Abstract
Viscoelastic hemostatic assay (VHAs) are whole blood point-of-care tests that have become an essential method for assaying hemostatic competence in liver transplantation, cardiac surgery, and most recently, trauma surgery involving hemorrhagic shock. It has taken more than three-quarters of a century of research and clinical application for this technology to become mainstream in these three clinical areas. Within the last decade, the cup and pin legacy devices, such as thromboelastography (TEG® 5000) and rotational thromboelastometry (ROTEM® delta), have been supplanted not only by cartridge systems (TEG® 6S and ROTEM® sigma), but also by more portable point-of-care bedside testing iterations of these legacy devices (e.g., Sonoclot®, Quantra®, and ClotPro®). Here, the legacy and new generation VHAs are compared on the basis of their unique hemostatic parameters that define contributions of coagulation factors, fibrinogen/fibrin, platelets, and clot lysis as related to the lifespan of a clot. In conclusion, we offer a brief discussion on the meteoric adoption of VHAs across the medical and surgical specialties to address COVID-19-associated coagulopathy.
Keywords: thromboelastography, rotational thromboelastometry, COVID-19, coagulopathy, hemorrhage, thrombosis, personalized medicine, fibrinogen, heparin
1. Introduction: The Long History of Viscoelastic Hemostatic Assaying in Research and Clinical Medicine
Introduced in 1948 as a research tool to describe the hemostatic competence of whole blood, the viscoelastic hemostatic assay (VHA) thromboelastography (TEG®) first entered the operating theater in the late 1960s. It was here that TEG® began its first routine use for liver transplantations in guiding blood component therapy (BCT) and hemostatic adjunct therapy (HAT), such as antifibrinolytics and heparin reversal with protamine sulfate [1,2,3,4,5,6]. Beyond liver transplantation and cardiac surgery, TEG® adoption was nearly stagnant through the first decade of the 21st century. In recent years, TEG® has also been adopted for guiding trauma resuscitation in a goal-directed fashion. Around the same time, in the early 21st century, rotational thromboelastometry (ROTEM®) technology was also used successfully in similar areas [5,7,8,9,10,11,12].
Since the 1960s, the delay in the wide acceptance of TEG® and ROTEM® has largely been a function of the lengthy process of confirmation by large randomized controlled trials (RCTs) and Cochrane analyses. Specifically, the clinical value of the VHAs in question includes their point-of-care (POC) utility in the following settings: liver transplantation, cardiac surgery, trauma, obstetrical bleeding, and, most recently, severe hemorrhage in the medical intensive care unit [13,14,15,16,17,18,19,20].
Traditionally, blood banking specialists and hematologists have typically used plasma-based coagulation tests to assess bleeding and clotting risks in surgical, trauma, and non-trauma patients. However, such tests were initially developed to assess patients with isolated clotting factor deficiencies or who were being treated with anticoagulant therapy. These common coagulation tests (CCTs) included the international normalized ratio (INR), prothrombin time (PT), activated partial thromboplastin time (aPTT), platelet counts, levels of fibrinogen, D-dimer, and anti-Xa levels. These tests were subsequently extrapolated for utilization in diverse clinical scenarios.
The CCTs’ utility in evaluating severely hemorrhaging and septic patients has been questioned with the advent of the cell-based model of hemostasis, supported by the CCTs’ lack of sensitivity and slow turnaround time. These shortcomings have prompted trauma surgeons, anesthesiologists, and most recently, obstetricians and intensivists, to turn to VHA-guided BCT for evaluating their bleeding patients [1,3,8,9,16,17,21,22,23,24,25]. For the reasons mentioned above, there has been an increased interest in the use of VHAs to guide BCT by a broad range of medical and surgical specialties. Summarized below are the principles and uses of the most common VHAs in the research and the clinical arenas.
2. Principles of Viscoelastic Hemostatic Assays (VHAs)
The term “viscoelasticity” refers to the property of certain materials to exhibit both viscous and elastic characteristics when undergoing deformation. Blood is a viscous material under normal conditions. However, during the process of coagulation, blood experiences radical changes that cause it to lose viscosity and become more elastic in nature. Complex clot structure enables clots to resist deformation under shear forces. The ability of a material to resist deformation is called shear modulus (G), or modulus of rigidity, and is a measure of the elastic shear stiffness of a material. With VHA systems, even though the term “clot strength” is used frequently, clot stiffness is measured either indirectly or directly. Using TEG® 5000 and ROTEM® delta, shear modulus is assessed indirectly by submerging a pin in whole blood, whereas in Quantra®, it is assessed directly with a sonographic method. The TEG® 5000 and ROTEM® delta “cup and pin” technologies are referred to as “legacy devices” [26,27].
2.1. Thromboelastography (TEG® 5000)
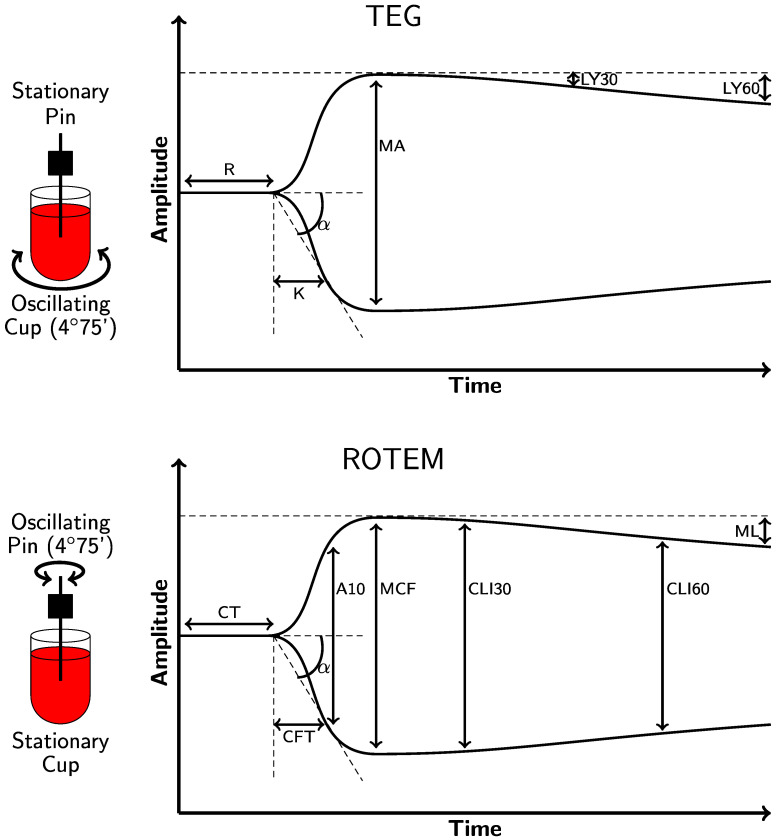
For the TEG® 5000 (Haemonetics Corporation, Boston, MA, USA), a 0.36 cc sample of whole blood is placed into a cup which rotates at 4.45 degrees every 10 s. Blood is recalcified and activated with activators. A pin is placed into this cup, and as a clot forms between the rotating cup and the stationary pin, a force is transmitted to the pin. This force is measured on a computer as an output where the x-axis represents the time in minutes, and the y-axis represents the movement of the pin in millimeters. The TEG® 5000 parameters include the reaction time (R), clot formation/kinetics (K), α-angle, maximum amplitude (MA), and lysis at 30 min (LY30) (Figure 1 and Table 1) [28,29,30,31]. In addition, when quicker results are necessary, such as with cardiac surgery, hypotensive resuscitation during trauma, and liver transplantation, the addition of tissue factor (TF) to the cup is defined for TEG® as RapidTEG® (rTEG®) [32,33,34].
Figure 1.
Depictions of the physiologic TEG® 5000 (top) and ROTEM® delta (bottom) tracings. As the left side of the figure illustrates, a pin descends into a cup containing a sample of whole blood that is maintained at 37 °C. TEG® 5000 and ROTEM® delta analyzers use equivalent parameters that are labeled differently. Reaction time (R) and clotting time (CT) measure the time required for the transducer to displace by 2 mm on the y-axis. Clot formation/kinetics (K) and clot formation time (CFT) measure the initial clot strength and the time needed to displace the transducer by 20 mm, measured from when it first reached 2 mm. The α-angle measures the rate of clot formation in both the TEG® 5000 and ROTEM® delta analyzers by analyzing the angle formed between the end of the R/CT (which is called the split point) and the 20 mm point on the y-axis. The fibrinogen level is broadly correlated with both the K/CFT and α-angle. The reference ranges and definitions of each parameter are provided in Table 1. The clot amplitude at 5 and 10 min (A5 and A10) measures the amplitude at 5 min intervals after the end of R/CT. The maximum amplitude (MA) and maximum clot firmness (MCF) measure the maximum displacement and are indicative of the maximum clot strength. They also correlate with the maximum clot retraction and reflect the crosslinking of fibrin with platelets. Fibrinolysis is depicted by differing parameters in the TEG® 5000 and ROTEM® delta analyzers. The lysis at 30 and 60 min (LY30 and LY60) is a measure of the percent of decrease in amplitude at 30 and 60 min after achieving MA. The clot lysis index (CLI30 and CLI60) is the residual clot remaining 30 and 60 min after CT measured as a percentage of MCF. The maximum lysis (ML) is a measure of the percent of decrease in amplitude at the end of the run [20,23,34,35,36,37,38,39,40,41].
Table 1.
TEG® 5000 and ROTEM® delta “legacy device” parameters and reference ranges [7,27,35,37,38,42,43,44,45,46,47,48,49,50,51,52].
| Parameter | TEG® 5000 Analyzer 1 | ROTEM® Delta Analyzer |
|---|---|---|
| Clot initiation: the time from the test start to amplitude = 2 mm | R (Kaolin)/ACT (rTEG®) Kaolin: 4.6–9.1 min rTEG®: 86–118 s |
CT INTEM: 137–246 s EXTEM: 42–74 s |
| Clot formation and clot kinetics: the time taken to achieve a level of clot strength, amplitude = 20 mm | K Kaolin: 0.8–2.1 min rTEG®: 1–2 min |
CFT INTEM: 40–100 s EXTEM: 46–148 s |
| Angle of clot formation | α-angle Kaolin: 53–72° rTEG®: 64–80° |
α-angle INTEM: 71–82° EXTEM: 63–81° |
| Maximum clot strength | MA Kaolin: 50–70 mm rTEG®: 52–71 mm MAff/CFF: 15–32 mm |
MCF INTEM: 52–72 mm EXTEM: 49–71 mm FIBTEM: 9–25 mm |
| Lysis 2 TEG®: rate of clot breakdown 30 min after MA is reached. ROTEM®: the residual % of MCF amplitude when measured 30 min after CT (CLI30); the % reduction MCF amplitude at a given timepoint (ML) |
LY30 Kaolin: 0–7.5% rTEG®: 0–7.5% |
CLI30: 94–100% ML: <15% |
Abbreviations: activated clotting time (ACT); clot formation time (CFT); clot lysis index at 30 min (CLI30); clotting time (CT); extrinsic thromboelastometry (EXTEM); fibrin-based thromboelastometry (FIBTEM); intrinsic thromboelastometry (INTEM); kinetics (K); lysis at 30 min (LY30); maximum amplitude (MA); maximum clot firmness (MCF); maximum lysis (ML); RapidTEG (rTEG®); reaction time (R); rotational thromboelastometry (ROTEM®); thromboelastography (TEG®); TEG functional fibrinogen (MAff/CFF). 1 For the TEG® 6s and the TEG® 5000, the manufacturer (Haemonetics, Braintree, Massachusetts) makes clear that the ranges are interchangeable, but that any difference in the values is a consequence of the Clinical and Laboratory Standards Institute (CLSI) methodology used for the TEG® 6s values. Additionally, the manufacturer’s ranges are not globally prescriptive, as every laboratory must establish their own reference intervals [48]. 2 The values for clinically significant fibrinolysis vary greatly in the literature.
2.2. Rotational Thromboelastometry (ROTEM® Delta)
With the ROTEM® delta (Instrumentation Laboratory, Bedford, MA), the cup remains stationary while the pin revolves. This results in a curve similar to that of the TEG® 5000, based on similar rheological principles but with different parameters and terminology (Figure 1 and Table 1). In liver transplantation, cardiac surgery, postpartum hemorrhage, and trauma resuscitation, ROTEM® delta has been demonstrated to be effective for goal-directed BCT. ROTEM® has also been used in the diagnosis of bleeding disorders. Extrinsic thromboelastometry (EXTEM) as a parameter of ROTEM® delta, modified by the addition of TF to the cup, provides “interim results” much the same as the TF-enhanced rTEG® produces threshold parameters that trigger action by the clinician prior to the completion of the test in emergency situations [11,29,32,37,53,54].
2.3. Chemical Activators and Inhibitors of VHAs and Their Interpretation
The TEG® 5000 and ROTEM® delta parameters have general similarities. For example, EXTEM and rTEG® both provide 5 min and 10 min interval evaluations of the width of the curve from the split point defined as CA5 and CA10 in EXTEM and A5 and A10 in rTEG®. These values reflect the addition of the TF-enhanced width of the clot from the split point until it reaches MCF for the EXTEM or MA for the rTEG® as a “real-time” reflection of the maximum clot firmness. Therefore, clinical specialists who are responsible for the bedside monitoring of the hemostatic competence of patients can better anticipate blood component needs with greater accuracy and speed [11,32,34,55,56].
Different chemical activators and inhibitors are used by the TEG® 5000 and ROTEM® delta analyzers, allowing for the depiction of the mechanisms of coagulation. In addition, the thresholds for intervention are not uniform and depend on local standards that determine the triggers for intervention [13,36,57]. VHA guidance of BCTs, and pro-hemostatic agents with simplified algorithms, facilitate goal-directed BCT and HAT for bleeding and anticoagulated patients [44].
By adding different coagulation enhancers or inhibitors to the cup, modified TEG® 5000 or ROTEM® delta analysis allows for more detailed analysis of specific coagulation mechanisms, including fibrinolysis and the effect of heparin on clot strength (Table 2). For example, to assess hypocoagulopathy in the operating theater or in the emergency department, tissue factor is used to run the rTEG® or EXTEM [32].
