Abstract
Polypharmacy is a challenging issue in geriatrics. The aim of the study was to characterize correlates of polypharmacy in the PolSenior project. The PolSenior project, was a comprehensive survey in a large and longitudinal representative sample of thePolish older population. The project was conducted by the International Institute of Molecular and Cell Biology in Warsaw between 2008 and 2011. All medications consumed during the week preceding the survey were evaluated for each participant (n = 4793, including 2314 females (48.3%)). Thereafter, the percentage of those with polypharmacy (at least 5 medications) and excessive polypharmacy (at least 10 medications) was calculated, and their correlates were determined. The average number of medications used by participants was 5.1 ± 3.6, and was higher in females than in males (5.5 ± 3.5 vs. 4.8 ± 3.5; p < 0.001). Polypharmacy characterized 2650 participants (55.3%) and excessive polypharmacy—532 of them (11.1%). The independent correlates associated withpolypharmacy were: age over 70 years, female sex, higher than primary education, living in an urban area, comorbidities, any hospitalization during past five years, and visiting general practicioners at least yearly. As for correlates with excessive polypharmacy, they were: age 80–84 years, female sex, living in an urban area, diagnosis of at least four chronic diseases, and at least two hospitalizations in the last five years. This study serves as a starting place to understand patient characteristics associated with polypharmacy, excessive polypharmacy, and identify targeted interventions.
Keywords: PolSenior, polypharmacy, excessive polypharmacy, older adults, correlates
1. Introduction
Multimorbidity is highly prevalent in older adults [1] and is typically accompanied by multiple drug regimens, described as polypharmacy. As there are various definitions of polypharmacy (reviewed by Fulton et al. [2]), it is challenging to compare its prevalence. In a nationally representative sample of Korean older patients [3], polypharmacy was defined as the concurrent use of six or more medications, and was present in as many as 86.4% of studied subjects. Notably, the prevalence was almost half as common (44%) in a registry-based prospective cohort study from Sweden, even though polypharmacy was defined as concurrent use of five or more medications (versus six in the Korean study) [4]. Despite these differences, the prevalence of polypharmacy generally increases over time. Jyrkka et al. [5] reported that in Finland, between 1998 and 2003, in a cohort of older adults, polypharmacy prevalence (>5 medicines in use) increased from 54% to 67%, and excessive polypharmacy (≥10 medications in use) increased from 19% to 28%. In more recent times, Swedish nationwide registry-based study by Zhang et al. [6] reported that the prevalence of polypharmacy (≥5 medications) and excessive polypharmacy (≥10 medicines in use) significantly increased between 2006 and 2014. The authors of this study stated that the prevalence of polypharmacy and excessive polypharmacy increased radically with age and peaked up to 79.6% and 36.4% in individuals aged 90 and above, respectively. These upward trends in polypharmacy may have many unpredictable effects [7]. One trend for certain is that polypharmacy is related to adverse clinical outcomes [8]. It was also shown that medication adherence is negatively associated with greater number of mediactions [9]. Several previous studies have reported that polypharmacy was associated with increased incidence of adverse drug reactions, drug–drug interactions, and inappropriateness of pharmacological treatment [10,11,12]. Moreover, polypharmacy is linked to poorer health status as it increases the risk of geriatric syndromes such as falls [13], malnutrition [14], urinary incontinence [15], and depression [16]. Additionally, it has been established that inappropriately prescribed polypharmacy leads to functional impairment and increases mortality risk [17,18]. Consequently, polypharmacy contributes to an increase in both direct and indirect costs of medical care [19]. Furthermore, polypharmacy regimens constitute a well-known risk factor of non-adherence [9]. According to Pasina et al. [20], an increased number of medications at hospital discharge strongly correlates to non-adherence, which averages to as much as 69.6% among community-dwelling older subjects three months after discharge.
To address the challenges resulting from polypharmacy and its adverse outcomes, frameworks for various interventions are proposed. According to the Canadian Agency for Drugs and Technologies in Health (CADTH), several types of interventions directed at different health system stakeholders can reduce the polypharmacy burden among older individuals [21]. They include those targeting health professionals, drug consumers, as well as organizational, financial, and regulatory interventions, which aim to change the delivery of health services. All of these interventions require continuous actions aimed at identifying and solving medication-related problems to decrease the risk of polypharmacy and increase the efficacy and safety of treatment [22].
Fifteen years ago, Zarowitz et al. demonstrated the positive effect of a teamwork intervention, including a physician, a pharmacist, and the patient, on the reduction in polypharmacy in community-dwelling older subjects [23]. Currently, there is also a large body of evidence on the effectiveness of various interventions in reducing the risks associated with polypharmacy. The studies by Cooper et al. [24] and Olaniyan et al. [25] showed that both professional, organizational, and multifaceted interventions resulted in the reduction in potentially inappropriate prescriptions and the improvement of adherence, appropriateness, and safety of medications.
Given that polypharmacy is associated with adverse health outcomes and can be reduced by applying different methods of medication revision, it is vital to define the subjects who are likely to benefit most from such interventions and find the predictors of polypharmacy. Thus, the aim of the study was to investigate the prevalence of polypharmacy in older individuals in Poland and to delineate the predictors of polypharmacy within a nationwide representative study group. A similar comprehensive population-based study has not been published to date to the best of our knowledge.
2. Materials and Methods
PolSenior was a nationwide multidisciplinary project conducted by International Institute of Molecular and Cell Biology in Warsaw between 2008 and 2011 on a group representative of the Polish population of older adults to assess medical, psychological, social, and economic aspects of aging in Poland. Therefore, the aim of the project was to define the status of study participants and identify their social and medical needs. The outcomes were expected to facilitate the establishment of proper care for the growing population of older individuals [26].
There were 4979 older people included in the project (2412 women and 2567 men) aged 65 years and older. A detailed description of the study design has been published and can be found at https://doi.org/10.1016/j.exger.2011.09.006 (accessed on 1 December 2021) [26].
