Abstract
Periodontitis and chronic kidney disease are both chronic inflammatory diseases and share some common risk factors. This 3-month pilot study aimed to clarify whether non-surgical periodontal therapy is beneficial in clinical, biochemical, and microbiological conditions in patients with periodontitis and kidney failure. Kidney failure patients with moderate to severe periodontitis were recruited from two hospitals. Treatment group received non-surgical periodontal therapy, and control group received oral hygiene instruction only. Outcome assessments were conducted 1 and 3 months after treatment. Non-parametric tests were used to analyze the patient-level data. Periodontal site-level assessments were analyzed by Student t-test and paired t-test. Statistical significance was set at p-value < 0.05. A total of 11 subjects completed the study. There was no significant difference between groups in all-cause mortality, cardiovascular events, infection events, systemic parameters, and serum biomarkers. Comparing to control group, clinical periodontal parameters, gingival crevicular fluid interleukin-1β (IL-1β) level and periodontal pathogens showed significant improvement in the treatment group. Non-surgical periodontal treatment did not change systemic outcomes in kidney failure patients, but changed the local micro-environment.
Keywords: non-surgical periodontal treatment, renal dialysis, kidney failure
1. Introduction
Periodontitis is a chronic inflammatory disease which causes loss of periodontal tissues by bacterial infection [1]. Periodontal pathogens, such as Porphyromonas gingivalis (P. gingivalis), Treponema denticola (T. denticola), and Tannerella forsythia (T. forsythia), accumulating on tooth surfaces may not only induce local but systemic inflammatory reaction [2,3]. The eliciting of systemic pro-inflammatory cytokine production originating from the periodontal region may also aggravate the severity of systemic diseases including cardiovascular disease (CVD), diabetes, chronic kidney disease (CKD), rheumatoid arthritis, chronic obstructive pulmonary disease (COPD), etc. [4].
CKD is characterized by impairment of renal function and its related complications [5]. End-stage renal disease (ESRD), the most severe form of CKD, defined as patients with an estimated glomerular filtration rate (eGFR) < 15 mL/min per 1.73 m2, and a need for regular dialysis [5,6]. High prevalence of CKD burdens the financial expenditures and healthcare system in Taiwan and worldwide [7]. CKD is associated with persistent and chronic systemic inflammation which increases the risks of CVD, especially in patients with diabetes [8]. Meanwhile, CVD is the most common cause of mortality in patients with CKD.
The association between periodontitis and CKD has been reported over the last decade [9,10]. Both diseases have chronic inflammatory characteristics and share some common risk factors [10]. Elevated systemic inflammatory cytokines, such as Interleukin-1β (IL-1β), Interleukin-6 (IL-6), C-Reactive protein (CRP), and Tumor necrosis factor-α (TNF-α), were attributable to periodontitis have been documented by previous studies [11,12]. It could cause vascular endothelial dysfunction and further cardiovascular events [13,14]. A recent consensus report suggests that periodontal treatment could decrease systemic inflammatory response and incidence of cardiovascular events [13].
Until now, limited randomized-controlled clinical trial (RCT) studies comparing the outcomes in patients with ESRD after either non-surgical periodontal treatment or none have been published [15,16]. Much uncertainty still exists in the relationship between the intervention of periodontitis and risk of CKD complications. Therefore, in this study, we aimed to investigate the clinical, biochemical, and microbiological effect of non-surgical periodontal treatment in patients with periodontitis and ESRD.
2. Materials and Methods
2.1. Study Design
This is a 3-month pilot study conducted in Taipei Medical University Hospital (TMUH) and TMU-affiliated Shuang-Ho Hospital (TMU-SHH) from September 2017 till December 2019. For allocation of included participants, randomization was achieved by a computer-generated list. Only clinicians and study staff members were aware of group assignment, i.e., treatment group or control group. Ethical approval was obtained from TMU-JIRB, Taipei Medical University (N201604007). The study was conducted in accordance with the Helsinki Declaration, following CONSORT guidelines.
2.2. Periodontal Participants
As a preliminary study, all hemodialysis patients who were well-informed and signed their informed consent at the hemodialysis department of two hospitals were sent to dental screening for eligibility. Inclusion criteria were as follows: maintained hemodialysis thrice a week for at least 3 months [17]; aged 20 or more than 20; at least 5 natural retainable teeth; and generalized moderate to severe periodontitis according to AAP/CDC criteria [18]. Exclusion criteria were: active infection under antibiotic treatment within the past 4 weeks for preventing the influence of antibiotics to the baseline condition [19]; unable to receive dental treatment or complete the entire course of the study. Patients with other systemic diseases, such as diabetes or cardiovascular disease, were not excluded from this study. We collected the demographics and medical information from the electronic records in the two hospitals. The medical information included baseline blood pressure, body mass index (BMI), dialysis vintage, past medical history, smoking, and laboratory results.
2.3. Periodontal Examination
The participants underwent a full periodontal examination at the baseline and after 3 months. An additional periodontal examination for treatment group was performed 4 to 6 weeks after treatment. The following 5 periodontal parameters were collected: plaque index, periodontal probing depth (PD), gingival recession depth (REC), clinical attachment loss (CAL), bleeding on probing (BOP). Six measurement sites per tooth for plaque index, PD, REC, CAL, and BOP were recorded. The periodontal probe (PQ-W, Hu-Friedy, Chicago, IL, USA) was used for periodontal examination by two experienced periodontists.
2.4. Periodontal Intervention
Subjects in both groups received data collection and oral hygiene instruction at the baseline and at 3 months. Amoxicillin (2 g) for infection prophylaxis was prescribed prior to periodontal examination and treatment appointments [20]. In the treatment group, subjects received standard non-surgical periodontal therapy for removing supragingival and subgingival biofilm and dental calculus by certified periodontists. Re-evaluation of periodontal condition was carried out 4 to 6 weeks after treatment. In an attempt to eradicate or reduce periopathogenic bacterial levels in remaining deep pockets, subgingival minocycline gel (Sun Star, Osaka, Japan) delivery was conducted in sites of periodontal pocket depth remaining ≥ 5 mm [21].