Table 2.
| VHA | Test | Activator/Inhibitor | Significance |
|---|---|---|---|
| TEG | Kaolin | Kaolin, CaCl2 | Contact activation.; similar information as aPTT; isolates the intrinsic pathway. |
| rTEG® | Kaolin, TF, CaCl2 | Clotting is accelerated by activation of extrinsic TF and intrinsic kaolin pathways; contact activation; roughly analogous to an ACT; information about coagulation kinetics initiated via contact activation alone is lost. | |
| HTEG® | Kaolin, lyophilized heparinase, CaCl2 | Lyophilized heparinase neutralizes UFH; compared to kaolin TEG® to assess the heparin effect. | |
| MAff/CFF | Kaolin, TF, Abciximab, CaCl2 | Abciximab is a GPIIb/IIIa platelet receptor inhibitor that blocks the platelet contribution to clot formation; compared to kaolin TEG® to assess the fibrinogen contribution to clot strength independent of platelets. | |
| Native TEG® | Calcium | Native whole blood sample analyzed following recalcification only; impractical for clinical use given long R. | |
| ROTEM | INTEM | Ellagic acid, CaCl2 | Tests clotting activation through the intrinsic coagulation pathway, FXII, FXI, FIX, FVIII, FX, FV, FII, and fibrinogen; sensitive to the heparin effect; similar information as aPTT. |
| EXTEM | Recombinant TF, CaCl2, polybrene | Polybrene neutralizes UFH; tests clotting activation through the extrinsic coagulation pathway, FVII, FX, FV, FII, and fibrinogen. | |
| HEPTEM | Ellagic acid, CaCl2, lyophilized heparinase | Tests heparin and protamine sulfate effects in patients with high heparin concentration when compared with INTEM. | |
| FIBTEM | Recombinant TF, CaCl2, polybrene, cytochalasin D | Cytochalasin D blocks platelet activation; tests fibrinogen component contribution to clot stability; more sensitive to lysis. | |
| APTEM | Recombinant TF, CaCl2, polybrene, aprotinin/TXA | Tests fibrinolysis when performed together with the EXTEM. | |
| NATEM | CaCl2 | Native whole blood sample analyzed following recalcification only; impractical for clinical use given long CT. |
Abbreviations: activated clotting time (ACT); aprotinin thromboelastometry (APTEM); activated partial thromboplastin time (aPTT); clot formation time (CFT); clotting time (CT); extrinsic thromboelastometry (EXTEM); fibrin-based thromboelastometry (FIBTEM); heparin thromboelastometry (HEPTEM); intrinsic thromboelastometry (INTEM); TEG functional fibrinogen (MAff/CFF); non-activated thromboelastometry (NATEM); reaction time (R); rapid TEG® (rTEG®); rotational thromboelastometry (ROTEM®); thromboelastography (TEG®); tissue factor (TF); tranexamic acid (TXA); unfractionated heparin (UFH).
2.4. Sonoclot®
The TEG® 5000 and the ROTEM® delta systems are considered cup and pin “legacy” systems. Another legacy linear motion system is called Sonoclot®; however, it is not a rotation-based system. An empty plastic probe is attached to the transducer head and submerged into an assay sample with potentially varying clotting factors. The oscillation of the probe within the sample transmits a force to a transducer which emits a signal that is proportional to the deflection of the tube. The oscillatory patterns of the movement of the test probe directly reflect the viscoelastic properties of the blood sample. On the x-axis, time is marked, and on the y-axis, millimeters of the movement of the test probe are marked, similar to the function of the TEG® 5000 and ROTEM® delta [27,61].
2.5. New Clinical Technology for VHAs
2.5.1. TEG® 6s
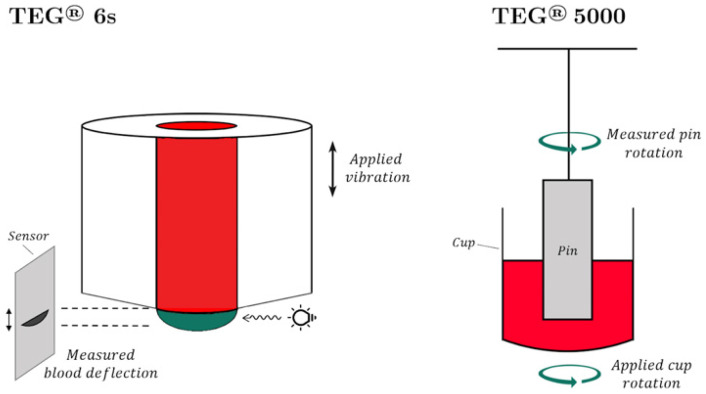
The TEG® 6s Hemostasis Analyzer (Haemonetics Corporation, Boston, MA, USA) is a cartridge-based system which confronts the problem of operator-dependent variability in the pipetting technique [62]. The TEG® 6s cartridge system measures the resonance frequency of a whole blood sample that is exposed to frequency vibrations caused by the motion of the blood meniscus. The resulting resonance frequency of the whole blood sample is measured by illuminating the sample with a light-emitting diode (LED). As the clot forms and the alteration of resonance is measured by the LED, the collected data is converted into a graph that is identical to that used in the cup and pin method (Figure 2) [36,63].
Figure 2.
(Left): TEG® 6s. The vibration of the sample induces blood deflection; the measures change with the resonance frequency. (Right): TEG® 5000. The difference in the rotations of the cup and pin is measured via a torsional spring [64,65].
The TEG® 5000 and the TEG® 6s devices have demonstrated a high degree of reliability, close correlation, and the equivalency of results with the exception of LY30 [66]. Differences in equivalency regarding the manufacturer’s (Haemonetics Corporation, Boston, MA, USA) reference range values between TEG® 6s and TEG® 5000 can be associated with the CLSI methodology used for their TEG® 6s ranges. It has also been suggested that the TEG® 6s offers a significant advantage as a point-of-care test to determine hemostatic integrity [67]. Currently, three TEG® 6s cartridges are Food and Drug Administration (FDA) approved in the United States for adult patients: global hemostasis with lysis, global hemostasis, and the Platelet Mapping adenosine diphosphate (ADP) and arachidonic acid (AA) cartridge. Each has different indications and assay combinations. Although the TEG® 6s and the TEG® 5000 use slightly different mechanisms to assess similar coagulation components, there is a small difference in absolute values of respective parameters of the two devices [62,66,67]. Therefore, the absolute values are not interchangeable. The definition and clinical significance of TEG® 6s parameters are detailed in Table 3 [27].
Table 3.
A description of the four standard VHA assay parameters and their clinical significance with the addition of the most recent tools for measuring POC clot dynamics with the TEG® 5000, TEG® 6s, ROTEM® delta/sigma, Quantra® QPlus®, and the ClotPro® systems [18,27,53,59,65,68,69,70,71,72,73,74].
| Coagulation Event | Main Contributor | TEG® 5000 | TEG® 6s | ROTEM® Delta/Sigma | Quantra® QPlus® QStat® |
ClotPro® | Clinical Significance |
|---|---|---|---|---|---|---|---|
| Clot initiation | Coagulation factors | Reaction time (R), minutes | R | Clotting time (CT), seconds | CT | CT | A short R/CT/CTH time indicates a hypercoagulable state. A prolonged R/CT time indicates either hypocoagulability or the presence of an anticoagulant. A short CTH/CKH in the presence of a long CT /CK-R or CTR > 1.1.indicates the presence of heparin anticoagulation. Specifically, heparin and DOAC tests are available with TEG® 6s, ROTEM® sigma, and ClotPro®. 6 |
| Citrated Kaolin (CK) R-time, minutes | CK-R-time, minutes | INTEM 1 CT | CT | IN-test CT | |||
| rTEG® Activated clotting time (ACT), seconds 1 | Citrated Rapid TEG (CRT) ACT, seconds |
EXTEM 1 CT |
n/a | EX-test CT | |||
| Citrated kaolin-heparinase (CKH) 1 | CKH 1 | HEPTEM 1 CT | Heparinase Clot Time (CTH), seconds | HI-test RVV-test ECA-test NA-test |
|||
| n/a | n/a | n/a | Clot time ratio (CTR) | n/a | |||
| Clot kinetics: amplification | Fibrinogen | Kinetic time (K), minutes | K | Clot formation time (CFT), seconds | Fibrinogen contribution to stiffness (FCS), hPA 2 | CFT | Angle reflects fibrin kinetics, including fibrin formation and cross-linking. FCS measures the direct contribution of stiffness generated by fibrinogen. |
| ɑ angle | ɑ angle | ɑ angle | n/a | ɑ angle | |||
| Citrated functional fibrinogen (MAff/CFF) | MAff/CFF 1 | FIBTEM 1 | n/a | FIB-test 1 | |||
| Clot stiffness: propagation | Fibrinogen, Platelets | CK Maximum amplitude (MA), mm | CK MA, mm | Maximum clot firmness (MCF), mm | Clot stiffness (CS), hPA 2 | MCF | MA, MCF, and CS reflect platelet and fibrinogen contributions to the clot stiffness and full platelet potential under maximal stimulation by thrombin. PCS isolates the platelet contribution to clot stiffness. |
| rTEG® MA, mm | CRT MA, mm | EXTEM 3 MCF | Platelet contribution to clot stiffness (PCS), hPA2 | EX-test MCF 3 | |||
| Clot stability: termination | Fibrinolytic enzymes and inhibitors, Factor XIII | Lysis at 30 min after MA, (LY30), % | LY30 | Clot Lysis Index at 30/60 min after CT (CLI30/CLI60), residual % of MCF 4 Maximum Lysis (ML), % of MCF lysed during run |
Clot Stability to Lysis (CSL), % 5 | Clot Lysis Index at 30/60 min (CLI30/CLI60), % of MCF 4 | Hyperfibrinolysis is suggested by increased clot lysis that starts within 30 min of clot formation. |
| n/a | n/a | APTEM 1 | n/a | AP-test 3 | |||
| n/a | n/a | n/a | n/a | TPA 3 |
1 See Figure 1 and Figure 3 and Table 1 and Table 2 for the definition of the parameters. 2 hPa, hectopascals are units of pressure used to assay clot stiffness in Quantra®. 3 See Section 2.5.3 and Section 2.5.4 in the text and Figure 3 for definitions of the Quantra® and ClotPro® assays and parameters. 4 For the purposes of this review, in ROTEM® sigma/delta and ClotPro®, fibrinolysis is defined uniformly as the clot lysis index (CLI) 5 Measurement of Clot Stability to Lysis (CSL) is only available with the QStat® cartridge. 6 Assays for DOACs (Factor Xa inhibitors and direct thrombin inhibitors) are in various stages of approval for commercial use.
2.5.2. ROTEM® Sigma
The ROTEM® sigma device is a completely automated device which has replaced the practice of pipetting in favor of inserting a tube of blood directly into the instrument. This technology also uses the pin and cup technique similar to the ROTEM® delta. This allows for the use of the same algorithms that are already established for the ROTEM® delta device. Recent papers have been published by teams in Europe approving its comparability with the ROTEM® delta device. Currently, the FDA validation for the specific use of A5 in the USA is pending [12,59,75,76,77]. The definition and clinical significance of the ROTEM® sigma parameters are detailed in Table 3.
2.5.3. Quantra®
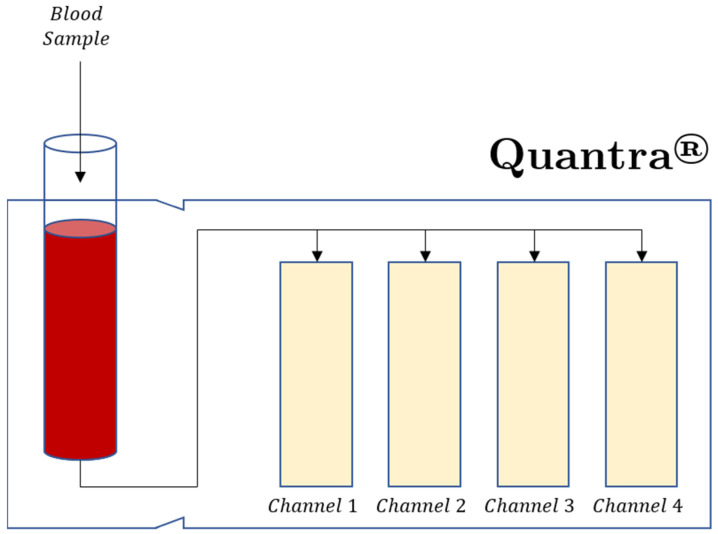
Newer bedside POC VHAs have also recently been reviewed, although the number of these papers is limited, but surely destined to grow with time. The Quantra® analyzer by Hemosonics is an example of one of these new VHAs. The Quantra® VHA is based on the sonic estimation of elasticity via resonance (SEER), or sonorheometry. This is a technology that measures clot time and clot stiffness by using ultrasound to monitor changes in the viscoelastic properties of a whole blood sample during coagulation. Shear modulus is measured by ultrasound without the use of moving mechanical parts or direct contact with the blood sample (Figure 3) [27,78].
Figure 3.
The Quantra® plus cartridge has four channels with reagents designed to measure clot stiffness (CS) and clot time (CT). Channel 1 measures CT with kaolin activation. Channel 2 measures CT with kaolin activation and heparin neutralization. Channel 3 measures CS and tissue factor activation with heparin neutralization. Channel 4 measures CS with tissue factor activation, platelet inhibition, and heparin neutralization. Channel 4 measures the fibrinogen contribution to CS, (FCS). The platelet contribution to CS, (PCS) is equal to CS-FCS. Clot Time Ratio (CTR) = CT/CTH and indicates the level of heparinization of the patient blood sample [69,78].
The Quantra® system is a cartridge-based, fully automated, four-channel device. Currently, the QPlus® cartridge is cleared by the FDA for adult patients and it is indicated for use in the perioperative setting of cardiac and major orthopedic surgery. A second cartridge, QStat®, intended for use in trauma and liver transplant surgery, is currently only available outside the USA. An important distinction between classical VHA technologies and SEER sonorheometry is that SEER sonorheometry is based on direct measurements of the clot’s shear modulus in rational pascal units, an objective parameter that describes the elastic properties of a solid material. It enables Quantra® to provide a true assessment of clot stiffness [79]. Unlike TEG® 5000 and ROTEM® delta tracings, the Quantra® analyzer organizes its test results in three different views: trend data, clot stiffness curves, and dial results. It shows very good correlation with equivalent metrics from other VHA systems [68,70,80,81,82]. It has gained clearance both in Europe and in the US and it is cleared by the FDA for use in cardiac and major orthopedic surgeries. A few studies have reported the use of the Quantra® in coronavirus disease 2019 (COVID-19) patients [80,82,83].
