Abstract
Obesity is associated with negative prostate cancer outcomes (e.g., specific mortality, all-cause mortality, biochemical recurrence, etc.), according to the current scientific literature. Nevertheless, recommendations on weight loss and healthy lifestyles are poorly covered by clinicians. We aimed at identifying these recommendations from clinical practice guidelines (CPGs) for prostate cancer. We systematically searched MEDLINE, EMBASE, Web of Science, Scopus, guideline databases and online sources for CPGs updated from January 2015 to August 2021. The searches were independently conducted by two researchers, without language restrictions. A total of 97 prostate cancer guidelines, including 84 (86.6%) CPGs and 13 (13.4%) consensus statements, were included. Recommendations on reaching and maintaining a healthy weight or healthy lifestyles were provided by 7 (7.2%) and 13 (13.4%) documents, respectively. No differences regarding recommendations were found by type of document, year of publication or country. Our results suggest that professional societies and governments should update prostate cancer guidelines to include these recommendations for improving prostate cancer prognosis.
Keywords: clinical guidelines, consensus statement, prostate cancer, obesity, mortality, body weight
1. Introduction
Prostate cancer (PC) is the most frequent cancer in men [1]. Nevertheless, few prognostic factors have been clearly associated with PC outcomes, mainly older age, ethnicity and family history of PC [2], none of them modifiable. For decades, obesity has been associated with negative PC outcomes, although results were not always consistent [3,4]. According to the PRACTICAL consortium [5] and the REDUCE study [6], among others, obesity may be considered a modifiable risk factor for prostate cancer according to current data. Recently, new studies on the molecular mechanisms linking obesity to prostate cancer have been developed [7], and several systematic reviews and meta-analyses have pointed to obesity, measured as body mass index (BMI) ≥ 30 kg/m2, as a prognostic factor associated with a higher frequency of prostate cancer specific mortality [8], higher frequency of all-cause mortality [8] and higher frequency of biochemical recurrence after radical prostatectomy [9]. The World Cancer Research Fund [10] also reported an increased risk of being diagnosed with advanced PC in obese patients. Other authors have reported the increased difficulties of prostate cancer surgery in obese patients, which can lead to adverse events or disease recurrence [11], and a higher association with the need for chemotherapy [12]. Other recent studies have pointed to an association between higher BMI and multiple pelvic lymph node metastasis [13].
Given that obesity is associated with poorer health outcomes in the general population [14,15], and the wide range of works reporting its implications for negative PC outcomes, it seems logical to include recommendations on weight loss from clinicians to newly diagnosed PC patients. Therefore, several authors have pointed out the need for including recommendations on reaching and maintaining a healthy weight in clinical practice guidelines (CPGs), as weight loss programs have proven to be effective [16,17]. In fact, current research is focused on designing healthy lifestyle interventions and weight loss programs [18,19]. CPGs are documents that compile current evidence-based recommendations on how to diagnose and treat a medical condition, usually endorsed by medical organizations or governments. Consensus statements (CSs) are a comprehensive summary of the opinions of an expert panel to provide guidance on controversial or poorly understood aspects of healthcare. Therefore, both documents should include updated evidence-based information on modifiable prognostic factors such as weight loss or lifestyle habits.
The aim of this study was to compile all recent CPGs and CSs on prostate cancer diagnosis and treatment developed by professional societies or governments and to analyze the presence of recommendations regarding healthy weight and lifestyles.
2. Materials and Methods
The systematic review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [20] (Supplementary Table S1).
2.1. Search Strategy and Data Source
We conducted a systematic search covering the period from January 2015 to August 2021 to avoid selection bias, as most of the guidelines before this period had been updated and replaced by more recent ones, combining MeSH terms “clinical practice guidelines”, “guidelines”, “consensus”, “prostate cancer”, “prostate cancer diagnosis” and “prostate cancer treatment” and including word variants in the TRIP database and MEDLINE, without language restrictions, to collect all updated CPGs and CSs. When the language of the document was not the mother tongue of the researchers (i.e., different from English or Spanish), we tried to contact researchers fluent in this language from our center. When this was not possible, we completely translated the document using free translator software, DeepL (https://www.deepl.com/translator, accessed on: 15 December 2021).
Afterwards, we extended the search to other databases, such as EMBASE, Web of Science, Scopus, Cochrane Database of Systematic Reviews and the ACP Journal Club. Eight guideline databases were searched, including the National Institute for Health and Care Excellence (NICE), the National Comprehensive Cancer Network (NCCN), the Scottish Intercollegiate Guidelines Network (SIGN), Fisterra, the Canadian Clinical Practice Guideline (CPG), the CMA Infobase, the National Health and Medical Research Council (NHMRC), the Health Services Technology Assessment Texts (HSTAT) and the Guidelines International Network (GIN). Finally, 77 professional society websites were visited to complete the search (Supplementary Table S2), and references from other relevant studies were manually searched.
2.2. Study Selection and Data Extraction
We covered CPGs and CSs on the diagnosis and therapeutic management of prostate cancer, developed by professional societies, organizations or government agencies. We also included guidelines on the management of cancer complications (e.g., castration-resistant prostate cancer). The documents were considered as CPGs and CSs as depicted by the authors after full-text reading, or when the search database considered it as so. The presence of keywords in the title, such as “guideline” for CPGs or “consensus” for CSs, helped us in the classification of the documents. Obsolete documents updated in more recent years from the same organization or government, CPGs or CSs for education or information purposes and documents designed only for patients were excluded. Two independent reviewers (MR-I and VM-R) identified titles and abstracts and performed full-text assessment of the eligible studies. Disagreements or inconsistences were solved by consensus with a third senior reviewer (JJJ-M). Duplicate documents were identified and removed. Data extraction and identification of duplicates were conducted using the software Mendeley Reference Manager version 2.61.1. (Mendeley, London, UK).
2.3. Assessment
All CPGs and CSs were thoroughly assessed for the inclusion of recommendations concerning weight loss or lifestyle. The variables collected from each document were the type of document (CPG or CS), focus of the document (diagnostic or treatment of PC), area (divided by continent and country), year of the last update and publication in a journal. The variables of interest were divided into the following groups: (1) acknowledgement of obesity, weight or body mass index (BMI) as a potential risk factor for PC; (2) acknowledgement of lifestyle as a risk factor for PC; (3) acknowledgement of obesity, weight or BMI as possible prognostic factors for PC; (4) acknowledgement of lifestyle as a prognostic factor for PC; (5) recommendations on healthy weight for PC patients; (6) recommendations on healthy lifestyle for PC patients; (7) recommendations on healthy diet for PC patients and (8) recommendations on physical activity for PC patients. Finally, a quality assessment of CPGs that included such recommendations was conducted using the AGRE-II tool. For points (1) to (5), we searched the guideline text for an appropriate statement that included the presence of body weight or lifestyle as recognized risk or prognostic factors for PC, after full-text reading. For points (6) to (8), we looked for specific recommendations provided in the document. All the selected documents were assessed independently by two reviewers (MR-I and VM-R), and disagreements were resolved by consensus with a third reviewer (JJJ-M).
2.4. Statistical Analyses
We conducted descriptive analysis on the presence of obesity, weight, BMI or lifestyle in the guidelines. Country, year, type of document and focus of the document were considered for bivariate analyses. Differences in the presence of the variables of interest were analyzed using T-tests and chi-square tests for quantitative and qualitative variables, respectively. When chi-square conditions for applications were not met, Fisher’s exact test was applied.