2.5. Biochemical Examination
Blood samples were drawn for blood chemistry analysis. Inflammatory biomarkers including high-sensitivity CRP (hsCRP), TNF-α, IL-1β, IL-6, Pentraxin 3 (PTX3) in serum and gingival crevicular fluid (GCF) were measured at baseline and 3-month visits [22,23]. GCF samples were collected by using Periopaper strips (HARCO Electronics, Irvine, CA, USA) from the deepest periodontal pocket. According to the method of our previous study [24], prior to sampling, the test area was air-dried and isolated with gauze. The first paper strip was slipped into the gingival pocket 1 mm subgingivally for 5 s and discarded immediately in order to avoid contamination of saliva. A second paper strip was inserted in the selected site for another 30 s. The remaining paper strip was the dipped in a 200-μL phosphate-buffered saline container and stored at −80 °C. Routine blood chemistries were analyzed by a central laboratory in the hospital. The cytokine levels were analyzed by ELISA using commercially available kits (R&D Systems, Minneapolis, MN, USA).
2.6. Microbiological Analysis
Subgingival biofilm was sampled from the 3 deepest periodontal sites using sterile periodontal curette at baseline and 3-month visits for both groups. The subgingival biofilm samples were then suspended in TE buffer, vortexed and sonicated. The DNA was extracted from subgingival biofilm samples.
The subgingival biofilm samples were mixed with buffer RDD and Benzonase and incubated at 37 °C for 30 min, followed by digestion with Proteinase K and incubated for 30 min at 56 °C [25,26]. They were then homogenized in Lysis Buffer. DNA purification was performed using a QIAamp DNA Microbiome Kit (Qiagen), per manufacturer instructions. Next, 16S rRNA gene amplification and library construction were performed according to the protocols provided by Illumina. Nextera XT Index kit was used to add the Illumina sequencing adapters and dual–index barcodes to the amplicon targets. Quantification and quality of the sequencing libraries were checked using a QSep100 Analyzer (BiOptic Inc., New Taipei City, Taiwan). Lastly, the libraries were normalized and pooled in an equimolar ratio and sequenced with an Illumina Miseq platform with V3 chemistry.
2.7. 16. S rRNA Gene Sequence Analysis
Preprocessing of the raw reads includes the removal of universal primers and low-quality bases using cutadapt (v1.18) [27]. Then, the paired reads were processed and analyzed with the DADA2/phyloseq workflow in the R environment. The taxonomy assignment of the inferred amplicon sequence variants (ASVs) was performed using the SILVA reference database (v132) with a minimum bootstrap confidence of 80 [28]. Multiple sequence alignment of the ASVs was performed with DECIPHER (v2.8.1) and phylogenetic tree was constructed using RAxML (v8.2.11) [29,30]. The frequency table, taxonomy and phylogenetic tree information were used to create a phyloseq object for downstream bacterial community analyses using phyloseq (v1.24.2) [31]. The α-diversity indices were calculated using the estimate richness function from the phyloseq package. The R package GUniFrac was used to calculate the various versions of the UniFrac distances by determining the community dissimilarity between groups (β-diversity) [32]. Microbiota enrichment analysis was conducted using the Linear Dis-criminant Analysis (LDA) Effect Size method and visualized as cladogram by using GraPhlAn [33,34].
2.8. Outcome Measurement
Our primary outcomes were all-cause mortality, cardiovascular (CV) events, and infection events. Prespecified secondary outcomes included Hemoglobin A1c (HbA1c), cardiac function, and peripheral vessel evaluation. In addition, periodontal parameters, serum/GCF inflammatory biomarkers, and subgingival microbes were collected.
2.9. Statistical Analysis
Baseline clinical characteristics were analyzed by Mann–Whitney U test, except gender and periodontal severity, which were analyzed by Fisher’s exact test. Baseline periodontal parameters, plaque index, PD, REC, CAL, and BOP were analyzed in patient-level by Mann–Whitney U test. Paired t-test and Student t-test were used for comparing changes in PD, REC, and CAL in site-level between the baseline and 3-month visits, and between treatment and control groups. Primary and secondary outcomes were analyzed by Mann–Whitney U test. For evaluating changes in level of inflammatory biomarkers in serum and GCF, and microbials in subgingival biofilm, Wilcoxon signed-rank test and Mann–Whitney U test were used for intra-group and inter-groups comparison. Weighted UniFrac analyses was used to compare the similarity among microbial community before and after the periodontal treatment in treatment group. All calculations were performed using Graphpad Prism software, version 8.4.0 for Mac (Graphpad software Inc., SanDiego, CA, USA) and Microsoft Office Excel 2016 for Windows (Microsoft Co., Redmond, WA, USA). A p-value < 0.05 was considered to indicate statistical significance.
3. Results
3.1. Study’s Sample and Demographics
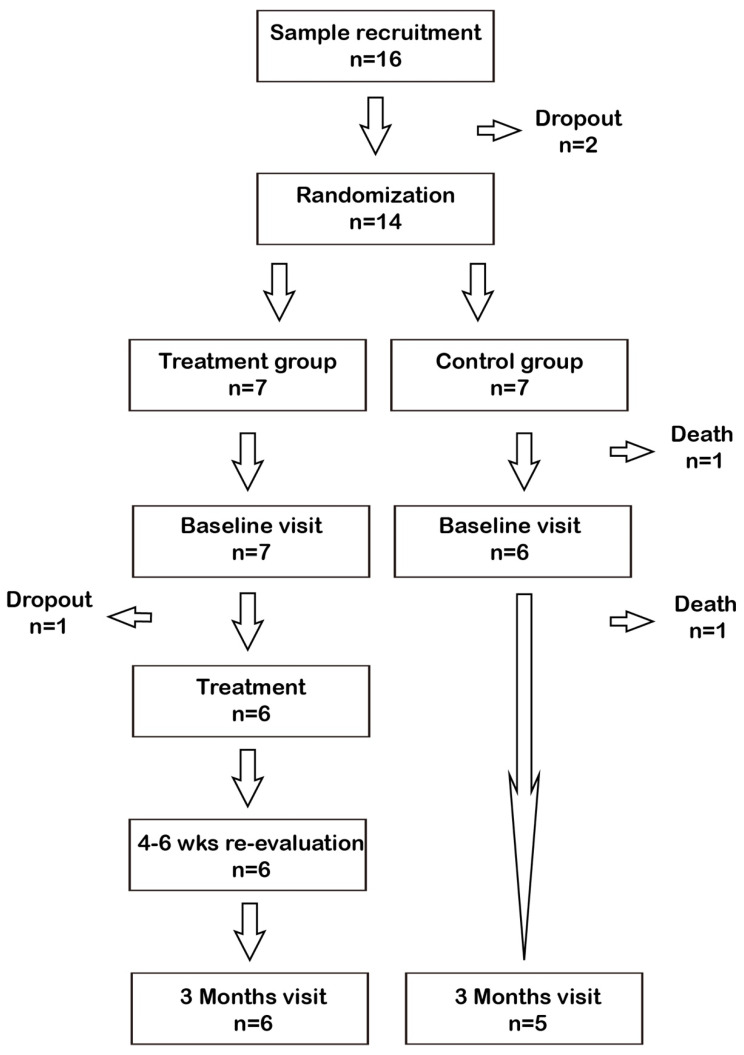
A total of 14 eligible ESRD patients consented to participate the study (Figure 1). A total of 11 ESRD patients completed the course of study (Treatment group, n = 6; Control group, n = 5). After randomization, there were two patients who died in the control group before any intervention and comparison. Clinical characteristics are summarized in Table 1. The mean age was 61 ± 12 years and 71% of the patients were men. 64% of the patients had a history of diabetes and 86% of the patients had severe periodontitis. The clinical parameters were similar between groups, including BMI, systolic blood pressure, periodontitis severity, dialysis vintage, and laboratory results. Baseline periodontal characteristics are summarized in Table 1.
