Abstract
Purpose:
To describe our results with the AssiAnchor capsule device in cases of subluxated crystalline lenses.
Methods:
This was a retrospective consecutive case series. Seven eyes of four patients with subluxated crystalline lenses underwent lensectomy/phacoemulsification with intraocular lens (IOL) implantation using the AssiAnchor capsule device in the Kaplan medical center, ophthalmology department. Three patients had Marfan syndrome and one patient had experienced blunt trauma. Demographic data were collected as well as parameters of pre- and postoperative distance visual acuity and refraction, intra-, and postoperative complications, and IOL stability and centration.
Results:
Six out of the seven surgical procedures were uneventful with in-the-bag implantation of the IOL. In the first surgery, a tear of the capsular bag lead to IOL exchanging and fixating to the AssiAnchor and to the iris. In the traumatic cataract case, two AssiAnchors were used. A capsular tension ring was implanted in six out of seven surgeries. The average follow-up time was 9.5 ± 6.8 months. All the IOLs were stable and well centered except for the first IOL that exhibited a slight temporal, but not clinically significant, decentration. The distance visual acuity and the refractive parameters improved significantly in all cases.
Conclusion:
We found the AssiAnchor capsule device an effective tool with a short learning curve for treating subluxated lenses.
Keywords: AssiAnchor capsule device, capsular bag, fixation, stabilization, subluxation
Subluxated lenses represent one of the most difficult surgical challenges even for experienced cataract surgeons and a number of devices for capsular support and improving lens stability have been developed to preserve the capsular bag and allow the implantation of an intraocular lens (IOL). Capsular tension ring (CTR) implantations provide equal distribution and restore the circular contour of the capsule equator in cases of mild generalized zonular weakness or in the presence of up to 3–4 h of segmental zonulysis. Modified CTRs (Cionni endocapsular ring, Ahmed capsular tension segment, or Malyugin-Cionni endocapsular ring) are rings or segments with one or two short loops, and with an eyelet that extends out of the capsular bag while the ring itself is implanted inside. The loop is fixed to the scleral wall and stabilizes the capsular bag.[1,2,3,4,5,6]
The AssiAnchor is a relatively new capsule-anchoring device, designed to treat moderate to severe subluxated lenses. Fig. 1 presents an illustration of the AssiAnchor capsule device.
Figure 1.

Illustration of the AssiAnchor capsule device. This is a PMMA intraocular implant. The lateral arms are inserted beneath the capsulorhexis, while the central portion remains above the capsular bag and is used to secure the anterior capsular bag to the sclera. (courtesy of Hanita Lenses, Israel)
The device is a poly-methyl methacrylate (PMMA) intraocular implant that anchors the anterior capsule to the sclera. The principle is similar to that of a paper clip: two lateral arms are inserted beneath the capsulorhexis, while a central portion remains above the capsule. The device is then sutured and secured to the scleral wall, fixing the anterior capsule to the sclera and allowing CTR implantation while maintaining the circular contours of the lens capsule.[5] The anchor can be inserted at any time during surgery, either before or after lens removal and IOL implantation.
The purpose of this study was to present our results using the AssiAnchor capsule device for the treatment of subluxated crystalline lenses.
Methods
The study included four patients (seven eyes) with subluxated crystalline lenses, three patients with Marfan syndrome, and one who had experienced postocular trauma. All the patients underwent lensectomy/phacoemulsification by a single experienced surgeon between 01/2016 and 03/2018, with an IOL implantation following fixation of the anterior capsule to the scleral wall using the AssiAnchor capsule device.
The patients’ medical records were retrospectively reviewed for the following data: patient demographics, pre- and postoperative, best-corrected and uncorrected, distance visual acuity, refraction at the last follow-up, preoperative IOLMaster-500 [Carl Zeiss Meditec AG, Jena, Germany] measurements, intra and postoperative complications, IOL stability, and centration.
The study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board.