The cartridge-based methodology of the TEG® 6s and Quantra® use dry reagents and are fully automated, providing greater reproducibility and simplified quality assurance for these POC tests [71,74,84]. The definition and clinical significance of the Quantra® parameters are detailed in Table 3.
2.5.4. ClotPro®
The ClotPro® is a viscoelastic cup and pin method like the original cup and pin technologies of the TEG® 5000 and ROTEM® delta analyzers. With ClotPro®, the pin is stationary and the cup spins [65]. ClotPro® has simplified the multiple pipetting procedures involved with the first generation ROTEM® and TEG® with the use of a standard pipette that contains pre-dosed reagents that activate on contact with the blood sample. This sample is deposited into the cup prior to the automatic initiation of the test run. The basic parameters are similar to those of ROTEM® delta with the addition of specialized testing and the exception that the parameters are listed as assays. The assays include specialized tests that are dependent on specific activators and inhibitors. These tests are: the EX-test, activated by recombinant TF, which assesses the extrinsic coagulation pathway and its interaction with blood platelets in citrated blood; the IN-test, which assesses the effect of heparin and is sensitive to FVIII; the HI-test, the IN-test with heparin inhibition; the RVV-test, which is highly sensitive to direct oral anticoagulants (DOAC) and detects Factor Xa (FXa) antagonists in citrated blood; the ECA-test, which is sensitive to and detects direct thrombin inhibitors (DTIs), such as dabigatran; the NA-test, which is a non-activated test; the FIB-test, which involves the examination of the fibrinogen level and fibrin polymerization in citrated blood, and where platelets are inhibited by dual inhibition with cytochalasin D and a synthetic GPIIb/IIIa antagonist); the AP-test, in which fibrinolysis is inhibited in-vitro using aprotinin, a potent direct antagonist of plasmin, the effector protease of fibrinolysis; and the TPA-test, in which the recombinant tissue plasminogen activator (r-tPA) triggers fibrinolysis, permitting the in vitro detection of antifibrinolytic agents in citrated blood. The definition and clinical significance of the ClotPro® parameters are detailed in Table 3 [27].
2.6. Emerging Technologies
The emerging technologies of POC hemostatic assays involve the use of micro/nano electromechanical systems, fluorescent microscopy, photoacoustic detection, microfluidics [85], and electrochemical sensing [86]. Examples of these new technologies are laser speckle rheometry [87,88], mechanical resonant frequency [89], ultrasonic deformation, and parallel plate viscometry [90]. Parallel plate viscometry is a compact system which could be adapted for prehospital areas such as emergency medical services or potentially, in far forward combat areas for goal-directed POC-guided resuscitation [90]. These assays remain an area of vigorous research with emerging clinical applications which are beyond the scope of this commentary [27,91,92,93].
2.7. VHA Limitations
Because of an inherent lack of contact with collagen (representing endothelial disruption) and the lack of variability in shear stress to assess arterial vs. venous systems in the cup and pin technology, the fluid mechanics of VHAs do not replicate vascular hemodynamics. A solution to the biomechanical differences (which are not present in VHAs) is a method of rapid multichannel micro-fluidic detection which has been described to address the lack of venous and arterial sheer forces on the endothelial surface. This ex vivo testing reflects intravascular hemostasis more accurately than the VHAs [94,95].
Other limitations of TEG® and ROTEM® are their inability to detect (due to the overwhelming effect of thrombin) specific platelet receptor abnormalities without the use of specialized testing [96,97]. In addition, the detection of the hemostatic competence of patients treated with DOACs, DTIs, or warfarin also requires specialized reagents and testing. This is because the standard TEG®/ROTEM® parameters demonstrate poor sensitivity within drug concentrations at therapeutic ranges, in addition to poor sensitivity for trough samples, and an overlap with controls. For warfarin, a lack of sensitivity in detecting anticoagulation and a low correlation with thrombin generation assays renders the TEG®/ROTEM® unsuitable for detecting the therapeutic efficacy for heparinized patients [10,98,99,100].
VHAs are not sensitive to von Willebrand disease (vWD). The activation of the von Willebrand factor (vWF) requires high shear rate forces and collagen. Since VHA assesses blood flow under low shear rate, which represents venous flow, the detection of vWD is not possible using standard VHAs. The literature regarding the utilization of VHAs in the assessment of vWD has not demonstrated robust applicability. However, there have been research modifications to TEG® and ROTEM® that attempt to address this limitation. Specialized TEG®, called ristocetin-enhanced TEG with Platelet Mapping® (TEG/PM®), has suggested that the TEG® 5000, as well as ROTEM® delta assays with ristocetin thromboelastometry (RicoTEM®), can be used to assess vWD [101,102,103,104,105,106,107,108].
TEG® without platelet mapping, ROTEM® without platelet assays, and Quantra® are unable to measure the results of antiplatelet therapies (e.g., clopidogrel and aspirin) on the level of inhibition of specific platelet receptor activities [71].
VHAs are not sensitive to the effects of FXa inhibitors (apixaban, rivaroxaban, edoxaban) or DTIs. Modified TEG® and ROTEM® systems have been described that measure the effects of FXa inhibitors, as well as DTIs [17,50,100,109,110,111,112].
TEG® 6s global and Platelet Mapping® cartridges, as well as QPlus® Quantra® cartridges, do not display the lysis parameter. Intensive care patients manifest significant correlation of the MA and R, substantial correlation in α angle and K, but poor correlation in LY30, as measured by the TEG® 6S and TEG® 5000 analyzers. Apart from LY30, the TEG® 6S and TEG® 5000 platforms appear to be interchangeable. This has important implications for use in clinical practice and multi-site research programs [66].
2.8. Viscoelastic Hemostatic Assay Guidance of Blood Component Therapy and Pro-Hemostatic Agents
The use of VHAs to guide BCT, pro-hemostatic agents, and anticoagulants for those on extracorporeal membrane oxygenation (ECMO) represents a conceptual application of precision-based medicine (PBM) whereby each patient’s hemostatic phenotype is defined by the VHA [113,114]. Then, resuscitation or anticoagulation is guided by changes in the individual patient’s evolving phenotype indicated by the VHA parameters. These changes in hemostatic phenotype can be rapid in all areas of bleeding or clotting and are known as moments of “phenotype switching” [17,20,38,113,115]. Targeted, goal-directed administration of BCT, guided by VHA POC testing, allows for a more accurate and personalized method of resuscitation [10,11,113,116,117,118].
2.8.1. General Principles of VHA-Guided BCT, Hemostatic Adjuncts, and Anticoagulation
Tailored resuscitation or anticoagulation of patients with acquired coagulopathies can be achieved with the administration of pro-hemostatic adjuncts, BCT, or anticoagulants in response to the parameters of the VHA. A long CT/R value in hypocoagulopathic patients can be corrected with fresh frozen plasma (FFP) and prothrombin complex concentrate (PCC). For those patients anticoagulated with UFH, a reduction in UFH and/or reversal with protamine sulfate can correct the long CT/R value. Note that there is no standardized TEG protocol for protamine reversal and that these protocols vary by institution [119]. A prolonged CFT/K or decreased α-angle requires fibrinogen concentrates or cryoprecipitate. A narrow MCF/MA may be corrected with fibrinogen concentrate, cryoprecipitate, and platelets. Epsilon aminocaproic acid or tranexamic acid is given for an elevated lysis demonstrated by elevations of parameters such as CLI30 and LY30 [11,120,121,122]. Hypercoagulability in the post-trauma resuscitation period is indicated by a wide MCF (ROTEM®), wide MA (TEG®), a low CLI30/ML (ROTEM®), and a low LY30 (TEG®) [123]. When specific activators or inhibitors are added to the cup to identify specific disruptions in coagulation, such as platelet dysfunction or fibrinogen, tailored therapies may be given [11,31,36]. Sample VHA guidelines are reproduced in Table 4.
Table 4.
| rTEG® Trigger Value | ROTEM® Trigger Value | Intervention |
|---|---|---|
| ACT > 128 s | EXTEM CT > 80 s | PCC/FFP |
| α-angle < 65° MAff/CFF < 11 mm |
EXTEM α-angle < 63° FIBTEM CA10 < 7 mm |
fibrinogen/cryoprecipitate |
| MA < 55 mm | MCF < 45 mm | fibrinogen/cryoprecipitate/platelets |
| LY30/60 > 7.5% 1 citrated TEG/r-TEG |
EXTEM CLI30/60 < 82% ML > 15% 1 |
TXA/aminocaproic acid |
Abbreviations: Activated clotting time (ACT); clot amplitude at 10 min (CA10); clot lysis index 60 min after CT (CLI60); clotting time (CT); extrinsic activator thromboelastometry (EXTEM); fresh frozen plasma (FFP); fibrin-based thromboelastometry (FIBTEM); lysis at 30 min (LY30); maximum amplitude (MA); TEG functional fibrinogen (MAff/CFF); maximum clot firmness (MCF); prothrombin complex concentrate (PCC); Maximum lysis after 30/60 min (ML30/60); rotational thromboelastometry (ROTEM®); RapidTEG® (rTEG®); thromboelastography (TEG®); tranexamic acid (TXA). 1 The values for LY30/60, CLI30/60, and ML as markers for clinically significant fibrinolysis vary significantly in the literature.
2.8.2. Specialized Testing: TEG Platelet Mapping® (TEG/PM®), ROTEM Platelet Analysis®, Isolated Platelet Dysfunction, Multiple Electrode Aggregometry (Multiplate®)
Platelet dysfunction as a manifestation of the early coagulopathy in cases of trauma is a recently described phenomenon. The methodology for determining platelet activation in circulating blood is an area of continued interest since the measurement of platelet activation at the luminal site of the clot does not reflect the platelet activation at the core of the clot at the site of the endothelial injury [125,126,127,128].
An improved survival rate has been demonstrated by epidemiological studies on those combat and civilian patients who received higher ratios of platelets than FFP and red cells [129]. As a result, in massive transfusion protocols, platelets are now given in the earlier rounds of transfusion. However, because ROTEM Platelet Analysis®, TEG/PM®, and Multiplate® rely on completely different technologies, their place in guiding platelet administration in the cases of hemorrhagic shock and massive transfusion remains an area of active research (Table 5) [36,125,127,130]. Therefore, the clinical indications to administer platelets based on these assays remains in the early stages of development [126,131,132].
Table 5.
| VHA | Assay | Reagents | Clinical Significance |
|---|---|---|---|
| TEG/PM® | Kaolin TEG MA | Kaolin | MACK parameter is a proxy for the maximum potential function of the platelets. Thrombin overrides inhibition via anti-platelet agents, thus kaolin-activated TEG® samples will not exhibit their effects. |
| Activator TEG MA | Heparin, reptilase, FXIIIa | MAActivator represents the isolated fibrin contribution to clot strength. Performed alongside K-TEG®. |
|
| TEG MAAA | Heparin, reptilase, FXIIIa, AA | Measures AA contribution of platelet activity to clot strength. Performed alongside K-TEG®. |
|
| TEG MAADP | Heparin, reptilase, FXIIIa, ADP | Measures the ADP/GPIIb/IIIa pathways’ contribution of platelet activity to clot strength. Performed alongside K-TEG®. |
|
| ROTEM Platelet Analysis® | ARATEM | AA | Determines GPIIb/IIIa and COX-1 receptor inhibition. |
| ADPTEM | ADP | Determines GPIIb/IIIa and ADP (P2Y12) receptor inhibition. | |
| TRAPTEM | TRAP-6 | Determines GPIIb/IIIa and thrombin (PAR-1) receptor inhibition. |
Abbreviations: Adenosine di-phosphate (ADP); Adenosine di-phosphate thromboelastometry (ADPTEM); Arachidonic acid (AA); Arachidonic acid thromboelastometry (ARATEM); Citrated kaolin (CK); Kaolin-TEG (K-TEG®); Maximum amplitude (MA); Rotational thromboelastometry (ROTEM); Thrombin receptor-activating peptide-6 (TRAP-6); thrombin receptor-activating peptide thromboelastometry (TRAPTEM); thromboelastography (TEG); TEG® Platelet Mapping (TEG® P/M).
2.8.3. VHAs Reflecting Anticoagulation
Unfractionated heparin activity can be effectively evaluated by VHAs. However, direct and indirect thrombin inhibitors, as well as low molecular weight heparin, cannot be assayed well with unspecialized VHAs. The addition of heparinase to one of the cups allows the VHA assays to quantify the heparin affect, and these assays are therefore used frequently in liver transplantation and cardiac surgery. Most recently, they have been used to monitor ECMO patients, as well as heparinized COVID-19 patients [36,114,133,134,135,136]. The assessment of non-thrombin-based platelet activation/inhibition can be assayed using TEG/PM® and Multiplate®, which is often used in concert with ROTEM®. TEG/PM® parameters of AA and ADP platelet receptor activity and Multiplate® parameters have demonstrated a correlation between the percent of inhibition and the severity of the hemorrhage in bleeding trauma patients [22,36,41,125,127,137,138,139,140,141,142,143,144,145,146]. Moreover, ROTEM® has demonstrated its use for the personalized titration of anticoagulation for patients with difficult coagulopathies. For example, for perioperative patients who require anticoagulation because of the risk of thrombosis, but who also have hypofibrinogenemia, ROTEM® assists in the mitigation of both the bleeding and thrombosis [147].
3. Discussion and Conclusions
Compared to the historically delayed uptake in the use of VHAs, the recent National Institutes of Health and FDA statements, the major international society guidelines from hematology and critical care societies, and the meteoric rise in the number of related papers in the most recent literature since the advent the COVID-19 pandemic have revealed a changing landscape regarding the acceptance of VHAs in guiding the assessment of hemostatic competence in severely bleeding and septic patients [71,134,149,150,151,152,153,154].
