Abstract
Mobile technologies are becoming ubiquitous in the world, changing the way we communicate and provide patient care and services. Some of the most compelling benefits of mobile technologies are in the areas of disease prevention, health management, and care delivery. For all the advances that are occurring in mobile health, its full potential for older adults is only starting to emerge. Yet, existing mobile health applications have design flaws that may limit usability by older adults. The aim of this paper is to review barriers and identify knowledge gaps where more research is needed to improve the accessibility of mobile health use in aging populations. The same observations might apply to those who are not elderly, including individuals suffering from severe mental or medical illnesses.
Keywords: Design considerations, mHealth, mobile health, mobile technology, older adults
The World Health Organization (WHO) defines mobile health (mHealth) as the delivery of medical practice by mobile devices, including smartphones, tablets, or wearable monitoring devices [1]. mHealth has many functions including: facilitating medication management through alerts and logs, providing self-care advice to patients, supporting self- and clinician-monitoring of biometrics (e.g., heart rate, blood pressure, activity), facilitating patient-provider communication, or educating patients on disease outcomes [2, 3]. With the ubiquity of mobile devices and internet access, the scope and availability of mHealth have markedly increased in recent years. There are estimated to be over 250,000 mHealth applications currently available to consumers [4]. While the availability of mHealth continues to increase, mHealth research is still in the relatively early stages [5]. Notably, these studies generally exclude adults 65 and older [6, 7]. Such a knowledge gap may greatly reduce the efficacy of mHealth applications for the elderly populations.
Since 2013, the percentage of U.S. older adults ages 65 and up who own a smartphone has risen from 18% to 42% [8]. Similarly, internet usage in older adult has increased rapidly over the last 5 years, with almost two-thirds of older adults reporting internet usage in 2016 [8]. While this group is more digitally connected than ever, older adults consistently have lower rates of technology adoption than the general public [8]. Numerous studies report that adults over the age of 65 use fewer new technologies and use them less frequently than younger adults [9]. Similarly, the actual usage and adoption of mHealth remains low and inconsistent in this population [10]. An early study found that some of the primary reasons that older adults do not use technology include limited access to internet, cost, and lack of knowledge [11]. Other researchers found that although older adults were eager to learn how to use technologies, they also perceived that they might have difficulty learning to use technologies and that they would need more time to learn them than would younger adults [12]. A lack of experience with technology might be an obstacle to the use of mHealth by older adults. Older adults did not grow up in the age of technology and were not required to learn to use the computer as part of their education. It was reported that older adults with no computer experience are more likely to report concern and fear of using technology [13]. Similarly, researchers found that age was negatively linked to technology knowledge and interest and positively linked to technology anxiety [14].
mHealth applications offer a number of benefits to older adults. They can enhance the lives of older adults by allowing them to live independently longer [15]. In addition, they can provide an opportunity to alleviate the cost and burden for older adults to engage in health care services [16]. Overall, mHealth applications align well with the increasing interest of older adults to integrate technologies into their own health care, particularly those who live in remote locations, far away from local health facilities, or in areas with shortages of medical professionals. However, such technological advances also pose a great challenge to the elderly populations [17]. Cognitive impairment is one of the most common health problems for adults aged 65 years or above [18]. It is estimated that the prevalence of cognitive impairment is higher than 40% among older adults aged 80 years and above [19, 20]. Cognitive impairment is also a common feature for individuals with significant mental problems, such as schizophrenia [21] and mood disorders [22]. However, the actual age patterns of mHealth use for different patient populations have not been well documented.
While much remains unknown regarding factors that affect older adults’ engagement in mHealth, usability studies show that existing mHealth applications do not meet the specific needs and expectations of older adults [23]. Similarly, an integrative review also commented that even though there are a wide range of telehealth technologies available to chronically ill patients, not all of those technologies may be appropriate for the elderly populations [24]. Overall, previous literature identified several key categories of barriers to mHealth use by older adults [25–27]: 1) cognitive and physical declines; 2) perceptual changes (vision and audition); as well as 3) reduced motivation. The purpose of this paper is to provide a summary report, based on the results of current literature, to identify research gaps and needs to establish efficacy of mHealth designs targeting older adults. The same observations might also apply to other populations, including those who are mentally or medically ill.
BARRIERS TO THE USE OF MHEALTH IN OLDER ADULTS
Cognitive and physical barriers
Many age-related cognitive changes, including reduced attention, processing speed, executive function, visuomotor skills, and memory, may all negatively influence mHealth use [28–31]. A recent case-study reported that cognitive barriers (e.g., declines in attention and thinking skills) were the second largest category of aging barriers negatively affecting usability of mHealth app [32]. In the study, users age 50 or above had difficulty returning to previously shown information in the app, determining where to find information, and understanding app’s functionalities. Within this context, another study showed that senior mobile phone users, even after more than one year of experience, still had trouble understanding basic operations and functions [33].
