Abstract
Purpose:
Ocular trauma is one of the major preventable causes of ocular morbidity and blindness in children and young adults. Firework injuries account for 20% of ocular trauma. The purpose of this study was to describe the clinical profile and assess the severity of the ocular injuries sustained from fireworks in Eastern India mainly during the festive season.
Methods:
This was a retrospective, hospital-based case study of patients with ocular injuries sustained from fireworks during the year 2017–2020. The study was conducted at a tertiary care hospital in Eastern India. Demographic details, type of injury, duration of injury, visual status, diagnostic tests, and management were recorded.
Results:
Sixty-five patients were reported to suffer from firework-related ocular injuries. The majority of cases were male (51/78.5%). The mean age was 21.78 ± 16.82 years (range: 0–90 years). Children and young adult males were mostly affected (n = 40, 61.5%). Most common offending agent was the bottle rockets (n = 23, 35.4%), followed by bomb and crackers in (n = 18, 27.7%). Majority of the injuries occurred at home environment (n = 37, 56.9%), followed by street (n = 15, 23.1%). About (n = 39, 60%) of the injuries occurred among bystanders. About 40 cases (61.5%) hailed from rural areas. The majority of the cases (n = 46, 70.8%) suffered from closed globe injuries and surgical intervention was required in (n = 40, 61.5%) of the cases. The mean length of hospital stay of fewer than 5 days was required in (n = 42, 64.6%). The final visual acuity of 6/18 or better was achieved in 41 cases (63.1%).
Conclusion:
Ocular injuries from fireworks remain a public health problem. Awareness among the masses, preventive measures, and strict implementation of government legislation may help in bringing down the incidence of firework-related ocular morbidity and blindness.
Keywords: Blindness, Diwali, fireworks, ocular injuries
Fireworks have been the main source of entertainment and celebration during various festive occasions all over the world. The instant joy felt by the visual and auditory display produced by these fireworks makes them popular in all types of occasions, such as the New Year celebrations in China, Deepavali in India, the Prophet’s birthday in Libya, and the Fourth of July in the USA.[1,2,3,4] Though fireworks are used for enjoyment, the ocular injuries caused by them vary from trivial to devastating injuries which may lead to permanent loss of vision. The law and legislation in India are not strict as in the Western countries; hence, there is misuse of fireworks in public places and mass gatherings. Various disabilities and visual impairment in both children and adults can result in an economic loss to the individual and society.
India is a country of cultural diversity. Different regional festivals are celebrated around the year. Diwali is a common festival celebrated all over the country in November with great enthusiasm, and fireworks form an essential part of it. During this festival season, there is a dramatic increase in the number of patients with ocular injuries due to fireworks presenting to the emergency department. Although there are various papers in the literature documenting the firework injuries from different parts of the world[5,6,7], only a few studies are available from Eastern India.[8]
We conducted this retrospective study to document and evaluate the clinical profile, visual outcome, and management of firework-related ocular injuries in a tertiary care hospital in Eastern India. The purpose of this study was to create awareness about the consequences of such injury among the general population and preventive measures to be followed during this period.
Methods
This was a retrospective, observational, hospital-based study that was carried out on 65 patients treated at a tertiary hospital in Eastern India for firework-related ocular injuries between two weeks of the Diwali festival from the year 2017–2020. This study has been approved by the Institutional ethical committee and has been conducted in accordance with the Helsinki protocol. The medical records of all patients who attended the emergency services of the Ophthalmology department for ocular trauma caused by firework injury were included in the study. Patients with extraocular injuries that were severe and life-threatening requiring multispecialty management were excluded from this study. A specific proforma was prepared to record the demographic data, socioeconomic status, type of injury, cause of injury, and details of ocular examination and management procedures. Ocular B-scan ultrasonography, gonioscopy, fundus photography, and X-ray orbit or CT scan of brain and orbit were done as and when indicated. The initial visual acuity and the final visual acuity after treatment were also recorded. The injuries were classified according to the Birmingham eye trauma terminology system. The medical and surgical treatment were also noted. The primary surgeries were lid tear repair, corneal and scleral tear repair, and traumatic cataract. The causes of severe visual loss and blindness were also recorded. Poor visual outcome was defined as vision of <6/60 and unilateral blindness as vision of <3/60 in the injured eye.
Statistical analysis
In patients with bilateral involvement, both eyes were used for statistical analysis. Data was entered in an excel sheet, and statistical analysis was performed using STATA version 13. Frequency and percentage were calculated for categorical variables, and mean ± standard deviation for continuous variables. Logistic regression analyses were performed to calculate the odds ratio of poor visual outcome as a function of age, type of injury, and hospital reporting time. A value of P < 0.05 was considered statistically significant by the student’s t-test.