Analysis of pharmacotherapy was performed among 4793 participants (including 2314 women—48.3% of the total, and 2479 men). In 186 participants (3.7% of the total study group), analysis of pharmacotherapy was not possible due to a lack of information on participants’ medication regimens.
For each of the studied participants, the evaluation of all pharmaceutical preparations (including dietary supplements, complementary/alternative medicines, and herbal remedies), referred to as “medications,” consumed during the week preceding the survey was performed. The interviewer wrote down the name, the formulation (e.g., tablets, capsules, drops), the single dose, and the frequency of dosage of each medication that was taken more than once a week. Information on pharmacotherapy was obtained directly from the respondent or their family/caregivers, who were also asked to provide a “brown bag” containing all consumed pharmaceutical preparations to the interviewer.
Each medicine taken by the respondent was coded according to the alphanumeric Anatomical Therapeutic Chemical (ATC) classification system. Quantitative analysis of the medication involved the calculation of the average number of all medications (both prescribed, Rx and over-the-counter, OTC) consumed by the studied subjects. The percentages of respondents (by gender) not taking any medication and of those receiving five or more and ten or more medications in the last week were calculated.
The only morbidities (disease states) included in the analysis were cardiovascular diseases (including hypertension, coronary heart disease, myocardial infarction, and stroke), respiratory, digestive, endocrine, and metabolic diseases (including diabetes mellitus), blood diseases (anemia), kidney diseases, osteoporosis, and eye diseases.
To delineate the non-biomedical health predictors of polypharmacy, the following variables were taken into account: age, sex, marital status (unmarried/married or in a relationship), education (less than primary, primary, vocational, at least secondary), place of residence (city/rural area), living conditions (alone/with others/in an institution), number of diseases (0/1–3, or at least 4), number of hospitalizations during the last 5 years (0/1 or 2 or more than 2), frequency of general practicioners consultations (less than once a year/several times a year/at least once a month), and self-reported poverty (YES—if they could not afford to buy even the most inexpensive food and clothing).
Statistical Analysis
The statistical analysis was performed with STATISTICA 13.0 software by TIBCO Software (Palo Alto, CA, USA). For the analyzed variables, mean values and standard deviations were calculated. Normality in the distribution of variables was assessed with the Shapiro–Wilk test. Comparison between two unpaired groups was made with the Mann–Whitney test and the Kruskal–Wallis test for more than two groups. In the case of significant differences between studied variables detected by the Kruskal–Wallis test, a post hoc Dunn test was performed. Statistical significance of differences in the distribution of quality variables between two or more groups was analyzed with the χ2 test.
To assess simultaneous interdependence between many variables, a multiple regression model (logistic regression) was used, specifying the odds ratio and the confidence interval with the confidence limit of 95%. All variables that were significant for polypharmacy and excessive polypharmacy in the univariable analysis were included in multiple linear regression analysis. p < 0.05 was considered statistically significant.
The Polsenior project sample was intended to include balance in the total numbers of participants as well as balanced numbers of men and women in all age cohorts, which allowed for precise assessment of studied factors in the oldest groups. However, it caused an overestimation of older groups and men in terms of the population structure. Consequently, in order to make the sample representative of the Polish population and obtain results reflecting the distribution of studied characteristics in the entire population of older people in Poland, post-stratification was necessary.
3. Results
Of the 4793 respondents with a mean age of 79.3 ± 8.7 years, 2314 were women (48.3%). There was no difference in age between gender groups, of females and males (79.2 ± 8.9 and 79.4 ± 8.5, respectively). However, studied females had lower education than males (p < 0.0001), more often lived alone (p < 0.0001) and reported poverty less common than males (p < 0.0001). Table 1 shows detailed characteristics of the studied group, including gender.
Table 1.
The characteristics of study participants including sex (base rate: % of line).
| Sex | ||||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Males | Females | ||||||
| n | % | n | % | n | % | p | ||
| Age (years) | 65–69 | 772 | 15.8% | 372 | 48.2% | 400 | 51.8% | |
| 70–74 | 908 | 18.6% | 474 | 52.2% | 434 | 47.8% | ||
| 75–79 | 827 | 17.0% | 434 | 52.5% | 393 | 47.5% | ||
| 80–84 | 774 | 15.9% | 412 | 53.2% | 362 | 46.8% | 0.1040 | |
| 85–89 | 846 | 17.4% | 460 | 54.4% | 386 | 45.6% | ||
| at least 90 | 746 | 15.3% | 367 | 49.2% | 379 | 50.8% | ||
| Marital status | Unmarried | 2324 | 49.4% | 737 | 31.0% | 1643 | 69.0% | <0.0001 |
| Married | 2380 | 50.6% | 1699 | 73.1% | 625 | 26.9% | ||
| Education | Less than primary | 653 | 13.9% | 262 | 40.1% | 391 | 59.9% | |
| Primary | 2080 | 44.2% | 955 | 45.9% | 1125 | 54.1% | <0.0001 | |
| Vocational | 906 | 19.2% | 488 | 53.9% | 418 | 46.1% | ||
| At least secondary | 1069 | 22.7% | 735 | 68.8% | 334 | 31.2% | ||
| Place of residence | Urban area | 2933 | 60.2% | 1547 | 52.7% | 1386 | 47.3% | 0.0756 |
| Rural area | 1940 | 39.8% | 972 | 50.1% | 968 | 49.9% | ||
| Living conditions | Alone | 1008 | 21.4% | 354 | 35.1% | 654 | 64.9% | |
| With others | 3660 | 77.6% | 2063 | 56.4% | 1597 | 43.6% | <0.0001 | |
| In institutions | 46 | 1.0% | 24 | 52.2% | 22 | 47.8% | ||
| Number of diseases | 0 | 416 | 10.6% | 272 | 65.4% | 144 | 34.6% | |
| 1–3 | 2853 | 73.0% | 1496 | 52.4% | 1357 | 47.6% | <0.0001 | |
| 4 or more | 639 | 16.4% | 291 | 45.5% | 348 | 54.5% | ||
| Number of hospitalizations during past 5 years | 0 | 2087 | 45.7% | 1028 | 49.3% | 1059 | 50.7% | |
| 1 | 1111 | 24.4% | 596 | 53.7% | 515 | 46.4% | 0.0033 | |
| 2 or more | 1366 | 29.9% | 747 | 54.7% | 619 | 45.3% | ||
| Frequency of GP consultation | Less than once a year | 736 | 16.3% | 429 | 58.3% | 307 | 41.7% | |
| Several times a year | 1470 | 32.4% | 735 | 50.0% | 735 | 50.0% | 0.0003 | |
| At least ones a month | 2327 | 51.3% | 1171 | 50.3% | 1156 | 49.7% | ||
| Self-reported poverty | NO | 3747 | 88.4% | 2026 | 54.1% | 1721 | 45.9% | <0.0001 |
| YES | 490 | 11.6% | 201 | 41.0% | 289 | 59.0% | ||
Note: The numbers in the table may not add up to the total number of participants in the survey, as not all participants answered all the survey questions.
