Dear Editor,
COVID-19 pandemic has significantly affected surgical training of residents, especially for nonemergency surgeries.[1] Cataract surgeries are one of them. Also, patients eligible and willing for astigmatism correcting surgeries with toric intraocular lenses (IOL) form a minor chunk of cataract surgery eligible patients on which a trainee/resident rarely gets a hand on, more so during current COVID-19 times.
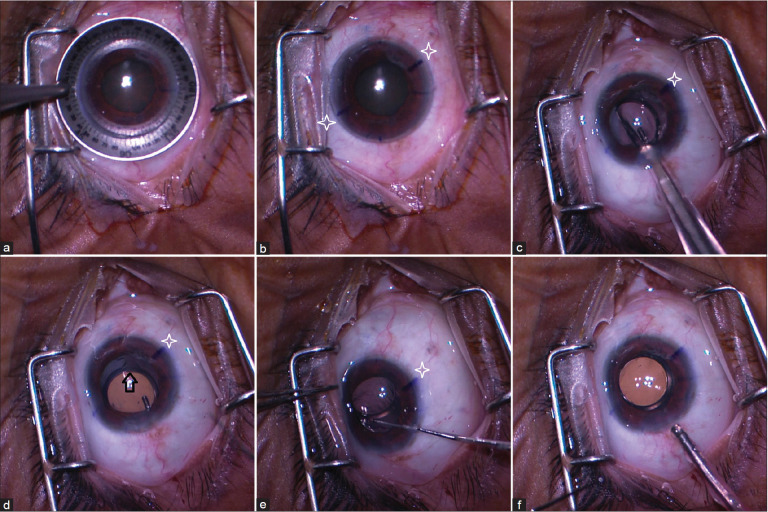
We propose that even normal cataract surgery (nontoric) can be a training tool for toric IOL implantation with our method as described below. The surgeon can mark 0, 180, and 270 degrees axes on the cornea (in standing position) before taking the patient on operating table. The marks are to be verified on table [Fig. 1a] in supine position (keeping cyclotorsion of the eye in supine position in mind). A random axis can be marked on the cornea [here 30 degrees from vertical, Fig. 1b]. The normal steps of phacoemuslification and foldable IOL implantation[2] have to be followed [Fig. 1c]. The surgeon’s aims should be to align the haptic–optic junction [Fig. 1d, arrow] with the 30-degree mark [Fig. 1e, star] at the end of the surgery [Fig. 1f]. Here, we are taking the haptic–optic junction of nontoric IOL as equivalent to toric mark on the toric IOL. All patients with a good dilating pupil and corneal clarity are eligible for such surgery.
Figure 1.
(a) Axis marking on table; (b) axis marked 30 degrees from vertical (star); (c) foldable nontoric IOL implantation; (d) haptic–optic junction is marked with arrow; (e) surgeon trying to rotate and align arrow (haptic–optic junction) with star (30-degree axis); and (f) alignment done and surgery completed
The advantage is that during early learning curve, where malalignment/rotations of the IOL are likely, our technique will theoretically eliminate any cylindrical refractive error (our IOL being nontoric) that can occur with malalignment/rotation of an actual toric IOL. A resident/trainee can practice enough to improve his surgical skills before shifting on toric cases. To conclude, we propose using haptic–optic junction of nontoric IOL as alignment reference to practice for toric IOL surgeries.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1. Aziz H, James T, Remulla D, Sher L, Genyk Y, Sullivan ME, et al. Effect of COVID-19 on surgical training across the United States: A national survey of general surgery residents. J Surg Educ. 2021;78:431–9. doi: 10.1016/j.jsurg.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sen S, Patil M, Saxena R, Kumar A, Amar SP, Das D, et al. Perceived difficulties and complications in learners of phacoemulsification: A principal component analysis model. Indian J Ophthalmol. 2019;67:213–6. doi: 10.4103/ijo.IJO_1133_18. [DOI] [PMC free article] [PubMed] [Google Scholar]