Results
Demographic and spectrum of ocular injuries
There were 65 participants with ocular injuries from firecrackers who presented during the Diwali period from 2017–2020. The age and sex distribution are shown in Table 1. Majority of the cases were males (n = 51, 78.5%). The mean age of males was 21.4 ± 17.01 years and that of females was 23.03 ± 16.64 years. Around 40 cases (61.5%) were children and young adults (0–20 years). Majority of them were from rural area (n = 40, 61.5%).
Table 1.
Distribution of socio-demographic profile among Ocular firecracker injuries
| Male (n=51) | Female (n=14) | Total (n=65) | P | |
|---|---|---|---|---|
| Mean age (years) | 21.44±17.01 | 23.03±16.64 | 21.78±16.82 | 0.76* |
| Age category | 0.785# | |||
| 0-20 years | 33 (64.71%) | 7 (50.0%) | 40 (61.54%) | |
| 21-40 years | 12 (23.53%) | 5 (35.71%) | 17 (26.15%) | |
| 41-60 years | 3 (5.88%) | 1 (7.14%) | 4 (6.15%) | |
| >60 years | 3 (5.88%) | 1 (7.14%) | 4 (6.15%) | |
| Residence | 0.007# | |||
| Urban | 24 (47.06%) | 1 (7.14%) | 25 (38.46%) | |
| Rural | 27 (52.94%) | 13 (92.86%) | 40 (61.54%) | |
| Type of firecracker | 0.923# | |||
| Bottle rocket | 18 (35.29%) | 5 (35.71%) | 23 (35.38%) | |
| Bomb cracker | 15 (29.41%) | 3 (21.43%) | 18 (27.69%) | |
| Sparkles | 6 (11.76%) | 3 (21.43%) | 9 (13.85%) | |
| Cone fountain | 5 (9.80%) | 1 (7.14%) | 6 (9.23%) | |
| Flame | 2 (3.92%) | 1 (7.14%) | 3 (4.62%) | |
| Ground spinners | 5 (9.80%) | 1 (7.14%) | 6 (9.23%) | |
| Place of injury | 0.780# | |||
| Home | 27 (52.94%) | 10 (71.43%) | 37 (56.92%) | |
| Recreational | 6 (11.76%) | 1 (7.14%) | 7 (10.77%) | |
| Street | 13 (25.49%) | 2 (14.29%) | 15 (23.08%) | |
| Unknown | 1 (1.96%) | 0 (0.00%) | 1 (1.54%) | |
| Others | 4 (7.84%) | 1 (7.14%) | 5 (7.69%) | |
| Occurrence of injury | 0.109# | |||
| Involved | 23 (45.10%) | 3 (21.43%) | 26 (40%) | |
| Bystander | 28 (54.90%) | 11 (78.57%) | 39 (60%) | |
| Eye protection device | 0.052# | |||
| Yes | 1 (1.96%) | 2 (14.29%) | 3 (4.62%) | |
| No | 50 (98.04%) | 12 (85.71%) | 62 (95.38%) |
*t-test and #Chi-square test were used as test significance for association
Most common type of firecracker injury sustained was due to bottle rocket (n = 23,35.4%), followed by bomb and firecrackers (n = 18, 27.7%), sparkles (n = 9, 13.9%), and others (n = 15, 23.1%). Majority of the injuries occurred in home environment (n = 37, 56.9%), followed by street (n = 15, 23.1%). About 39 cases (60%) occurred among bystanders and (n = 26,40%) were actively involved with the firecrackers. Majority (n = 62, 95.4%) of cases had not used any eye protection devices while playing with the firecrackers [Table 1].
In this study, 38 (58.46%) patients reported early to the hospital, within 24 hours of injury, as shown in [Fig. 1]. Most of them had no associated injuries other than in the eye. Majority of the cases (57, 87.7%) had unilateral ocular involvement. There were closed globe injuries in 46 (70.8%) cases and open globe injuries in 19 (29.23%) cases as described in [Table 2]. Most of the injuries sustained were confined to the anterior segment in 53 (81.5%) cases. Among them, corneal abrasions were seen in 35 eyes (20.5%), followed by corneal foreign body, subconjunctival hemorrhage, and conjunctival laceration in 25 eyes (14.6%). Other lesions were lid and conjunctival burns in 24 eyes (14.0%), hyphema and corneoscleral lacerations in 9 eyes (5.3%) each, and iridodialysis in 6 eyes (3.5%), traumatic iritis in 5 eyes (2.9%), and sphincter tear in one eye (0.6%) [Fig. 2]. Traumatic cataract was seen in 6 eyes (3.5%), while subluxation of the lens was seen in 5 eyes (2.9%). The posterior segment involvement was observed in 12 cases (18.5%). Among them, the most common was retinal detachment in 5 eyes (2.9%), followed by vitreous hemorrhage in 4 eyes (2.3%) and commotion retinae in 2 eyes (1.2%). Intraocular foreign body was seen in 2 eyes (1.2%) as shown in [Fig. 3].
