Abstract
The ongoing COVID-19 pandemic requires wearing face masks in many areas of our daily life; hence, the potential side effects of mask use are discussed. Therefore, the present study explores whether wearing a medical face mask (MedMask) affects physical working capacity (PWC). Secondary, the influence of a filtering facepiece mask with exhalation valve class 2 (FFP2exhal) and a cotton fabric mask (community mask) on PWC was also investigated. Furthermore, corresponding physiological and subjective responses when wearing face masks as well as a potential moderating role of subjects’ individual cardiorespiratory fitness and sex on face mask effects were analyzed. Thirty-nine subjects (20 males, 19 females) with different cardiorespiratory fitness levels participated in a standardized submaximal bicycle ergometer protocol using either a MedMask, FFP2exhal, community mask, or no mask (control) on four days, in randomized order. PWC130 and PWC150 as the mechanical load at the heart rates of 130 and 150 beats per minute were measured as well as transcutaneous carbon dioxide partial pressure, saturation of peripheral capillary oxygen, breathing frequency, blood pressure, perceived respiratory effort, and physical exhaustion. Using the MedMask did not lead to changes in PWC or physiological response compared to control. Neither appeared changes exceeding normal ranges when the FFP2exhal or community mask was worn. Perceived respiratory effort was up to one point higher (zero-to-ten Likert scale) when using face masks (p < 0.05) compared to control. Sex and cardiorespiratory fitness were not factors influencing the effects of the masks. The results of the present study provide reason to believe that wearing face masks for infection prevention during the COVID-19 pandemic does not pose relevant additional physical demands on the user although some more respiratory effort is required.
Keywords: physical working capacity, COVID-19, occupational health and safety, personal protective equipment
1. Introduction
After the onset of the COVID-19 pandemic, politicians and medical experts established rules to avoid the spreading of the coronavirus (SARS-CoV-2) in order to protect the population [1,2,3]. In this context, face masks have become an important measure since they are effective in reducing respiratory transmission by droplet infection and aerosols [4], and in many areas of life, such as work, wearing face masks has become mandatory [2]. Current recommendations for infection prevention at the workplace in Germany either suggest wearing a medical face mask (MedMask), also called surgical mask, or filtering facepieces class 2 (FFP2) or N95 masks to protect oneself or others, respectively [5]. Besides the protective effects of the face masks, undesirable side effects are discussed [6], as the masks have a direct effect on breathing air supply. The scientific evidence on the effects of wearing face masks on worker health, work ability, and performance is controversial. Two recent reviews, one scoping review focusing on negative effects by face masks and a systematic review analyzing the effects of face masks during exercise, have summarized the current scientific evidence on this topic with different perspectives. While Sha, et al. [7] reported that masks have only small effects on physiological responses and no effect on performance during exercise, Kisielinski et al. [8] concluded that face masks can “have a negative effect on the basis of all aerobic life (…) with physical, psychological, and social consequences for the individual human being” [8] (p. 35).
Despite these contradictive views, wearing face masks is generally recommended [2,9]. With respect to the workplace setting, the Coordination Center for Biological Hazards of the German Statutory Accident Insurance (DGUV) recommends that the masks used for general infection protection during the pandemic are worn no longer than 2 h at a time. Then, a 30-min period without mask is required before the mask can be worn for another period of 2 h. Thus, a total of three wearing periods per working day can take place [10]. This pandemic-specific recommendation was based on another document by the German Statutory Accident Insurance addressing occupational health and safety when wearing respirators [11]. In this document, wear-time limitations are suggested for the different classes of respirators to prevent overloading of the users. Hence, the wear-time limits suggested in the latter document are based on working conditions where FFP2 masks with exhalation valve (FFPexhal) are used as protective measures against hazardous dust, which simply has been adopted as the wear-time recommendation for any face mask during the COVID-19 pandemic. This recommendation, which has not been supported by scientific evidence so far, significantly affects the daily work in German companies from different occupational sectors.
As seen for many of the governmental regulations during the pandemic, recommendations may change when more scientific data become available. A major problem of the currently available scientific literature dealing with side effects of face masks is a substantial risk of bias, as shown by Shaw, Zello, Butcher, Ko, Bertrand, and Chilibeck [7]. This risk refers to small sample sizes (insufficient statistical power); low methodological quality; testing the masks under maximum performance, which is not representative for occupational tasks; using masks that are currently not recommended during the COVID-19 pandemic [12]; or improper use of the masks resulting from the applied scientific methods, e.g., wearing a respiratory mask over the face mask, leading to unrealistic leakage [13,14]. Despite the mentioned shortcoming of the available literature and the scoping review by Kisilinsky et al. (2021) focusing on negative outcomes related to face masks, the majority of available data indicate minor physiological responses within a non-relevant range by using face masks [7,15]. Even less response has been associated by using a MedMask compared to FFP2 or N95 masks [7,16].
In addition, an interaction of wearing face masks with individual factors, such as a person’s cardiorespiratory fitness level, age, or sex, known to modify physical capacity [17,18,19,20,21,22] has almost not been considered when evaluating face masks [15,16]. The controversial scientific debate about face masks and their impact on employees’ health [23] indicates the need for further high-quality studies as a solid basis for proper recommendations during the COVID-19 pandemic. Therefore, this study investigated whether face masks would impair physical performance and affect physiological and subjective response during submaximal physical activity as well as a potential moderating role of cardiorespiratory fitness level and sex on the mask effects.
2. Materials and Methods
2.1. Participants
Thirty-nine healthy subjects (20 men; 19 women) were included. All gave their written informed consent prior to participating and received financial compensation. Participants were recruited by announcements mails within the University of Tübingen, the University Hospital of Tübingen, and by mouth to mouth propaganda. Individuals with metabolic diseases, including diabetes, cardiovascular or respiratory diseases, or existing pregnancy, were excluded from participation. A medically unremarkable pulmonary function test (spirometry) and electrocardiogram during a bicycle ergometer test until exhaustion were mandatory for study participation. The complete list of in- and exclusion criteria is shown in Appendix A and corresponds to recommended absolute and relative contra-indications for bicycle ergometer testing within occupational medical examinations [24]. The initial bicycle test until exhaustion was also used to determine participants’ individual maximal physical working capacity (PWCmax), with the mechanical power in Watt per kilogram body weight (W/kg) as indicator of cardiorespiratory fitness [25]. Based on PWCmax, participants were categorized in three fitness levels with respect to proposed norm values for PWCmax [26]. Sex-specific categorization was as follows: PWCmax below the norm (men: < 3.0, women: < 2.6 W/kg), corresponding to the norm (men: 3.0 W/kg ≤ x < 4.1 W/kg, women: 2.6 W/kg ≤ x < 3.5 W/kg), and above the norm (men: ≥4.1 W/kg, women: ≥3.6 W/kg).
2.2. Study Design, Research Aims and Sample Size
This randomized, intra-subject, cross-over design study included four experimental conditions, each on a separate day, during which the subjects had to accomplish four submaximal bicycle ergometer tests while wearing either no mask (control), a MedMask, and a FFP2exhal or a fabric mask (community mask). The study was registered in the German clinical trial register (DRKS00024531).
The primary aim was to confirm that there are no relevant differences in physical working capacity (PWC) as an indicator of physical performance at a medium level of physical activity (heat rate of 130 beats per minute (bpm)) when wearing a MedMask since wearing a MedMask is the minimal legal requirement for infection prevention in German occupational settings when required distances cannot be guaranteed [2,27].
Secondary, potential performance differences between no mask and MedMask and FFP2exhal and community mask in PWC at the heart rates of 130 and 150 bpm were examined. Complementary, physiological, and subjective responses due to wearing the face masks were analyzed as well as the influence of cardiorespiratory fitness level and sex on potential mask effects.
Sample size was calculated and set according to preliminary results from eight subjects, including four men and four women (Appendix B), assuming equality between MedMask and control at PWC130 during a bicycle ergometer test (primary outcome). Mean differences in PWC130 while wearing MedMask or no mask as well as the corresponding standard deviation were determined. These preliminary data were not included in the final study sample. A relevant effect of the MedMask on PWC130 was considered as a shift in PWC130 to an adjacent fitness level according to published normative values for PWC130 with a change of 0.3 and 0.4 W/kg in females and males, respectively [26]. Using a more conservative approach, 0.3 W/kg was set as relevant change. According to this a sample size, only n = 4 would have been necessary for showing noninferiority of the MedMask compared to no mask condition on a statistical significance level of alpha = 0.05. However, we doubted external validity of a study with only 4 subjects. Moreover, due to the secondary research questions and multiple statistical testing, a further increase of sample size was necessary. With a Bonferroni correction of 15, effect sizes of 0.67 could have been shown. Finally, a Williams design preventing first-order carry-over effects with 9 subjects per one of the four randomization sequences (based on four experimental conditions) and balanced for sex and fitness level led to 36 (18 women, 18 men) participants. Due to practical reasons, we had to include three additional participants so that the final sample size was 39 (20 males and 19 females).
2.3. Procedures
Participants were invited to an initial visit in the laboratory on which written informed consent was collect, in -and exclusion criteria were verified, and the PWCmax test was conducted. After final inclusion, subjects had to fill out the Nordic Questionnaire and the Physical Activity, Exercise, and Sport Questionnaire. Thereafter, subjects performed the PWCsubmax test on four separate days in randomized order. The first PWCsubmax test took place at least three days after the initial day with the PWCmax test to ensure complete recovery. The PWCsubmax tests were performed at the same time of the day on four consecutive days. Actual intervals between the test conditions can be found in Appendix C. Temperature in the laboratory was kept constant during all measurements at about 23 °C.
2.4. Physical Working Capacity Tests and Face Masks
The initial PWCmax test and the submaximal PWC tests (PWCsubmax) were performed on a bicycle ergometer (custo ec5000, custo med GmbH, Ottobrunn, Germany) according to the World Health Organization scheme [28] and followed the updated recommendations for ergometer testing in occupational medicine [24].
PWCmax: At the beginning of the protocol, there was a 3-min phase in which all physiological parameters were measured at rest. Subsequently, cycling started with a resistance of 25 W and cadence of 60 repetitions per minute and increased every 2 min by 25 W until subjective maximal physical exhaustion, or the given cadence could not be maintained. The abort criterion was a decrease of more than 5 repetitions per minute for more than 5 s.
PWCsubmax: The protocol also started with a 3-min rest phase followed by subsequent cycling at 60 repetition per minute with a resistance of 25 W or 50 W. The starting resistance was set according to the PWC150 during the initial PWCmax test. In the case of a PWC150 below 125 W, the starting resistance of 25 W was chosen in order to have more similar cycling durations between subjects. Resistance was also increased by 25 W every two minutes until the level corresponding to at least 70 but no more than 80% of the initial PWCmax was reached. This procedure ensured that every subject reached PWC150 during each submaximal PWC test according to the results of preliminary tests in the 8 subjects also used for sample size calculation. Immediately following both tests (PWCmax, PWCsubmax), the recovery phase began with a 1-min step-out at 25 W and 30 rpm, followed by nine minutes of seated rest. During all ergometer tests, a physician observed subjects’ ECG and health status. Criteria for premature termination of the test can be found in Appendix D. The following face masks were used in this study:
MedMask (Figure 1A): Disposable medical face mask without exhaling valve (NITRAS Medical Care Dental GmbH, 4331//PROTECT, medical face mask, made of fiberglass-free non-woven fabric, blue, 3-ply, integrated nosepiece, round and latex-free elastic bands, manufactured according to EN 14683 Type IIRv). This type of mask has been chosen since in Germany it is the minimal legal requirement for infection prevention in occupational settings when the minimum distance cannot be guaranteed [2].
