Abstract
Background
Mental disorders are associated with immune dysregulation as measured by serum levels of biological markers of immunity. Adults with mental disorders have also been reported to have attenuated post vaccine immune response. The COVID-19 pandemic has invited the need to determine whether individuals with mental disorders exhibit differential immune response following the administration of vaccines for other infections.
Methods
A systematic search of MEDLINE, Embase, Cochrane, and PsycInfo was conducted from inception to May 2021 investigating vaccine response in persons with mental disorders, as measured by biological markers of immunity (i.e., antibodies, cytokines).
Results
Thirteen articles were identified which evaluated vaccine efficacy in persons with mental disorders. Individuals with major depressive disorder (MDD) or schizophrenia revealed attenuated immune response to vaccination, or no statistical difference compared to control subjects. Individuals with anorexia nervosa or post-traumatic stress disorder (PTSD) displayed no attenuated post-vaccination antibody level. Individuals with insomnia displayed lower levels of antibodies after vaccination, whereas individuals with obstructive sleep apnea (OSA) displayed no difference in vaccine response compared to control subjects.
Limitations
The limitations of this review include the relatively few articles included (n = 13) and small sample sizes (less than thirty subjects) in the majority of articles.
Conclusion
Vaccine response in adults with a mental disorder remains inconclusive. Notwithstanding the heterogeneity and relatively small number of studies, available evidence does suggest attenuated immune response across disparate vaccinations. Future research is required to confirm vaccine efficacy in persons with mental disorders, especially regarding immune responses to COVID-19 vaccination.
Keywords: Mental illness, Vaccination, Immune function, COVID-19, Depression, Mood, Disorders, Inflammation, Public Health
1. Introduction
Approximately 10.7% of individuals worldwide are affected by a mental disorder (Ritchie and Roser, 2018). Psychological, social, and biological factors contribute to the incidence and prevalence of common mental disorders (National Collaborating Centre for Mental Health, 2011). Replicated evidence suggests an attenuation of vaccine response among individuals with symptoms of mental disorders. For example, individuals with depressive symptoms have been reported to exhibit an attenuated post vaccine immune response (Gidron et al., 2005; Lasserre et al., 2012; Petry et al., 1991; Costanzo et al., 2004). Studies have also reported attenuated immune response to vaccines in subjects with higher stress levels (Marsland et al., 2001; Wong et al., 2013; Snyder et al., 1990; Burns et al., 2003; Smith et al., 2004) and poor quality or duration of sleep (Miller et al., 2004; Prather et al., 2012; Lange et al., 2003; Spiegel et al., 2002), which are both symptoms of common mental disorders. It is also well documented that individuals with mental disorders exhibit immune dysregulation as measured by natural killer cell activity, lymphocyte response to mitogen stimulation, and increased risk of infection (Kronfol, 2002; Andersson et al., 2016). However, these findings are not fully supported as contradictory evidence suggests that there is no association between depressive mood and immune response following vaccination (Moynihan et al., 2004).
Given the association between the COVID-19 pandemic and increased symptoms of mental disorders (i.e., psychological stress), and the vaccination campaigns occurring around the world, it is especially important to consider the efficacy of vaccines in individuals with mental disorders (Madison et al., 2021). Taken together, there is a need to determine whether individuals with a mental disorder mount a sufficient immune response to vaccines. If persons with mental disorders are incapable of mounting an adequate response to COVID-19 vaccines, this could pose a significant global health issue.
A majority of existing literature focuses on symptoms of mental disorders and vaccine response, or mental disorders and serum analysis without vaccination. To our knowledge, there has not been a previous review evaluating immune response from vaccination among individuals with a mental disorder. Herein, the aim of this systematic review is to synthesize the extant literature of vaccine response in persons with a mental disorder as measured by biological markers of immunity.
2. Methods
This systematic review was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., 2009). The protocol for this review is registered with PROSPERO (registration number CRD42021262619).
2.1. Search strategy
A systematic database search of MEDLINE, Embase, Cochrane, and PsycInfo for studies of mental disorders and vaccine efficacy was conducted from database inception to May 2021. The following search terms were used to yield relevant references: mental illness, mental disorder, psychiatric disorder, mood disorder, personality disorder, depression, anxiety, schizophrenia, vaccine, antibody, T cell, immune response.
Two independent reviewers (K.X. and E.S.G.) screened the titles and abstracts of all initial search results. The full texts of select articles were then screened to identify the articles included in this review. Disagreements were resolved by external reviewers (L.M.W.L. and R.S.M.). Additional articles were identified through the reference lists of relevant articles.
The results of all included articles underwent qualitative analysis via narrative synthesis. Due to the prominent sources of heterogeneity between studies arising from the wide range of mental disorders, vaccines administered, outcome measured, and study design, no quantitative analyses were undertaken.
2.2. Study selection criteria
Inclusion criteria were as follows:
-
(1)
Participants were adults (18–65 years) clinically diagnosed with a mental disorder listed in the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM–5; American Psychiatric Association, 2013).
-
(2)
Participants were administered the same vaccine, or a vaccine against the same virus, as all other participants in the study.
-
(3)
Primary or secondary outcome was quantitative measures of biological markers of immunity (e.g. antibodies, T lymphocytes, cytokines).
-
(4)
Full text available in English.
The exclusion criteria was as follows:
-
(1)
Case studies, conference abstracts, reviews and meta-analyses of the literature, and studies based solely on qualitative assessment or self-reported responses to questionnaires.
-
(2)
Studies limited to children and adolescents (<18 years) and elderly subjects (>65 years).
-
(3)
Studies limited to subjects with autoimmune disorders or other critical physical illnesses.
2.3. Data extraction
K.X. extracted data using a data extraction spreadsheet, and E.S.G. reviewed the extracted data. The following information was extracted: author and year of publication, mental disorder, sample size, demographics of subjects with mental disorders and control subjects, vaccine administered, time of measurements, biomarkers measured, and relevant findings.
2.4. Bias assessment
To assess methodological quality and risk of bias for all full-text articles included, all randomized control trials were assessed using Cochrane's Risk of Bias 2 (RoB 2) tool (Sterne et al., 2019), and all non-randomized studies were assessed using Cochrane's Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) tool (Sterne et al., 2016).
The five domains of bias addressed in the RoB 2 assessment tool relate to the randomization process, deviations from intended interventions, missing outcome data, outcome measurement, and selection of reported results (Sterne et al., 2019). Studies were ranked as having a low, moderate, or high risk of bias.
The seven domains of bias addressed in the ROBINS-I assessment tool are biases that arise from confounding variables, participant selection, classification of interventions, deviations from intended intervention, missing data, outcome measurement, and selection of the reported results (Sterne et al., 2016). The ROBINS-I tool was used to determine if a study's overall risk of bias was low, moderate, serious, or critical.
3. Results
3.1. Search results
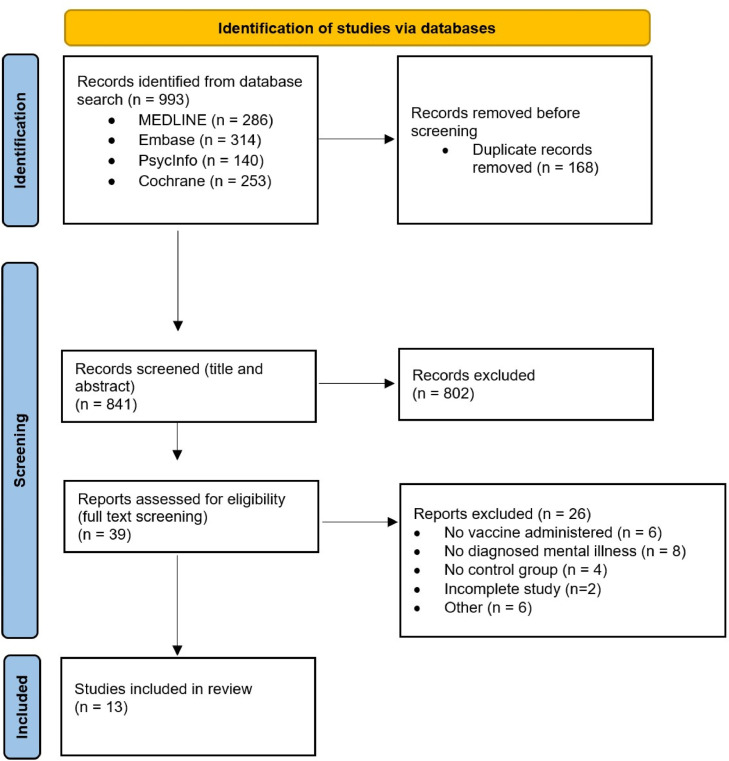
A total of 993 articles were identified from the database searches. After removing duplicates and screening the titles and abstracts, 39 articles were eligible for full-text screening. The full-text screening yielded 13 relevant articles that were eligible for analysis. The PRISMA flow diagram is presented in Fig. 1 . The articles eligible for analysis reported on the following mental disorders: major depressive disorder (MDD) (n = 3), schizophrenia (n = 5), anorexia nervosa (AN) (n = 2), insomnia (n = 1), obstructive sleep apnea (OSA) (n = 1), and post-traumatic stress disorder (PTSD) (n = 1). Study characteristics are summarized in Table 1 .
Fig. 1.
PRISMA flow diagram for study identification and selection.
Table 1.