Figure 1.
Flow-chart.
Table 1.
Baseline clinical and dental characteristics.
| All (n = 14) |
Treatment (n = 7) |
Control (n = 7) |
p Value | |
|---|---|---|---|---|
| Male, n (%) | 10 (71%) | 5 (71%) | 5 (71%) | 0.721 |
| Age | 61 ± 12 | 63 ± 8 | 60 ± 16 | 0.675 |
| BMI | 22.8 ± 3.7 | 22.5 ± 2.0 | 23.2 ± 5.0 | 0.751 |
| SBP (mmHg) | 145 ± 17 | 137 ± 21 | 152 ± 9 | 0.093 |
| DBP (mmHg) | 76 ± 16 | 67 ± 9 | 86 ± 15 | 0.014 |
| Severity | 1.000 | |||
| Mild | 0 | 0 | 0 | |
| Moderate | 2 | 1 | 1 | |
| Severe | 12 | 6 | 6 | |
| Dialysis vintage (months) |
46 ± 59 | 60 ±81 | 31 ± 20 | 0.381 |
| Diabetes, n (%) | 9 (64%) | 5 (71%) | 4 (57%) | 0.577 |
| Hypertension, n (%) | 12 (86%) | 5 (71%) | 7 (100%) | 0.127 |
| Smoking, n (%) | 0 (0%) | 1 (14%) | 2 (29%) | 0.213 |
| Alb (g/dL) | 4.3 ± 0.4 | 4.3 ± 0.4 | 4.2 ± 0.4 | 0.597 |
| Hb (g/dL) | 11.4 ± 0.9 | 11.8 ± 0.8 | 11.0 ± 0.8 | 0.084 |
| K (mg/dL) | 4.7 ± 0.5 | 4.8 ± 0.5 | 4.5 ± 0.4 | 0.395 |
| Ca (mg/dL) | 9.2 ± 0.9 | 9.1 ± 0.8 | 9.4 ± 1.1 | 0.534 |
| P (mg/dL) | 5.2 ± 1.2 | 5.1 ± 1.0 | 5.2 ± 1.4 | 0.914 |
| PTH (pg/mL) | 310 ± 259 | 252 ± 175 | 368 ± 328 | 0.423 |
| Fe (ug/dL) | 84 ± 37 | 82 ± 23 | 85 ± 48 | 0.870 |
| TIBC (ug/dL) | 227 ± 33 | 233 ± 38 | 221 ± 28 | 0.501 |
| Ferritin (ng/mL) | 570 ± 367 | 608 ± 439 | 540 ± 349 | 0.804 |
| HbA1c (%) | 6.3 ± 1.4 | 6.8 ± 1.7 | 5.7 ± 0.7 | 0.301 |
| Periodontal characteristics (patient-level analysis) | ||||
| Plaque index (%) (mean ± SD) (%) | 99.57 ± 0.79 | 88.14 ± 20.48 | 0.08 | |
| Probing depth (PD) (mm) (mean ± SD) | 2.97 ± 0.74 | 2.99 ± 0.53 | 0.46 | |
| Gingival recession depth (mm) (REC) (mean ± SD) | 1.18 ± 0.84 | 0.83 ± 0.80 | 0.22 | |
| Clinical attachment loss (CAL) (mm) (mean ± SD) | 4.18 ± 1.46 | 3.99 ± 1.31 | 0.41 | |
| Bleeding on probing (BOP) (%) (mean ± SD) (%) | 62.29 ± 21.55 | 77.57 ± 16.33 | 0.08 | |
Statistics by Mann–Whitney U test for baseline characteristics, except baseline gender and periodontal severity which were by Fisher’s exact test. Statistics by Mann–Whitney U test for baseline plaque index, PD, REC, CAL, BOP. Significance level set at p-value < 0.05.
3.2. Primary Outcome and Secondary Outcomes
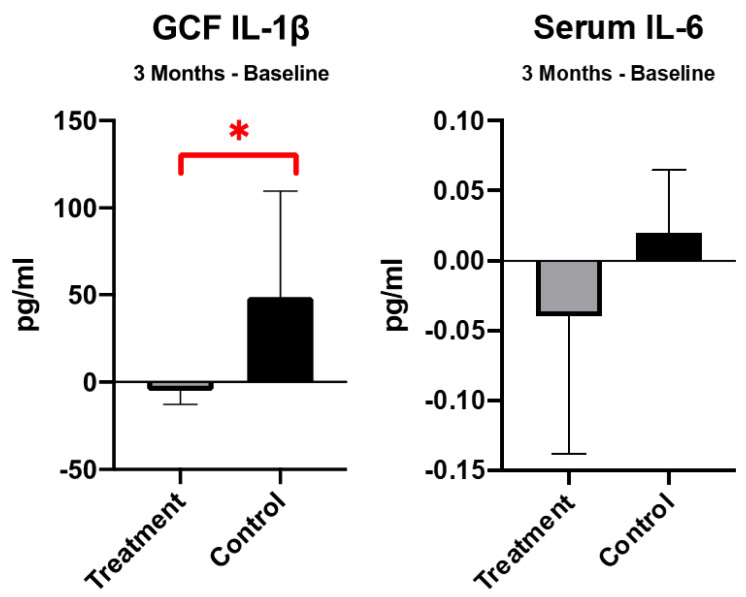
At 3 months, no significant difference was found between groups in all-cause mortality (OR 0.15, 95% CI 0.01–3.71, p = 0.244), CV events (OR 0.29, 95% CI 0.01–8.39, p = 0.470), and infection events (OR 1.88, 95% CI 0.20–17.27, p = 0.579) (Table 2). In the secondary outcomes, there was no significant difference in either diabetic control, cardiac function, or peripheral vessel evaluation. In the biomarkers, the IL-1β in GCF was significantly reduced in the treatment group as compared to control group. Meanwhile, the IL-6 in serum was non-significantly reduced in the treatment group (Figure 2). Otherwise, other cytokines, including hsCRP, TNF-α, and PTX3 were not significantly changed between groups.