Surgical technique
The same surgeon performed all the operations. The technique is similar to that described by Assia et al.[5] Briefly, a scleral pocket was created adjacent to the area with the missing zonules followed by a 2.4 mm clear corneal incision. A capsulorhexis was created in as central a position as possible. Gentle and local hydrodissection was performed to separate the anterior capsule from the cortex, allowing the insertion of the anchor’s lateral arms beneath the anterior capsule. A double-armed 10-0 polypropylene suture on a 16.0-mm-long curved needle (12” CU-1 spatula, double armed, Alcon, USA) was inserted through a designed hole in the anchor base and then through the corneal incision. A 27-gauge needle was passed through the scleral pocket and served as a guide to withdraw the needle through the scleral pocket. The same procedure was repeated with the other needle. The AssiAnchor capsule device (Hanita Lenses, Israel) was inserted into the anterior chamber through the main corneal incision and fixed to the anterior capsule with the two lateral arms beneath the capsule and the central portion above the capsule. The suture was temporarily tied gently while centering the crystalline lens. A lensectomy or a phacoemulsification was performed. A standard CTR (Hanita Lenses, Israel) was implanted in six out of seven cases, after complete lens removal, to further stabilize the bag and restore the round contour, and an IOL was implanted. In the six uneventful surgeries, an Alcon AcrySof SA60AT (Alcon Laboratories, Fort Worth, Texas, USA), was implanted into the capsular bag. In the first surgery, an Alcon AcrySof MA60AC (Alcon Laboratories, Fort Worth, Texas, USA) was sutured on one side to the AssiAnchor capsule device and to the iris on the other side. An anterior vitrectomy, guided by triamcinolone acetate, was performed in two cases. As the last step, the 10-0 polypropylene temporary knot was opened, and the suture was retrieved from the scleral pocket and was tied permanently. Postoperative medication regimen consisted of topical treatment with dexamethasone 0.1% (Sterodex, Fischer Pharmaceutical Labs. Ltd. Tel-Aviv, Israel) and ofloxacin 0.3% (Oflox, Allergan Pharmaceuticals, Ireland Castlebar Road Westport, Co, Mayo Ireland) eye drops six times daily for the first week. Ofloxacin was discontinued after 1 week, and dexamethasone 0.1% was tapered down over 4 weeks.
Results
The mean age of the patients was 36 ± 23 years, with a range of 10–70 years. All the patients were males. The crystalline lenses in all the Marfan syndrome cases were clear with significant subluxation superiorly or superior nasally. The lens of the traumatic case had +2 nuclear sclerosis with damage to the superior temporal zonules and correspondingly inferior nasal subluxation of the lens and phacodonesis. In this case, the anterior capsule was anchored to the sclera using two AssiAnchor capsule devices to stabilize the capsular bag.
The patients’ demographic and preoperative characteristics are presented in Table 1.
Table 1.
Demographic and preoperative characteristics
| Case | Age (Y) | Sex | Eye | Follow-up (Mo) | Diagnosis | Lens status |
|---|---|---|---|---|---|---|
| 1 | 43 | M | R | 7 | Marfan syndrome | Clear lens dislocated superior nasal, vitreous fibers in the anterior chamber of the left eye |
| 2 | L | 4 | ||||
| 3 | 10 | M | R | 18 | Marfan syndrome | Clear lens superior dislocation |
| 4 | L | 3 | ||||
| 5 | 20 | M | R | 17 | Marfan syndrome | Clear lens superior nasal dislocation |
| 6 | L | 14 | ||||
| 7 | 70 | M | L | 2.5 | Trauma | Nuclear sclerosis inferior dislocation, zonulysis, and phacodonesis |
A gentle and challenging capsulorhexis was created as centrally as possible, working partly under the iris plane due to the decentered lens, in some of the cases. CTR was implanted in all but the first surgery. A major complication was seen only in the first surgery, when due to the relatively small capsulorhexis, a radial tear occurred that extended from the anterior to the posterior capsule during the manipulation to insert the Alcon AcrySof SA60AT IOL into the capsular bag. As a result, the IOL was replaced by a MA60AC IOL that was implanted into the sulcus. Since the AssiAnchor was stable and already fixated to the sclera using the Hoffman pocket so the suture was hidden and not easy to break, we decided to avoid another penetration with the needle through the sclera or the iris with its potential complication. The IOL haptic adjacent to the AssiAnchor was secured to it on one side, and the second haptic was sutured to the iris on the contralateral side. During these manipulations, the vitreous prolapsed into the anterior chamber, and an anterior vitrectomy was performed.
In one eye, vitreous fibers were seen in the anterior chamber through the large zonular defect before the surgery, and therefore an anterior vitrectomy was performed as planned.