Summary of study design and results.
| Author and Date | Mental illness | Sample size | Vaccine | Time of measurements | Relevant biomarker | Findings |
|---|---|---|---|---|---|---|
| Ford et al. (2019) | MDD: current/cMDD and remitted/rMDD Bipolar Disorder: BD Type I and II, and NOS (Not otherwise specified) Criteria: DSM-IV-TR |
cMDD (n = 85) rMDD (n = 82) BD (n = 64) Controls (n = 202) |
Measles vaccine (specifics varied and were not disclosed). | Unknown; years after childhood vaccination | Antibodies | cMDD and rMDD were less likely to test seropositive for measles (p = 0.015, adj OR = 0.53, 95% CI: 0.74–2.37). BD: did not differ from HC (p = 0.329) or cMDD (0.355) or rMDD (0.449) |
|
Cassiers et al. (2019) |
Remitted MDD (rMDD), including Moderate-to-severe recurrent MDD without psychotic features Criteria: DSM-IV-TR Most recent depressive episode was within 24 months, but stable for the past 3 months |
rMDD (n = 21) Controls (n = 18) |
Typhoid vaccine (0.5 mL containing 23 ug Salmonella typhi capsular polysaccharide; Typhim Vi; Sanofi Pasteur MSD, Diegem, Belgium) Placebo: 0.5 mL NaCl, 0.9% |
Baseline and 30, 60, 90, 150, 180, 240, 360 min post-vaccine | Proinflammatory cytokines: interferon (IFN)-y, tumor necrosis factor (TNF)-a, and interleukin (IL)−6 | Trauma was associated w lower TNF-a after vaccination for rMDD but not HC (suggests a "trauma-associated MDD endophenotype"). Found no effects of trauma on IL-6 and IFN-y in rMDD or HC after statistical correction. |
| Niemegeers et al. (2016) | Moderate-to-severe recurrent MDD without psychotic features, currently in (partial) remission Criteria: DSM-IV-TR |
MDD (n = 21) Controls (n = 18) |
Typhoid vaccine (0.5 mL containing 25 μg S. t yphi capsular polysaccharide; Typhim ® Vi; Sanofi Pasteur MSD, Diegem, Belgium). Placebo: 0.5 mL NaCl, 0.9% |
Baseline and after vax, then 30, 60, 90, 150, 180, 240, 360 min post-vaccine | Proinflammatory cytokines: interferon (IFN)-y, tumor necrosis factor (TNF)-a, and interleukin (IL)−6 | No significant difference in increased inflammatory measures from vaccine alone; some changes were measured only if patients underwent vaccine and psychosocial stressor. IFN-y only increased in patients after TSST (psychosocial stress) and vaccine together, but not after any individual intervention. TNF-a and IL-6 were not different between HC and MDD. |
| Hussar et al. (1971) | Schizophrenia (SCZ) SCZ types: 11 paranoid, 7 hebephrenic, 2 catatonic, 1 undifferentiated Criteria: American Psychiatric Association Diagnostic Manual |
SCZ (n = 21) Controls (n = 16) |
First injection: 0.5 cc. of concentrated diphtheria toxoid Second injection: 0.5 cc. diphtheria toxoid (30 days after 1st injection) |
Prior to injections, and at 10th, 20th, 35th, 45th, and 60th day after 1st injection | Antibodies | No statistical difference between SCZ and controls (t-test: p > 0.05). |
|
Friedman et al. (1967) |
Schizophrenia (SCZ) and Depression* (DEP) *whether all depressed subjects had a diagnosis of depression is unclear. |
SCZ (n = 10) DEP (n = 22) Controls (n = 7) |
0.5 cc of cholera vaccine (India strains) | Day 1 (day of injection), 4, 6, 8, 10 Note: Some subjects were also measured on day 12 and 15, if possible. |
Antibodies | No significant difference before day 8. SCZ had higher titers than controls on day 8, 10, 15 (and higher than DEP on day 8, 10, 12). No significant differences between controls and DEP. Antibody levels were highest in SCZ but lowest in DEP. |
| Solomon et al. (1968) | Schizophrenia (SCZ) Non-SCZ psychiatric disorders (neurotic, affective, character, or substance-related disorders) |
SCZ (n = 13) non-SCZ psychiatric patients (n = 13) Controls (n = 6) |
Booster dose of tetanus toxoid (0.5 ml of aluminum hydroxide adsorbed toxoid) | Baseline, 2, 4, 7, 14 days after vaccine | Antibodies (antitoxins) | SCZ and HC were nearly identical before and after vaccination. Non-SCZ psychiatric patients had somewhat lower measurements but not statistically significant. |
| Wang et al. (2016) | Schizophrenia (SCZ) Criteria: DSM-IV-TR |
SCZ (n = 415) Controls (n = 3038) |
Hepatitis-B vaccine (unknown specifics but vaccination records were requested from all subjects). | Unknown; years after childhood vaccination | Hep B surface antigens (HBsAg), Hep B surface antibodies (HBsAb) | HBsAg showed significant differences between groups, but HBsAb had no significant differences. SCZ were more at risk for HBV infection even after vaccination. |
| Vaughan et al. (1949) | Schizophrenia (SCZ) Subtypes of Dementia Praecox: paranoid (5), catatonic (4), hebephrenic (6), simple (2), other (5) |
SCZ (n = 22) Controls (n = 17) |
Plain Pertussis Vaccine (4 weeks of injections) 1 cc for week 1, 2 cc for weeks 2–4. (Total: 7 cc of vaccine.) |
Weekly for 8 weeks | Antibodies | SCZ had significantly lower antibody response than controls. |
| Armstrong-Esther et al. (1978) | Anorexia nervosa (AN) Types: vomiting, and carbohydrate-abstaining |
AN (n = 15) Controls (n = 15) |
0.5 ml of Admune influenza vaccine; contains: A/England/42/72, 400 i.u., A/Port Chalmers/1/73, 400 i.u., and A/Hong Kong/1/68, 360 i.u. Also administered 0.1 ml tuberculin purified derivative (PPD) of Mycobacterium tuberculosis. |
Baseline, 10th and 28th day after vaccine. Final test on day 50 (measure haemag antibody titre and CIR to tuberculin) On day 48, tested for tuberculin; 48 h later, examine injury site to measure/record reactive zone |
Antibodies and cell-mediated immunity (CMI) against tuberculin | 8 patients (53%) and 10 controls (6%) were positive for tuberculin. Control titres were higher than AN by day 10, but AN titres were higher than controls on day 28 and 50 in all 3 strains, with 1 of the 3 strains being statistically significant. |
| Zastrow et al. (2012) | Anorexia nervosa (AN) Subtypes: 2 F with purging subtype (ANp); the other 8 had restrictive subtype (ANr) |
AN (n = 10) | Adjuvanted Influenza A virus H1N1 subtype (Pandemrix, GlaxoSmithKline, Rixensart, Belgium). Contains 375 lg of hemagglutinin antigen derived from influenza virus A(H1N1) California/7/2009. |
Baseline, 2 weeks and 3 weeks post-vaccine | Antibodies | AN's H1N1 vaccine was sufficiently immunogenic and safe. The seroconversion and seroprotection rates were comparable with the healthy rates of 100%. |
| Taylor et al. (2017) | Insomnia Types: 67.7% sleep onset insomnia, 24.6% maintenance insomnia, and 20% terminal insomnia (>=3 nights/week) Criteria: DSM-IV and DSM-5 |
Insomnia (n = 65) Controls (n = 68) |
Influenza Novartis Fluvirin preparation of the influenza vaccine; 2011–2012 contained A/California/7/2009 (H1N1), A/Perth/16/2009 (H3N2), and B/Brisbane/60/2009 virus 2012–2013 contained: A/California/7/09 (H1N1), A/Victoria/361/2011 (H3N2), and B/Wisconsin/1/2010 |
Baseline and 4 weeks after vaccine | Antibodies | Lower overall HI antibody count in insomnia both at baseline and at 4 weeks post-vaccine. Statistically significant difference was found for H3N2 strain in both years, and for B strain in 2012–2013. |
| Dopp et al. (2007) | Moderate-to-severe Obstructive Sleep Apnea (OSA); untreated | OSA (n = 14) Controls (n = 17) |
Influenza 2004–2005 or 2005–2006 vaccine | Baseline and 2–4 weeks after vaccine. | Antibodies | No significant differences were observed in changes in antibody concentration, frequencies of seroconversion, or rates of seroprotection between subjects with OSA and control subjects. |
| Kosor Krnic et al. (2007) | Combat-related chronic PTSD | PTSD (n = 28) Controls (n = 15) |
Agrippal (Chiron, Italy) influenza vaccine Contains: influenza A (A/New Caledonia/H1N1-like, A/Moscow/H3N2-like), and B (B/Hong Kong/-like, B/Shangdong-like) purified antigens |
Baseline and 14 days after | Antibodies | Mean fold increase in titers did not differ significantly between groups. HC had lower seroconversion rate to A/Moscow/H3N2. Seroconversion and seroprotection rates were similar for all strains in both groups. |
3.2. Risk of bias assessments
The risk of bias assessments are displayed in Table 2 . All five studies on schizophrenia had a moderate risk of bias due to a lack of controlling for confounding factors (Hussar et al., 1971; Solomon et al., 1968; Friedman et al., 1967; Vaughan et al., 1949; Wang et al., 2016), and all three studies on MDD/rMDD had a low risk of bias (Ford et al., 2019; Niemegeers et al., 2016; Casseirs et al., 2019). Both the study on insomnia (Taylor et al., 2017) and OSA (Dopp et al., 2007) had low risks of bias, as did the study on PTSD (Kosor Krnic et al., 2007) and the anorexia study by Armstrong-Esther et al. (1978). A separate study reporting on anorexia, by Zatrow et al. (2012), had a serious risk of bias due to the lack of control group, lack of consideration for confounding variables, and the sample size of only 10 participants. Overall, seven studies were deemed low, five studies were deemed moderate, and one study was deemed serious regarding the risk of bias.
Table 2.
Risk of Bias Assessments using the RoB 2 tool or the ROBINS-I tool.
| Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Study Name | Domain 1: Risk of bias due to confounding | Domain 2: Risk of bias in selection of participants into the study | Domain 3: Risk of bias in classification of interventions | Domain 4: Risk of bias due to deviations from intended interventions | Domain 5: Risk of bias due to missing data | Domain 6: Risk of bias in measurement of outcomes | Domain 7: Risk of bias in selection of the reported result | Overall risk of bias |
| Ford et al. (2019) | Low | N/A | N/A | N/A | Low | Low | Low | Low |
| Hussar et al. (1971) | Serious | Low | Low | Low | Low | Low | Low | Serious |
| Friedman et al. (1967) | Moderate | Low | Low | Low | Low | Low | Low | Moderate |
| (Solomon et al., 1968) | Moderate | Low | Low | Low | Low | Low | Low | Moderate |
| Wang et al. (2016) | Moderate | N/A | N/A | N/A | Low | Low | Low | Moderate |
| Vaughan et al. (1949) | Moderate | Low | Low | Low | Low | Low | Low | Moderate |
| Armstrong-Esther et al. (1978) | Low | Low | Low | Low | Low | Low | Low | Low |
| Taylor et al. (2017) | Low | Low | Low | Low | Moderate | Low | Low | Low |
| Dopp et al. (2007) | Moderate | Low | Low | Low | Low | Low | Low | Low |
| Kosor Krnic et al. (2007) | Moderate | Low | Low | Low | Low | Low | Low | Low |
| Risk of Bias 2 (RoB 2) | ||||||||
| Domain 1: Risk of bias arising from the randomization process | Domain 2: Risk of bias due to deviations from the intended intervention (effect of assignment to intervention) | Domain 3: Risk of bias due to missing outcome data | Domain 4: Risk of bias in measurement of the outcome | Domain 5: Risk of bias in selection of the reported result | Overall risk of bias | |||
| Cassiers et al. (2019) | Low | Low | Low | Low | Low | Low | ||
| Niemegeers et al. (2016) | Low | Low | Low | Low | Low | Low | ||
Note: N/A refers to domains that were not applicable for that study.
