Abstract
Background: Disability is an important problem in aging societies globally. However, the research findings of the prevalence of disability have been inconsistent. This study aims to estimate the prevalence of disability and its influencing factors among the Chinese older population from 1979 to 31 July 2021. Methods: A systematic review and meta-analysis were conducted using both international (PubMed, Web of Science, CBMdisc, PsycINFO, the Cochrane Library, and EMBASE) and Chinese (CNKI, CQVIP, and WanFang) databases. Meta-analysis was performed using a random-effects model to account for heterogeneity. Subgroup analyses were also done. Results: The pooled prevalence of disability across all 97 studies was 26.2% (95% CI: 23.7–28.6%). The estimates varied according to the types of activities of daily living (ADL), gender, age, and region. Studies based on the identification of cases by using the complete ADL scale showed a higher prevalence than those using the basic ADL scale. The prevalence was slightly higher among female older individuals than among male older individuals. The highest rates were seen in older individuals aged 80 years or older. Elders in central China, southwest China, and northwest China were more likely to be BADL-disabled. Conclusion: Prevalence of disability among the Chinese older population is high, around 26%. Using standardized diagnostic systems to correctly estimate the prevalence of disability would be helpful for public health professionals in China.
Keywords: prevalence, disability, activities of daily living, older population, Chinese, meta-analysis
1. Introduction
With the continuous extension of average life expectancy, the proportion of older individuals is increasing dramatically. In 2017, there were an estimated 962 million people aged 60 years or above, accounting for 13% of the global population [1]. The older population in China has reached a prevalence of 18.7%, according to China’s seventh census [2]. With the rapid aging that is occurring in all regions of the world, the prevalence of older individuals in the whole world, except Africa, will reach 25% by 2050. Therefore, the problems associated with an aging society are becoming more severe, and one of the associated problems is a high rate of disability. Figuring out the rate of disability and the number of disabled elders is vital for a country to make improvements and promotion strategies for the old, disabled population’s quality of life. Relevant agencies can also make better plans for financial support, nursing services, and medical services.
According to the World Health Organization (WHO) report on disability, the estimated prevalence of disability was 10.2% in people aged 60 years or above in 194 countries and regions around the world [3]. However, in China, the second national sample survey on disability pointed out that the disabled elders accounted for 24.43% of all older individuals [4]. This difference in the prevalence of disability was more apparent in individual studies. We found that the prevalence of disability among the Chinese older population varies greatly, ranging from 1.85% to 71.28% [5,6], after combining the results of different studies. The pooled prevalence rates given by three relevant meta-analyses were 20.1% (95% CI: 14.7–25.6%), 28.5% (95% CI: 25.9–31.2%), and 34% (95% CI: 14–53%), which also seem to be quite different [7,8,9].
One of the reasons for this discrepancy is the different understanding and measurements. Disability can be defined in various ways, including impairment, limitations in mobility, physical function decline, and activities of daily living (ADLs). World Health Organization (WHO)’s International Classification of Functioning, Disability, and Health (ICF) uses disability as an umbrella term for impairments, activity limitations, or participation restrictions [10]. Additionally, it points out that disability represents the negative aspects of the interaction between the health condition and life situations (personal factors and environmental factors). Thus, the ADL is considered a suitable measurement of disability and also has good robustness and comparability [11,12].
Although several studies calculated the prevalence of ADL disability among the older population, a synthesis of these studies to derive a general risk estimate has not been well conducted. Hence, we have carried out a systematic review and meta-analysis to comprehensively analyze the related studies and extract a more accurate and general prevalence of disability by avoiding differences in individual studies caused by biased samples and moderating factors.
2. Materials and Methods
2.1. Literature Search
This research protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO: CRD42021269367). The literature search was conducted using the Chinese National Knowledge Infrastructure (CNKI), VIP Database (CQVIP), China Biology Medicine disc (CBMdisc), Wanfang, PubMed, Web of Science, Embase, and the Cochrane Library. All databases were searched from 1979 (the earliest year available on the CNKI database) to 31 July 2021. The search terms were keywords related to the older population (elderly OR elder OR old population OR old adults), ADL (activities of daily living OR disable OR disabled OR ADL OR BADL OR IADL), and China (China OR Chinese).
The screening procedure is shown below: (a) the titles were reviewed to determine potential articles related to the topic, (b) the abstracts were reviewed to narrow down the list of articles, and (c) the full text of the articles was read to make a final decision.
2.2. Inclusion and Exclusion Criteria
The complete type of ADL includes basic activities of daily living (BADL) and instrumental activities of daily living (IADL). The most commonly used scales for assessing BADL are the Katz independence index and the Barthel independence index, which have 6 or 10 items, consisting of relatively simple self-care tasks such as dressing, eating, and bathing [13,14]. Moreover, the frequently used tool for assessing IADL was designed by Lawton and Brody and has 8 items, such as shopping, cooking, financial management, and other more complex activities [15]. Those standard scales provide good support for us to merge the rates and compare. Some researchers used a self-made scale or increased or decreased the ADL items, and we did not include these studies.
Studies were included only if they met the following criteria: (a) the study was published between 1979 and 31 July 2021; (b) the study was conducted using a questionnaire survey, and the measurement tool was the Barthel independence index, the Katz independence index or the scale designed by Lawton and Brody; (c) the study reported the prevalence of disability with accurate and clear data; and (d) all older respondents were aged 60 years or above and came from Mainland China.
Studies were excluded if they met the following criteria: (a) for literature published with the same data, only the latest data were included; (b) reviews, conferences, lectures, or unpublished essays; (b) an unscientific research design, such as convenience sampling, was used in the study; and (c) the study was based on a sample population involving patients, elders living in nursing homes, and other special groups with specific health-related characteristics.
2.3. Data Extraction
The data in the studies, including the authors, publication year, survey year, sampling locations, diagnostic tools, participants, and disability cases, were collected. Additionally, the prevalence of disability among older individuals of different diagnostic tools, genders, ages, and regions was collected.
All studies were reviewed and coded by two authors to determine the consistency of the inclusion and exclusion criteria. In addition, each study included in the meta-analysis was coded by two authors to extract major outcomes. The discrepancies were resolved through discussions.
2.4. Quality of Assessment
The quality of included studies was assessed by the 11-item checklist recommended by the Agency for Healthcare Research and Quality (AHRQ). The item would be scored 1 for the answer of “Yes” and would get a score of 0 if the answer was “No” or “Unclear” (opposite for the 5th item). A total score of 0–3 = low quality, 4–7 = moderate quality, and 8–11 = high quality [16].
2.5. Statistical Analysis
The meta-analysis was carried out by using STATA 16.0. Combined effect sizes with corresponding confidence intervals (95%) were calculated, and these indicated the magnitude of the effect across all studies. The Q test and I2 statistics were used to assess heterogeneity among the included studies. p > 0.05 and I2 < 50% indicated no statistical heterogeneity between the studies. If no heterogeneity was observed, the fixed-effects model was employed; otherwise, the random-effects model was used [17]. The homogeneity test showed that Q = 81,405.53 (p < 0.001) and I2 = 99.9%. Therefore, we adopted the random-effects model for all meta-analyses.
Subgroup analyses and meta-regression analyses were conducted to eliminate heterogeneity and identify potential influencing factors. Sensitivity analyses were conducted by removing one study at a time and then recalculating the prevalence of the remaining studies to test the robustness of the primary results. Publication bias was diagnosed through Begg’s test. The significance level was set at 0.05 (two-sided) in all analyses.
3. Results
3.1. Search Strategy and Selection Criteria
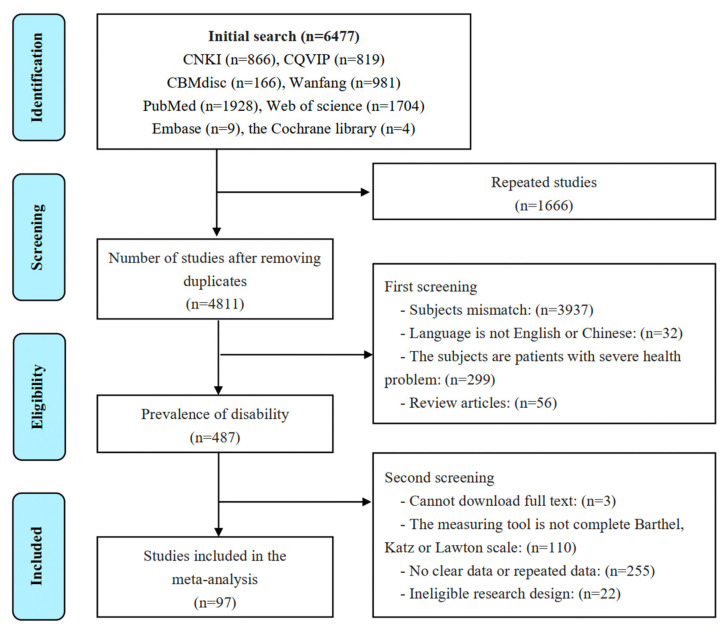
Figure 1 shows a flow diagram of the systematic search of the literature. A total of 6444 articles were identified in 8 electronic databases. Among them, 1666 duplicates were eliminated, the titles and abstracts studies were screened, and the full text of 484 studies was evaluated. In the end, 97 studies passed the evaluation and were included in the meta-analysis.
Figure 1.
Flow chart of the study selection process.
3.2. Quality Assessment
The results of the quality assessment are shown in Table 1. Based on the AHRQ checklist, 97 studies reached moderate quality and above.
Table 1.