In addition, physical impairments can make holding a device in one’s hand uncomfortable [29, 34]. Common age-related illnesses that may negatively influence mHealth use include arthritis, slower movement and reflexes, stiffer muscles and joints, hand tremor, and poor balance [24, 28, 35]. More than 75% of the American population aged 65 or older have difficulty with physical functioning [36], presenting challenges in mHealth implementation for elderly populations [37].
Considerations for age-related cognitive and physical decline
Recent design guidelines for mobile interfaces acknowledge the relevance of cognitive function to interacting with mobile services and suggest that cognitive load should be minimized, such as by a clear navigational structure and supporting an interface that matches the needs of older adults [31, 33]. Three publications reported that a consistent interface is an important feature when designing technology for older adults [30, 38, 39]. For example, consistent use in language or terminology (e.g., use of the words “previous” or “back” to instruct an individual to move backwards on a screen) might reduce confusion among older adults who are not familiar with technology terms [38]. Similarly, inconsistencies in the processes for entering and saving information in the applications, such as interchangeable use of the terms “done” and “finish” may also increase user confusion, leading to unsuccessful attempts to enter data [30]. To minimize user confusion, some recommend that the colors, sizes, and language used for labeling buttons and icons be standardized [39]. However, additional works are needed to evaluate these features in older adults across cognitive spectrums and establish empirical guidelines to provide a consistent interface for diverse elderly populations.
Changes in executive functioning can cause difficulty with filtering irrelevant information and learning how to use technology [40]. Working memory may also become easily overloaded with age, interfering with technology use [41]. A recent review study reported that even though older adults are interested in using smartphones and tablets for obtaining health information [2], over 75% indicates that they would need help to walk them through the process of learning how to use the new device [42]. Similarly, other researchers noted that majority of elderly participants expressed interest in mHealth use if they were provided with adequate training [43]. A recent focus group study suggest that simple step-by-step tutorials may help maximize a sense of mastery in older adults [44]. However, further investigation is necessary before any definite conclusion can be drawn. Specifically, it remains unclear whether a step-by-step walkthrough will increase or decrease the cognitive burden for senior users. Additional works are required to determine to what degree of guidance fits the greater need of senior users experiencing cognitive decline. On the other hand, while self-paced designs seem to be an appropriate option for some senior users given their cognitive decline, investigation on this topic are largely understudied. Understanding timing of tutorials or implementation of self-paced design could help maximize efficiency and flexibility.
A qualitative analysis of a focus group study reported simplicity as one of the key considerations in designing technology-based tools for older adults [45]. Similarly, two publications mention that user-friendliness is a facilitating factor of mHealth use by older adults [43, 46]. As mentioned by the authors, older adults are more likely to keep using mHealth application if it is simple and works easily. For instance, data entry involving clicking through multiple options may reduce user motivation. To minimize cognitive demands of mHealth use, some suggested using fewer than three steps for entering data and providing an auto-save function for finalizing entries [39]. While simple instructions with fewer buttons and a minimalist design are preferable for seniors [44], additional research is needed to guide design decisions in the appropriate balance between features and simplicity of mHealth applications for older adults.
A home screen containing many icons requiring users to scroll to view all of the icons was described as a poor design for older adults [39]. To ensure all key functions are visible on the home screen without the need to scroll, some researchers recommend the number of key functions available on the home screen be limited to 12 or fewer for tablets and 6 or fewer for smartphones [39]. The researchers also suggest information and questions be split up into two separate pages to simplify intra-app navigation and eliminate scrolling. However, it is unclear if removal of scroll bars will increase acceptability of mHealth among older adults.
Prior researchers noting the importance of specific user interface designs for older adults report that use of large targets and characters should be considered [31]. In addition, the researchers emphasized the importance of using a proper visual display with objects, such as buttons, that older adults can differentiate from other visual display features. Subsequent investigators further support the notion that user interface design elements such as font size and buttons should be modified to aid the senior user population [32]. Specifically, interactive elements are recommended be large enough to allow for less precise motor control [47]. A guide for app developers recommends each interactive element have a focusable area or touch target size of at least 48 × 48 dp [35]. A recent article suggests developers using large round or square buttons/icons of at least 15 mm in diameter rather than narrow or rectangular buttons, to ensure they are usable by older adults with poor fine motor control [39]. The article also suggests more space between buttons/icons within an application to reduce errors with button selection [39]. Future research is needed to determine the effectiveness of these suggestions on improving mHealth utilization in older adults.