3.3. Study results
3.3.1. Major depressive disorder
Three studies reported on adults with MDD or remitted MDD and immune response to vaccination (Ford et al., 2019; Niemegeers et al., 2016; Casseirs et al., 2019). Ford et al. (2019) measured serum levels of IgG antibodies against measles in subjects with current mild, moderate, or severe MDD (cMDD; n = 85), and subjects with MDD in full or partial remission (rMDD; n = 82). This study also included a separate group of subjects with bipolar disorder (BD) (n = 64). The three groups were compared to a healthy control group (n = 202). Subjects had received measles vaccines during their childhood. Relative to controls, both the group with current major depressive disorder (cMDD) (p = 0.021, adjusted OR = 0.47, CI = 0.24–0.90) and the group with remitted major depressive disorder (rMDD) (p = 0.038, adjusted OR = 0.50, CI = 0.26–0.97) were less likely to test seropositive for measles. Seropositivity for individuals with BD did not differ from the control (p = 0.329), the cMDD (p = 0.355), or the rMDD (p = 0.449) groups. Since attenuated seropositivity was present in both rMDD and cMDD groups, the weakened immune response was not limited to the symptomatic phase of MDD (Ford et al., 2019).
The two remaining studies reported on women with remitted major depressive disorder (rMDD) (Montgomery–Åsberg depression rating scale score < 15) (Niemegeers et al., 2016; Casseirs et al., 2019). Both Niemegeers et al. (2016) and Cassiers et al. (2019) used the same population of women with rMDD (n = 21) and healthy controls (n = 18). Niemegeers et al. (2016) aimed to investigate the effects of inflammatory stress, psychosocial stress, or a combination of both factors on mood in women with rMDD. Cassiers et al. (2019) aimed to investigate the effects of childhood trauma on their responses to psychosocial and inflammatory stress. In both studies, the Typhoid vaccine was administered as an inflammatory stressor in participants. Both studies measured proinflammatory cytokines (interferon (IFN)-γ, tumor necrosis factor (TNF)-ɑ, and interleukin (IL)-6) in response to intervention (i.e., vaccination, TSST, or both). Niemegeers et al. (2016) reported no significant differences in the cytokine (INF-y, IL-6, TNF-ɑ) responses between rMDD and healthy subjects after vaccination alone. Cassiers et al. (2019) conducted a study using similar methodology, except the rMDD and control subjects were divided into “traumatized” or “non-traumatized” groups based on self-reported responses to the Childhood Trauma Questionnaire (CTQ). In this study, trauma was associated with a statistically significant decrease in TNF-ɑ after vaccination for subjects with rMDD (Tukey's t = 3.25, p = 0.0286; 99% CI (0.0068 to 0.2237)), but not for healthy control subjects. Cassiers et al. (2019) thus suggested the existence of a trauma-associated MDD endophenotype with a weakened TNF-ɑ response to vaccination.
3.3.2. Schizophrenic disorders
Five studies evaluated the response to vaccination in subjects with schizophrenia, with inconsistent results (Hussar et al., 1971; Solomon et al., 1968; Friedman et al., 1967; Vaughan et al., 1949; Wang et al., 2016). Hussar et al. (1971) compared male patients with schizophrenia (n = 21) to a control group of male hospital employees (n = 16). The types of schizophrenia included paranoid (n = 11), hebephrenic (n = 7), catatonic (n = 2), and undifferentiated (n = 1). All subjects received an injection of 0.5 cc. of concentrated diphtheria toxoid, followed by a second injection of 0.5 cc. diphtheria toxoid 30 days later. There was no significant difference (p > 0.05) between the patients with schizophrenia and healthy subjects in their ability to form antibodies following vaccination. Similarly, Solomon et al. (1968) administered a booster dose of the tetanus toxoid vaccine in patients with schizophrenia (n = 13) and healthy controls (n = 6), as well as compared titres for participants with schizophrenia with literature values of antibody response in Navy personnel. The antitoxin titres for both the subjects with schizophrenia and healthy subjects were nearly identical; the difference did not reach the 0.1 level of significance, and the titres for participants with schizophrenia were also comparable to the antibody response in Navy personnel (n = 25).
Further, Friedman et al. (1967) compared antibody responses to 0.5 cc. of cholera vaccination in patients with schizophrenia (n = 10), patients with depression (n = 22), and a healthy control group (n = 7) of medical students. Compared to the control group, patients with schizophrenia had significantly higher antibody titres starting eight days after vaccination. The authors reported lower titres in the depressed group of patients; however, the difference was not statistically significant nor did the authors report that the participants received a clinical diagnosis of MDD or another depressive disorder.
However, the foregoing results are not in accordance with the outcomes reported by Vaughan et al. (1949), who found that patients with schizophrenia (n = 22) had a weaker immune response than control subjects (n = 17) following weekly Plain Pertussis vaccinations. The logarithmic mean of the reciprocal maximum serum titres was 2.2071 (s.d. ± 0.4030) in subjects with schizophrenia, and 2.5582 (s.d ± 0.3862) in the healthy control group. This difference was statistically significant (p = 0.008), suggesting that patients with schizophrenia have a weaker response to antigenic stimulation compared to control subjects.
Furthermore, Wang et al. (2016) conducted a study of hospitalized adult patients with schizophrenia (n = 415) compared to a control group (n = 3038). All subjects had received a childhood vaccination against hepatitis B virus (HBV). There was a significant difference between the two groups for seroprevalence of hepatitis B antigens (p < 0.001), although there was no statistical difference in the rate of hepatitis B antibody production between groups. It was concluded that patients with schizophrenia may be at greater risk for HBV than healthy controls even after vaccination. Given the studies which suggest that patients with schizophrenia acquire post vaccine immunity comparable to healthy controls (Hussar et al., 1971; Solomon et al., 1968; Friedman et al., 1967), and the studies that suggest an attenuated response to vaccination in persons with schizophrenia (Vaughan et al., 1949; Wang et al., 2016), the overall results remain inconclusive.
3.3.3. Eating disorders
Two studies reported on the relationship between anorexia nervosa (AN) and antibody response to vaccination, both of which yielded no statistical significance when compared to the vaccine response of a normal weight population (Armstrong-Esther et al., 1978; Zastrow et al., 2012). Armstrong-Esther et al. (1978), administered the Admune influenza vaccine to female patients with AN (n = 15) and a healthy female control group (n = 15). The influenza vaccine contained three strains: A/England/42/72, A/Port Chalmers/1/73, and A/Hong Kong/1/68. Baseline measurements were not different between the group with AN and the control group. Although healthy controls had higher titres against the A/Port Chalmers/1/73 strain than subjects with AN up to the 10th day after vaccination (t = 2.344; p < 0.05), the quantitatively measured immune response as proxy by antibody titres for all three strains was greater in subjects with AN compared to healthy control subjects when measured on the 28th and 50th day after vaccination. Specifically, the increase in antibodies against the A/Hong Kong/1/68 strain for subjects with AN compared to controls was statistically significant (day 28: t = 2.2098 and p < 0.05; day 50: t = 2.7491 and p < 0.05).
A pilot study also assessed patients with AN (n = 10) and their antibody response to vaccination with adjuvanted influenza A virus H1N1 subtype (Zastrow et al., 2012). Compared with standardized values of a normal-weight population after controlling for body mass index and duration of illness, subjects with AN had seroprotection and seroconversion rates of 100%. The authors suggest that patients with AN mount a sufficient and safe response to H1N1 vaccination.
3.3.4. Sleep disorders
Two studies investigated vaccine response of individuals with sleep disorders (Taylor et al., 2017; Dopp et al., 2007). Taylor et al. (2017) studied young adult students diagnosed with chronic insomnia (n = 65), compared to healthy, age and sex-matched controls (n = 68). This study took place over two years, with half the participants (i.e., ninsomnia = 31 subjects, ncontrols = 28) vaccinated against influenza in 2011 and the other half (i.e., ninsomnia = 34, ncontrols = 40) in 2012. Patients with insomnia had lower overall counts of antibodies against influenza at baseline and 4 weeks post-vaccine, and a statistically significant between-groups main effect was found for the H3N2 strain in both 2011 and 2012 (p = 0.041 and p = 0.008, respectively). A statistically significant between-groups main effects were also found for the B strain, but only in 2012–2013 (p = 0.009). Although the study found no Group x Time interactions, subjects with insomnia had lower overall HI antibody levels (p = 0.002) than controls when averaging pre- and post vaccination responses.
However, these results differ from that of Dopp et al. (2007), who assessed immune response to the influenza vaccine in subjects with obstructive sleep apnea (OSA). This study compared post-vaccination influenza antibody titers in subjects with OSA (n = 14) and a control group (n = 17) . No significant differences (p > 0.05) were observed in the changes in antibody concentration, frequencies of seroconversion, or rates of seroprotection between subjects with OSA and control subjects. Neither the severity of sleep apnea nor the measures of sleepiness or sleep disruption were correlated with immune responses.
3.3.5. Stress and trauma disorders
One study investigated influenza vaccine response in subjects with PTSD (Kosor Krnic et al., 2007). Subjects diagnosed with combat-related chronic PTSD according to DSM-IV criteria (n = 28) and healthy controls (n = 15) were vaccinated with the Agrippal influenza vaccine. There was no mean fold increase in titres between subjects with PTSD and control subjects, and the seroprotection rates were similar between groups. The researchers also measured CD8+ T lymphocytes for the A/New Caledonia/H1N1 strain. Although the magnitude of change in the number of CD8+ T cells for subjects with PTSD was less than that of control subjects, there was no significant difference in the number of HA-541,549-specific CD8+ T cells between the two groups.