FFP2exhal (Figure 1B): Disposable filtering face-piece mask with exhaling valve, protection class II (Honeywell, SuperOne 3206, VALVE, EN 149). This mask was used since suggested wear time limits in Germany for any face mask during the COVID-19 pandemic are based on working conditions where FFP2 masks with exhalation (FFPexhal) valve are used as protective measures against hazardous dust [10].
Community mask (Figure 1C): Cotton mouth-nose-cover without exhaling valve (van Laack, Art.49.0946.Z51022.003, CE—2012-16632). A community mask was additionally included as an experimental condition because this type of mask can be used by the general public under the age of 60 and who do not have underlying health conditions according to the recommendation of the WHO [9].
Figure 1.
Investigated face masks. (A) MedMask medical face mask (NITRAS PROTECT, EN14683), (B) FFP2exhal filtering facepiece with exhalation valve (Honeywell, SuperOne 3206, VALVE, EN 149) and (C) community mask fabric mask (van Laack, CE—2012–16632).
2.5. Outcomes and Measurements
Ergometric PWC testing has a long tradition in occupational medicine for assessing whether a sufficiently high level of physical performance for coping with the daily work requirements is given [29]. An imbalance between physical workload and physical work capacity related to aging workers has been suggested to result in chronic overload, increasing the risk of long-term health effects [30,31]. PWC can be tested maximally or submaximally, using performance indicators like VO2max [32] or the mechanical power [33]. In the case of submaximal PWC testing measuring the mechanical power, the achieved power at a given heart rate serves as performance indicator. There are age- and sex-specific norm values [26] that can be used to judge whether differences or changes are within the normal range or can be considered significant. With respect to potential impairments in submaximal performance by wearing a face mask, the assessment of PWC at a certain heart rate level on a bicycle ergometer appears to be an appropriate setting for testing face masks, assuming that increased physiological demands will result in reduced PWC or compensatory mechanisms. In this respect, physiological and subjective responses will serve as important complementary measures.
Physical working capacity 130 and 150:
The mechanical power (Watt) during bicycle ergometer testing (custo ec5000, custo med GmbH, Ottobrunn, Germany) was determined with simultaneously measuring the heart rate by a 12-lead electrocardiogram (custo cardio 400, custo med GmbH, Ottobrunn, Germany). Both were recorded at a sample rate of 1 Hz. PWC130 and PWC150 were calculated automatically by the cycle ergometer-ecg system according to linear interpolation. Details will be given in the data analysis section.
Physiological responses
Transcutaneous carbon dioxide partial pressure (tcpCO2)
A transcutaneous gas measurement device (IntelliVue TcG10, Philips Medical Systems DMC GmbH, Boeblingen, Germany and tc sensor 84, Radiometer GmbH, Krefeld, Germany) was used for non-invasive measurement of carbon dioxide partial pressure at a sample rate of around 0.125 Hz. The assessment of tcpCO2 has already been shown to provide reliable data during exercise testing [34]. The skin sensor electrode with a temperature of 44° Celsius (C) was placed on the right upper arm over the middle deltoid muscle 10 min prior the start of the ergometer test in order to fulfill the warming requirements of this electrode.
Saturation of peripheral capillary oxygen (SpO2)
Blood oxygen saturation level represents the amount of oxygen carried in the hemoglobin and is expressed as a percentage of the maximum amount of oxygen that hemoglobin in the blood can carry. Measurements were conducted using an ear pulse oximetry sensor with a sample rate of 0.1 Hz (ES-3227, EnviteC-Wismar GmbH, Wismar, Germany), which was connected to the ergometer system. Using spectrophotometric methodology, pulse oximetry measures oxygen saturation by illuminating the skin and measuring changes in light absorption of oxygenated and deoxygenated blood [35].
Blood pressure
Systolic and diastolic blood pressure were measured using a blood pressure cuff applying the riva rochi method at the right arm (blood pressure cuff for ec5000, custo med GmbH, Ottobrunn, Germany). Participants were asked to keep their hand on the handlebars but relax their arm when the measurement took place. The blood pressure cuff was connected to the ergometer system and measured automatically at the end of each load level (sample rate of 0.008 Hz).
Breathing frequency
Breathing frequency was measured continuously throughout the test protocols using a sensor belt placed around the chest (NeXus Atem Sensor NEXU2050, Hasomed GmbH, Magdeburg, Germany and AMS42-LAN16fx, BMCM Messsysteme GmbH, Maisach, Germany). The sensor attached to a chest belt recognizes extensions and reductions of the thorax during respiration. The sensor output is a breath-dependent voltage change sampled at the rate of 16 Hz. Breathing frequency was calculated from the end of each load level. However, this interfered with the assessment of perceived exhaustion and perceived respiratory effort, which took place within the last 20 s of each load level. Therefore, and with an additional 5-s buffer, the respiratory rate was calculated from about 30 s before the last 25 s of each load level. Concretely, to calculate the respiratory rate, data from second 63 to second 95 were selected in each 120-s load level. The 512 voltage readings of these 32 s were transferred from the time domain to the frequency domain using Fast Fourier Transform (FFT). The input vector of an FFT must have a length of two to the power of n. Thus, in combination with the 16-Hz sampling rate, data from 32 s were used. No windowing and 512 FFT points were used for this purpose. To filter possible interferences (transients), only spectral amplitudes in the frequency range from 0.078 Hz to 1.85 Hz (corresponding to 4.7 breaths/min to 111 breaths/min) were included in the subsequent calculations. A seven FFT point wide moving average filter was used to smooth the frequency-amplitudes for unifying closely spaced spectral local amplitude maxima that may arise due to a gradually increasing respiratory frequency within the 32-s phase. In addition, smoothing reduces occasional peaks caused by motion artifacts. Finally, the mean respiratory rate of each 32-s period corresponds to the frequency of the highest spectral amplitude.
Subjective responses
Respiratory effort and perceived physical exertion
Respiratory effort and perceived physical exertion were assessed using a modified Borg CR10 scale (0 = nothing at all, 10 = maximal) within the last 20 s of each load level. Although this scale is commonly used for assessing the level of perceived exertion, it is also used for assessing alterations in respiration during bicycle ergometer testing [36].
Supplemental measurements for characterizing the study sample
The Nordic questionnaire was used to gather subjects’ age, body weight, gender, laterality, current profession, and weekly working hours [37]. Additionally, the Physical Activity, Exercise, and Sport Questionnaire was used to assess physical activity at work and during leisure time [38].
2.6. Data Analysis
Parameter calculation: All outcome variables were assessed at the time points when PWC130 and PWC150 were reached. Due to the incremental test protocol, linear interpolations were necessary to determine the exact point of time and corresponding value for each outcome variable.
Calculation of physical working capacity: The PWC defines the capacity that the subject achieves at the time when it reaches a heart rate of 130 (PWC 130) or 150 (PWC 150) beats per minute. For the calculation of PWC130 and PWC150, the load levels with a minimum duration of 30 s were considered only. Baseline and recovery periods were not included. If the target heart rate was not reached within the last 10 s of a load level, the PWC value was calculated by interpolation or, in case of the last load level, by extrapolation. In the case of extrapolation, the test subject must have reached a heart rate of at least 120 or 140 beats per minute; otherwise, PWC130 or PWC150 were not calculated. The PWC130 and PWC150 values were calculated according to the following Equation:
| PWC(HR) = W1 + (W2 − W1) × (HR − HR1) / (HR2 − HR1) [W] |
R = target heart rate, i.e., 130 or 150
HR1 = mean HR of the last 10 s of the load level before the level in which the target HR was reached in the case of extrapolation: mean HR of the last 10 s of the load level before the level in which the target HR of 120 or 140 was reached, respectively.
HR2 = mean HR of the last 10 s of the load level in which the target HR was reached in the case of extrapolation: HR2 = HR
W1 = watt of the level before the level in which the target HR was reached
W2 = watt of the level in which the target HR was reached
In addition, the PWC related to the body weight was calculated:
Calculation of outcomes at the time points when PWC130 and PWC150 were reached: For the variables peripheral capillary oxygen saturation (SpO2), systolic and diastolic blood pressure (SBP and DBP), and transcutaneous carbon dioxide partial pressure (tcpCO2), a linear regression was performed around the time when PWC130 or PWC150 were reached. The regression included as many as possible but at least two of the measured values belonging to the respective variable. Only values recorded during the exercise period were considered; baseline and recovery periods were not included in the regression. SpO2 was considered over an interval of 40 s around the time of PWC with a maximum of 5 values (sampling interval of approximately 10 s). SBP and DBP were determined over an interval of 260 s around the time of PWC with a maximum of 3 values (sampling interval of approximately 120 s) considered. Linear regression of tcpCO2 was performed over an interval of approximately 45 s around the time of PWC with a maximum of 6 values (sampling interval of approximately 7–9 s).
For the variables breathing frequency, respiratory effort and perceived physical exertion a linear increase was assumed at each 2-min load level when the respective power of the cycling protocol was reached (end of a load level). For the calculation of the linear regression, all measured values of the parameter from the beginning of the measurement to the end of the exercise period (sampling interval of approximately 120 s) were considered. Values were than taken from the corresponding time points of PWC130 and PWC150.
Statistical analysis: The primary hypothesis was to show noninferiority of the MedMask condition in comparison to not wearing a mask. This was done by calculating the two-sided 95% confidence interval of the difference in the primary endpoint (PWC130) between control condition and MedMask (regression coefficient for type of mask in a linear mixed model including only these two conditions, coded as 0 and 1, and sex).
For all secondary aims of this study, linear mixed models (LMM) were applied to analyze the influence of the independent variables mask condition, sex, cardiorespiratory fitness (PWCmax), the interaction of mask condition with sex, and mask condition with cardiorespiratory fitness on the dependent variables (primary outcome: PWC130; secondary outcomes: PWC150, additional parameters at the time points when PWC130 and PWC150 were reached, i.e., tcpCO2, SpO2, systolic and diastolic blood pressure, breathing frequency, perceived respiratory effort, and perceived physical exertion). Therefore, five variations of the LMM were performed per outcome variable. The first LMM included only mask condition as independent variable. The second LMM additionally included sex, and the third LMM included sex and cardiorespiratory fitness. LMM four and LMM five additionally included the interaction terms mask condition x sex and mask condition x cardiorespiratory fitness. Alpha level was Bonferroni corrected for 15 comparisons. All outcome variables were visually inspected for extreme values and normal distribution. Means and standard deviations or boxplots, including median and the upper and lower quartiles or frequencies, were used to describe the results. Differences in anthropometric data between the three fitness level groups were analyzed using a one factorial Analysis of Variance (ANOVA) and Tukey’s honestly significant differences test for post-hoc comparison. The statistical software IBM® SPSS® Statistics Version 27 was used for statistical analyses.
3. Results
3.1. Dropouts
Nineteen subjects were not included after the initial visit. In 18 cases, the reason for not being included was that the presumed fitness level (based on participants self-report) was not reached during the PWCmax test. These subjects could not be included in the study because the required number of participants at the next lower or higher fitness level had already been fully recruited. One subject refused to participate after the initial visit due time constraints. No participant dropped out for medical reasons or due to adverse events during the measurements.