Perceptual barriers (vision and audition)
Globally, the majority of individuals with vision impairment are over the age of 50 years [48]. A visual impairment, such as macular degeneration, makes viewing a digital screen difficult [49]. Age-related visual changes include reduced ability to resolve detail, focus on close objects, discriminate between colors (i.e., violet, blues, and greens), detect contrast, as well as adapt to darker conditions and glare [25, 26, 28, 31, 34, 35]. A study assessing mHealth usability problems by older adults reported that senior users oversaw important icons or feedback messages and had trouble reading small-font texts in apps [32]. In the study, 90% of the participants wore a visual aid such as glasses during the testing of mHealth apps, but nonetheless experienced usability issues due to perception barriers. In addition, hearing abilities decline with age [50], which also impacts their overall satisfaction on mHealth use [51]. Older adults with moderate to severe hearing impairments showed lower internet use compared to those with no hearing impairments [50].
Considerations for aged-related perceptual changes
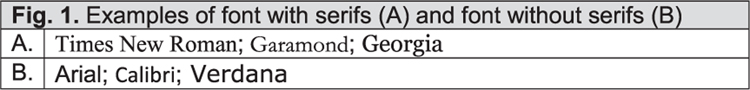
Previous research made a number of evidenced-based recommendations for how to design patient websites to make them easier for older adults to use, including organizing information in a way that matches with older adults’ expectations, simplifying website navigation with shallow menus and quick links, and using fonts and formats that are easy for older adults to read [52]. However, many of the recommendations apply more generally to making websites easier for elderly patients. A systematic review of 57 telehealth studies concluded that reading materials must be explicit and clear for older adults with reduced vision [37]. Given decreased visual acuity in older adults, researchers suggested that size of icons and texts on the mobile app be increased [43]. Some researchers recommend zoom features (e.g., a magnifier) be implemented to allow images and text to be resized [38]. The American Printing House for the Blind recommends use of a sans serif typeface (see Fig. 1). Serifs are small lines or stroke regularly attached to the end of a larger stroke in a letter or symbol within a particular font or family of fonts [53]. In addition, headings and subheadings are recommended to be larger and bolder than the regular text and left-only justification for a clear organizational pattern [53]. However, more studies are needed to evaluate if these recommendations remain relevant in mHealth applications targeting older adults.
Fig. 1.
Examples of font with serifs (A) and font without serifs (B) A. Times New Roman; Garamond; Georgia B. Arial; Calibri; Verdana.
According to the American Printing House for the Blind, black print on white, ivory, cream, or yellow with a dull finish is recommended to avoid glare [53]. Some recommend using high-contrast combinations of bold colors rather than pale or fluorescent colors to accommodate age-related declines in color vision [39]. The World Wide Web Consortium recommends using a text-to-background contrast ratio of at least 4.5:1 for small text and at least 3:1 for text larger than 18-point regular font [54]. Online tools, such as WebAIM Contrast Checker and MSF&W color contrast ratio calculator, provide easy methods for measuring text-to-background contrast ratio. The choice of color and contrast could be evaluated in future studies to verify older adults’ preferences for color and contrast in mHealth applications.
A recent study exploring facilitators of mHealth use in older adults reveals that senior users appreciate audio feedback [43]. Similarly, another study exploring older adults’ preference regarding technology-based applications found that participants favored the use of voice navigation because of their vision issues [55]. Previous research has shown the value of audio-based cues for older adults who use technologies [56]. A voice assistant, such as a screen reader, may facilitate older adults with vision impairment in completing tasks or navigate the device. An app developer guide by google recommends the use of “touch interface screen readers” to allow users run their finger over the screen to hear the on-screen text and elements (such as buttons) directly underneath [57]. Most guidelines for communicating with older adults emphasize amplifying and augmenting speech to compensate for hearing impairment [58]. “Clear speech” recommendations focus on speaking slowly and loudly, inserting pauses between phrases and sentences, stressing key words, enunciating each word precisely, and minimizing background noise [59]. While it is well known that the use of audio-based cues can improve acceptability of mHealth applications in older adults, further studies are required to determine more precisely when and how to use the technique most effectively.
Motivational barriers
One of the most frequently mentioned barriers to technology use in older adults is motivation [60–68]. According to the publications reviewed, a lack of motivation also contributes to adherence to mHealth use in elderly populations. At the same time, when facilitating factors were studied, many report that strong motivation with adequate support and feedback are important for the promotion and continuity of mHealth use in older adults [60–62].