The mean number of comorbidities was 2.1 ± 1.6, and the mean number of hospitalizations—1.3 ± 2.0. The number of comorbidities was higher in females (2.3 ± 1.7 vs. 2.0 ± 1.5; p < 0.001), whereas the number of hospitalization was higher in in males (1.3 ± 2.0 vs. 1.2 ± 2.0; p < 0.01). The mean number of medications used by studied respondents was 5.1 ± 3.6. Females took more medications than males (5.5 ± 3.5 vs. 4.8 ± 3.5; p < 0.001).
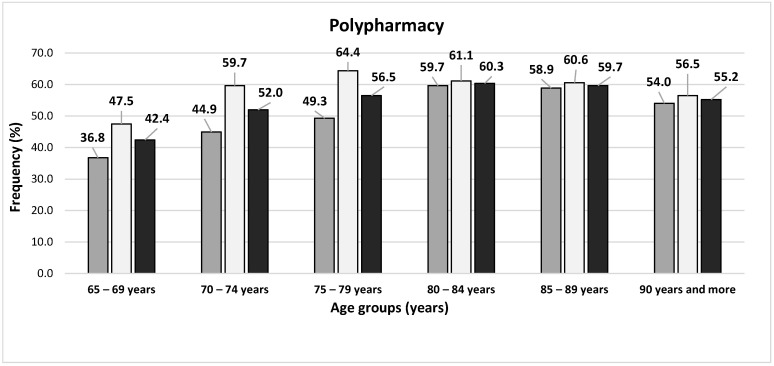
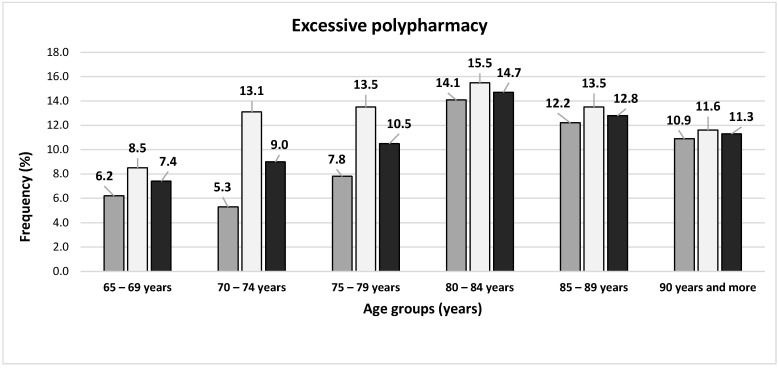
Among studied subjects, 507 (10.4%) did not take any medication, and more common inmales than females (331; 13.1% vs. 176; 7.4%, p < 0.0001). At least five medications were taken regularly by 2650 subjects (54.4%) and at least 10—by 532 (10.9%). Both polypharmacy and excessive polypharmacy were more common in females than males (58.2% vs. 50.8%, p < 0.0001 and 12.6% vs. 9.4%, p = 0.0003, respectively). Figure 1 presents the frequency of polypharmacy and excessive polypharmacy in age cohorts, including gender.
Figure 1.
The prevalence of polypharmacy and excessive polypharmacy in this study sample of the Polish older adult population, including gender: dark grey bars represent males, light grey bars—females, and black bars—the whole studied population.
The Participant Characteristics with Excessive Polypharmacy
In univariable analysis, the impact of single variables on the incidence of excessive polypharmacy among those with polypharmacy is presented in Table 2. The rate of excessive polypharmacy was the highest among subjects aged 80–84 (24.4%) and the lowest in the two youngest cohorts (60–64 years and 65–69 years: 17.4%). Subjects living in urban areas had excessive polypharmacy more often than those living in rural areas (p < 0.0001).
Table 2.
Study participant characteristics and prevalence of polypharmacy and excessive polypharmacy, in this sample of the Polish older adult population.