Since early 2020, many papers from case reports to narrative and systematic reviews have been published regarding the use of VHAs in the treatment of COVID-19-associated coagulopathy (CAC). Initially, single case reports were often submitted as letters to the editor in order to accelerate the speed of publication. These case reports demonstrated the utility of VHAs to diagnose and treat CAC. In early 2021, narrative and systematic reviews subsequently revealed a common thread describing the reproducible changes in parameters induced by early periods of the cytokine storm. As a result, many prospective, retrospective, and single-center observational studies have been published using ROTEM®, TEG®, and most recently, Quantra® and ClotPro® devices, to study critically ill COVID-19 patients. [134,150,151,155,156,157,158,159]. In a little over a year, the rapid adoption of VHAs to guide prophylactic and anticoagulant therapy in patients with CAC contrasts starkly with the more than the 73-year evolution of the use of these tests in other areas of medical research and practice. This unique period in history called for the adoption of a type of scientific methodology that met the demands of an urgent need to discover valid forms of therapy for these patients. The use of VHAs to define a patient’s hemostatic competence along the pathophysiologic spectrum of coagulopathies that characterize CAC has allowed for the rapid deployment and application of precision-based medicine that defines each patient’s hemostatic phenotype [38,113,134].
During this period in the history of the rapidly evolving COVID-19 pandemic, large randomized controlled trials and Cochrane analyses are not sufficient to determine the utility of the adoption of new technologies that provide individualized therapies to patients to address their evolving hemostatic phenotypes [151,160,161]. Smaller clinical observations, based on a mechanistic rationale, proved useful during the early period of the pandemic for those patients who did not respond to the standard venous thromboembolism (VTE) prophylaxis recommended by many institutions. As a result, after a period of support for the full anticoagulation of severe patients, a high incidence of bleeding was noted, confirming smaller studies involving fully anticoagulated COVID-19 patients [136,162].
In an attempt to accelerate the pace and accuracy of scientific discovery, the rapid deployment of multiplatform RCT (mpRCT)-type studies have been undertaken regarding therapeutic anticoagulation in these patients [163]. These studies have shown that early anticoagulation, with intermediate or full anticoagulation prior to arrival in the intensive care unit, may prevent endotracheal intubation and ECMO, and may reduce mortality [163]. Additionally, one study has shown that VHAs demonstrated platelet-driven hypercoagulability and that some patients may benefit from both anticoagulation and antiplatelet therapy [119]. In this area, it has been suggested that the utilization of VHAs may increase the sensitivity of the monitoring of these patients before and during ICU admission. In none of these mpRCTs have VHAs been uniformly studied and analyzed [67,163,164].
The COVID-19 pandemic has elevated the need for rapid POC testing to gauge the COVID-19 patient’s hemostatic competence, thus ushering in accelerated utilization of the VHAs to diagnose and treat patients with CAC [23,134,135,150,151,153,165,166]. The hypercoagulopathy of CAC inversely mirrors the hypocoagulopathy of many other areas of clinical medicine where hypocoagulopathies can quickly evolve in the medical and surgical intensive care units, obstetrical units, and operating theaters. Relying on CCTs has proven difficult in managing these acquired coagulopathies [7,36,42,126,167,168,169,170,171]. Unlike the hemorrhaging hypocoagulopathic patient, COVID-19 patients most often present with hypercoagulopathic findings and clinical thromboses in all vascular beds as a reflection of the intensity of the cytokine storm [172,173].
Immuno-thrombosis has been described as the dysregulation of the crosstalk between coagulations and immunity [152,173,174]. Since the pathophysiology of CAC involves an endotheliitis which affects all systems, the concept of immuno-thrombotic crosstalk also occurs with the cross-hybridization of the research and clinical experiences of the many specialties which care for patients with endothelial dysfunction, specifically, those specialties that have observed the condition called Shock-Induced Endotheliopathy (SHINE) [175], which often presents with coagulopathies that are a function of immune-thrombotic dysregulation in trauma and sepsis [17,172,175,176].
CAC may be characterized as “upside-down trauma,” whereby COVID-19 patients present in a hypercoagulopathic state but may quickly evolve into a hypocoagulopathic state, opposed to progression of the typical trauma patient [151,173]. The index VHAs of severely bleeding trauma patients begin with hypocoagulopathy, manifested with long R/CT, flat alpha angle, thin MA/MCF, and increased LY30% and ML [10,20]. On the other hand, the index VHAs of hospitalized COVID-19 patients display a hypercoagulopathic presentation [134,150,177,178]. Hypercoagulability in CAC can quickly be modulated by either anticoagulant administration or by the innate changes caused by the vagaries of the cytokine storm. Eventually, these patients are rendered hypocoagulapathic either by anticoagulation or by the natural course of disease. As the cytokine storm recedes, these patients often develop an increased sensitivity to anticoagulation, causing them to bleed at varying times after the institution of anticoagulation. Hence, these patients are said to often “clot and bleed at the same time” [151,162,164,172,179,180,181,182].
Therefore, the monitoring of CAC patients can be quite difficult when the task has fallen to CCTs. As in trauma, adjunctive VHAs have also been used to guide therapies for CAC patients. This is due to the fact that CCTs provide inadequate data in severely hemorrhaging patients. CAC strikes the endothelium, influencing every aspect of anticoagulation from initiation to termination, so more information than what is provided by CCTs is needed [133,160,172]. Increased D-dimer levels have often been described in COVID-19 patients, but the half-life of D-dimer is approximately eight hours or longer in cases of compromised renal function and in elderly patients; this indicates that highly increased D-dimer depicts fibrinolysis that occurred at a point earlier in time rather than fibrinolysis that is currently occurring [178]. COVID-19 patients have also demonstrated a degree of fibrinolytic shutdown as manifested by the increasing thickness of VHA parameters, such as increased MA in TEG® and MCF® in ROTEM, whereby the SARS-CoV-2-mediated elevation of endogenous fibrinolytic inhibitors (e.g., plasminogen activator inhibitor-1 [PAI-1], thrombin activatable fibrinolysis inhibitor [TAFI], and alpha2-antiplasmin) leads to the increased resistance to clot lysis in COVID-19 patients [178,183,184,185]. Moreover, the capacity for thrombin generation has been demonstrated to be normal despite anticoagulation with heparin [184].
Because the endothelium possesses a surface area up to 7000 square meters (the surface area of a soccer pitch), the myriad of hemostatic phenotype changes that can occur in septic and hemorrhagic patients requires POC bedside testing that allows the clinician to adapt to the rapid changes in the hemostatic profiles and phenotypes of these patients [176]. The many interrelated mechanisms of immunologic and thrombotic dysregulation can now be monitored by many specialties at the patient’s bedside. The need to assay every aspect of the life span of a clot has resulted in a recent joining of forces among medical intensivists, anesthesiologists, trauma critical care physicians, transplant surgeons, obstetricians, emergency physicians, pathologists, blood banking specialists, and hematologists. They have gathered to share their experiences with not just the traditional post-operative and intraoperative associated coagulopathies of liver, heart, and trauma-induced coagulopathies, but also in areas where VHAs were less commonly used, such as sepsis-induced coagulopathy, obstetric hemorrhage, major medical hemorrhages, and now CAC [16,17,151]. Hence, every specialty has been confronted with the coagulopathies of COVID-19, and these specialties have reported their diverse respective experiences during the pandemic in the current literature. This meteoric expansion of the literature regarding VHAs and CAC has led to an increased adoption of POC VHAs, assisting clinicians at the bedside in the care of these patients with a significant heterogeneity of results. This heterogeneity is not merely a reflection on the multiple specialties who have been called upon to care for these patients, but also a reflection of the immune-thrombotic crosstalk at the level of the endothelium. This has resulted in a similar crosstalk among the many specialties who care for these patients [71,134,149,150,151,152].
The relatively rapid deployment of VHAs by specialists throughout the world from all areas of medicine has created a formidable foundation of research that allows for such an expansion of this POC bedside technique to monitor hemostatic competence [134,168]. As much as there is a spectrum of coagulopathy, a similar spectrum of inquiry is required that adopts both hypotheses-generating smaller studies and larger randomized control trials with the mpRCT functioning in between [67,151,164,172,173]. Hence, the use of both forms of inquiry will allow multiple specialists treating the endothelial immune-thrombotic derangement of many organs to approach the array of phenotypes of coagulation disorders in the endothelial beds. Thus, hematologists, medical intensivists, anesthesiologists, trauma critical-care surgeons, obstetricians, pathologists, blood banking specialists, as well as emergency physicians, can all contribute to broadening and filling the knowledge gaps within the spectrum of coagulopathies in the many medical specialties by using both CCTs and VHAs to monitor hemostasis across heterogeneous groups of patients.
Author Contributions
Conceptualization, O.V., E.E.M., H.B.M., H.C.K., M.D.N., S.G.T., L.G., R.Z.K., M.Z., D.F. and M.M.W.; writing—original draft preparation, O.V., C.M.B., N.Z., M.D.A.-F., S.S.P., G.W., H.D.A.-F., M.L.M., A.V.T. and M.M.W.; writing—review and editing, O.V., C.M.B., N.Z., E.E.M., H.B.M., H.C.K., M.D.N., M.D.A.-F., S.S.P., G.W., H.D.A.-F., M.L.M., A.V.T., S.G.T., L.G., R.Z.K., P.K., M.Z., D.F. and M.M.W.; visualization, O.V., N.Z., M.D.A.-F. and A.V.T.; supervision, M.M.W.; project administration, C.M.B., N.Z., M.M.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
O.V. is a consultant for Haemonetics Corporation (Boston, MA, USA), served on the Clinical Care Improvement Steering Committee for Diagnostica Stago, Inc., and received honoraria for consultancy outside the submitted work. E.E.M., H.B.M., M.D.N. and M.M.W. have received research grants from Haemonetics Corporation outside the submitted work. M.D.N. has received an honorarium from Haemonetics Corporation for speaking engagements, as well as research support from Janssen Pharmaceuticals (Beerse, Belgium) and Noveome Biotherapeutics (Pittsburgh, PA, USA) outside the submitted work. He has served as a consultant to Janssen and CSL Behring (King of Prussia, PA, USA) and serves on the Scientific Advisory Board of Haima Therapeutics (Cleveland, OH, USA). M.M.W. has received honoraria from Alexion Pharmaceuticals (Boston, MA, USA). D.F. has received study funding, honoraria for consultancy, and shows board activity from Astra Zeneca, AOP orphan, Baxter, Bayer, B. Braun Medical, Biotest, CSL Behring, Delta Select, Dade Behring, Edwards, Fresenius, Glaxo, Haemoscope, Hemogem, Lilly, LFB, Mitsubishi Pharma, Novo Nordisk, Octapharma, Pfizer, and Tem Innovations outside the submitted work.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Starzl T.E. The saga of liver replacement, with particular reference to the reciprocal influence of liver and kidney transplantation (1955–1967) J. Am. Coll. Surg. 2002;195:587–610. doi: 10.1016/S1072-7515(02)01498-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Groth C.G., Pechet L., Starzl T.E. Coagulation during and after orthotopic transplantation of the human liver. Arch. Surg. 1969;98:31–34. doi: 10.1001/archsurg.1969.01340070049006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kang Y.G., Martin D.J., Marquez J., Lewis J.H., Bontempo F.A., Shaw B.W., Jr., Starzl T.E., Winter P.M. Intraoperative changes in blood coagulation and thrombelastographic monitoring in liver transplantation. Anesth. Analg. 1985;64:888–896. doi: 10.1213/00000539-198509000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Starzl T.E., Marchioro T.L., Vonkaulla K.N., Hermann G., Brittain R.S., Waddell W.R. Homotransplantation of the Liver in Humans. Surg. Gynecol. Obstet. 1963;117:659–676. [PMC free article] [PubMed] [Google Scholar]