Risk of bias using quality assessment forms.
| Item | Yes | No | Unclear |
|---|---|---|---|
| (1) Define the source of information (survey, record review) | 97 | 0 | 0 |
| (2) List inclusion and exclusion criteria for exposed and unexposed subjects (cases and controls) or refer to previous publications | 97 | 0 | 0 |
| (3) Indicate time period used for identifying patients | 78 | 19 | 0 |
| (4) Indicate whether or not subjects were consecutive if not population-based | 97 | 0 | 0 |
| (5) Indicate if evaluators of subjective components of the study were masked to other aspects of the status of the participants | 0 | 97 | 0 |
| (6) Describe any assessments undertaken for quality assurance purposes (e.g., test/retest of primary outcome measurements) | 60 | 36 | 1 |
| (7) Explain any patient exclusions from the analysis | 89 | 7 | 1 |
| (8) Describe how confounding was assessed and/or controlled. | 65 | 32 | 0 |
| (9) If applicable, explain how missing data were handled in the analysis | 13 | 82 | 2 |
| (10) Summarize patient response rates and completeness of data collection | 86 | 11 | 0 |
| (11) Clarify what follow-up, if any, was expected and the percentage of patients for which incomplete data or follow-up was obtained | 0 | 97 | 0 |
3.3. Study Characteristics
Table A1 in Appendix A summarizes the characteristics and findings of the included studies. A total of 97 eligible studies reported the prevalence of disability in Chinese older individuals, with a total of 110 results. Eight studies reported multiple results because they used several cross-sectional data sets or used several types of ADL.
Most of the included studies were cross-sectional, and two were longitudinal. For the longitudinal study, we included only the results from the cross-sectional analysis of the baseline data. In addition, 18 studies used national data, while the remaining studies obtained samples from regions within China; 86 studies were conducted with the general older population (≥60 or ≥65 years), but 11 studies only included the oldest elders (≥80 years) or centenarians. The sample size ranged from 182 to 32,281. The time of data collection spanned nearly three decades.
3.4. Pooled Prevalence of Disability
In total, 97 studies met the inclusion criteria, with 110 results. The whole sample included 561,800 subjects, of whom 116,813 had disabilities. Table 2 shows that the pooled prevalence of disability among the Chinese older population was 26.2% (95% CI: 23.7–28.6%).
Table 2.
Pooled prevalence of disability and subgroup analyses.
| Variables | Classification | Number of Studies | Number of Results | Event Rate (%) | 95% CI (%) | Heterogeneity I2 (%) | Q-Value | p-Value |
|---|---|---|---|---|---|---|---|---|
| Pooled prevalence | 97 | 110 | 26.2 | 23.7–28.6 | 99.9 | 81,405.53 | ||
| Type of ADL | BADL | 56 | 62 | 20.5 | 17.7–23.3 | 99.9 | 26.55 | <0.001 |
| IADL | 7 | 7 | 31.8 | 21.2–42.4 | 99.9 | |||
| BADL + IADL | 41 | 41 | 33.8 | 29.4–38.3 | 99.6 | |||
| Gender | Male | 53 | 60 | 22.7 | 20.0–25.5 | 99.7 | 5.35 | 0.021 |
| Female | 53 | 60 | 28.5 | 24.5–32.5 | 99.8 | |||
| Age group | 60–69 | 23 | 26 | 12.8 | 10.1–15.5 | 99.6 | 104.92 | <0.001 |
| 70–79 | 23 | 26 | 22.4 | 16.5–28.3 | 99.7 | |||
| ≥80 | 36 | 44 | 36.8 | 33.1–40.5 | 99.6 | |||
| Region | Eastern China | 32 | 33 | 27.0 | 22.3–31.7 | 99.8 | 2.44 | 0.786 |
| Northern China | 18 | 20 | 26.0 | 19.9–32.1 | 99.7 | |||
| Southern China | 6 | 6 | 24.2 | 8.0–40.3 | 99.7 | |||
| Central China | 7 | 7 | 26.9 | 17.9–35.8 | 99.4 | |||
| Southwest China | 10 | 13 | 30.9 | 22.3–39.4 | 99.7 | |||
| Northwest China | 4 | 4 | 21.3 | 12.3–30.3 | 97.8 | |||
| Hukou | Urban | 17 | 22 | 22.4 | 16.9–27.9 | 99.9 | 2.13 | 0.143 |
| Rural | 26 | 31 | 28.0 | 22.9–33.0 | 99.9 | |||
| Survey year | 1999 and before | 5 | 6 | 21.4 | 10.4–32.4 | 99.8 | 2.16 | 0.706 |
| 2000–2004 | 6 | 7 | 23.7 | 13.0–34.3 | 99.8 | |||
| 2005–2009 | 10 | 12 | 29.1 | 21.6–36.7 | 99.7 | |||
| 2010–2014 | 41 | 43 | 27.7 | 23.6–31.8 | 99.8 | |||
| 2015–2019 | 36 | 38 | 25.3 | 20.9–29.7 | 99.9 | |||
3.5. Subgroup Analyses
The prevalence varied greatly according to the types of ADL. The prevalence of disability detected by BADL was 20.5% (95% CI: 17.7–23.3%), which was significantly lower than that detected by complete ADL (33.8%, 95% CI: 29.4–38.3%) (p < 0.001).
The prevalence in women (28.5%, 95% CI: 24.5–32.5%) was slightly higher than that in men (22.7%, 95% CI: 20.0–25.5%). A significant difference was found among different age groups (p < 0.001). The prevalence of disability in the oldest age group (≥80 years) was 36.8% (95% CI: 33.1–40.5%), which was higher than that in the 60–69 years age group (12.8%, 95% CI: 10.1–15.5%) and the 70–80 years age group (22.4%, 95% CI: 16.5–28.3%).
3.6. Assessment of Disability by Using a Specific Type of ADL
3.6.1. BADL
As Table 3 shown, 56 studies provided information about the BADL. The random-effects analysis showed that the pooled prevalence of BADL disability was 20.5% (95% CI: 17.7–23.3%). Furthermore, older individuals aged 80 years or over (30.0%, 95% CI: 26.2–33.9%, p < 0.001) had a significantly higher BADL disability rate than younger elders. To avoid the limitation of insufficient studies, we merged some regional subgroups and found that other parts of China had an obviously higher BADL prevalence (24.4%, 95% CI: 26.2–33.9%, p < 0.001) than northern China.
Table 3.
Pooled prevalence of BADL disabilities and subgroup analyses.
| Variables | Classification | Number of Studies | Number of Results | Event Rate (%) | 95% CI (%) | Heterogeneity I2 (%) | Q-Value | p-Value |
|---|---|---|---|---|---|---|---|---|
| Pooled prevalence | 56 | 62 | 20.5 | 17.7–23.3 | 99.9 | 45,852.90 | ||
| Gender | Male | 37 | 41 | 19.4 | 16.4–22.4 | 99.7 | 3.95 | 0.047 |
| Female | 37 | 41 | 25.1 | 20.3–29.9 | 99.8 | |||
| Age group | 60–69 | 17 | 17 | 7.3 | 5.7–8.9 | 98.6 | 111.60 | <0.001 |
| 70–79 | 17 | 17 | 13.1 | 10.4–15.9 | 98.4 | |||
| ≥80 | 29 | 33 | 30.0 | 26.2–33.9 | 99.6 | |||
| Region | Eastern China | 15 | 15 | 16.8 | 13.5–20.1 | 99.3 | 10.45 | 0.005 |
| Northern China | 6 | 8 | 12.9 | 9.7–16.1 | 99.2 | |||
| Other regions * | 16 | 16 | 24.4 | 18.0–30.7 | 99.5 | |||
| Hukou | Urban | 14 | 18 | 22.6 | 16.1–29.2 | 99.9 | 0.00 | 0.944 |
| Rural | 16 | 20 | 22.4 | 17.4–27.3 | 99.9 | |||
| Survey year | 2009 and before * | 8 | 14 | 21.7 | 14.2–29.1 | 99.9 | 0.78 | 0.678 |
| 2010–2014 | 25 | 25 | 21.3 | 17.6–25.1 | 99.7 | |||
| 2015–2019 | 20 | 20 | 18.9 | 14.3–23.4 | 99.8 | |||
* To avoid the limitation of insufficient studies, we merged Central China, Southwest China, and Northwest China into a group called “Other regions”. In addition, the studies published in 2009 and before were merged into one group.
3.6.2. Complete ADL
As Table 4 shown, 41 studies combined the basic and instrumental activities of daily living as a complete measurement tool, which consisted of 14 items. The pooled prevalence of disability according to complete ADL was 33.8% (95% CI: 29.4–38.3%). The oldest elders (≥80 years) also had an evidently higher prevalence (61.9%, 95% CI: 51.9–71.9%, p < 0.001).
Table 4.
Pooled prevalence of complete ADL and subgroup analyses.
| Variables | Classification | Number of Studies | Number of Results | Event Rate (%) | 95% CI (%) | Heterogeneity I2 (%) | Q-Value | p-Value |
|---|---|---|---|---|---|---|---|---|
| Pooled prevalence | 41 | 41 | 33.8 | 29.4–38.3 | 99.6 | 10,997.47 | ||
| Gender | Male | 16 | 16 | 32.2 | 23.1–41.4 | 99.5 | 0.52 | 0.472 |
| Female | 16 | 16 | 36.7 | 28.7–44.7 | 99.4 | |||
| Age group | 60–69 | 6 | 6 | 25.5 | 14.0–36.9 | 99.7 | 22.45 | <0.001 |
| 70–79 | 6 | 6 | 40.5 | 24.9–56.1 | 99.6 | |||
| ≥80 | 7 | 7 | 61.9 | 51.9–71.9 | 97.3 | |||
| Region | Eastern China | 16 | 16 | 36.4 | 27.8–44.9 | 99.8 | 1.10 | 0.578 |
| Northern China | 12 | 12 | 34.7 | 26.9–42.4 | 99.6 | |||
| Other regions * | 12 | 12 | 31.2 | 25.1–37.2 | 99.6 | |||
| Survey year | 2009 and before * | 10 | 10 | 32.9 | 24.4–41.5 | 99.5 | 0.38 | 0.827 |
| 2010–2014 | 15 | 15 | 35.9 | 27.4–44.3 | 99.7 | |||
| 2015–2019 | 16 | 16 | 32.5 | 24.9–40.1 | 99.7 | |||
* To avoid the limitation of insufficient studies, we merged Central China, Southwest China, and Northwest China into a group called “Other regions”. In addition, the studies published in 2009 and prior to 2009 were merged into one group.