3. Results
3.1. Study Selection
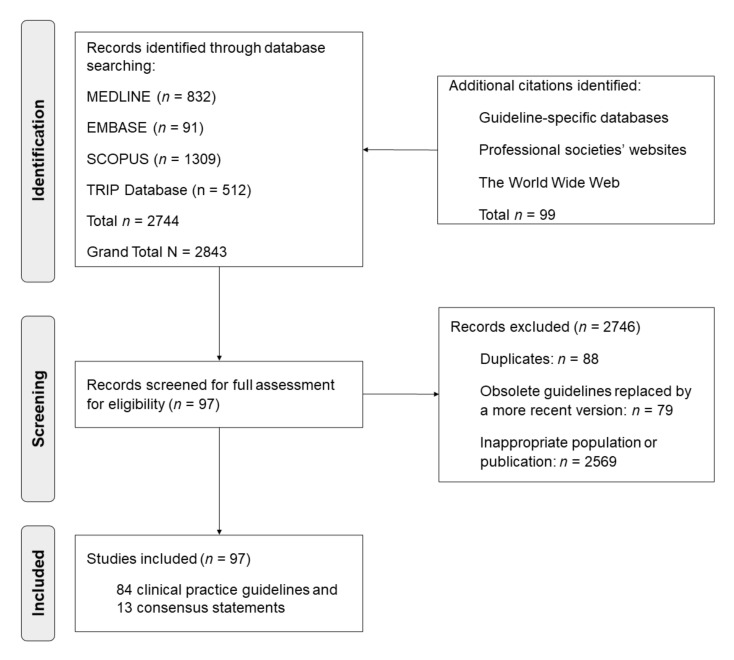
Of the 2905 identified citations, 97 CPGs and CSs met the inclusion criteria; 45 were (46.5%) published in a journal [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65] and 52 (53.6%) were published in other sources (Supplementary Table S3). Figure 1 shows the flow chart of the study selection.
Figure 1.
Flow chart of the study selection of the systematic review according to PRISMA guidelines.
3.2. Characteristics of the Studies
Table 1 shows the main characteristics of the selected documents, including the title, year and country. There was a total of 40 (41.2%) North American guidelines, 35 (36.5%) European guidelines, 12 (12.4%) Asian guidelines, 6 (6.2%) South American guidelines and 4 (4.1%) from other continents (African, Oceanian or international guidelines that covered countries from different continents). From the selected documents, 84 (86.6%) were CPGs and 13 (13.4%) were CSs. A total of 45 (46.4%) documents corresponded to diagnostic guidelines and 78 (80.4%) included information on therapeutic approaches and recommendations.
Table 1.
Clinical guidelines and consensus statements on diagnosis and treatment of prostate cancer (n = 97), 2015–2021.
| Name of the Clinical Practice Guideline | Entity | Country | Year | Recommendation 1 |
|---|---|---|---|---|
| PMB definition guideline: Prostate cancer | CMS | South Africa | 2020 | No |
| South African prostate cancer guidelines | SAUA | South Africa | 2017 | Yes |
| Chinese guidelines for diagnosis and treatment of prostate cancer 2018 | NHC China | China | 2018 | No |
| Evidenced-based clinical practice guideline for prostate cancer (summary: Japanese Urological Association, 2016 edition) | JUA | Japan | 2016 | No |
| 2020 Korean guidelines for the management of metastatic prostate cancer. | KSMO | Korea | 2020 | No |
| Prostate cancer | MIMS | Malaysia | 2021 | Yes |
| Singapore Cancer Network (SCAN) Guidelines for the Management of Advanced Castrate-Resistant Prostate Cancer. | SCAN | Singapore | 2015 | No |
| Saudi Oncology Society and Saudi Urology Association combined clinical management guidelines for prostate cancer 2017 | SOS-SUA | Saudi Arabia | 2017 | No |
| EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer—2020 Update. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent | EAU-EANM-ESTRO-ESUR-SIOG | Europe | 2020a | No |
| EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer. Part II-2020 Update: Treatment of Relapsing and Metastatic Prostate Cancer | EAU-EANM-ESTRO-ESUR-SIOG | Europe | 2020b | Yes |
| Biochemical recurrence in prostate cancer: The EAU Prostate Cancer Guidelines Panel’s recommendations. | EAU-EANM-ESTRO-ESUR-SIOG | Europe | 2020c | No |
| ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up of prostate cancer | ESMO | Europe | 2020 | Yes |
| Guidelines on Prostate Cancer | EAU-ESTRO-ESOR-SIOG | Europe | 2018 | No |
| EAU-ESTRO-SIOG Guidelines on prostate cancer: screening, diagnosis and local treatment with curative intent | EAU-ESTRO-SIOG | Europe | 2017 | No |
| DUCG’s National Guidelines for Diagnosis and Treatment of Prostate Cancer | DUCG | Denmark | 2015 | No |
| French ccAFU guidelines—update 2020–2022: prostate cancer | CCAFU | France | 2020 | No |
| S3—Prostate cancer guideline | AWMF-DKG-DKH | Germany | 2021 | Yes |
| PSMA ligand PET/CT in the diagnosis of prostate carcinoma. | AWMF | Germany | 2019 | No |
| National Prostate Cancer GP Referral Guideline | NCCP | Ireland | 2018 | No |
| Diagnosis, staging and treatment of patients with prostate cancer. National Clinical Guideline No. 8 | NCCP | Ireland | 2016 | Yes |
| Prostate cancer, national guideline version 3.0 | IKNL | Netherlands | 2017 | Yes |
| Appropriate use of pharmaceutical products for patients with castration-refractory prostate cancer | Zorginstituut Nederland | Netherlands | 2016 | No |
| Prostate cancer | NVU | Netherlands | 2016 | No |
| SEOM clinical guidelines for the treatment of advanced prostate cancer (2020) | SEOM | Spain | 2020 | No |
| SEOM clinical guidelines for the treatment of metastatic prostate cancer (2017) | SEOM | Spain | 2017 | No |
| Enzalutamide for treating hormone-sensitive metastatic prostate cancer (technology appraisal guidance TA712) | NICE | UK | 2021 | No |
| Darolutamide with androgen deprivation therapy for treating hormone-relapsed non-metastatic prostate cancer (technology appraisal guidance TA660) | NICE | UK | 2020 | No |
| Prostate cancer: diagnosis and management. (NICE guideline NG131) | NICE | UK | 2019a | No |
| Enzalutamide for hormone-relapsed non-metastatic prostate cancer (Technology appraisal guidance TA580) | NICE | UK | 2019b | No |
| Padeliporfin for untreated localised prostate cancer (Technology appraisal guidance TA546) | NICE | UK | 2018a | No |
| Memokath-051 stent for ureteric obstruction (Medical technologies guidance MTG35) | NICE | UK | 2018b | No |
| Prostate cancer screening with prostate-specific antigen (PSA) test: a clinical practice guideline | MAGIC–BMJ | UK | 2018 | No |
| Biodegradable spacer insertion to reduce rectal toxicity during radiotherapy for prostate cancer (Interventional procedures guidance IPG590) | NICE | UK | 2017 | No |
| Irreversible electroporation for treating prostate cancer Interventional procedures guidance [IPG572] |
NICE | UK | 2016a | No |
| Radium-223 dichloride for treating hormone-relapsed prostate cancer with bone metastases (Technology appraisal guidance TA412) | NICE | UK | 2016b | No |
| Cabazitaxel for hormone-relapsed metastatic prostate cancer treated with docetaxel (Technology appraisal guidance TA391) | NICE | UK | 2016c | No |
| Degarelix for treating advanced hormone-dependent prostate cancer (Technology appraisal guidance TA404) | NICE | UK | 2016d | No |
| Abiraterone for castration-resistant metastatic prostate cancer previously treated with a docetaxel-containing regimen (Technology appraisal guidance TA259) | NICE | UK | 2016e | No |
| Abiraterone for treating metastatic hormone-relapsed prostate cancer before chemotherapy is indicated (Technology appraisal guidance TA387) | NICE | UK | 2016f | No |
| Enzalutamide for treating metastatic hormone-relapsed prostate cancer before chemotherapy is indicated (Technology appraisal guidance TA377) | NICE | UK | 2016g | No |
| Suspected cancer: recognition and referral (NICE guideline NG12) | NICE | UK | 2015 | No |
| Brachytherapy for Patients with Prostate Cancer: American Society of Clinical Oncology/Cancer Care Ontario Joint Guideline Update | ASCO/CCOJ | USA/ Canada |
2017 | No |
| Canadian Urological Association guideline on androgen deprivation therapy: Adverse events and management strategies | CUA | Canada | 2021a | Yes |
| Canadian Urological Association best practice report: Prostate-specific membrane antigen positron emission tomography/computed tomography (PSMA PET/CT) and PET/magnetic resonance (MR) in prostate cancer | CUA | Canada | 2021b | No |
| 2021 Canadian Urological Association (CUA)-Canadian Uro-Oncology Group (CUOG) guideline: Management of castration-resistant prostate cancer (CRPC) | CUA | Canada | 2021c | No |