3.2. Characteristics of the Final Study Sample
Participants were 38.2 years old, had a BMI of 23.7 kg/m², and their length of employment in the current occupational profession was 10.5 years. Furthermore, participants had a weekly working time of 34 h and reported their weekly physical activity at work and at leisure time being 492 min and 206 min, respectively. Only four participants were smokers. A detailed overview of the characteristics of the final study sample is provided in Table 1. Participants with a high cardiorespiratory fitness level (level 3) were younger in age, had a shorter duration in their current profession, and were more active during leisure time then the participants from the other two fitness levels. Furthermore, BMI was lower than from participants from fitness level 1.
Table 1.
Characteristics of the study sample.
| Parameter | Overall |
Fitness Level 1 | Fitness Level 2 | Fitness Level 3 | ||
|---|---|---|---|---|---|---|
| PWCmax | (W/kg) | mean SD |
3.3 1.0 |
2.3 * 0.3 |
3.2 * 0.3 |
4.4 * 0.6 |
| sex | (n, %) | overall men women |
39, 100% 20, 51.3% 19, 48.7% |
13, 33.3% 6, 15.4% 7, 18.0% |
13, 33.3% 7, 18.0% 6, 15.4% |
13, 33.3% 7, 18.0% 6, 15.4% |
| smokers | (n, %) | 4, 10.3% | 1, 2.6% | 3, 7.7% | 0, 0% | |
| age | (years) | mean SD |
38.2 14.2 |
43.1 16.9 |
43.8 13.1 |
28.7 ** 6.1 |
| BMI | (kg/m²) | mean SD |
23.7 2.4 |
25.0 3.1 |
23.5 1.9 |
22.5 * 1.4 |
| Duration of current occupational profession | (years) | mean SD |
10.5 10.7 |
13.8 13.5 |
12.9 9.9 |
5.0 ** 5.5 |
| Weekly working time | (hours) | mean SD |
34.3 13.2 |
30.5 14.2 |
32.6 11.3 |
39.7 13.2 |
| Physical activity at work |
(minutes/week) | mean SD |
491.8 589.0 |
424.3 488.1 |
609.3 726.6 |
441.7 556.5 |
| Physical activity leisure time | (minutes/week) | mean SD |
206.4 207.3 |
99.1 103.7 |
112.3 100.2 |
407.7 ** 222.2 |
PWCmax, physical working capacity (mechanical power, Watt/kg) during a bicycle ergometer test until maximum exhaustion; BMI, body mass index; ** statistically significant difference to the other two fitness level groups (p < 0.05), * statistically significant difference to fitness level group 1 (p < 0.05).
3.3. Normal Distribution and Missing Data
After visual inspection of the outcome variables an acceptable level of normal distribution based on histograms, skewness and kurtosis (between –1 and 1) could be assumed. Only for the variable SpO2 did an obvious violation of normal distribution occur. The amount of missing data varied between variables and time point of assessment. Generally, there were fewer missing data at the time point of PWC130 than at PWC150, and the primary outcome variable physical performance at the heart rate of 130 bpm had the lowest amount of missing data (≤5%). The highest amount of missing data occurred in the parameters tcpCO2, SpO2, and blood pressure. A comprehensive overview of missing data per variable is given in Appendix E. The applied statistical analysis (linear mixed models) are considered being robust against violation of normal distribution [39] and able to deal with missing data without causing problems with power and bias when missing data are at random [40].
3.4. Primary Outcome—Physical Working Capacity at the Heart Rate of 130 Beats per Minute Using a MedMask
The confidence limit for the difference between the MedMask and the no mask condition, adjusted for sex, was −0.058, 95% CI −0.188 to 0.002. Thus, the noninferiority criterion was met, and the study could successful prove noninferiority of the MedMask vs. the control situation without mask (Table 2). Statistical models without sex and models including sex and cardiorespiratory fitness did not change the differences between mask conditions or standard errors or CIs. Furthermore, no interaction of mask condition with sex and mask condition with cardiorespiratory fitness occurred. All statistical models can be found in Appendix F.
Table 2.
Comparison between the no mask and MedMask condition.
| Model | Outcome Parameter | Dependent Variable | Degree of Freedom | F-Value | p-Value |
|---|---|---|---|---|---|
| 1 | PWC130 | Face mask condition | 1 | 3.472 | 0.07 |
| 2 | PWC130 | Face mask condition | 1 | 3.491 | 0.07 |
| sex | 1 | 13.245 | 0.001 |
3.5. Secondary Outcomes
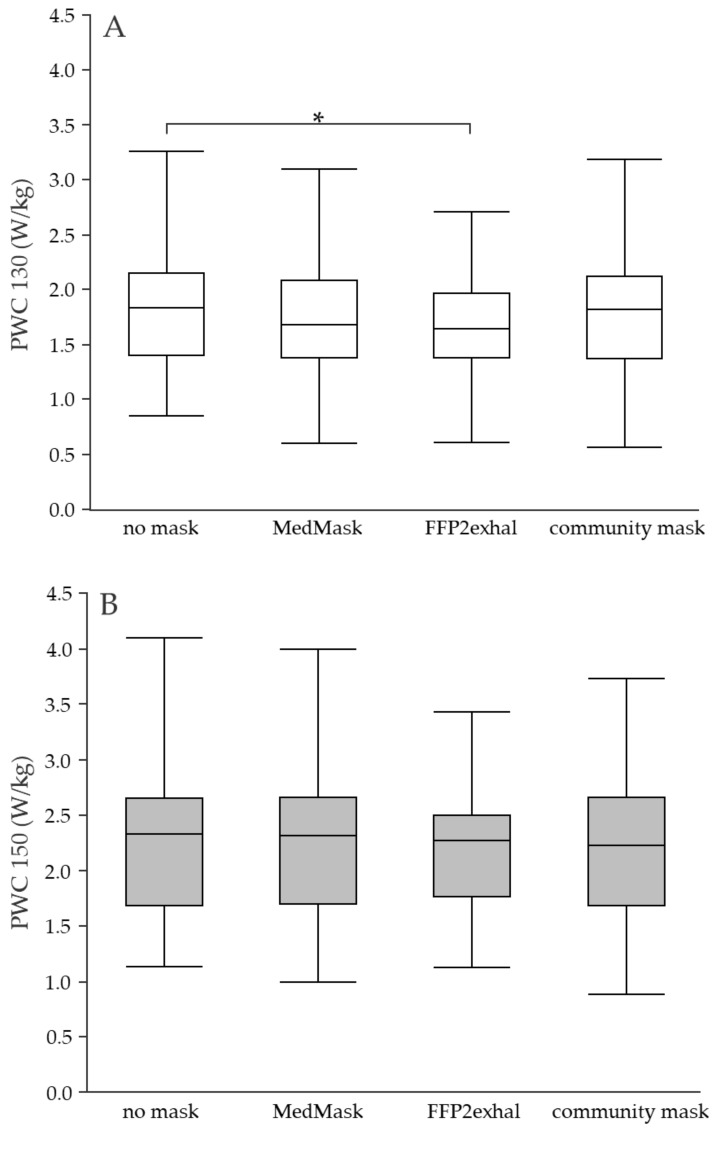
Physical working capacity at a heart rate of 130 and 150 bpm using a MedMask, FFP2exhal, and community mask: Using the MedMask did not lead to a statistically significant change in PWC150 vs. control. Again, sex and cardiorespiratory fitness level had no effects, as seen from LMM2 to LMM5 (Appendix F). Wearing the community mask was also not associated with any statistically significant changes in PWC130 or PWC150 vs. control. When FFP2exhal was used, a slightly lower PWC130 value was found compared to control (FFP2exhal: −0.17 W/kg, p < 0.0001) without exceeding the a-priori defined relevant change of 0.3 W/kg. No change in PWC occurred at the heart rate of 150 bpm. Adding sex and cardiorespiratory fitness to the model (LMM 2 and LMM3) did not induce further changes, and no interaction of mask condition with sex and mask condition with cardiorespiratory fitness occurred (LMM4 and LMM5). Boxplots of PWC130 and PWC150 resulting from the four experimental conditions are shown in Figure 2. Means and standard deviations from all outcomes and experimental conditions are shown in Table 3.
Figure 2.
(A,B) Physical working capacity at the heart rate of 130 and 150 beats per minute using different face masks. Grey shaded boxplots represent the physical working capacity at the heart rate of 150 beats per minute. Asterisks indicate statistically significant differences (Bonferroni corrected p < 0.003). PWC, physical working capacity; MedMask, medical face mask; FFP2exhal, filtering facepiece with exhalation valve.
Table 3.
Mean values of all assessed outcome parameters during the four experimental conditions.
| Outcome Parameter | No Mask | MedMask | FFP2exhal | Community Mask | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| PWC130 (W/kg) | 1.91 | 0.70 | 1.84 | 0.72 | 1.74 | 0.65 | 1.83 | 0.70 |
| PWC150 (W/kg) | 2.35 | 0.83 | 2.32 | 0.81 | 2.28 | 0.76 | 2.35 | 0.89 |
| tcpCO2 at PWC130 (mmHg) | 32.37 | 6.22 | 34.07 | 4.28 | 33.64 | 4.29 | 33.70 | 4.48 |
| tcpCO2 at PWC150 (mmHg) | 31.18 | 6.15 | 34.33 | 4.70 | 33.45 | 4.54 | 32.78 | 4.29 |
| SpO2 at PWC 130 (%) | 97.30 | 3.74 | 97.42 | 3.38 | 98.29 | 2.94 | 97.90 | 4.03 |
| SpO2 at PWC 150 (%) | 97.45 | 4.84 | 98.11 | 3.02 | 98.66 | 2.17 | 98.18 | 2.71 |
| Systolic blood pressure at PWC130 (mmHg) | 151.00 | 28.67 | 149.34 | 29.18 | 152.38 | 29.30 | 150.79 | 25.75 |
| Systolic blood pressure at PWC150 (mmHg) | 157.45 | 28.28 | 160.80 | 28.54 | 155.11 | 24.18 | 152.51 | 24.34 |
| Dyastolic blood pressure at PWC130 (mmHg) | 75.19 | 13.81 | 74.76 | 14.37 | 76.13 | 15.84 | 74.32 | 10.57 |
| Dyastolic blood pressure PWC150 (mmHg) | 78.61 | 14.48 | 77.88 | 14.15 | 77.02 | 12.24 | 79.22 | 11.68 |
| Breathing frequency at PWC130 (1/min) | 22.34 | 5.79 | 21.60 | 4.59 | 21.76 | 10.97 | 21.38 | 4.53 |
| Breathing frequency at PWC150 (1/min) | 24.15 | 6.64 | 23.09 | 4.74 | 22.26 | 4.87 | 23.00 | 4.67 |
| Perceived respiratory effort at PWC130 (0–10) | 3.19 | 1.52 | 3.89 | 1.70 | 4.30 | 1.92 | 3.96 | 1.59 |
| Perceived respiratory effort at PWC150 (0–10) | 3.97 | 1.71 | 5.12 | 1.92 | 5.34 | 1.95 | 5.12 | 1.83 |
| Perceived physical exertion at PWC130 (0–10) | 3.51 | 1.25 | 3.80 | 1.67 | 3.59 | 1.83 | 3.42 | 1.39 |
| Perceived physical exertion at PWC150 (0–10) | 4.47 | 1.35 | 4.87 | 1.70 | 4.59 | 1.83 | 4.51 | 1.66 |
Bold and grey shaded numbers indicate statistically significant differences in comparison to the no mask condition (Bonferroni corrected p < 0.003). tcpCO2, transcutaneous carbon dioxide partial pressure; SpO2, saturation of peripheral capillary oxygen; PWC, physical working capacity; MedMask, medical face mask; FFP2exhal, filtering facepiece with exhalation valve.