- 5.Shore-Lesserson L., Manspeizer H.E., DePerio M., Francis S., Vela-Cantos F., Ergin M.A. Thromboelastography-guided transfusion algorithm reduces transfusions in complex cardiac surgery. Anesth. Analg. 1999;88:312–319. doi: 10.1213/00000539-199902000-00016. [DOI] [PubMed] [Google Scholar]
- 6.Spiess B.D., Gillies B.S.A., Chandler W., Verrier E. Changes in transfusion therapy and reexploration rate after institution of a blood management program in cardiac surgical patients. J. Cardiothorac. Vasc. Anesth. 1995;9:168–173. doi: 10.1016/S1053-0770(05)80189-2. [DOI] [PubMed] [Google Scholar]
- 7.Holcomb J.B., Minei K.M., Scerbo M.L., Radwan Z.A., Wade C.E., Kozar R.A., Gill B.S., Albarado R., McNutt M.K., Khan S., et al. Admission rapid thrombelastography can replace conventional coagulation tests in the emergency department: Experience with 1974 consecutive trauma patients. Ann. Surg. 2012;256:476–486. doi: 10.1097/SLA.0b013e3182658180. [DOI] [PubMed] [Google Scholar]
- 8.Schöchl H., Voelckel W., Schlimp C.J. Management of traumatic haemorrhage–the European perspective. Anaesthesia. 2015;70:e102–e137. doi: 10.1111/anae.12901. [DOI] [PubMed] [Google Scholar]
- 9.Enriquez L.J., Shore-Lesserson L. Point-of-Care coagulation testing and transfusion algorithms. Br. J. Anaesth. 2009;103:i14–i22. doi: 10.1093/bja/aep318. [DOI] [PubMed] [Google Scholar]
- 10.Walsh M., Fritz S., Hake D., Son M., Greve S., Jbara M., Chitta S., Fritz B., Miller A., Bader M.K., et al. Targeted Thromboelastographic (TEG) Blood Component and Pharmacologic Hemostatic Therapy in Traumatic and Acquired Coagulopathy. Curr. Drug. Targets. 2016;17:954–970. doi: 10.2174/1389450117666160310153211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schöchl H., Maegele M., Solomon C., Görlinger K., Voelckel W. Early and individualized goal-directed therapy for trauma-induced coagulopathy. Scand. J. Trauma Resusc. Emerg. Med. 2012;20:15. doi: 10.1186/1757-7241-20-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Veigas P.V., Callum J., Rizoli S., Nascimento B., da Luz L.T. A systematic review on the rotational thrombelastometry (ROTEM®) values for the diagnosis of coagulopathy, prediction and guidance of blood transfusion and prediction of mortality in trauma patients. Scand. J. Trauma Resusc. Emerg. Med. 2016;24:114. doi: 10.1186/s13049-016-0308-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hunt H., Stanworth S., Curry N., Woolley T., Cooper C., Ukoumunne O., Zhelev Z., Hyde C. Thromboelastography (TEG) and rotational thromboelastometry (ROTEM) for trauma-induced coagulopathy in adult trauma patients with bleeding. Cochrane Libr. 2015;2:CD010438. doi: 10.1002/14651858.CD010438.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wikkelsø A., Wetterslev J., Møller A.M., Afshari A. Thromboelastography (TEG) or thromboelastometry (ROTEM) to monitor haemostatic treatment versus usual care in adults or children with bleeding. Cochrane Database Syst. Rev. 2016;2016:CD007871. doi: 10.1002/14651858.CD007871.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wikkelsø A., Wetterslev J., Møller A.M., Afshari A. Thromboelastography (TEG) or rotational thromboelastometry (ROTEM) to monitor haemostatic treatment in bleeding patients: A systematic review with meta-analysis and trial sequential analysis. Anaesthesia. 2017;72:519–531. doi: 10.1111/anae.13765. [DOI] [PubMed] [Google Scholar]
- 16.Bugaev N., Como J.J., Golani G., Freeman J.J., Sawhney J.S., Vatsaas C.J., Yorkgitis B.K., Kreiner L.A., Garcia N.M., Aziz H.A. Thromboelastography and Rotational Thromboelastometry in Bleeding Patients with Coagulopathy: Practice Management Guideline from the Eastern Association for the Surgery of Trauma. J. Trauma Acute Care Surg. 2020;89:999–1017. doi: 10.1097/TA.0000000000002944. [DOI] [PubMed] [Google Scholar]
- 17.Walsh M., Thomas S., Kwaan H., Aversa J., Anderson S., Sundararajan R., Zimmer D., Bunch C., Stillson J., Draxler D. Modern methods for monitoring hemorrhagic resuscitation in the United States: Why the delay? J. Trauma Acute Care Surg. 2020;89:1018–1022. doi: 10.1097/TA.0000000000002977. [DOI] [PubMed] [Google Scholar]
- 18.Sahli S.D., Rössler J., Tscholl D.W., Studt J.-D., Spahn D.R., Kaserer A. Point-of-care diagnostics in coagulation management. Sensors. 2020;20:4254. doi: 10.3390/s20154254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Černý V., Maegele M., Agostini V., Fries D., Leal-Noval S.R., Nardai G., Nardi G., Östlund A., Schöchl H. Variations and obstacles in the use of coagulation factor concentrates for major trauma bleeding across Europe: Outcomes from a European expert meeting. Eur. J. Trauma Emerg. Surg. 2021:1–12. doi: 10.1007/s00068-020-01563-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moore E.E., Moore H.B., Kornblith L.Z., Neal M.D., Hoffman M., Mutch N.J., Schöchl H., Hunt B.J., Sauaia A. Trauma-induced coagulopathy. Nat. Rev. Dis. Primers. 2021;7:30. doi: 10.1038/s41572-021-00264-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johansson P.I. Goal-Directed hemostatic resuscitation for massively bleeding patients: The Copenhagen concept. Transfus. Apher. Sci. 2010;43:401–405. doi: 10.1016/j.transci.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 22.Tanaka K.A., Ogawa S., Bolliger D. A primer for clinical use of rotational thromboelastometry. Point Care. 2012;11:77–84. doi: 10.1097/POC.0b013e318259b18a. [DOI] [Google Scholar]
- 23.Görlinger K., Almutawah H., Almutawaa F., Alwabari M., Alsultan Z., Almajed J., Alwabari M., Alsultan M., Shahwar D., Yassen K.A. The role of rotational thromboelastometry during the COVID-19 pandemic: A narrative review. Korean J. Anesthesiol. 2021;74:91. doi: 10.4097/kja.21006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Snegovskikh D., Souza D., Walton Z., Dai F., Rachler R., Garay A., Snegovskikh V.V., Braveman F.R., Norwitz E.R. Point-of-Care viscoelastic testing improves the outcome of pregnancies complicated by severe postpartum hemorrhage. J. Clin. Anesth. 2018;44:50–56. doi: 10.1016/j.jclinane.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 25.McNamara H., Mallaiah S. Managing coagulopathy following PPH. Best Pract. Res. Clin. Obs. Gynaecol. 2019;61:106–120. doi: 10.1016/j.bpobgyn.2019.04.002. [DOI] [PubMed] [Google Scholar]
- 26.Meyers M.A., Chawla K.K. Mechanical Behavior of Materials. Cambridge University Press; Cambridge, UK: 2009. [Google Scholar]
- 27.Hartmann J., Murphy M., Dias J.D. Viscoelastic hemostatic assays: Moving from the laboratory to the site of care—A review of established and emerging technologies. Diagnostics. 2020;10:118. doi: 10.3390/diagnostics10020118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gonzalez E., Pieracci F.M., Moore E.E., Kashuk J.L. Coagulation abnormalities in the trauma patient: The role of point-of-care thromboelastography. Semin. Thromb. Hemost. 2010;36:723–737. doi: 10.1055/s-0030-1265289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kashuk J., Moore E., Sawyer M., Wohlauer M., Pezold M., Barnett C., Biffl W., Burlew C., Johnson J., Sauaia A. Primary fibrinolysis is integral in the pathogenesis of the acute coagulopathy of trauma. Ann. Surg. 2010;252:434–444. doi: 10.1097/SLA.0b013e3181f09191. [DOI] [PubMed] [Google Scholar]
- 30.MacDonald S.G., Luddington R.J. Critical factors contributing to the thromboelastography trace. Semin. Thromb. Hemost. 2010;36:712–722. doi: 10.1055/s-0030-1265288. [DOI] [PubMed] [Google Scholar]
- 31.Luddington R.J. Thrombelastography/thromboelastometry. Clin. Lab. Haematol. 2005;27:81–90. doi: 10.1111/j.1365-2257.2005.00681.x. [DOI] [PubMed] [Google Scholar]
- 32.Schochl H., Voelckel W., Grassetto A., Schlimp C.J. Practical application of point-of-care coagulation testing to guide treatment decisions in trauma. J. Trauma Acute Care Surg. 2013;74:1587–1598. doi: 10.1097/TA.0b013e31828c3171. [DOI] [PubMed] [Google Scholar]
- 33.Einersen P.M., Moore E.E., Chapman M.P., Moore H.B., Gonzalez E., Silliman C.C., Banerjee A., Sauaia A. Rapid-Thrombelastography (r-TEG) thresholds for goal-directed resuscitation of patients at risk for massive transfusion. J. Trauma Acute Care Surg. 2017;82:114. doi: 10.1097/TA.0000000000001270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Laursen T.H., Meyer M.A., Meyer A.S.P., Gaarder T., Naess P.A., Stensballe J., Ostrowski S.R., Johansson P.I. Thrombelastography early amplitudes in bleeding and coagulopathic trauma patients: Results from a multicenter study. J. Trauma Acute Care Surg. 2018;84:334–341. doi: 10.1097/TA.0000000000001735. [DOI] [PubMed] [Google Scholar]
- 35.Wirtz M.R., Baumann H.M., Klinkspoor J.H., Goslings J.C., Juffermans N.P. Viscoelastic testing in trauma. Semin. Thromb. Hemost. 2017;43:375–385. doi: 10.1055/s-0037-1598057. [DOI] [PubMed] [Google Scholar]
- 36.Curry N.S., Davenport R., Pavord S., Mallett S.V., Kitchen D., Klein A.A., Maybury H., Collins P.W., Laffan M. The use of viscoelastic haemostatic assays in the management of major bleeding: A British Society for Haematology Guideline. Br. J. Haematol. 2018;182:789–806. doi: 10.1111/bjh.15524. [DOI] [PubMed] [Google Scholar]
- 37.Gorlinger K., Bhardwaj V., Kapoor P.M. Simulation in coagulation testing using rotational thromboelastometry: A fast emerging, reliable point of care technique. Ann. Card. Anaesth. 2016;19:516–520. doi: 10.4103/0971-9784.185546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stettler G.R., Moore E.E., Moore H.B., Nunns G.R., Silliman C.C., Banerjee A., Sauaia A. Redefining postinjury fibrinolysis phenotypes using two viscoelastic assays. J. Trauma Acute Care Surg. 2019;86:679–685. doi: 10.1097/TA.0000000000002165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hartmann J., Sikorski R.A. Thromboelastography (TEG® 5000 and TEG® 6s Hemostasis Analyzers with TEG Manager® Software) In: Moore H.B., Moore E.E., Neal M.D., editors. Trauma Induced Coagulopathy. 2nd ed. Spring Nature Switzerland AG; Cham, Switzerland: 2021. pp. 313–331. [Google Scholar]
- 40.Bocci M., Maviglia R., Consalvo L., Grieco D., Montini L., Mercurio G., Nardi G., Pisapia L., Cutuli S., Biasucci D. Thromboelastography clot strength profiles and effect of systemic anticoagulation in COVID-19 acute respiratory distress syndrome: A prospective, observational study. Eur. Rev. Med. Pharmacol. Sci. 2020;24:12466–12479. doi: 10.26355/eurrev_202012_24043. [DOI] [PubMed] [Google Scholar]
- 41.Whiting P., Al M., Westwood M., Ramos I.C., Ryder S., Armstrong N., Misso K., Ross J., Severens J., Kleijnen J. Viscoelastic point-of-care testing to assist with the diagnosis, management and monitoring of haemostasis: A systematic review and cost-effectiveness analysis. Health Technol. Assess. 2015;19:1–228. doi: 10.3310/hta19580. v–vi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Johansson P.I., Stensballe J., Oliveri R., Wade C.E., Ostrowski S.R., Holcomb J.B. How I treat patients with massive hemorrhage. Blood. 2014;124:3052–3058. doi: 10.1182/blood-2014-05-575340. [DOI] [PubMed] [Google Scholar]
- 43.Stein P., Kaserer A., Spahn G.H., Spahn D.R. Point-of-Care Coagulation Monitoring in Trauma Patients. Semin. Thromb. Hemost. 2017;43:367–374. doi: 10.1055/s-0037-1598062. [DOI] [PubMed] [Google Scholar]
- 44.Sankarankutty A., Nascimento B., da Luz L.T., Rizoli S. TEG® and ROTEM® in trauma: Similar test but different results? World J. Emerg. Surg. 2012;7:S3. doi: 10.1186/1749-7922-7-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Walsh M., Moore E.E., Moore H., Thomas S., Lune S.V., Zimmer D., Dynako J., Hake D., Crowell Z., McCauley R. Use of Viscoelastography in Malignancy-Associated Coagulopathy and Thrombosis: A Review. Semin. Thromb. Hemost. 2019;45:354–372. doi: 10.1055/s-0039-1688497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schöchl H. Use of Viscoelastography in Malignancy-Associated Coagulopathy and Thrombosis: A Review. J. Trauma Acute Care Surg. 2013;74:1587–1598. doi: 10.1097/TA.0b013e31828c3171. [DOI] [PubMed] [Google Scholar]
- 47.Lang T., Bauters A., Braun S.L., Pötzsch B., von Pape K.-W., Kolde H.-J., Lakner M. Multi-centre investigation on reference ranges for ROTEM thromboelastometry. Blood Coagul. Fibrinolysis. 2005;16:301–310. doi: 10.1097/01.mbc.0000169225.31173.19. [DOI] [PubMed] [Google Scholar]
- 48.Haemonetics Corporation. Introducing TEG 6s—White Paper. [(accessed on 4 February 2022)]. Available online: https://pdf.medicalexpo.com/pdf/haemonetics/introducing-teg-6s-white-paper/78504-152619.html.
- 49.Thromboelastography (TEG) Is available 24/7 at UCM. [(accessed on 4 February 2022)]. Available online: https://uchicagomedlabs.testcatalog.org/catalogs/367/files/12824.