| Variable | Number of Medications | Number of Medications | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1–4 | 5+ | p | 5–9 | 10+ | p | ||||||
| Age (years) | 65–69 | 330: | 50.2% | 327: | 49.8% | <0.0001 | 270: | 82.6% | 57: | 17.4% | 0.0693 |
| 70–74 | 331: | 41.2% | 472: | 58.8% | 390: | 82.6% | 82: | 17.4% | |||
| 75–79 | 287: | 38.1% | 467: | 61.9% | 380: | 81.4% | 87: | 18.6% | |||
| 80–84 | 244: | 34.3% | 467: | 65.7% | 353: | 75.6% | 114: | 24.4% | |||
| 85–89 | 269: | 34.8% | 505: | 65.2% | 397: | 78.6% | 108: | 21.4% | |||
| At least 90 | 255: | 38.2% | 412: | 61.8% | 328: | 79.6% | 84: | 20.4% | |||
| Marital status | Married | 861: | 42.0% | 1190: | 58.0% | 0.0010 | 1075: | 80.8% | 289: | 19.2% | 0.2213 |
| Unmarried | 801: | 37.0% | 1364: | 63.0% | 962: | 78.8% | 228: | 21.2% | |||
| Education | Less than primary | 228: | 40.7% | 332: | 59.3% | 0.0003 | 257: | 82.8% | 57: | 17.2% | 0.0574 |
| Primary | 781: | 42.1% | 1073: | 57.9% | 866: | 80.7% | 207: | 19.3% | |||
| Vocational | 281: | 33.4% | 561: | 66.6% | 424: | 75.6% | 137: | 24.4% | |||
| At least secondary | 374: | 38.8% | 591: | 61.2% | 474: | 80.2% | 117: | 19.8% | |||
| Place of residence | Urban area | 964: | 35.8% | 1728: | 64.2% | <0.0001 | 1336: | 77.3% | 392: | 22.7% | <0.0001 |
| Rural area | 752: | 44.9% | 922: | 55.1% | 782: | 84.8% | 140: | 15.2% | |||
| Living conditions | Alone | 321: | 34.8% | 602: | 65.2% | 0.0050 | 479: | 79.6% | 123: | 20.4% | 0.1805 |
| With others | 1326: | 40.7% | 1932: | 59.3% | 1546: | 80.0% | 386: | 20.0% | |||
| In istitutions | 18: | 40.9% | 26: | 59.1% | 17: | 65.4% | 9: | 34.6% | |||
| Number of diseases | 0 | 197: | 69.1% | 88: | 30.9% | <0.0001 | 79: | 89.8% | 9: | 10.2% | <0.0001 |
| 1–3 | 1124: | 43.6% | 1455: | 56.4% | 1203: | 82.7% | 252: | 17.3% | |||
| 4+ or more | 111: | 17.7% | 517: | 82.3% | 367: | 71.0% | 150: | 29.0% | |||
| Number of hospitalizations during past 5 years | 0 | 912: | 52.5% | 826: | 47.5% | <0.0001 | 693: | 83.9% | 133: | 16.1% | <0.0001 |
| 1 | 403: | 39.2% | 625: | 60.8% | 517: | 82.7% | 108: | 17.3% | |||
| 2 or more | 300: | 22.7% | 1022: | 77.3% | 761: | 74.5% | 261: | 25.5% | |||
| Frequency of general practioners’ consultation | Less than once a year | 305: | 62.4% | 184: | 37.6% | <0.0001 | 156: | 84.8% | 28: | 15.2% | p = 0.1672 |
| Several times a year | 591: | 43.4% | 770: | 56.6% | 617: | 80.1% | 153: | 19.9% | |||
| At least once a month | 697: | 31.0% | 1553: | 69.0% | 1226: | 78.9% | 327: | 21.1% | |||
| Self-reported poverty | NO | 1327: | 39.4% | 2037: | 60.6% | 0.6314 | 1626: | 79.8% | 411: | 20.2% | p = 0.6960 |
| YES | 167: | 38.1% | 271: | 61.9% | 213: | 78.6% | 58: | 21.4% | |||
Note: The numbers in the table may not add up to the total number of participants in the survey, as not all participants answered all the survey questions.
As far as biomedical health-related characteristics associated with polypharmacy are concerned, subjects with at least four chronic diseases consumed at least ten medications more frequently, compared with those with no chronic diseases (p < 0.001, Table 3). Moreover, excessive polypharmacy was more common in those who were hospitalized at least twice in the last five years in comparison with the subjects not hospitalized at all (p < 0.001).
Table 3.
Multi regression analysis of polypharmacy correlates in this sample of the Polish older adult population.
| Number of Medications: 1–4 vs. 5+ | ||||
|---|---|---|---|---|
| Variable | OR | 95% CI | p | |
| Sex | Males | - | - | - |
| Females | 1.35 | 1.14–1.62 | 0.001 | |
| Age (years) | 65–69 | - | - | - |
| 70–74 | 1.48 | 1.15–1.91 | 0.002 | |
| 75–79 | 1.58 | 1.22–2.06 | 0.001 | |
| 80–84 | 2.01 | 1.52–2.66 | <0.001 | |
| 85–89 | 2.34 | 1.76–3.10 | <0.001 | |
| At least 90 | 2.12 | 1.62–2.98 | <0.001 | |
| Marital status | Married | - | - | - |
| Unmarried | 0.91 | 0.74–1.12 | 0.37 | |
| Education | Less than primary | 0.96 | 0.74–1.23 | 0.729 |
| Primary | - | - | - | |
| Vocational | 1.43 | 1.15–1.79 | 0.001 | |
| At least secondary | 1.32 | 1.07–1.63 | 0.010 | |
| Place of residence | City | 1.30 | 1.09–1.54 | 0.003 |
| Rural area | - | - | - | |
| Living conditions | Alone | 1.20 | 0.95–1.50 | 0.121 |
| With others | - | - | - | |
| In istitutions | 1.11 | 0.45–2.71 | 0.826 | |
| Number of diseases | 0 | - | - | - |
| 1–3 | 2.41 | 1.80–3.22 | <0.001 | |
| 4 or more | 6.75 | 4.70–9.69 | <0.001 | |
| Number of hospitalization during past 5 years |
0 | - | - | - |
| 1 | 1.49 | 1.23–1.79 | <0.001 | |
| 2 or more | 2.52 | 2.08–3.06 | <0.001 | |
| Frequency of general practiocioners’ consultation | Less than once a year | - | - | - |
| Less than once a year | 1.70 | 1.32–2.20 | <0.001 | |
| At least once a month | 2.88 | 2.25–3.68 | <0.001 | |
The multiple regression model established the following associations with excessive polypharmacy: age 80–84 years, female sex, living in an urban area, diagnosis of at least four chronic diseases, and at least two hospitalizations in the last five years. The detailed results are presented in Table 4.
