Abstract
The tuck-and-pull technique was developed for practical and safe explantations of posterior chamber phakic intraocular lenses (PCPIOLs). In this technique, after the creation of a side port, viscoelastic (or OVD [ophthalmic viscosurgical device]) is initially injected behind the PCPIOL to widen the space between PCPIOL and the crystalline lens. The old incisions can be used after recent implantations rendering the enlargement of the main incision unnecessary. After additional OVD over and under the PCPIOL, the haptic is tucked by a chopper and pulled through the main incision with a single maneuver. The haptic is grasped by two suture forceps and explanted with a “hand-to-hand” maneuver. The tuck-and-pull technique provided high protection of the corneal endothelium, crystalline lens, anterior chamber structures, and the PCPIOL itself. This technique is a practical, easy, and safe approach for explantations of all PCPIOL types, whatever the reason for its explantation may be.
Keywords: Explantation, ICL, myopia, new technique, posterior chamber phakic IOL
Every posterior chamber phakic intraocular lens (PCPIOL) implantation will eventually require explantation due to complications, clear lens extraction, or cataract surgery.[1]
Misplacements (upside-down implantation or wrong PCPIOL) or intraoperative tears, usually during the early training period,[2,3] are followed by inadequate vault, PCPIOL rotation, cataract induction,[4] uncontrolled high intraocular pressure (IOP), and pigment dispersion.[5,6] In case of senile cataract development or of the need of clear lens extraction for presbyopia correction, PCPIOL explantation is needed beforehand.
An ideal PCPIOL explantation should accomplish (1) small incision that does not induce astigmatism or wound closure problems, (2) protection of the corneal endothelium, (3) preservation of the crystalline lens capsular integrity, (4) preservation of the PCPIOL integrity, and (5) protection of the anterior chamber (AC) structures. To achieve that, we developed a new tuck-and-pull technique. It is applicable to all types of PCPIOL, whatever the reason of its explantation may be.
Surgical Technique
Full mydriasis pre- or intraoperatively is necessary as it facilitates the rescue of the lens from posterior chamber and diminishes the touch and damage to the iris and the zonulae. The technique is as follows:
One side port is enough to explant PCPIOL [Fig. 1a]. Right-handed surgeons need a side port on the right side. If a PCPIOL reimplantation or cataract surgery is planned at the same session, two side ports are preferred.
Injection of OVD behind the PCPIOL is done to widen the space between PCPIOL and the crystalline lens, thus protecting it throughout the procedure [Fig. 1b]. If applied initially into AC, PCPIOL will move backward toward the crystalline lens, not allowing safe manipulation. If reimplantation is planned, cohesive OVD should be used because it can be washed easily. If crystalline lens extraction is planned, dispersive OVD is preferred to protect the corneal endothelium.
After separating PCPIOL from the natural lens, OVD is injected into the AC to protect all the AC structures [Fig. 1c].
Up to 1 year, the original main incision is used, as 2.8 mm is enough. It is easily found with a blunt LASIK (laser in situ keratomileusis) spatula or a Sinskey hook [Fig. 1d]. Enlargement up to 3.0 mm is suggested during the training period. Late postoperatively, a new main corneal incision should be created, avoiding the place of the first incision.
The nearest PCPIOL haptic is elevated with the additional injection of OVD under the PCPIOL [Fig. 1e].
Tucking of the PCPIOL haptic and pulling through the main incision are the most important steps [Fig. 1f]. The haptic is hooked and tucked using a chopper with a long blunted tip, pulled through the main incision, and held out [Fig. 1g].
The haptic that is held through the main incision by the chopper in one hand is grasped by a suture forceps (preferably curved) in the other hand [Fig. 1h]. Then, the haptic is taken out by two suture forceps in both hands successively with a “hand-to-hand” maneuver, keeping them parallel to the incision plane. The hand motion should be very slow in order not to tear the lens. This gives the lens time to slowly fold through the incision on the way out. If the reimplantation of the same PCPIOL is planned, the integrity of the PCPIOL must be checked. Video Clip 1 shows the tuck-and-pull technique in an explantation of ICL because of improper vault. Video Clip 2 shows the tuck-and-pull technique in an eye with ICL during femtosecond laser–assisted cataract surgery.