- 50.Hartmann J., Walsh M., Grisoli A., Thomas A.V., Shariff F., McCauley R., Lune S.V., Zackariya N., Patel S., Farrell M.S., et al. Diagnosis and Treatment of Trauma-Induced Coagulopathy by Viscoelastography. Semin. Thromb. Hemost. 2020;46:134–146. doi: 10.1055/s-0040-1702171. [DOI] [PubMed] [Google Scholar]
- 51.Cotton B.A., Faz G., Hatch Q.M., Radwan Z.A., Podbielski J., Wade C., Kozar R.A., Holcomb J.B. Rapid Thrombelastography Delivers Real-Time Results That Predict Transfusion Within 1 Hour of Admission. J. Trauma Acute Care Surg. 2011;71:407–417. doi: 10.1097/TA.0b013e31821e1bf0. [DOI] [PubMed] [Google Scholar]
- 52.Cotton B.A., Minei K.M., Radwan Z.A., Matijevic N., Pivalizza E., Podbielski J., Wade C.E., Kozar R.A., Holcomb J.B. Admission rapid thrombelastography predicts development of pulmonary embolism in trauma patients. J. Trauma Acute Care Surg. 2012;72:1470–1477. doi: 10.1097/TA.0b013e31824d56ad. [DOI] [PubMed] [Google Scholar]
- 53.Görlinger K., Dirkmann D., Hanke A.A. Rotational Thromboelastometry (ROTEM®) In: Moore H.B., Moore E.E., Neal M.D., editors. Trauma Induced Coagulopathy. 2nd ed. Spring Nature Switzerland AG; Cham, Switzerland: 2021. pp. 279–312. [Google Scholar]
- 54.Simurda T., Asselta R., Zolkova J., Brunclikova M., Dobrotova M., Kolkova Z., Loderer D., Skornova I., Hudecek J., Lasabova Z., et al. Congenital Afibrinogenemia and Hypofibrinogenemia: Laboratory and Genetic Testing in Rare Bleeding Disorders with Life-Threatening Clinical Manifestations and Challenging Management. Diagnostics. 2021;11:2140. doi: 10.3390/diagnostics11112140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Niles S.E., McLaughlin D.F., Perkins J.G., Wade C.E., Li Y., Spinella P.C., Holcomb J.B. Increased mortality associated with the early coagulopathy of trauma in combat casualties. J. Trauma. 2008;64:1459–1463; discussion 1463–1465. doi: 10.1097/TA.0b013e318174e8bc. [DOI] [PubMed] [Google Scholar]
- 56.Meyer A.S., Meyer M.A., Sorensen A.M., Rasmussen L.S., Hansen M.B., Holcomb J.B., Cotton B.A., Wade C.E., Ostrowski S.R., Johansson P.I. Thrombelastography and rotational thromboelastometry early amplitudes in 182 trauma patients with clinical suspicion of severe injury. J. Trauma Acute Care Surg. 2014;76:682–690. doi: 10.1097/TA.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 57.Hunt B.J., Lyons G. Thromboelastography should be available in every labour ward. Int. J. Obstet. Anesth. 2005;14:324–325. doi: 10.1016/j.ijoa.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 58.Görlinger K., Pérez-Ferrer A., Dirkmann D., Saner F., Maegele M., Calatayud Á.A.P., Kim T.-Y. The role of evidence-based algorithms for rotational thromboelastometry-guided bleeding management. Korean J. Anesthesiol. 2019;72:297–322. doi: 10.4097/kja.19169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Görlinger K., Iqbal J., Dirkmann D., Tanaka K.A. Whole Blood Assay: Thromboelastometry. In: Teruya J., editor. Management of Bleeding Patients. Spring Nature Switzerland AG; Cham, Switzerland: 2021. pp. 45–87. [Google Scholar]
- 60.Whiting D., DiNardo J.A. TEG and ROTEM: Technology and clinical applications. Am. J. Hematol. 2014;89:228–232. doi: 10.1002/ajh.23599. [DOI] [PubMed] [Google Scholar]
- 61.Ganter M.T., Hofer C.K. Coagulation monitoring: Current techniques and clinical use of viscoelastic point-of-care coagulation devices. Anesth. Analg. 2008;106:1366–1375. doi: 10.1213/ane.0b013e318168b367. [DOI] [PubMed] [Google Scholar]
- 62.Haemonetics Corporation TEG 6s Hemostasis System. No. 02184. U.S. Patent. 2019
- 63.Gurbel P.A., Bliden K.P., Tantry U.S., Monroe A.L., Muresan A.A., Brunner N.E., Lopez-Espina C.G., Delmenico P.R., Cohen E., Raviv G., et al. First report of the point-of-care TEG: A technical validation study of the TEG-6S system. Platelets. 2016;27:642–649. doi: 10.3109/09537104.2016.1153617. [DOI] [PubMed] [Google Scholar]
- 64.Dias J.D., Haney E.I., Mathew B.A., Lopez-Espina C.G., Orr A.W., Popovsky M.A. New-Generation Thromboelastography: Comprehensive Evaluation of Citrated and Heparinized Blood Sample Storage Effect on Clot-Forming Variables. Arch. Pathol. Lab. Med. 2017;141:569–577. doi: 10.5858/arpa.2016-0088-OA. [DOI] [PubMed] [Google Scholar]
- 65.Leyser H. Devices and Methods for Measuring Viscoelastic Changes of a Sample. Patent No. WO 2018/137766 Al. [(accessed on 6 January 2022)];2018 Available online: https://patentimages.storage.googleapis.com/08/d3/f3/f31384ed000c19/WO2018137766A1.pdf.
- 66.Lloyd-Donald P., Churilov L., Zia F., Bellomo R., Hart G., McCall P., Mårtensson J., Glassford N., Weinberg L. Assessment of agreement and interchangeability between the TEG5000 and TEG6S thromboelastography haemostasis analysers: A prospective validation study. BMC Anesthesiol. 2019;19:45. doi: 10.1186/s12871-019-0717-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Neal M.D., Moore E.E., Walsh M., Thomas S., Callcut R.A., Kornblith L.Z., Schreiber M., Ekeh A.P., Singer A.J., Lottenberg L. A comparison between the TEG 6s and TEG 5000 analyzers to assess coagulation in trauma patients. J. Trauma Acute Care Surg. 2020;88:279–285. doi: 10.1097/TA.0000000000002545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hauck J., Welsby I.J., Groves D.S., Naik B., Tanaka K., Finley A., Greenberg C., Viola F., Winegar D. American Society of Anesthesiologist Annual Meeting. 2001. [(accessed on 6 January 2022)]. Multi-Center Investigation of the Clinical Performance of the Quantra System versus the Rotem Delta in Surgical Patients. Available online: http://www.asaabstracts.com/strands/asaabstracts/abstract.htm?year=2018&index=8&absnum=4844. [Google Scholar]
- 69.Groves D.S., Winegar D.A., Fernandez L.G., Huffmyer J.L., Viola F. Comparison of Coagulation Parameters in Arterial and Venous Blood in Cardiac Surgery Measured Using the Quantra System. J. Cardiothorac. Vasc. Anesth. 2019;33:976–984. doi: 10.1053/j.jvca.2018.08.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Groves D.S., Welsby I.J., Naik B.I., Tanaka K., Hauck J.N., Greenberg C.S., Winegar D.A., Viola F. Multicenter evaluation of the Quantra QPlus system in adult patients undergoing major surgical procedures. Anesth. Analg. 2020;130:899–909. doi: 10.1213/ANE.0000000000004659. [DOI] [PubMed] [Google Scholar]
- 71.Volod O., Selby R., Gil M.R., Kreuziger L.B., Lee A.Y. COVID-19 and Viscoelastic Hemostasis Assays: Frequently Asked Questions. [(accessed on 19 June 2021)]. Available online: https://www.hematology.org/covid-19/covid-19-and-ve.
- 72.Hemosonics Quantra® Hemostasis System Brochure. [(accessed on 4 February 2022)]. Available online: https://hemosonics.com/wp-content/uploads/2020/10/HemoSonics-Quantra-Brochure.pdf.
- 73.ClotPro ClotPro® System New Generation Viscoelastic Diagnostics. [(accessed on 21 June 2021)]. Available online: https://www.clot.pro/site/assets/files/1053/product_specification_rev001_enicor_en_2019_06.pdf.
- 74.Carll T., Wool G.D. Basic principles of viscoelastic testing. Transfusion. 2020;60:S1–S9. doi: 10.1111/trf.16071. [DOI] [PubMed] [Google Scholar]
- 75.Gillissen A., van den Akker T., Caram-Deelder C., Henriquez D.D., Bloemenkamp K.W., Eikenboom J., van der Bom J.G., de Maat M.P. Comparison of thromboelastometry by ROTEM® Delta and ROTEM® Sigma in women with postpartum haemorrhage. Scand. J. Clin. Lab. Investig. 2019;79:32–38. doi: 10.1080/00365513.2019.1571220. [DOI] [PubMed] [Google Scholar]
- 76.Schenk B., Görlinger K., Treml B., Tauber H., Fries D., Niederwanger C., Oswald E., Bachler M. A comparison of the new ROTEM® sigma with its predecessor, the ROTEMdelta. Anaesthesia. 2019;74:348–356. doi: 10.1111/anae.14542. [DOI] [PubMed] [Google Scholar]
- 77.Simurda T., Zolkova J., Snahnicanova Z., Loderer D., Skornova I., Sokol J., Hudecek J., Stasko J., Lasabova Z., Kubisz P. Identification of Two Novel Fibrinogen Bβ Chain Mutations in Two Slovak Families with Quantitative Fibrinogen Disorders. Int. J. Mol. Sci. 2017;19:100. doi: 10.3390/ijms19010100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Allen T.W., Winegar D., Viola F. The Quantra® System and SEER Sonorheometry. In: Moore H.B., Moore E.E., Neal M.D., editors. Trauma Induced Coagulopathy. 2nd ed. Spring Nature Switzerland AG; Cham, Switzerland: 2021. pp. 693–704. [Google Scholar]
- 79.Hochleitner G., Sutor K., Levett C., Leyser H., Schlimp C.J., Solomon C. Revisiting Hartert’s 1962 calculation of the physical constants of thrombelastography. Clin. Appl. Thromb. Hemost. 2017;23:201–210. doi: 10.1177/1076029615606531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Huffmyer J.L., Fernandez L.G., Haghighian C., Terkawi A.S., Groves D.S. Comparison of SEER Sonorheometry With Rotational Thromboelastometry and Laboratory Parameters in Cardiac Surgery. Anesth. Analg. 2016;123:1390–1399. doi: 10.1213/ANE.0000000000001507. [DOI] [PubMed] [Google Scholar]
- 81.Naik B.I., Durieux M.E., Knisely A., Sharma J., Bui-Huynh V.C., Yalamuru B., Terkawi A.S., Nemergut E.C. SEER sonorheometry versus rotational thromboelastometry in large volume blood loss spine surgery. Anesth. Analg. 2016;123:1380–1389. doi: 10.1213/ANE.0000000000001509. [DOI] [PubMed] [Google Scholar]
- 82.Reynolds P.S., Middleton P., McCarthy H., Spiess B.D. A Comparison of a New Ultrasound-Based Whole Blood Viscoelastic Test (SEER Sonorheometry) Versus Thromboelastography in Cardiac Surgery. Anesth. Analg. 2016;123:1400–1407. doi: 10.1213/ANE.0000000000001362. [DOI] [PubMed] [Google Scholar]
- 83.Baryshnikova E., Di Dedda U., Ranucci M. A Comparative Study of SEER Sonorheometry Versus Standard Coagulation Tests, Rotational Thromboelastometry, and Multiple Electrode Aggregometry in Cardiac Surgery. J. Cardiothorac. Vasc. Anesth. 2019;33:1590–1598. doi: 10.1053/j.jvca.2019.01.011. [DOI] [PubMed] [Google Scholar]
- 84.Selby R. “TEG talk”: Expanding clinical roles for thromboelastography and rotational thromboelastometry. Hematol. Am. Soc. Hematol. Educ. Program. 2020;2020:67–75. doi: 10.1182/hematology.2020000090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Diamond S.L., Rossi J.M. Point of care whole blood microfluidics for detecting and managing thrombotic and bleeding risks. Lab Chip. 2021;21:3667–3674. doi: 10.1039/D1LC00465D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mohammadi Aria M., Erten A., Yalcin O. Technology advancements in blood coagulation measurements for point-of-care diagnostic testing. Front. Bioeng. Biotechnol. 2019;7:395. doi: 10.3389/fbioe.2019.00395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Nadkarni S.K. Optical thromboelastography system and method for evaluation of blood coagulation metrics. J. Biophotonics. 2015;8:372–381. doi: 10.1002/jbio.201300197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Nadkarni S.K. Comprehensive coagulation profiling at the point-of-care using a novel laser-based approach. Semin. Thromb. Hemost. 2019;45:264–274. doi: 10.1055/s-0039-1683842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Abhishek R., Yoshimizu N. Methods, Devices, and Systems for Measuring Physical Properties of Fluid. Patent No. US 2013/0192349 A1. [(accessed on 6 January 2022)];2016 Available online: https://patentimages.storage.googleapis.com/40/1b/79/6e41ce3defdfbc/US20130192349A1.pdf.
- 90.Dennis R.G., Fischer T.H., Dacorta J.A. Portable Coagulation Monitoring Device and Method of Assessing Coagulation Response. Patent No. WO/2011/075614. [(accessed on 6 January 2022)];2013 Available online: https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2011075614.
