Abstract
BACKGROUND
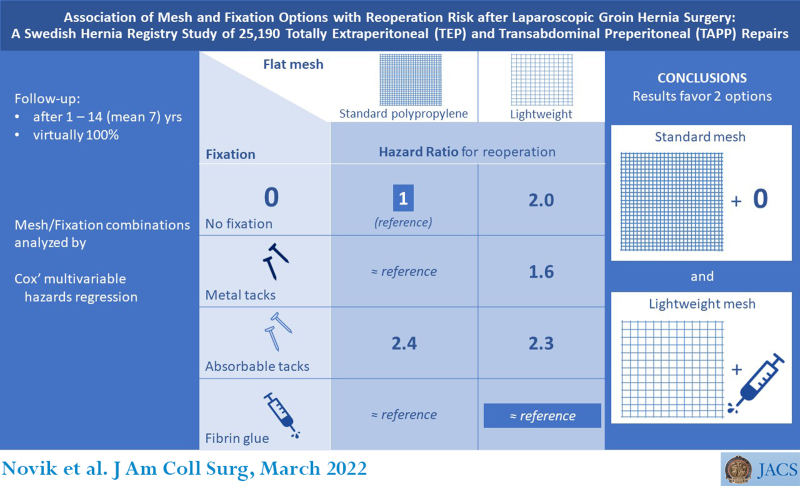
International guidelines concerning mesh and mesh fixation options in laparoscopic totally extraperitoneal (TEP) and transabdominal preperitoneal (TAPP) groin hernia repair are based on studies focusing on either mesh or fixation. We hypothesized that the value of such recommendations is limited by lacking knowledge on how mesh and fixation interact. The current registry-based nationwide cohort study compared different mesh/fixation combinations for relative risks for reoperation after TEP and TAPP groin hernia repair.
STUDY DESIGN
All TEP and TAPP registered in the Swedish Hernia Registry 2005 to 2017 with standard polypropylene (StdPPM) or lightweight (LWM) flat mesh, having tack, fibrin glue, or no fixation, were included. The endpoint was reoperation due to recurrence as of December 31, 2018. Multivariable Cox regression rendered relative risk differences between the exposures, expressed as hazard ratios (HR) with 95% CIs.
RESULTS
Of 25,190 repairs, 924 (3.7%) were later reoperated for recurrence. The lowest, mutually equivalent, reoperation risks were associated with StdPPM without fixation (HR 1), StdPPM with metal tacks (HR 0.8, CI 0.4 to 1.4), StdPPM with fibrin glue (HR 1.1, CI 0.7 to 1.6), and LWM with fibrin glue (HR 1.2, CI 0.97 to 1.6). Except for with fibrin glue, LWM correlated with increased risk, whether affixed with metal (HR 1.7, CI 1.1 to 2.7), or absorbable tacks (HR 2.4, CI 1.8 to 3.1), or deployed without fixation (HR 2.0, CI 1.6 to 2.6).
CONCLUSIONS
With StdPPM, neither mechanical nor glue fixation seemed to improve outcomes. Thus, for this mesh category, we recommend nonfixation. With LWM, we recommend fibrin glue fixation, which was the only LWM alternative on par with nonaffixed StdPPM.
Swedish Hernia Registry data on laparoscopic groin hernia repair were analyzed regarding the impact of mesh fixation. Lightweight mesh vs standard polypropylene mesh was associated with higher reoperation risk, which could be eliminated with fibrin glue fixation. Tacks did not seem to reduce reoperation risk for either mesh type.
CONTINUING MEDICAL EDUCATION CREDIT INFORMATION.
Accreditation: The American College of Surgeons is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
AMA PRA Category 1 CreditsTM: The American College of Surgeons designates this live activity for a maximum of AMA PRA Category 1 CreditTM. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Of the AMA PRA Category 1 CreditsTM listed above, a maximum of 1 credits meet the requirement for Self-Assessment.
The routine use of mesh in groin hernia surgery has engendered substantially decreased recurrence risk.1,2 However, current long-term reoperation rates for recurrence are still disappointing, in the range of 8% to 15%.3-7
Since laparoscopic totally extraperitoneal (TEP)8 and transabdominal preperitoneal (TAPP)9 mesh-based groin hernia repairs were introduced in the early 1990s, they have become well-established. The main principles of TEP and TAPP are similar, and recurrence rates for the 2 methods appear comparable.3,10,11 The mesh is deployed in the same position and anatomical plane in both these procedures, which implies that the required features of optimum mesh and fixation options are identical for TEP and TAPP.
The pioneers of TEP/TAPP typically implanted a flat standard pure polypropylene mesh (StdPPM) and considered mesh fixation mandatory.12 Disposable staplers and tackers were soon devised to evade cumbersome suturing. Eventually, some randomized controlled trials (RCTs) suggested that the preperitoneal mesh position in itself renders fixation redundant, but this controversy is yet not settled.13-18
With a growing interest in reducing chronic postoperative pain, 2 potential improvements were introduced about 2 decades ago: lightweight mesh (LWM) and atraumatic fibrin glue fixation.19,20 Whether these modifications might influence reoperation risk, and if so, in which direction and to which extent, have previously not been conclusively investigated.
The HerniaSurge Group in 2018 compiled the current evidence concerning groin hernias in the extensive International Guidelines for Hernia Management.3 These guidelines are endorsed by affected surgical societies and are now widely acknowledged.21
Concerning risks for recurrence after TEP/TAPP, HerniaSurge states that there are no relevant long-term differences between standard (aka “heavyweight”) and lightweight meshes. In contrast, a large RCT with a 5-year follow-up published in 2018 and more recent meta-analyses have shown that LWM for laparoscopic groin hernia repairs confers a higher recurrence risk without reducing chronic postoperative pain.22-24 However, these studies have not illuminated whether different fixation modalities might modify the less satisfactory outcome with LWM.
On TEP/TAPP, HerniaSurge favors glue fixation instead of staples and tacks (hereafter denoted “tacks” only), however, solely for reducing early postoperative pain. Foremost, the guidelines state that nonfixation will suffice in almost all cases, except for large medial hernias.
Notably, the HerniaSurge statements and recommendations about mesh and fixation in TEP/TAPP are generally based on relatively low levels of evidence; hence, further research is warranted. There is a knowledge gap concerning how different mesh and fixation options interact.
We hypothesized that when evaluating the influence of mesh type and fixation method on the risk of recurrence, it is insufficient to study these 2 variables separately. Rather, each mesh/fixation combination should be assessed as an entity.
The current study was designed to detect relative differences in risk for reoperation associated with the type of flat mesh, depending on the type of fixation (tacks vs fibrin glue vs nonfixation).
METHODS
This report complies with the Strengthening the Reporting of Observational Studies in Epidemiology statement and its Reporting of studies Conducted using Observational Routinely-collected health Data extension.25,26 The study is registered at ClinicalTrials.gov (ID: NCT03755219) and approved by the Regional Ethical Review Board in Stockholm, Sweden: EPN 2008/1082-31/2, with 2 revisions, EPN 2014/2176-32 and EPN 2018/2050-32.
Study design and setting
This population-based observational cohort study retrieved data from the Swedish Hernia Registry (SHR), detailing all TEP/TAPP procedures between January 1, 2005, and December 31, 2017, with complete follow-up about subsequent reoperations and deaths, through December 31, 2018.
The analysis consisted of 2 stages: We first assessed mesh and fixation modalities separately to post hoc determine mesh/fixation combinations suitable for final risk determinations.
The SHR
The SHR records groin hernia repairs in adult patients (age 15 years or older). During the study period, SHR’s nationwide coverage exceeded 95%.6,27 Each repair was prospectively entered together with the date of operation and demographic and intraoperative data. Reoperations for recurrence were recorded in SHR in the same manner as index repairs.