Table 4.
Multi regression analysis of excessive polypharmacy correlates in the PolSenior project.
| Variable | Number of Medications: 5–9 vs. 10+ | |||
|---|---|---|---|---|
| OR | 95% CI | p | ||
| Sex | Males | - | - | - |
| Females | 1.39 | 1.09–1.77 | 0.007 | |
| Age (years) | 65–69 | - | - | - |
| 70–74 | 0.95 | 0.62–1.44 | 0.794 | |
| 75–79 | 0.99 | 0.64–1.51 | 0.953 | |
| 80–84 | 1.53 | 1.01–2.33 | 0.044 | |
| 85–89 | 1.50 | 0.98–2.28 | 0.062 | |
| At least 90 | 1.32 | 0.84–2.09 | 0.224 | |
| Education | Less than primary | 0.74 | 0.49–1.12 | 0.149 |
| Primary | - | - | - | |
| Vocational | 1.32 | 0.98–1.79 | 0.070 | |
| At least secondary | 1.09 | 0.80–1.49 | 0.599 | |
| Place of residence | City | 1.35 | 1.03–1.77 | 0.029 |
| Rural area | - | - | - | |
| Number of diseases | 0 | - | - | - |
| 1–3 | 1.64 | 0.80–3.35 | 0.175 | |
| 4 or more | 2.91 | 1.39–6.07 | 0.004 | |
| Number of hospitalizations during past 5 years | 0 | - | - | - |
| 1 | 0.96 | 0.70–1.33 | 0.818 | |
| 2 or more | 1.55 | 1.17–2.04 | 0.002 | |
4. Discussion
The growing incidence of polypharmacy among older adults and the associated adverse health consequences make the search for its correlates of particular importance to characterize those at risk of its occurrence. To the best of our knowledge, this is the first observational, nationwide study describing comprehensive associations with polypharmacy and exploring the potential determinants of polypharmacy with unique data collection. We asked older individuals or their caregivers to show us all pharmaceutical preparations being consumed, which allowed for real insight into the treatment used, including OTC medications and dietary supplements/natural health products/alternative medicines. Such preparations often remained unmentioned by older people in various surveys and are sometimes not captured in electronic medical records and claims data. However, their potential interactions and adverse drug reactions can be significant, especially within a multi-medication regimen [27].
Our study indicated that over 50% of older individuals took at least five medications, and more than 10% took at least ten. In the SHARE project, based on a representative sample of community-based older populations from 17 European countries, the prevalence of concurrent use of at least five medications ranged from 26.3% to 39.9% (in Poland, 33.8%) [28]. However, the methodology of data collection used in the SHARE project (i.e., simple question whether the number of medications taken is at least 5) justifies the differences observed in relation to our study, because the SHARE participants may not have included all of the pharmaceutical preparations consumed (supplements, etc.). In older subjects, the main reason for not providing information on taking alternative medicines is failing to ask a directional question about it [29]. The SHARE study also did not include excessive polypharmacy, greater than ten products.
Analyses regarding polypharmacy are often based on national registries, so they only include prescription medications, and in addition, as each country has its own rules for medications reimbursement lists (claims data), the possibilities for comparing results are limited. According to a data registry-based study from Sweden, the prevalence of polypharmacy was higher than in our study, at 44.0%, and excessive polypharmacy at 11.7% [4].
From a methodological point of view, the study of Walckiers et al. [30] is similar to ours, based on the Belgian Health Interview Survey, in which respondents showed medicines to the interviewer. However, the comparison is also difficult in this case because the analysis considered only medications listed in the Belgian pharmacopeia. Notably, despite adopting a lower cut-off point for excessive polypharmacy in the Belgian study (at least nine medications), its frequency was lower than in our assessment (8.2%).
The fact that we included all the preparations consumed appears to be relevant to some of the relationships we observed. It is known that among individuals with higher education, there is a greater tendency to self-treatment [31]. They thus often add OTC medications and dietary supplements, natural health products, and alternative medicines to their medication regimen, which increases the polypharmacy level. It seems possible that this phenomenon had its significance in our study for the observed association of polypharmacy with a higher-than-primary level of education. However, one may speculate that the preparations added to pharmacotherapy in self-treatment are not so numerous as to cause an increase in the number of medications taken to ten and more. Moreover, we did not observe an association of self-treatment and the use of ten or more medications with education.
As for people with higher income, it can be expected that they more often use OTC preparations (e.g., medications advertised as aging modifiers or dietary supplements). In turn, an earlier analysis of general practicioners’ data suggests that more money is spent on prescriptions for those with a lower socioeconomic position because it is known that social determinants of health (to which low income and poverty belong) impact higher disease burdens, which may, in turn, cause higher polypharmacy [32]. The overlapping of these two phenomena may lead to the observed lack of relationship between polypharmacy and income.
In our study—as in many others—the female sex was associated with both polypharmacy and excessive polypharmacy. Women’s life expectancy is longer than men’s, which predisposes them to chronic comorbidities that are present for a longer period of their lives, and could have some impacted our results. Women’s attention to their health status (more pronounced than with men) results in a higher frequency of health consultations [33]. Women appear to be more likely to report both symptoms and complaints [34] and take part in preventive health care initiatives. This makes them more likely to be prescribed and self-treated with a higher number of primary and secondary prevention medicines.
As far as age (as a risk factor of polypharmacy) is concerned, we found the so-called survivor effect, as the oldest old had no increased severity of polypharmacy (nor excessive polypharmacy) observed. This is in agreement with previous studies, which suggested an inverted association between age and the number of medications after the age of 85 years [35]. Our findings are also consistent with other branches of the PolSenior projects, pointing to decreased prevalence of hypertension and pain in the oldest old. The less frequent occurrence of these conditions in the most senior group also suggests lower use of cardiovascular and analgesic medications, which are the categories of medications most commonly taken by older adults [36].