3.7. Meta-Regression
In this study, score, mean age, the proportion of females, the proportion of rural hukou, publication year, and survey year can be taken as a continuous variable. Additionally, meta-regression was performed to assess the relationship between those variables and the pooled prevalence. The results showed that only mean age had a significant linear relationship with the prevalence of disability (b = 0.0094, p < 0.001). Thus, the prevalence of ADL disability in Chinese older adults showed an ascending trend with age.
3.8. Publication Bias and Sensitivity Analyses
Begg’s test showed that there was no obvious publication bias (z = 1.65, p = 0.099). The results of sensitivity analysis were between 25.7% (95% CI: 23.3–28.2%) and 26.4% (95% CI: 23.9–28.9%), indicating that the primary result had good robustness.
4. Discussion
To the best of our knowledge, this is the first meta-analysis to examine the prevalence of disability among older adults in mainland China over such an extensive period based on both international and Chinese databases. The total number of older persons in this analysis was large enough to be conclusive on several issues. The meta-analysis of 97 studies revealed that the prevalence was 26.2% (95% CI: 23.7–28.6%), which means there are nearly 69 million older people suffering from disabilities in China. Additionally, the prevalence of disability presented differences in terms of types of ADL, gender, age, and region.
We divided ADL into three types when collating and analyzing the data and found that we obtained a higher pooled prevalence for complete ADL, especially compared with BADL. These findings might be related to the characteristics of BADL and IADL. BADL and IADL represent different positions along the spectrum of the disablement process. BADL reflects the elders’ basic self-care independence, whereas IADL reflects the ability of older people to live independently. The IADL disability is more likely to happen earlier with age. Hence, the more items that are included, the more sensitive the tool will be.
Several studies had shown that the ADL ability of older individuals was negatively correlated with age [18,19]. Therefore, it is not surprising that the pooled prevalence of disability among the oldest people (age 80 years or above) was significantly higher than that of younger individuals. Meanwhile, the regression results suggest that the increase in the prevalence of disability is about a 0.09 percent point for each 1-year increase in the mean age of the population. With increasing age, the physiological functions of older adults continue to decline, the risk of chronic disease and accidental injury increases, and the disability trend could further increase [20].
The prevalence of disability differs significantly by gender, and the prevalence in females was significantly higher than that in males. This finding is consistent with the results of numerous studies, showing that females are more likely to experience disabilities [21]. Especially in BADL disability, that females’ disability rate was 1.29 times that of males. This difference was mainly attributed to two aspects. Compared with females, males have usually had better social status, income, and degree of education since ancient times. They have a stronger awareness of health care and more social resources to obtain health care [22]. In addition, the average life expectancy of females is longer than that of males [23], leading to a higher risk of disability.
Compared with northern China, elders in other regions (including central China, southwest China, and northwest China) were more likely to be BADL-disabled. Although the economic conditions have been greatly improved recently in most areas of China, many older adults living in remote areas are still unable to obtain timely and high-quality medical services.
This analysis provides useful information for the public health professionals of China. Over a quarter of all Chinese older individuals may have different levels of disability. This result indicates that we should strengthen community-based intervention and provide more health services, such as disability assessments and functional exercises. Once an individual has a severe functional impairment, medical assistance and financial subsidies should be provided promptly. This is especially true for older individuals aged over 80 years and female older individuals.
5. Limitations
There are some limitations of our study. First, this study included only published studies, and there may have been publication bias even though no such bias was indicated by statistical tests. Second, the included studies suffered from high heterogeneity, although the measurement tools were controlled and subgroup analyses were performed to address this shortcoming. High heterogeneity may reflect differences in the design and conduct of the studies (methodological heterogeneity) or in the participants and outcomes measured (clinical heterogeneity) [24,25]. In this meta-analysis, we collected many studies published over nearly three decades. It was inevitable that we did not fully identify the studies with low-quality research design. Additionally, we may have ignored some important confounding factors, such as disease and social-economic status. Moreover, the large sample size included in the study may also make the I2 value increase [26]. In addition, when using dependency measures, much information about the severity of the disability was lost, which is worthy of further study.
6. Conclusions
The meta-analysis of 97 studies on the prevalence of disability among the Chinese elderly population from 1979 to 2021 found that (1) the pooled prevalence reached 26.2% (95% CI: 23.7–28.6%) and (2) differences in prevalence exist in terms of types of ADL, gender and age. Considering the negative impact of disability on personal well-being and financial expenditure, regular and appropriate interventions are needed for this vulnerable group.
Appendix A
Table A1.
Characteristics of the 97 studies included in the meta-analysis.
| NO. | Study | Publication Year | Language | Survey Year | Sampling Province | Age (Mean) |
Type of ADL | Sample Size | Female (N, %) |
Rural (N, %) |
Cases of Disability | Rate | Score of Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Huang et al. [27] | 1993 | CH | 1991 * | Sichuan | ≥60 (68.8) | PADL + IADL ** | 1242 | 657 (52.9) | NR | 422 | 33.98 | 6 |
| 2. | Meng et al. [28] | 1996 | CH | 1992 | Beijing | ≥60 | PADL + IADL | 3257 | 1415 (43.44) | NR | 778 | 23.90 | 7 |
| 3. | Tang et al. [29] | 1999 | EN | 1990 | Beijing | ≥60 (71.0) | PADL ** | 3440 | 1733 (50.38) | NR | 629 | 18.28 | 9 |
| 4. | Lv et al. [30] | 2001 | CH | 2000 | Anhui | ≥60 | PADL + IADL | 1424 | NR | NR | 274 | 19.24 | 5 |
| 5a. | Meng et al. [31] | 2002 | CH | 1992 | Beijing | ≥60 (72.3) | PADL | 2783 | NR | NR | 262 | 9.41 | 8 |
| 5b. | Meng et al. [31] | 2002 | CH | 1997 | Beijing | ≥60 (72.0) | PADL | 2786 | NR | NR | 171 | 6.14 | 8 |
| 5c. | Meng et al. [31] | 2002 | CH | 2000 | Beijing | ≥60 (72.9) | PADL | 2667 | NR | NR | 214 | 8.02 | 8 |
| 6. | Wang et al. [32] | 2002 | CH | 2000 | Guangzhou | ≥60 | PADL ** | 1161 | 631 (54.35) | NR | 94 | 8.10 | 7 |