4. Discussion
In this systematic review, we identified thirteen studies assessing vaccine response in subjects with a mental disorder (Ford et al., 2019; Niemegeers et al., 2016; Casseirs et al., 2019; Hussar et al., 1971; Solomon et al., 1968; Friedman et al., 1967; Vaughan et al., 1949; Wang et al., 2016; Armstrong-Esther et al., 1978; Zastrow et al., 2012; Taylor et al., 2017; Dopp et al., 2007; Kosor Krnic et al., 2007). Results from the included studies were mixed; five studies suggested an attenuated vaccine response in individuals with MDD (n = 2) (Ford et al., 2019; Casseirs et al., 2019), schizophrenia (n = 2) (Vaughan et al., 1949; Wang et al., 2016), and insomnia (n = 1) (Taylor et al., 2017), whereas the remaining eight studies did not report differential immune response to vaccination in individuals with MDD (n = 1) (Niemegeers et al., 2016), schizophrenia (n = 3) (Hussar et al., 1971; Solomon et al., 1968; Friedman et al., 1967), obstructive sleep apnea (n = 1) (Dopp et al., 2007), anorexia nervosa (n = 2) (Armstrong-Esther et al., 1978; Zastrow et al., 2012), or PTSD (n = 1) (Kosor Krnic et al., 2007).
4.1. Mood disorders
Studies have supported the use of TNF-ɑ as an indicator of vaccine efficacy, with studies reporting a positive correlation between IgG antibody levels and both TNF-ɑ and IL-6 (Frasca et al., 2013). However, Cassiers et al. (2019) only found an attenuation in TNF-ɑ but not IL-6 levels. Thus, the results from Cassiers et al. (2019) only partially support findings that psychological well-being is correlated with cellular immunity as measured by post-vaccine cytokine production (Phillips et al., 2005b).
The foregoing association has been reported in a limited number of articles. The focus of this review was on adults (18–65 years) affected by a mental disorder. We excluded individuals older than 65 years due to the paucity of evidence which suggests that elderly subjects with major or minor depression have an attenuated antibody response to vaccination relative to age and sex-matched controls (Irwin et al., 2013; Trzonkowski et al., 2004), and the confounding effect of age on immune response to vaccination (Goodwin et al., 2006). Children with MDD were also excluded, on the basis that they are reportedly less likely to verbalize their emotions or meet DSM-5 MDD criteria (Mullen, 2018). Given that only one of the three identified mood disorder articles in this review measured biomarkers as the primary outcome, there is a need to conduct additional research with vaccine response as the primary outcome in adults with MDD between 18 and 65 years of age. There is also a need to investigate the effects of immune response to vaccines in individuals with other mood disorders (e.g., bipolar disorder) (McIntyre et al., 2020).
The altered immune function outside of vaccination contexts provides support for the notion that individuals with MDD suffer weakened immune responses to vaccination. Moreover, it has been reported that individuals with MDD have attenuated varicella-zoster virus immunity measured by a significantly lower VZV-specific responder cell frequency than subjects without depression (Irwin et al., 1998). A separate review indicated that chronic depression is associated with attenuated immune function in subjects with HIV/AIDS (Leserman, 2008), and depressive symptoms in women with breast cancer have been associated with suppressed cell-mediated immunity (Sephton, 2009).
A separate line of evidence suggests that depression is associated with immunological dysregulation regarding the quantity and function of immune cells, including lymphocyte function impairment and attenuated natural killer cell activity (Kronfol, 2002). Findings from an observational study suggest that individuals with depression conferred an increased risk of developing infection, such as sepsis, urogenital, respiratory, and bacterial infections, among others (Andersson et al., 2016). Persons with pre-existing mood disorders are also at a higher risk of hospitalization and death from COVID-19, which may be partly attributable to dysregulated immunity (Ceban et al., 2021). Greater severity of Hospital Anxiety and Depression (HAD) scores was correlated with delayed healing in patients with chronic wounds (Cole-King and Harding, 2001). Lymphocyte stimulation by mitogens was also significantly attenuated in subjects with MDD (Miller et al., 1999), and was worse in subjects with major compared to minor depression (Cosyns et al., 1989).
Extant literature reporting on the inflammation in mood disorders provides evidence of significantly higher concentrations of proinflammatory cytokines (i.e., IL-6, TNF-ɑ) and levels of acute-phase proteins (i.e., C-reactive protein), chemokines, and soluble adhesion molecules in subjects with mood disorders, especially depressive disorders (Dowlati et al., 2010; Miller, 2020; Miller and Raison, 2016; Rosenblat et al., 2014). These findings support the notion of a persistent proinflammatory state in MDD, including rMDD (Maes et al., 2001), which can result in chronic inflammation. However, this chronic inflammation differs from the decreased vaccine-induced TNF-ɑ that indicated potentially attenuated immunity in Cassiers and colleagues’ (2019) study. Thus, it is possible that subjects with MDD suffer the presence of both high inflammation and immune suppression.
Not all studies evaluating MDD reported an association between MDD diagnosis and attenuated immune response to vaccination. The foregoing observation opposes the extensive literature associating symptoms of mood disorders (e.g., depressive symptoms, psychological stress, low social support) with lower immunity biomarkers following vaccination (Costanzo et al., 2004; Hayney et al., 2003; Afsar et al., 2009; Li et al., 2007). Studies have also found that low self esteem and fatigue (Morag et al., 1999), neuroticism (Phillips et al., 2005a), and loneliness (Pressmen et al., 2005) were associated with attenuated post-vaccination antibodies. Marsland et al. (2001) found that healthy subjects with negative trait affect, but not higher stress levels or Beck Depression Inventory scores, had lower antibodies following hepatitis B vaccination. Social support has also been positively correlated with immunoglobulin M response to vaccination with pneumococcal polysaccharides (Gallagher et al., 2008). However, Moynihan et al. (2004) found a negative correlation between high social support and influenza vaccine antibody titres, and no correlations between vaccine response and depression.
Psychological stress is another notable predictor of depressive disorders associated with weakened immune response. The development of depressive disorders are often preceded by stressful situations (Van Praag, 2005). Subjects with high perceived stress or distress have been shown to yield lower post-vaccination antibody titres (Miller et al., 2004; Snyder et al., 1990; Pedersen et al., 2009; Wong et al., 2013; Glaser et al., 1998; Vedhara et al., 1999; Li et al., 2007) and post-immunization lymphocyte proliferation (Snyder et al., 1993). However, a limited number of studies have also found no association (Jabaaij et al., 1996; Costanzo et al., 2004), or even a positive association (Petry et al., 1991) between stress levels and antibody or cytokine response to vaccination. In addition, research specifically regarding stressful life events has been contradictory: Gallagher et al. (2008) and Phillips et al. (2005b) found that stressful life events - but not overall psychological stress levels in Gallagher and colleagues’ study - were associated with low antibody titres, whereas Burns et al. (2002) found that high perceived stress - but not life events stress - was associated with low antibody titres.
Our results highlight the distinction between experiencing symptoms of a mental disorder, and actually having a diagnosed mental disorder: an individual suffering from symptoms of mood disorders without a diagnosed mental disorder may still be subject to attenuated immune response. Similarly, it cannot be established that all individuals with MDD suffer attenuated immunization response.
4.2. Schizophrenia
Schizophrenia and related psychiatric disorders have been associated with higher detection rates of viral infection, including hepatitis B virus (HBV) (Klinkenberg et al., 2003; Rosenberg et al., 2001; Zhu et al., 2015; Lluch and Miller, 2019), hepatitis C virus (HCV) (Rosenberg et al., 2001; Lluch and Miller, 2019), and human immunodeficiency virus (HIV) (Rosenberg et al., 2001), which may be due to increased infection susceptibility and environmental risk factors (Lluch and Miller, 2019). Schizophrenia has also been correlated with altered cytokine levels and inflammatory responses. Wang et al. (2016) discussed the abnormal CD4+ and CD8+ T lymphocyte counts as well as Th1 and Th2 imbalance in subjects with schizophrenia. There is also evidence of increased C-reactive protein and proinflammatory cytokines in subjects with schizophrenia (Fernandes et al., 2016.; Suvisaari et al., 2011), which suggests altered inflammatory and immune function in individuals with schizophrenia in line with two articles discussed in this review (Wang et al., 2016; Vaughan et al., 1949).
However, it is crucial to note the small sample sizes and moderate risks of bias in this review's studies on patients with schizophrenia. The publication years for included studies is also a potential cause for concern, as only one (Wang et al., 2016) of the five studies on schizophrenia in this review was conducted after 1972. The remaining four studies (Hussar et al., 1971; Solomon et al., 1968; Friedman et al., 1967; Vaughan et al., 1949) were thus written prior to the development of increasingly rigorous diagnostic criteria through the DSM-III, which was published in 1980 (American Psychiatric Association, 2022) and was considered a turning point in the conceptualization of psychiatric disorders, particularly schizophrenia (Jablensky, 2010). Following the introduction of the DSM-IV in 1994 (American Psychiatric Association, 2022) and the ICD-10 in 1990 (World Health Organization), the reliability of psychiatrists' schizophrenia diagnoses is also considered to have improved (Jablensky. 2010). In addition, the past few decades have resulted in great progress regarding scientific understanding of the human immune system, as well as improvements in vaccine composition and adjuvants (Rappuoli et al., 2011). The measurement accuracy of immunologic biomarkers such as antibodies has also improved over time due to the development of validation methodologies for techniques such as ELISA (Minic and Zivkovic, 2021). Thus, in addition to the inconclusivity arising from the contradicting results between the five studies, the publication dates of these articles warrant caution when interpreting this review's synthesis of schizophrenia-related studies.
4.4. Eating disorders
A potential explanation for the null findings in both studies of eating disorders (Armstrong-Esther et al., 1978; Zastrow et al., 2012) is that the form of malnutrition present in anorexia and bulimia may affect cellular immunity rather than humoral immunity (Nova et al., 2002). Anorexic patients experience an impairment of cell-mediated immune responses and phagocyte function (Nova et al., 2002), a significant increase in TNF-α and IL-6 mRNA expression (Kahl et al., 2004), and an attenuated proliferative response after stimulation with mitogens or anti-CD2 antibodies (Cason et al., 1986; Allende et al., 1998).
However, the literature varies with regards to immunosuppression in individuals with eating disorders. Fink et al. (1996) discussed the various conflicting studies that found normal CD4+ and CD8+ counts, low CD4+ and CD8+ counts, and elevated CD8+ counts in subjects with AN. In addition, Silber and Chan (1996) found no immune system impairment in subjects with AN when assessing lymphocyte proliferation with mitogen stimulation. Taken together, although certain immune impairments in anorexic subjects are similar to those observed in subjects with malnutrition, they are rarer and milder, and immune function appears adequately preserved, especially considering that patients with anorexia experience defective nutritional status (Silber and Chan, 1996; Nova et al., 2002).