The state-assigned Personal Identity Number is unique for each resident in Sweden, and all Swedish healthcare providers and authorities ubiquitously use it.28 The Personal Identity Number enables prospective life-long follow-up in SHR, with a negligible dropout rate.
To reduce information bias caused by misclassifications, SHR-appointed officials perform annual validations of randomly assigned 10% of the participating surgical units.6
Participants
Virtually all TEP/TAPP repairs operated in Sweden during the inclusion period were recorded in SHR and constitute the study population.
Each repair is considered 1 “participant.” A bilateral operation yields 2 repairs.
Variables
Characteristics of variables at baseline are listed in Table 1 and Table 2.
Table 1.
Baseline Variables
| Variable, category | Male repair | Female repair | All repairs |
|---|---|---|---|
| Repairs included in study, from 82 surgical units | |||
| TEP | 18,720 (74) | 3,442 (14) | 22,162 (88) |
| TAPP | 2,236 (9) | 792 (3) | 3,028 (12) |
| TEP + TAPP | 20,956 (83) | 4,234 (17) | 25,190 (100) |
| Patient age, y | |||
| Range | 15–93 | 15–95 | 15–95 |
| Mean/median (IQR) | 58/60 (49–68) | 57/60 (44–71) | 58/60 (48–69) |
| Primary or recurrent hernia | |||
| Primary hernia | 16,449 (78) | 3,965 (94) | 20,414 (81) |
| Recurrent hernia | 4,507 (22) | 269 (6) | 4,776 (19) |
| Elective or emergency repair | |||
| Elective repair | 20,755 (99) | 4,102 (97) | 24,857 (99) |
| Emergency | 201 (1) | 132 (3) | 333 (1.3) |
| Unilateral repairs | |||
| Right | 4,845 (57) | 1,886 (58) | 6,731 (27) |
| Left | 3,686 (43) | 1,359 (42) | 5,045 (20) |
| All repairs, unilateral | 8,531 (41) | 3,245 (77) | 11,776 (47) |
| Bilateral repairs, each side = 1 repair | |||
| Right | 6,214 (50) | 500 (51) | 6,714 (27) |
| Left | 6,211 (50) | 489 (49) | 6,700 (27) |
| All repairs, part of bilateral operation | 12,425 (59) | 989 (23) | 13,414 (53) |
| Hernia anatomy | |||
| EHS classification | |||
| Lateral | 9,591 (46) | 2,472 (58) | 12,063 (48) |
| Medial | 8,839 (42) | 535 (13) | 9,374 (37) |
| Lateral + medial | 1,620 (8) | 99 (2.3) | 1,719 (7) |
| Femoral | 291 (1.4) | 770 (18) | 1,061 (4) |
| Lateral + femoral | 156 (0.7) | 174 (4.1) | 330 (1.3) |
| Medial + femoral | 152 (0.7) | 60 (1.4) | 212 (0.8) |
| Lateral + medial + femoral | 50 (0.2) | 11 (0.3) | 61 (0.2) |
| Sum | 20,699 (99) | 4,121 (97) | 24,820 (99) |
| Unknown/unspecified | 257 (1) | 113 (3) | 370 (1) |
| Hernia defect size | |||
| EHS classification | |||
| EHS I (< 1.5 cm) | 3,891 (19) | 1,819 (43) | 5,710 (23) |
| EHS II (1.5–3 cm) | 1,390 (59) | 2,135 (50) | 14,525 (58) |
| EHS III (> 3 cm) | 4,239 (20) | 259 (6) | 4,498 (18) |
| EHS I–III | 20,520 (98) | 4,213 (99.5) | 24,733 (98) |
| Unknown/unspecified | 436 (2) | 21 (0.5) | 457 (2) |
Data presented as n (%) unless otherwise noted.
EHS, European Hernia Society; IQR, interquartile range; TAPP, (laparoscopic) transabdominal preperitoneal mesh repair; TEP, (laparoscopic) totally extraperitoneal mesh repair.
Table 2.
Mesh and Fixation Alternatives
| Variable, category | Male repair | Female repair | All repairs |
|---|---|---|---|
| Stage 1a, preliminary mesh analysis | |||
| Mesh | |||
| StdPPM | 8,404 (40) | 1,010 (24) | 9,414 (37) |
| LWM | 11,678 (56) | 2,938 (69) | 14,616 (58) |
| LWPPM | 5,555 (27) | 1,324 (31) | 6,879 (27) |
| Ultrapro | 5,658 (27) | 1,552 (37) | 7,210 (29) |
| Timesh | 275 (1.3) | 31 (0.7) | 306 (1.2) |
| Vypro | 190 (0.9) | 31 (0.7) | 221 (0.9) |
| Polyester | 874 (4) | 286 (6.8) | 1,160 (5) |
| Sum | 20,956 (100) | 4,234 (100) | 25,190 (100) |
| Stage 1b, preliminary fixation analysis | |||
| Fixation | |||
| No fixation | 6,438 (31) | 1,443 (34) | 7,881 (31) |
| Tacks, all | 8,575 (41) | 1,289 (30) | 9,864 (39) |
| Tacks, metal | 1,219 (6) | 322 (8) | 1,541 (6) |
| Tacks, absorbable | 2,761 (13) | 580 (14) | 3,341 (13) |
| Tacks, unclassified | 4,595 (22) | 387 (9) | 4,982 (20) |
| Fibrin glue | 5,943 (28) | 1,502 (35) | 7,445 (30) |
| Sum | 20,956 (100) | 4,234 (100) | 25,190 (100) |
| Stage 2, final analysis of mesh/fixation combination | |||
| Mesh + fixation | |||
| StdPPM/without fixation | 3,457 (22) | 405 (11) | 3,862 (20) |
| StdPPM/metal tacks | 543 (3.5) | 172 (4.9) | 715 (3.8) |
| StdPPM/absorbable tacks | 370 (2.4) | 69 (2.0) | 439 (2.3) |
| StdPPM/fibrin glue | 888 (5.8) | 121 (3.4) | 1,009 (5.3) |
| LWM/without fixation | 2,738 (18) | 953 (27) | 3,691 (19) |
| LWM/metal tacks | 490 (3.2) | 104 (2.9) | 594 (3.1) |
| LWM/absorbable tacks | 1,976 (13) | 355 (10) | 2,331 (12) |
| LWM/fibrin glue | 4,978 (32) | 1,357 (38) | 6,335 (33) |
| Sum | 15,440 (100) | 3,536 (100) | 18,976 (100) |
LWM (stage 1) = LWPPM + Ultrapro + Timesh + Vypro. LWM (stage 2) = LWPPM + Ultrapro + Timesh.
LWM, lightweight mesh; LWPPM, lightweight pure polypropylene mesh; StdPPM, standard pure polypropylene mesh.
Outcomes
Our endpoints occurred at identifiable exact dates, which enabled a time-to-event analysis approach with high precision (1 day).
The primary endpoint was reoperation for recurrence, defined as any hernioplasty in a groin in which a hernia has previously been repaired when the patient was 15 years or older. Even if the index repair was for a different anatomic hernia type, we regarded the subsequent hernia a recurrence. A fundamental principle in TEP/TAPP repair is that the mesh should reinforce the entire myopectineal orifice of Fruchaud to prevent all anatomic types of recurrence.29 We thereby considered the patient’s perspective, from which it is irrelevant whether an “actual” recurrence or an anatomically “new” hernia causes a need for another operation.30
The secondary endpoint was death. The Swedish Population Registry continuously reports new demises to SHR. The date of death concluded the individual follow-up if an antecedent reoperation had not already been recorded.
Exposures
We investigated 2 main exposures, separate and in combination: type of mesh and type of mesh fixation. The first author (BN) originally devised the current SHR classifications of, respectively, mesh and fixation, which were used in this study.