| 7. | Lin et al. [33] | 2002 | CH | 2000 | Beijing | ≥60 | PADL | 895 | NR | NR | 174 | 19.44 | 7 |
| 8. | Ji et al. [34] | 2007 | CH | 2005 * | Jiangsu | ≥60 | PADL + IADL | 337 | NR | NR | 103 | 30.56 | 6 |
| 9. | Yin and Lu [35] | 2007 | EN | 2002 | National | ≥80 | PADL | 8844 | 4938 (55.83) | 4627 (52.3) | 3153 | 35.65 | 10 |
| 10a. | Huang et al. [36] | 2008 | CH | 2006 * | Guizhou | ≥60 (70.2) | PADL | 3221 | 1995 (61.94) | NR | 171 | 5.31 | 7 |
| 10b. | Huang et al. [36] | 2008 | CH | 2006 * | Guizhou | ≥60 (70.2) | IADL | 3221 | 1995 (61.94) | NR | 382 | 11.86 | 7 |
| 11. | Tang et al. [37] | 2009 | CH | 2008 | Hunan | ≥60 | PADL + IADL | 203 | 124 (61.08) | NR | 102 | 50.25 | 7 |
| 12. | Xu et al. [38] | 2011 | CH | 2009 * | Zhejiang | ≥60 (70.0) | PADL + IADL | 753 | 404 (53.65) | 753(100.00) | 129 | 17.13 | 7 |
| 13. | Chen et al. [39] | 2011 | CH | 2010 | Zhejiang | ≥80 (84.8) | PADL ** | 454 | 268 (59.03) | NR | 138 | 30.40 | 9 |
| 14. | Li et al. [40] | 2011 | EN | 2006 | Beijing | ≥60 | PADL + IADL | 1882 | 990 (52.60) | NR | 817 | 43.41 | 5 |
| 15. | Xue et al. [41] | 2011 | CH | 2010 | Shanghai | ≥80 (83.1) | PADL + IADL | 1027 | 140 (13.63) | NR | 674 | 65.63 | 9 |
| 16. | Li et al. [42] | 2012 | CH | 2009 | Shanghai | ≥60 (73.3) | PADL + IADL | 11,338 | 6043 (53.30) | NR | 2013 | 17.75 | 8 |
| 17. | Shi et al. [43] | 2012 | CH | 2011 | Shandong | ≥65 | PADL | 504 | 234 (46.43) | NR | 96 | 19.05 | 8 |
| 18. | Li et al. [44] | 2012 | CH | 2010 * | Ningxia | ≥60 | PADL + IADL ** | 904 | 459 (50.77) | NR | 261 | 28.87 | 7 |
| 19. | Zhang et al. [45] | 2012 | CH | 2010 * | Hebei | ≥60 | PADL + IADL ** | 2161 | NR | NR | 796 | 36.83 | 7 |
| 20. | Yu et al. [46] | 2012 | CH | 2011 | Shanghai | ≥60 | PADL + IADL | 1500 | 842 (56.13) | NR | 589 | 39.27 | 8 |
| 21. | Huang et al. [47] | 2012 | CH | 2008 | Anhui | ≥60 (70.2) | PADL + IADL ** | 1117 | 764 (68.40) | 1117(100.00) | 764 | 68.40 | 8 |
| 22. | Yin et al. [48] | 2012 | CH | 2009 | Zhejiang | ≥60 (71.2) | PADL + IADL ** | 2184 | 1218 (55.77) | 2184(100.00) | 566 | 25.92 | 8 |
| 23. | Zhang and Wei [49] | 2014 | CH | 2013 | Beijing | ≥60 | PADL | 2031 | NR | NR | 200 | 9.85 | 9 |
| 24. | Zhong et al. [50] | 2014 | CH | 2008 | Zhejiang, Gansu | ≥60 | PADL ** | 1157 | 547 (47.28) | 647 (55.92) | 214 | 18.50 | 9 |
| 25. | Yin et al. [51] | 2014 | EN | 2011 | National | ≥80 (92.3) | PADL | 5495 | 3192 (58.09) | NR | 1856 | 33.78 | 9 |
| 26. | Chen et al. [52] | 2015 | CH | 2013* | Fujian | ≥60 (71.5) | PADL | 14,292 | 7404 (51.81) | NR | 610 | 4.27 | 8 |
| 27. | Li et al. [53] | 2015 | CH | 2013* | Ningxia | ≥60 (70.0) | PADL + IADL ** | 817 | 457 (55.94) | NR | 84 | 10.28 | 7 |
| 28. | Li and Yuan [54] | 2015 | CH | 2013 | Shandong | ≥60 | PADL | 416 | 276 (66.19) | 172 (41.25) | 67 | 16.11 | 7 |
| 29. | Zhang et al. [55] | 2015 | CH | 2011 | Chongqing | ≥80 | PADL ** | 227 | 131 (57.71) | NR | 84 | 37.00 | 9 |
| 30. | Zhang et al. [56] | 2016 | EN | 2013 | Shanghai | ≥60 (72.1) | IADL | 8237 | 4473 (53.26) | NR | 1360 | 16.51 | 7 |
| 31. | Gong [57] | 2016 | CH | 2014 | Shanghai | ≥60 | PADL + IADL | 1233 | NR | NR | 226 | 18.33 | 6 |
| 32. | Zhong [58] | 2016 | CH | 2012–2014 | Guangdong | ≥60 | PADL | 1706 | NR | NR | 331 | 19.40 | 7 |
| 33. | Liu et al. [59] | 2016 | EN | 2013 | Beijing | ≥60 (71.4) | PADL | 1036 | 522 (50.40) | NR | 219 | 21.10 | 7 |
| 34. | Peng and Wu [60] | 2016 | CH | 2011 | National | ≥65 | PADL | 9097 | 4918 (54.06) | 4755 (52.27) | 1948 | 21.41 | 10 |
| 35. | Huang et al. [61] | 2016 | CH | 2013–2015 | Zhejiang | ≥60 (73.8) | PADL | 883 | 490 (55.49) | NR | 191 | 21.63 | 8 |
| 36a | Su et al. [62] | 2016 | EN | 2013 | Shanghai | ≥80 | PADL | 2058 | 1191 (57.87) | NR | 478 | 23.23 | 7 |
| 36b. | Su et al. [62] | 2016 | EN | 2013 | Shanghai | ≥80 | IADL | 2058 | 1191 (57.87) | NR | 780 | 37.90 | 7 |
| 37. | Yue and Liu [63] | 2016 | CH | 2011 | National | ≥65 | PADL | 5118 | 2861 (55.90) | NR | 1214 | 23.72 | 10 |
| 38. | Chen et al. [64] | 2016 | CH | 2014 | Shanghai | ≥60 (74.2) | PADL + IADL | 3556 | 2114 (59.45) | NR | 879 | 24.72 | 8 |
| 39. | Yi et al. [65] | 2016 | CH | 2013 | Hubei | ≥65 (73.3) | PADL + IADL ** | 4002 | 2058 (51.42) | 4002(100.00) | 1375 | 34.36 | 8 |
| 40. | Zhang et al. [66] | 2016 | CH | 2014* | Hebei | ≥60 (68.7) | PADL + IADL ** | 2548 | 1322 (51.88) | 1350 (52.98) | 1076 | 42.23 | 7 |
| 41. | Zhai et al. [67] | 2016 | CH | 2011 | Shandong | ≥65 | PADL + IADL | 1355 | 706 (52.10) | 729 (53.80) | 921 | 67.97 | 10 |
| 42. | Luo et al. [68] | 2016 | CH | 2011 | Shandong, Henan, Hebei, Hunan, Guangdong, Guangxi, Hainan, Jiangsu | ≥65 | PADL ** | 2227 | 1227 (55.10) | NR | 553 | 24.83 | 10 |
| 43. | Dong et al. [5] | 2017 | EN | 2011 | Shanghai | ≥60 (71.6) | PADL | 1997 | 1153 (57.74) | NR | 37 | 1.85 | 6 |
| 44a. | Zhang et al. [69] | 2017 | EN | 2005–2014 | National | ≥65 (72.0) | PADL | 26,604 | 13,515 (50.80) | 16,022 (60.22) | 1862 | 7.00 | 9 |
| 44b. | Zhang et al. [69] | 2017 | EN | 2005–2014 | National | ≥65 (72.0) | IADL | 26,604 | 13,515 (50.80) | 16,022 (60.22) | 8513 | 32.00 | 9 |
| 45. | Zhou and Ma [70] | 2017 | CH | 2013 | National | ≥60 (68.9) | PADL | 7629 | 3988 (52.27) | 7629 (100.00) | 668 | 8.76 | 9 |
| 46. | Ding and Wang [71] | 2017 | CH | 2014 | National | 60–79 (67.7) | PADL + IADL | 6959 | 3549 (50.99) | 3897 (56.00) | 1038 | 14.92 | 9 |
| 47. | Jin [72] | 2017 | CH | 2011 | National | ≥60 | PADL ** | 9765 | NR | NR | 2084 | 21.34 | 9 |
| 48. | Li et al. [73] | 2017 | CH | 2013 | Anhui | ≥60 (72.3) | PADL + IADL ** | 746 | 438 (58.71) | NR | 211 | 28.28 | 9 |
| 49. | Hao et al. [74] | 2017 | EN | 2016 | Beijing | ≥60 | PADL + IADL | 1083 | 543 (50.14) | NR | 347 | 32.04 | 8 |
| 50. | Liu et al. [75] | 2017 | CH | 2016 | Shandong | ≥65 | PADL ** | 1196 | NR | NR | 404 | 33.78 | 8 |
| 51. | Wang et al. [76] | 2017 | CH | 2015* | Hebei | ≥60 (75.5) | PADL + IADL ** | 724 | 378 (52.20) | NR | 309 | 42.68 | 6 |
| 52a. | Hu et al. [77] | 2017 | CH | 2014 | National | ≥65 (66.4) | PADL ** | 6168 | 2813 (45.61) | NR | 1517 | 24.59 | 8 |
| 52b. | Hu et al. [77] | 2017 | CH | 2014 | National | ≥65 (66.4) | IADL ** | 6168 | NR | NR | 3864 | 62.65 | 8 |
| 53. | Wu et al. [78] | 2017 | EN | 2010 | Chongqing | ≥100 | PADL | 564 | 471 (83.51) | 564 (100.00) | 370 | 65.60 | 9 |
| 54. | Yang et al. [79] | 2018 | EN | 2015–2016 | Hubei | ≥65 (72.6) | PADL ** | 2096 | 1065 (50.81) | NR | 149 | 7.11 | 8 |
| 55. | Liu et al. [80] | 2018 | CH | 2013 | National | ≥60 | PADL ** | 8751 | NR | NR | 842 | 9.62 | 8 |
| 56. | Ding and Yan [81] | 2018 | CH | 2011 | National | ≥60 | PADL | 7626 | 3801 (49.84) | 5765 (75.60) | 845 | 11.08 | 8 |
| 57a. | Chen et al. [82] | 2018 | EN | 2016–2017 | Guangxi | ≥60 | PADL | 2300 | 1350 (58.70) | NR | 266 | 11.57 | 7 |
| 57b. | Chen et al. [82] | 2018 | EN | 2016–2017 | Guangxi | ≥60 | IADL | 2300 | 1350 (58.70) | NR | 976 | 42.43 | 7 |
| 57c. | Chen et al. [82] | 2018 | EN | 2016–2017 | Guangxi | ≥60 | PADL + IADL | 2300 | 1350 (58.70) | NR | 998 | 43.39 | 7 |
| 58. | Zhai et al. [83] | 2018 | CH | 2016* | Shanghai | ≥60 | PADL + IADL | 4003 | 2257 (56.38) | NR | 473 | 11.82 | 7 |
| 59. | Liu et al. [84] | 2018 | CH | 2010–2014 | Beijing | ≥60 (70.3) | PADL | 4499 | 2684 (59.66) | 2397 (53.28) | 544 | 12.10 | 8 |