Table 2.
Primary and secondary outcomes.
| N | Event | OR (95% CI) | p Value | |
|---|---|---|---|---|
| Primary outcomes | ||||
| All-cause mortality | 14 | 2 | 0.244 | |
| Treatment | 7 | 0 | 0.15 (0.01–3.71) | |
| Control | 7 | 2 | 1.0 (ref.) | |
| CV events | 14 | 1 | 0.470 | |
| Treatment | 7 | 0 | 0.29 (0.01–8.39) | |
| Control | 7 | 1 | 1.0 (ref.) | |
| Infection events | 14 | 5 | 0.579 | |
| Treatment | 7 | 3 | 1.88 (0.20–17.27) | |
| Control | 7 | 2 | 1.0 (ref.) | |
| Secondary outcomes | Treatment (n = 6) | Control (n = 5) | p value | |
| HbA1c | 6.6 ± 1.3 | 5.8 ± 1.2 | 0.401 | |
| Cardiac function | ||||
| LVEF | 61 ± 17 | 61 ± 7 | 0.923 | |
| LV mass | 281 ± 70 | 266 ± 58 | 0.795 | |
| Peripheral vessel | ||||
| Right ABI | 1.1 ± 0.2 | 1.1 ± 0.1 | 0.831 | |
| Left ABI | 1.0 ± 0.2 | 1.1 ± 0.1 | 0.097 | |
| Right PWV | 16.6 ± 3.9 | 14.6 ± 4.3 | 0.523 | |
| Left PWV | 15.4 ± 4.2 | 15.2 ± 4.7 | 0.945 | |
Statistics by Mann–Whitney U test. Significance level set at p-value < 0.05. LVEF: left ventricular ejection fraction. LV: left ventricular. ABI: ankle-brachial index PWV: pulse wave velocity.
Figure 2.
Change of biomarkers level in gingival crevicular fluid (GCF) and serum. *: p-value < 0.05.
3.3. Periodontal Outcomes
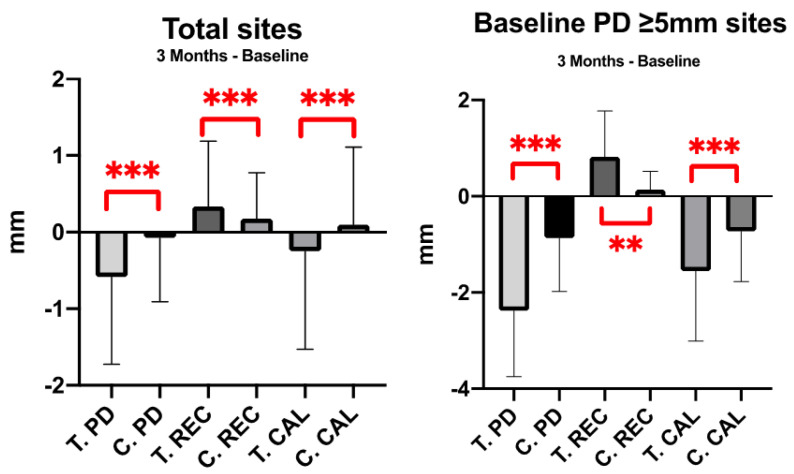
At patient-level analysis, no significant difference was shown in changes in plaque index, PD, REC, CAL, BOP in intra-group and inter-group comparisons. The exception was the change in REC in treatment group, the gingival recession increased 0.03 mm after treatment (p < 0.05). At site-level analysis, changes in PD, REC, and CAL showed significant difference in both groups at the 3 month visit (p < 0.001) (Figure 3). There was net attachment gain of 0.25 mm attachment in treatment group, and net attachment loss of 0.1 mm in control group. The significant improvement in PD, REC, and CAL changes were shown in treatment group. Specifically, in severe periodontitis sites (PD ≥ 5 mm sites), the improvement was more obvious in treatment group than control group (Figure 3).
Figure 3.
Change of periodontal parameters by site-level analysis. **: p-value < 0.003; ***: p-value < 0.001.