Among the socio-demographic correlates of polypharmacy, living in an urban area predisposed to both polypharmacy and excessive polypharmacy. Similar results were found in Chinese residents by Yang et al. [37]. They suggested that higher drug consumption among urban residents was due to the fact that they are more likely to have numerous doctors’ appointments and more often use self-treatment. Likewise, in Poland, access to health care (both primary and specialist) is easier in urban than in rural areas. This applies equally to the access to pharmacies, and thus also to pharmaceutical advice and preparations available in self-treatment, which can considerably contribute to the increase in polypharmacy among the city residents we describe.
We found an association of polypharmacy and excessive polypharmacy with a greater number of diseases. Multimorbidity is a common feature in geriatrics about which there is an agreement that it translates into an increase in the number of medications used [38,39]. Not surprisingly, polypharmacy was also associated with a higher number of hospitalizations within the past five years. Walckier et al. also showed an association between multiple drug prescriptions and inpatient hospitalizations in the past 12 months [30].
Notably, in our study, polypharmacy (but not excessive polypharmacy) was related to a high number of general practicioners’ consultations. One can speculate that patients with substantial multimorbidity are frequently consulted by specialists, which increases thepolypharmacy level. Our observations complement the study of Walckiers et al. [30], who claimed that visits to specialists in the past two months were associated with excessive polypharmacy only and not so with (lower level) polypharmacy. A possible explanation for this phenomenon is that patients with polypharmacy are consulted more often by general practicioners, whereas those with excessive polypharmacy are additionally consulted by specialists.
In our study, excessive polypharmacy was also related to living in an institution. According to a study conducted in nursing homes in eight European countries, 24% of residents were exposed to excessive polypharmacy [39]. Moreover, a prospective cohort study conducted in Sweden proved that living in a nursing home not only was associated with an increased risk of excessive polypharmacy at baseline but also with the incidence of excessive polypharmacy in the future [4]. It is therefore likely that multimorbidity, as well as lower functional status of nursing home residents, causes the number of preparations to quickly reach or even exceed the landmark number of ten for excessive polypharmacy.
Our study has some limitations. The study was cross-sectional thus it can not imply causality. The participation rate in the PolSenior project was not very high (49%), which may have affected the findings. To assess the association between polypharmacy and the number of diseases, only selected conditions were taken into account; however, such an approach was also applied by other authors [40]. The strength of the study was the methodology of collecting data and the high number of the oldest participants, including men. All questionnaires were administered by trained staff. Data on drug consumption were not obtained via a simple questionnaire in which the respondent is only verbally asked about medications taken. This method is potentially inaccurate since the participant may not remember all medications taken. As far as we know, this is the only study where the methodology of ‘brown bag session’ was applied throughout, and all pharmaceutical preparations (not only prescribed medicines) were presented by the participant or caregiver to the interviewer.
In summary, polypharmacy associated with hospitalization and institutionalization has the highest possibility of modification through efforts to improve medication management and deprescribing in hospital and institutional settings. Therefore, in order to reduce the risk of polypharmacy and related (potential) adverse outcomes, focusing on the impact of hospitalization and institutionalization on polypharmacyshould yield measurable results. In a Swiss study of 900 older inpatients of an internal medicine ward, the introduction of an easy-to-use checklist aimed at supporting the therapeutic decision of physicians significantly reduced the risk of prescribing unnecessary medications at discharge [41]. In regard to nursing home settings, it was also shown that an effective geriatrician-led intervention based on consultations offered to patients’ primary physicians substantially reduced polypharmacy [42].
5. Conclusions
The results of our study indicate that the prevalence of polypharmacy is high in the Polish older population. To assess the actual incidence and define the determinants of the occurrence of analyzed phenomena, comprehensive methodology of data collection is essential, including all pharmaceutical preparations consumed (both prescribed and OTC), with alternative medicines, dietary supplements, herbal remedies, etc.
With the aging population and increased availability of medicines, polypharmacy will become an escalating health problem in the coming years. To assure the effectiveness and safeness of pharmacotherapy, it is essential to find a balance between adequate control of diseases and avoiding unnecessary multi-medication regimens. To reduce the risk of polypharmacy, multifaceted interventions based on medication use review and deprescribing strategies as well as organizational interventions, with targeted prescribers both within the hospital and nursing home settings, are needed. This study serves as a starting place to understand patient characteristics associated with polypharmacy and excessive polypharmacy for targeted interventions.
Author Contributions
Conceptualization, A.N.-P., S.T. and K.W.-T.; methodology A.N.-P., S.T., D.A. and M.S.; formal analysis J.C.; investigation, M.P.-K., B.W., M.S., Z.I.N. and B.K.; writing—original draft preparation, A.N.-P. and S.T.; writing—review and editing, J.C., M.M., D.A., M.P.-K., L.W., B.W., M.S., P.M., B.K., Z.I.N. and K.W.-T.; visualization, S.T., supervision, K.W.-T., project administration, M.M. All authors have read and agreed to the published version of the manuscript.
Funding
This analysis received no external funding. The underlying study was implemented under the state-funded project entitled, “Medical, psychological, sociological and economic aspects of aging in Poland”— PolSenior, No. PBZ-MEIN-9/2/2006, The Ministry of Science and Higher Education.
Institutional Review Board Statement
The Polsenior project was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Bioethics Committee of the Medical University of Silesia in Katowice, Poland (protocol code KNW-6501-38/I/08).