| Multiparametric Magnetic Resonance Imaging in the Diagnosis of Clinically Significant Prostate Cancer. Guideline 27-2 version 2 | CCO | Canada | 2021 | No |
| A Canadian framework for managing prostate cancer during the COVID-19 pandemic: Recommendations from the Canadian Urologic Oncology Group and the Canadian Urological Association | CUA | Canada | 2020a | No |
| Canadian Urological Association-Canadian Urologic Oncology Group guideline on metastatic castration-naive and castration-sensitive prostate cancer | CUA | Canada | 2020b | Yes |
| Local prostate cancer. Clinical Practice Guideline GU-012—Version 3 | CCA | Canada | 2020a | No |
| Advanced/Metastatic prostate cancer. Clinical Practice Guideline GU-010—Version 2 | CCA | Canada | 2020b | No |
| Prostate Cancer Part 1: Diagnosis and Referral in Primary Care | BC | Canada | 2020a | No |
| Prostate Cancer Part 2: Follow-up in Primary Care | BC | Canada | 2020b | Yes |
| An Endorsement of the 2018 Guideline on Hypofractionated Radiation Therapy for Localized Prostate Cancer: An ASTRO, ASCO, and AUA Evidence-Based Guideline | CCO | Canada | 2018 | No |
| Guideline for Optimization of Surgical and Pathological Quality Performance for Radical Prostatectomy in Prostate Cancer Management. Evidence-Based Series 17-3 Version 2 | CCO | Canada | 2017a | No |
| Follow-up Care for Survivors of Prostate Cancer—Clinical Management: a Program in Evidence-Based Care Systematic Review and Clinical Practice Guideline | CCO | Canada | 2017b | No |
| Canadian Urological Association recommendations on prostate cancer screening and early diagnosis | CUA | Canada | 2017 | No |
| Multiparametric magnetic resonance imaging for pre-treatment local staging of prostate cancer: A Cancer Care Ontario clinical practice guideline | CCO | Canada | 2016a | No |
| Bone Health and Bone-Targeted Therapies for Prostate Cancer. Guideline 3-14 Version 2 | CCO | Canada | 2016b | Yes |
| Prostate cancer, 2015. | CCA | Canada | 2015 | No |
| Society for Immunotherapy of Cancer (SITC) clinical practice guideline on immunotherapy for the treatment of urothelial cancer | SITC | USA | 2021 | No |
| Initial Management of Noncastrate Advanced, Recurrent, or Metastatic Prostate Cancer: ASCO Guideline Update | ASCO | USA | 2021 | No |
| Advanced prostate cancer: AUA-ASTRO-SUO guideline | AUA-ASTRO-SUO | USA | 2020 | No |
| Bone Health and Bone-Targeted Therapies for Prostate Cancer: ASCO Endorsement of a Cancer Care Ontario Guideline | ASCO | USA | 2020 | No |
| Prostate cancer: NCCN Clinical Practice Guidelines in Oncology | NCCN | USA | 2019a | No |
| Prostate cancer early detection. NCCN Clinical Practice Guidelines in Oncology | NCCN | USA | 2019b | No |
| Incontinence after Prostate Treatment: AUA/SUFU Guideline (2019) | AUA-SUFU | USA | 2019 | No |
| Adjuvant and Salvage Radiotherapy after Prostatectomy: ASTRO/AUA Guideline | ASTRO-AUA | USA | 2019 | No |
| Prostate cancer prevention and early detection. | ACS | USA | 2019 | No |
| Castration-resistant prostate cancer | AUA | USA | 2018 | No |
| Screening for Prostate Cancer: US Preventive Services Task Force Recommendation Statement | USPSTF | USA | 2018 | No |
| Early detection of prostate cancer: AUA guideline | AUA | USA | 2018 | No |
| Clinically Localized Prostate Cancer: ASCO Clinical Practice Guideline Endorsement | ASCO | USA | 2018 | Yes |
| ASTRO/ASCO/AUA Guideline on Hypofractionation for Localized Prostate Cancer | ASTRO-ASCO-AUA | USA | 2018 | No |
| American Joint Committee on Cancer. Prostate | AJCC | USA | 2017 | No |
| Clinically Localized Prostate Cancer: AUA-ASTRO-SUO Guideline. | AUA-ASTRO-SUO | USA | 2017 | Yes |
| NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines). Version 3. | NCCN | USA | 2016 | No |
| Radiotherapy for recurrent prostate cancer: 2018 Recommendations of the Australian and New Zealand Radiation Oncology Genito-Urinary group | FROGG | Australia and New Zealand | 2018 | No |
| Clinical practice guidelines: PSA Testing and Early Management of Test-Detected Prostate Cancer | PCFA | Australia and New Zealand | 2016 | No |
| AUGE Clinical Guidelines. Prostate cancer in patients over 15 years old. | MSC | Chile | 2015 | No |
| Prostate cancer. Risk factors, early detection and PSA: screening, use and correct interpretation | AMUC | Costa Rica | 2018 | No |
| Prostate cancer diagnosis and treatment. Clinical practice guidelines. | IMSS | Mexico | 2018 | No |
| Clinical practice guideline: prostate cancer | AUNA | Peru | 2019 | No |
| Clinical practice guideline for the screening, diagnosis and treatment of localized and locally advanced prostate cancer | IETSI | Peru | 2021 | No |
| Clinical Practice Guideline for the early detection, diagnosis, staging, treatment, rehabilitation and follow-up of patients with prostate cancer. | INEN | Peru | 2021 | No |
| Name of the Consensus Statement | Entity | Country | Year | Recommendation 1 |
| Update of Guidelines for Management of Prostate Cancer in West Africa 2019: Consensus Working Document. | WA | West Africa |
2019 | No |
| NCCN Asia Consensus Statement prostate cancer | NCCN | Asia | 2018 | No |
| Chinese Expert Consensus on the Diagnosis and Treatment of Castration-Resistant Prostate Cancer (2019 Update) | CEC | China | 2019 | No |
| Consensus statements on the management of clinically localized prostate cancer from the Hong Kong Urological Association and the Hong Kong Society of Uro-Oncology | HKUA-HKSUO | China | 2019 | No |
| Expert Group Consensus Opinion on Prostate Cancer Diagnosis and Management in India | Consensus | India | 2020 | No |
| Guidance for the assessment and management of prostate cancer treatment induced bone loss. A consensus position statement from an expert group | Expert group | UK | 2020 | Yes |
| Canadian consensus forum of key controversial areas in the management of advanced prostate cancer | GURC | Canada | 2021 | No |
| Current topics in radiotherapy for genitourinary cancers: Consensus statements of the Genitourinary Radiation Oncologists of Canada | GUROC | Canada | 2020 | No |
| Canadian consensus algorithm for erectile rehabilitation following prostate cancer treatment | CUA | Canada | 2018 | No |
| Cancer Care Ontario Position Statement on Prostate Cancer Screening using the Prostate-Specific Antigen (PSA) Test | CCO | Canada | 2017 | No |
| Second-Line Hormonal Therapy for Men with Chemotherapy-Naïve, Castration-Resistant Prostate Cancer: ASCO Provisional Clinical Opinion | ASCO | USA | 2017 | No |
| Role of Genetic Testing for Inherited Prostate Cancer Risk: Philadelphia Prostate Cancer Consensus Conference 2017. | PPCCC | USA | 2017 | No |
| Management of patients with advanced prostate cancer: APCCC consensus conference | APCCC | International | 2019 | No |
The guidelines are presented divided by type of document (CPGs or CSs), continent, country and year. The complete names of the entities (abbreviations) are available in Supplementary Table S2. 1 Presence of any recommendation regarding body weight or lifestyle in the document.