3.4. Periodontal Microbiome
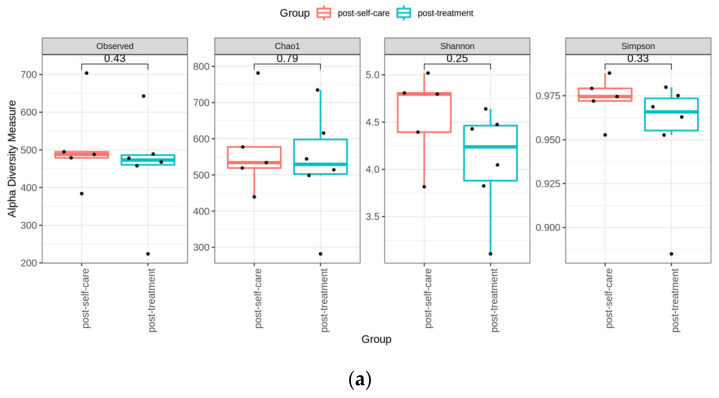
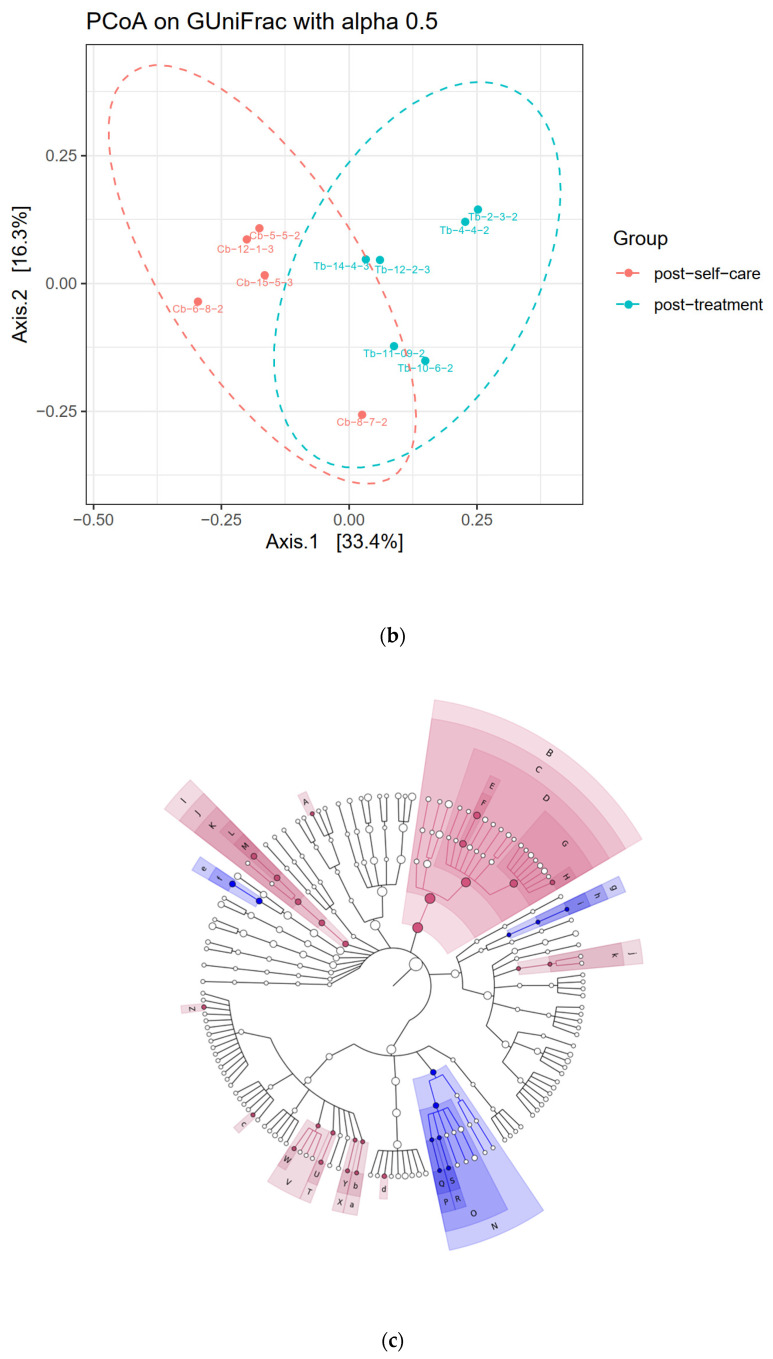
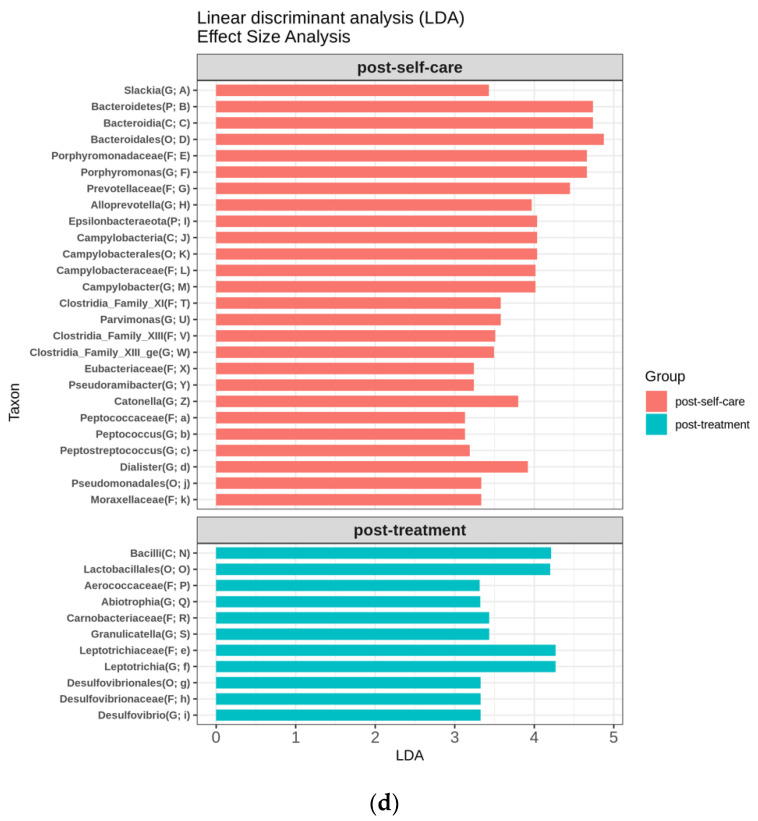
We applied α-diversity indices to determine the ecological diversity of the microbial community. Comparison of α-diversity between the two groups was performed. Four indices were not significantly different between groups (Figure 4a). Further, we used the principal coordinate analysis (PCoA), which is a dimensional reduction method to illustrate the relationship between samples, depending on the distance matrix. GUniFrac distance analysis was performed and showed a significant difference between groups (ADONIS analysis, p = 0.006) (Figure 4b). Significantly discriminative taxa between groups were determined using the LDA Effect Size (Figure 4c). LDA shows only the taxa meeting the thresholds (>3) (Figure 4d).
Figure 4.
Subgingival microbial diversity. (a) Comparison of the α-diversity between the microbiota of the treatment and control group patients. We used the four indices to represent the α-diversity (the observed, Chao, Shannon, Simpson index). (b) Principal coordinate analysis. It showed the grouping patterns of the microbiota between the post-treatment and post self-care patients based on the GUniFrac distances, which showed a significant difference between groups (ADONIS analysis, p = 0.006). (Each closed circle represents a sample. Distances between any pair of samples represent their dissimilarities.) (c) Significantly discriminative taxa between groups were determined using the Linear Discriminant Analysis (LDA) Effect Size. (d) LDA shows the taxa meeting the thresholds (>3). (Different colored regions represent different groups. From the interior to the exterior, each layer represents the phylum, class, order, family, and genus level).