Mesh
The SHR classifies polypropylene-based flat meshes by weight, arbitrarily as standard (50 g/m2 or greater) or lightweight (less than 50 g/m2), but disregards pore size.31 Accordingly, pure polypropylene meshes are either StdPPM or lightweight pure polypropylene mesh (LWPPM).
SHR further registers 3 lightweight composite polypropylene-based mesh options for laparoscopic repair by their brand names, Vypro and Ultrapro (Ethicon), and Timesh (PFM Medical). The SHR has not distinguished various generations and versions of these 3 trademarks.
Because polyester meshes are not classified by weight in SHR, they were included only in the first stage of the analyses.
The final study stage comprised solely polypropylene-based meshes, dichotomously classified as StdPPM or LWM.
Fixation
The subjects of this study are the predominant fixation alternatives: tacks, fibrin glue, and nonfixation.
From 2012 onwards, SHR classifies tacks by their material: metal, absorbable, and (excluded due to negligible numbers) plastic nonabsorbable. Before then, SHR did not specify tack material; repairs with any type of tacks from 2005 to 2011 are listed as “Tacks, unclassified” in Table 2.
In the first stage of analysis, we compared metal, absorbable, and unclassified tacks to reveal whether they rendered similar outcomes, which would have justified merging them in the final stage analysis.
Exclusion criteria
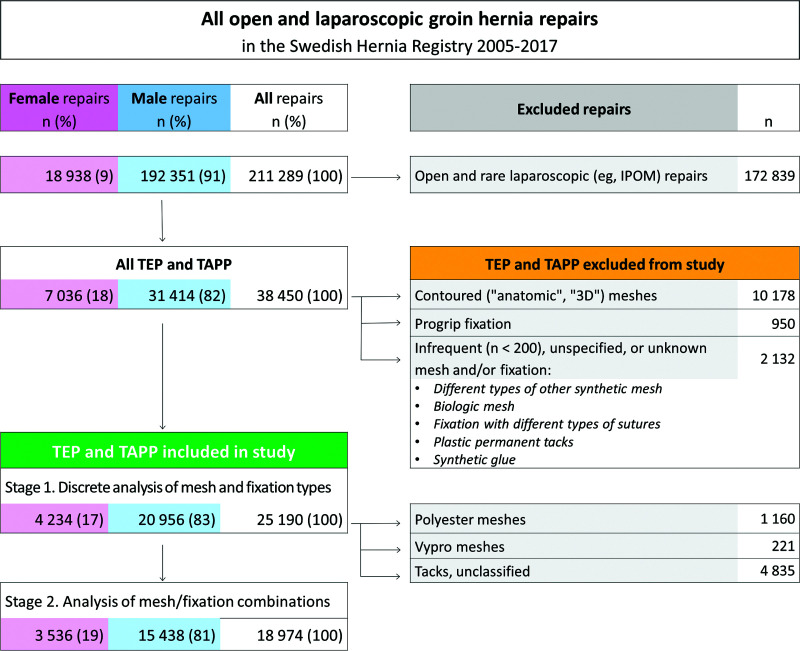
See Figure 1. Contoured, aka “anatomic” or “three-dimensional,” meshes were excluded because SHR has not recorded their material and weight.
Figure 1.
Study flow chart. 3D, three-dimensional; IPOM intraperitoneal onlay mesh; TAPP, (laparoscopic) transabdominal preperitoneal mesh repair; TEP, (laparoscopic) totally extraperitoneal mesh repair.
Various mesh materials and designs with Progrip fixation technology (Medtronic) have been marketed.32 Due to the subgrouping complexity, SHR recordings of these mesh materials are unreliable; therefore, we excluded them.
Repairs with infrequent (n < 200), unspecified, or unknown type of mesh or fixation were also excluded.
Effect modifiers and confounders
In the multivariable model, we adjusted for 10 plausible risk factors (Table 1). We adjusted for TEP vs TAPP, the patient’s sex and age, primary vs recurrent hernia, elective vs emergency procedure, bilateral vs unilateral repair, right vs left groin, hernia anatomy and size, and surgical unit (center, facility).
In the first stage, the separate analysis of meshes was also adjusted for fixation modality, and the discrete analysis of fixation was also adjusted for mesh type (Table 2).
Age was a continuous variable. Sex was defined by genotype as male or female.33 SHR does not register race/ethnicity and socioeconomic indicators.34
Hernia anatomy and defect size were registered according to the European Hernia Society (EHS) classification. Anatomically, a groin hernia is termed lateral, medial, femoral, or combinations thereof. The defect diameter is defined as small (EHS I; less than 1.5 cm), medium-sized (EHS II; 1.5 to 3 cm), or large (EHS III; more than 3 cm).35 Swedish surgeons typically bridge large defects without fascia closure.
The individual surgeon and the surgical unit are indisputably important confounders.36-39 Because these 2 predictors interrelate, only 1 of them could be chosen for the multivariable model. Our retrieved database essentially did not allow assessing individual practitioners, and therefore we adjusted for the surgical unit.
Statistical methods
All analyses were based on time-to-event data, with an accuracy of 1 day.
Life tables computed observed cumulative reoperation rates, graphically depicted as inverse Kaplan–Meier plots. The attached tables detail annual numbers at risk.
Relative risks for reoperation were calculated by multivariable Cox proportional hazards regression for each assessed exposure, expressed as hazard ratio (HR) with a 2-tailed, 95% CI. Statistical significance was defined as p < 0.05. To justify using the Cox model, we have tested and verified that our data fulfilled the proportional hazards assumption, ie, that the HRs between the compared groups remained constant over time.40 In the Cox graphs, the compared curves have different inclinations but otherwise similar shapes because the proportional hazards model constructs each plot to mirror the curve of the reference.
We compared excluded vs included repairs, to reveal any significant overall difference in cumulative reoperation rate.
Analysis was conducted in IBM SPSS Statistics, version 22 (IBM).
RESULTS
Participants
During the inclusion period, the SHR overall recorded 211,289 repairs of groin hernias. Of those, TEP and TAPP accounted for 38,450 (18%), of which 25,190 (66%) fulfilled the inclusion criteria and constituted the study cohort (Fig. 1).
Baseline characteristics
Table 1 and Table 2 summarize the baseline data. Although annual numbers of groin hernia operations in Sweden remained relatively constant during the study period, the percentage of laparoscopic repairs steadily increased from 8% in 2005 to 36% in 2018. Some 82 surgical units contributed at least 1 repair that fulfilled the inclusion criteria.
Mesh
Among included repairs, 95% had a polypropylene-based mesh. Of those, more than 60% were LWM.
Mesh fixation
There was a somewhat even distribution between tacks (39%), fibrin glue (30%), and nonfixation (31%).
Outcome data
All repairs were followed until December 31, 2018, after 1 to 14 (mean 6.9, median 6.8) years. By then, 924 (3.7%) groins had been reoperated due to recurrence. Patients who died during the observation period accounted for 1,884 (7.5%) index repairs, of whom 60 (3.2%) had been reoperated before the demise.
There was no reoperation difference between excluded (HR 1.1, CI 0.9 to 1.2) vs included (HR 1) repairs (Fig. 2), with unadjusted and multivariable analysis rendering similar HRs and CIs.
Figure 2.
Included vs excluded (laparoscopic) totally extraperitoneal mesh and (laparoscopic) transabdominal preperitoneal mesh repairs. Cumulative incidence of reoperations. postop, post operation; Reop, reoperation.
Main results
In the proportional hazards regressions, the differences between the unadjusted and the multivariable analyses were quite small and did not essentially affect the relationships between the subgroups. We therefore present only the multivariable results.