3.3. Factors Associated with Recommendations on Obesity and Healthy Lifestyles
Only 11 (11.3%) documents acknowledged obesity, body mass index or weight as a risk factor for prostate cancer, and five (5.2%) as a prognostic factor. Similarly, 15 (15.5%) documents considered lifestyle factors as risk factors, and seven (7.2%) as prognostic factors. Regarding recommendations, only seven (7.2%) guidelines provided advice on reaching or maintaining a healthy weight for PC patients, and 13 (13.4%) provided advice on healthy lifestyles. These 13 documents that presented recommendations showed reasonably high quality according to AGREE-II (Supplementary Table S4). Supplementary Table S5 shows examples of the specific recommendations provided by these 13 documents. Specifically, healthy diet and physical activity advice was provided in 9 (9.3%) and 10 (10.3%) documents, respectively (Table 2).
Table 2.
Characteristics of the clinical practice guidelines (CPGs) and consensus statements (CSs) on prostate cancer regarding assessment or recommendations on obesity and healthy lifestyles.
| Characteristics | N | % |
|---|---|---|
| Total sample | 97 | 100.0 |
| Obesity, body mass index or weight are considered as risk factors for prostate cancer in the guideline | 11 | 11.3 |
| Lifestyle factors are considered as risk factors for prostate cancer in the guideline | 15 | 15.5 |
| Obesity, body mass index or weight are considered as prognostic factors for prostate cancer in the guideline | 5 | 5.2 |
| Lifestyle factors are considered as prognostic factors for prostate cancer in the guideline | 7 | 7.2 |
| Recommendations on reaching or maintaining a healthy weight are provided within the guideline | 7 | 7.2 |
| Recommendations on reaching or maintaining healthy lifestyle habits are provided within the guideline | 13 | 13.4 |
| Recommendations on healthy diet are provided within the guideline | 9 | 9.3 |
| Recommendations on physical activity are provided within the guideline | 10 | 10.3 |
Table 3 shows the different characteristics of the guidelines when comparing the 13 documents that provided recommendations on healthy lifestyles with the 84 documents that did not. Although no significant differences were found between the two subgroups, a tendency to provide more recommendations was observed in more recent documents, in CPGs compared with CSs and in therapeutic guidelines. Nevertheless, recommendations on healthy lifestyles were very infrequent for all subgroups
Table 3.
Characteristics of the clinical practice guidelines (CPGs) and consensus statements (CSs) stratified by the presence of recommendations on obesity or healthy lifestyle.
| Characteristics | Total (n = 97) |
Presence of Recommendations (n = 13) | Absence of Recommendations (n = 84) | p-Value 1 |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | ||
| Year of publication | 0.668 | |||
| Published in 2018 or after | 35 (36.1) | 9 (14.5) | 53 (85.5) | |
| Published before 2018 | 62 (63.9) | 4 (11.4) | 31 (88.6) | |
| Type of document | 0.689 | |||
| CPGs | 84 (86.6) | 12 (14.3) | 72 (85.7) | |
| CSs | 13 (13.4) | 1 (7.7) | 12 (92.3) | |
| Continent | ||||
| European guidelines | 35 (36.1) | 6 (17.1) | 29 (82.9) | 0.537 |
| North American guidelines | 40 (41.2) | 5 (12.5) | 35 (87.5) | 0.827 |
| South American guidelines | 6 (6.2) | 0 (0.0) | 6 (100.0) | 0.594 |
| Asian guidelines | 12 (12.4) | 2 (16.7) | 10 (83.3) | 0.723 |
| Publication in a journal | ||||
| Published in a journal | 45 (46.4) | 6 (13.3) | 39 (86.7) | 1.000 |
| Not published in a journal | 52 (53.6) | 7 (13.5) | 45 (86.5) | |
| Focus of the guideline 2 | ||||
| Diagnostic guidelines | 45 (46.4) | 6 (13.3) | 39 (86.7) | 0.985 |
| Therapeutic guidelines | 78 (80.4) | 12 (15.4) | 66 (84.6) | 0.246 |
1p-value of chi-square test or Fisher’s exact test, when appropriate. 2 Diagnostic and treatment guidelines account for more than 100% as several documents were both diagnostic and treatment guidelines. Bold: distinguish between groups of variables.
4. Discussion
We present a thorough systematic review including CPGs and CSs regarding prostate cancer diagnosis and treatment from 2015 to 2021 with no language restrictions. We found that acknowledgment and recommendations on healthy weight and lifestyle for PC patients were very infrequent, regardless of the type of document, year of publication and country. We surprisingly found a high quantity of guidelines (n = 97), most of them on the same topics, suggesting that there may exist a redundancy in prostate cancer guidelines.
Several studies have proved that obesity and other lifestyle factors, such as healthy diet or physical exercise, are risk factors for a diagnosis of PC [66] and prognostic factors once the diagnosis is established [8,9]. Therefore, the World Cancer Research Fund [10] and the World Health Organization [67] have included obesity as an important factor to be controlled for improving PC risk or prognosis. Importantly, PC-specific mortality, all-cause mortality and biochemical recurrence have been reported to be increased in obese patients [8,9]; therefore, current studies are focused on testing programs for reaching and maintaining a healthy weight after PC diagnosis [16,17,18,19]. There are also multiple agencies, including the Prostate Cancer Foundation, Mayo Clinic and multiple patient advocacy groups, that make recommendations on healthy lifestyles for PC patients. Nevertheless, as proven in this study, PC guidelines throughout the world poorly cover recommendations on this important aspect. As healthy lifestyles also improve different outcomes such as cardiovascular events [68], chronic diseases [69] and overall survival [8], it seems evident that recommendations on this topic should be reinforced from clinicians and official guidelines provided for all PC patients.
Specifically, guideline developers should include appropriate professionals (e.g., nutritional therapists or experts in adapted physical exercise) and patient representatives as proper members in guideline panels, to ensure that nutritional and healthy lifestyle topics are included in the prioritized guideline questions. It is also advisable to perform scoping exercises at the beginning of guideline development to make sure that all aspects of health related to PC are properly covered. Moreover, clinicians and healthcare professionals that interact with PC patients should use our data to reinforce recommendations regarding weight loss and healthy lifestyles. According to the recommendations summarized in Supplementary Table S5, PC patients should be counseled regarding the importance of modifiable health-related behaviors or risk factors, such as smoking and obesity, through healthy diet, toxic habits and physical exercise assessment and counselling [32]. This is especially recommended, according to evidence-based data, for patients undergoing androgen-deprivation therapies [33] and for patients that receive surgical treatment (i.e., prostatectomy), where obesity has been more clearly associated with poorer prognosis [32].
It is important to note that different recommendations might be individualized according to the disease stage. For example, behavioral interventions regarding vegetable consumption have not been proven to decrease cancer progression at early stages [70]. In this regard, several clinical trials are being developed to analyze the impact of weight loss interventions in patients with clinically localized PC [71]. A recent systematic review on the MARTINI-Lifestyle cohort also pointed out that the adherence to lifestyle recommendations is very poor in PC patients [72]. However, this adherence has been proven to reduce mortality in several types of cancer [73]. For PC, preclinical and observational studies have identified potential benefits for high-vegetable, low-fat, low-meat diets and increased exercise, but Level I evidence is still limited [74]. Therefore, randomized clinical trials are still needed to inform specific recommendations for PC patients, considering the stage of the disease and the most appropriate intervention.