Vaccine responses are not definitively influenced by malnourishment (Zimmermann et al., 2019), although malnourished children have displayed attenuated antibody response to T-cell-dependent and T-cell-independent antigens (Brussow et al., 1995), as well as meningococcal vaccine (Mohammed and Damisah, 1982) and pertussis toxin (Gaayeb et al., 2014). However, findings of correlation between attenuated vaccine response and malnutrition focus largely on malnourished children, rather than adults with eating disorders or nutritional deficits.
4.3. Sleep disorders
Given the small sample sizes of both sleep disorder studies (Taylor et al., 2017; Dopp et al., 2007) and their contradictory results, the relationship between sleep disorders and vaccine response remains inconclusive.
Taylor and colleagues’ (2017) results are supported by extensive research correlating poor sleep with attenuated antibody response to vaccination. Short sleep duration near vaccination date was associated with lower antibody responses to hepatitis A (Lange et al., 2003, 2011), hepatitis B (Prather et al. 2012), and influenza (Miller et al., 2004) vaccinations. The study of individuals with OSA included in this review administered trivalent inactivated vaccines (TIV), and although antibody responses were found to be adequately robust, other studies in healthy participants have mixed results following TIV vaccination: Spiegel et al. (2002) found that deliberately sleep-deprived healthy participants had lower antibody responses in the week following vaccination, while Ayling et al. (2018) found no association between sleep duration and immune response.
However, the foregoing studies only assessed humoral immune response, and did not take a potential attenuation of cellular immune response into consideration. In fact, sleep disturbance appears to lead to a shift away from cellular immunity (Type 1 T helper cell function) (Axelsson et al., 2013; Sakami et al., 2002). In line with this evidence, Dopp et al. (2007) suggest that their null findings regarding antibody responses in subjects with OSA may be a result of the humoral immune system compensating for a lack of cellular immunity. Future research should thus investigate the cellular immune response to vaccination in subjects with a diagnosed sleep disorder, rather than focusing only on healthy subjects who undergo a period of sleep deprivation, or on the humoral immune response alone.
While previous literature suggests a weakened immune response in subjects with sleep deprivation, these mixed results may be partially due to naturalistic short sleep duration and sleep deprivation which are not synonymous with chronic insomnia (Taylor et al., 2017). Individuals with insomnia do not necessarily experience excessive daytime sleepiness indicative of sleep deprivation, but rather, may appear similar to healthy people with typical sleep habits (Riedel and Lichstein, 2000; Stepanski et al., 1988).
4.4. Trauma or stress disorders
Kosor Krnic et al. (2007) found no association between PTSD diagnosis and response to influenza vaccine, despite the apparent multi-tiered and bidirectional relationship between PTSD and the immune system, especially with regards to inflammation (Neigh and Ali, 2016). PTSD is associated with chronic inflammation and elevated cytokine (i.e., IL-6, IL-1β, TNF-α, and IFN-γ) production (Passos et al., 2015). Given that cytokines contribute to the differentiation of T cell subsets, PTSD and adaptive immunity may be correlated with one another (Neigh and Ali, 2016). Furthermore, in a study of infections within a population of persons with a mental disorder, PTSD was a significant predictor of HBV and HIV (Essock et al., 2003), and a separate study found that individuals with a history of PTSD had a 58% higher risk for select autoimmune diseases than the control group (O'Donovan et al., 2015). PTSD is also associated with an aged immune phenotype, suggesting early immunosenescence and thus additional susceptibility and increased severity of infection or disease (Aiello et al., 2016). Thus, Kosor Krnic and colleagues’ results contradict the evidence suggesting that individuals with PTSD suffer from attenuated or altered immune function. Since only one study focused on PTSD, our conclusions regarding PTSD or trauma and stress-based disorders are limited.
4.5. A brief discussion of comorbidities and symptoms of mental disorders
Mental disorders are increasingly associated with physical comorbidities (Sartorius, 2013). The association between mental disorders and chronic physical diseases has been extensively researched, with comorbidities a focus of many studies and reviews (Dare et al., 2019; Stubbs et al., 2015; Vancampfort et al., 2015; Nakash et al., 2014). Therefore, attenuated immunity in persons with mental disorders may be due in part to the comorbid physical diseases that many individuals with a mental disorder suffer from, rather than the mental disorder being the root cause of attenuated immunity. Mental disorders are also associated with increased risk of psychiatric comorbidity (Plana-Ripoll et al., 2019), and symptoms of various mental disorders often overlap. For instance, sleep disturbance is considered a significant risk factor for the development of depression (Baglioni et al., 2011; Cho et al., 2008; Lee et al., 2013; Franzen and Buysse, 2008), PTSD diagnosis is based on negative cognition or mood (Neigh and Ali, 2016), and patients with AN often experience major depression or anxiety disorders (Klump et al., 2009). Thus, our analysis of one particular mental disorder may apply to individuals diagnosed with a separate mental disorder but who express similar symptoms to the analyzed mental disorder (e.g., depressive mood is frequently exhibited both by individuals with bipolar disorder and those with MDD).
4.6. Limitations
The limitations of this review include the relatively small number of articles (n = 13) with high heterogeneity regarding mental disorders studied and vaccines administered, and thus the lack of quantitative analysis. The limited number of studies is indicative of the limited literature on this topic. A majority of the studies were published over a decade ago with sample sizes of under 30 subjects, and with less well-defined methods compared to the more recent studies. The results of these studies were mixed, highlighting the need for future studies to confirm the findings with more rigorous methodology.
Another limitation of this review is the wide variety of vaccine types included. The specific immune responses elicited (e.g., cellular vs. humoral) and the duration of immunity varies amongst different vaccine types (e,g., live attenuated vaccines, inactivated vaccines, toxoid vaccines) (Amanna and Slifka, 2011). Thus, the immunologic outcomes following vaccination may be influenced by whether the vaccine type elicits responses in a specific component of the immune system that is compromised in individuals with mental disorders. For instance, individuals with MDD exhibit reduced cellular immunity (Beurel et al., 2020), and therefore, these individuals may react poorly to vaccines that primarily induce T cells. Due to the limited number of studies assessing each vaccine type (i.e., live attenuated vaccines, inactivated vaccines, toxoid vaccines, etc.), the role of vaccine type in immunologic outcomes for individuals with mental disorders remains inconclusive. The studies included herein focused almost exclusively on humoral rather than cellular immune response. Additional research on post-vaccine cellular immunity will provide a more in-depth understanding of the overall immune function in persons with mental disorders. Furthermore, certain studies included in this review did not disclose the specific vaccine administered. For instance, the specific measles vaccine administered to each subject was not specified by Ford and colleagues (2019), who assessed biomarkers indicative of protection against measles in adults who received childhood vaccination.
Few studies reported whether participants were taking psychotropic medications, and fewer studies assessed medication use and immunologic outcomes. Thus, it is unclear whether medications for mental disorders influence immune response to vaccination. Further research is required to evaluate the effect of psychotropic medications on immunity, given that the psychopharmacology impacts on the immune system and inflammatory response may result in altered immunologic responses to vaccination, including the COVID-19 vaccination. For instance, antidepressants such as selective serotonin reuptake inhibitors (SSRI) have been shown to act as functional inhibitors of acid sphingomyelinase (FIASMA) (Kornhuber et al., 2021). Acid sphingomyelinase (ASM) inhibition plays a protective role against SARS-CoV-2 infection, as supported by multiple studies suggesting that fluvoxamine, an SSRI antidepressant, is associated with improved COVID-19 outcomes in hospitalized and high-risk patients (Lenze et al., 2020; Reis et al., 2022).
Lastly, the correlations between select mental disorders and vaccines are not necessarily indicative of a causal relationship; although many confounding factors were accounted for in the studies, there may be other variables independent of mental disorder diagnoses that contributed towards vaccine response. This is especially relevant concerning the two studies reported on immune biomarker levels in adults who received childhood vaccination (Wang et al., 2016; Ford et al., 2019). The decay rate of vaccine response over time differs between individuals, and may vary due to a combination of factors specific to each individual (Anita et al., 2018). There may have been various factors other than psychiatric diagnoses which contributed towards the lower titers in individuals with mental disorders, given the duration of time between vaccine administration and the biomarker measurement many years later. The results from these two studies must therefore be interpreted with additional caution compared to results of studies assessing immune response shortly after vaccine administration.
5. Conclusion
Taken together, reports of the association between mental disorder and vaccine response are mixed. While individuals with mental disorders have been reported to experience immune dysfunction, not all studies supported the foregoing relationship. Future research should aim to investigate the relationship between attenuated vaccine response in persons with mental disorders using larger sample sizes, well-defined methods, as well as expand to other mental disorders. The results of our synthesis of the literature provide further impetus to characterize the immune response amongst persons with mental disorders to COVID-19 vaccination, and to identify covariates and moderating factors of immune response in this population (Xiong et al., 2020).
Disclosures
Dr. Roger McIntyre has received research grant support from CIHR/GACD/Chinese National Natural Research Foundation; speaker/consultation fees from Lundbeck, Janssen, Alkermes, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Abbvie, Atai Life Sciences. Dr. Roger McIntyre is a CEO of Braxia Scientific Corp.
Leanna M.W. Lui is a contractor to Braxia Scientific Corp.
Kayla M. Teopiz receives personal fees from Braxia Scientific Corp.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Karren Xiao: Conceptualization, Visualization, Writing – original draft, Writing – review & editing. Emily S. Gillissie: Writing – review & editing. Leanna M.W. Lui: Writing – review & editing. Felicia Ceban: Writing – review & editing. Kayla M. Teopiz: Writing – review & editing. Hartej Gill: Writing – review & editing. Bing Cao: Writing – review & editing. Roger Ho: Writing – review & editing. Joshua D. Rosenblat: Writing – review & editing. Roger S. McIntyre: Conceptualization, Writing – review & editing.
Declaration of Competing Interest
All authors declare no conflicts of interest.
Acknowledgments
None.