Figure 1.
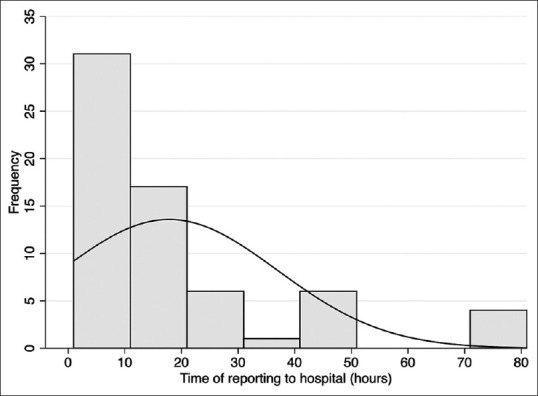
Distribution of hospital reporting hours
Table 2.
Distribution of clinical profile of firecracker ocular injuries
| Male (n=51) | Female (n=14) | Total | P # | |
|---|---|---|---|---|
| Nature of injury | 0.547 | |||
| Closed | 37 (72.55%) | 9 (64.29%) | 46 (70.77%) | |
| Open | 14 (27.45%) | 5 (35.71%) | 19 (29.23%) | |
| Spectrum of injury | 0.286 | |||
| Anterior | 40 (78.43%) | 13 (92.86%) | 53 (81.54%) | |
| Posterior | 3 (5.88%) | 1 (7.14%) | 4 (6.15%) | |
| Both | 8 (15.69%) | 0 (0.00%) | 8 (12.31%) | |
| Laterality | 0.114 | |||
| Unilateral | 43 (84.31%) | 14 (100%) | 57 (87.69%) | |
| Bilateral | 8 (15.69%) | 0 (0.00%) | 8 (12.31%) | |
| Associated injuries | 0.456 | |||
| Yes | 12 (23.53%) | 2 (14.29%) | 14 (21.54%) | |
| No | 39 (76.47%) | 12 (85.71%) | 51 (78.46%) |
#Chi-square test was used as test significance for association
Figure 2.
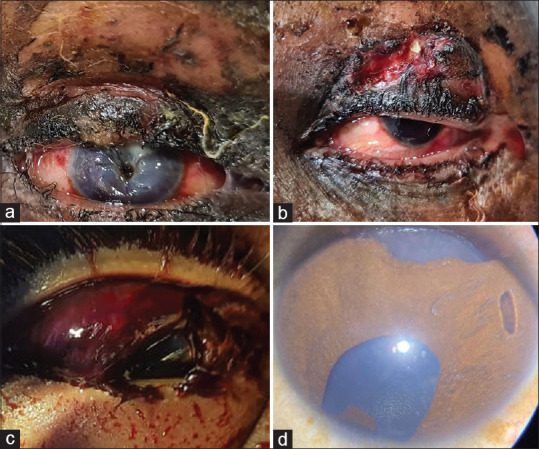
(a, b, c, d) Clinical photographs showing different types of firecracker injuries. (a) central corneal tear in the right eye; (b) hyphaema with upper lid laceration in the left eye, (c) corneal tear with subconjunctival hemorrhage and chemosis in the right eye; (d) traumatic iridodialysis in the right eye
Figure 3.
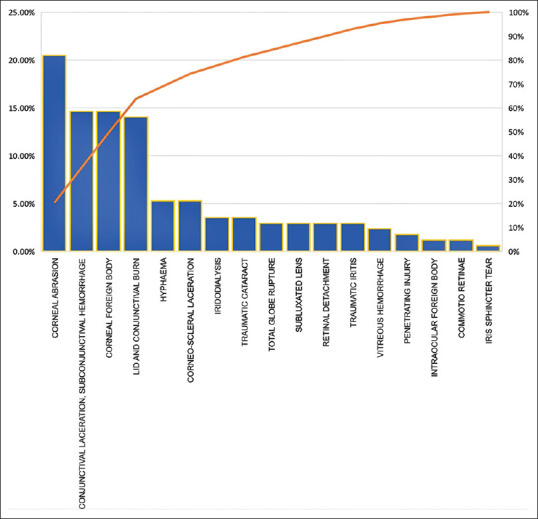
Pareto chart showing the spectrum of firecracker ocular injuries
Visual acuity at presentation was ≤ 6/60 in 39 patients (60.0%), and about 40 cases (61.5%) required some type of surgical intervention. Most of the patients (n = 42, 64.6%) required hospitalization for less than 5 days, and (n = 41, 63.1%) of them achieved a final visual acuity between 6/6–6/18 after treatment and one-month follow-up [Fig. 4].