Another important aspect for future research is to add information on the perspectives and values of patients through qualitative research, to optimize the design of healthy lifestyle interventions that better adhere to patients’ possibilities and perspectives.
A key strength of our study was the global perspective, including guidelines from all countries included in our search, with almost one hundred documents included. No restriction to specific languages, data sources or types of documents were considered. For documents not written in English or Spanish (mother tongue of the researchers), we attempted to contact a pertinent researcher in our center, but, when this was not possible, we used free translation software. This could imply a limitation given that the translation software may present mistakes. Another perceived limitation of the study was the difficulties in finding documents with languages different from English, French, Spanish, German and Chinese. We tried to minimize this issue by duplicating data extraction through two independent reviewers. An additional important limitation of this study is that no specific tool for evaluating the presence of recommendations in clinical guidelines was available; therefore, we analyzed their presence manually through extensive reading of the selected documents, and we used the tool AGREE-II for evaluating the quality of the guidelines that covered weight loss or lifestyle recommendations. We did not prospectively register the protocol of this systematic review.
We found that only a seventh of all PC guidelines recommended the adoption of healthy lifestyles and only 7.2% provided advice on reaching or maintaining a healthy weight, despite the current evidence regarding its usefulness. Our data suggest that professional societies and governments should update their guidelines and documents regarding PC and include recommendations on healthy lifestyles after diagnosis. Clinicians from Oncology, Urology and Primary Care units should advise their PC patients to reach and maintain a healthy weight through recommendations on diet and adapted physical activity, according to the patients’ preferences. Future studies should provide reflections or data on how to systematically introduce weight loss or healthy lifestyle programs for improving PC prognosis.
5. Conclusions
Recommendations on healthy weight or lifestyles are very infrequently provided in PC clinical guidelines from professional societies or governments, regardless of the date of publication, type of document or country. Nevertheless, the current literature indicates that healthy weight and lifestyles improve PC risk and prognosis. Future clinical trials should be developed for informing each PC patient about the best lifestyle intervention, considering the disease stage. Therefore, there may not be a standard recommendation, but different approaches depending on the patient’s disease state, lipid profile, genetics or other unknown variables. PC guidelines should be updated to cover this important issue. Future strategies or intervention programs to reach and maintain a healthy weight should be designed for improving PC care.
Acknowledgments
We thank Khalid Saeed Khan, Jan Stener Joergensen and his team in the Southern Denmark University for assisting in the design and the searching of clinical guidelines and for their methodological support.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph19031452/s1, Table S1: PRISMA 2020 Checklist, Table S2: Data sources and search strategy, Table S3: Identified clinical guidelines and consensus statements not published in a journal. Table S4. Appraisal of Guidelines for Research & Evaluation (AGREE-II) assessment of clinical practice guidelines on prostate cancer that complied with recommendations for healthy weight or lifestyle habits (n = 13). Table S5. Examples of recommendations regarding healthy weight or lifestyles in clinical practice guidelines of prostate cancer.
Author Contributions
Conceptualization, M.R.-I. and J.J.J.-M.; methodology, M.R.-I., V.M.-R. and J.J.J.-M.; validation, V.M.-R. and J.J.J.-M. formal analysis, M.R.-I.; investigation, M.R.-I., V.M.-R. and J.J.J.-M.; resources, J.J.J.-M.; data curation, M.R.-I. and V.M.-R.; writing—original draft preparation, M.R.-I.; writing—review and editing, M.R.-I., V.M.-R. and J.J.J.-M.; visualization, M.R.-I., V.M.-R. and J.J.J.-M.; supervision, V.M.-R. and J.J.J.-M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All datasets used for this study are presented in the manuscript and its Supplementary Materials.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sung H., Ferlay J., Siegel R.L., Laversanne M., Soerjomataram I., Jemal A., Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Schatten H. Brief Overview of Prostate Cancer Statistics, Grading, Diagnosis and Treatment Strategies. Adv. Exp. Med. Biol. 2018;1095:1–14. doi: 10.1007/978-3-319-95693-0_1. [DOI] [PubMed] [Google Scholar]
- 3.Zhong S., Yan X., Wu Y., Zhang X., Chen L., Tang J., Zhao J. Body mass index and mortality in prostate cancer patients: A dose-response meta-analysis. Prostate Cancer Prostatic Dis. 2016;19:122–131. doi: 10.1038/pcan.2015.64. [DOI] [PubMed] [Google Scholar]
- 4.Zhang X., Zhou G., Sun B., Zhao G., Liu D., Sun J., Liu C., Guo H. Impact of obesity upon prostate cancer-associated mortality: A meta-analysis of 17 cohort studies. Oncol. Lett. 2015;9:1307–1312. doi: 10.3892/ol.2014.2841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davies N.M., Gaunt T.R., Lewis S.J., Holly J., Donovan J.L., Hamdy F.C., Kemp J.P., Eeles R., Easton D., Kote-Jarai Z., et al. The effects of height and BMI on prostate cancer incidence and mortality: A Mendelian randomization study in 20,848 cases and 20,214 controls from the PRACTICAL consortium. Cancer Causes Control. 2015;26:1603–1616. doi: 10.1007/s10552-015-0654-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vidal A.C., Howard L.E., Moreira D.M., Castro-Santamaria R., Andriole G.L., Jr., Freedland S.J. Obesity increases the risk for high-grade prostate cancer: Results from the REDUCE study. Cancer Epidemiol. Biomark. Prev. 2014;23:2936–2942. doi: 10.1158/1055-9965.EPI-14-0795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chau C.H., Till C., Price D.K., Goodman P.J., Neuhouser M.L., Pollak M.N., Thompson I.M., Figg W.D. Serum markers, obesity and prostate cancer risk: Results from the prostate cancer prevention trial. Endocr. Relat. Cancer. 2022;20:99–109. doi: 10.1530/ERC-21-0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rivera-Izquierdo M., Pérez de Rojas J., Martínez-Ruiz V., Pérez-Gómez B., Sánchez M.J., Khan K.S., Jiménez-Moleón J.J. Obesity as a Risk Factor for Prostate Cancer Mortality: A Systematic Review and Dose-Response Meta-Analysis of 280,199 Patients. Cancers. 2021;13:4169. doi: 10.3390/cancers13164169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rivera-Izquierdo M., Pérez de Rojas J., Martínez-Ruiz V., Arrabal-Polo M.Á., Pérez-Gómez B., Jiménez-Moleón J.J. Obesity and biochemical recurrence in clinically localised prostate cancer: A systematic review and meta-analysis of 86,490 patients. Prostate Cancer Prostatic Dis. 2022 doi: 10.1038/s41391-021-00481-7. [DOI] [PubMed] [Google Scholar]
- 10.World Cancer Research Fund. American Institute for Cancer Research Body Fatness and Weight Gain. [(accessed on 15 November 2021)]. Available online: https://www.wcrf.org/dietandcancer/exposures/body-fatness.