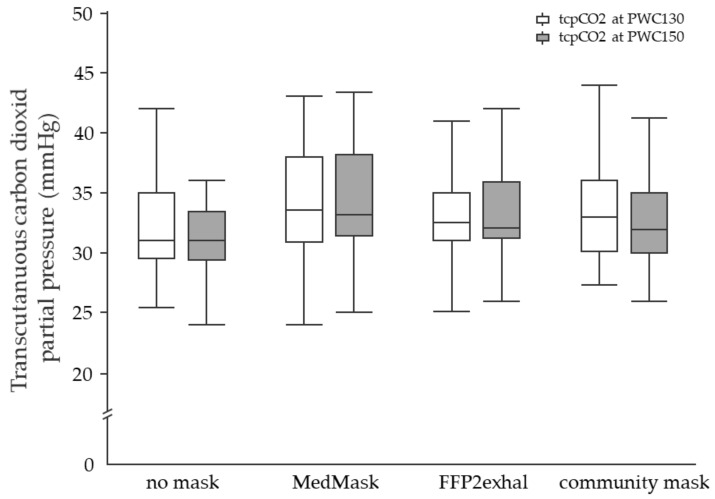
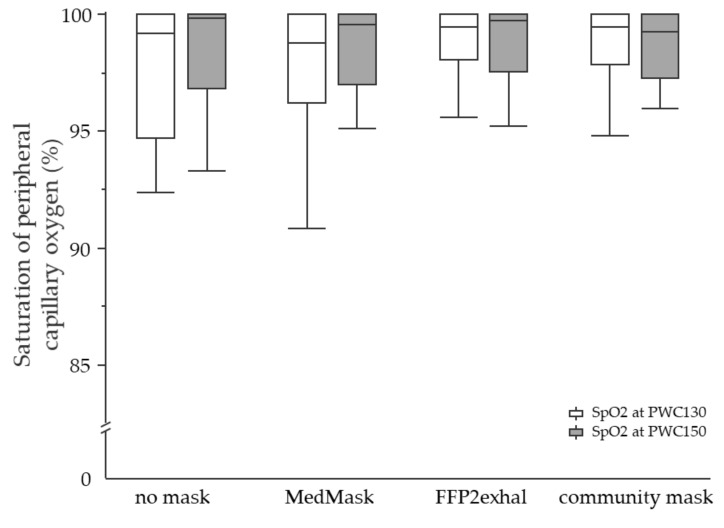
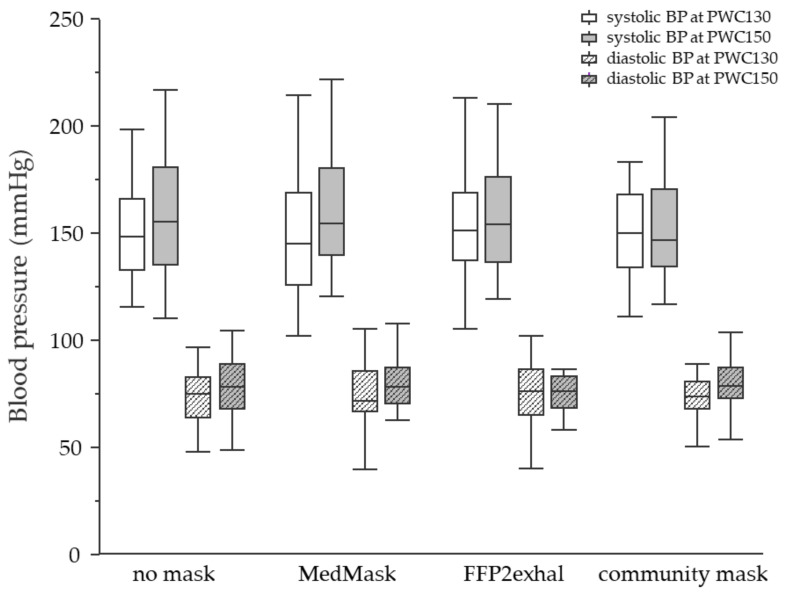
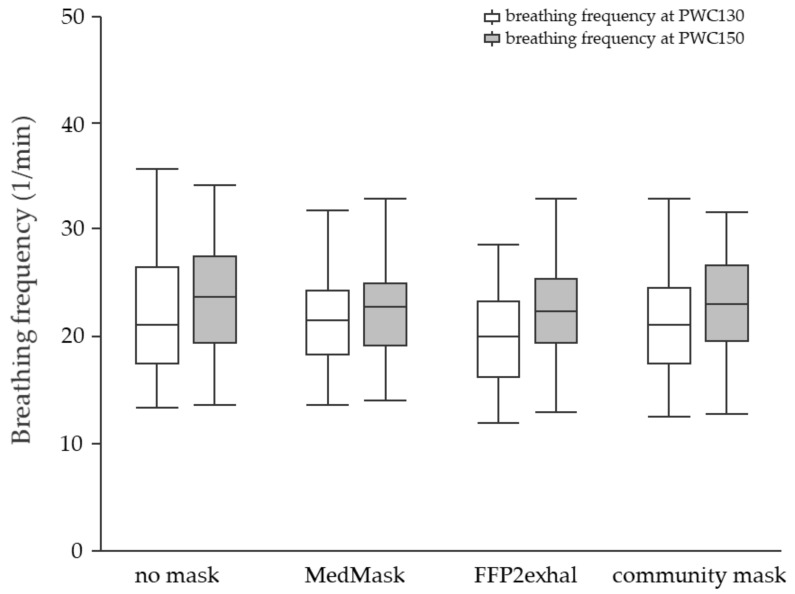
Physiological responses at PWC130 and PWC150: None of the investigated face masks led to statistically significant changes in the physiological response at PWC130 or PWC150 compared to the control condition without mask. Neither sex nor cardiorespiratory fitness level influenced physiological responses due to mask application. Figure 3, Figure 4, Figure 5 and Figure 6 include tcpCO2, SpO2, systolic and diastolic blood pressure, and breathing frequency in response to the four experimental conditions.
Figure 3.
Transcutaneous carbon dioxide partial pressure at the heart rate of 130 and 150 beats per minute using different face masks. Grey shaded boxplots represent the tcpCO2 at PWC150. tcpCO2, transcutaneous carbon dioxide partial pressure; PWC, physical working capacity; MedMask, medical face mask; FFP2exhal, filtering facepiece with exhalation valve.
Figure 4.
Saturation of peripheral capillary oxygen at the heart rate of 130 and 150 beats per minute using different face masks. Grey shaded boxplots represent oxygen saturation at PWC150. SpO2, saturation of peripheral capillary oxygen; PWC, physical working capacity; MedMask, medical face mask; FFP2exhal, filtering facepiece with exhalation valve.
Figure 5.
Systolic and diastolic blood pressure at the heart rate of 130 and 150 beats per minute using different face masks. Filled boxplots represent the systolic blood pressure and grey shaded boxplots represent blood pressure at PWC150. SpO2, saturation of peripheral capillary oxygen; PWC, physical working capacity; MedMask, medical face mask; FFP2exhal, filtering facepiece with exhalation valve.
Figure 6.
Breathing frequency at the heart rate of 130 and 150 beats per minute using different face masks. Grey shaded boxplots represent breathing frequency at PWC150. PWC, physical working capacity; MedMask, medical face mask; FFP2exhal, filtering facepiece with exhalation valve.
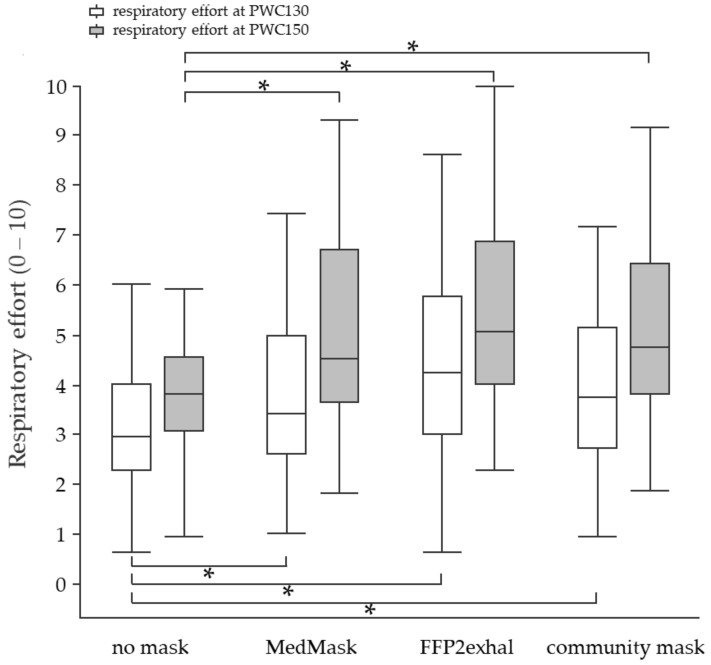
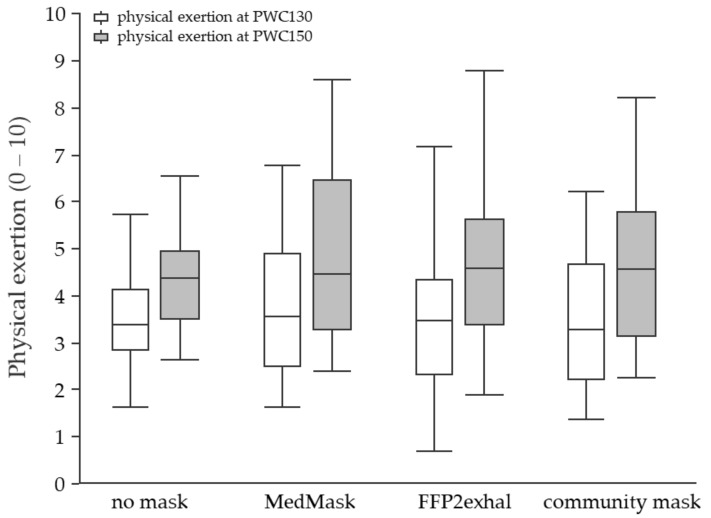
Subjective responses at PWC130 and PWC150: The perceived respiratory effort was higher when masks were worn (Figure 7). The mean difference between the control condition and the MedMask was 0.6 points (CI 0.3 to 0.9, p < 0.0001). In comparison to not using a face mask, the community mask and FFP2exhal led to a mean increase of 0.8 (CI 0.5 to 1.1, p < 0.0001) and 1 point (CI 0.7 to 1.3, p < 0.0001) on the zero-to-ten Borg-CR10 scale, respectively. The perceived level of physical exertion did not change when wearing any of the three face masks (Figure 8).
Figure 7.
Perceived respiratory effort at the heart rate of 130 and 150 beats per minute using different face masks. Grey shaded boxplots represent respiratory effort at PWC150. Asterisks indicate statistically significant differences (Bonferroni corrected p < 0.003). 0 = no respiratory effort, 10 = maximum respiratory effort. PWC, physical working capacity; MedMask, medical face mask; FFP2exhal, filtering facepiece with exhalation valve.