Informed Consent Statement
Not applicable. The analysis was based on the data of the PolSenior project.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bayliss E.A., Edwards A.E., Steiner J.F., Main D.S. Processes of care desired by elderly patients with multimorbidities. Fam. Pract. 2008;25:287–293. doi: 10.1093/fampra/cmn040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fulton M.M., Allen E.R. Polypharmacy in the elderly: A literature review. J. Am. Acad. Nurse Pract. 2005;17:123–132. doi: 10.1111/j.1041-2972.2005.0020.x. [DOI] [PubMed] [Google Scholar]
- 3.Kim H.A., Shin J.Y., Kim M.H., Park B.J. Prevalence and predictors of polypharmacy among Korean elderly. PLoS ONE. 2014;9:e98043. doi: 10.1371/journal.pone.0098043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morin L., Johnell K., Laroche M.L., Fastbom J., Wastesson J.W. The epidemiology of polypharmacy in older adults: Register-based prospective cohort study. Clin. Epidemiol. 2018;10:289–298. doi: 10.2147/CLEP.S153458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jyrkkä J., Vartiainen L., Hartikainen S., Sulkava R., Enlund H. Increasing use of medicines in elderly persons: A five-year follow-up of the Kuopio 75+Study. Eur. J. Clin. Pharmacol. 2006;62:151–158. doi: 10.1007/s00228-005-0079-6. [DOI] [PubMed] [Google Scholar]
- 6.Zhang N., Sundquist J., Sundquist K., Ji J. An Increasing Trend in the Prevalence of Polypharmacy in Sweden: A Nationwide Register-Based Study. Front. Pharmacol. 2020;11:326. doi: 10.3389/fphar.2020.00326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moßhammer D., Haumann H., Mörike K., Joos S. Polypharmacy-an Upward Trend with Unpredictable Effects. Dtsch Arztebl Int. 2016;113:627–633. doi: 10.3238/arztebl.2016.0627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maher R.L., Hanlon J., Hajjar E.R. Clinical consequences of polypharmacy in elderly. Expert Opin. Drug Saf. 2014;13:57–65. doi: 10.1517/14740338.2013.827660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zelko E., Klemenc-Ketiš Z., TusekBunc K. Medication Adherence in Elderly with Polypharmacy Living at Home: A Systematic Review of Existing Studies. Mater. Socio Med. 2016;28:129. doi: 10.5455/msm.2016.28.129-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rodrigues M.C., Oliveira C. Drug-drug interactions and adverse drug reactions in polypharmacy among older adults: An integrative review. Rev. Lat. Am. Enferm. 2016;24:e2800. doi: 10.1590/1518-8345.1316.2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davies L.E., Spiers G., Kingston A., Todd A., Adamson J., Hanratty B. Adverse Outcomes of Polypharmacy in Older People: Systematic Review of Reviews. J. Am. Med. Dir. Assoc. 2020;21:181–187. doi: 10.1016/j.jamda.2019.10.022. [DOI] [PubMed] [Google Scholar]
- 12.Novaes P.H., da Cruz D.T., Lucchetti A.L.G., Leite I.C.G., Lucchetti G. The “iatrogenic triad”: Polypharmacy, drug–drug interactions, and potentially inappropriate medications in older adults. Int. J. Clin. Pharm. 2017;39:818–825. doi: 10.1007/s11096-017-0470-2. [DOI] [PubMed] [Google Scholar]
- 13.Agostini J.V., Han L., Tinetti M.E. The relationship between number of medications and weight loss or impaired balance in older adults. J. Am. Geriatr. Soc. 2004;52:1719–1723. doi: 10.1111/j.1532-5415.2004.52467.x. [DOI] [PubMed] [Google Scholar]
- 14.Ramgoolie P., Nichols S. Polypharmacy and the Risk of Malnutrition among Independently-living Elderly Persons in Trinidad. West Indian Med. J. 2015;65:323–327. doi: 10.7727/wimj.2014.285. [DOI] [PubMed] [Google Scholar]
- 15.Ruby C.M., Hanlon J.T., Fillenbaum G.G., Pieper C.F., Branch L.G., Bump R.C. Medication use and control of urination among community-dwelling older adults. J. Aging Health. 2005;17:661–674. doi: 10.1177/0898264305279875. [DOI] [PubMed] [Google Scholar]
- 16.Madan A., Oldham J.M., Gonzalez S., Fowler J.C. Reducing Adverse Polypharmacy in Patients With Borderline Personality Disorder: An Empirical Case Study. Prim. Care Companion CNS Disord. 2015;17 doi: 10.4088/PCC.14m01760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leelakanok N., Holcombe A.L., Lund B.C., Gu X., Schweizer M.L. Association between polypharmacy and death: A systematic review and meta-analysis. J. Am. Pharm. Assoc. 2003;57:729–738.e10. doi: 10.1016/j.japh.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 18.Jyrkkä J., Enlund H., Korhonen M.J., Sulkava R., Hartikainen S. Polypharmacy status as an indicator of mortality in an elderly population. Drugs Aging. 2009;26:1039–1048. doi: 10.2165/11319530-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 19.Masoudi F.A., Baillie C.A., Wang Y., Bradford W.D., Steiner J.F., Havranek E.P., Foody J.M., Krumholz H.M. The complexity and cost of drug regimens of older patients hospitalized with heart failure in the United States, 1998–2001. Arch. Intern. Med. 2005;165:2069–2076. doi: 10.1001/archinte.165.18.2069. [DOI] [PubMed] [Google Scholar]
- 20.Pasina L., Brucato A.L., Falcone C., Cucchi E., Bresciani A., Sottocorno M., Taddei G.C., Casati M., Franchi C., Djade C.D., et al. Medication non-adherence among elderly patients newly discharged and receiving polypharmacy. Drugs Aging. 2014;31:283–289. doi: 10.1007/s40266-014-0163-7. [DOI] [PubMed] [Google Scholar]
- 21.Higgins J.P.T., Green S. Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons; London, UK: 2011. (Volume 4 de Wiley Cochrane Series). [Google Scholar]