Preliminary analysis: discrete examination of mesh and fixation types
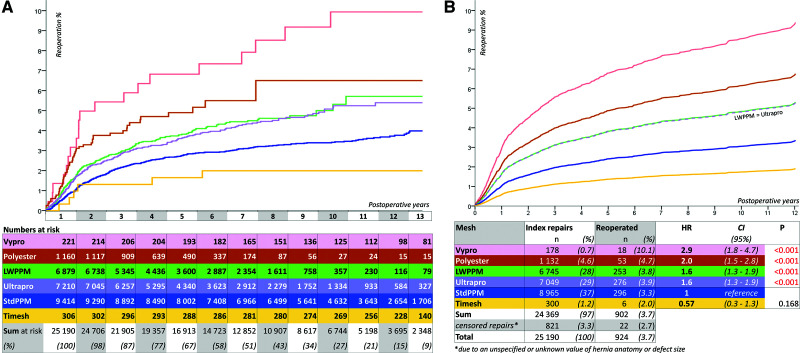
Mesh.
Figure 3 details the results of the mesh analysis.
Figure 3.
Mesh. (A) Cumulative incidence of reoperations. (B) Multivariable proportional hazards regression. Adjusted for (laparoscopic) totally extraperitoneal mesh repair vs (laparoscopic) transabdominal preperitoneal mesh repair, the patient’s sex and age, emergency vs elective procedures, recurrent vs primary hernia, bilateral vs unilateral repair, right vs left groin, hernia anatomy and size, surgical unit, and fixation type. Note that the LWPPM and Ultrapro curves are identical, reflecting equal hazard ratios (HRs). LWPPM, lightweight pure polypropylene mesh; postop, post operation; Reop, reoperation; StdPPM, standard pure polypropylene mesh.
With StdPPM chosen as reference (HR 1), Ultrapro and LWPPM had identical, 60% elevated HR. Polyester was associated with a doubled and Vypro with an almost tripled HR.
In our sample, even a high-volume surgeon has accounted for a mere fraction of all repairs. Hence, individual practitioners’ impact on the overall results was marginal. Exceptions were the Timesh repairs, where 1, by chance identified, surgeon contributed 255 (83%) of 306 repairs. These resulted in a far below average reoperation rate. The remaining 51 Timesh repairs were distributed among 19 surgical units and had a reoperation rate more typical for other LWMs.
In contrast, the 221 Vypro repairs were more widely dispersed among centers, suggesting that its radically worse outcome was likely attributable to the mesh construction per se. In addition, Vypro has progressively been substituted by Ultrapro and has not been reported in SHR for TEP/TAPP since 2015.
For the final analysis, we deemed LWPPM, Ultrapro, and Timesh to be comparable, which justified merging them into 1 LWM category. The outlier and obsolete Vypro was eliminated from further analysis.
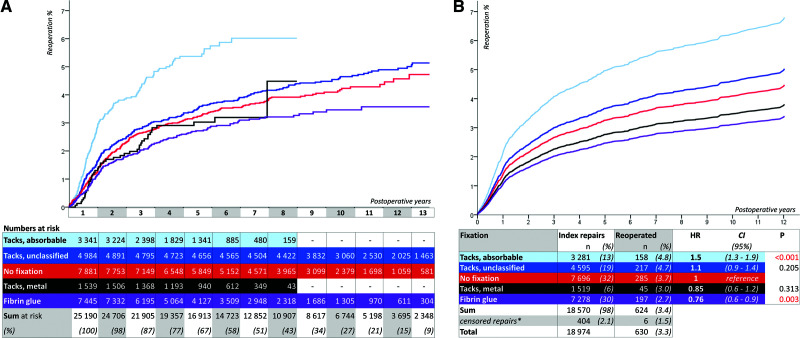
Mesh fixation.
Figure 4 details the results of the fixation modality analysis.
Figure 4.
Fixation. (A) Cumulative incidence of reoperations; (B) Multivariable proportional hazards regression. Adjusted for (laparoscopic) totally extraperitoneal mesh repair vs (laparoscopic) transabdominal preperitoneal mesh repair, the patient’s sex and age, emergency vs elective procedures, recurrent vs primary hernia, bilateral vs unilateral repair, right vs left groin, hernia anatomy and size, surgical unit, and mesh type. HR, hazard ratio; postop, post operation; Reop, reoperation.
Reference (HR 1) was nonfixation. Fibrin glue was the only fixation modality associated with a lower reoperation risk. Metal tacks were on par with nonfixation, whereas absorbable tacks correlated with a higher risk. Unclassified tacks rendered an outcome in between metal and absorbable tacks.
The disparate results of the tack subgroups precluded merging them for the final analysis. Accordingly, we retained metal and absorbable tacks as distinct variable categories and omitted unclassified tacks.
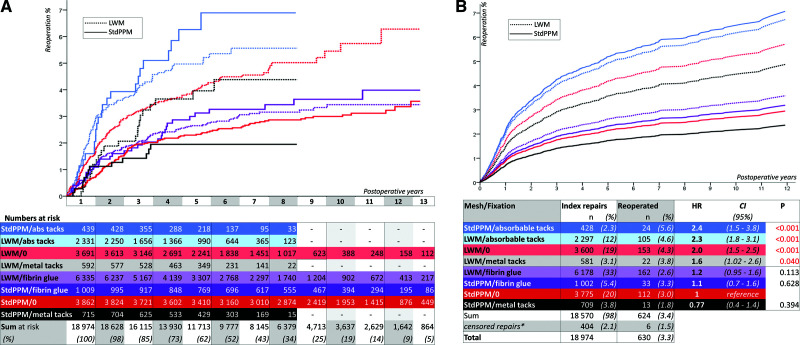
Final analysis: 8 combinations of mesh and fixation
We dichotomously categorized meshes selected for final analysis as either StdPPM or LWM. The 4 fixation alternatives retained for the final analysis were metal tacks, absorbable tacks, fibrin glue, and nonfixation. With 2 mesh and 4 fixation options, we constructed a mesh/fixation variable having 8 configurations (Fig. 5).
Figure 5.
Mesh/fixation combinations. (A) Cumulative incidence of reoperations. 0, no fixation; abs, absorbable. (B) Multivariable proportional hazards regression. Adjusted for (laparoscopic) totally extraperitoneal mesh repair vs (laparoscopic) transabdominal preperitoneal mesh repair, the patient’s sex and age, emergency vs elective procedures, recurrent vs primary hernia, bilateral vs unilateral repair, right vs left groin, hernia anatomy and size, and surgical unit. HR, hazard ratio; LWM, lightweight mesh; postop, post operation; Reop, reoperation; StdPPM, standard pure polypropylene mesh.
We chose StdPPM without fixation (StdPPM/0) to be the reference. The best results were associated with StdPPM/0, StdPPM/metal tacks, StdPPM/fibrin glue, and LWM/fibrin glue. LWM/0 correlated with a doubled risk. Notably, no category of tacks was associated with any significant benefit for either StdPPM or LWM.
Other analyses
Sex
Initially, we intended to present all results stratified by sex.41 Noteworthy was that repairs of women’s hernias had an overall strikingly lower reoperation risk, not affected by multivariable adjustment (HR 0.3, CI 0.2 to 0.4, p < 0.001). Depending on mesh/fixation, female outcomes displayed patterns resembling those for male repairs, albeit they were underpowered for meaningful stratified presentation.
Hernia categories
At the early preparatory stage of the current study, we surveyed all potential risk factors recorded in SHR to determine which ones to adjust for in the multivariable model. In an unadjusted analysis, large (EHS III; HR 1.5, CI 1.2 to 1.9, p < 0.001), and medium-sized (EHS II; HR 1.2, CI 1.04 to 1.5, p = 0.015) defects were, not unexpectedly, linked to somewhat higher reoperation risks in comparison with small (EHS I; HR 1) defects.