Figure 1.
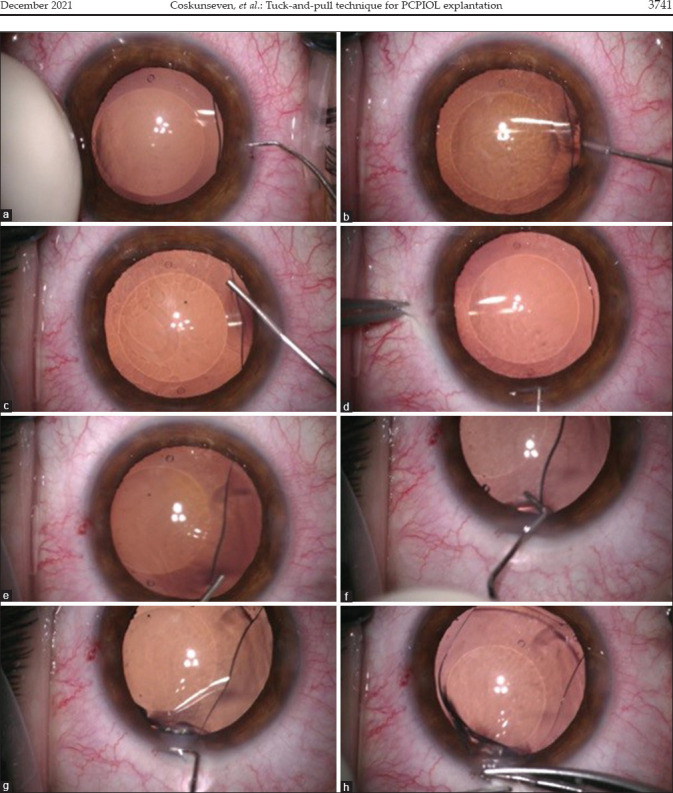
Tuck-and-pull technique. (a) Opening of the previous side port with a blunt tip of LASIK spatula. (b) Injection of OVD behind the PCPIOL. (c) Injection of OVD into the anterior chamber. (d)The original main incision is easily found with a blunt LASIK spatula or a Sinskey hook. (e) The nearest PCPIOL haptic is elevated with the additional injection of OVD under the PCPIOL. (f) The haptic is hooked and tucked with a blunted tip chopper. (g) The tucked haptic is pulled through the main incision. (h) The haptic is taken out by suture forceps with a “hand-to-hand” maneuver
Discussion
This technique enables PCPIOLs to be explanted through a small 2.8 mm incision. In any situation, be it exchange of the PCPIOL or a cataract surgery, inducing astigmatism should be avoided. Moreover, during cataract surgery, the small corneal incision is essential to prevent corneal wound leakage. Up to 1 year, we separated the old incision sites with a standard LASIK flap spatula and explanted all PCPIOLs through their original incisions. When the creation of a new main corneal incision and side ports was necessary, it was never done at the same site, as it can overlap with the old incision creating a possible irregularity. No enlargement of the incision site or stitch was necessary, and no corneal wound leakage was found.
The tuck-and-pull technique requires minimal manipulation, short time for PCPIOL explantation, and simple instrumentation. Bringing the PCPIOL haptic into the incision site is the most critical part of an explantation. In other studies, OVD is initially injected into AC, and then a special forceps inside the AC is used to grasp and pull PCPIOL haptic.[7,8,9,10] Differently, we used a standard blunt-tipped chopper to hook and pull the PCPIOL very quickly with minimal maneuvers. Having brought the haptic into the incision site, all techniques explant PCPIOL with a “hand-over-hand” technique. Bigger instruments than a simple, blunt-tipped chopper require more manipulation and thus the risk for corneal endothelium and crystalline lens damage is increased. Moreover, it may be more traumatic to the incision site.
Another difference is the injection of OVD under the PCPIOL before applying it into the AC. This moves the PCPIOL away from the crystalline lens, thus enabling safe maneuvers by creating more space between the PCPIOL and the crystalline lens. It also facilitates the safe tucking and pulling of the PCPIOL by the chopper.