- 91.Peng H.T. Hemostatic agents for prehospital hemorrhage control: A narrative review. Mil. Med. Res. 2020;7:13. doi: 10.1186/s40779-020-00241-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ziegler B., Bachler M., Haberfellner H., Niederwanger C., Innerhofer P., Hell T., Kaufmann M., Maegele M., Martinowitz U., Nebl C., et al. Efficacy of prehospital administration of fibrinogen concentrate in trauma patients bleeding or presumed to bleed (FIinTIC): A multicentre, double-blind, placebo-controlled, randomised pilot study. Eur. J. Anaesthesiol. 2021;38:348–357. doi: 10.1097/EJA.0000000000001366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Prat N.J., Meyer A.D., Ingalls N.K., Trichereau J., DuBose J.J., Cap A.P. Rotational thromboelastometry significantly optimizes transfusion practices for damage control resuscitation in combat casualties. J. Trauma Acute Care Surg. 2017;83:373. doi: 10.1097/TA.0000000000001568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Walsh M., Shreve J., Thomas S., Moore E., Moore H., Hake D., Pohlman T., Davis P., Ploplis V., Piscoya A. Fibrinolysis in trauma:“myth,”“reality,” or “something in between”. Semin. Thromb. Hemost. 2017;43:200–212. doi: 10.1055/s-0036-1597900. [DOI] [PubMed] [Google Scholar]
- 95.Li R., Elmongy H., Sims C., Diamond S.L. Ex Vivo recapitulation of trauma-induced coagulopathy and assessment of trauma patient platelet function under flow using microfluidic technology. J. Trauma Acute Care Surg. 2016;80:440. doi: 10.1097/TA.0000000000000915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bochsen L., Wiinberg B., Kjelgaard-Hansen M., Steinbrüchel D.A., Johansson P.I. Evaluation of the TEG® platelet mapping™ assay in blood donors. Thromb. J. 2007;5:3. doi: 10.1186/1477-9560-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Craft R.M., Chavez J.J., Bresee S.J., Wortham D.C., Cohen E., Carroll R.C. A novel modification of the Thrombelastograph assay, isolating platelet function, correlates with optical platelet aggregation. J. Lab. Clin. Med. 2004;143:301–309. doi: 10.1016/j.lab.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 98.Schmidt D.E., Chaireti R., Bruzelius M., Holmström M., Antovic J., Ågren A. Correlation of thromboelastography and thrombin generation assays in warfarin-treated patients. Thromb. Res. 2019;178:34–40. doi: 10.1016/j.thromres.2019.03.022. [DOI] [PubMed] [Google Scholar]
- 99.Gosselin R.C., Adcock D.M., Bates S.M., Douxfils J., Favaloro E.J., Gouin-Thibault I., Guillermo C., Kawai Y., Lindhoff-Last E., Kitchen S. International Council for Standardization in Haematology (ICSH) recommendations for laboratory measurement of direct oral anticoagulants. Thromb. Haemost. 2018;118:437–450. doi: 10.1055/s-0038-1627480. [DOI] [PubMed] [Google Scholar]
- 100.Dias J.D., Lopez-Espina C.G., Ippolito J., Hsiao L.H., Zaman F., Muresan A.A., Thomas S.G., Walsh M., Jones A.J., Grisoli A., et al. Rapid point-of-care detection and classification of direct-acting oral anticoagulants with the TEG 6s: Implications for trauma and acute care surgery. J. Trauma Acute Care Surg. 2019;87:364–370. doi: 10.1097/TA.0000000000002357. [DOI] [PubMed] [Google Scholar]
- 101.Regling K., Kakulavarapu S., Thomas R., Hollon W., Chitlur M.B. Utility of thromboelastography for the diagnosis of von Willebrand disease. Pediatr. Blood Cancer. 2019;66:e27714. doi: 10.1002/pbc.27714. [DOI] [PubMed] [Google Scholar]
- 102.Topf H.-G., Weiss D., Lischetzki G., Strasser E., Rascher W., Rauh M. Evaluation of a modified thromboelastography assay for the screening of von Willebrand disease. Thromb. Haemost. 2011;105:1091–1099. doi: 10.1160/TH10-12-0782. [DOI] [PubMed] [Google Scholar]
- 103.Toukh M., Ozelo M., Angelillo-Scherrer A., Othman M. A novel use of thromboelastography in type 2B von Willebrand disease. Int. J. Lab. Hematol. 2013;35:e11–e14. doi: 10.1111/ijlh.12095. [DOI] [PubMed] [Google Scholar]
- 104.Guzman-Reyes S., Osborne C., Pivalizza E.G. Thrombelastography for perioperative monitoring in patients with von Willebrand disease. J. Clin. Anesth. 2012;24:166–167. doi: 10.1016/j.jclinane.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 105.Schmidt D.E., Majeed A., Bruzelius M., Odeberg J., Holmström M., Ågren A. A prospective diagnostic accuracy study evaluating rotational thromboelastometry and thromboelastography in 100 patients with von Willebrand disease. Haemophilia. 2017;23:309–318. doi: 10.1111/hae.13121. [DOI] [PubMed] [Google Scholar]
- 106.Boyd E.Z., Riha K., Escobar M.A., Pivalizza E.G. Thrombelastograph platelet mapping in a patient with von Willebrand disease who was treated with Humate-P. J. Clin. Anesth. 2011;23:600. doi: 10.1016/j.jclinane.2010.12.019. [DOI] [PubMed] [Google Scholar]
- 107.Topf H.-G., Strasser E.R., Breuer G., Rascher W., Rauh M., Fahlbusch F.B. Closing the gap–detection of clinically relevant von Willebrand disease in emergency settings through an improved algorithm based on rotational Thromboelastometry. BMC Anesthesiol. 2019;19:10. doi: 10.1186/s12871-018-0672-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ramiz S., Hartmann J., Young G., Escobar M.A., Chitlur M. Clinical utility of viscoelastic testing (TEG and ROTEM analyzers) in the management of old and new therapies for hemophilia. Am. J. Hematol. 2019;94:249–256. doi: 10.1002/ajh.25319. [DOI] [PubMed] [Google Scholar]
- 109.Artang R., Anderson M., Nielsen J.D. Fully automated thromboelastograph TEG 6s to measure anticoagulant effects of direct oral anticoagulants in healthy male volunteers. Res. Pract. Thromb. Haemost. 2019;3:391–396. doi: 10.1002/rth2.12206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Gosselin R.C., Adcock D.M., Douxfils J. An update on laboratory assessment for direct oral anticoagulants (DOACs) Int. J. Lab. Hematol. 2019;41:33–39. doi: 10.1111/ijlh.12992. [DOI] [PubMed] [Google Scholar]
- 111.Sokol J., Nehaj F., Ivankova J., Mokan M., Zolkova J., Lisa L., Linekova L., Mokan M., Stasko J. Impact of Dabigatran Treatment on Rotation Thromboelastometry. Clin. Appl. Thromb. Hemost. 2021;27 doi: 10.1177/1076029620983902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Seyve L., Richarme C., Polack B., Marlu R. Impact of four direct oral anticoagulants on rotational thromboelastometry (ROTEM) Int. J. Lab. Hematol. 2018;40:84–93. doi: 10.1111/ijlh.12744. [DOI] [PubMed] [Google Scholar]
- 113.Moore E.E., Moore H.B., Chapman M.P., Gonzalez E., Sauaia A. Goal-Directed hemostatic resuscitation for trauma induced coagulopathy: Maintaining homeostasis. J. Trauma Acute Care Surg. 2018;84:S35–S40. doi: 10.1097/TA.0000000000001797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Colman E., Yin E.B., Laine G., Chatterjee S., Saatee S., Herlihy J.P., Reyes M.A., Bracey A.W. Evaluation of a heparin monitoring protocol for extracorporeal membrane oxygenation and review of the literature. J. Thorac. Dis. 2019;11:3325–3335. doi: 10.21037/jtd.2019.08.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Christie S.A., Kornblith L.Z., Howard B.M., Conroy A.S., Kunitake R.C., Nelson M.F., Hendrickson C.M., Calfee C.S., Callcut R.A., Cohen M.J. Characterization of distinct coagulopathic phenotypes in injury: Pathway-specific drivers and implications for individualized treatment. J. Trauma Acute Care Surg. 2017;82:1055. doi: 10.1097/TA.0000000000001423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Gonzalez E., Moore E.E., Moore H.B., Chapman M.P., Chin T.L., Ghasabyan A., Wohlauer M.V., Barnett C.C., Bensard D.D., Biffl W.L., et al. Goal-directed Hemostatic Resuscitation of Trauma-induced Coagulopathy: A Pragmatic Randomized Clinical Trial Comparing a Viscoelastic Assay to Conventional Coagulation Assays. Ann. Surg. 2016;263:1051–1059. doi: 10.1097/SLA.0000000000001608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Theusinger O., Felix C., Spahn D. Strategies to reduce the use of blood products: A European perspective. Curr. Opin. Anaesthesiol. 2012;25:59–65. doi: 10.1097/ACO.0b013e32834dec98. [DOI] [PubMed] [Google Scholar]
- 118.Theusinger O.M., Madjdpour C., Spahn D.R. Resuscitation and transfusion management in trauma patients: Emerging concepts. Curr. Opin. Crit. Care. 2012;18:661–670. doi: 10.1097/MCC.0b013e328357b209. [DOI] [PubMed] [Google Scholar]
- 119.Hranjec T., Estreicher M., Rogers B., Kohler L., Solomon R., Hennessy S., Cibulas M., Hurst D., Hegazy M., Lee J. Integral Use of Thromboelastography with Platelet Mapping to Guide Appropriate Treatment, Avoid Complications, and Improve Survival of Patients with Coronavirus Disease 2019–Related Coagulopathy. Crit. Care Explor. 2020;2:e0287. doi: 10.1097/CCE.0000000000000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Chapman M.P., Moore E.E., Ramos C.R., Ghasabyan A., Harr J.N., Chin T.L., Stringham J.R., Sauaia A., Silliman C.C., Banerjee A. Fibrinolysis greater than 3% is the critical value for initiation of antifibrinolytic therapy. J. Trauma Acute Care Surg. 2013;75:961. doi: 10.1097/TA.0b013e3182aa9c9f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Napolitano L., Cohen M., Cotton B., Schreiber M., Moore E. Tranexamic acid in trauma: How should we use it? J. Trauma Acute Care Surg. 2013;74:1575–1586. doi: 10.1097/TA.0b013e318292cc54. [DOI] [PubMed] [Google Scholar]
- 122.Theusinger O., Wanner G., Emmert M., Billeter A., Eismon J., Seifert B., Simmen H.-P., Spahn D., Baulig W. Hyperfibrinolysis diagnosed by rotational thromboelastometry (ROTEM) is associated with higher mortality in patients with severe trauma. Anesth. Analg. 2011;113:1003–1012. doi: 10.1213/ANE.0b013e31822e183f. [DOI] [PubMed] [Google Scholar]
- 123.Kashuk J.L., Moore E.E., Sabel A., Barnett C., Haenel J., Le T., Pezold M., Lawrence J., Biffl W.L., Cothren C.C., et al. Rapid thrombelastography (r-TEG) identifies hypercoagulability and predicts thromboembolic events in surgical patients. Surgery. 2009;146:764–772; discussion 772–774. doi: 10.1016/j.surg.2009.06.054. [DOI] [PubMed] [Google Scholar]
- 124.Nunns G.R., Moore H.B., Moore E.E. Goal-Directed Massive Transfusion Management. In: Moore H.B., Moore E.E., Neal M.D., editors. Trauma Induced Coagulopathy. 2nd ed. Spring Nature Switzerland AG; Cham, Switzerland: 2021. pp. 487–494. [Google Scholar]
- 125.Solomon C., Traintinger S., Ziegler B., Hanke A., Rahe-Meyer N., Voelckel W., Schochl H. Platelet function following trauma. A multiple electrode aggregometry study. Thromb. Haemost. 2011;106:322–330. doi: 10.1160/TH11-03-0175. [DOI] [PubMed] [Google Scholar]
- 126.Kornblith L.Z., Moore H.B., Cohen M.J. Trauma-induced coagulopathy: The past, present, and future. J. Thromb. Haemost. 2019;17:852–862. doi: 10.1111/jth.14450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Wohlauer M.V., Moore E.E., Thomas S., Sauaia A., Evans E., Harr J., Silliman C.C., Ploplis V., Castellino F.J., Walsh M. Early platelet dysfunction: An unrecognized role in the acute coagulopathy of trauma. J. Am. Coll. Surg. 2012;214:739–746. doi: 10.1016/j.jamcollsurg.2012.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Walsh M., Shreve J., Thomas S. The value of cold storage whole blood platelets in trauma resuscitation is like real estate: A function of ‘location, location, location’. Br. J. Haematol. 2017;179:699–702. doi: 10.1111/bjh.14998. [DOI] [PubMed] [Google Scholar]
- 129.Holcomb J.B., Wade C.E., Michalek J.E., Chisholm G.B., Zarzabal L.A., Schreiber M.A., Gonzalez E.A., Pomper G.J., Perkins J.G., Spinella P.C., et al. Increased plasma and platelet to red blood cell ratios improves outcome in 466 massively transfused civilian trauma patients. Ann. Surg. 2008;248:447–458. doi: 10.1097/SLA.0b013e318185a9ad. [DOI] [PubMed] [Google Scholar]
- 130.Paniccia R., Priora R., Liotta A.A., Abbate R. Platelet function tests: A comparative review. Vasc. Health Risk Manag. 2015;11:133–148. doi: 10.2147/VHRM.S44469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Moore H.B., Moore E.E., Gonzalez E. Mortality and ratio of blood products used in patients with severe trauma. JAMA. 2015;313:2077. doi: 10.1001/jama.2015.4418. [DOI] [PubMed] [Google Scholar]
- 132.Holcomb J.B., Tilley B.C., Baraniuk S., Fox E.E., Wade C.E., Podbielski J.M., del Junco D.J., Brasel K.J., Bulger E.M., Callcut R.A., et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs. a 1:1:2 ratio and mortality in patients with severe trauma: The PROPPR randomized clinical trial. JAMA. 2015;313:471–482. doi: 10.1001/jama.2015.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Bunch C.M., Thomas A.V., Stillson J.E., Gillespie L., Lin K.P., Speybroeck J., Kwaan H.C., Fulkerson D.H., Zamlut M., Khan R., et al. Thromboelastography-Guided Anticoagulant Therapy for the Double Hazard of Thrombohemorrhagic Events in COVID-19: A Report of 3 Cases. Am. J. Case Rep. 2021;22:e931080. doi: 10.12659/AJCR.931080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Bareille M., Hardy M., Douxfils J., Roullet S., Lasne D., Levy J.H., Stépanian A., Susen S., Frère C., Lecompte T. Viscoelastometric Testing to Assess Hemostasis of COVID-19: A Systematic Review. J. Clin. Med. 2021;10:1740. doi: 10.3390/jcm10081740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Gergi M., Goodwin A., Freeman K., Colovos C., Volod O. Viscoelastic hemostasis assays in septic, critically ill coronavirus disease 2019 patients: A practical guide for clinicians. Blood Coagul. Fibrinolysis. 2021;32:225–228. doi: 10.1097/MBC.0000000000000999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Stillson J.E., Bunch C.M., Gillespie L., Khan R., Wierman M., Pulvirenti J., Phyu H., Anderson S., Al-Fadhl M., Thomas A.V., et al. Thromboelastography-Guided Management of Anticoagulated COVID-19 Patients to Prevent Hemorrhage. Semin. Thromb. Hemost. 2021;47:442–446. doi: 10.1055/s-0041-1723754. [DOI] [PubMed] [Google Scholar]
- 137.Matthay Z.A., Kornblith L.Z. Platelets. In: Moore H.B., Moore E.E., Neal M.D., editors. Trauma Induced Coagulopathy. 2nd ed. Spring Nature Switzerland AG; Cham, Switzerland: 2021. pp. 85–100. [Google Scholar]