References
- Afsar B., Elsurer R., Eyileten T., Yilmaz M.I., Caglar K. Antibody response following hepatitis B vaccination in dialysis patients: does depression and life quality matter? Vaccine. 2009;27(42):5865–5869. doi: 10.1016/j.vaccine.2009.07.055. [DOI] [PubMed] [Google Scholar]
- Aiello A.E., Dowd J.B., Jayabalasingham B., Feinstein L., Uddin M., Simanek A.M., Cheng C.K., Galea S., Wildman D.E., Koenen K., Pawelec G. PTSD is associated with an increase in aged T cell phenotypes in adults living in Detroit. Psychoneuroendocrinology. 2016;67:133–141. doi: 10.1016/j.psyneuen.2016.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allende L.M., Corell A., Manzanares J., Madruga D., Marcos A., Madroño A., López-Goyanes A., García-Pérez M.A., Moreno J.M., Rodrigo M., Sanz F., Arnaiz-Villena A. Immunodeficiency associated with anorexia nervosa is secondary and improves after refeeding. Immunology. 1998;94(4):543–551. doi: 10.1046/j.1365-2567.1998.00548.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amanna I.J., Slifka M.K. Contributions of humoral and cellular immunity to vaccine-induced protection in humans. Virology. 2011;411(2):206–215. doi: 10.1016/j.virol.2010.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . 5th ed. 2013. Diagnostic and Statistical Manual of Mental Disorders. [DOI] [Google Scholar]
- Andersson N.W., Goodwin R.D., Okkels N., Gustafsson L.N., Taha F., Cole S.W., Munk-Jørgensen P. Depression and the risk of severe infections: prospective analyses on a nationwide representative sample. Int. J. Epidemiol. 2016;45(1):131–139. doi: 10.1093/ije/dyv333. [DOI] [PubMed] [Google Scholar]
- Antia A., Ahmed H., Handel A., Carlson N.E., Amanna I.J., Antia R., Slifka M. Heterogeneity and longevity of antibody memory to viruses and vaccines. PLoS Biol. 2018;16(8) doi: 10.1371/journal.pbio.2006601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong-Esther C.A., Lacey J.H., Crisp A.H., Bryant T.N. An investigation of the immune response of patients suffering from anorexia nervosa. Postgrad. Med. J. 1978;54(632):395–399. doi: 10.1136/pgmj.54.632.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Axelsson J., Rehman J.U., Akerstedt T., Ekman R., Miller G.E., Höglund C.O., Lekander M. Effects of sustained sleep restriction on mitogen-stimulated cytokines, chemokines and T helper 1/T helper 2 balance in humans. PLoS One. 2013;8(12):e82291. doi: 10.1371/journal.pone.0082291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayling K., Fairclough L., Tighe P., Todd I., Halliday V., Garibaldi J., Royal S., Hamed A., Buchanan H., Vedhara K. Positive mood on the day of influenza vaccination predicts vaccine effectiveness: a prospective observational cohort study. Brain Behav. Immun. 2018;67:314–323. doi: 10.1016/j.bbi.2017.09.008. [DOI] [PubMed] [Google Scholar]
- Baglioni C., Battagliese G., Feige B., Spiegelhalder K., Nissen C., Voderholzer U., Lombardo C., Riemann D. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J. Affect. Disord. 2011;135(1–3):10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- Beurel E., Toups M., Nemeroff C.B. The bidirectional relationship of depression and inflammation: double trouble. Neuron. 2020;107(2):234–256. doi: 10.1016/j.neuron.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brüssow H., Sidoti J., Dirren H., Freire W.B. Effect of malnutrition in Ecuadorian children on titers of serum antibodies to various microbial antigens. Clin. Diagn. Lab. Immunol. 1995;2(1):62–68. doi: 10.1128/cdli.2.1.62-68.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns V.E., Carroll D., Drayson M., Whitham M., Ring C. Life events, perceived stress and antibody response to influenza vaccination in young, healthy adults. J. Psychosom. Res. 2003;55(6):569–572. doi: 10.1016/s0022-3999(03)00073-4. [DOI] [PubMed] [Google Scholar]
- Burns V.E., Drayson M., Ring C., Carroll D. Perceived stress and psychological well-being are associated with antibody status after meningitis C conjugate vaccination. Psychosom. Med. 2002;64(6):963–970. doi: 10.1097/01.psy.0000038936.67401.28. [DOI] [PubMed] [Google Scholar]
- Cason J., Ainley C.C., Wolstencroft R.A., Norton K.R., Thompson R.P. Cell-mediated immunity in anorexia nervosa. Clin. Exp. Immunol. 1986;64(2):370–375. [PMC free article] [PubMed] [Google Scholar]
- Cassiers L., Niemegeers P., Fransen E., Morrens M., De Boer P., Van Nueten L., Claes S., Sabbe B., Van Den Eede F. Neuroendocrine and inflammatory effects of childhood trauma following psychosocial and inflammatory stress in women with remitted major depressive disorder. Brain Sci. 2019;9(12):375. doi: 10.3390/brainsci9120375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceban F., Nogo D., Carvalho I.P., Lee Y., Nasri F., Xiong J., Lui L., Subramaniapillai M., Gill H., Liu R.N., Joseph P., Teopiz K.M., Cao B., Mansur R.B., Lin K., Rosenblat J.D., Ho R.C., McIntyre R.S. Association between mood disorders and risk of COVID-19 infection, hospitalization, and death: a systematic review and meta-analysis. JAMA Psychiatry. 2021 doi: 10.1001/jamapsychiatry.2021.1818. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho H.J., Lavretsky H., Olmstead R., Levin M.J., Oxman M.N., Irwin M.R. Sleep disturbance and depression recurrence in community-dwelling older adults: a prospective study. Am. J. Psychiatry. 2008;165(12):1543–1550. doi: 10.1176/appi.ajp.2008.07121882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole-King A., Harding K.G. Psychological factors and delayed healing in chronic wounds. Psychosom. Med. 2001;63(2):216–220. doi: 10.1097/00006842-200103000-00004. [DOI] [PubMed] [Google Scholar]
- Costanzo E.S., Lutgendorf S.K., Kohut M.L., Nisly N., Rozeboom K., Spooner S., Benda J., McElhaney J.E. Mood and cytokine response to influenza virus in older adults. J. Gerontol. Ser. A. 2004;59(12):1328–1333. doi: 10.1093/gerona/59.12.1328. Biol. Sci. Med. Sci. [DOI] [PubMed] [Google Scholar]
- Cosyns P., Maes M., Vandewoude M., Stevens W.J., De Clerck L.S., Schotte C. Impaired mitogen-induced lymphocyte responses and the hypothalamic-pituitary-adrenal axis in depressive disorders. J. Affect. Disord. 1989;16(1):41–48. doi: 10.1016/0165-0327(89)90054-2. [DOI] [PubMed] [Google Scholar]
- Daré L.O., Bruand P.E., Gérard D., Marin B., Lameyre V., Boumédiène F., Preux P. Co-morbidities of mental disorders and chronic physical diseases in developing and emerging countries: a meta-analysis. BMC Public Health. 2019;19(304) doi: 10.1186/s12889-019-6623-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dopp J.M., Wiegert N.A., Moran J.J., Muller D., Weber S., Hayney M.S. Humoral immune responses to influenza vaccination in patients with obstructive sleep apnea. Pharmacotherapy. 2007;27(11):1483–1489. doi: 10.1592/phco.27.11.1483. [DOI] [PubMed] [Google Scholar]
- Dowlati Y., Herrmann N., Swardfager W., Liu H., Sham L., Reim E.K., Lanctôt K.L. A meta-analysis of cytokines in major depression. Biol. Psychiatry. 2010;67(5):446–457. doi: 10.1016/j.biopsych.2009.09.033. [DOI] [PubMed] [Google Scholar]
- Essock S.M., Dowden S., Constantine N.T., Katz L., Swartz M.S., Meador K.G., Osher F.C., Rosenberg S.D., Five-Site Health and Risk Study Research Committee Risk factors for HIV, hepatitis B, and hepatitis C among persons with severe mental illness. Psychiatr. Serv. 2003;54(6):836–841. doi: 10.1176/appi.ps.54.6.836. [DOI] [PubMed] [Google Scholar]
- Fernandes B.S., Steiner J., Bernstein H.G., Dodd S., Pasco J.A., Dean O.M., Nardin P., Gonçalves C.A., Berk M. C-reactive protein is increased in schizophrenia but is not altered by antipsychotics: meta-analysis and implications. Mol. Psychiatry. 2016;21(4):554–564. doi: 10.1038/mp.2015.87. [DOI] [PubMed] [Google Scholar]
- Fink S., Eckert E., Mitchell J., Crosby R., Pomeroy C. T-lymphocyte subsets in patients with abnormal body weight: longitudinal studies. in anorexia nervosa and obesity. Int. J. Eat. Disord. 1996;20(3):295–305. doi: 10.1002/(SICI)1098-108X(199611)20:3%3C295::AID-EAT9x3E3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- Ford B.N., Yolken R.H., Dickerson F.B., Teague T.K., Irwin M.R., Paulus M.P., Savitz J. Reduced immunity to measles in adults with major depressive disorder. Psychol. Med. 2019;49(2):243–249. doi: 10.1017/S0033291718000661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franzen P.L., Buysse D.J. Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues Clin. Neurosci. 2008;10(4):473–481. doi: 10.31887/DCNS.2008.10.4/plfranzen. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frasca D., Diaz A., Romero M., Mendez N.V., Landin A.M., Blomberg B.B. Effects of age on H1N1-specific serum IgG1 and IgG3 levels evaluated during the 2011-2012 influenza vaccine season. Immun. Ageing. 2013;10(1):14. doi: 10.1186/1742-4933-10-14. I & A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman S.B., Cohen J., Iker H. Antibody response to cholera vaccine. Differences between depressed, schizophrenic, and normal subjects. Arch. Gen. Psychiatry. 1967;16(3):312–315. doi: 10.1001/archpsyc.1967.01730210052009. [DOI] [PubMed] [Google Scholar]
- Gaayeb L., Pinçon C., Cames C., Sarr J.B., Seck M., Schacht A.M., Remoué F., Hermann E., Riveau G. Immune response to Bordetella pertussis is associated with season and undernutrition in Senegalese children. Vaccine. 2014;32(27):3431–3437. doi: 10.1016/j.vaccine.2014.03.086. [DOI] [PubMed] [Google Scholar]
- Gallagher S., Phillips A.C., Ferraro A.J., Drayson M.T., Carroll D. Social support is positively associated with the immunoglobulin M response to vaccination with pneumococcal polysaccharides. Biol. Psychol. 2008;78(2):211–215. doi: 10.1016/j.biopsycho.2008.01.001. [DOI] [PubMed] [Google Scholar]
- Gidron Y., Hassid A., Yisrael H., Biderman A. Do psychological factors predict occurrence of influenza-like symptoms in vaccinated elderly residents of a sheltered home? Br. J. Health Psychol. 2005;10(Pt 3):411–420. doi: 10.1348/135910704X20026. [DOI] [PubMed] [Google Scholar]
- Glaser R., Kiecolt-Glaser J.K., Malarkey W.B., Sheridan J.F. The influence of psychological stress on the immune response to vaccines. Ann. N. Y. Acad. Sci. 1998;840:649–655. doi: 10.1111/j.1749-6632.1998.tb09603.x. [DOI] [PubMed] [Google Scholar]