Figure 4.

Comparison of pre- and post-treatment visual outcome in firecracker ocular injuries
We considered few variables such as age, nature of injury, reporting time to hospital after injury, spectrum of injury, type of firecrackers, use of eye protection devices (EPDs), and their association with final visual outcome. There was a significant difference in final visual outcomes with nature of injury and spectrum of injury categories by Chi-square test with the P value of < 0.0001 and 0.041 [Table 3]. In univariate analysis, the odds of having blindness in open globe injury and in those not wearing EPDs was 16.0 (95% CI; 2.97–86.23) and 13.5 (95% CI; 1.09–166.56) with P value of 0.001 and 0.042, respectively. These odds were significant in multivariate logistic regression on adjusting for variables with P value < 0.2 as shown in Table 3. The adjusted odds ratio (AOR) was 26.84 (95% CI; 2.86–252.01) and 38.07 (95% CI; 1.05–1372.43) with P value of 0.004 and 0.047 among open globe injury and in those not wearing EPDs, respectively. All the other variables were not significant in univariate and multivariate logistic regression [Table 4].
Table 3.
Association of final visual outcome with age, reporting hours and nature of injury
| 6/6-6/9 (n=22) | 6/12-6/18 (n=19) | 6/24-6/36 (n=5) | ≤6/60 (n=9) | No PL (n=10) | Total (n=65) | P* | |
|---|---|---|---|---|---|---|---|
| Age category | 0.180 | ||||||
| 0-20 years | 17 (77.27%) | 15 (78.95%) | 2 (40.00%) | 2 (22.22%) | 4 (40.00%) | 40 (61.54%) | |
| 21-40 years | 3 (13.64%) | 2 (10.53%) | 3 (60.00%) | 5 (55.56%) | 4 (40.00%) | 17 (26.15%) | |
| 41-60 years | 1 (4.55%) | 1 (5.26%) | 0 (0.00%) | 1 (11.11%) | 1 (10.00%) | 4 (6.15%) | |
| >60 years | 1 (4.55%) | 1 (5.26%) | 0 (0.00%) | 1 (11.11%) | 1 (10.00%) | 4 (6.15%) | |
| Sex | 0.695 | ||||||
| Male | 16 (72.73%) | 17 (89.47%) | 4 (80.00%) | 7 (77.78%) | 7 (70.00%) | 51 (78.46%) | |
| Female | 6 (27.27%) | 2 (10.53%) | 1 (20.00%) | 2 (22.22%) | 3 (30.00%) | 14 (21.54%) | |
| Nature of injury | <0.001 | ||||||
| Close globe | 20 (90.91%) | 16 (84.21%) | 5 (100%) | 3 (33.33%) | 2 (20.00%) | 46 (70.77%) | |
| Open globe | 2 (9.09%) | 3 (15.79%) | 0 (0.00%) | 6 (66.67%) | 8 (80.00%) | 19 (29.23%) | |
| Hospital reporting hours | 0.193 | ||||||
| Early | 16 (72.73%) | 12 (63.16%) | 3 (60.00%) | 4 (44.44%) | 3 (30.00%) | 38 (58.46%) | |
| Late | 6 (27.27%) | 7 (36.84%) | 2 (40.00%) | 5 (55.56%) | 7 (70.00%) | 27 (41.54%) | |
| Spectrum | 0.041 | ||||||
| Anterior | 21 (95.45%) | 16 (84.21%) | 2 (40.00%) | 6 (66.67%) | 8 (80.00%) | 53 (81.54%) | |
| Posterior | 1 (4.55%) | 3 (15.79%) | 3 (60.00%) | 3 (33.33%) | 2 (20.00%) | 12 (18.46%) | |
| Firecrackers | 0.630 | ||||||
| Bottle rocket | 7 (31.82%) | 5 (26.32%) | 2 (40.00%) | 4 (44.44%) | 5 (50.00%) | 23 (35.38%) | |
| Bomb crackers | 6 (27.27%) | 6 (31.58%) | 2 (40.00%) | 2 (22.22%) | 2 (20.00%) | 18 (27.69%) | |
| Sparkles | 2 (9.09%) | 5 (26.32%) | 1 (20.00%) | 0 (0.00%) | 1 (10.00%) | 9 (13.85%) | |
| Cone fountain | 4 (18.18%) | 1 (5.26%) | 0 (0.00%) | 1 (11.11%) | 0 (0.00%) | 6 (9.23%) | |
| Flame | 1 (4.55%) | 2 (10.53%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 3 (4.62%) | |
| Ground spinners | 2 (9.09%) | 0 (0.00%) | 0 (0.00%) | 2 (22.22%) | 2 (20.00%) | 6 (9.23%) | |
| Use of EPDs# | 0.137 | ||||||
| Yes | 1 (4.55%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 2 (20.00%) | 3 (4.62%) | |
| No | 21 (95.45%) | 19 (100%) | 5 (100%) | 9 (100%) | 8 (80.00%) | 62 (95.38%) |
*Chi-square test was used for testing significance of association. #EPD - Eye Protection Device
Table 4.