We also found that the defect size more than the anatomic category predicted reoperation risk. When adjusted for hernia defect size and sex, medial (HR 0.97, CI 0.84 to 1.1, p = 0.73) vs lateral (HR 1) hernias correlated with similar reoperation risks. In particular, among large defects, medial hernias (HR 1.1, CI 0.8 to 1.5, p = 0.6) exhibited no higher reoperation risk than lateral (HR 1) ones. This finding refutes the common conception that medial hernia per se is a significant risk factor.3,42-44
Subsequently, we reanalyzed our mesh/fixation combinations with the same multivariable analysis as previously, now stratified by hernia defect size. Notwithstanding problematic low statistical power for many of the combinations, LWM/0 vs StdPPM/0 (HR 1) correlated with significantly higher reoperation risks in small (HR 1.7, CI 1.001 to 3.0, p = 0.049) and medium-sized (HR 2.3, CI 1.7 to 3.2, p < 0.001) defects, consistent with the main study findings.
The multivariable model yielded insufficient power for large defects, preventing adequate statistical inference, whereas in the unadjusted analysis, LWM/0 was linked to a higher risk (HR 1.8, CI 1.4 to 2.2, p < 0.001).
DISCUSSION
Key results
With a population-based cohort of laparoscopic groin hernia repairs, we in 2 stages investigated reoperation risks depending on various combinations of mesh and mesh fixation.
The first stage assessed meshes and fixations separately. We found various LWM types and absorbable tacks to be associated with higher reoperation risks, whereas fibrin glue correlated with a lower risk.
The second stage analysis of mesh/fixation combinations was the cardinal objective of the study. The results support our hypothesis that the need for fixation depends on the mesh category. With StdPPM, none of the fixation modalities correlated with a significantly better outcome than nonfixation. In contrast, fibrin glue, but neither type of tacks, eliminated the higher reoperation risk associated with LWM.
The discrete mesh analysis results contradict HerniaSurge but corroborate recent studies showing LWM to be an independent risk factor for recurrence.24 On the other hand, our findings support HerniaSurge in that tack fixation, in general, did not seem to reduce the reoperation risk.3 An entirely novel discovery was that fibrin glue was associated with significantly improved results for LWM, albeit not for StdPPM.
To our knowledge, this is the first investigation using clinical data to assess how standard vs lightweight meshes interact with diverse fixation modalities to affect the recurrence risk after TEP and TAPP. Moreover, it is one of the largest TEP and/or TAPP studies yet published. The cohort size has allowed finally addressing some controversial issues with sufficient power.
Interpretation
Our hypothesis was confirmed; investigating the mesh/fixation combination as 1 entity might lead to results different from those one would infer if only having analyzed the 2 variables discretely. Mesh/fixation interaction has previously been demonstrated by a Danish group who used an ingenious sheep model for studying long-term mesh shrinkage and adhesions after laparoscopic ventral hernia repair.45,46
We attempted to detect small but clinically relevant differences in reoperation risk that could be ascribed exclusively to the mesh and/or the fixation, in a surgical procedure with an abundance of other potential risk factors, of which some (eg, surgeon skill, patient sex, connective tissue frailty) probably will have more impact than the choice of mesh and fixation. To this end, a comprehensive registry study outperforms a RCT.3,47
With virtually complete nationwide coverage, SHR compiles a huge database with a low bias risk. The quality of surgical care is very homogeneous throughout Sweden, with a tax-financed healthcare system available to all residents at an affordable fee. Race/ethnicity, socioeconomic indicators, and place of residence minimally influence access to adequate operations and may not confound outcomes.
The broad range of surgeons and centers involved strengthens the external validity; the outcome reflects real-world routine practice.
Patients with a recurrence may choose to undergo the next repair at a different facility than the previous repair. Therefore, personal or institutional reoperation rates typically underestimate the factual rates.48 In contrast, the ubiquitous use of the Personal Identity Number in Swedish healthcare, and SHR’s nationwide coverage, ensure negligible dropout rates, ie, there is no attrition bias.49
The open hernia mesh pioneers René Stoppa and George Wantz taught that fixation is unnecessary in the preperitoneal position. On the topic of mesh fixation in laparoscopic repairs, Wantz referenced Stoppa and remarked, “The mesh is held in place initially by intraabdominal pressure and later by connective tissue that renders the peritoneum inextensible so it can’t protrude.”14 However, that insight was acquired before the advent of LWM. Now our results indicate that Stoppa’s principle may not always apply when using LWM in TEP and TAPP, at least not for some patients.
Certain mesh/fixation combinations were associated with significantly elevated risks of reoperation. After 12 years, the reoperation rate was about 6.5% for LWM/0, in contrast with 3.5% for StdPPM/0 as well as for LWM/fibrin glue. We deem this difference has substantial clinical relevance. For example, with 800,000 groin hernioplasties annually in the US an overall 3 percentage points higher reoperation rate would translate to an extra 24,000 repairs and even more actual recurrences.50
Fibrin glue was associated with significantly lower reoperation risk for LWM but did not seem to add any benefit for StdPPM. We have empirically observed that for fibrin to glue effectively, most of the mesh must lie in immediate contact with the underlying tissue and adapt to its contours, relatively straightforward to accomplish with a pliable LWM but nearly impossible with a more rigid StdPPM.12,14
Although fibrin glue correlated with improved results for LWM, tacks did not. One reason might be that tacks are typically applied at only a few spots, for safety reasons. Conversely, fibrin glue allows fixation of almost the entire mesh surface, including in the anatomic triangles of pain and doom, where tacks are prohibited.20 Moreover, although probably not a common phenomenon, tacks have been reported to be able to cause recurrence by traumatizing either the patient’s tissue or the mesh.51,52
Reoperation and death were the only endpoints. Nevertheless, our results implicitly concern postoperative pain and economics.14 Tissue-penetrating mesh fixation is a well-known cause of chronic postoperative pain.18,53 Our findings indicate that avoiding tacks will not increase the overall reoperation risk. A tacker costs approximately $300 to $450 in the US.54 If we assume TEP/TAPP to constitute 50% of all 800,000 annual groin hernioplasties in US, refraining from tacks in half of the laparoscopic repairs would save $60 to $90 million per year.
Furthermore, regular LWPPM and the 2 to 3 times more expensive Ultrapro were associated with almost identical reoperation risks. Hence, when choosing between different LWMs, it seems the “premium” price for Ultrapro does not translate into any evident clinical benefit.
Reoperation as endpoint
Reoperation rate figures without reported follow-up time are meaningless. Reoperations will continue to occur for decades after the index repairs, but at a progressively slower pace.55-60 The average adult groin hernia patient in Sweden is about 60 years at the operation. With increasing age comes deteriorating health, and hence, every additional postoperative year will reduce the likelihood for a recurrence to be reoperated. This phenomenon may, in part, explain why the increase of cumulative reoperation percentages tend to decelerate with time and eventually plateau at around 8% to 15%, despite that a recurrence may occur during the remainder of a patient’s life.3-6,60 Hence, the approximately 5% reoperation rate after 12 years in our study might possibly double with lifelong follow-up.
Intuitively, some would consider recurrence a more pertinent outcome variable than reoperation. Indeed, in short- and midterm clinical hernia trials, recurrence is a more common primary endpoint than reoperation. However, for pragmatic reasons, recurrence is then typically assessed at long intervals. From a scientific methodology standpoint, that may be problematic. In practice, those intervals will vary somewhat among the study participants and thereby preclude the possibility of establishing precise time-to-event figures, which will complicate adequate comparison between groups. With a massive cohort like the one in the current study, using reoperation instead as the endpoint is more practical and accurate. Further, in analogy with what is well established in long-term outcomes research of orthopedic implants, we consider the cumulative reoperation rate a clinically relevant outcome measure.61
In a defined population and at any given postoperative time of follow-up, the factual recurrence rate will always pronouncedly exceed the reoperation rate.62 A previous SHR-based cohort study on consecutive, unselected groin hernia patients operated in 1 county hospital, with clinical follow-up after 3 years, found the recurrence/reoperation ratio to be 3:1.50
The recurrence/reoperation ratio typically will turn out smaller in a RCT. First, RCTs tend to exclude patients (eg, language difficulties, elderly, frail) who are more inclined to have a reoperation of recurrence delayed or never done. Second, due to the organized follow-up in a RCT, the detection and consequent reoperation of a recurrence will be more expeditious. In a recent Dutch RCT on TEP, with an 83% follow-up after 5 years, the recurrence/reoperation ratio was 1.5:1.22 Accordingly, we presume the factual recurrence rate in our cohort to surpass the found reoperation rate by at least 50%, and probably to a significantly higher degree.