- Goodwin K., Viboud C., Simonsen L. Antibody response to influenza vaccination in the elderly: a quantitative review. Vaccine. 2006;24(8):1159–1169. doi: 10.1016/j.vaccine.2005.08.105. [DOI] [PubMed] [Google Scholar]
- Hayney M.S., Love G.D., Buck J.M., Ryff C.D., Singer B., Muller D. The association between psychosocial factors and vaccine-induced cytokine production. Vaccine. 2003;21(19–20):2428–2432. doi: 10.1016/s0264-410x(03)00057-4. [DOI] [PubMed] [Google Scholar]
- Hussar A.E., Cradle J.L., Beiser S.M. A study of the immunologic and allergic responsiveness of chronic schizophrenics. Br. J. Psychiatry J. Ment. Sci. 1971;118(542):91–92. doi: 10.1192/bjp.118.542.91. [DOI] [PubMed] [Google Scholar]
- Irwin M.R., Levin M.J., Laudenslager M.L., Olmstead R., Lucko A., Lang N., Carrillo C., Stanley H.A., Caulfield M.J., Weinberg A., Chan I.S., Clair J., Smith J.G., Marchese R.D., Williams H.M., Beck D.J., McCook P.T., Zhang J.H., Johnson G., Oxman M.N. Varicella zoster virus-specific immune responses to a herpes zoster vaccine in elderly recipients with major depression and the impact of antidepressant medications. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2013;56(8):1085–1093. doi: 10.1093/cid/cis1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin M., Costlow C., Williams H., Artin K.H., Chan C.Y., Stinson D.L., Levin M.J., Hayward A.R., Oxman M.N. Cellular immunity to varicella-zoster virus in patients with major depression. J. Infect. Dis. 1998;178(Suppl 1):S104–S108. doi: 10.1086/514272. [DOI] [PubMed] [Google Scholar]
- Jabaaij L., van Hattum J., Vingerhoets J.J., Oostveen F.G., Duivenvoorden H.J., Ballieux R.E. Modulation of immune response to rDNA hepatitis B vaccination by psychological stress. J. Psychosom. Res. 1996;41(2):129–137. doi: 10.1016/0022-3999(96)00123-7. [DOI] [PubMed] [Google Scholar]
- Jablensky A. The diagnostic concept of schizophrenia: its history, evolution, and future prospects. Dialog. Clin. Neurosci. 2010;12(3):271–287. doi: 10.31887/DCNS.2010.12.3/ajablensky. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahl K.G., Kruse N., Rieckmann P., Schmidt M.H. Cytokine mRNA expression patterns in the disease course of female adolescents with anorexia nervosa. Psychoneuroendocrinology. 2004;29(1):13–20. doi: 10.1016/s0306-4530(02)00131-2. [DOI] [PubMed] [Google Scholar]
- Klinkenberg W.D., Caslyn R.J., Morse G.A., Yonker R.D., McCudden S., Ketema F., Constantine N.T. Prevalence of human immunodeficiency virus, hepatitis B, and hepatitis C among homeless persons with co-occurring severe mental illness and substance use disorders. Compr. Psychiatry. 2003;44(4):293–302. doi: 10.1016/S0010-440X(03)00094-4. [DOI] [PubMed] [Google Scholar]
- Klump K.L., Bulik C.M., Kaye W.H., Treasure J., Tyson E. Academy for eating disorders position paper: eating disorders are serious mental illnesses. Int. J. Eat. Disord. 2009;42(2):97–103. doi: 10.1002/eat.20589. [DOI] [PubMed] [Google Scholar]
- Kornhuber J., Hoertel N., Gulbins E. The acid sphingomyelinase/ceramide system in COVID-19. Mol. Psychiatry. 2021 doi: 10.1038/s41380-021-01309-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosor Krnic E., Gagro A., Kozaric-Kovacic D., Vilibic M., Grubisic-Ilic M., Folnegovic-Smalc V., Drazenovic V., Cecuk-Jelicic E., Gjenero-Margan I., Kuzman I., Jeren T., Sabioncello A., Kerhin-Brkljacic V., Kaic B., Markotic A., Gotovac K., Rabatic S., Mlinaric-Galinovic G., Dekaris D. Outcome of influenza vaccination in combat-related post-traumatic stress disorder (PTSD) patients. Clin. Exp. Immunol. 2007;149(2):303–310. doi: 10.1111/j.1365-2249.2007.03410.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kronfol Z. Immune dysregulation in major depression: a critical review of existing evidence. Int. J. Neuropsychopharmacol. 2002;5(4):333–343. doi: 10.1017/S1461145702003024. [DOI] [PubMed] [Google Scholar]
- Lange T., Dimitrov S., Bollinger T., Diekelmann S., Born J. Sleep after vaccination boosts immunological memory. J. Immunol. 2011;187(1):283–290. doi: 10.4049/jimmunol.1100015. [DOI] [PubMed] [Google Scholar]
- Lange T., Perras B., Fehm H.L., Born J. Sleep enhances the human antibody response to hepatitis A vaccination. Psychosom. Med. 2003;65(5):831–835. doi: 10.1097/01.psy.0000091382.61178.f1. [DOI] [PubMed] [Google Scholar]
- Lasserre A., Blaizeau F., Gorwood P., Bloch K., Chauvin P., Liard F., Blanchon T., Hanslik T. Herpes zoster: family history and psychological stress-case-control study. J. Clin. Virol. 2012;55(2):153–157. doi: 10.1016/j.jcv.2012.06.020. Off. Publ. Pan Am. Soc. Clin. Virol. [DOI] [PubMed] [Google Scholar]
- Lee E., Cho H.J., Olmstead R., Levin M.J., Oxman M.N., Irwin M.R. Persistent sleep disturbance: a risk factor for recurrent depression in community-dwelling older adults. Sleep. 2013;36(11):1685–1691. doi: 10.5665/sleep.3128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenze E.J., Mattar C., Zorumski C.F., Stevens A., Schweiger J., Nicol G.E., Miller J.P., Yang L., Yingling M., Avidan M.S., Reiersen A.M. Fluvoxamine vs placebo and clinical deterioration in outpatients with symptomatic COVID-19. JAMA. 2020;324(22):2292. doi: 10.1001/jama.2020.22760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leserman J. Role of depression, stress, and trauma in HIV disease progression. Psychosom. Med. 2008;70(5):539–545. doi: 10.1097/PSY.0b013e3181777a5f. [DOI] [PubMed] [Google Scholar]
- Li J., Cowden L.G., King J.D., Briles D.A., Schroeder H.W., Stevens A.B., Perry R.T., Chen Z., Simmons M.S., Wiener H.W., Tiwari H.K., Harrell L.E., Go R.C. Effects of chronic stress and interleukin-10 gene polymorphisms on antibody response to tetanus vaccine in family caregivers of patients with Alzheimer's disease. Psychosom. Med. 2007;69(6):551–559. doi: 10.1097/PSY.0b013e3180cc2c61. [DOI] [PubMed] [Google Scholar]
- Lluch E., Miller B.J. Rates of hepatitis B and C in patients with schizophrenia: a meta-analysis. Gen. Hosp. Psychiatry. 2019;61:41–46. doi: 10.1016/j.genhosppsych.2019.10.007. [DOI] [PubMed] [Google Scholar]
- Madison A.A., Shrout M.R., Renna M.E., Kiecolt-Glaser J.K. Psychological and behavioral predictors of vaccine efficacy: considerations for COVID-19. Perspect. Psychol. Sci. 2021;16(2):191–203. doi: 10.1177/1745691621989243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maes M., Ombelet W., De Jongh R., Kenis G., Bosmans E. The inflammatory response following delivery is amplified in women who previously suffered from major depression, suggesting that major depression is accompanied by a sensitization of the inflammatory response system. J. Affect. Disord. 2001;63(1–3):85–92. doi: 10.1016/s0165-0327(00)00156-7. [DOI] [PubMed] [Google Scholar]
- Marsland A.L., Cohen S., Rabin B.S., Manuck S.B. Associations between stress, trait negative affect, acute immune reactivity, and antibody response to hepatitis B injection in healthy young adults. Health psychology: official journal of the division of health psychology. Am. Psychol. Assoc. 2001;20(1):4–11. [PubMed] [Google Scholar]
- McIntyre R.S., Berk M., Brietzke E., Goldstein B.I., López-Jaramillo C., Kessing L.V., Malhi G.S., Nierenberg A.A., Rosenblat J.D., Majeed A., Vieta E., Vinberg M., Young A.H., Mansur R.B. Bipolar disorders. Lancet. 2020;396(10265):1841–1856. doi: 10.1016/S0140-6736(20)31544-0. (London, England), [DOI] [PubMed] [Google Scholar]
- Miller A.H. Beyond depression: the expanding role of inflammation in psychiatric disorders. World Psychiatry Off. J. World Psychiatr. Assoc. (WPA) 2020;19(1):108–109. doi: 10.1002/wps.20723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller A.H., Raison C.L. The role of inflammation in depression: from evolutionary imperative to modern treatment target. Nat. Rev. Immunol. 2016;16(1):22–34. doi: 10.1038/nri.2015.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller G.E., Cohen S., Herbert T.B. Pathways linking major depression and immunity in ambulatory female patients. Psychosom. Med. 1999;61(6):850–860. doi: 10.1097/00006842-199911000-00021. [DOI] [PubMed] [Google Scholar]
- Miller G.E., Cohen S., Pressman S., Barkin A., Rabin B.S., Treanor J.J. Psychological stress and antibody response to influenza vaccination: when is the critical period for stress, and how does it get inside the body? Psychosom. Med. 2004;66(2):215–223. doi: 10.1097/01.psy.0000116718.54414.9e. [DOI] [PubMed] [Google Scholar]
- Minic R., Zivkovic I. Optimization, validation and standardization of Elisa. Norovirus. 2021 doi: 10.5772/intechopen.94338. [DOI] [Google Scholar]
- Mohammed I., Damisah M.M. The immunological response to polyvalent meningococcal vaccine in Bauchi State, Nigeria. Trans. R. Soc. Trop. Med. Hyg. 1982;76(3):351–353. doi: 10.1016/0035-9203(82)90188-2. [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., Group PRISMA. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morag M., Morag A., Reichenberg A., Lerer B., Yirmiya R. Psychological variables as predictors of rubella antibody titers and fatigue–a prospective, double blind study. J. Psychiatr. Res. 1999;33(5):389–395. doi: 10.1016/s0022-3956(99)00010-2. [DOI] [PubMed] [Google Scholar]
- Moynihan J.A., Larson M.R., Treanor J., Duberstein P.R., Power A., Shore B., Ader R. Psychosocial factors and the response to influenza vaccination in older adults. Psychosom. Med. 2004;66(6):950–953. doi: 10.1097/01.psy.0000140001.49208.2d. [DOI] [PubMed] [Google Scholar]
- Mullen S. Major depressive disorder in children and adolescents. Ment. Health Clin. 2018;8(6):275–283. doi: 10.9740/mhc.2018.11.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakash O., Levav I., Aguilar-Gaxiola S., Alonso J., Andrade L.H., Angermeyer M.C., Bruffaerts R., Caldas-de-Almeida J.M., Florescu S., de Girolamo G., Gureje O., He Y., Hu C., de Jonge P., Karam E.G., Kovess-Masfety V., Medina-Mora M.E., Moskalewicz J., Murphy S., Nakamura Y.…Scott K.M. Comorbidity of common mental disorders with cancer and their treatment gap: findings from the World Mental Health Surveys. Psychooncology. 2014;23(1):40–51. doi: 10.1002/pon.3372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2022). DSM history. https://www.psychiatry.org/psychiatrists/practice/dsm/history-of-the-dsm (Accessed Aug 6, 2021).