- 11.Han H., Cao Z., Qin Y., Wei X., Ruan Y., Cao Y., He J. Morbid obesity is adversely associated with perioperative outcomes in patients undergoing robot-assisted laparoscopic radical prostatectomy. Can. Urol. Assoc. J. 2020;14:E574–E581. doi: 10.5489/cuaj.6389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bardhi O., Garcia-Zapirain B., Nuño-Solinis R. Factors influencing care pathways for breast and prostate cancer in a hospital setting. Int. J. Environ. Res. Public Health. 2021;18:7913. doi: 10.3390/ijerph18157913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Porcaro A.B., Tafuri A., Sebben M., Processali T., Pirozzi M., Amigoni N., Rizzetto R., Shakir A., Cerruto M.A., Brunelli M., et al. High body mass index predicts multiple prostate cancer lymph node metastases after radical prostatectomy and extended pelvic lymph node dissection. Asian J. Androl. 2020;22:323–329. doi: 10.4103/aja.aja_70_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lean M.E. Prognosis in obesity. BMJ. 2005;330:1339–1340. doi: 10.1136/bmj.330.7504.1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ortega-Loubon C., Fernández-Molina M., Singh G., Correa R. Obesity and its cardiovascular effects. Diabetes Metab. Res. Rev. 2019;35:e3135. doi: 10.1002/dmrr.3135. [DOI] [PubMed] [Google Scholar]
- 16.Wilson R.L., Shannon T., Calton E., Galvão D.A., Taaffe D.R., Hart N.H., Lyons-Wall P., Newton R.U. Efficacy of a weight loss program prior to robot assisted radical prostatectomy in overweight and obese men with prostate cancer. Sur. Oncol. 2020;35:182–188. doi: 10.1016/j.suronc.2020.08.006. [DOI] [PubMed] [Google Scholar]
- 17.Hamilton-Reeves J.M., Johnson C.N., Hand L.K., Bechtel M.D., Robertson H.L., Michel C., Metcalf M., Chalise P., Mahan N.J., Mirza M., et al. Feasibility of a weight management program tailored for overweight men with localized prostate cancer—A pilot study. Nutr. Cancer. 2020;73:2671–2686. doi: 10.1080/01635581.2020.1856890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Freedland S.J., Allen J., Jarman A., Oyekunle T., Armstrong A.J., Moul J.W., Sandler H.M., Posadas E., Levin D., Wiggins E., et al. A Randomized Controlled Trial of a 6-Month Low-Carbohydrate Intervention on Disease Progression in Men with Recurrent Prostate Cancer: Carbohydrate and Prostate Study 2 (CAPS2) Clin. Cancer Res. 2020;26:3035–3043. doi: 10.1158/1078-0432.CCR-19-3873. Erratum in Clin. Cancer Res. 2021, 27, 1823. [DOI] [PubMed] [Google Scholar]
- 19.Van Rooijen S., Carli F., Dalton S., Thomas G., Bojesen R., Le Guen M., Barizien N., Awasthi R., Minnella E., Beijer S., et al. Multimodal prehabilitation in colorectal cancer patients to improve functional capacity and reduce postoperative complications: The first international randomized controlled trial for multimodal prehabilitation. BMC Cancer. 2019;19:98. doi: 10.1186/s12885-018-5232-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Osaghae S.O. Update of Guidelines for Management of Prostate Cancer in West Africa 2019: Consensus Working Document. West Afr. J. Med. 2020;37:159–172. [PubMed] [Google Scholar]
- 22.Hinotsu S., Namiki M., Ozono S., Akaza H. NCCN Asia Consensus Statement prostate cancer. Jpn. J. Clin. Oncol. 2018;48:964–965. doi: 10.1093/jjco/hyy116. [DOI] [PubMed] [Google Scholar]
- 23.China National Cancer Registration Institute, Chinese guidelines for diagnosis and treatment of prostate cancer 2018 (English version) Chin. J. Cancer Res. 2019;31:67–83. doi: 10.21147/j.issn.1000-9604.2019.01.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhu Y., Ye D., Expert Group Chinese Expert Consensus on the Diagnosis and Treatment of Castration-Resistant Prostate Cancer (2019 Update) Cancer Manag. Res. 2020;12:2127–2140. doi: 10.2147/CMAR.S236879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ma W.K., Poon D.M., Chan C.K., Chan T.W., Cheung F.Y., Ho L.Y., Lee E.K., Leung A.K., Leung S.Y., So H.S., et al. Consensus statements on the management of clinically localized prostate cancer from the Hong Kong Urological Association and the Hong Kong Society of Uro-Oncology. BJU Int. 2019;124:221–241. doi: 10.1111/bju.14681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ghose A., Khochikar M., Sabnis R., Parmar N.M. Expert Group Consensus Opinion on Prostate Cancer Diagnosis and Management in India. Korean J. Urol. Oncol. 2020;18:170–182. doi: 10.22465/kjuo.2020.18.3.170. [DOI] [Google Scholar]
- 27.Kakehi Y., Sugimoto M., Taoka R., Committee for Establishment of the Evidenced-Based Clinical Practice Guideline for Prostate Cancer of the Japanese Urological Association Evidenced-based clinical practice guideline for prostate cancer (summary: Japanese Urological Association, 2016 edition) Int. J. Urol. 2017;24:648–666. doi: 10.1111/iju.13380. [DOI] [PubMed] [Google Scholar]
- 28.Kim I.H., Shin S.J., Kang B.W., Kang J., Kim D., Kim M., Kim J.Y., Kim C.K., Kim H.J., Maeng C.H., et al. 2020 Korean guidelines for the management of metastatic prostate cancer. Korean J. Intern. Med. 2021;36:491–514. doi: 10.3904/kjim.2020.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singapore Cancer Network Genitourinary Cancer Workgroup. Singapore Cancer Network (SCAN) Guidelines for the Management of Advanced Castrate-Resistant Prostate Cancer. Ann. Acad. Med. Singap. 2015;44:397–405. [PubMed] [Google Scholar]
- 30.Aljubran A., Abusamra A., Alkhateeb S., Alotaibi M., Rabah D., Bazarbashi S., Alkushi H., Al-Mansour M., Alharbi H., Eltijani A., et al. Saudi Oncology Society and Saudi Urology Association combined clinical management guidelines for prostate cancer 2017. Urol. Ann. 2018;10:138–145. doi: 10.4103/UA.UA_177_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mottet N., van den Bergh R.C.N., Briers E., Van den Broeck T., Cumberbatch M.G., De Santis M., Fanti S., Fossati N., Gandaglia G., Gillessen S., et al. EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer-2020 Update. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. Eur. Urol. 2021;79:243–262. doi: 10.1016/j.eururo.2020.09.042. [DOI] [PubMed] [Google Scholar]
- 32.Cornford P., van den Bergh R.C.N., Briers E., Van den Broeck T., Cumberbatch M.G., De Santis M., Fanti S., Fossati N., Gandaglia G., Gillessen S., et al. EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer. Part II-2020 Update: Treatment of Relapsing and Metastatic Prostate Cancer. Eur. Urol. 2021;79:263–282. doi: 10.1016/j.eururo.2020.09.046. [DOI] [PubMed] [Google Scholar]
- 33.Parker C., Castro E., Fizazi K., Heidenreich A., Ost P., Procopio G., Tombal B., Gillessen S., ESMO Guidelines Committee Prostate cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2020;31:1119–1134. doi: 10.1016/j.annonc.2020.06.011. [DOI] [PubMed] [Google Scholar]