The average follow-up time was 9.5 ± 6.8 months, ranging between 2.5 and 18 months (as can be seen on Table 1). All the IOLs were stable and well centered (pre- and postoperative clinical slit-lamp photos of three representative eyes can be seen in Fig. 2), except for the first IOL, which exhibited a slight, but not clinically significant, temporal decentration (Fig. 3 postoperative clinical slit-lamp photo of the eye of the first case). The uncorrected distance visual acuity, best-corrected distance visual acuity, and the refractive parameters improved in all eyes [Table 2]. In one case (No’ 3), high astigmatism was manifested in the postoperative refraction; preoperative IOL Master measurements confirmed that this was corneal astigmatism and not due to a tilt of the IOL.
Figure 2.
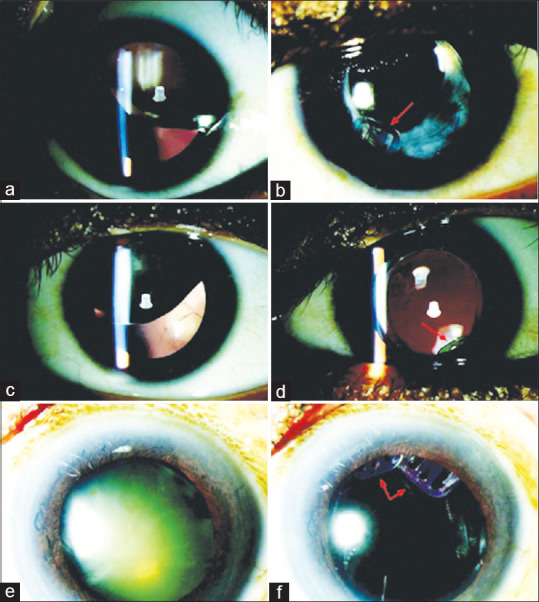
Pre- and postoperative clinical slit-lamp photos of three representative eyes. (a–d) Photos of the eyes of the 10-year-old child with Marfan syndrome (a and c right eye, b and d left eye). Photos (a) and (c) present the clear lens with significant superior nasal subluxation before the surgery. Photos (b) and (d) present the postoperative well-centered IOLs secured with the AssiAnchor (red arrows). Photos E and F are the clinical photos of the eye of the 70-year old man with cataract and damage to the superior temporal zonules, due to ocular trauma, with correspondingly inferior nasal subluxation of the lens and phacodonesis (e). In this case, two AssiAnchor devices were used to stabilize the capsular bag (red arrows) (f)
Figure 3.
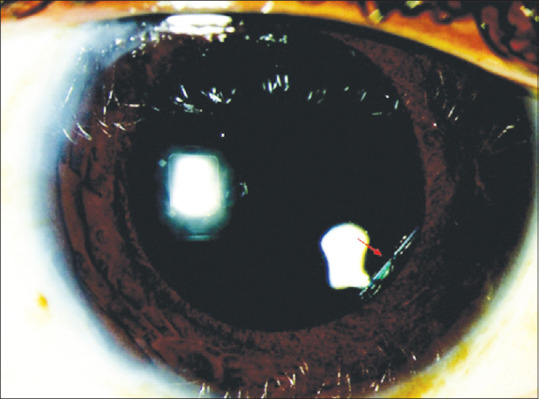
Postoperative clinical slit-lamp photo of the eye of the first case 7 months after the surgery, demonstrating a slight temporal, but not significant clinically, decentration of the IOL
Table 2.