Univariate and multivariate logistic regression of visual outcome with various determinants
| Variables | COR* (95% CI) | P | AOR# (95% CI) | P |
|---|---|---|---|---|
| Age | 1.01 (0.98-1.05 | 0.487 | 0.99 (0.94-1.04) | 0.701 |
| Open globe injury | 16 (2.97-86.23) | 0.001 | 26.68 (2.86-248.64) | 0.004 |
| Early hospital reporting | 4.08 (0.95-17.58) | 0.059 | 2.01 (0.32-12.63) | 0.458 |
| Posterior segment injury | 1.12 (0.21-6.12) | 0.892 | 0.81 (0.06-11.26) | 0.876 |
| No eye protection devices | 13.5 (1.09-166.56) | 0.042 | 38.07 (1.05-1372.43) | 0.047 |
*COR=Crude odds ratio, #AOR=Adjusted odds ratio
Discussion
Globally, there is a great concern for firework-related ocular injuries. Several studies have emphasized the high incidence of firework injuries, mainly during holiday and religious periods.[2,5,9,10,13] In the USA, 95% of such injuries occur around the Independence Day celebration; in Greece, there is a peak during the Greek Orthodox Easter; in Iran during their end-of-year celebrations; and in India during the Diwali festival.[12,14,15,16]
In our study, although all age groups were affected, the majority of the patients were below 20 years (61.5%). The patients were mainly teenagers and young adult males in their productive years of life, who were daring and adventurous. Our findings for the age of <20 years are consistent with the various studies reported worldwide.[17,18,19,20,21,22,23] Further, there were only eight children among 25 affected children who had direct supervision during the period of firework celebration. The loss of vision in children is a matter of great concern as it changes their entire lifestyle, adding to psychological trauma and social burden to the family and society at large.
The most common injuries in our study were sustained from bottle rockets, followed by bombs (sound-emitting devices) and crackers, similar to reports from other Indian studies.[8] Bottle rockets, although meant for emanating flare and lights only, frequently explode, causing multiple injuries. Singh et al.[18] reported that injuries caused by rockets were more frequently associated with facial lacerations, intraocular foreign body, endophthalmitis, and poor visual outcome. Sparklers are usually considered safe and innocuous but attain a temperature of 1200 degrees Fahrenheit, which can cause grievous burns.[9] Children usually play with these types of fireworks and must be under supervision to avoid burn injuries. The other cause of ocular injuries are failed crackers that on fiddling leads to an unpredictable explosion and multiple injuries.
In this study, the proportion of bystanders sustaining injuries were high (60%) and 12.8% had serious injuries with no projection of light. There were only a few cases (4.6%) who were wearing eye protection shields. These findings indicate that public awareness among those watching fireworks and the use of protective glasses must be emphasized. See et al.[24] (1994) and Kong et al.[25] (2015) suggested the use of protective polycarbonate glasses to reduce the incidence and severity of ocular injuries. Initiatives can be taken by the government to provide free protective glasses in conjunction with firework purchases to at least protect the person handling the fireworks.
Ocular injuries in 14 patients (21.5%) had associated/co-existing injuries such as facial burns, head and neck, and limb injuries that required a multidisciplinary approach. The ocular injuries sustained involved both superficial and deep ocular structures as well as periocular tissues. The most common injuries were lid injuries, corneal abrasions, superficial foreign bodies of the cornea and conjunctiva, and hyphema, which were analogous to findings of other large series as described in [Table 5].[1,5,6,8,13,14,19,21,23,26,27,28,30]
Table 5.