Figure 8.
Perceived physical exertion at the heart rate of 130 and 150 beats per minute using different face masks. Grey shaded boxplots represent physical exertion at PWC150. 0 = no physical exertion, 10 = maximum physical exertion. PWC, physical working capacity; MedMask, medical face mask; FFP2exhal, filtering facepiece with exhalation valve.
4. Discussion
The primary aim of the present study was to confirm that wearing a MedMask does not decrease physical working capacity (PWC). Secondary, the influence of a filtering facepiece mask with exhalation valve class 2 (FFP2exhal) and a cotton fabric mask (community mask) on PWC was also investigated. Complementary, corresponding physiological and subjective responses as well as a potential moderating role of subjects’ cardiorespiratory fitness and sex on mask effects were analyzed.
Noninferiority of the MedMask in PWC130 compared to not wearing a mask could be proved. Additionally, the results clearly indicated that wearing typical face masks recommended during the COVID-19 pandemic does not influence PWC, as was shown by the mechanical power in watt per kilogram bodyweight at the heart rates 130 and 150 bpm during a standardized bicycle ergometer protocol in a relevant manner although PWC130 was slightly and statistically significant reduced when using the FFP2exhal compared to the no mask condition. Neither was wearing a MedMask nor a FFP2exhal or community mask associated with any relevant changes in physiological response. However, respiratory effort has been perceived somewhat more demanding when wearing face masks. Sex and cardiorespiratory fitness level did not change the influence of the face masks.
In many occupational settings, wearing a MedMask has become mandatory, and depending on the circumstances at work, different face masks are required. Many types of masks have been shown to have a high potential in reducing the risk for aerosol transmission of SARS-CoV-2 when properly used [4]. Potential negative side effects of the masks on wearers’ physical performance and health were already addressed by several studies summarized by Kisilinsky and colleagues [8]. However, the currently available literature is considered to lacking high-quality data from well-design studies [15]. The present well-powered study with its randomized intra-individual cross-over design and 39 participants (grouped in three cardiorespiratory fitness levels, mixed age structure, balanced for sex) aims to address this shortcoming in the scientific literature.
Several studies already tested potential side effects of face masks using different bicycle ergometer protocols and outcomes [13,14,16]. Fikenzer, Uhe, Lavall, Rudolph, Falz, Busse, Hepp, and Laufs [14] applied a ramp protocol until maximum exertion with an increase of 50 W within 3 min. In the study by Georgi and colleagues, three load levels (50, 75, and 100 W) were applied for a period of 3 min, and steady state cycling for 30 min was used [13]. Furthermore, Fikenzer et al. and Lässing et al. measured pulmonary function parameters by putting an additional spirometry mask over the face mask. Both found increased physiological demands when wearing a MedMask, and Fiekenzer et al. reported additional impairments by using a FFP2/N95 mask [13,14]. This approach has significant limitations in terms of generalizability since the typical leakage characteristics under daily use has been changed. Georgi, Haase-Fielitz, Meretz, Gasert, and Butter [16] did not use measurements interfering with the face masks and found clinically non-relevant changes in tcpCO2 when wearing either a MedMask, FFP2, or fabric mask compared to the no mask. SpO2 was slightly reduced when a FFP2 mask was worn but again in a clinically non-relevant range. Our study revealed no changes in tcpCO2 or SpO2 between mask and control conditions. Of course, our experimental approach was different from Georgi et al. since we did not use absolute load levels. However, our results also showed no change in the individual mechanical power when a MedMask or community mask were worn. Minor reductions in PWC130 occurred when the FFP2exhal was used, but these changes of 0.17 W/kg can also be regarded as non-relevant related to proposed norm values [26]. Furthermore, we used a FFP2 mask with exhalation valve instead of a common FFP2/N95 mask. By using a FFP2exhal, carbon dioxide rebreathing can be avoided by a better breathing gas exchange during the exhalation phase, which may be the main reason for discrepancies between our results and the results of Georgi et al. [16]. The reason for using an FFP2exhal in the present study are the German recommendations for wear-time limits at the workplace, which will be discussed in a later paragraph of the paper. Generally, our study confirms many results of previously conducted studies. We did not find any relevant change in physical performance and physiological response when wearing a face mask. This was also shown by Ramos-Camp, et al. [41], who reported similar strength performance and physiological response when using a surgical or FFP2 mask during resistance training in people with sarcopenia. In addition, the authors of a recent review article [15] concluded that although dyspnea may be increased, and perceived effort may be altered when using face masks, the effects on work of breathing, blood gases, and other physiological parameters during physical activity are small, often too small to be detected. This conclusion exactly represents the results of the present study with higher self-reported respiratory effort when wearing a mask but no effects on breathing frequency or any other physiological response. Additionally, no conclusions for moderating factors, such as sex-based differences in the physiological responses to exercise while wearing a face mask, could be drawn in the review [15]. To investigate the potential moderating role of sex and cardiorespiratory fitness was a secondary study outcome. In this respect, neither sex nor cardiorespiratory fitness were identified as moderating factors of mask effects. A previous study indicated an association of a low cardiorespiratory fitness level with more negative responses when wearing face masks [16], which could not be confirmed by the present study.
As already mentioned in the introduction section, scientific results regarding potential side effects of face masks are urgently required not only for improving scientific knowledge but for providing a scientific basis for face mask recommendations during the COVID-19 pandemic. In Germany, wear-time limitations for masks worn for COVID-19 prevention at the workplace have been adopted from wear-time limits to avoid overload of the users when using particle-filtering half-masks with an exhalation valve (similar to N95 masks with respect to the respiratory resistance and the total leakage) as protective measure against hazardous dust [10]. It is further recommended to adjust wear-time limits based the required physical workload at a workplace. In this context, a low physical workload would allow up to three hours of mask use, and high workloads would further reduce the recommended wearing time of two hours [11]. Although our study was not directly designed to investigate the effects of different wearing times, the results of the present study do not provide any reason to support this recommendation. There were no additional physical demands when wearing face masks at a medium physical activity (heat rate of 130 bpm) resulting in lower PWC values. The continuous exercising without removing the masks until the heart rate of 150 bpm did also not lead to any impairments regarding PWC or negative physiological responses. Another recommendation regarding wearing-time limitations of face masks at the workplace, which is in better agreement with the results of the present study, is given by the German Federal Institute of Occupational Safety and Health. For medical masks, no health hazards are assumed [42]; for FFP2 masks, individual and occupational activity-dependent regulations should be made according to a risk assessment at the workplace and in consultation with an occupational physician [43].
Limitations
A limitation of the present study is the rather short observation period. In a study with a 30-min steady-state bicycle ergometer protocol, changes in heart rate due to wearing a MedMask only appeared at the end of the 30-min period [13]. Although Lassing, Falz, Pokel, Fikenzer, Laufs, Schulze, Holldobler, Rudrich, and Busse [13] applied a spirometry mask over a surgical mask, leading to an unrealistic leakage, it could be that changes may occur after prolonged face mask use. Another limitation to be mentioned is an increasing number of missing data in SpO2, tcpCO2, and blood pressure (Appendix E) with increasing workload. Although all methods are used during exercise [34,44,45], data loss was unsatisfying. However, the relatively large sample size and the fact that data losses occurred in all experimental conditions, as well as a statistical analysis able to deal with missing data, allow us to consider the results reliable. Finally, psychological aspects of face-mask wearing were not considered.
5. Conclusions
The results of the present study provide reason to believe that wearing face masks for infection prevention during the COVID-19 pandemic does not pose relevant additional physical strain on the user although some more respiratory effort is required.
Acknowledgments
We would like to thank the physicians of Kern medical GmbH and Ümityaz Dilek for their support in data acquisition. We acknowledge support by Open Access Publishing Fund of University of Tübingen.
Appendix A. In- and Exclusion Criteria
Verification of the in- and exclusion criteria was done by a physician by assessing subjects’ medical history, blood pressure, breathing sounds, the results of a spirometric pulmonary function test, and the performance and electrocardiogram during a physical performance test (until subjective exhaustion) on standard bicycle ergometer.
Inclusion Criteria
Age between 18 and 67 years
Being able to work full shift
No diseases of the metabolism or cardiovascular or respiratory system
Written informed consent
Medically unobtrusive physical maximum endurance test and pulmonary function test.
The pulmonary function test was applied according to the American Thoracic Society [46] using peak flow meters (spiro mobile, custo med GmbH, Ottobrunn, Germany or SpiroPro+, CareFusion Germany 234 GmbH).
Exclusion Criteria
Acute myocardial infarction (within the last 48 h)
Unstable angina pectoris with a high risk of infection
Uncontrolled symptomatic and hemodynamically unstable arrhythmias
Severe symptomatic aortic stenosis
Uncontrolled symptomatic heart failure
Acute myo- or pericarditis
Acute pulmonary embolism or acute pulmonary infarction
Acute aortic dissection
Main stem stenosis
Slight aortic stenosis
Arrhythmias tachyarrhythmia, bradyarrhythmia, frequent ventricular extra systoles
Higher atrioventricular block
Severe hypertrophic obstructive cardiomyopathy of an outflow tract
Severe arterial hypertension (systolic BD > 200 mmHg and/or diastolic BD > 110 mmHg)
Electrolyte disorders, especially hyperkalemia
Physical or psychological impairments, due to which an optimal examination is not possible (e.g., febrile infection)
According to [24]:
Diabetes
Acute illness
Under- or overweight (adipositas degree 1)—BMI < 18,5 kg/m²; or >30 kg/m²
Indications of a disease or disorder of the cardiovascular system assessed by a physical performance test (until subjective exhaustion on a standard bicycle ergometer).
Indications of a disease or disorder of the respiratory system assessed by the pulmonary function test.
Pregnancy.
Appendix B. Preliminary Results of Eight Subjects for Sample Size Calculation
Table A1.
PWC130 values of eight preliminary assessed participants.
| Subject | Sex | Body Weight | PWC 130 (W/kg) | Difference in PWC130 (No Mask − MedMask) |
|
|---|---|---|---|---|---|
| No Mask | MedMask | ||||
| 1 | m | 105 | 2.02 | 1.93 | 0.09 |
| 2 | m | 78 | 2.19 | 2.38 | −0.19 |
| 4 | m | 72 | 1.3 | 1.41 | −0.11 |
| 3 | w | 70 | 0.69 | 0.73 | −0.04 |
| 5 | w | 70 | 1.63 | 1.81 | −0.18 |
| 6 | w | 67 | 1.29 | 1.34 | −0.05 |
| 7 | w | 63 | 1.26 | 0.89 | 0.37 |
| 8 | m | 84 | 0.92 | 1.05 | −0.13 |
Appendix C. Time Intervals between Ergometer Testing
Table A2.
Time intervals between the maximum and submaximum bicycle ergometer tests.
| Time Interval | Time Difference | ||||
|---|---|---|---|---|---|
| Minimum | 25th Percentile | Median | 75th Percentile | Maximum | |
| difference between PWCmax and first PWCsubmax test (days) | 2 | 3 | 4 | 6 | 24 |
| difference between first and second PWCsubmax test (days) | 0 | 0 | 1 | 4 | 11 |
| difference between second and third PWCsubmax test (days) | 0 | 0 | 1 | 4 | 7 |
| difference between third and fourth PWCsubmax test (days) | 0 | 0 | 1 | 4 | 12 |
| differnce between PWCsubmax tests (days) | 0 | 0.33 | 1.67 | 3.67 | 7.33 |
| differences between the start of the PWCsubmax tests on the examination days (min) | 2 | 6 | 10 | 20 | 93 |
Appendix D. Abort Criteria for the Bicycle Ergometer Testing According
Abort criteria followed the recommendations by [24], and all bicycle ergometer tests were monitored by a physician.