| 60. | Xu et al. [85] | 2018 | CH | 2016 | Sichuan | ≥60 | PADL | 890 | 577 (64.83) | NR | 119 | 13.37 | 9 |
| 61. | Wu et al. [86] | 2018 | CH | 2016* | Beijing | ≥60 | PADL + IADL | 1158 | 713 (61.57) | NR | 220 | 19.00 | 8 |
| 62. | Fu et al. [87] | 2018 | EN | 2014 | Hubei | ≥65 (74.3) | PADL + IADL | 1210 | 672 (55.54) | NR | 249 | 20.58 | 7 |
| 63. | Liu et al. [88] | 2018 | EN | 2016* | Hubei | ≥65 | PADL + IADL | 622 | 358 (57.56) | NR | 179 | 28.78 | 6 |
| 64. | Gu and Feng [89] | 2018 | EN | 2000–2009 | National | ≥65 (88.1) | PADL ** | 32,281 | 18,914 (58.59) | NR | 9361 | 29.00 | 9 |
| 65a. | Hou et al. [90] | 2018 | EN | 1998 | National | ≥80 (92.0) | PADL | 8768 | 5240 (59.76) | 5455 (62.21) | 3236 | 36.91 | 10 |
| 65b. | Hou et al. [90] | 2018 | EN | 2000 | National | ≥80 (91.1) | PADL | 10,940 | 6356 (58.10) | 4181 (38.22) | 3805 | 34.78 | 10 |
| 65c. | Hou et al. [90] | 2018 | EN | 2002 | National | ≥80 (92.3) | PADL | 10,905 | 6579 (60.33) | 5785 (53.05) | 4414 | 40.48 | 10 |
| 65d. | Hou et al. [90] | 2018 | EN | 2005 | National | ≥80 (92.5) | PADL | 10,393 | 6260 (60.23) | 5723 (55.07) | 3516 | 33.83 | 10 |
| 65e. | Hou et al. [90] | 2018 | EN | 2008 | National | ≥80 (92.4) | PADL | 11,658 | 7074 (60.68) | 7016 (60.18) | 3318 | 28.46 | 10 |
| 66. | Bai et al. [91] | 2018 | CH | 2013 | Hebei | ≥60 | PADL + IADL | 1374 | 785 (57.13) | NR | 584 | 42.50 | 7 |
| 67. | Gong et al. [92] | 2018 | EN | 2016* | Anhui | ≥60 (70.7) | PADL + IADL | 3182 | 1862 (58.52) | 3182 (100.00) | 1942 | 61.03 | 6 |
| 68. | Dong et al. [93] | 2018 | EN | 2014 | Anhui | ≥60 | PADL + IADL | 945 | 580 (61.38) | 945 (100.00) | 599 | 63.39 | 9 |
| 69a. | Zhang et al. [94] | 2019 | CH | 2015 | Beijing, Shanghai, Hebei, Sichuan, Yunnan, Guangxi | ≥60 | PADL | 23,803 | 13,234 (55.60) | 11,029 (46.33) | 500 | 2.10 | 9 |
| 69b. | Zhang et al. [94] | 2019 | CH | 2015 | Beijing, Shanghai, Hebei, Sichuan, Yunnan, Guangxi | ≥60 | IADL | 23,803 | 13,234 (55.60) | 11,029 (46.33) | 4570 | 19.20 | 9 |
| 79. | Li et al. [95] | 2019 | CH | 2015 | Fujian | ≥60 | PADL ** | 5174 | 2716 (52.49) | NR | 280 | 5.41 | 9 |
| 71. | Liu et al. [96] | 2019 | CH | 2016–2017 | Hebei | ≥60 | PADL + IADL | 3125 | 1670 (53.44) | NR | 324 | 10.37 | 8 |
| 72. | Fu et al. [97] | 2019 | CH | 2017 * | Sichuan | ≥60 | PADL ** | 1000 | 562 (56.20) | NR | 158 | 15.80 | 7 |
| 73. | Chen et al. [98] | 2019 | EN | 2016 | Jiangsu | ≥60 | PADL | 2493 | 1314 (52.71) | 1584 (63.54) | 402 | 16.13 | 7 |
| 74. | Chen et al. [99] | 2019 | EN | 2014 | National | ≥80 | PADL | 4076 | 2308 (56.62) | 2259 (55.42) | 1083 | 26.57 | 9 |
| 75. | Xu et al. [100] | 2019 | CH | 2017 | Hunan | ≥60 | PADL + IADL ** | 194 | NR | 194 (100.00) | 55 | 28.35 | 8 |
| 76. | Bai et al. [101] | 2019 | CH | 2016–2017 | Hebei | ≥60 | PADL + IADL ** | 6171 | 3024 (49.00) | NR | 2489 | 40.33 | 9 |
| 77. | Ma et al. [102] | 2019 | CH | 2016–2017 | Hebei | ≥60 | PADL + IADL ** | 6171 | NR | NR | 2489 | 40.33 | 8 |
| 78. | Zhao et al. [103] | 2019 | CH | 2017 * | Hebei | ≥60 (75.5) | PADL + IADL | 724 | NR | NR | 309 | 42.68 | 7 |
| 79. | Yao et al. [6] | 2019 | CH | 2014–2016 | Hainan | ≥100 (102.8) | PADL | 940 | 765 (81.38) | NR | 670 | 71.28 | 9 |
| 80. | Chen et al. [104] | 2020 | CH | 2015 | National | ≥60 | PADL | 4485 | 2422 (54.00) | NR | 297 | 6.62 | 9 |
| 81. | Ning et al. [105] | 2020 | CH | 2018 | Shandong | ≥60 (69.9) | PADL | 3349 | 1715 (51.21) | NR | 229 | 6.84 | 9 |
| 82. | Xu et al. [106] | 2020 | CH | 2018 * | Hainan | ≥60 | PADL ** | 365 | 213 (58.36) | 221 (60.55) | 29 | 7.95 | 8 |
| 83. | Gu et al. [107] | 2020 | CH | 2018 | Jiangsu | ≥60 (69.4) | PADL | 3259 | 1644 (50.44) | 1544 (47.38) | 344 | 10.56 | 9 |
| 84. | Peng et al. [108] | 2020 | EN | 2018 | Guangdong | ≥60 (71.6) | PADL | 1321 | NR | NR | 160 | 12.11 | 8 |
| 85. | Xu et al. [20] | 2020 | EN | 2018 | Ningxia | ≥60 (70.5) | PADL | 1040 | 513 (49.33) | NR | 179 | 17.21 | 8 |
| 86. | Zhang et al. [109] | 2020 | CH | 2018* | Henan | ≥60 (70.9) | PADL | 5570 | 2825 (50.72) | 4074 (73.14) | 1139 | 20.45 | 6 |
| 87. | Cai et al. [110] | 2020 | CH | 2015 | Yunnan | ≥60 (70.9) | PADL + IADL | 3978 | 2213 (55.63) | 2000 (50.28) | 1017 | 25.57 | 9 |
| 88. | Song et al. [111] | 2020 | CH | 2014 | Shandong | ≥65 | PADL ** | 559 | 254 (45.44) | 312 (55.81) | 143 | 25.58 | 9 |
| 89. | Liu et al. [112] | 2020 | CH | 2015–2018 | Guangdong | ≥60 (74.3) | PADL + IADL ** | 221 | 104 (47.06) | NR | 58 | 26.24 | 9 |
| 90. | Du et al. [113] | 2020 | CH | 2016 | Anhui | ≥60 (71.7) | PADL | 983 | 527 (53.61) | NR | 312 | 31.74 | 10 |
| 91. | Zhang et al. [114] | 2020 | CH | 2016 | Chongqing | ≥65 | PADL + IADL ** | 1341 | 609 (45.41) | NR | 596 | 44.44 | 8 |
| 92. | Lin et al. [115] | 2020 | CH | 2018 * | Yunnan | ≥60 (76.7) | PADL | 182 | 118 (64.84) | NR | 96 | 52.75 | 8 |
| 93. | Xiao et al. [116] | 2021 | EN | 2018 | Guizhou, Yunnan, Sichuan, Xinjiang | ≥60 (69.4) | PADL | 3770 | NR | NR | 488 | 12.94 | 8 |
| 94. | Cheng and Yan [117] | 2021 | EN | 1998–2014 | National | ≥80 | PADL | 30,317 | 17,663 (58.26) | NR | 4884 | 16.11 | 10 |
| 95. | Gao et al. [118] | 2021 | CH | 2017 | Shandong | ≥60 (69.8) | PADL + IADL | 7070 | 4224 (59.75) | NR | 1603 | 22.67 | 9 |
| 96. | Chen et al. [119] | 2021 | CH | 2014 | National | ≥60 (70.5) | PADL | 6182 | 3305 (53.46) | 3337 (53.98) | 1517 | 24.54 | 9 |
| 97. | Yan et al. [120] | 2021 | CH | 2018 | National | ≥65 (85.6) | PADL | 15,771 | 8902 (56.45) | NR | 4196 | 26.61 | 10 |
* Survey year is the year the data were collected; if the survey year was not reported, the data was computed by subtracting two from the year of publication; ** Some studies did not indicate the source of the scale. We determined by the items and calculation methods used; CH = Chinese; EN = English; NR = not reported.
Author Contributions
Conceptualization, Z.-J.W. and P.-P.Z.; Collection, curation, and interpretation of data: Z.-L.G. and X.-J.D.; writing—original draft preparation, P.-P.Z.; writing—review and editing, P.-P.Z., H.-M.Y. and Z.-J.W.; supervision, Z.-J.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by UKRI’s Global Challenge Research Fund (ES/P011055/1).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All relevant data are within the paper.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.United Nations Department of Economic and Social Affairs/Population Division World Population Prospects: The 2017 Revision, Key Findings, and Advance Tables. 2017. [(accessed on 6 December 2021)]. Available online: https://esa.un.org/unpd/wpp/Publications/Files/WPP2017_KeyFindings.pdf.
- 2.National Bureau of Statistics The Outcome of the Seventh National Population Census. [(accessed on 6 December 2021)];2021 Available online: http://www.stats.gov.cn/tjsj/sjjd/202105/t20210512_1817336.html.
- 3.World Health Organization World Report on Disability. 2011. [(accessed on 6 December 2021)]. Available online: www.who.int/disabilities/world_report/2011/en/
- 4.The Central People’s Government of the People’s Republic of China China Releases the Results of the Second National Sample Survey on Disability. [(accessed on 6 December 2021)];2007 Available online: http://www.gov.cn/jrzg/2007-05/28/content_628517.htm.