- 138.Dias J.D., Pottgiesser T., Hartmann J., Duerschmied D., Bode C., Achneck H.E. Comparison of three common whole blood platelet function tests for in vitro P2Y12 induced platelet inhibition. J. Thromb. Thromb. 2020;50:135–143. doi: 10.1007/s11239-019-01971-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Schimmer C., Hamouda K., Sommer S.P., Özkur M., Hain J., Leyh R. The predictive value of multiple electrode platelet aggregometry (multiplate) in adult cardiac surgery. Thorac. Cardiovasc. Surg. 2013;61:733–743. doi: 10.1055/s-0033-1333659. [DOI] [PubMed] [Google Scholar]
- 140.Kander T., Larsson A., Taune V., Schött U., Tynngård N. Assessment of haemostasis in disseminated intravascular coagulation by use of point-of-care assays and routine coagulation tests, in critically ill patients; a prospective observational study. PLoS ONE. 2016;11:e0151202. doi: 10.1371/journal.pone.0151202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Katz D., Beilin Y. Disorders of coagulation in pregnancy. Br. J. Anaesth. 2015;115((Suppl. 2)):ii75–ii88. doi: 10.1093/bja/aev374. [DOI] [PubMed] [Google Scholar]
- 142.Prinz V., Finger T., Bayerl S., Rosenthal C., Wolf S., Liman T., Vajkoczy P. High prevalence of pharmacologically induced platelet dysfunction in the acute setting of brain injury. Acta Neurochir. 2016;158:117–123. doi: 10.1007/s00701-015-2645-8. [DOI] [PubMed] [Google Scholar]
- 143.Da Luz L.T., Nascimento B., Shankarakutty A.K., Rizoli S., Adhikari N.K. Effect of thromboelastography (TEG(R)) and rotational thromboelastometry (ROTEM(R)) on diagnosis of coagulopathy, transfusion guidance and mortality in trauma: Descriptive systematic review. Crit. Care. 2014;18:518. doi: 10.1186/s13054-014-0518-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Lam H., Katyal N., Parker C., Natteru P., Nattanamai P., Newey C.R., Kraus C.K. Thromboelastography with platelet mapping is not an effective measure of platelet inhibition in patients with spontaneous intracerebral hemorrhage on antiplatelet therapy. Cureus. 2018;10:e2515. doi: 10.7759/cureus.2515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Connelly C.R., Yonge J.D., McCully S.P., Hart K.D., Hilliard T.C., Lape D.E., Watson J.J., Rick B., Houser B., Deloughery T.G. Assessment of three point-of-care platelet function assays in adult trauma patients. J. Surg. Res. 2017;212:260–269. doi: 10.1016/j.jss.2017.01.008. [DOI] [PubMed] [Google Scholar]
- 146.Ranucci M., Baryshnikova E. Sensitivity of viscoelastic tests to platelet function. J. Clin. Med. 2020;9:189. doi: 10.3390/jcm9010189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Simurda T., Casini A., Stasko J., Hudecek J., Skornova I., Vilar R., Neerman-Arbez M., Kubisz P. Perioperative management of a severe congenital hypofibrinogenemia with thrombotic phenotype. Thromb. Res. 2020;188:1–4. doi: 10.1016/j.thromres.2020.01.024. [DOI] [PubMed] [Google Scholar]
- 148.Volod O., Arabia F.A., Lam L.D., Runge A., Cheng C., Czer L.S. Platelet Mapping by Thromboelastography and Whole Blood Aggregometry in Adult Patients Supported by Mechanical Circulatory Support Device on Aspirin Therapy. J. Extra Corpor. Technol. 2020;52:13. doi: 10.1182/ject-1900029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Görlinger K., Dirkmann D., Gandhi A., Simioni P. COVID-19 associated coagulopathy and inflammatory response: What do we know already and what are the knowledge gaps? Anesth. Analg. 2020;131:1324–1333. doi: 10.1213/ANE.0000000000005147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Hartmann J., Ergang A., Mason D., Dias J.D. The Role of TEG Analysis in Patients with COVID-19-Associated Coagulopathy: A Systematic Review. Diagnostics. 2021;11:172. doi: 10.3390/diagnostics11020172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Walsh M.M., Khan R., Kwaan H.C., Neal M.D. Fibrinolysis Shutdown in COVID-19-Associated Coagulopathy: A Crosstalk among Immunity, Coagulation, and Specialists in Medicine and Surgery. J. Am. Coll. Surg. 2021;232:1003–1006. doi: 10.1016/j.jamcollsurg.2021.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Jayarangaiah A., Kariyanna P.T., Chen X., Jayarangaiah A., Kumar A. COVID-19-associated coagulopathy: An exacerbated immunothrombosis response. Clin. Appl. Thromb. Hemost. 2020;26 doi: 10.1177/1076029620943293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Baron D., Franchini M., Goobie S., Javidroozi M., Klein A., Lasocki S., Liumbruno G., Muñoz M., Shander A., Spahn D. Patient blood management during the COVID–19 pandemic: A narrative review. Anaesthesia. 2020;75:1105–1113. doi: 10.1111/anae.15095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Coagulation Systems for Measurement of Viscoelastic Properties: Enforcement Policy during the Coronavirus Disease 2019 (COVID-19) Public Health Emergency (Revised) USA Food & Drug Administration; Rockville, MD, USA: 2021. [Google Scholar]
- 155.Klok F.A., Kruip M., van der Meer N.J.M., Arbous M.S., Gommers D., Kant K.M., Kaptein F.H.J., van Paassen J., Stals M.A.M., Huisman M.V., et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb. Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Panigada M., Bottino N., Tagliabue P., Grasselli G., Novembrino C., Chantarangkul V., Pesenti A., Peyvandi F., Tripodi A. Hypercoagulability of COVID-19 patients in intensive care unit: A report of thromboelastography findings and other parameters of hemostasis. J. Thromb. Haemost. 2020;18:1738–1742. doi: 10.1111/jth.14850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.NIH ACTIV Initiative Launches Adaptive Clinical Trials of Blood-Clotting Treatments for COVID-19. [(accessed on 21 February 2021)]; Available online: https://www.nih.gov/news-events/news-releases/nih-activ-initiative-launches-adaptive-clinical-trials-blood-clotting-treatments-covid-19.
- 158.Bachler M., Bösch J., Stürzel D.P., Hell T., Giebl A., Ströhle M., Klein S.J., Schäfer V., Lehner G.F., Joannidis M. Impaired fibrinolysis in critically ill COVID-19 patients. Br. J. Anaesth. 2021;126:590–598. doi: 10.1016/j.bja.2020.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Bunch C.M., Thomas A.V., Stillson J.E., Gillespie L., Khan R.Z., Zackariya N., Shariff F., Al-Fadhl M., Mjaess N., Miller P.D., et al. Preventing Thrombohemorrhagic Complications of Heparinized COVID-19 Patients Using Adjunctive Thromboelastography: A Retrospective Study. J. Clin. Med. 2021;10:3097. doi: 10.3390/jcm10143097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Iba T., Levy J.H., Levi M., Connors J.M., Thachil J. Coagulopathy of coronavirus disease 2019. Crit. Care Med. 2020;48:1358–1364. doi: 10.1097/CCM.0000000000004458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Cannegieter S.C., Klok F.A. COVID-19 associated coagulopathy and thromboembolic disease: Commentary on an interim expert guidance. Res. Pract. Thromb. Haemost. 2020;4:439–445. doi: 10.1002/rth2.12350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Fraissé M., Logre E., Pajot O., Mentec H., Plantefève G., Contou D. Thrombotic and hemorrhagic events in critically ill COVID-19 patients: A French monocenter retrospective study. Crit. Care. 2020;24:275. doi: 10.1186/s13054-020-03025-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Full-Dose Blood Thinners Decreased Need for Life Support and Improved Outcome in Hospitalized COVID-19 Patients. [(accessed on 26 January 2021)]; Available online: https://www.nih.gov/news-events/news-releases/full-dose-blood-thinners-decreased-need-life-support-improved-outcome-hospitalized-covid-19-patients.
- 164.Lawler P.R., Goligher E.C., Berger J.S., Neal M.D., McVerry B.J., Nicolau J.C., Gong M.N., Carrier M., Rosenson R.S., Reynolds H.R., et al. Therapeutic Anticoagulation with Heparin in Noncritically Ill Patients with Covid-19. N. Eng. J. Med. 2021;385:790–802. doi: 10.1056/NEJMoa2105911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Tsantes A.E., Tsantes A.G., Kokoris S.I., Bonovas S., Frantzeskaki F., Tsangaris I., Kopterides P. COVID-19 Infection-Related Coagulopathy and Viscoelastic Methods: A Paradigm for Their Clinical Utility in Critical Illness. Diagnostics. 2020;10:817. doi: 10.3390/diagnostics10100817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Słomka A., Kowalewski M., Żekanowska E. Hemostasis in Coronavirus Disease 2019—Lesson from Viscoelastic Methods: A Systematic Review. Thromb. Haemost. 2021;121:1181–1192. doi: 10.1055/a-1346-3178. [DOI] [PubMed] [Google Scholar]
- 167.Johansson P.I., Stissing T., Bochsen L., Ostrowski S.R. Thrombelastography and tromboelastometry in assessing coagulopathy in trauma. Scand. J. Trauma Resusc. Emerg. Med. 2009;17:45. doi: 10.1186/1757-7241-17-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Subramanian M., Kaplan L.J., Cannon J.W. Thromboelastography-Guided Resuscitation of the Trauma Patient. JAMA Surg. 2019;154:1152–1153. doi: 10.1001/jamasurg.2019.3136. [DOI] [PubMed] [Google Scholar]
- 169.Görlinger K., Fries D., Dirkmann D., Weber C.F., Hanke A.A., Schöchl H. Reduction of fresh frozen plasma requirements by perioperative point-of-care coagulation management with early calculated goal-directed therapy. Transfus. Med. Hemother. 2012;39:104–113. doi: 10.1159/000337186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Spahn D.R., Bouillon B., Cerny V., Duranteau J., Filipescu D., Hunt B.J., Komadina R., Maegele M., Nardi G., Riddez L., et al. The European guideline on management of major bleeding and coagulopathy following trauma: Fifth edition. Crit. Care. 2019;23:98. doi: 10.1186/s13054-019-2347-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Cohen T., Haas T., Cushing M.M. The strengths and weaknesses of viscoelastic testing compared to traditional coagulation testing. Transfusion. 2020;60:S21–S28. doi: 10.1111/trf.16073. [DOI] [PubMed] [Google Scholar]
- 172.Meizoso J.P., Moore H.B., Moore E.E. Fibrinolysis shutdown in COVID-19: Clinical manifestations, molecular mechanisms, and therapeutic implications. J. Am. Coll. Surg. 2021;232:995–1003. doi: 10.1016/j.jamcollsurg.2021.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Kwaan H.C., Lindholm P.F. The Central Role of Fibrinolytic Response in COVID-19-A Hematologist’s Perspective. Int. J. Mol. Sci. 2021;22:1283. doi: 10.3390/ijms22031283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Foley J.H., Conway E.M. Cross talk pathways between coagulation and inflammation. Circ. Res. 2016;118:1392–1408. doi: 10.1161/CIRCRESAHA.116.306853. [DOI] [PubMed] [Google Scholar]
- 175.Johansson P.I., Stensballe J., Ostrowski S.R. Shock induced endotheliopathy (SHINE) in acute critical illness—A unifying pathophysiologic mechanism. Crit. Care. 2017;21:25. doi: 10.1186/s13054-017-1605-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Dobson G.P., Letson H.L., Sharma R., Sheppard F.R., Cap A.P. Mechanisms of early trauma-induced coagulopathy: The clot thickens or not? J. Trauma Acute Care Surg. 2015;79:301–309. doi: 10.1097/TA.0000000000000729. [DOI] [PubMed] [Google Scholar]
- 177.Katz D., Maher P., Getrajdman C., Hamburger J., Zhao S., Madek J., Bhatt H., Levin M., Görlinger K. Monitoring of COVID-19-Associated Coagulopathy and Anticoagulation with Thromboelastometry. Transfus. Med. Hemother. 2021;48:168–172. doi: 10.1159/000514486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Creel-Bulos C., Sniecinski R. Fibrinolysis Shutdown and Thrombosis in a COVID-19 ICU. Shock. 2021;55:845–846. doi: 10.1097/SHK.0000000000001666. [DOI] [PubMed] [Google Scholar]
- 179.Sadeghipour P., Talasaz A.H., Rashidi F., Sharif-Kashani B., Beigmohammadi M.T., Farrokhpour M., Sezavar S.H., Payandemehr P., Dabbagh A., Moghadam K.G., et al. Effect of Intermediate-Dose vs Standard-Dose Prophylactic Anticoagulation on Thrombotic Events, Extracorporeal Membrane Oxygenation Treatment, or Mortality among Patients with COVID-19 Admitted to the Intensive Care Unit: The INSPIRATION Randomized Clinical Trial. JAMA. 2021;325:1620–1630. doi: 10.1001/jama.2021.4152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Chowdhury J.F., Moores L.K., Connors J.M. Anticoagulation in hospitalized patients with COVID-19. N. Engl. J. Med. 2020;383:1675–1678. doi: 10.1056/NEJMclde2028217. [DOI] [PubMed] [Google Scholar]
- 181.Al-Samkari H., Karp Leaf R.S., Dzik W.H., Carlson J.C., Fogerty A.E., Waheed A., Goodarzi K., Bendapudi P., Bornikova L., Gupta S. COVID and Coagulation: Bleeding and Thrombotic Manifestations of SARS-CoV2 Infection. Blood. 2020;136:489–500. doi: 10.1182/blood.2020006520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Musoke N., Lo K.B., Albano J., Peterson E., Bhargav R., Gul F., DeJoy R., 3rd, Salacup G., Pelayo J., Tipparaju P., et al. Anticoagulation and bleeding risk in patients with COVID-19. Thromb. Res. 2020;196:227–230. doi: 10.1016/j.thromres.2020.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Hammer S., Häberle H., Schlensak C., Bitzer M., Malek N.P., Handgretinger R., Lang P., Hörber S., Peter A., Martus P., et al. Severe SARS-CoV-2 Infection Inhibits Fibrinolysis Leading to Changes in Viscoelastic Properties of Blood Clot: A Descriptive Study of Fibrinolysis in COVID-19. Thromb. Haemost. 2021;121:1417–1426. doi: 10.1055/a-1400-6034. [DOI] [PubMed] [Google Scholar]
- 184.Nougier C., Benoit R., Simon M., Desmurs-Clavel H., Marcotte G., Argaud L., David J.S., Bonnet A., Negrier C., Dargaud Y. Hypofibrinolytic state and high thrombin generation may play a major role in SARS-COV2 associated thrombosis. J. Thromb. Haemost. 2020;18:2215–2219. doi: 10.1111/jth.15016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Hulshof A.M., Braeken D.C.W., Ghossein-Doha C., van Santen S., Sels J.E.M., Kuiper G., van der Horst I.C.C., Ten Cate H., van Bussel B.C.T., Olie R.H., et al. Hemostasis and fibrinolysis in COVID-19 survivors 6 months after intensive care unit discharge. Res. Pract. Thromb. Haemost. 2021;5:e12579. doi: 10.1002/rth2.12579. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.