The objective of this study was not to pinpoint factual recurrence rates, but to define relative risk differences depending on the mesh and the fixation. It is then vital to understand that at any given time, the proportion of recurrences not (yet) operated were likely dependent on nonsurgical factors that were comparable in all our study groups. Hence, it is reasonable to assume the calculated HRs for reoperation to have been approximately the same as the factual HRs for recurrence.27 For example, if LWM/0 doubled the reoperation risk compared with StdPPM/0, this also implies a doubled recurrence risk.
Limitations
Like in any clinical study, our results should be considered general estimates and may not be applicable in every conceivable situation.
Limitations specific to this study are mainly related to inherent imperfections typical for large databases or attributable to SHR shortcomings.49 With an observational, nonrandomized study, one must always consider the risk of undetected confounding and bias.
The SHR does not register why the surgeon opted for a laparoscopic repair or chose a specific mesh/fixation combination. We have attempted to mitigate selection bias by adjusting for several potential effect modifiers and confounders and, in the final stage analysis, by either excluding small subgroups or merging them into larger ones.
The SHR query options are pragmatic compromises between scientific rigor and realistic requirements to obtain accurate registrations nationwide, including from surgeons with a limited interest in hernioplasty materials.
For instance, although the mesh size might affect the need for fixation, SHR does not record it. However, it is recommended and generally accepted among Swedish laparoscopic surgeons that the mesh must be at least 10 cm × 15 cm. The only meshes marketed in Sweden for laparoscopic repair that are indeed slightly smaller are a few models in the excluded three-dimensional mesh alternative.
Also, SHR lacks information about the anatomic sites for fixation, the number of tacks, and the amount of glue.
Furthermore, SHR does not record the extent of dissection or whether the surgeon at the carbon dioxide deflation checked for inadvertent displacement or folding of the mesh.
Although some details were not available, like those mentioned above, we still believe SHR contained the essential data necessary for the current study’s core purpose.
Absorbable tacks correlated with less favorable results than their metal counterparts did. This is puzzling but corroborates studies in vitro and on routine laparoscopic incisional hernia repair.63-65 Yet we refrain from far-reaching conclusions about absorbable tacks, for many reasons.
Because SHR bundles all absorbable tack models in 1 group, we cannot exclude the possibility of individual outcome differences depending on the heterogeneous tack designs.
Adequate multivariable regression demands large samples to minimize the risk of bias successfully. Unfortunately, by constituting a mere 428 (2%) repairs, the subgroup StdPPM/absorbable tacks barely fulfilled this prerequisite. Our attempts at stratified analysis revealed seemingly inconsistent trends, but with unsatisfactory low power not allowing statistical inference. We cannot rule out that the few repairs with StdPPM/absorbable tacks might have been subjected to residual confounding, eg, selection bias by being chosen unproportionally more often in high-risk cases or by less skilled surgeons.
No matter which fixation option in TEP and TAPP, including non-fixation, the same well-established principles apply: to reduce all potential hernias and prepare an adequately wide landing zone for the mesh, the dissection must achieve the so-called critical view of the myopectineal orifice.29,66 An insufficiently wide dissection may, eg, cause folding of the mesh, which is a well-known cause of recurrence and chronic postoperative pain.14
Regardless of the aforementioned caveats, a key finding was that in comparison with either StdPPM/0 or LWM/0, neither metal nor absorbable tacks were associated with significantly improved results. Nonetheless, our results are averages from a nationwide cohort and did not allow us to rule out the existence of individual clinical situations in which tacks might still be advisable.
The current study only implicitly addressed discomfort caused by implanted devices. An upcoming sequel in our project will focus on how the risk of chronic postoperative pain correlates with different mesh/fixation options.
CONCLUSIONS
Our results corroborate our initiating hypothesis. Separately investigating mesh or fixation is insufficient, and may to a certain extent even be misleading, also after adjusting for the other one in a multivariable model.
With no statistical difference, 4 of the 8 mesh/fixation combinations examined in our study were associated with the lowest reoperation risk after TEP and TAPP. Even without yet having analyzed the combinations’ influence on risk for chronic postoperative pain, we recommend the following: the most cost-effective alternative is StdPPM/0, because StdPPM is the least expensive mesh, and neither tacks nor glue seemed to significantly improve the StdPPM results. When a LWM is preferred, we recommend fixation with fibrin glue because this was the only LWM alternative associated with a reoperation risk on par with StdPPM/0.
The HerniaSurge guidelines are about to be revised. Our results fill some knowledge gaps in the first version and may therefore contribute to the upcoming update.
Author Contributions
Study conception and design: Novik
Acquisition of data: Novik
Analysis and interpretation of data: Novik, Sandblom, Ansorge, Thorell
Drafting of manuscript: Novik
Critical revision: Novik, Sandblom, Ansorge, Thorell
Obtaining funding: Novik, Ansorge
Supervision: Novik, Sandblom, Ansorge, Thorell
Investigation: Novik, Sandblom, Ansorge, Thorell
Methodology: Novik, Sandblom, Ansorge, Thorell
Project administration: Novik, Sandblom, Ansorge, Thorell
Resources: Novik, Sandblom, Ansorge, Thorell
Software: Novik, Ansorge
Validation: Novik, Sandblom, Ansorge, Thorell
Visualization: Novik
Acknowledgment:
The raw study database was retrieved, prepared, and delivered by the SHR chief statistician Henrik Holmberg, Oncological Center, Norrland University Hospital, Sweden. Statisticians Nicklas Pihlström and Bei Yang at the Centre for Clinical Research Sörmland, Eskilstuna, Sweden, and Fredrik Johansson, Department of Clinical Sciences, Karolinska Institutet, Danderyd Hospital, Stockholm, Sweden, contributed with indispensable SPSS consulting and statistics discussions. At the initial phase of the study in 2011 to 2012, the now former statistician at SHR, Benjamin Häggqvist, provided a preliminary database on which he made the statistical analyses. We thank Susan Hull Grasso, MSE, Biden School of Public Policy and Administration, University of Delaware, for English language review. Associate Professor Bo Povlsen MD, PhD, Emeritus Consultant Orthopedic Surgeon, Guy’s & St Thomas’ Hospitals NHS Trust, London, UK, contributed with inspirational discussions.
Abbreviations and Acronyms
- EHS =
- European Hernia Society
- HR =
- hazard ratio
- LWM =
- lightweight mesh (pure or composite polypropylene)
- LWM/0 =
- lightweight mesh without fixation
- LWPPM =
- lightweight pure polypropylene mesh
- RCT =
- randomized controlled trial
- SHR =
- Swedish Hernia Registry
- StdPPM =
- standard pure polypropylene mesh
- StdPPM/0 =
- standard pure polypropylene mesh without fixation
- TAPP =
- (laparoscopic) transabdominal preperitoneal mesh repair
- TEP =
- (laparoscopic) totally extraperitoneal mesh repair
CME questions for this article available at http://jacscme.facs.org
Disclosure Information: Authors have nothing to disclose. Timothy J Eberlein, Editor-in-Chief, has nothing to disclose. Ronald J Weigel, CME Editor, has nothing to disclose.