- 5.Dong W., Wan J., Xu Y., Chen C., Bai G., Fang L., Sun A., Yang Y., Wang Y. Determinants of self-rated health among shanghai elders: A cross-sectional study. BMC Public Health. 2017;17:807. doi: 10.1186/s12889-017-4718-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yao Y., Fu S.H., Zhang C., Lv F.Q., Zhang F., Luan F.X., Zhao Y.L. A study of health status in Hainan centenarians. Chin. J. Geriatr. 2019;38:1413–1417. (In Chinese) [Google Scholar]
- 7.Li T., Liu B.Y., Wang J.Y., Wang J., Wu X., Liu B.Y. Meta-analysis on the impaired rate of activities of daily living in the Chinese elderly aged 60 or above from 2010 to 2017. Chin. J. Gerontol. 2020;40:2439–2442. (In Chinese) [Google Scholar]
- 8.Wang Z.J., Liu B., Guo Z.Y., Yang H.M. Meta-analysis on the disability of the elderly in China. Chin. J. Gerontol. 2020;40:1671–1674. (In Chinese) [Google Scholar]
- 9.Shao P. A meta-analysis on the activities of daily living of the Chinese elderly from 2004 to 2014. Chin. J. Gerontol. 2017;37:3865–3866. (In Chinese) [Google Scholar]
- 10.World Health Organization . International Classification of Functioning, Disability and Health: ICF. WHO; Geneva, Switzerland: 2001. [Google Scholar]
- 11.Barberger-Gateau P., Rainville C., Letenneur L., Dartigues J.-F. A hierarchical model of domains of disablement in the elderly: A longitudinal approach. Disabil. Rehabil. 2000;22:308–317. doi: 10.1080/096382800296665. [DOI] [PubMed] [Google Scholar]
- 12.Salvador-Carulla L., Gasca V.I. Defining disability, functioning, autonomy and dependency in person-centered medicine and integrated care. Int. J. Integr. Care. 2010;10:e025. doi: 10.5334/ijic.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katz S., Ford A.B., Moskowitz R.W., Jackson B.A., Jaffe M.W. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 14.Mahoney F.I., Barthel D.W. Functional evaluation: The barthel index. Md. State Med. J. 1965;14:61–65. [PubMed] [Google Scholar]
- 15.Lawton M.P., Brody E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. doi: 10.1093/geront/9.3_Part_1.179. [DOI] [PubMed] [Google Scholar]
- 16.Rostom A., Dubé C., Cranney A., Saloojee N., Sy R., Garritty C., Sampson M., Zhang L., Yazdi F., Mamaladze V., et al. Celiac Disease. Evid. Rep./Technol. Assess. 2004:1–6. [PMC free article] [PubMed] [Google Scholar]
- 17.Borenstein M., Hedges L.V., Higgins J.P., Rothstein H.R. Introduction to Meta-Analysis || When Does It Make Sense to Perform a Meta-Analysis? John Wiley & Sons; Chichester, UK: 2009. [DOI] [Google Scholar]
- 18.Wu X.L., Liu J., Dong T.Y. Longitudinal dynamic analysis of Chinese Elderly’s activities of daily living. Sci. Res. Aging. 2018;6:28–45. (In Chinese) [Google Scholar]
- 19.Chen F., Liu K. The activities of daily living of the older adults in the community and its influencing factors. Chin. J. Gerontol. 2015;35:4662–4664. (In Chinese) [Google Scholar]
- 20.Xu X., Yang L., Miao X., Hu X.Y. An investigation and analysis of the activities of daily living of older adults living at home in Ningxia Hui Autonomous Region of China: A cross-sectional study. BMC Geriatr. 2020;20:369. doi: 10.1186/s12877-020-01765-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chalise H.N., Saito T., Kai I. Functional disability in activities of daily living and instrumental activities of daily living among Nepalese Newar elderly. Public Health. 2008;122:394–396. doi: 10.1016/j.puhe.2007.07.015. [DOI] [PubMed] [Google Scholar]
- 22.Ma L.N., Li Z.Z., Tang Z., Sun F., Diao L.J., Li J., He Y., Dong B.R., Li Y. Prevalence and socio-demographic characteristics of disability in older adults in China: Findings from China Comprehensive Geriatric Assessment Study. Arch. Gerontol. Geriat. 2017;73:199–203. doi: 10.1016/j.archger.2017.07.029. [DOI] [PubMed] [Google Scholar]
- 23.Modig K., Andersson T., Vaupel J., Rau R., Ahlbom A. How long do centenarians survive? Life expectancy and maximum lifespan. J. Intern. Med. 2017;282:156–163. doi: 10.1111/joim.12627. [DOI] [PubMed] [Google Scholar]
- 24.Thompson S.G. Why sources of heterogeneity in meta-analysis should be investigated. Br. Med. J. 1994;309:1351–1355. doi: 10.1136/bmj.309.6965.1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Egger M., Smith G.D., Altman D.G. Systematic Reviews in Health Care: Meta-Analysis in Context. BMJ Publishing Group; London, UK: 2001. [Google Scholar]
- 26.Gerta R., Guido S., James R.C., Martin S. Undue reliance on I2 in assessing heterogeneity may mislead. BMC Med. Res. Methodol. 2008;8:79. doi: 10.1186/1471-2288-8-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang S.Z., Zhou J.C. A preliminary study of the ability of the elderly to move in daily life and related factors. Sichuan Ment. Health. 1993;6:112–114. (In Chinese) [Google Scholar]
- 28.Meng J.M., Xiang M.J., Zhu H. Prevalence of Physical Dependence and Factors Related in Beijing Elderly. Geriatr. Health Care. 1996;2:1–4. (In Chinese) [Google Scholar]
- 29.Tang Z., Wang H.X., Meng C., Wu X.G., Ericsson K., Winblad B., Pei J.J. The prevalence of functional disability in activities of daily living and instrumental activities of daily living among elderly Beijing Chinese. Arch. Gerontol. Geriat. 1999;29:115–125. doi: 10.1016/S0167-4943(99)00026-6. [DOI] [PubMed] [Google Scholar]
- 30.Lv H., Li S., Ni Z.Z. The status of chronic conditions among the elderly and the influencing factors related to ADL of old people. Acta Univ. Med. Nahui. 2001;36:29–32. (In Chinese) [Google Scholar]
- 31.Meng C., Xiang M.J. Epidemiological status and prospect of daily life activity in Beijing. Int. J. Med. 2002;6:63–65. (In Chinese) [Google Scholar]
- 32.Wang M.H., Liu Q., Yang J.R. Related Factors Analysis on Dependency of Activities of Daily Life for the Elderly. Chin. J. Public Health. 2002;18:107–109. (In Chinese) [Google Scholar]
- 33.Lin H., Zhang T.H., Yang H., Wang C.B., Liu N., Zhang X.P., Gong G.C. Analysis of Influential Factors of Activities of Daily Life of the Elderly. Chin. Health Serv. Manag. 2002;18:495–497. (In Chinese) [Google Scholar]
- 34.Ji J., Zhang H., Geng Q. Relative Analysis on the Depression and ADL Function of the Elderly. China J. Health Psychol. 2007;11:1031–1032. (In Chinese) [Google Scholar]
- 35.Yin D.T., Lu J.H. Hierarchical Linear Model Approach to the Determinants of Activities of Daily Living of Chinese Oldest Old at Both Individual and Regional levels. Chin. J. Popul. Resour. 2007;5:31–41. doi: 10.1080/10042857.2007.10677529. [DOI] [Google Scholar]
- 36.Huang W.Y., Yang J.Y., Yang X., Cai Y.Y., Wang J.H. The relationship between chronic diseases and daily life function of the elderly in Guiyang community. J. Guiyang Med. Coll. 2008;33:132–135. (In Chinese) [Google Scholar]
- 37.Tang Y., Xue G.E., Chen Z.Y. A Survey of Self-Care Ability in Elderly People of Ethnic Minority Area of Western Hunan Province. Chin. Gen. Pract. 2009;12:1783–1784. (In Chinese) [Google Scholar]
- 38.Xu X.Q., Dong B., Zhou W., Li Y.J., Liu J., Wang S.H., Jiang Z.Q. A Study on Activities of Daily Living and Its Risk Factors of the Aged in the Rural Areas. Zhejiang J. Prev. Med. 2011;23:1–3. (In Chinese) [Google Scholar]
- 39.Chen X.P., Fan Y.F., Xu H., Cao J.X., Lu Y.M. Survey on living status and long-term care of aged citizens in Hangzhou city. J. Nurs. Sci. 2011;26:86–89. (In Chinese) [Google Scholar]
- 40.Li N., Pang L.H., Chen G., Song X.M., Zhang J., Zheng X.Y. Risk factors for depression in older adults in Beijing. Can. J. Psychiat. 2011;56:466–473. doi: 10.1177/070674371105600804. [DOI] [PubMed] [Google Scholar]
- 41.Xue B., Chen X.B., Ding D.X., Shen Q., Mou Y.Y., Zhong G.J. Survey and influencing factors on chronic diseases and daily life ability of the elderly. Chin. J. Gerontol. 2011;31:4431–4432. (In Chinese) [Google Scholar]
- 42.Li Y.T., Feng X.S., Yang F.H., Gu X.Y., Zong W.H. The Evaluation and Risk Factors of ADL among the Elderly People in Zhabei District. Chin. Prim. Health Care. 2012;26:42–44. (In Chinese) [Google Scholar]
- 43.Shi H.W., Song A.Q., Guo L.Y., Zhai J.H., Wang W.J., Kang D.M. Assessment on the Ability in Activity of Daily Living Among the Urban Elderly in Jining City, 2011. Prev. Med. Trib. 2012;18:203–205. (In Chinese) [Google Scholar]
- 44.Li W.P., Liu L., Song Q.R., Zhang Y.H., Wang H., Gong A.H. Analysis on the life quality of over 60-year elderly in Litong district of Wuzhong. Ningxia Med. J. 2012;34:642–644. (In Chinese) [Google Scholar]
- 45.Zhang J.Y., Chang Y., Hu G.Y., Wu X.H., Li Y.H. A survey on the correlation between daily life ability and cognitive function in the elderly. Chin. J. Misdiagn. 2012;12:1642. (In Chinese) [Google Scholar]
- 46.Yu Q., Li H., Zhang X., Gong Q.Q., Xu D.H., Zhou J.H. Survey of the needs of the elderly and community care for the elderly who are inaction in the Caohejing community. Shanghai Med. Pharm. J. 2012;33:45–47. (In Chinese) [Google Scholar]