Comparative study on firecracker ocular injuries
| Author and year of publication | Type of study | Sample size | Age group (years) | Bystanders | Nature of injury | Final visual outcome | Follow-up (months) | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| CG | OG | |||||||
| Sundelin K et al, 2000[1] | Prospective | 52 (72 eyes) | Median 13 | 29% | 67 eyes | 5 eyes | 32 (62%) cases recovered | - |
| Kuhn F et al, 2000[5] | Retrospective | 187 | - | 67% | N/A | 80% eyes improved | - | |
| Arya SK et al, 2001[8] | Prospective | 42 | Mean 15.5 | - | 39 (92.9%) | 3 (7.1%) | 29 (69%) cases final VA of 6/6-6/9 | 3 |
| Kumar R et al, 2010 [13] | Retrospective | 51 | Mean 19 | 56.9% | 49 eyes | 9 eyes | 4 eyes - >20/200 | - |
| Jing Y et al, 2010 [14] | Retrospective | 24 (25 eyes ) | Mean 25.0±17.3 | 33.3% | 9 cases | 15 | 7 eyes- final BCVA >0.05 | 5 |
| Malik A et al, 2013 [6] | Retrospective | 101 | Mean17.60±11.9 | 37.6% | 84 | 17 | Final VA 0.09 and 0.58 for CGI and OGI, respectively | - |
| Patel R et al, 2016 [19] | Prospective | 49 | Mean 17 | 48.9% | 33 (67.34%) | 13 (26.53%) | 31 (63.3%) cases - final VA >20/40 | - |
| Venkatesh R et al, 2017[21] | Retrospective | 45 (53 eyes ) | Mean 20.55 | 55.6% | 48 (90.56%) eyes | 5 (9.43%) eyes | 22 eyes - final BCVA 6/6 | - |
| Pujari A et al, 2018 [30] | Cross-sectional | 68 | Mean 16 | 64.7% | 12 (17.65%) | 56 cases (82.35%) | - | - |
| Kurien NA et al, 2020[23] | Observational | 96 (122 eyes) | Median (IQR) 14 (8-28.5) | 53.8% | 114 eyes | 8 eyes | 78 cases-final VA 6/6 | 11.5 |
CG: closed globe, OG: open globe
Corneal injuries were the commonest manifestation in our series (40.3%), followed by eyelid injuries (14.0%). Closed globe injuries accounted for 46 (70.7%) cases, while open globes injuries were 19 (29.2%) cases. This was comparable to the study by Venkatesh et al. where they reported CGI (64.2%) as the majority of all injuries while a study from China reported a higher preponderance of open globe injuries.[14,21] Posterior segment injuries were observed in 12 patients (18.5%); among these, the most common was retinal detachment (2.9%), followed by vitreous hemorrhage 2.3%. Further delayed complications of ocular trauma, such as angle recession glaucoma and traumatic cataract, were also seen during follow-up. Evisceration of severely damaged eye was advised in two (3.1%) of our patients. The percentage of cases requiring surgical intervention in our study was 61.5%. There is a wide variation in surgical intervention (12%–91%) reported in different studies.[2,23] Our hospital, being a tertiary care institute, the majority of cases had moderate to severe forms of injuries compared to other settings.[23]
Despite diagnostic and therapeutic advances, firework-related ocular injuries remain a significant cause of visual loss.[9,19] In our study, 20 (30.7%) patients had light perception at presentation, which reduced to 10 (15.4%) patients following treatment in the final visit. Smith et al.[9] reported a hospitalization rate of 11% in their study. In our study, 42 (64.6%) patients required hospital stay of less than 5 days, while 23 (35.4%) patients more than 5 days, highlighting the severity of injury and possible impact on their economic burden.
There are reports from different parts of the world stating the negative effects of ocular injuries on the rise after the removal of the ban on fireworks.[20,21] Chan et al.[15] reported tripling of ocular injuries after the removal of the ban on fireworks in 1996 in Ireland. In 1984, WHO recommended a worldwide ban on the manufacture of all fireworks.[20,21,29] Countries using restrictive fireworks legislation showed 87% less ocular trauma (P < 0.005).[24] Pujari et al.[30] reported a reduction of 59.5% in firecracker-related ocular injuries in India. This index study also reported the decrease in the number of firecracker injuries to two cases during Diwali in the COVID-19 period (2020) as there was a nationwide ban on sale of firecrackers, thus laying the emphasis on strict legislative policies.
Patel et al.[19] reported that about INR 5000 cores worth of consumer fireworks are spent in India during Diwali season. Apart from burn injuries, noise and air pollution are two other health hazards noticed. The Central Pollution Control Board estimates that 95% of firecrackers violate noise and pollution norms.[20,21] Hence, to reduce the health hazards, the Government of India restricted the use of firecrackers after 10.00 pm. Strategies are needed to reduce the hazards of ocular injuries by standardizing the quality of the firecrackers sold in the market. Public display of fireworks in open wide grounds with trained professionals must be encouraged. Social and seasonal awareness programs mainly in schools can play a key role in preventing firework injuries. Children, parents, and teachers can be made aware of the damage caused by firecrackers. Media, in the form of television, mobile, or newspaper, can also be used for public education.