Support: The project was principally funded by The Centre for Clinical Research Sörmland, Uppsala University, Eskilstuna, and in an early phase by The Western Region Research Council and The Skaraborg Hospital Research and Development Center. It was also supported by The Swedish Hernia Registry.
Disclaimer: All funders/supporters are public, tax-financed, non-profit Swedish institutions. They had no role in the design, analysis, or interpretation of the data; or writing of the manuscript. No commercial company or any other competing interest was affiliated with this study in any way. None of the authors has had any conflict of interest related to this study.
Presented at the 8th European Hernia Society and Americas Hernia Society Joint Congress, Copenhagen, Denmark, October 2021.
REFERENCES
- 1.EU Hernia Trialists Collaboration. Repair of groin hernia with synthetic mesh: meta-analysis of randomized controlled trials. Ann Surg. 2002;235:322–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bisgaard T, Bay-Nielsen M, Christensen IJ, et al. Risk of recurrence 5 years or more after primary Lichtenstein mesh and sutured inguinal hernia repair. Br J Surg. 2007;94:1038–1040. [DOI] [PubMed] [Google Scholar]
- 3.HerniaSurge Group. International guidelines for groin hernia management. Hernia. 2018;22:1–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murphy BL, Ubl DS, Zhang J, et al. Trends of inguinal hernia repairs performed for recurrence in the United States. Surgery. 2018;163:343–350. [DOI] [PubMed] [Google Scholar]
- 5.Murphy BL, Zhang J, Ubl DS, et al. Surgical trends of groin hernia repairs performed for recurrence in Medicare patients. Hernia. 2019;23:677–683. [DOI] [PubMed] [Google Scholar]
- 6.Swedish Hernia Registry. Annual report 2019 [in Swedish] 2020. Available at: http://www.svensktbrackregister.se/images/reviderad_%C3%A5rsber%C3%A4ttelsen_2019.pdf. Accessed December 25, 2021.
- 7.Palser TR, Swift S, Williams RN, et al. Variation in outcomes and use of laparoscopy in elective inguinal hernia repair. BJS Open. 2019;3:466–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dulucq J. Traitement des hernies de l’aine par mise en place d’un patch prothétique sous-péritonéal en rétro-péritonéoscopie. Cahiers de Chirurgie. 1991;79:15–16. [PubMed] [Google Scholar]
- 9.Arregui ME, Davis CJ, Yucel O, et al. Laparoscopic mesh repair of inguinal hernia using a preperitoneal approach: a preliminary report. Surg Laparosc Endosc. 1992;2:53–58. [PubMed] [Google Scholar]
- 10.Köckerling F, Bittner R, Kuthe A, et al. TEP or TAPP for recurrent inguinal hernia repair-register-based comparison of the outcome. Surg Endosc. 2017;31:3872–3882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aiolfi A, Cavalli M, Ferraro SD, et al. Treatment of inguinal hernia: systematic review and updated network meta-analysis of randomized controlled trials. Ann Surg. 2021;274:954–961. [DOI] [PubMed] [Google Scholar]
- 12.Lowham AS, Filipi CJ, Fitzgibbons RJ, Jr, et al. Mechanisms of hernia recurrence after preperitoneal mesh repair. Traditional and laparoscopic. Ann Surg. 1997;225:422–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferzli GS, Frezza EE, Pecoraro AM, Jr, et al. Prospective randomized study of stapled versus unstapled mesh in a laparoscopic preperitoneal inguinal hernia repair. J Am Coll Surg. 1999;188:461–465. [DOI] [PubMed] [Google Scholar]
- 14.Wantz GE. Laparoscopic hernioplasty without staples. J Am Coll Surg. 1999;188:531. [DOI] [PubMed] [Google Scholar]
- 15.Moreno-Egea A, Torralba Martínez JA, Morales Cuenca G, et al. Randomized clinical trial of fixation vs nonfixation of mesh in total extraperitoneal inguinal hernioplasty. Arch Surg. 2004;139:1376–1379. [DOI] [PubMed] [Google Scholar]
- 16.Novik B. Randomized trial of fixation vs nonfixation of mesh in total extraperitoneal inguinal hernioplasty. Arch Surg. 2005;140:811–812; author reply 812. [DOI] [PubMed] [Google Scholar]
- 17.Sahebally SM, Horan J, Rogers AC, et al. Fixation versus no fixation in laparoscopic totally extraperitoneal repair of primary inguinal hernia-a systematic review and meta-analysis of randomized controlled trials. Langenbecks Arch Surg. 2020;405:435–443. [DOI] [PubMed] [Google Scholar]
- 18.Habib Bedwani NAR, Kelada M, Smart N, et al. Glue versus mechanical mesh fixation in laparoscopic inguinal hernia repair: meta-analysis and trial sequential analysis of randomized clinical trials. Br J Surg. 2021;108:14–23. [DOI] [PubMed] [Google Scholar]
- 19.Klinge U, Klosterhalfen B, Conze J, et al. Modified mesh for hernia repair that is adapted to the physiology of the abdominal wall. Eur J Surg. 1998;164:951–960. [DOI] [PubMed] [Google Scholar]
- 20.Novik B, Hagedorn S, Mörk UB, et al. Fibrin glue for securing the mesh in laparoscopic totally extraperitoneal inguinal hernia repair: a study with a 40-month prospective follow-up period. Surg Endosc. 2006;20:462–467. [DOI] [PubMed] [Google Scholar]
- 21.van Veenendaal N, Simons M, Hope W, et al. ; HerniaSurge Group. Consensus on international guidelines for management of groin hernias. Surg Endosc. 2020;34:2359–2377. [DOI] [PubMed] [Google Scholar]
- 22.Roos MM, Bakker WJ, Schouten N, et al. Higher recurrence rate after endoscopic totally extraperitoneal (TEP) inguinal hernia repair with Ultrapro lightweight mesh: 5-year results of a randomized controlled trial (TULP-trial). Ann Surg. 2018;268:241–246. [DOI] [PubMed] [Google Scholar]
- 23.Wu F, Zhang X, Liu Y, et al. Lightweight mesh versus heavyweight mesh for laparo-endoscopic inguinal hernia repair: a systematic review and meta-analysis. Hernia. 2020;24:31–39. [DOI] [PubMed] [Google Scholar]
- 24.Bakker WJ, Aufenacker TJ, Boschman JS, et al. Heavyweight mesh is superior to lightweight mesh in laparo-endoscopic inguinal hernia repair: a meta-analysis and trial sequential analysis of randomized controlled trials. Ann Surg. 2021;273:890–899. [DOI] [PubMed] [Google Scholar]
- 25.von Elm E, Altman DG, Egger M, et al. ; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–1457. [DOI] [PubMed] [Google Scholar]
- 26.Benchimol EI, Smeeth L, Guttmann A, et al. ; RECORD Working Committee. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12:e1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Novik B, Nordin P, Skullman S, et al. More recurrences after hernia mesh fixation with short-term absorbable sutures: a registry study of 82 015 Lichtenstein repairs. Arch Surg. 2011;146:12–17. [DOI] [PubMed] [Google Scholar]
- 28.Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, et al. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol. 2009;24:659–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Claus C, Furtado M, Malcher F, et al. Ten golden rules for a safe MIS inguinal hernia repair using a new anatomical concept as a guide. Surg Endosc. 2020;34:1458–1464. [DOI] [PubMed] [Google Scholar]
- 30.Novik B. Defining recurrence from the patient’s point of view (reply to comment) [JAMA Network web site]; c2011. Available at: https://jamanetwork.com/journals/jamasurgery/fullarticle/406587. Accessed October 24, 2021.