- 47.Huang W., Ge X.J., Hou S., Gao G.P., Zhang X.J., Yu Y.L. Ability of daily living and its influencing factors among rural elderly in Dabieshan Mountain area. Chin. J. Public Health. 2012;28:884–886. (In Chinese) [Google Scholar]
- 48.Yin Z.Q., Yang Y.X., Chen L.L., Tu H.X., Chen J. Health status and its influential factors among rural elderly in Zhejiang province. Chin. J. Public Health. 2012;28:293–295. (In Chinese) [Google Scholar]
- 49.Zhang W.J., Wei M. A Study on the Factors Associated with Preferences for Institutional Care of the Elderly in Urban China: Evidences from Xicheng District of Beijing. Popul. Econ. 2014;6:22–34. (In Chinese) [Google Scholar]
- 50.Zhong Y.Q., Wang J., Zhang G.J. Analysis on ability of daily living and its influence factors among the elderly. Mod. Prev. Med. 2014;41:852–855. (In Chinese) [Google Scholar]
- 51.Yin Z., Shi X., Kraus V.B., Brasher M.S., Chen H., Liu Y., Lv Y., Zeng Y. Gender-Dependent Association of Body Mass Index and Waist Circumference with Disability in the Chinese Oldest. Obesity. 2014;22:1918–1925. doi: 10.1002/oby.20775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chen W., Hao S.C., Mao F.Z., Fang Y. Research on the Situation of Elderly Disability and its Impact Factors in Xiamen. Chin. J. Health Stat. 2015;32:770–773. (In Chinese) [Google Scholar]
- 53.Li Y., Yang C., Li W.P., Wang X.X., Song Q.R. Activity of daily living and its influencing factors of people over 60, Yinchuan. Mod. Prev. Med. 2015;42:1621–1623. (In Chinese) [Google Scholar]
- 54.Li W.F., Yuan C.J. Study on long-term care needs and influencing factors of the elderly. Shandong Soc. Sci. 2015;12:67–72. (In Chinese) [Google Scholar]
- 55.Zhang C.H., Wang Y.L., Ding X.B., Mao D.Q., Lv X.Y., Jiao Y., Qi L., Shen Z.Z. The investigation of activities of daily living (ADL) and chronic non-communicable diseases (NCD) for people over age of 80 in Chongqing City. Chin. J. Dis. Control Prev. 2015;19:894–896. (In Chinese) [Google Scholar]
- 56.Zhang W., Ding H., Su P., Duan G., Chen R., Long J., Du L., Xie C., Jin C., Hu C., et al. Does disability predict attempted suicide in the elderly? A community-based study of elderly residents in Shanghai, China. Aging Ment. Health. 2015;20:81–87. doi: 10.1080/13607863.2015.1031641. [DOI] [PubMed] [Google Scholar]
- 57.Gong X.Q. The impact of living arrangement and social support on health services’ utilization among the elderly: Taking shanghai as an example. South China J. Econ. 2016;1:11–27. (In Chinese) [Google Scholar]
- 58.Zhong C.Y., Wu C.P., Huang S.Q., Li L.W., Ni D.J., Xia H.M. The investigation of the status quo of community disability elderly and their quality of life and family bed service needs. Heilongjiang Med. J. 2016;40:457–459. (In Chinese) [Google Scholar]
- 59.Liu T., Hao X., Zhang Z. Identifying community health care supports for the elderly and the factors affecting their aging care model preference: Evidence from three districts of Beijing. BMC Health Serv. Res. 2016;16:83–92. doi: 10.1186/s12913-016-1863-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Peng C., Wu M. Research and Analysis on Disability, Dementia and Long-Term Care among Chinese Elders. J. Prev. Med. Chin. People’s Lib. Army. 2016;34:382–384. (In Chinese) [Google Scholar]
- 61.Huang X.A., Lin J., Jiang X.F., Liang H.B., Liu X.L., Zang R., Wang D.D., Li J.R. An investigation on the situation of disability and its influencing factors among the elderly in community. Zhejiang J. Prev. Med. 2016;28:541–545. (In Chinese) [Google Scholar]
- 62.Su P., Ding H.S., Zhang W., Duan G.F., Yang Y.T., Chen R., Duan Z.J., Du L.X., Xie C.Y., Jin C.L., et al. The association of multimorbidity and disability in a community-based sample of elderly aged 80 or older in Shanghai, China. BMC Geriatr. 2016;16:178. doi: 10.1186/s12877-016-0352-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yue Z., Liu E.P. An empirical study on the influencing mechanisms of health services on rural elderly disability—based on the 2011 Chinese longitudinal healthy longevity survey data. J. China Agric. Univ. (Soc. Sci.) 2016;33:124–132. (In Chinese) [Google Scholar]
- 64.Chen J., Li W.X., Liu Y.X., Luo L., Hua G.C., Liang Y., Yu J.L., Deng H.J. Daily living activities of the elderly and their influencing factors in Putuo District. Chin. Health Resour. 2016;19:65–69. doi: 10.1186/s12960-021-00608-w. (In Chinese) [DOI] [Google Scholar]
- 65.Yi L.P., Zhang X.H., Wang K.Y., Sun B. Status of the daily living ability among people over 65 years old in rural mountainous area and its influence factors. J. Public Health Prev. Med. 2016;27:49–52. (In Chinese) [Google Scholar]
- 66.Zhang J., Li S.X., Chen C.X., Dou N., Zhang M., Shao T. The current status of the quality of life among the elderly in Tangshan. Chin. J. Gerontol. 2016;36:3306–3307. (In Chinese) [Google Scholar]
- 67.Zhai X.M., Zhu Q.L., Li H.Y., Li Y. The elderly disability situation and influencing factors in Shandong province. Chin. Nurs. Manag. 2016;16:1633–1638. (In Chinese) [Google Scholar]
- 68.Luo J.S., Yin Z.X., Lv Y.B., Wang J.L., Shi X.M. Association between the hypersensitive C-reactive protein and activities of daily living among elderly adults in longevity areas of China. Chin. J. Prev. Med. 2016;50:605–610. doi: 10.3760/cma.j.issn.0253-9624.2016.07.008. (In Chinese) [DOI] [PubMed] [Google Scholar]
- 69.Zhang X., Dupre M.E., Qiu L., Zhou W., Zhao Y., Gu D. Urban-rural differences in the association between access to health care and health outcomes among older adults in China. BMC Geriatr. 2017;17:151. doi: 10.1186/s12877-017-0538-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhou X.F., Ma Y.N. Prevalence and impact factors of disability among elderly people in rural China. Chin. J. Public Health. 2017;33:1665–1668. (In Chinese) [Google Scholar]
- 71.Ding B.R., Wang Y.J. From Body to Mind: Chinese Elderly People’s Disability Status and Happiness. Popul. Dev. 2017;23:82–90. (In Chinese) [Google Scholar]
- 72.Jin H. Social status and life care of disabled elderly: An analysis based on CLHLS 2011. Zhejiang Acad. J. 2017;2:45–50. (In Chinese) [Google Scholar]
- 73.Li C., Zhang X.L., Zhang P., Wang F.L., Dong L.S., Xing F.M. Ability of daily living and its influencing factors among community elderlies in Bengbu city. Chin. J. Public Health. 2017;33:991–993. (In Chinese) [Google Scholar]
- 74.Hao X., Gu J., Ying X., Bo T., Fu W. Social support and care needs of the disabled elderly population: An empirical study based on survey data from Beijing, China. Biosci. Trends. 2017;11:507–515. doi: 10.5582/bst.2017.01234. [DOI] [PubMed] [Google Scholar]
- 75.Liu X.Y., Song P., Liu X.X., Liu W.H. Investigation on physical function situation of long-term care of disabled elderly in community. Chin. Nurs. Res. 2017;31:3875–3876. (In Chinese) [Google Scholar]
- 76.Wang F.L., Zhang L.N., Zhang P., Sun S.F., Dong S.L., Zhang X.L., Xing F.M., Liu X.W., Guo X.W. Survey and analysis on the requirements for elderly care service among elderlies with different ADL. Mod. Prev. Med. 2017;44:1044–1046. (In Chinese) [Google Scholar]
- 77.Hu H.W., Li Y.Y., Zhang C., Zhang J.X. Participation of Social Activities, Health Promotion and Disability Prevention: Empirical Analysis based on Active Ageing Structure. Chin. J. Popul. Sci. 2017;4:87–96. (In Chinese) [Google Scholar]
- 78.Wu T.T., Lu L., Luo L., Guo Y.Q., Ying L.Y., Tao Q.L., Zeng H., Han L.L., Shi Z.M., Zhao Y. Factors Associated with Activities of Daily Life Disability among Centenarians in Rural Chongqing, China: A Cross-Sectional Study. Int. J. Environ. Res. Public Health. 2017;14:1364. doi: 10.3390/ijerph14111364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yang M., Guo Y., Gong J., Deng M., Yang N., Yan Y. Relationships between functional fitness and cognitive impairment in Chinese community-dwelling older adults: A cross-sectional study. BMJ Open. 2018;8:e020695. doi: 10.1136/bmjopen-2017-020695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Liu D., Dai T., Huang J. Demand and utilization of medical service among home-dwelling elderly with disability in China: 2011–2015. Chin. J. Public Health. 2018;34:687–689. (In Chinese) [Google Scholar]
- 81.Ding H., Yan J. Research on Disability Rate Estimation of Chinese Elderly and Its Trend. Chin. J. Popul. Sci. 2018;3:97–108. (In Chinese) [Google Scholar]
- 82.Chen S.Y., Qin J., Li Y., Wei Y., Long B.S., Cai J.S., Tang J.X., Xu X., Yu G.Q., Zhang Z.Y. Disability and Its Influencing Factors among the Elderly in a County, Guangxi Province, China. Int. J. Environ. Res. 2018;15:1967. doi: 10.3390/ijerph15091967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zhai X.T., Huang L.M., Ruan Y., Huang Z.Z., Fei J.H., Ding G.M., Qi S.G., Wang Z.H. Status of elderly daily life ability in Songjiang District, Shanghai. Shanghai J. Prev. Med. 2018;30:320–323. (In Chinese) [Google Scholar]