Electro-cardiology findings:
Progressive arrhythmias
Frequent ventricular extrasystoles (e.g., couplets, bursts)
Ventricular tachycardia
Increasing supraventricular extrasystoles
Atrial tachycardia
Atrial flutter
Newly occurring atrial fibrillation.
Progressive excitation conduction disorders
Increasing QRS widening
Occurrence of a thigh block
Progressive excitatory dysfunction,
e.g., horizontal or descending ST line depression > 0.2 mV
Progressive ST-segment elevation
Monophasic deformation.
Hemodynamics:
Progressive drop in blood pressure
Insufficient blood pressure rise
Excessive blood pressure rise (>250 mmHg systolic and/or >120 mmHg diastolic)
Insufficient increase in heart rate, decrease in heart rate
Appendix E. Missing Data
Table A3.
Missing data per outcome parameter.
| Outcome Parameter | Number of Missing Data (Total Number of Data = 156) |
|---|---|
| PWC130 | 8 |
| PWC150 | 33 |
| tcpCO2 at PWC130 | 17 |
| tcpCO2 at PWC150 | 65 |
| SpO2 at PWC 130 | 15 |
| SpO2 at PWC 150 | 66 |
| Systolic blood pressure at PWC130 | 28 |
| Systolic blood pressure at PWC150 | 28 |
| Dyastolic blood pressure at PWC130 | 74 |
| Dyastolic blood pressure PWC150 | 74 |
| Breathing frequency at PWC130 | 9 |
| Breathing frequency at PWC150 | 34 |
| Perceived respiratory effort at PWC130 | 8 |
| Perceived respiratory effort at PWC150 | 34 |
| Perceived physical exertion at PWC130 | 8 |
| Perceived physical exertion at PWC150 | 33 |
Appendix F. Statistical Models
Table A4.
Comparison between all face mask conditions—linear mixed model 1.
| Model | Outcome Parameter | Dependent Variable | Degree of Freedom | F-Value | p-Value |
|---|---|---|---|---|---|
| 1 | PWC130 | Face mask condition | 3 | 8.900 | <0.0001 |
| SpO2 | Face mask condition | 3 | 0.783 | 0.506 | |
| tcPCO2 | Face mask condition | 3 | 2.240 | 0.088 | |
| Systolic blood presurre | Face mask condition | 3 | 0.149 | 0.930 | |
| Diastolic blood presurre | Face mask condition | 3 | 0.299 | 0.826 | |
| Breathing frequency | Face mask condition | 3 | 0.367 | 0.777 | |
| Perceived respiratory effort | Face mask condition | 3 | 16.907 | <0.0001 | |
| Perceived physical exertion | Face mask condition | 3 | 1.115 | 0.346 | |
| 1 | PWC150 | Face mask condition | 3 | 1.530 | 0.213 |
| SpO2 | Face mask condition | 3 | 0.532 | 0.662 | |
| tcPCO2 | Face mask condition | 3 | 4.292 | 0.008 | |
| Systolic blood presurre | Face mask condition | 3 | 0.677 | 0.570 | |
| Diastolic blood presurre | Face mask condition | 3 | 0.284 | 0.837 | |
| Breathing frequency | Face mask condition | 3 | 1.165 | 0.328 | |
| Perceived respiratory effort | Face mask condition | 3 | 16.274 | <0.0001 | |
| Perceived physical exertion at PWC150 | Face mask condition | 3 | 1.280 | 0.286 |
Bonferroni corrected alpha level is 0.003. Statistically significant results are shaded in grey and written in bold letters.
Table A5.
Comparison of all face masks including face mask condition and sex—linear mixed model 2.
| Model | Outcome Parameter | Dependent Variable | Degree of Freedom | F-Value | p-Value |
|---|---|---|---|---|---|
| 2 | PWC130 | Face mask condition | 3 | 8.931 | <0.0001 |
| sex | 1 | 14.220 | 0.001 | ||
| SpO2 | Face mask condition | 3 | 0.787 | 0.504 | |
| sex | 1 | 0.002 | 0.964 | ||
| tcPCO2 | Face mask condition | 3 | 2.166 | 0.097 | |
| sex | 1 | 5.138 | 0.030 | ||
| Systolic blood presurre | Face mask condition | 3 | 0.143 | 0.934 | |
| sex | 1 | 7.750 | 0.009 | ||
| Diastolic blood presurre | Face mask condition | 3 | 0.283 | 0.837 | |
| sex | 1 | 5.459 | 0.025 | ||
| Breathing frequency | Face mask condition | 3 | 0.367 | 0.777 | |
| sex | 1 | 0.034 | 0.854 | ||
| Perceived respiratory effort | Face mask condition | 3 | 16.927 | <0.0001 | |
| sex | 1 | 7.925 | 0.008 | ||
| Perceived physical exertion | Face mask condition | 3 | 1.125 | 0.342 | |
| sex | 1 | 8.923 | 0.005 | ||
| 2 | PWC150 | Face mask condition | 3 | 1.484 | 0.225 |
| sex | 1 | 14.091 | 0.001 | ||
| SpO2 | Face mask condition | 3 | 0.416 | 0.742 | |
| sex | 1 | 7.443 | 0.011 | ||
| tcPCO2 | Face mask condition | 3 | 4.278 | 0.008 | |
| sex | 1 | 1.338 | 0.258 | ||
| Systolic blood presurre | Face mask condition | 3 | 0.834 | 0.481 | |
| sex | 1 | 8.429 | 0.008 | ||
| Diastolic blood presurre | Face mask condition | 3 | 0.293 | 0.830 | |
| sex | 1 | 1.104 | 0.304 | ||
| Breathing frequency | Face mask condition | 3 | 1.143 | 0.336 | |
| sex | 1 | 1.356 | 0.253 | ||
| Perceived respiratory effort | Face mask condition | 3 | 16.375 | <0.0001 | |
| sex | 1 | 4.897 | 0.034 | ||
| Perceived physical exertion at PWC150 | Face mask condition | 3 | 1.253 | 0.295 | |
| sex | 1 | 8.318 | 0.007 |
Bonferroni corrected alpha level is 0.003. Statistically significant results are shaded in grey and written in bold letters.
Table A6.
Comparison of all face masks including face mask condition and cardiorespiratory fitness (maximum physical working performance of an initial bicycle ergometer test)—linear mixed model 3.
| Model | Outcome Parameter | Dependent Variable | Degree of Freedom | F-Value | p-Value |
|---|---|---|---|---|---|
| 3 | PWC130 | Face mask condition | 3 | 8.857 | <0.0001 |
| Cardiorespiratory fitness | 1 | 64.454 | <0.0001 | ||
| SpO2 | Face mask condition | 3 | 0.774 | 0.511 | |
| Cardiorespiratory fitness | 1 | 0.558 | 0.461 | ||
| tcPCO2 | Face mask condition | 3 | 2.254 | 0.087 | |
| Cardiorespiratory fitness | 1 | 9.957 | 0.003 | ||
| Systolic blood presurre | Face mask condition | 3 | 0.133 | 0.940 | |
| Cardiorespiratory fitness | 1 | 8.930 | 0.005 | ||
| Diastolic blood presurre | Face mask condition | 3 | 0.293 | 0.830 | |
| Cardiorespiratory fitness | 1 | 0.507 | 0.481 | ||
| Breathing frequency | Face mask condition | 3 | 0.370 | 0.775 | |
| Cardiorespiratory fitness | 1 | 0.633 | 0.432 | ||
| Perceived respiratory effort | Face mask condition | 3 | 16.912 | <0.0001 | |
| Cardiorespiratory fitness | 1 | 35.445 | 0.235 | ||
| Perceived physical exertion | Face mask condition | 3 | 1.116 | 0.346 | |
| Cardiorespiratory fitness | 1 | 0.630 | 0.433 | ||
| 3 | PWC150 | Face mask condition | 3 | 1.419 | 0.243 |
| Cardiorespiratory fitness | 1 | 87.273 | <0.0001 | ||
| SpO2 | Face mask condition | 3 | 0.464 | 0.708 | |
| Cardiorespiratory fitness | 1 | 0.579 | 0.452 | ||
| tcPCO2 | Face mask condition | 3 | 4.244 | 0.009 | |
| Cardiorespiratory fitness | 1 | 0.915 | 0.347 | ||
| Systolic blood presurre | Face mask condition | 3 | 0.801 | 0.498 | |
| Cardiorespiratory fitness | 1 | 5.041 | 0.033 | ||
| Diastolic blood presurre | Face mask condition | 3 | 0.295 | 0.829 | |
| Cardiorespiratory fitness | 1 | 0.138 | 0.713 | ||
| Breathing frequency | Face mask condition | 3 | 1.153 | 0.333 | |
| Cardiorespiratory fitness | 1 | 4.440 | 0.043 | ||
| Perceived respiratory effort | Face mask condition | 3 | 16.348 | <0.0001 | |
| Cardiorespiratory fitness | 1 | 2.621 | 0.115 | ||
| Perceived physical exertion at PWC150 | Face mask condition | 3 | 1.303 | 0.279 | |
| Cardiorespiratory fitness | 1 | 2.225 | 0.145 |
Bonferroni corrected alpha level is 0.003. Statistically significant results are shaded in grey and written in bold letters.
Table A7.
Comparison of all face masks including face mask condition, sex, and the interaction term face mask condition x sex—linear mixed model 4.