Considerations to increase motivation in using mHealth applications
According to three publications, rewards are important as a mechanism to enhance mHealth use by older adults [46, 63, 69]. The rewards could be opportunities to enhance health care interactions, increased peer communication and support, greater access to medical information, and identification of meaningful information [69]. A survey study revealed that close to 95% of elderly participants expressed preferences for technologies designed to support healthy aging, including physical and cognitive health, self-manage existing conditions, and track changes in cognitive changes over time [70]. The survey also revealed that most participants reported interest in technologies designed to specifically assess mood-related concerns and changes. When asked about technology-based intervention, there was an overwhelming interest in technologies designed to improve individual risk factors for cognitive loss and dementia. In addition, utilization of performance-based reward is also recommended to boost users’ engagement (e.g., sending a quick congratulatory message after completing a task) [71]. Additional research is needed to determine which reward options and reward strategy may translate into increase mHealth use in older adults.
In a systematic literature review, researchers mentioned lack of time or other priorities as one of the factors influencing the low use rate of mHealth in older adults [46]. In the review, researchers suggest developing an app that can be paused and the use can be readily resumed when the older adult has time. However, the review adds that mHealth use is a challenge in senior users as older adults do not always have the proper skills to work with technology. A study on computer literacy in older adults reported that there was a negative relationship between computer self-efficacy and computer anxiety [72]. To keep senior users motivated, the Health Information Management and Systems Society guidelines for mHealth recommend that if a user make a mistake, the application may help to avoid it or provides a mechanism to recover from errors smoothly [73]. In line with the guideline, a recent study proposed using feedback messages in interfaces and suggest that these messages should not only inform users on their actions, but also provide the user options to recover from erroneous actions and return to previously retrieved information or action [32]. In addition, the study proposes using a clear video instruction on how to use an app to help older users register for an app, including help to return to the instruction during any point in an app’s usage. However, future studies are needed to evaluate how to best provide support and feedback for senior mHealth users.
According to a Bloomberg report, cybercriminals steal almost $40 billion from older adults in the United States every year [74]. A recent survey found that 67% of surveyed older adults have been the victim of an online scam or hack [75]. Many older adults are concerned with data privacy in their day-to-day usage of technology [44]. A recent focus-group study with adults aged 50 + found that the most common concerns raised about technologies centered around privacy [69]. For some participants in the study, concerns about security and privacy (e.g., who can access their data) appeared to outweigh potential benefits. While all participants expressed a desire to have increased access to their medical records, opinions varied as to who should be responsible for managing the medical information. Some researchers recommended using personalized privacy settings, where mHealth users can selectively share information with specific people or hide it from others [39]. Overall, more studies are necessary to identify how to educate users on protecting their information from being hacked and how to provide training to reduce older adult’s concerns about data privacy and security.
Co-design is defined as “the voluntary or involuntary involvement of public service users in any of the design, management, delivery and/or evaluation of public services” [76]. In a co-design process, designers and users work together to identify problems and explore possible solutions to address user-related issues [77]. Co-design is an evolving approach that is increasingly used by healthcare organization to improve the care and well-being of end-users [78]. A systematic review seem to suggest that co-designed technologies have a positive impact on health outcomes, such as increased ability to manage a disease, better access to healthcare, reductions in medical errors or incidents, improved patient satisfaction, increase disease knowledge, and reductions in medical costs [79]. While the review recognizes an increasing interest to involve older adults in the co-design of technology, the researchers also comments that the co-design processes varied greatly in their methodology and intensity of older adult involvement. What remains unknown is whether the beneficial effects of co-design technologies are greater than those reported for non-co-designed technologies. There is also a need to standardize the definition of co-design to facilitate comparison across studies and identification of effective approaches.
CONCLUSION
mHealth applications are an innovative approach for the delivery of healthcare and health information outside of a physician’s office. As older adults increasingly adopt mobile devices, there is a need to ensure that they can use mHealth applications effectively. In this paper, we reviewed a range of common barriers to mHealth adoption in older adults. We also identify research questions that might have an impact on improving mHealth use by older adults. While this paper focuses on design features that might improve the uptake of mHealth by older individuals, other facilitating factors such as improved health and economic status or improved familiarity in technology in the older population today were not discussed. However, this paper is not intended to give a complete and extensive overview of all the factors involved. Rather, the goal is to stimulate future investigation on this topic and support evidence-based designs for senior mHealth users. To date, there have been relatively few studies looking at barriers and resolution strategies to improve mHealth use by older adults. Our observations warrant future studies to provide evidence base for standard mHealth design guidelines.