The limitations of this study were its retrospective nature and cases which presented to the government hospital were analyzed; thus, the status of patients presenting to private hospitals was missed and hence the epidemiological pattern may vary. Second, the sample size was small in our study. Clinical studies with longer follow-up can predict long-term complications. Planning population-based studies can help in estimating the incidence, impact, and economic implications in the future.
Conclusion
Firework injuries present a hazard to ocular health. This study supports the worldwide reports that ocular injuries from fireworks are mainly a problem of the nation’s youth and can be prevented. Vision loss can be profound, leading to economic loss to the nation. Hence, there is a need for a nationwide campaign on firework safety to increase its effectiveness. Public awareness and strict implementation of government legislation in this regard may help in bringing down the incidence and severity of firework-related ocular injuries.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1. Sundelin K, Norrsell K. Eye injuries from fireworks in Western Sweden. Acta Ophthalmol Scand. 2000;78:61–4. doi: 10.1034/j.1600-0420.2000.078001061.x. [DOI] [PubMed] [Google Scholar]
- 2. Lee RT. Fire-cracker injury to the eyes in Hong Kong. Br J Ophthalmol. 1966;50:666–9. doi: 10.1136/bjo.50.11.666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Levitz LM. Children and fireworks--A dangerous combination. S Afr Med J. 1997;87:1554–6. [PubMed] [Google Scholar]
- 4. McFarland LV, Harris JR, Kobayashi JM, Dicker RC. Risk factors for fireworks-related injury in Washington State. JAMA. 1984;251:3251–4. [PubMed] [Google Scholar]
- 5. Kuhn F, Morris R, Witherspoon CD, Mann L, Mester V, Módis L, et al. Serious fireworks-related eye injuries. Ophthalmic Epidemiol. 2000;7:139–48. [PubMed] [Google Scholar]
- 6. Malik A, Bhala S, Arya SK, Sood S, Narang S. Five-year study of ocular injuries due to fireworks in India. Int Ophthalmol. 2013;33:381–5. doi: 10.1007/s10792-013-9714-x. [DOI] [PubMed] [Google Scholar]
- 7. Vassilia K, Eleni P, Dimitrios T. Firework-related childhood injuries in Greece:A national problem. Burns. 2004;30:151–3. doi: 10.1016/j.burns.2003.09.019. [DOI] [PubMed] [Google Scholar]
- 8. Arya SK, Malhotra S, Dhir SP, Sood S. Ocular fireworks injuries. Clinical features and visual outcome. Indian J Ophthalmol. 2001;49:189–90. [PubMed] [Google Scholar]
- 9. Smith GA, Knapp JF, Barnett TM, Shields BJ. The rockets'red glare, the bombs bursting in air:fireworks-related injuries to children. Pediatrics. 1996;98:1–9. [PubMed] [Google Scholar]
- 10. Thygesen J. Ocular injuries caused by fireworks. 25 years of experience with preventive campaigns in Denmark. Acta Ophthalmol Scand. 2000;78:1–2. [PubMed] [Google Scholar]
- 11. Mansouri MR, Mohammadi SF, Hatef E, Rahbari H, Khazanehdari MS, Zandi P, et al. The persian wednesday eve festival “Charshanbe-Soori”fireworks eye injuries:A case series. Ophthalmic Epidemiol. 2007;14:17–24. doi: 10.1080/09286580600878836. [DOI] [PubMed] [Google Scholar]
- 12. Knox FA, Chan WC, Jackson AJ, Foot B, Sharkey JA, McGinnity FG. A British Ophthalmological Surveillance Unit study on serious ocular injuries from fireworks in the UK. Eye. 2008;22:944–7. doi: 10.1038/sj.eye.6702778. [DOI] [PubMed] [Google Scholar]
- 13. Kumar R, Puttanna M, Sriprakash KS, Rathod BS, Prabhakaran VC. Firecracker eye injuries during Deepavali festival:A case series. Indian J Ophthalmol. 2010;58:157–9. doi: 10.4103/0301-4738.60095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jing Y, Yi-Qiao X, Yan-Ning Y, Ming A, An-Huai Y, Lian-Hong Z. Clinical analysis of firework-related ocular injuries during Spring Festival 2009. Graefes Arch Clin Exp Ophthalmol. 2010;248:333–8. doi: 10.1007/s00417-009-1292-2. [DOI] [PubMed] [Google Scholar]