- 31.Weyhe D, Schmitz I, Belyaev O, et al. Experimental comparison of monofile light and heavy polypropylene meshes: less weight does not mean less biological response. World J Surg. 2006;30:1586–1591. [DOI] [PubMed] [Google Scholar]
- 32.Chastan P. Tension free open inguinal hernia repair using an innovative self gripping semi-resorbable mesh. J Minim Access Surg. 2006;2:139–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kibbe MR. Reporting of sex as a variable in research published in surgical journals. JAMA Surg. 2018;153:983. [DOI] [PubMed] [Google Scholar]
- 34.Flanagin A, Frey T, Christiansen SL; AMA Manual of Style Committee. Updated guidance on the reporting of race and ethnicity in medical and science journals. JAMA. 2021;326:621–627. [DOI] [PubMed] [Google Scholar]
- 35.Miserez M, Alexandre JH, Campanelli G, et al. The European hernia society groin hernia classification: simple and easy to remember. Hernia. 2007;11:113–116. [DOI] [PubMed] [Google Scholar]
- 36.Aquina CT, Fleming FJ, Becerra AZ, et al. Explaining variation in ventral and inguinal hernia repair outcomes: a population-based analysis. Surgery. 2017;162:628–639. [DOI] [PubMed] [Google Scholar]
- 37.Stulberg JJ, Huang R, Kreutzer L, et al. Association between surgeon technical skills and patient outcomes. JAMA Surg. 2020;155:960–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Andresen K, Friis-Andersen H, Rosenberg J. Laparoscopic repair of primary inguinal hernia performed in public hospitals or low-volume centers have increased risk of reoperation for recurrence. Surg Innov. 2016;23:142–147. [DOI] [PubMed] [Google Scholar]
- 39.Maneck M, Köckerling F, Fahlenbrach C, et al. Hospital volume and outcome in inguinal hernia repair: analysis of routine data of 133,449 patients. Hernia. 2020;24:747–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.IBM. Test of Proportional Hazards [IBM SPSS Statistics V23.0 documentation web site]. Available at: https://www.ibm.com/docs/en/spss-statistics/23.0.0?topic=regression-test-proportional-hazards. Accessed August 16, 2021.
- 41.Lillemoe KD. Joint statement by the Surgery Journal Editors Group 2018. Ann Surg. 2018;267:991. [DOI] [PubMed] [Google Scholar]
- 42.Mayer F, Niebuhr H, Lechner M, et al. When is mesh fixation in TAPP-repair of primary inguinal hernia repair necessary? The register-based analysis of 11,230 cases. Surg Endosc. 2016;30:4363–4371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Köckerling F, Hantel E, Adolf D, et al. Differences in the outcomes of scrotal vs. lateral vs. medial inguinal hernias: a multivariable analysis of registry data. Hernia. 2021;25:1169–1181. [DOI] [PubMed] [Google Scholar]
- 44.Burcharth J, Pommergaard HC, Bisgaard T, et al. Patient-related risk factors for recurrence after inguinal hernia repair: a systematic review and meta-analysis of observational studies. Surg Innov. 2015;22:303–317. [DOI] [PubMed] [Google Scholar]
- 45.Zinther NB, Wara P, Friis-Andersen H. Intraperitoneal onlay mesh: an experimental study of adhesion formation in a sheep model. Hernia. 2010;14:283–289. [DOI] [PubMed] [Google Scholar]
- 46.Harsløf S, Zinther N, Harsløf T, et al. Mesh shrinkage depends on mesh properties and anchoring device: an experimental long-term study in sheep. Hernia. 2017;21:107–113. [DOI] [PubMed] [Google Scholar]
- 47.Klinge U, Koch A, Weyhe D, et al. Bias-variation dilemma challenges clinical trials: inherent limitations of randomized controlled trials and meta-analyses comparing hernia therapies. Int J Clin Pract. 2014; 5:778–789. [Google Scholar]
- 48.Nolsøe A, Andresen K, Rosenberg J. Repair of recurrent hernia is often performed at a different clinic. Hernia. 2016;20:783–787. [DOI] [PubMed] [Google Scholar]
- 49.Schwab R, Dietz UA, Menzel S, et al. Pitfalls in interpretation of large registry data on hernia repair. Hernia. 2018;22:947–950. [DOI] [PubMed] [Google Scholar]
- 50.Haapaniemi S, Nilsson E. Recurrence and pain three years after groin hernia repair. Validation of postal questionnaire and selective physical examination as a method of follow-up. Eur J Surg. 2002;168:22–28. [DOI] [PubMed] [Google Scholar]
- 51.LeBlanc KA. Tack hernia: a new entity. JSLS. 2003;7:383–387. [PMC free article] [PubMed] [Google Scholar]
- 52.Lerdsirisopon S, Frisella MM, Matthews BD, et al. Biomechanical evaluation of potential damage to hernia repair materials due to fixation with helical titanium tacks. Surg Endosc. 2011;25:3890–3897. [DOI] [PubMed] [Google Scholar]
- 53.Poobalan AS, Bruce J, Smith WC, et al. A review of chronic pain after inguinal herniorrhaphy. Clin J Pain. 2003;19:48–54. [DOI] [PubMed] [Google Scholar]
- 54.Vigneswaran Y, Linn JG, Gitelis M, et al. Educating surgeons may allow for reduced intraoperative costs for inguinal herniorrhaphy. J Am Coll Surg. 2015;220:1107–1112. [DOI] [PubMed] [Google Scholar]
- 55.Staarink M, van Veen RN, Hop WC, et al. A 10-year follow-up study on endoscopic total extraperitoneal repair of primary and recurrent inguinal hernia. Surg Endosc. 2008;22:1803–1806. [DOI] [PubMed] [Google Scholar]
- 56.Brandt-Kerkhof A, van Mierlo M, Schep N, et al. Follow-up period of 13 years after endoscopic total extraperitoneal repair of inguinal hernias: a cohort study. Surg Endosc. 2011;25:1624–1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Peitsch WK. A modified laparoscopic hernioplasty (TAPP) is the standard procedure for inguinal and femoral hernias: a retrospective 17-year analysis with 1,123 hernia repairs. Surg Endosc. 2014;28:671–682. [DOI] [PubMed] [Google Scholar]
- 58.Barbaro A, Kanhere H, Bessell J, et al. Laparoscopic extraperitoneal repair versus open inguinal hernia repair: 20-year follow-up of a randomized controlled trial. Hernia. 2017;21:723–727. [DOI] [PubMed] [Google Scholar]
- 59.Roos MM, van Hessen CV, Verleisdonk EJMM, et al. An 11-year analysis of reoperated groins after endoscopic totally extraperitoneal (TEP) inguinal hernia repair in a high volume hernia center. Hernia. 2019;23:655–662. [DOI] [PubMed] [Google Scholar]
- 60.Köckerling F, Koch A, Lorenz R, et al. How long do we need to follow-up our hernia patients to find the real recurrence rate? Front Surg. 2015;2:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370:1508–1519. [DOI] [PubMed] [Google Scholar]
- 62.Helgstrand F, Rosenberg J, Kehlet H, et al. Reoperation versus clinical recurrence rate after ventral hernia repair. Ann Surg. 2012;256:955–958. [DOI] [PubMed] [Google Scholar]
- 63.Sadava EE, Krpata DM, Gao Y, et al. Laparoscopic mechanical fixation devices: does firing angle matter? Surg Endosc. 2013;27:2076–2081. [DOI] [PubMed] [Google Scholar]
- 64.Zihni AM, Cavallo JA, Thompson DM, Jr, et al. Evaluation of absorbable mesh fixation devices at various deployment angles. Surg Endosc. 2015;29:1605–1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Christoffersen MW, Brandt E, Helgstrand F, et al. Recurrence rate after absorbable tack fixation of mesh in laparoscopic incisional hernia repair. Br J Surg. 2015;102:541–547. [DOI] [PubMed] [Google Scholar]
- 66.Daes J, Felix E. Critical view of the myopectineal orifice. Ann Surg. 2017;266:e1–e2. [DOI] [PubMed] [Google Scholar]