Footnotes
DISCLOSURE STATEMENT
Authors’ disclosures available online (https://www.j-alz.com/manuscript-disclosures/20-0485r3).
REFERENCES
- [1].Searcy RP, Summapund J, Estrin D, Pollak JP, Schoenthaler A, Troxel AB, Dodson JA (2019) Mobile health technologies for older adults with cardiovascular disease: Current evidence and future directions. Curr Geriatr Rep 8, 31–42. [Google Scholar]
- [2].Kim BY, Lee J (2017) Smart devices for older adults managing chronic disease: A scoping review. JMIR Mhealth Uhealth 5, e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Joe J, Demiris G (2013) Older adults and mobile phones for health: A review. J Biomed Inform 46, 947–954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Bostrom J, Sweeney G, Whiteson J, Dodson JA (2020) Mobile health and cardiac rehabilitation in older adults. Clin Cardiol 43, 118–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Nilsen W, Kumar S, Shar A, Varoquiers C, Wiley T, Riley WT, Pavel M, Atienza A (2012) Advancing the science of mHealth. J Health Commun 17, 5–10. [DOI] [PubMed] [Google Scholar]
- [6].Hall AK, Cole-Lewis H, Bernhardt JM (2015) Mobile text messaging for health: A systematic review of reviews. Annu Rev Public Health 36, 393–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Head KJ, Noar SM, Iannarino NT, Grant Harrington N (2013) Efficacy of text messaging-based interventions for health promotion: A meta-analysis. Soc Sci Med 97, 41–48. [DOI] [PubMed] [Google Scholar]
- [8].Technology use among seniors, https://www.pewresearch.org/internet/2017/05/17/technology-use-among-seniors/, Last updated May 17, 2017, Accessed on April 2, 2020.
- [9].Vesel L, Hipgrave D, Dowden J, Kariuki W (2015) Application of mHealth to improve service delivery and health outcomes: Opportunities and challenges. Etude Popul Afr 29, 1683–1698. [Google Scholar]
- [10].Bender MS, Choi J, Arai S, Paul SM, Gonzalez P, Fukuoka Y (2014) Digital technology ownership, usage, and factors predicting downloading health apps among Caucasian, Filipino, Korean, and Latino Americans: The digital link to health survey. JMIR Mhealth Uhealth 2, e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Morrell RW, Mayhorn CB, Bennett J (2000) A survey of World Wide Web use in middle-aged and older adults. Hum Factors 42, 175–182. [DOI] [PubMed] [Google Scholar]
- [12].Rogers WA, Meyer B, Walker N, Fisk AD (1998) Functional limitations to daily living tasks in the aged: A focus group analysis. Hum Factors 40, 111–125. [DOI] [PubMed] [Google Scholar]
- [13].Vaportzis E, Clausen MG, Gow AJ (2017) Older adults perceptions of technology and barriers to interacting with tablet computers: A focus group study. Front Psychol 4, 1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Ellis D, Allaire JC (1999) Modeling computer interest in older adults: The role of age, education, computer knowledge, and computer anxiety. Hum Factors 41, 345–355. [DOI] [PubMed] [Google Scholar]
- [15].Bauer AM RT, Keppel GA, Cole AM, Baldwin LM, Katon W (2014) Use of mobile health (mHealth) tools by primary care patients in the WWAMI region Practice and Research Network (WPRN). J Am Board Fam Med 27, 780–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Bardram JE (2008) Pervasive healthcare as a scientific discipline. Methods Inf Med 47, 178–185. [DOI] [PubMed] [Google Scholar]
- [17].Harvey PDSKR (2012) Technology, society, and mental illness: Challenges and opportunities for assessment and treatment. Innov Clin Neurosci 9, 47–50. [PMC free article] [PubMed] [Google Scholar]
- [18].Ren L, Zheng Y, Wu L, Gu Y, He Y, Jiang B, Zhang J, Zhang L, Li J (2018) Investigation of the prevalence of cognitive impairment and its risk factors within the elderly population in Shanghai. Sci Rep 8, 3575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Yaffe K, Middleton LE, Lui LY, Spira AP, Stone K, Racine C, Ensrud KE, Kramer JH (2011) Mild cognitive impairment, dementia, and their subtypes in oldest old women. Arch Neurol 68, 631–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Hebert LE, Scherr PA, Beckett LA, Albert MS, Pilgrim DM, Chown MJ, Funkenstein HH, Evans DA (1995) Age-specific incidence of Alzheimer’s disease in a community population. JAMA 273, 1354–1359. [PubMed] [Google Scholar]