- 15. Chan WC, Knox FA, McGinnity FG, Sharkey JA. Serious eye and adnexal injuries from fireworks in Northern Ireland before and after lifting of the firework ban-An ophthalmology unit's experience. Int Ophthalmol. 2004;25:167–9. doi: 10.1007/s10792-004-1958-z. [DOI] [PubMed] [Google Scholar]
- 16. Hatamabadi HR, Tabatabaey A, Heidari K, Khoramian MK. Firecracker injuries during Chaharshanbeh Soori festival in Iran:A case series study. Arch Trauma Res. 2013;2:46–9. doi: 10.5812/atr.9250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lin Y, Liang X, Liu X, Qu B, Ni Y, Jiang S, et al. Prognostic factors and visual outcome for fireworks-related burns during spring festival in South China. J Burn Care Res. 2012;33:e109–14. doi: 10.1097/BCR.0b013e3182335998. [DOI] [PubMed] [Google Scholar]
- 18. Singh DV, Sharma YR, Azad RV. Visual outcome after fireworks injuries. J Trauma Acute Care Surg. 2005;59:109–11. doi: 10.1097/01.ta.0000172643.61750.af. [DOI] [PubMed] [Google Scholar]
- 19. Patel R, Mukherjee B. Crash and burn:Ocular injuries due to fireworks. Semin Ophthalmol. 2016;31:243–8. doi: 10.3109/08820538.2014.962157. [DOI] [PubMed] [Google Scholar]
- 20. John D, Philip SS, Mittal R, John SS, Paul P. Spectrum of ocular firework injuries in children:A 5-year retrospective study during a festive season in Southern India. Indian J Ophthalmol. 2015;63:843–6. doi: 10.4103/0301-4738.171966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Venkatesh R, Gurav P, Tibrewal S, Agarwal M, Dubey S, Mathur U, et al. Appraising the spectrum of firework trauma and the related laws during Diwali in North India. Indian J Ophthalmol. 2017;65:140–3. doi: 10.4103/ijo.IJO_527_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Frimmel S, de Faber JT, Wubbels RJ, Kniestedt C, Paridaens D. Type, severity, management and outcome of ocular and adnexal firework-related injuries:The Rotterdam experience. Acta Ophthalmol. 2018;96:607–15. doi: 10.1111/aos.13711. [DOI] [PubMed] [Google Scholar]
- 23. Kurien NA, Peter J, Jacob P. Spectrum of ocular injuries and visual outcome following firework injury to the eye. J Emerg Trauma Shock. 2020;13:39–44. doi: 10.4103/JETS.JETS_62_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. See LC, Lo SK. Epidemiology of fireworks injuries:The national electronic injury surveillance system, 1980-1989. Ann Emerg Med. 1994;24:46–50. doi: 10.1016/s0196-0644(94)70161-x. [DOI] [PubMed] [Google Scholar]
- 25. Kong Y, Tang X, Kong B, Jiang H, Chen Y. Six-year clinical study of firework-related eye injuries in North China. Postgrad Med J. 2015;91:26–9. doi: 10.1136/postgradmedj-2014-132837. [DOI] [PubMed] [Google Scholar]
- 26. Smittenberg MN, Lungelow D, Rode H, Van As AB, Millar AJ. Can fireworks-related injuries to children during festivities be prevented? S Afr Med J. 2010;100:525–8. doi: 10.7196/samj.3964. [DOI] [PubMed] [Google Scholar]
- 27. Wilson RS. Ocular fireworks injuries and blindness:an analysis of 154 cases and a three-state survey comparing the effectiveness of model law regulation. Ophthalmology. 1982;89:291–7. doi: 10.1016/s0161-6420(82)34789-2. [DOI] [PubMed] [Google Scholar]
- 28. Wisse RP, Bijlsma WR, Stilma JS. Ocular firework trauma:A systematic review on incidence, severity, outcome and prevention. Br J Ophthalmol. 2010;94:1586–91. doi: 10.1136/bjo.2009.168419. [DOI] [PubMed] [Google Scholar]
- 29.World Health Organisation. Strategies for the Prevention of Blindness in National Programs. Geneva: WHO; 1984. [Google Scholar]
- 30. Pujari A, Kumar A, Chawla R, Khokhar S, Agarwal D, Gagrani M, et al. Impact on the pattern of ocular injuries and awareness following a ban on firecrackers in New Delhi:A tertiary eye hospital-based study. Indian J Ophthalmol. 2018;66:837–40. doi: 10.4103/ijo.IJO_1290_17. [DOI] [PMC free article] [PubMed] [Google Scholar]