- 34.Mottet N., Bellmunt J., Bolla M., Briers E., Cumberbatch M.G., De Santis M., Fossati N., Gross T., Henry A.M., Joniau S., et al. EAU-ESTRO-SIOG Guidelines on Prostate Cancer. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. Eur. Urol. 2017;71:618–629. doi: 10.1016/j.eururo.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 35.Rozet F., Mongiat-Artus P., Hennequin C., Beuzeboc P., Cormier L., Fromont-Hankard G., Mongiat-Artus P., Ploussard G., Mathieu R., Brureau L., et al. Recommandations françaises du Comité de cancérologie de l’AFU—actualisation 2020–2022: Cancer de la prostate [French ccAFU guidelines—update 2020–2022: Prostate cancer] Prog. Urol. 2020;30:S136–S251. doi: 10.1016/S1166-7087(20)30752-1. Erratum in Prog. Urol. 2021, 31, 381–382. [DOI] [PubMed] [Google Scholar]
- 36.González Del Alba A., Méndez-Vidal M.J., Vazquez S., Castro E., Climent M.A., Gallardo E., Gonzalez-Billalabeitia E., Lorente D., Maroto J.P., Arranz J.A. SEOM clinical guidelines for the treatment of advanced prostate cancer (2020) Clin. Transl. Oncol. 2021;23:969–979. doi: 10.1007/s12094-021-02561-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cassinello J., Arranz J.Á., Piulats J.M., Sánchez A., Pérez-Valderrama B., Mellado B., Climent M.Á., Olmos D., Carles J., Lázaro M. SEOM clinical guidelines for the treatment of metastatic prostate cancer (2017) Clin. Transl. Oncol. 2018;20:57–68. doi: 10.1007/s12094-017-1783-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brown J.E., Handforth C., Compston J.E., Cross W., Parr N., Selby P., Wood S., Drudge-Coates L., Walsh J.S., Mitchell C., et al. Guidance for the assessment and management of prostate cancer treatment-induced bone loss. A consensus position statement from an expert group. J. Bone Oncol. 2020;25:100311. doi: 10.1016/j.jbo.2020.100311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tikkinen K.A.O., Dahm P., Lytvyn L., Heen A.F., Vernooij R.W.M., Siemieniuk R.A.C., Wheeler R., Vaughan B., Fobuzi A.C., Blanker M.H., et al. Prostate cancer screening with prostate-specific antigen (PSA) test: A clinical practice guideline. BMJ. 2018;362:k3581. doi: 10.1136/bmj.k3581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chin J., Rumble R.B., Kollmeier M., Heath E., Efstathiou J., Dorff T., Berman B., Feifer A., Jacques A., Loblaw D.A. Brachytherapy for Patients With Prostate Cancer: American Society of Clinical Oncology/Cancer Care Ontario Joint Guideline Update. J. Clin. Oncol. 2017;35:1737–1743. doi: 10.1200/JCO.2016.72.0466. [DOI] [PubMed] [Google Scholar]
- 41.Saad F., Hotte S.J., Finelli A., Malone S., Niazi T., Noonan K., Shayegan B., So A.I., Danielson B., Basappa N.S., et al. Results from a Canadian consensus forum of key controversial areas in the management of advanced prostate cancer: Recommendations for Canadian healthcare providers. Can. Urol. Assoc. J. 2021;15:353–358. doi: 10.5489/cuaj.7347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kokorovic A., So A.I., Serag H., French C., Hamilton R.J., Izard J.P., Nayak J.G., Pouliot F., Saad F., Shayegan B., et al. Canadian Urological Association guideline on androgen deprivation therapy: Adverse events and management strategies. Can. Urol. Assoc. J. 2021;15:E307–E322. doi: 10.5489/cuaj.7355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shaygan B., Zukotynski K., Bénard F., Ménard C., Kuk J., Sistani G., Bauman G., Veit-Haibach P., Metser U. Canadian Urological Association best practice report: Prostate-specific membrane antigen positron emission tomography/computed tomography (PSMA PET/CT) and PET/magnetic resonance (MR) in prostate cancer. Can. Urol. Assoc. J. 2021;15:62–72. doi: 10.5489/cuaj.7268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Saad F., Aprikian A., Finelli A., Fleshner N.E., Gleave M., Kapoor A., Niazi T., North S.A., Pouliot F., Rendon R.A., et al. 2021 Canadian Urological Association (CUA)-Canadian Uro Oncology Group (CUOG) guideline: Management of castration-resistant prostate cancer (CRPC) Can. Urol. Assoc. J. 2021;15:E81–E90. doi: 10.5489/cuaj.7074. Erratum in Can. Urol. Assoc. J. 2021, 15, E304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kokorovic A., So A.I., Hotte S.J., Black P.C., Danielson B., Emmenegger U., Finelli A., Niazi T., Pouliot F., Shayegan B., et al. A Canadian framework for managing prostate cancer during the COVID-19 pandemic: Recommendations from the Canadian Urologic Oncology Group and the Canadian Urological Association. Can. Urol. Assoc. J. 2020;14:163–168. doi: 10.5489/cuaj.6667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.So A.I., Chi K.N., Danielson B., Fleshner N.E., Kapoor A., Niazi T., Pouliot F., Rendon R.A., Shayegan B., Sridhar S., et al. Canadian Urological Association-Canadian Urologic Oncology Group guideline on metastatic castration-naive and castration-sensitive prostate cancer. Can. Urol. Assoc. J. 2020;14:17–23. doi: 10.5489/cuaj.6384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Morgan S.C., Morton G.C., Berlin A., Cheung P., Chung P., Ménard C., Pickles T., Souhami L., Warde P.R., Lukka H.R. Current topics in radiotherapy for genitourinary cancers: Consensus statements of the Genitourinary Radiation Oncologists of Canada. Can. Urol. Assoc. J. 2020;14:E588–E593. doi: 10.5489/cuaj.6649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Elterman D.S., Petrella A.R., Walker L.M., Van Asseldonk B., Jamnicky L., Brock G.B., Elliott S., Finelli A., Gajewski J.B., Jarvi K.A., et al. Canadian consensus algorithm for erectile rehabilitation following prostate cancer treatment. Can. Urol. Assoc. J. 2018;13:239–245. doi: 10.5489/cuaj.5653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rendon R.A., Mason R.J., Marzouk K., Finelli A., Saad F., So A., Violette P.D., Breau R.H. Canadian Urological Association recommendations on prostate cancer screening and early diagnosis. Can. Urol. Assoc. J. 2017;11:298–309. doi: 10.5489/cuaj.4888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Loblaw A., Souter L.H., Canil C., Breau R.H., Haider M., Jamnicky L., Morash R., Surchin M., Matthew A. Follow-up Care for Survivors of Prostate Cancer—Clinical Management: A Program in Evidence-Based Care Systematic Review and Clinical Practice Guideline. Clin. Oncol. 2017;29:711–717. doi: 10.1016/j.clon.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 51.Salerno J., Finelli A., Morash C., Morgan S.C., Power N., Schieda N., Haider M.A. Multiparametric magnetic resonance imaging for pre-treatment local staging of prostate cancer: A Cancer Care Ontario clinical practice guideline. Can. Urol. Assoc. J. 2016;10:E332–E339. doi: 10.5489/cuaj.3823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Galsky M.D., Balar A.V., Black P.C., Campbell M.T., Dykstra G.S., Grivas P., Gupta S., Hoimes C.J., Lopez L.P., Meeks J.J., et al. Society for Immunotherapy of Cancer (SITC) clinical practice guideline on immunotherapy for the treatment of urothelial cancer. J. Immunother. Cancer. 2021;9:e002552. doi: 10.1136/jitc-2021-002552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Virgo K.S., Rumble R.B., de Wit R., Mendelson D.S., Smith T.J., Taplin M.E., Wade J.L., 3rd, Bennett C.L., Scher H.I., Nguyen P.L., et al. Initial Management of Noncastrate Advanced, Recurrent, or Metastatic Prostate Cancer: ASCO Guideline Update. J. Clin. Oncol. 2021;39:1274–1305. doi: 10.1200/JCO.20.03256. [DOI] [PubMed] [Google Scholar]