- [21].Ben-Zeev D SE, Gottlieb JD, Rotondi AJ, Brunette MF, Achtyes ED, Mueser KT, Gingerich S, Brenner CJ, Begale M, Mohr DC, Schooler N, Marcy P, Robinson DG, Kane JM (2016) mHealth for schizophrenia: Patient engagement with a mobile phone intervention following hospital discharge. JMIR Ment Health 3, e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Switsers L DA, Vanhoudt A, Van Dyck H, Lombaerts K, Oldenburg J (2018) Users’ perspectives on mhealth self-management of bipolar disorder: Qualitative focus group study. JMIR Mhealth Uhealth 6, e108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Wildenbos GA, Peute L, Jaspers M (2018) Aging barriers influencing mobile health usability for older adults: A literature-based framework (MOLD-US). Int J Med Inform 114, 66–75. [DOI] [PubMed] [Google Scholar]
- [24].Foster MV, Sethares KA (2014) Facilitators and barriers to the adoption of telehealth in older adults: An integrative review. Comput Inform Nurs 32, 523–533. [DOI] [PubMed] [Google Scholar]
- [25].Holzinger A, Searle G, Nischelwitzer A (2007) On Some Aspects of Improving Mobile Applications for Elderly: Universal Access in Human Computer Interaction Coping with Diversity, Springer, Berlin Heidelberg, pp. 923–932. [Google Scholar]
- [26].Rogers WA, Fisk AD (2010) Toward a psychological science of advanced technology design for older adults. J Gerontol B Psychol Sci Soc Sci 65, 645–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Czaja SJ, Sharit J, Lee CC, Nair SN, Hernandez MA, Arana N, Fu SH (2013) Factors influencing use of an e-health website in a community sample of older adults. J Am Med Inform Assoc 20, 277–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Farage MA, Miller KW, Ajayi F, Hutchins D (2012) Design principles to accommodate older adults. Glob J Health Sci 4, 2–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Bolle S, Romijn G, Smets EM, Loos EF, Kunneman M, van Weert JC (2016) Older cancer patients’ user experiences with web-based health information tools: A think-aloud study. J Med Internet Res 18, e208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Grindrod KA, Li M, Gates A (2014) Evaluating user perceptions of mobile medication management applications with older adults: A usability study. JMIR Mhealth Uhealth 2, e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Or C, Tao D (2012) Usability study of a computer-based self-management system for older adults with chronic diseases. JMIR Res Protoc 1, e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Wildenbos GA, Jaspers MWM, Schijven MP, Dusseljee-Peute LW (2019) Mobile health for older adult patients: Using an aging barriers framework to classify usability problems. Int J Med Inform 124, 68–77. [DOI] [PubMed] [Google Scholar]
- [33].Kascak L, Harrington CN, Sanford J (2017) Universal design mobile interface guidelines for mobile health and wellness apps for an aging population including people aging with disabilities. Int J Adv Softw 10, 372–384. [Google Scholar]
- [34].Harte RP, Glynn LG, Broderick BJ, Rodriguez-Molinero A, Baker PMA, McGuiness B, O’Sullivan L, Diaz M, Quinlan LR, OLaighin G (2014) Human centred design considerations for connected health devices for the older adult. J Pers Med 4, 245–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Fischer SH, David D, Crotty BH, Dierks M, Safran C (2014) Acceptance and use of health information technology by community-dwelling elders. Int J Med Inform 83, 624–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].U.S. Department of Health and Human Services (2014) National Center for Health Statistics Summary Health Statistics: National Health Interview Survey. https://www.cdc.gov/nchs/nhis/shs.htm, Last updated October 9, 2020, Accessed on October 10, 2020.
- [37].Kruse C, Fohn J, Wilson N, Nunez Patlan E, Zipp S, Mileski M (2020) Utilization barriers and medical outcomes commensurate with the use of telehealth among older adults: Systematic review. JMIR Med Inform 8, e20359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Reeder B, Zaslavksy O, Wilamowska KM, Demiris G, Thompson HJ (2011) Modeling the oldest old: Personas to design technology-based solutions for older adults. AMIA Annual Symposium proceedings AMIA Symposium, pp. 1166–1175. [PMC free article] [PubMed] [Google Scholar]
- [39].Morey SA, Stuck RE, Chong AW, Barg-Walkow LH, Mitzner TL, Rogers WA (2019) Mobile health apps: Improving usability for older adult users. Ergon Des 27, 4–13. [Google Scholar]
- [40].Czaja SJ, Charness N, Fisk AD, Hertzog C, Nair SN, Rogers WA, Sharit J (2006) Factors predicting the use of technology: Findings from the Center for Research and Education on Aging and Technology Enhancement (CREATE). Psychol Aging 21, 333–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Kowtko M (2012) Using assistive technologies to improve lives of older adults and people with disabilities. https://s3-us-west-2.amazonaws.com/ieeeshutpages/xplore/xplore-shut-page.html, Accessed September 12, 2020.