Visual acuity and refractive parameters before the surgery and at the last follow-up
| Eye | UCDVA (LogMAR) | BCDVA (LogMAR) | Refraction Preop | Refraction Postop | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||
| Preop | Postop | Preop | Postop | Sphere | Astigmatism | S.E | Sphere | Astigmatism | S.E | |
| 1 | 1.0 | 0.7 | 0.4 | 0.3 | +13.5 | +1.00X30 | +14.0 | -2.25 | +2.25X50 | -1.25 |
| 2 | 0.7 | 0.3 | 0.3 | 0.18 | † | † | † | -0.50 | 0 | -0.50 |
| 3 | 0.78 | 0.7 | 0.7 | 0.3 | -12.0 | +8.00X90 | -8.0 | -2.00 | +4.00X90‡ | 0 |
| 4 | 0.78 | 0.7 | 0.7 | 0.3 | -12.0 | +9.00X90 | -7.5 | -1.50 | +1.50X75 | -0.75 |
| 5 | 0.7 | 0.18 | 0.4 | 0.1 | -17.5 | +9.00X83 | -13.0 | -0.75 | 0 | -0.75 |
| 6 | 0.48 | 0.1 | 0.3 | 0.0 | -17.5 | +9.00X95 | -13.0 | 0.00 | +1.00X30 | +0.5 |
| 7 | 0.78 | 0.3 | 0.48 | 0.18 | † | † | † | -1.25 | +1.00X4 | -0.75 |
| Average±SD | 0.75±0.15 | 0.43±0.27 | 0.47±0.17 | 0.19±0.12 | - 9±12.9 | +7.2±3.4 | -5.5±11.2 | -1.18±0.8 | +1.4±1.4 | -0.5±0.57 |
| Median | 0.78 | 0.3 | 0.4 | 0.18 | -12.0 | +9.0 | -8.0 | -1.25 | +1.0 | -0.75 |
| Range | 0.48-1.0 | 0.1-0.7 | 0.3-0.7 | 0.0-0.3 | (-17.5) - (+13.5) | (+1.0) - (+9.0) | (-13.0) - (+14.0) | (-2.25) - (0) | (0) - (+4.0) | (-1.25) - (0.5) |
UCDVA=uncorrected distance visual acuity, BCDVA=best-corrected distance visual acuity, and S.E=Spherical equivalent. †No refractive values were available; ‡Corneal astigmatism
No postoperative complications were recorded during the follow-up time in any of the eyes.
Discussion
CTR and their modifications (Cionni endocapsular ring, Ahmed capsular tension segment, or Malyugin-Cionni endocapsular ring) have been designed to enable safe phacoemulsification and in-the-bag IOL implantation while securing the capsule to the scleral wall, even in the presence of profound zonular dehiscence.[7] The AssiAnchor capsule device is a relatively new device, whose purpose is to secure the anterior capsule to the sclera in cases of moderate to severe subluxated lenses.[5,7]
We found the AssiAnchor capsule device to be effective in treating moderate to severe subloxated IOL with a short learning curve for an experienced surgeon. In the first case, due to a small capsulorhexis, the manipulation required to insert the IOL into the capsular bag resulted in tearing of the capsule. The intended IOL was therefore exchanged for a three-piece IOL that was secured on one side to the AssiAnchor capsule device and on the other side to the iris, with good results. All other surgeries were uneventful with no postoperative complications and a significant improvement in the patients’ refraction and visual acuity. All the IOLs, including the one in the first case, were found to be centered and stable during the follow-up period.
Our experience is similar to the report by Assia et al.,[5] who reported the results of treating four eyes with subluxated lenses, two secondary to trauma, and two due to Marfan syndrome. They suggested that scleral fixation of the bag using the anchor device was simple, independent of cataract density, and nontraumatic to the intact zonules. They also reported an anterior capsule tear in one case. Cystoid macular edema (CME) was reported in another case. Similar results were also reported by Mojzis et al.,[8] who described the results of three cases of subluxated cataracts following blunt injury, in which the use of the AssiAnchor capsule device provided a successful outcome. They had one case of capsule tear, with no postoperative complications. The AssiAnchor capsule device achieved centration of the capsular bag and, consequently of the IOL, with no significant postoperative complications during the 12–24 months of follow-up period, and with excellent visual outcomes. Another advantage of the AssiAnchor capsule device is the fixation at the level of the capsular bag rather than the capsule equator (5). Our experience with the AssiAnchor capsule device is similar to Mojzis et al.[8] in that we found it to be easily insertable under the edge of the capsulorhexis even before removal of the crystalline lens. Effective centration of the IOL–capsular bag complex could then be achieved after the lens removal and IOL implantation. This differs from the experience of Ahmed et al.[9] and Buttanri et al.,[10] who reported that the ideal timing for the implantation of the Cionni modified CTR is after phacoemulsification and decompression of the capsular bag.
Ton et al.,[11] also used the AssiAnchor capsule device for the fixation of six cases of subluxated IOL and reported good centration and stabilization. One eye developed postoperative CME and one eye developed retinal detachment one month after the IOL reposition due to prior ocular trauma.