| Model | Outcome Parameter | Dependent Variable | Degree of Freedom | F-Value | p-Value |
|---|---|---|---|---|---|
| 4 | PWC130 | Face mask condition | 3 | 8.718 | <0.001 |
| sex | 1 | 14.252 | 0.001 | ||
| Face mask condition × sex | 3 | 0.448 | 0.719 | ||
| SpO2 | Face mask condition | 3 | 8.718 | <0.001 | |
| sex | 1 | 14.252 | 0.001 | ||
| Face mask condition × sex | 3 | 0.448 | 0.719 | ||
| tcPCO2 | Face mask condition | 3 | 8.718 | <0.001 | |
| sex | 1 | 14.252 | 0.001 | ||
| Face mask condition × sex | 3 | 0.448 | 0.719 | ||
| Systolic blood presurre | Face mask condition | 3 | 8.718 | <0.001 | |
| sex | 1 | 14.252 | 0.001 | ||
| Face mask condition × sex | 3 | 0.448 | 0.719 | ||
| Diastolic blood presurre | Face mask condition | 3 | 8.718 | <0.001 | |
| sex | 1 | 14.252 | 0.001 | ||
| Face mask condition × sex | 3 | 0.448 | 0.719 | ||
| Breathing frequency | Face mask condition | 3 | 8.718 | <0.001 | |
| sex | 1 | 14.252 | 0.001 | ||
| Face mask condition × sex | 3 | 0.448 | 0.719 | ||
| Perceived respiratory effort | Face mask condition | 3 | 17.287 | <0.001 | |
| sex | 1 | 7.938 | 0.008 | ||
| Face mask condition × sex | 3 | 2.799 | 0.044 | ||
| Perceived physical exertion | Face mask condition | 3 | 1.134 | 0.339 | |
| sex | 1 | 8.949 | 0.005 | ||
| Face mask condition × sex | 3 | 0.595 | 0.62 | ||
| 4 | PWC150 | Face mask condition | 3 | 1.703 | 0.173 |
| sex | 1 | 14.001 | 0.001 | ||
| Face mask condition × sex | 3 | 2.215 | 0.93 | ||
| SpO2 | Face mask condition | 3 | 0.191 | 0.902 | |
| sex | 1 | 7.738 | 0.01 | ||
| Face mask condition × sex | 3 | 0.309 | 0.819 | ||
| tcPCO2 | Face mask condition | 3 | 3.133 | 0.032 | |
| sex | 1 | 1.649 | 0.21 | ||
| Face mask condition × sex | 3 | 0.883 | 0.455 | ||
| Systolic blood presurre | Face mask condition | 3 | 0.881 | 0.456 | |
| sex | 1 | 8.535 | 0.007 | ||
| Face mask condition × sex | 3 | 0.402 | 0.752 | ||
| Diastolic blood presurre | Face mask condition | 3 | 0.17 | 0.916 | |
| sex | 1 | 1.259 | 0.273 | ||
| Face mask condition × sex | 3 | 0.711 | 0.549 | ||
| Breathing frequency | Face mask condition | 3 | 1.432 | 0.239 | |
| sex | 1 | 1.409 | 0.244 | ||
| Face mask condition × sex | 3 | 2.522 | 0.063 | ||
| Perceived respiratory effort | Face mask condition | 3 | 17.911 | <0.001 | |
| sex | 1 | 4.702 | 0.037 | ||
| Face mask condition × sex | 3 | 2.843 | 0.043 | ||
| Perceived physical exertion at PWC150 | Face mask condition | 3 | 1.299 | 0.28 | |
| sex | 1 | 8.223 | 0.007 | ||
| Face mask condition × sex | 3 | 0.634 | 0.595 |
Bonferroni corrected alpha level is 0.003. No statistically significant interactions of face mask condition with sex appeared.
Table A8.
Comparison of all face masks including mask condition, cardiorespiratory fitness, and the interaction term face mask condition x cardiorespiratory fitness—linear mixed model 5.
| Model | Outcome Parameter | Dependent Variable | Degree of Freedom | F-Value | p-Value |
| 5 | PWC130 | Face mask condition | 3 | 0.754 | 0.522 |
| Cardiorespiartory fitness | 1 | 64.576 | < 0.001 | ||
| Face mask condition × cardiorespiratory fitness | 3 | 1.884 | 0.137 | ||
| SpO2 | Face mask condition | 3 | 1.526 | 0.213 | |
| Cardiorespiartory fitness | 1 | 0.584 | 0.45 | ||
| Face mask condition × cardiorespiratory fitness | 3 | 2.198 | 0.093 | ||
| tcPCO2 | Face mask condition | 3 | 2.182 | 0.095 | |
| Cardiorespiartory fitness | 1 | 9.903 | 0.003 | ||
| Face mask condition × cardiorespiratory fitness | 3 | 1.401 | 0.247 | ||
| Systolic blood presurre | Face mask condition | 3 | 1.021 | 0.387 | |
| Cardiorespiartory fitness | 1 | 9.117 | 0.005 | ||
| Face mask condition × cardiorespiratory fitness | 3 | 1.171 | 0.326 | ||
| Diastolic blood presurre | Face mask condition | 3 | 0.321 | 0.810 | |
| Cardiorespiartory fitness | 1 | 0.518 | 0.477 | ||
| Face mask condition × cardiorespiratory fitness | 3 | 0.522 | 0.669 | ||
| Breathing frequency | Face mask condition | 3 | 3.417 | 0.020 | |
| Cardiorespiartory fitness | 1 | 0.647 | 0.426 | ||
| Face mask condition × cardiorespiratory fitness | 3 | 3.690 | 0.014 | ||
| Perceived respiratory effort | Face mask condition | 3 | 0.431 | 0.731 | |
| Cardiorespiartory fitness | 1 | 1.446 | 0.237 | ||
| Face mask condition × cardiorespiratory fitness | 3 | 0.943 | 0.423 | ||
| Perceived physical exertion | Face mask condition | 3 | 0.221 | 0.882 | |
| Cardiorespiartory fitness | 1 | 0.625 | 0.434 | ||
| Face mask condition × cardiorespiratory fitness | 3 | 0.495 | 0.687 | ||
| 5 | PWC150 | Face mask condition | 3 | 1.703 | 0.173 |
| Cardiorespiartory fitness | 1 | 14.001 | 0.001 | ||
| Face mask condition × cardiorespiratory fitness | 3 | 2.215 | 0.93 | ||
| SpO2 | Face mask condition | 3 | 0.191 | 0.902 | |
| Cardiorespiartory fitness | 1 | 7.738 | 0.01 | ||
| Face mask condition × cardiorespiratory fitness | 3 | 0.309 | 0.819 | ||
| tcPCO2 | Face mask condition | 3 | 3.133 | 0.032 | |
| Cardiorespiartory fitness | 1 | 1.649 | 0.21 | ||
| Face mask condition × cardiorespiratory fitness | 3 | 0.883 | 0.455 | ||
| Systolic blood presurre | Face mask condition | 3 | 0.881 | 0.456 | |
| Cardiorespiartory fitness | 1 | 8.535 | 0.007 | ||
| Face mask condition × cardiorespiratory fitness | 3 | 0.402 | 0.752 | ||
| Diastolic blood presurre | Face mask condition | 3 | 0.17 | 0.916 | |
| Cardiorespiartory fitness | 1 | 1.259 | 0.273 | ||
| Face mask condition × cardiorespiratory fitness | 3 | 0.711 | 0.549 | ||
| Breathing frequency | Face mask condition | 3 | 1.432 | 0.239 | |
| Cardiorespiartory fitness | 1 | 1.409 | 0.244 | ||
| Face mask condition × cardiorespiratory fitness | 3 | 2.522 | 0.063 | ||
| Perceived respiratory effort | Face mask condition | 3 | 17.911 | <0.001 | |
| Cardiorespiartory fitness | 1 | 4.702 | 0.037 | ||
| Face mask condition × cardiorespiratory fitness | 3 | 2.843 | 0.043 | ||
| Perceived physical exertion at PWC150 | Face mask condition | 3 | 1.299 | 0.28 | |
| Cardiorespiartory fitness | 1 | 8.223 | 0.007 | ||
| Face mask condition × cardiorespiratory fitness | 3 | 0.634 | 0.595 |
Bonferroni corrected alpha level is 0.003. No statistically significant interactions of face mask condition with cardiorespiratory fitness level appeared.
Author Contributions
Conceptualization, B.S., R.S., A.B. and M.A.R.; methodology, B.S., R.S, R.B., M.B., J.G., M.M., T.D. and A.B.; formal analysis, P.M.; investigation, M.M., T.D. and R.B.; data curation, J.B. and J.G.; writing—original draft preparation, B.S.; writing—review and editing, M.A.R., R.S., J.G. and M.B.; visualization, B.S., J.G. and J.B.; project administration, B.S., M.B. and J.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Daimler AG.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the Medical Faculty of the University of Tübingen (851/2020BO1).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data are not publicly available due to data use restrictions contained in study participants’ information material.
Conflicts of Interest
The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results. Furthermore, the Institute of Occupational and Social Medicine and Health Services Research receives an unrestricted grant of the employers’ association of the metal and electrical industry Baden-Württemberg (Südwestmetall; Germany).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Federal Ministry of Health Novel Coronavirus SARS-CoV-2—Information and Practical Advice. Berlin. 2020. [(accessed on 28 October 2021)]. Available online: https://assets.zusammengegencorona.de/eaae45wp4t29/29lyMngJAvYypiWvqOTtVr/5707e9a6f5ea1681c4d0d1d5e09019f4/BMG_Corona_Information_englisch.pdf.
- 2.Federal State Baden-Württemberg CORONA-VERORDNUNG—Maßnahmen Gegen die Ausbreitung des Coronavirus. 2021. [(accessed on 28 October 2021)]. Available online: https://www.baden-wuerttemberg.de/de/system/pdf/?tx_rsmbwbrowserlesspdf_pi1%5Burls%5D%5B0%5D=https%3A%2F%2Fwww.baden-wuerttemberg.de%2Fde%2Fservice%2Faktuelle-infos-zu-corona%2Faktuelle-corona-verordnung-des-landes-baden-wuerttemberg%2F%3Ftype%3D98&print=1.
- 3.Worl Health Organization Advice for the Public: Coronavirus Disease (COVID-19) [(accessed on 28 October 2021)]. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.
- 4.Abboah-Offei M., Salifu Y., Adewale B., Bayuo J., Ofosu-Poku R., Opare-Lokko E.B.A. A rapid review of the use of face mask in preventing the spread of COVID-19. Int. J. Nurs. Stud. Adv. 2021;3:100013. doi: 10.1016/j.ijnsa.2020.100013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Federal Institute for Occupational Safety and Health Empfehlungen der BAuA zum Einsatz von Schutzmasken in der Arbeitswelt im Zusammenhang mit SARS-CoV-2. 2021. [(accessed on 28 October 2021)]. Available online: https://www.baua.de/DE/Themen/Arbeitsgestaltung-im-Betrieb/Coronavirus/pdf/Schutzmasken.pdf?__blob=publicationFile&v=20.
- 6.De Brouwer C. Wearing a Mask, a Universal Solution against COVID-19 or an Additional Health Risk? 2020. [(accessed on 28 October 2021)]. Available online: https://ssrn.com/abstract=3676885.
- 7.Shaw K.A., Zello G.A., Butcher S.J., Ko J.B., Bertrand L., Chilibeck P.D. The impact of face masks on performance and physiological outcomes during exercise: A systematic review and meta-analysis. Appl. Physiol. Nutr. Metab. 2021;46:693–703. doi: 10.1139/apnm-2021-0143. [DOI] [PubMed] [Google Scholar]
- 8.Kisielinski K., Giboni P., Prescher A., Klosterhalfen B., Graessel D., Funken S., Kempski O., Hirsch O. Is a Mask That Covers the Mouth and Nose Free from Undesirable Side Effects in Everyday Use and Free of Potential Hazards? Int. J. Environ. Res. Public Health. 2021;18:4344. doi: 10.3390/ijerph18084344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Worl Health Organization Coronavirus Disease (COVID-19) Advice for the Public: When and How to Use Masks. [(accessed on 28 October 2021)]. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/when-and-how-to-use-masks.
- 10.Koordinierungskreises für Biologische Arbeitsstoffe (KOBAS) Empfehlung zur Tragezeitbegrenzung für Mund-Nase-Bedeckungen (MNB) im Sinne des SARS-CoV-2-Arbeitsschutzstandards und der SARS-CoV-2-Arbeitsschutzregel. Deutsche Gesetzliche Unfallversicherung e.V. 2020. [(accessed on 28 October 2021)]. Available online: https://www.dguv.de/medien/inhalt/praevention/themen_a_z/biologisch/kobas/stellungnahme_gefaehrdung_durch_co2_beim_tragen-von-masken_16_11_2020.pdf.