- [42].Smith A (2014) Older Adults and Technology Use. https://www.pewresearch.org/internet/2014/04/03/older-adults-and-technology-use/, Last updated April 3, 2014, Accessed September 25, 2020.
- [43].Cajita MI, Hodgson NA, Lam KW, Yoo S, Han HR (2018) Facilitators of and barriers to mHealth adoption in older adults with heart failure. Comput Inform Nurs 36, 376–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Wang S, Bolling K, Mao W, Reichstadt J, Jeste D, Kim HC, Nebeker C (2019) Technology to support aging in place: Older adults’ perspectives. Healthcare (Basel) 7, 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Joe J, Hall A, Chi NC, Thompson H, Demiris G (2018) IT-based wellness tools for older adults: Design concepts and feedback. Inform Health Soc Care 43, 142–158. [DOI] [PubMed] [Google Scholar]
- [46].Kampmeijer R, Pavlova M, Tambor M, Golinowska S, Groot W (2016) The use of e-health and m-health tools in health promotion and primary prevention among older adults: A systematic literature review. BMC Health Serv Res 16, 290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].González L, Mashat M, López S (2013) Creating and updating models of activities for people with Alzheimer disease using JClic platform. https://s3-us-west-2.amazonaws.com/ieeeshutpages/xplore/xplore-shut-page.html, Accessed September 22, 2020.
- [48].World Health Organization (2019) Blindness and vision impairment. https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment2019, Last updated October 8, 2020, Accessed October 1, 2020.
- [49].Lober WB, Zieler B, Herbaugh A, Shinstrom SE, Syolyar A, Kim EH, Kim Y (2006) Barriers to the use of a personal health record by an elderly population. AMIA 2006 Symposium Proceedings, pp. 515–518. [PMC free article] [PubMed] [Google Scholar]
- [50].Henshaw H, Clark DP, Kang S, Ferguson MA (2012) Computer skills and internet use in adults aged 50–74 years: Influence of hearing difficulties. J Med Internet Res 14, e113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Dham P, Gupta N, Alexander J, Black W, Rajji T, Skinner E (2018) Community based telepsychiatry service for older adults residing in a rural and remote region- utilization pattern and satisfaction among stakeholders. BMC Psychiatry 18, 316–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Morrow DCJ (2012) Technology as a bridge between health care systems and older adults. In Engaging Older Adults with Modern Technology: Internet Use and Information Access Needs, Zheng R, Hill R, Gardner M, ed. Information Science Reference, Hershey, PA. [Google Scholar]
- [53].American Printing House for the Blind Large print (2020) Guidelines for optimal readability and APHont™ a font for low vision. https://sun1.aph.org/edresearch/lpguide.htm, Last updated September 11, 2019, Accessed March 18, 2020.
- [54].World Wide Web Consortium. (2016) Contrast (minimum): Understanding success criterion 1.4.3. https://www.w3.org/TR/UNDERSTANDING-WCAG20/visual-audio-contrast-contrast.html, Accessed March 12, 2020.
- [55].Greenhalgh T, Wherton J, Shaw S, Morrison C (2020) Video consultations for covid-19. Br Med J 368, m998. [DOI] [PubMed] [Google Scholar]
- [56].Zajicek M (2004) Successful and available: Interface design exemplars for older users. Interact Comput 16, 411–30. [Google Scholar]
- [57].Google (2012) Accessibility. https://material.io/design/usability/accessibility.html#hierarchy, Accessed October 1, 2020.
- [58].Kemper S, Lacal, Jose C (2004) Technology for Adaptive Aging. In National Research Council (US) Steering Committee for the Workshop on Technology for Adaptive Aging, Pew RW, Van Hemel SB, eds. National Academies Press (US), Washington, DC. [PubMed] [Google Scholar]
- [59].Bollinger R, Hardiman CJ. Dementia (1989) The confused-disordered communicatively disturbed elderly. In Communication Disorders in Adults, Hull RH, Griffin KM, ed. Sage, CA, pp. 61–78. [Google Scholar]
- [60].Eysenbach G (2001) What is e-health? J Med Internet Res 3, e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Lindeman D (2011) mHealth technologies: Applications to benefit older adults. https://www.techandaging.org/mHealth_Position_Paper_Discussion_Draft.pdf, Last updated March 2011, Accessed October 12, 2015.
