159. 10.3389/fpsyt.2014.00159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marconi A, Di Forti M, Lewis CM, et al. , 2016. Meta-analysis of the Association Between the Level of Cannabis Use and Risk of Psychosis. Schizophr. Bull 42, 1262–1269. 10.1093/schbul/sbw003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marijuana Policy Project, 2021. State policies. https://www.mpp.org/states/. (accessed 01 June 2021)
- Marwaha S, Johnson S, 2004. Schizophrenia and employment - a review. Soc. Psychiatry Psychiatr. Epidemiol 39, 337–349. 10.1007/s00127-004-0762-4 [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Population Health and Public Health Practice, Committee on the Health Effects of Marijuana: An Evidence Review and Research Agenda, 2017. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research, The National Academies Collection: Reports funded by National Institutes of Health. National Academies Press (US), Washington (DC). [Google Scholar]
- National Conference of State Legislatures, n.d. State Medical Marijuana Laws. https://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx. (accessed 01 June 2021) [Google Scholar]
- Pacek LR, Mauro PM, Martins SS, 2015. Perceived risk of regular cannabis use in the United States from 2002 to 2012: differences by sex, age, and race/ethnicity. Drug Alcohol Depend. 149, 232–244. 10.1016/j.drugalcdep.2015.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer BA, Pankratz VS, Bostwick JM, 2005. The lifetime risk of suicide in schizophrenia: a reexamination. Arch. Gen. Psychiatry 62, 247–253. 10.1001/archpsyc.62.3.247 [DOI] [PubMed] [Google Scholar]
- Phillips TJC, Cherry CL, Cox S, et al. , 2010. Pharmacological treatment of painful HIV-associated sensory neuropathy: a systematic review and meta-analysis of randomised controlled trials. PloS One 5, e14433. 10.1371/journal.pone.0014433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramsay CE, Stewart T, Compton MT, 2012. Unemployment among patients with newly diagnosed first-episode psychosis: prevalence and clinical correlates in a U.S. sample. Soc. Psychiatry Psychiatr. Epidemiol 47, 797–803. 10.1007/s00127-011-0386-4 [DOI] [PubMed] [Google Scholar]
- Sarvet AL, Wall MM, Fink DS, et al. , 2018. Medical marijuana laws and adolescent marijuana use in the United States: a systematic review and meta-analysis. Addiction 113, 1003–1016. 10.1111/add.14136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Y, Liang D, 2020. The association between recreational cannabis commercialization and cannabis exposures reported to the US National Poison Data System. Addiction 115, 1890–1899. 10.1111/add.15019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2019. 2017–2018 NSDUH State Estimates of Substance Use and Mental Disorders. https://www.samhsa.gov/data/report/2018-nsduh-detailed-tables (accessed 05 July 2021)
- Substance Abuse Center for Behavioral Health Statistics and Quality, 2019. Results from the 2018 National Survey on Drug Use and Health: Detailed Tables, SAMHSA. https://www.samhsa.gov/data/report/2018-nsduh-detailed-tables (accessed 05 July 2021)
- The Council of Economic Advisers, 2019. The State of Homelessness in America. https://www.whitehouse.gov/wp-content/uploads/2019/09/The-State-of-Homelessness-in-America.pdf. (accessed 15 June 2021)
- U.S. Census Bureau. Annual Estimates of the Resident Population for Selected Age Groups by Sex for the United States, States, Counties, and Puerto Rico Commonwealth and Municipios, 2017 Population Estimates. https://www2.census.gov/programs-surveys/popest/tables/2010-2017/state/asrh/ (accessed 10 June 2021)
- van Dijk D, Koeter MWJ, Hijman R, et al. , 2012. Effect of cannabis use on the course of schizophrenia in male patients: a prospective cohort study. Schizophr. Res 137, 50–57. 10.1016/j.schres.2012.01.016 [DOI] [PubMed] [Google Scholar]
- van Os J, 2002. Cannabis Use and Psychosis: A Longitudinal Population-based Study. Am. J. Epidemiol 156, 319–327. 10.1093/aje/kwf043 [DOI] [PubMed] [Google Scholar]
- Zajicek JP, Hobart JC, Slade A, et al. , 2012. Multiple sclerosis and extract of cannabis: results of the MUSEC trial. J. Neurol. Neurosurg. Psychiatry 83, 1125–1132. 10.1136/jnnp-2012-302468 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.