- 22.Soler O., Barreto J.O.M. Community-Level Pharmaceutical Interventions to Reduce the Risks of Polypharmacy in the Elderly: Overview of Systematic Reviews and Economic Evaluations. Front. Pharmacol. 2019;10:302. doi: 10.3389/fphar.2019.00302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zarowitz B.J., Stebelsky L.A., Muma B.K., Romain T.M., Peterson E.L. Reduction of high-risk polypharmacy drug combinations in patients in a managed care setting. Pharmacotherapy. 2005;25:1636–1645. doi: 10.1592/phco.2005.25.11.1636. [DOI] [PubMed] [Google Scholar]
- 24.Cooper J.A., Cadogan C.A., Patterson S.M., Kerse N., Bradley M.C., Ryan C., Hughes C.M. Interventions to improve the appropriate use of polypharmacy in older people: A Cochrane systematic review. BMJ Open. 2015;5:e009235. doi: 10.1136/bmjopen-2015-009235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Olaniyan J.O., Ghaleb M., Dhillon S., Robinson P. Safety of medication use in primary care. Int. J. Pharm. Pract. 2015;23:3–20. doi: 10.1111/ijpp.12120. [DOI] [PubMed] [Google Scholar]
- 26.Bledowski P., Mossakowska M., Chudek J., Grodzicki T., Milewicz A., Szybalska A., Wieczorowska-Tobis K., Wiecek A., Bartoszek A., Dabrowski A., et al. Medical, psychological and socioeconomic aspects of aging in Poland: Assumptions and objectives of the PolSenior project. Exp. Gerontol. 2011;46:1003–1009. doi: 10.1016/j.exger.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 27.Asher G.N., Corbett A.H., Hawke R.L. Common Herbal Dietary Supplement-Drug Interactions. Am. Fam. Physician. 2017;96:101–107. [PubMed] [Google Scholar]
- 28.Midão L., Giardini A., Menditto E., Kardas P., Costa E. Polypharmacy prevalence among older adults based on the survey of health, ageing and retirement in Europe. Arch. Gerontol. Geriatr. 2018;78:213–220. doi: 10.1016/j.archger.2018.06.018. [DOI] [PubMed] [Google Scholar]
- 29.Shelley B.M., Sussman A.L., Williams R.L., Segal A.R., Crabtree B.F., Rios Net Clinicians ‘They don’t ask me so I don’t tell them’: Patient-clinician communication about traditional, complementary, and alternative medicine. Ann. Fam. Med. 2009;7:139–147. doi: 10.1370/afm.947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walckiers D., Van der Heyden J., Tafforeau J. Factors associated with excessive polypharmacy in older people. Arch. Public Health. 2015;73:50. doi: 10.1186/s13690-015-0095-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chari H.S., Kadeangadi D.M., Mallapur M.D. Practice of Self Medication Among Urban Households—A Community Based Cross Sectional Study. Natl. J. Community Med. 2015;6:93–96. [Google Scholar]
- 32.Worrall A., Rea J.N., Ben-Shlomo Y. Counting the cost of social disadvantage in primary care: Retrospective analysis of patient data. Br. Med. J. 1997;314:38–42. doi: 10.1136/bmj.314.7073.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Agrawal S., Gołębiowska J., Makuch S., Mazur G. Prevalence of Use of Preventive Services in Poland: Result from a Population-Based Nationwide Study. J. Clin. Med. 2021;10:2084. doi: 10.3390/jcm10102084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Santalucia P., Franchi C., Djade C.D., Tettamanti M., Pasina L., Corrao S., Salerno F., Marengoni A., Marcucci M., Nobili A., et al. Gender difference in drug use in hospitalized elderly patients. Eur. J. Intern. Med. 2015;26:483–490. doi: 10.1016/j.ejim.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 35.Onder G., Marengoni A., Russo P., Degli Esposti L., Fini M., Monaco A., Bonassi S., Palmer K., Marrocco W., Pozzi G., et al. Advanced Age and Medication Prescription: More Years, Less Medications? A Nationwide Report From the Italian Medicines Agency. J. Am. Med. Dir. Assoc. 2016;17:168–172. doi: 10.1016/j.jamda.2015.08.009. [DOI] [PubMed] [Google Scholar]
- 36.Hosseini S.R., Zabihi A., Amiri S.R.J., Bijani A. Polypharmacy among the elderly. J. Mid-Life Health. 2018;9:97–103. doi: 10.4103/jmh.JMH_87_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yang M., Lu J., Hao Q., Luo L., Dong B. Does residing in urban or rural areas affect the incidence of polypharmacy among older adults in western China? Arch. Gerontol. Geriatr. 2015;60:328–333. doi: 10.1016/j.archger.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 38.Rawle M.J., Richards M., Davis D., Kuh D. The prevalence and determinants of polypharmacy at age 69: A British birth cohort study. BMC Geriatr. 2018;18:118. doi: 10.1186/s12877-018-0795-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Onder G., Liperoti R., Fialova D., Topinkova E., Tosato M., Danese P., Gallo P.F., Carpenter I., Finne-Soveri H., Gindin J., et al. Polypharmacy in nursing home in Europe: Results from the SHELTER study. J. Gerontol. A Biol. Sci. Med. Sci. 2012;67:698–704. doi: 10.1093/gerona/glr233. [DOI] [PubMed] [Google Scholar]
- 40.Sulicka J., Pac A., Puzianowska-Kuźnicka M., Zdrojewski T., Chudek J., Tobiasz-Adamczyk B., Mossakowska M., Skalska A., Więcek A., Grodzicki T. Health status of older cancer survivors-results of the PolSenior study. J. Cancer Surviv. 2018;12:326–333. doi: 10.1007/s11764-017-0672-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Urfer M., Elzi L., Dell-Kuster S., Bassetti S. Intervention to Improve Appropriate Prescribing and Reduce Polypharmacy in Elderly Patients Admitted to an Internal Medicine Unit. PLoS ONE. 2016;11:e0166359. doi: 10.1371/journal.pone.0166359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tamura B.K., Bell C.L., Lubimir K., Iwasaki W.N., Ziegler L.A., Masaki K.H. Physician intervention for medication reduction in a nursing home: The polypharmacy outcomes project. J. Am. Med. Dir. Assoc. 2011;12:326–330. doi: 10.1016/j.jamda.2010.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]