The red complex periodontal pathogens, T. forsythia, and T. denticola, showed significant decrease after periodontal treatment (p < 0.05). Bacterial count of P. gingivalis and A. actinomycetemcomitans were decreased in both groups, but intra-group comparisons did not show significant difference. A. naeslundii amount was elevated in treatment group and decreased in control group; however, the difference did not show statistical significance. Inter-group comparison did not show significant difference.
4. Discussion
Periodontal disease is a kind of chronic inflammation disease and highly prevalent in dialysis patients [35]. A previous prospective observational study indicated that compared to patients with mild or no periodontitis, all-cause mortality is higher in patients with moderate and severe periodontitis [36]. Another retrospective study with 168 patients under hemodialysis showed moderate to severe periodontitis was associated with increased risk of CV mortality, as compared to those with mild periodontitis [37]. However, the evidence of periodontal treatment reducing mortality in dialysis patients is still insufficient. Based on the present pilot study, periodontal non-surgical treatment group did not show significant difference in primary outcomes including all-cause mortality, CV events, and infection events.
Increased IL-1β in GCF has been considered as a sign of development of periodontal disease. Periodontitis might aggravate systemic inflammatory response [38]. A recent systematic review concluded that non-surgical periodontal treatment can reduce serum hsCRP levels in hemodialysis and/or peritoneal dialysis patients, but did not change IL-6 or albumin levels significantly [15]. However, in our study, even IL-1β in local GCF was significantly reduced in the treatment group, changes in serum level of IL-6, hsCRP, TNF-α, and PTX3 did not show significant difference between treatment and control groups.
Several pre-specified outcome measurements, including sugar change and vascular function, were performed in the present study. A previous review reported chronic periodontitis results in increased expression of pro-inflammatory cytokines, and vascular endothelial dysfunction [39]. A meta-analysis reported the association of periodontitis with carotid intima-media thickness and flow-mediated dilation [40]. The periodontal treatment improved the flow-mediated dilation, which indicated an improvement in endothelial function [40]. However, in our study, all of these outcomes showed no difference between groups during follow up. This result may be explained by the fact that most of the collected studies in the previous meta-analysis study were from patients with normal renal function [40]. Several lines of uremic toxins and uremic milieu effects on the vascular endothelial cell may not be improved dramatically with the locally periodontal inflammation improvement [41].
More than 1000 bacterial species host in the oral cavity [42]. Red complex bacterial species, constituted by P. gingivalis, T. denticola and T. forsythia, are considered as the most virulent periodontal pathogens [43]. In a previous study comprising of 32 periodontitis subjects treated by non-surgical periodontal therapy and maintained for 12-month period, A. naeslundii was increased significantly, and the red complex periodontal pathogens were decreased significantly in prevalence and levels after therapy [44]. Our findings are consistent with previous studies, periodontal pathogens were also reduced in treatment group after therapy. Microbial diversity showed significant difference between post-treatment and post self-care groups.
In the present study, all of the periodontal exams were performed by two experienced dentists. Microbiological changes in GCF sampling can also confirm the clinical effects of periodontal treatment, reducing the risk of clinical inconsistency. However, our study has several limitations. First, limited subjects enrolled in the study could diminish the outcomes. Second, differences in mortality would be apparent over a longer duration of time. Third, some possible confounding factors, such as diabetes and smoking, might have influenced the outcomes. Further research should be undertaken to investigate the systemic effects of periodontal treatment on more CKD patient numbers and for longer follow-up period. In clinical practice, clinicians could take periodontal health into consideration in dialysis patients.
5. Conclusions
In conclusion, the periodontal non-surgical intervention changes the pattern and distribution of microbiota in gingival sulcus. However, no significant association of the intervention in periodontitis and mortality improvement in dialysis patients was found in present study. Moreover, treatment of periodontitis did not bring beneficial effect in reducing systemic inflammation.
Acknowledgments
We thanks to the staff of the Taipei Medical University (TMU) Joint Biobank for biological specimen application and technical support. We also thanks to the support from Taipei Medical University (TMU109-AE1-B08).
Author Contributions
Conceptualization, W.-C.C., C.-C.K., C.-F.H. and M.-S.W.; methodology, W.-C.C. and C.-C.K.; software, W.-C.C. and C.-C.K.; validation, C.-F.H., H.-K.L. and M.-S.W.; formal analysis, W.-C.C., C.-C.K.; investigation, W.-C.C., C.-Y.L. and C.-C.K.; resources, C.-C.K. and M.-S.W.; data curation, W.-C.C. and C.-C.K.; writing—original draft preparation, W.-C.C. and C.-C.K.; writing—review and editing, W.-C.C. and C.-C.K.; visualization, W.-C.C. and C.-C.K.; supervision, C.-F.H. and M.-S.W.; project administration, C.-F.H. and M.-S.W.; funding acquisition, C.-F.H. and M.-S.W. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by grants from Taipei Medical University (TMU Joint Clinical Research Center, PI-Initiated Trial, IIT-105-4601-005-400), and Taipei Medical University Hospital (105TMUH-NE-01).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Taipei Medical University Joint Institutional Review Board (TMU-JIRB No. N201604007, approval date: 15 June 2016).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data will be available from authors upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Slots J. Periodontitis: Facts, fallacies and the future. Periodontology 2000. 2017;75:7–23. doi: 10.1111/prd.12221. [DOI] [PubMed] [Google Scholar]