- 54.Saylor P.J., Rumble R.B., Tagawa S., Eastham J.A., Finelli A., Reddy P.S., Kungel T.M., Nissenberg M.G., Michalski J.M. Bone Health and Bone-Targeted Therapies for Prostate Cancer: ASCO Endorsement of a Cancer Care Ontario Guideline. J. Clin. Oncol. 2020;38:1736–1743. doi: 10.1200/JCO.19.03148. [DOI] [PubMed] [Google Scholar]
- 55.Mohler J.L., Antonarakis E.S., Armstrong A.J., D’Amico A.V., Davis B.J., Dorff T., Eastham J.A., Enke C.A., Farrington T.A., Higano C.S., et al. Prostate Cancer, Version 2.2019, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Canc. Netw. 2019;17:479–505. doi: 10.6004/jnccn.2019.0023. [DOI] [PubMed] [Google Scholar]
- 56.Sandhu J.S., Breyer B., Comiter C., Eastham J.A., Gomez C., Kirages D.J., Kittle C., Lucioni A., Nitti V.W., Stoffel J.T., et al. Incontinence after Prostate Treatment: AUA/SUFU Guideline. J. Urol. 2019;202:369–378. doi: 10.1097/JU.0000000000000314. [DOI] [PubMed] [Google Scholar]
- 57.Pisansky T.M., Thompson I.M., Valicenti R.K., D’Amico A.V., Selvarajah S. Adjuvant and Salvage Radiotherapy after Prostatectomy: ASTRO/AUA Guideline Amendment 2018-2019. J. Urol. 2019;202:533–538. doi: 10.1097/JU.0000000000000295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.US Preventive Services Task Force. Grossman D.C., Curry S.J., Owens D.K., Bibbins-Domingo K., Caughey A.B., Davidson K.W., Doubeni C.A., Ebell M., Epling J.W., Jr., et al. Screening for Prostate Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;319:1901–1913. doi: 10.1001/jama.2018.3710. Erratum in JAMA 2018, 319, 2443. [DOI] [PubMed] [Google Scholar]
- 59.Bekelman J.E., Rumble R.B., Chen R.C., Pisansky T.M., Finelli A., Feifer A., Nguyen P.L., Loblaw D.A., Tagawa S.T., Gillessen S., et al. Clinically Localized Prostate Cancer: ASCO Clinical Practice Guideline Endorsement of an American Urological Association/American Society for Radiation Oncology/Society of Urologic Oncology Guideline. J. Clin. Oncol. 2018;36:3251–3258. doi: 10.1200/JCO.18.00606. [DOI] [PubMed] [Google Scholar]
- 60.Morgan S.C., Hoffman K., Loblaw D.A., Buyyounouski M.K., Patton C., Barocas D., Bentzen S., Chang M., Efstathiou J., Greany P., et al. Hypofractionated Radiation Therapy for Localized Prostate Cancer: Executive Summary of an ASTRO, ASCO, and AUA Evidence-Based Guideline. Pract. Radiat. Oncol. 2018;8:354–360. doi: 10.1016/j.prro.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 61.Amin M.B., Greene F.L., Edge S.B., Compton C.C., Gershenwald J.E., Brookland R.K., Meyer L., Gress D.M., Byrd D.R., Winchester D.P. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more "personalized" approach to cancer staging. CA Cancer J. Clin. 2017;67:93–99. doi: 10.3322/caac.21388. [DOI] [PubMed] [Google Scholar]
- 62.Virgo K.S., Basch E., Loblaw D.A., Oliver T.K., Rumble R.B., Carducci M.A., Nordquist L., Taplin M.E., Winquist E., Singer E.A. Second-Line Hormonal Therapy for Men With Chemotherapy-Naïve, Castration-Resistant Prostate Cancer: American Society of Clinical Oncology Provisional Clinical Opinion. J. Clin. Oncol. 2017;35:1952–1964. doi: 10.1200/JCO.2017.72.8030. Erratum in J. Clin. Oncol. 2017, 35, 2591; Erratum in J. Clin. Oncol. 2017, 20, 35, 4096. [DOI] [PubMed] [Google Scholar]
- 63.Giri V.N., Knudsen K.E., Kelly W.K., Abida W., Andriole G.L., Bangma C.H., Bekelman J.E., Benson M.C., Blanco A., Burnett A., et al. Role of Genetic Testing for Inherited Prostate Cancer Risk: Philadelphia Prostate Cancer Consensus Conference 2017. J. Clin. Oncol. 2018;36:414–424. doi: 10.1200/JCO.2017.74.1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lieng H., Hayden A.J., Christie D.R.H., Davis B.J., Eade T.N., Emmett L., Holt T., Hruby G., Pryor D., Shakespeare T.P., et al. Radiotherapy for recurrent prostate cancer: 2018 Recommendations of the Australian and New Zealand Radiation Oncology Genito-Urinary group. Radiother. Oncol. 2018;129:377–386. doi: 10.1016/j.radonc.2018.06.027. [DOI] [PubMed] [Google Scholar]
- 65.Gillessen S., Attard G., Beer T.M., Beltran H., Bjartell A., Bossi A., Briganti A., Bristow R.G., Chi K.N., Clarke N., et al. Management of Patients with Advanced Prostate Cancer: Report of the Advanced Prostate Cancer Consensus Conference 2019. Eur. Urol. 2020;77:508–547. doi: 10.1016/j.eururo.2020.01.012. [DOI] [PubMed] [Google Scholar]
- 66.Bandini M., Gandaglia G., Briganti A. Obesity and prostate cancer. Curr. Opin. Urol. 2017;27:415–421. doi: 10.1097/MOU.0000000000000424. [DOI] [PubMed] [Google Scholar]
- 67.World Health Organization Recommendations for Preventing Cancer. [(accessed on 15 November 2021)]. Available online: https://who.int/dietphysicalactivity/publications/trs916/en/gsfao_cancer.pdf.
- 68.Csige I., Ujvárosy D., Szabó Z., Lórincz I., Paragh D., Harangi M., Somodi S. The impact of obesity on the cardiovascular system. J. Diabetes Res. 2018;2018:3407306. doi: 10.1155/2018/3407306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lavie C.J., De Schutter A., Archer E., McAuley P.A., Blair S.N. Obesity and prognosis in chronic diseases—impact of cardiorespiratory fitness in the obesity paradox. Curr. Sports Med. Rep. 2014;13:240–245. doi: 10.1249/JSR.0000000000000067. Erratum in Curr. Sports Med Rep. 2014, 13, 349. [DOI] [PubMed] [Google Scholar]
- 70.Parsons J.K., Zahrieh D., Mohler J.L., Paskett E., Hansel D.E., Kibel A.S., Liu H., Seisler D.K., Natarajan L., White M., et al. Effect of a Behavioral Intervention to Increase Vegetable Consumption on Cancer Progression Among Men With Early-Stage Prostate Cancer: The MEAL Randomized Clinical Trial. JAMA. 2020;323:140–148. doi: 10.1001/jama.2019.20207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Schenk J.M., Neuhouser M.L., Beatty S.J., VanDoren M., Lin D.W., Porter M., Gore J.L., Gulati R., Plymate S.R., Wright J.L. Randomized trial evaluating the role of weight loss in overweight and obese men with early stage prostate Cancer on active surveillance: Rationale and design of the Prostate Cancer Active Lifestyle Study (PALS) Contemp. Clin. Trials. 2019;81:34–39. doi: 10.1016/j.cct.2019.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Thederan I., Chandrasekar T., Tennstedt P., Kuehl L., Sorbe C., Tilki D., Augustin M., Heinzer H., Zyriax B.C. Poor Adherence to International Cancer Prevention Recommendations among Patients with Prostate Cancer: First Results From the MARTINI-Lifestyle Cohort. Eur. Urol. Focus. 2020;6:935–940. doi: 10.1016/j.euf.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 73.Kohler L.N., Garcia D.O., Harris R.B., Oren E., Roe D.J., Jacobs E.T. Adherence to Diet and Physical Activity Cancer Prevention Guidelines and Cancer Outcomes: A Systematic Review. Cancer Epidemiol. Biomark. Prev. 2016;25:1018–1028. doi: 10.1158/1055-9965.EPI-16-0121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ballon-Landa E., Parsons J.K. Nutrition, physical activity, and lifestyle factors in prostate cancer prevention. Curr. Opin. Urol. 2018;28:55–61. doi: 10.1097/MOU.0000000000000460. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All datasets used for this study are presented in the manuscript and its Supplementary Materials.