A symptomatic posterior chamber IOL decentration was reported by Cionni et al.[2] in 6 of 90 eyes that were sutured with 10-0 polypropylene. All cases were related to breakage of the 10-0 polypropylene. They therefore recommend using 9-0 polypropylene or polytetrafluoroethylene CV-8 sutures for all modified CTR patients. A similar recommendation was reported by Ton et al.[11] regarding the AssiAnchor capsule device. They emphasized that suture degradation is a concern especially in young patients. Therefore, they also recommend using polytetrafluoroethylene sutures or 9-0 polypropylene sutures, which have significantly higher tensile force and durability than 10-0 sutures.
Conclusion
In conclusion, we found that the AssiAnchor is an effective tool for the stabilization of a subluxated crystalline lens during and after crystalline lens replacement surgery. The device enables the preservation of the capsular bag and allows for safe IOL implantation into the capsular bag with good centration and stabilization. We report a steep learning curve for an experienced surgeon. Visual acuity outcomes improved significantly as well as the patients’ refraction. A longer follow-up is required.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1. Blecher MH, Kirk MR. Surgical strategies for the management of zonular compromise. Curr Opin Ophthalmol. 2008;19:31–5. doi: 10.1097/ICU.0b013e3282f2ccc8. [DOI] [PubMed] [Google Scholar]
- 2. Cionni RJ, Osher RH. Endocapsular ring approach to the subluxed cataractous lens. J Cataract Refract Surg. 1995;21:245–9. doi: 10.1016/s0886-3350(13)80126-5. [DOI] [PubMed] [Google Scholar]
- 3. Hasanee K, Ahmed II. Capsular tension rings:Update on endocapsular support devices. Ophthalmol Clin North Am. 2006;19:507–19. doi: 10.1016/j.ohc.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 4. Gimbel HV, Sun R, Heston JP. Management of zonular dialysis in phacoemulsification and IOL implantation using the capsular tension ring. Ophthalmic Surg Lasers. 1997;28:273–81. [PubMed] [Google Scholar]
- 5. Assia EI, Ton Y, Michaeli A. Capsule anchor to manage subluxated lenses:Initial clinical experience. J Cataract Refract Surg. 2009;35:1372–9. doi: 10.1016/j.jcrs.2009.02.046. [DOI] [PubMed] [Google Scholar]
- 6. Jacob S, Agarwal A, Agarwal A, Agarwal S, Patel N, Lal V. Efficacy of a capsular tension ring for phacoemulsification in eyes with zonular dialysis. J Cataract Refract Surg. 2003;29:315–21. doi: 10.1016/s0886-3350(02)01534-1. [DOI] [PubMed] [Google Scholar]
- 7. Asano Y, Yaguchi S, Nishimura E, Soda M, Kozawa T. Modified capsule expander implantation to reposition and fixate the capsular bag in eyes with subluxated cataractous lenses and phacodonesis:Intermediate-term results. J Cataract Refract Surg. 2015;41:598–606. doi: 10.1016/j.jcrs.2014.06.031. [DOI] [PubMed] [Google Scholar]
- 8. Mojzis P, Ziak P, Piñero DP. Management of subluxated cataract with capsule anchor implantation. JCRS Online Case Rep. 2015;3:63–7. [Google Scholar]
- 9. Ahmed II, Cionn RJ, Kranemann C, Crandall AS. Optimal timing of capsular tension ring implantation:Miyake-Apple video analysis. J Cataract Refract Surg. 2005;31:1809–13. doi: 10.1016/j.jcrs.2005.02.048. [DOI] [PubMed] [Google Scholar]
- 10. Buttanri IB, Sevim MS, Esen D, Acar BT, Serin D, Acar S. Modified capsular tension ring implantation in eyes with traumatic cataract and loss of zonular support. J Cataract Refract Surg. 2012;38:431–6. doi: 10.1016/j.jcrs.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 11. Ton Y, Naftali M, Lapid Gortzak R, Assia EI. Management of subluxated capsular bag-fixated intraocular lenses using a capsular anchor. J Cataract Refract Surg. 2016;42:653–8. doi: 10.1016/j.jcrs.2016.04.002. [DOI] [PubMed] [Google Scholar]