- [62].Angevaren M, Aufdemkampe G, Verhaar H, Aleman A, Vanhees L (2008) Physical activity and enhanced fitness to improve cognitive function in older people without known cognitive impairment. Cochrane Database Syst Rev 3, CD005381. [DOI] [PubMed] [Google Scholar]
- [63].Andrews GR (2001) Promoting health and function in an ageing population. Br Med J 322, 728–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A (2007) Physical activity and public health: Updated recommendation for adults from the American college of sports medicine and the American heart association. Circulation 116, 1423–34 [DOI] [PubMed] [Google Scholar]
- [65].Locke EA, Latham GP (2002) Building a practically useful theory of goal setting and task motivation: A 35-year odyssey. Am Psychol 57, 705–717 [DOI] [PubMed] [Google Scholar]
- [66].Bashshur RL, Shannon GW, Krupinski EA, Grigsby J, Kwedar JC, Weinstein RS, Sanders JH, Rheuban KS, Nesbitt TS, Alverson DC, Merrell RC, Linkous JD, Ferguson AS, Waters RJ, Stachura M, Ellis DG, Antoniotti NM, Johnston B, Doarn CR, Yellowlees P, Normandin S, Tracy J (2009) National telemedicine initiatives: Essential to healthcare reform. Telemed J E Health 15, 600–10 [DOI] [PubMed] [Google Scholar]
- [67].Ryan RM, Frederick CM, Lepes D, Rubio N, Sheldon KM (1997) Intrinsic motivation and exercise adherence. Int J Sport Psychol 28, 335–354 [Google Scholar]
- [68].Clar C, Dyakova M, Curtis K, Dawson C, Donnelly P, Knifton L, Clarke A (2014) Just telling and selling: Current limitations in the use of digital media in public health. A scoping review. Public Health 128, 1066–75. [DOI] [PubMed] [Google Scholar]
- [69].Andrews JA, Brown LJ, Hawley MS, Astell AJ (2019) Older adults’ perspectives on using digital technology to maintain good mental health: Interactive group study. J Med Internet Res 21, e11694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].LaMonica HM, English A, Hickie IB, Ip J, Ireland C, West S, Shaw T, Mowszowski L, Glozier N, Duffy S, Gibson A, Naismith SL (2017) Examining internet and eHealth practices and preferences: Survey study of Australian older adults with subjective memory complaints, mild cognitive impairment, or dementia. J Med Internet Res 19, e358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Yerrakalva DYD, Hajna S, Griffin S (2019) Effects of mobile health app interventions on sedentary time, physical activity, and fitness in older adults: Systematic review and meta-analysis. J Med Internet Res 21, e14343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Moore AN, Rothpletz AM, Preminger JE (2015) The effect of chronological age on the acceptance of internet-based hearing health care. Am J Audiol 24, 280–283. [DOI] [PubMed] [Google Scholar]
- [73].HIHSS HER Usability Task Force (2009) Defining and Testing EMR Usability: Principles and Proposed Methods of EMR Usability Evaluation and Rating. https://digital.ahrq.gov/health-it-tools-and-resources/health-it-bibliography/usability/defining-and-testing-emr-usability, Accessed on October 3, 2020.
- [74].Leiber N (2018) How criminals steal $37 billion a year from America’s elderly. https://www.bloomberg.com/news/features/2018-05-03/america-s-elderly-are-losing-37-billion-a-year-to-fraud, Last updated May 3, 2018, Accessed on June 28, 2020.
- [75].Home Instead Senior Care, Two-Thirds of Seniors Have Been Scammed Online: Survey, https://www.homeinstead.com/news/two-thirds-of-seniors-have-been-scammed-online-survey2016, Accessed on June 27, 2020.
- [76].Clarke D, Jones F, Harris R, Robert G; Collaborative Rehabilitation Environments in Acute Stroke (CREATE) team (2017) What outcomes are associated with developing and implementing co-produced interventions in acute healthcare settings? A rapid evidence synthesis. Br Med J Open 7, e014650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Fischer B, Peine A, Östlund B (2019) The importance of user involvement: A systematic review of involving older users in technology design. Gerontologist 60, e513–e523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Rathnayake S, Moyle W, Jones C, Calleja P (2020) Co-design of an mHealth application for family caregivers of people with dementia to address functional disability care needs. Inform Health Social Care, doi: 10.1080/17538157.2020.1793347 [DOI] [PubMed] [Google Scholar]
- [79].Sumner J, Chong LS, Bundele A, Lim YW (2020) Co-designing technology for ageing in place: A systematic review. Gerontologist, doi: 10.1093/geront/gnaa064. [DOI] [PMC free article] [PubMed] [Google Scholar]