When PCPIOL explantation is performed because of an upside-down placement, torn PCPIOL, or an inappropriate vault level, any touch to the crystalline lens can induce clinically significant opacity requiring a cataract surgery later on. If PCPIOL explantation is planned together with a cataract surgery or pars plana vitrectomy, any contact to the anterior capsule can cause tears in the capsule leading to undesirable surprises during the cataract surgery.
The tuck-and-pull technique ensures the explantation of any PCPIOL without additional damage to its body or its haptic, enabling immediate reuse in cases of lens misplacements such as upside-down implantation.
This technique is respectful to other parts of the eye such as the trabecular meshwork, the iris, and the pupil. No hyphemia, pupil irregularity, or permanent rise in IOP in any eyes was observed.
Conclusion
We have described a novel technique for PCPIOL explantation of all types and in all situations. It is simple, safe, and efficient; protects all the intraocular structures; is easily applicable with a short learning curve; and needs simple instrumentation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos Available on: www.ijo.in
References
- 1. Packer M. Meta-analysis and review: Effectiveness, safety, and central port design of the intraocular collamer lens. Clin. Ophthalmol. 2016;10:1059–77. doi: 10.2147/OPTH.S111620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sanders DR, Vukich JA, Doney K, Gaston M. Implantable Contact Lens in Treatment of Myopia Study Group. U. S. Food and Drug Administration clinical trial of the Implantable Contact Lens for moderate to high myopia. Ophthalmology. 2003;110:255–66. doi: 10.1016/s0161-6420(02)01771-2. [DOI] [PubMed] [Google Scholar]
- 3. Sanders DR, Doney K, Poco M. ICL in Treatment of Myopia Study Group. United States Food and Drug Administration clinical trial of the Implantable Collamer Lens (ICL) for moderate to high myopia: Three-year follow-up. Ophthalmology. 2004;111:1683–92. doi: 10.1016/j.ophtha.2004.03.026. [DOI] [PubMed] [Google Scholar]
- 4. Alfonso JF, Lisa C, Fernández-Vega L, Almanzar D, Pérez-Vives C, Montés-Micó R. Prevalence of cataract after collagen copolymer phakic intraocular lens implantation for myopia, hyperopia, and astigmatism. J Cataract Refract Surg. 2015;41:800–5. doi: 10.1016/j.jcrs.2014.07.039. [DOI] [PubMed] [Google Scholar]
- 5. Khalifa YM, Goldsmith J, Moshirfar M. Bilateral explantation of Visian implantable collamer lenses secondary to bilateral acute angle closure resulting from a non-pupillary block mechanism. JRefract Surg. 2010;26:991–4. doi: 10.3928/1081597X-20100521-01. [DOI] [PubMed] [Google Scholar]
- 6. Ye C, Patel CK, Momont AC, Liu Y. Advanced pigment dispersion glaucoma secondary to phakic intraocular collamer lens implant. Am J Ophthalmol Case Rep. 2018;10:65–7. doi: 10.1016/j.ajoc.2018.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zeng Q, Xie X, Chen Q. Prevention and management of collagen copolymer phakic intraocular lens exchange: Causes and surgical techniques. JCataract Refract Surg. 2015;41:576–84. doi: 10.1016/j.jcrs.2014.06.036. [DOI] [PubMed] [Google Scholar]
- 8. Kamiya K, Shimizu K, Igarashi A, Aizawa D, Ikeda T. Clinical outcomes and patient satisfaction after Visian implantable collamer lens removal and phacoemulsification with intraocular lens implantation in eyes with induced cataract. Eye (Lond) 2010;24:304–9. doi: 10.1038/eye.2009.87. [DOI] [PubMed] [Google Scholar]
- 9. AlSabaani NA, Behrens A, Jastanieah S, Al Malki S, Al Jindan M, Al Motowa S. Causes of phakic implantable collamer lens explantation/exchange at King Khaled Eye Specialist Hospital. Middle East Afr J Ophthalmol. 2016;23:293–5. doi: 10.4103/0974-9233.194076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hayakawa H, Kamiya K, Ando W, Takahashi M, Shoji N. Etiology and outcomes of current posterior chamber phakic intraocular lens extraction. Sci Rep. 2020;10:21686. doi: 10.1038/s41598-020-78661-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