- 2.Holt S.C., Ebersole J.L. Porphyromonas gingivalis, Treponema denticola, and Tannerella forsythia: The “red complex”, a prototype polybacterial pathogenic consortium in periodontitis. Periodontology 2000. 2005;38:72–122. doi: 10.1111/j.1600-0757.2005.00113.x. [DOI] [PubMed] [Google Scholar]
- 3.Loos B.G. Systemic markers of inflammation in periodontitis. J. Periodontol. 2005;76:2106–2115. doi: 10.1902/jop.2005.76.11-S.2106. [DOI] [PubMed] [Google Scholar]
- 4.Linden G.J., Herzberg M.C., Working Group 4 of the Joint, EFP/AAP Workshop Periodontitis and systemic diseases: A record of discussions of working group 4 of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J. Periodontol. 2013;84:S20–S23. doi: 10.1902/jop.2013.1340020. [DOI] [PubMed] [Google Scholar]
- 5.Chen T.K., Knicely D.H., Grams M.E. Chronic Kidney Disease Diagnosis and Management: A Review. JAMA. 2019;322:1294–1304. doi: 10.1001/jama.2019.14745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eknoyan G., Lameire N., Eckardt K., Kasiske B., Wheeler D., Levin A., Stevens P., Bilous R., Lamb E., Coresh J. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 2013;3:5–14. [Google Scholar]
- 7.Bikbov B., Purcell C.A., Levey A.S., Smith M., Abdoli A., Abebe M., Adebayo O.M., Afarideh M., Agarwal S.K., Agudelo-Botero M., et al. Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395:709–733. doi: 10.1016/S0140-6736(20)30045-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Di Lullo L., House A., Gorini A., Santoboni A., Russo D., Ronco C. Chronic kidney disease and cardiovascular complications. Heart Fail. Rev. 2015;20:259–272. doi: 10.1007/s10741-014-9460-9. [DOI] [PubMed] [Google Scholar]
- 9.Chambrone L., Foz A.M., Guglielmetti M.R., Pannuti C.M., Artese H.P., Feres M., Romito G.A. Periodontitis and chronic kidney disease: A systematic review of the association of diseases and the effect of periodontal treatment on estimated glomerular filtration rate. J. Clin. Periodontol. 2013;40:443–456. doi: 10.1111/jcpe.12067. [DOI] [PubMed] [Google Scholar]
- 10.Deschamps-Lenhardt S., Martin-Cabezas R., Hannedouche T., Huck O. Association between periodontitis and chronic kidney disease: Systematic review and meta-analysis. Oral Dis. 2019;25:385–402. doi: 10.1111/odi.12834. [DOI] [PubMed] [Google Scholar]
- 11.Pan W., Wang Q., Chen Q. The cytokine network involved in the host immune response to periodontitis. Int. J. Oral Sci. 2019;11:30. doi: 10.1038/s41368-019-0064-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Torrungruang K., Katudat D., Mahanonda R., Sritara P., Udomsak A. Periodontitis is associated with elevated serum levels of cardiac biomarkers-Soluble ST2 and C-reactive protein. J. Clin. Periodontol. 2019;46:809–818. doi: 10.1111/jcpe.13149. [DOI] [PubMed] [Google Scholar]
- 13.Sanz M., Del Castillo A.M., Jepsen S., Gonzalez-Juanatey J.R., D’Aiuto F., Bouchard P., Chapple I., Dietrich T., Gotsman I., Graziani F., et al. Periodontitis and cardiovascular diseases: Consensus report. J. Clin. Periodontol. 2020;47:268–288. doi: 10.1111/jcpe.13189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tonetti M.S., D’Aiuto F., Nibali L., Donald A., Storry C., Parkar M., Suvan J., Hingorani A.D., Vallance P., Deanfield J. Treatment of periodontitis and endothelial function. N. Engl. J. Med. 2007;356:911–920. doi: 10.1056/NEJMoa063186. [DOI] [PubMed] [Google Scholar]
- 15.Yue H., Xu X., Liu Q., Li X., Xiao Y., Hu B. Effects of non-surgical periodontal therapy on systemic inflammation and metabolic markers in patients undergoing haemodialysis and/or peritoneal dialysis: A systematic review and meta-analysis. BMC Oral Health. 2020;20:18. doi: 10.1186/s12903-020-1004-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhao D., Khawaja A.T., Jin L., Chan K.W., Tonetti M., Tang S.C.W., Pelekos G. Effect of non-surgical periodontal therapy on renal function in chronic kidney disease patients with periodontitis: A systematic review and meta-analysis of interventional studies. Clin. Oral Investig. 2020;24:1607–1618. doi: 10.1007/s00784-019-03066-w. [DOI] [PubMed] [Google Scholar]
- 17.Hwang H.S., Hong Y.A., Yoon H.E., Chang Y.K., Kim S.Y., Kim Y.O., Jin D.C., Kim S.H., Kim Y.L., Kim Y.S., et al. Comparison of Clinical Outcome Between Twice-Weekly and Thrice-Weekly Hemodialysis in Patients With Residual Kidney Function. Medicine (Baltimore) 2016;95:e2767. doi: 10.1097/MD.0000000000002767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Page R.C., Eke P.I. Case definitions for use in population-based surveillance of periodontitis. J. Periodontol. 2007;78:1387–1399. doi: 10.1902/jop.2007.060264. [DOI] [PubMed] [Google Scholar]
- 19.Teughels W., Feres M., Oud V., Martin C., Matesanz P., Herrera D. Adjunctive effect of systemic antimicrobials in periodontitis therapy: A systematic review and meta-analysis. J. Clin. Periodontol. 2020;47((Suppl. S22)):257–281. doi: 10.1111/jcpe.13264. [DOI] [PubMed] [Google Scholar]
- 20.Costantinides F., Castronovo G., Vettori E., Frattini C., Artero M.L., Bevilacqua L., Berton F., Nicolin V., Di Lenarda R. Dental Care for Patients with End-Stage Renal Disease and Undergoing Hemodialysis. Int. J. Dent. 2018;2018:9610892. doi: 10.1155/2018/9610892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greenstein G., Polson A. The role of local drug delivery in the management of periodontal diseases: A comprehensive review. J. Periodontol. 1998;69:507–520. doi: 10.1902/jop.1998.69.5.507. [DOI] [PubMed] [Google Scholar]
- 22.Fujita Y., Ito H., Sekino S., Numabe Y. Correlations between pentraxin 3 or cytokine levels in gingival crevicular fluid and clinical parameters of chronic periodontitis. Odontology. 2012;100:215–221. doi: 10.1007/s10266-011-0042-1. [DOI] [PubMed] [Google Scholar]