- 84.Liu M., Wang J.H., Yang S.S., Yao Y., Wang S.S., He Y. Daily activities of the elderly in Beijing community and comparison between urban and rural areas. Chin. J. Epidemiol. 2018;39:268–272. doi: 10.3760/cma.j.issn.0254-6450.2018.03.004. (In Chinese) [DOI] [PubMed] [Google Scholar]
- 85.Xu X.F., Chen Q., Hu X.Y. Analysis on the present situation and influencing factors of the self-care ability of the elderly living at home in Chengdu. Chin. J. Mod. Nurs. 2018;24:2267–2270. (In Chinese) [Google Scholar]
- 86.Wu F.Q., Fan H., Xiao S.Q., Yang X., Xiao Y.Y., Wu Y. The demand for care and its influencing factors in community-dwelling disabled elderly in Beijing. Chin. J. Nurs. 2018;53:841–845. (In Chinese) [Google Scholar]
- 87.Fu C., Yang F., Mao Z. Factors associated with cognitive decline among elderly in Wuhan, China living alone versus those living with children. Southeast Asian J. Trop. Med. Public Health. 2018;49:696–706. [Google Scholar]
- 88.Liu X., Yin X., Tan A., He M., Jiang D., Hou Y., Lu Y., Mao Z. Correlates of Mild Cognitive Impairment of Community-Dwelling Older Adults in Wuhan, China. Int. J. Environ. Res. Public Health. 2018;15:2705. doi: 10.3390/ijerph15122705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gu D., Feng Q. Psychological resilience of Chinese centenarians and its associations with survival and health: A fuzzy set analysis. J. Gerontol. B-Psychol. 2018;73:880–889. doi: 10.1093/geronb/gbw071. [DOI] [PubMed] [Google Scholar]
- 90.Hou C., Ping Z., Yang K., Chen S., Liu X., Li H., Liu M., Halmlutterod N.V., Tao L. Trends of Activities of Daily Living Disability Situation and Association with Chronic Conditions among Elderly Aged 80 Years and Over in China. J. Nutr. Health Aging. 2018;22:439–445. doi: 10.1007/s12603-017-0947-7. [DOI] [PubMed] [Google Scholar]
- 91.Bai Y.P., Wang Q., Jin R., Zhang X.L., Wang F.L., Xing F.M. The present situation of the elderly at home in Hebei Province and its relationship with living habits and physical condition. Chin. J. Gerontol. 2018;38:201–203. (In Chinese) [Google Scholar]
- 92.Gong F.F., Zhao D.D., Zhao Y.Y., Lu S.S., Qian Z.Z., Sun Y.H. The factors associated with geriatric depression in rural China: Stratified by household structure. Psychol. Health Med. 2018;23:593–603. doi: 10.1080/13548506.2017.1400671. [DOI] [PubMed] [Google Scholar]
- 93.Dong B., Li J., Zhao D.D., Yu D.D., Ren Q.Q., Sun Y.H. The associated factors for the quality of life among Chinese rural elderly: 1-year follow-up study. J. Public Health-Heid. 2018;26:185–193. doi: 10.1007/s10389-017-0852-x. [DOI] [Google Scholar]
- 94.Zhang H., Wang Z.H., Wang L.M., Qi S.G., Li Z.X. Survey on the disability of the elderly residents in Chinese community. Chin. J. Epidemiol. 2019;3:266–271. (In Chinese) [Google Scholar]
- 95.Li Z., Xu H.N., Wang D.W. Care demand and its determinants among community disabled elderly in Fujian province. Chin. J. Public Health. 2019;35:1205–1209. (In Chinese) [Google Scholar]
- 96.Liu X.M., Chen C.X., Wang J.H. Analysis of frailty status and influencing factors of the elderly in community. Chin. Nurs. Res. 2019;33:390–393. (In Chinese) [Google Scholar]
- 97.Fu M.X., Lin Q., Zhang M.X., Liu L.F. The population structure of disabled elderly in Chengdu and its enlightenment to long-term care service model. World Latest Med. Inf. 2019;19:225–228. (In Chinese) [Google Scholar]
- 98.Chen N., Li X., Yuan N., Zhou C.C., Wang C.Q. Utilization willingness of institutional care between disabled and non-disabled seniors: Evidence from Jiangsu, China. BMC Health Serv. Res. 2019;19:410. doi: 10.1186/s12913-019-4259-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chen N., Li X., Wang J., Zhou C.C., Wang C.Q. Rural-urban differences in the association between disability and body mass index among the oldest-old in China. Arch. Gerontol. Geriat. 2019;81:98–104. doi: 10.1016/j.archger.2018.12.002. [DOI] [PubMed] [Google Scholar]
- 100.Xu R.X., Mao K., Wang K.D., Gong F., Zhang J., Wang W.H. The present situation of the daily living activities of the elderly in rural areas. Chin. J. Gerontol. 2019;39:5837–5840. (In Chinese) [Google Scholar]
- 101.Bai J.W., Ma X.B., Chen C.X. Disability Status of Community-dwelling Elderly and the Influence of Chronic Diseases on Them. Chin. Gen. Pract. 2019;22:43–47. (In Chinese) [Google Scholar]
- 102.Ma X.B., Bai J.W., Chen C.X. Disability status of the elderly in community and its influence on the behavior of seeking medical care. Chin. J. Gerontol. 2019;39:4079–4081. (In Chinese) [Google Scholar]
- 103.Zhao M., Zhang X.L., Han H., Wang F.L., Xing F.M. Influence of different health for the home endowment needs of elderly people. Chin. J. Gerontol. 2019;39:189–192. (In Chinese) [Google Scholar]
- 104.Chen J.F., Xiao C.H., Fang M.W., Ma X. The influence of physical fitness on the activity of daily living in Chinese elderly. Chin. J. Epidemiol. 2020;41:220–225. doi: 10.3760/cma.j.issn.0254-6450.2020.02.015. (In Chinese) [DOI] [PubMed] [Google Scholar]
- 105.Ning P., Du E.Q., Du C.J., Meng Q.H., Wu B.Y. Prevalence of the disability and inflection point age of the disability level change, Shandong Province. Mod. Prev. Med. 2020;47:1633–1636. (In Chinese) [Google Scholar]
- 106.Xu S., Huang X.L., Yan J.W., Li T., Gao F., Chen C.L. Analysis on the Self-care Ability of the Elderly in Haikou and Its Influencing Factors. Jiangsu Health Syst. Manag. 2020;31:1672–1676. (In Chinese) [Google Scholar]
- 107.Gu X.Y., Xu A.J., Dai S.Y., Chen A.Q. Study on the ability of daily life activities and its influencing factors among the elderly in Jiangsu province. Chin. J. Health Educ. 2020;36:821–825. (In Chinese) [Google Scholar]
- 108.Peng X., Bao X.Y., Xie Y.X., Zhang X.X., Huang J.X., Liu Y., Cheng M.J., Liu N., Wang P.X. The mediating effect of pain on the association between multimorbidity and disability and impaired physical performance among community-dwelling older adults in southern China. Aging Clin. Exp. Res. 2020;32:1327–1334. doi: 10.1007/s40520-019-01324-1. [DOI] [PubMed] [Google Scholar]
- 109.Zhang T.T., Tian Q.F., Cao M., Huang J.Y., Guo Q. The Study on the activity of daily living of the elderly in Henan Province and the inflection point of attenuation. Mod. Prev. Med. 2020;47:4129–4132. (In Chinese) [Google Scholar]
- 110.Cai Y.N., Xiao Y.Z., Zhang H.M. Impairment and influencing factors of ability in activities of daily living among residents aged 60 years and over in Yunnan Province. South China J. Prev. Med. 2020;46:205–209. (In Chinese) [Google Scholar]
- 111.Song Y.Y., Yang H., Hu X.H. Self-care ability of the elderly in daily life and its influencing factors in Shandong Province. Chin. J. Hosp. Stat. 2020;27:268–271. (In Chinese) [Google Scholar]
- 112.Liu Q.Y., Chang J., Su X.M. Exploring the impact of disability and chronic disease on the elderly in community. Cap. Food Med. 2020;27:142–143. (In Chinese) [Google Scholar]
- 113.Du Z.P., Wang Q., Li Y.L., Lu J., Feng S., Biao Y.S., Cao H.J., Yang L.S., Tao F.B. Associations between chronic diseases and activities of daily living of elderly in Liu’an urban and rural communities. Acta Univ. Med. Anhui. 2020;55:1758–1762. (In Chinese) [Google Scholar]
- 114.Zhang L., Chen J., Lu L., Rong H.H., Peng Y. Influencing factors for activities of daily living in the elderly people in Chongqing. Prev. Med. 2020;32:22–26. (In Chinese) [Google Scholar]
- 115.Lin Y., Dong Z.J., Xu C.Z., Zhao Y.N., You D.Y., Zhang J.J. Survey on disability status, its influencing factors and correlation with health utility among elderly residents in urban communities of Kunming. J. Kunming Med. Univ. 2020;41:44–50. (In Chinese) [Google Scholar]
- 116.Xiao Y., Jia S., Zhao W., Zhang Y., Qiao R., Xia X., Hou L., Dong B.R. The combined effect of hearing impairment and cognitive impairment with health-related outcomes in Chinese older people. J. Nutr. Health Aging. 2021;25:783–789. doi: 10.1007/s12603-021-1623-5. [DOI] [PubMed] [Google Scholar]
- 117.Cheng G., Yan Y. Sociodemographic, health-related, and social predictors of subjective well-being among Chinese oldest-old: A national community-based cohort study. BMC Geriatr. 2021;21:124. doi: 10.1186/s12877-021-02071-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Gao Z.R., Xu L.Z., Hu F.F., Hong Z. Demand analysis of long-term care services for the elderly based on daily living ability assessment. Chin. J. Hosp. Adm. 2021;37:130–134. (In Chinese) [Google Scholar]
- 119.Chen L., Wei X.X., Wang F.L., Jing L.W., Xing F.M., Hao Z.M. Disability status and related factors among the elderly over 60 years old in China. Mod. Prev. Med. 2021;48:1241–1245. (In Chinese) [Google Scholar]
- 120.Yan W., He M.J., Lu Y., Chang F. Research on status quo and influencing factors of elderly disability in China based on CLHLS. Chin. Nurs. Res. 2021;35:1807–1811. (In Chinese) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.