- 11.German Social Accident Insurance . DGUV Regel 112–190 Benutzung von Atemschutzgeräten. Volume 112–190. Deutsche Gesetzliche Unfallversicherung e.V. (DGUV); Berlin, Germany: 2011. [(accessed on 28 October 2021)]. Available online: https://publikationen.dguv.de/regelwerk/dguv-regeln/1011/benutzung-von-atemschutzgeraeten. [Google Scholar]
- 12.Laird I.S., Goldsmith R., Pack R.J., Vitalis A. The effect on heart rate and facial skin temperature of wearing respiratory protection at work. Ann. Occup. Hyg. 2002;46:143–148. doi: 10.1093/annhyg/mef015. [DOI] [PubMed] [Google Scholar]
- 13.Lassing J., Falz R., Pokel C., Fikenzer S., Laufs U., Schulze A., Holldobler N., Rudrich P., Busse M. Effects of surgical face masks on cardiopulmonary parameters during steady state exercise. Sci. Rep. 2020;10:22363. doi: 10.1038/s41598-020-78643-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fikenzer S., Uhe T., Lavall D., Rudolph U., Falz R., Busse M., Hepp P., Laufs U. Effects of surgical and FFP2/N95 face masks on cardiopulmonary exercise capacity. Clin. Res. Cardiol. 2020;109:1522–1530. doi: 10.1007/s00392-020-01704-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hopkins S.R., Dominelli P.B., Davis C.K., Guenette J.A., Luks A.M., Molgat-Seon Y., Sa R.C., Sheel A.W., Swenson E.R., Stickland M.K. Face Masks and the Cardiorespiratory Response to Physical Activity in Health and Disease. Ann. Am. Thorac Soc. 2021;18:399–407. doi: 10.1513/AnnalsATS.202008-990CME. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Georgi C., Haase-Fielitz A., Meretz D., Gasert L., Butter C. The Impact of Commonly-Worn Face Masks on Physiological Parameters and on Discomfort During Standard Work-Related Physical Effort. Dtsch. Arztebl. Int. 2020;117:674–675. doi: 10.3238/arztebl.2020.0674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wiecek M., Szymura J., Maciejczyk M., Cempla J., Szygula Z. Effect of sex and menstrual cycle in women on starting speed, anaerobic endurance and muscle power. Physiol. Int. 2016;103:127–132. doi: 10.1556/036.103.2016.1.13. [DOI] [PubMed] [Google Scholar]
- 18.Westerstahl M., Jansson E., Barnekow-Bergkvist M., Aasa U. Longitudinal changes in physical capacity from adolescence to middle age in men and women. Sci. Rep. 2018;8:14767. doi: 10.1038/s41598-018-33141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Proctor D.N., Joyner M.J. Skeletal muscle mass and the reduction of VO2max in trained older subjects. J. Appl. Physiol. 1997;82:1411–1415. doi: 10.1152/jappl.1997.82.5.1411. [DOI] [PubMed] [Google Scholar]
- 20.Lisman P.J., de la Motte S.J., Gribbin T.C., Jaffin D.P., Murphy K., Deuster P.A. A Systematic Review of the Association Between Physical Fitness and Musculoskeletal Injury Risk: Part 1-Cardiorespiratory Endurance. J. Strength Cond. Res. 2017;31:1744–1757. doi: 10.1519/JSC.0000000000001855. [DOI] [PubMed] [Google Scholar]
- 21.Cooper R., Kuh D., Hardy R., Mortality Review G., Falcon, Teams H.A.S. Objectively measured physical capability levels and mortality: Systematic review and meta-analysis. BMJ. 2010;341:c4467. doi: 10.1136/bmj.c4467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Clifton D.R., Nelson D.A., Choi Y.S., Edgeworth D.B., Nelson K.J., Shell D., Deuster P.A. Risk factors for musculoskeletal-related occupational disability among US Army soldiers. BMJ Mil. Health. :2021. doi: 10.1136/bmjmilitary-2021-001900. [DOI] [PubMed] [Google Scholar]
- 23.Petru R., Ochmann U., Nowak D. Letter to the editors referring to Fikenzer, S., Uhe, T., Lavall, D., Rudolph, U., Falz, R., Busse, M., Hepp, P., & Laufs, U. (2020). Effects of surgical and FFP2/N95 face masks on cardiopulmonary exercise capacity. Clinical Research in Cardiology. Clin. Res. Cardiol. 2020;109:1598–1599. doi: 10.1007/s00392-020-01735-5. [DOI] [PubMed] [Google Scholar]
- 24.Chatterjee M., Schmeißer G. Aktualisierter Leitfaden für die Ergometrie im Rahmen arbeitsmedizinischer Untersuchungen. Arb. Soz. Umweltmed. 2017;52:913–921. [Google Scholar]
- 25.Finger J.D., Krug S., Gößwald A., Härtel S., Bös K. English Version: Kardiorespiratorische Fitness bei Erwachsenen in Deutschland. Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1) Bundesgesundheitsbl. 2013;56:772–778. doi: 10.1007/s00103-013-1672-y. [DOI] [PubMed] [Google Scholar]
- 26.Stemper T. Gesundheit, Fitness, Freizeitsport: Praxis des Modernen Gesundheitssports. Bund; Köln, Germany: 1988. p. 144. [Google Scholar]
- 27.Occupational Health and Safety Committees at the BMAS SARS-CoV-2-Arbeitsschutzregel. Ed. Federal Government Germany. 2020. [(accessed on 28 October 2021)]. Available online: https://www.baua.de/DE/Angebote/Rechtstexte-und-Technische-Regeln/Regelwerk/AR-CoV-2/pdf/AR-CoV-2.pdf?__blob=publicationFile&v=15.
- 28.Trappe H.-J., Löllgen H. Leitlinien zur Ergometrie. Z. Kardiol. 2000;89:16. doi: 10.1007/s003920070190. [DOI] [PubMed] [Google Scholar]
- 29.Sammito S., Heblich F., Güttler N. Die Fahrradergometrie in der arbeitsmedizinischen Vorsorge. Zbl. Arbeitsmed. 2020;70:240–246. doi: 10.1007/s40664-020-00387-6. [DOI] [Google Scholar]
- 30.De Zwart B.C., Frings-Dresen M.H., van Dijk F.J. Physical workload and the aging worker: A review of the literature. Int. Arch. Occup. Environ. Health. 1995;68:1–12. doi: 10.1007/BF01831627. [DOI] [PubMed] [Google Scholar]
- 31.Kenny G.P., Yardley J.E., Martineau L., Jay O. Physical work capacity in older adults: Implications for the aging worker. Am. J. Ind. Med. 2008;51:610–625. doi: 10.1002/ajim.20600. [DOI] [PubMed] [Google Scholar]
- 32.Bugajska J., Makowiec-Dabrowska T., Bortkiewicz A., Gadzicka E., Marszalek A., Lewandowski Z., Konarska M. Physical capacity of occupationally active population and capability to perform physical work. Int. J. Occup. Saf. Ergon. 2011;17:129–138. doi: 10.1080/10803548.2011.11076883. [DOI] [PubMed] [Google Scholar]
- 33.Farazdaghi G.R., Wohlfart B. Reference values for the physical work capacity on a bicycle ergometer for women between 20 and 80 years of age. Clin. Physiol. 2001;21:682–687. doi: 10.1046/j.1365-2281.2001.00373.x. [DOI] [PubMed] [Google Scholar]
- 34.Carter R., Banham S.W. Use of transcutaneous oxygen and carbon dioxide tensions for assessing indices of gas exchange during exercise testing. Respir. Med. 2000;94:350–355. doi: 10.1053/rmed.1999.0714. [DOI] [PubMed] [Google Scholar]
- 35.Jubran A. Pulse oximetry. Crit. Care. 2015;19:272. doi: 10.1186/s13054-015-0984-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boshuizen R.C., Vincent A.D., van den Heuvel M.M. Comparison of modified Borg scale and visual analog scale dyspnea scores in predicting re-intervention after drainage of malignant pleural effusion. Support. Care Cancer. 2013;21:3109–3116. doi: 10.1007/s00520-013-1895-3. [DOI] [PubMed] [Google Scholar]
- 37.Kuorinka I., Jonsson B., Kilbom A., Vinterberg H., Biering-Sorensen F., Andersson G., Jorgensen K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl. Ergon. 1987;18:233–237. doi: 10.1016/0003-6870(87)90010-X. [DOI] [PubMed] [Google Scholar]
- 38.Fuchs R., Klaperski S., Gerber M., Seeling H. Messung der Bewegungs- und Sportaktivität mit dem BSA-Fragebogen. Eine methodische Zwischenbilanz. Z. Gesundh. 2015;23:16. doi: 10.1026/0943-8149/a000137. [DOI] [Google Scholar]
- 39.Schielzeth H., Dingemanse N.J., Nakagawa S., Westneat D.F., Allegue H., Teplitsky C., Reale D., Dochtermann N.A., Garamszegi L.Z., Araya-Ajoy Y.G. Robustness of linear mixed-effects models to violations of distributional assumptions. Methods Ecol. Evol. 2020;11:1141–1152. doi: 10.1111/2041-210X.13434. [DOI] [Google Scholar]
- 40.Grace-Martin K. Linear Mixed Models for Missing Data in Pre-Post Studies. In The Analysis Factor. 2021. [(accessed on 28 October 2021)]. Available online: https://www.theanalysisfactor.com/linear-mixed-models-for-missing-data-in-pre-post-studies/
- 41.Ramos-Campo D.J., Perez-Pinero S., Munoz-Carrillo J.C., Lopez-Roman F.J., Garcia-Sanchez E., Avila-Gandia V. Acute Effects of Surgical and FFP2 Face Masks on Physiological Responses and Strength Performance in Persons with Sarcopenia. Biology. 2021;10:213. doi: 10.3390/biology10030213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Federal Institute of Occupational Safety and Health Belastungen durch Mund-Nase-Bedeckungen. 2021. [(accessed on 28 October 2021)]. Available online: https://www.baua.de/DE/Themen/Arbeitsgestaltung-im-Betrieb/Coronavirus/FAQ/26-FAQ_node.html.
- 43.Ausschuss für Arbeitsmedizin—Arbeitsschutzausschüsse beim BMAS Stellungnahme des Ausschusses für Arbeitsmedizin (AfAMed) zu Tragezeitbegrenzungen für FFP2-Masken. Bundesanstalt für Arbeitsschutz und Arbeitsmedizin: 2021. [(accessed on 28 October 2021)]. Available online: https://www.baua.de/DE/Aufgaben/Geschaeftsfuehrung-von-Ausschuessen/AfAMed/pdf/Stellungnahme-Tragezeit-FFP2-Masken.pdf?__blob=publicationFile&v=3.
- 44.Escourrou P.J., Delaperche M.F., Visseaux A. Reliability of pulse oximetry during exercise in pulmonary patients. Chest. 1990;97:635–638. doi: 10.1378/chest.97.3.635. [DOI] [PubMed] [Google Scholar]
- 45.Becque M.D., Katch V., Marks C., Dyer R. Reliability and within subject variability of VE, VO2, heart rate and blood pressure during submaximum cycle ergometry. Int. J. Sports Med. 1993;14:220–223. doi: 10.1055/s-2007-1021167. [DOI] [PubMed] [Google Scholar]
- 46.Bonnie F., Marianna S., Suzanne L., American Thoracic S. Patient information series. Pulmonary function tests. Am. J. Respir. Crit. Care Med. 2014;189:P17–P18. doi: 10.1164/rccm.18910P17. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data are not publicly available due to data use restrictions contained in study participants’ information material.