- 23.Miyamoto T., Carrero J.J., Stenvinkel P. Inflammation as a risk factor and target for therapy in chronic kidney disease. Curr. Opin. Nephrol. Hypertens. 2011;20:662–668. doi: 10.1097/MNH.0b013e32834ad504. [DOI] [PubMed] [Google Scholar]
- 24.Lu H.K., Chen Y.L., Chang H.C., Li C.L., Kuo M.Y. Identification of the osteoprotegerin/receptor activator of nuclear factor-kappa B ligand system in gingival crevicular fluid and tissue of patients with chronic periodontitis. J. Periodontal Res. 2006;41:354–360. doi: 10.1111/j.1600-0765.2006.00883.x. [DOI] [PubMed] [Google Scholar]
- 25.Mohammed M.M.A., Nerland A.H., Al-Haroni M., Bakken V. Characterization of extracellular polymeric matrix, and treatment of Fusobacterium nucleatum and Porphyromonas gingivalis biofilms with DNase I and proteinase K. J. Oral Microbiol. 2013;5 doi: 10.3402/jom.v5i0.20015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Roky M., Trent J.O., Demuth D.R. Identification of functional domains of the minor fimbrial antigen involved in the interaction of Porphyromonas gingivalis with oral streptococci. Mol. Oral Microbiol. 2020;35:66–77. doi: 10.1111/omi.12280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Martin M. Cutadapt removes adapter sequences from high-throughput sequencing reads. EMBnet. J. 2011;17:10–12. doi: 10.14806/ej.17.1.200. [DOI] [Google Scholar]
- 28.Quast C., Pruesse E., Yilmaz P., Gerken J., Schweer T., Yarza P., Peplies J., Glockner F.O. The SILVA ribosomal RNA gene database project: Improved data processing and web-based tools. Nucleic Acids Res. 2013;41:D590–D596. doi: 10.1093/nar/gks1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stamatakis A. RAxML version 8: A tool for phylogenetic analysis and post-analysis of large phylogenies. Bioinformatics. 2014;30:1312–1313. doi: 10.1093/bioinformatics/btu033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wright E.S. DECIPHER: Harnessing local sequence context to improve protein multiple sequence alignment. BMC Bioinform. 2015;16:322. doi: 10.1186/s12859-015-0749-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McMurdie P.J., Holmes S. Phyloseq: An R package for reproducible interactive analysis and graphics of microbiome census data. PLoS ONE. 2013;8:e61217. doi: 10.1371/journal.pone.0061217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen J., Bittinger K., Charlson E.S., Hoffmann C., Lewis J., Wu G.D., Collman R.G., Bushman F.D., Li H. Associating microbiome composition with environmental covariates using generalized UniFrac distances. Bioinformatics. 2012;28:2106–2113. doi: 10.1093/bioinformatics/bts342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Asnicar F., Weingart G., Tickle T.L., Huttenhower C., Segata N. Compact graphical representation of phylogenetic data and metadata with GraPhlAn. PeerJ. 2015;3:e1029. doi: 10.7717/peerj.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Segata N., Izard J., Waldron L., Gevers D., Miropolsky L., Garrett W.S., Huttenhower C. Metagenomic biomarker discovery and explanation. Genome Biol. 2011;12:R60. doi: 10.1186/gb-2011-12-6-r60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ruospo M., Palmer S.C., Craig J.C., Gentile G., Johnson D.W., Ford P.J., Tonelli M., Petruzzi M., De Benedittis M., Strippoli G.F. Prevalence and severity of oral disease in adults with chronic kidney disease: A systematic review of observational studies. Nephrol. Dial. Transplant. 2014;29:364–375. doi: 10.1093/ndt/gft401. [DOI] [PubMed] [Google Scholar]
- 36.Chen L.P., Chiang C.K., Peng Y.S., Hsu S.P., Lin C.Y., Lai C.F., Hung K.Y. Relationship between periodontal disease and mortality in patients treated with maintenance hemodialysis. Am. J. Kidney Dis. 2011;57:276–282. doi: 10.1053/j.ajkd.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 37.Kshirsagar A.V., Craig R.G., Moss K.L., Beck J.D., Offenbacher S., Kotanko P., Klemmer P.J., Yoshino M., Levin N.W., Yip J.K., et al. Periodontal disease adversely affects the survival of patients with end-stage renal disease. Kidney Int. 2009;75:746–751. doi: 10.1038/ki.2008.660. [DOI] [PubMed] [Google Scholar]
- 38.Boch J.A., Wara-aswapati N., Auron P.E. Interleukin 1 signal transduction--current concepts and relevance to periodontitis. J. Dent. Res. 2001;80:400–407. doi: 10.1177/00220345010800020101. [DOI] [PubMed] [Google Scholar]
- 39.Gurav A.N. The implication of periodontitis in vascular endothelial dysfunction. Eur. J. Clin. Investig. 2014;44:1000–1009. doi: 10.1111/eci.12322. [DOI] [PubMed] [Google Scholar]
- 40.Orlandi M., Suvan J., Petrie A., Donos N., Masi S., Hingorani A., Deanfield J., D’Aiuto F. Association between periodontal disease and its treatment, flow-mediated dilatation and carotid intima-media thickness: A systematic review and meta-analysis. Atherosclerosis. 2014;236:39–46. doi: 10.1016/j.atherosclerosis.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 41.Bonan N.B., Schepers E., Pecoits-Filho R., Dhondt A., Pletinck A., De Somer F., Vanholder R., Van Biesen W., Moreno-Amaral A., Glorieux G. Contribution of the uremic milieu to an increased pro-inflammatory monocytic phenotype in chronic kidney disease. Sci. Rep. 2019;9:10236. doi: 10.1038/s41598-019-46724-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ximenez-Fyvie L.A., Haffajee A.D., Socransky S.S. Microbial composition of supra- and subgingival plaque in subjects with adult periodontitis. J. Clin. Periodontol. 2000;27:722–732. doi: 10.1034/j.1600-051x.2000.027010722.x. [DOI] [PubMed] [Google Scholar]
- 43.Socransky S.S., Haffajee A.D., Cugini M.A., Smith C., Kent R.L., Jr. Microbial complexes in subgingival plaque. J. Clin. Periodontol. 1998;25:134–144. doi: 10.1111/j.1600-051X.1998.tb02419.x. [DOI] [PubMed] [Google Scholar]
- 44.Cugini M.A., Haffajee A.D., Smith C., Kent R.L., Jr., Socransky S.S. The effect of scaling and root planing on the clinical and microbiological parameters of periodontal diseases: 12-month results. J. Clin. Periodontol. 2000;27:30–36. doi: 10.1034/j.1600-051x.2000.027001030.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be available from authors upon reasonable request.