- Neigh G.N., Ali F.F. Co-morbidity of PTSD and immune system dysfunction: opportunities for treatment. Curr. Opin. Pharmacol. 2016;29:104–110. doi: 10.1016/j.coph.2016.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niemegeers P., De Boer P., Dumont G.J.H., Van Den Eede F., Fransen E., Claes S.J., Morrens M., Sabbe B.G.C. Differential effects of inflammatory and psychosocial stress on mood, hypothalamic-pituitary-adrenal axis, and inflammation in remitted depression. Neuropsychobiology. 2016;74(3):150–158. doi: 10.1159/000466698. [DOI] [PubMed] [Google Scholar]
- Nova E., Samartín S., Gómez S., Morandé G., Marcos A. The adaptive response of the immune system to the particular malnutrition of eating disorders. Eur. J. Clin. Nutr. 2002;56(Suppl 3):S34–S37. doi: 10.1038/sj.ejcn.1601482. [DOI] [PubMed] [Google Scholar]
- O'Donovan A., Cohen B.E., Seal K.H., Bertenthal D., Margaretten M., Nishimi K., Neylan T.C. Elevated risk for autoimmune disorders in iraq and afghanistan veterans with posttraumatic stress disorder. Biol. Psychiatry. 2015;77(4):365–374. doi: 10.1016/j.biopsych.2014.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passos I.C., Vasconcelos-Moreno M.P., Costa L.G., Kunz M., Brietzke E., Quevedo J., Salum G., Magalhães P.V., Kapczinski F., Kauer-Sant'Anna M. Inflammatory markers in post-traumatic stress disorder: a systematic review, meta-analysis, and meta-regression. Lancet Psychiatry. 2015;2(11):1002–1012. doi: 10.1016/S2215-0366(15)00309-0. [DOI] [PubMed] [Google Scholar]
- Pedersen A.F., Zachariae R., Bovbjerg D.H. Psychological stress and antibody response to influenza vaccination: a meta-analysis. Brain Behav. Immun. 2009;23(4):427–433. doi: 10.1016/j.bbi.2009.01.004. [DOI] [PubMed] [Google Scholar]
- Petry L.J., Weems L.B., Livingstone J.N. Relationship of stress, distress, and the immunologic response to a recombinant hepatitis B vaccine. J. Fam. Pract. 1991;32(5):481–486. 2nd. [PubMed] [Google Scholar]
- Phillips A.C., Burns V.E., Carroll D., Ring C., Drayson M. The association between life events, social support, and antibody status following thymus-dependent and thymus-independent vaccinations in healthy young adults. Brain Behav. Immun. 2005;19(4):325–333. doi: 10.1016/j.bbi.2004.10.004. [DOI] [PubMed] [Google Scholar]
- Phillips A.C., Carroll D., Burns V.E., Drayson M. Neuroticism, cortisol reactivity, and antibody response to vaccination. Psychophysiology. 2005;42(2):232–238. doi: 10.1111/j.1469-8986.2005.00281.x. [DOI] [PubMed] [Google Scholar]
- Plana-Ripoll O., Pedersen C.B., Holtz Y., Benros M.E., Dalsgaard S., de Jonge P., Fan C.C., Degenhardt L., Ganna A., Greve A.N., Gunn J., Iburg K.M., Kessing L.V., Lee B.K., Lim C., Mors O., Nordentoft M., Prior A., Roest A.M., Saha S.…McGrath J.J. Exploring comorbidity within mental disorders among a Danish national population. JAMA Psychiatry. 2019;76(3):259–270. doi: 10.1001/jamapsychiatry.2018.3658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prather A.A., Hall M., Fury J.M., Ross D.C., Muldoon M.F., Cohen S., Marsland A.L. Sleep and antibody response to hepatitis B vaccination. Sleep. 2012;35(8):1063–1069. doi: 10.5665/sleep.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pressman S.D., Cohen S., Miller G.E., Barkin A., Rabin B.S., Treanor J.J. Loneliness, social network size, and immune response to influenza vaccination in college freshmen. Health psychology: official journal of the Division of Health Psychology. Am. Psychol. Assoc. 2005;24(3):297–306. doi: 10.1037/0278-6133.24.3.297. [DOI] [PubMed] [Google Scholar]
- Rappuoli R., Mandl C.W., Black S., De Gregorio E. Vaccines for the twenty-first century society. Nat. Rev. Immunol. 2011;11(12):865–872. doi: 10.1038/nri3085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reis G., dos Santos, Moreira-Silva E.A., Silva D.C., Thabane L., Milagres A.C., Ferreira T.S., dos Santos C.V., de Souza Campos V.H., Nogueira A.M., de Almeida A.P., Callegari E.D., de Figueiredo Neto A.D., Savassi L.C., Simplicio M.I., Ribeiro L.B., Oliveira R., Harari O., Forrest J.I., Ruton H.…Mills E.J. Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with covid-19: the together randomised, platform clinical trial. Lancet Glob. Health. 2022;10(1) doi: 10.1016/s2214-109x(21)00448-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riedel B.W., Lichstein K.L. Insomnia and daytime functioning. Sleep Med. Rev. 2000;4(3):277–298. doi: 10.1053/smrv.1999.0074. [DOI] [PubMed] [Google Scholar]
- National Collaborating Centre for Mental Health (2011). Common Mental Health Disorders: Identification and Pathways to Care. The British Psychological Society and The Royal College of Psychiatrists. Available from: https://www.ncbi.nlm.nih.gov/books/NBK92254/. [PubMed]
- Ritchie, H., & Roser, M. (2018). Mental health. https://ourworldindata.org/mental-health (Accessed Aug 2, 2021,).
- Rosenberg S.D., Goodman L.A., Osher F.C., Swartz M.S., Essock S.M., Butterfield M.I., Constantine N.T., Wolford G.L., Salyers M.P. Prevalence of HIV, hepatitis B, and hepatitis C in people with severe mental illness. Am. J. Public Health. 2001;91(1):31–37. doi: 10.2105/ajph.91.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblat J.D., Cha D.S., Mansur R.B., McIntyre R.S. Inflamed moods: a review of the interactions between inflammation and mood disorders. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2014;53:23–34. doi: 10.1016/j.pnpbp.2014.01.013. [DOI] [PubMed] [Google Scholar]
- Sakami S., Ishikawa T., Kawakami N., Haratani T., Fukui A., Kobayashi F., Fujita O., Araki S., Kawamura N. Coemergence of insomnia and a shift in the Th1/Th2 balance toward Th2 dominance. NeuroImmunoModulation. 2002;10(6):337–343. doi: 10.1159/000071474. [DOI] [PubMed] [Google Scholar]
- Sartorious N. Comorbidity of mental and physical diseases: a main challenge for medicine of the 21st century. Shanghai Arch. Psychiatry. 2013;25(2):68–69. doi: 10.3969/j.issn.1002-0829.2013.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sephton S.E., Dhabhar F.S., Keuroghlian A.S., Giese-Davis J., McEwen B.S., Ionan A.C., Spiegel D. Depression, cortisol, and suppressed cell-mediated immunity in metastatic breast cancer. Brain Behav. Immun. 2009;23(8):1148–1155. doi: 10.1016/j.bbi.2009.07.007. [DOI] [PubMed] [Google Scholar]
- Silber T.J., Chan M. Immunologic cytofluorometric studies in adolescents with anorexia nervosa. Int. J. Eat. Disord. 1996;19(4):415–418. doi: 10.1002/(sici)1098-108x(199605)19:4%3C415::aid-eat10%3E3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Smith A., Vollmer-Conna U., Bennett B., Wakefield D., Hickie I., Lloyd A. The relationship between distress and the development of a primary immune response to a novel antigen. Brain Behav. Immun. 2004;18(1):65–75. doi: 10.1016/s0889-1591(03)00107-7. [DOI] [PubMed] [Google Scholar]
- Snyder B.K., Roghmann K.J., Sigal L.H. Effect of stress and other biopsychosocial factors on primary antibody response. J. Adolesc. Health Care Off. Publ. Soc. Adolesc. Med. 1990;11(6):472–479. doi: 10.1016/0197-0070(90)90105-b. [DOI] [PubMed] [Google Scholar]
- Snyder B.K., Roghmann K.J., Sigal L.H. Stress and psychosocial factors: effects on primary cellular immune response. J. Behav. Med. 1993;16(2):143–161. doi: 10.1007/BF00844890. [DOI] [PubMed] [Google Scholar]
- Solomon G.F., Rubbo S.D., Batchelder E. Secondary immune response to tetanus toxoid in psychiatric patients. J. Psychiatr. Res. 1968;7(3):201–207. doi: 10.1016/0022-3956(70)90007-5. [DOI] [PubMed] [Google Scholar]
- Spiegel K., Sheridan J.F., Van Cauter E. Effect of sleep deprivation on response to immunization. JAMA. 2002;288(12):1471–1472. doi: 10.1001/jama.288.12.1471-a. [DOI] [PubMed] [Google Scholar]
- Stepanski E., Zorick F., Roehrs T., Young D., Roth T. Daytime alertness in patients with chronic insomnia compared with asymptomatic control subjects. Sleep. 1988;11(1):54–60. doi: 10.1093/sleep/11.1.54. [DOI] [PubMed] [Google Scholar]
- Sterne J.A.C., Savović J., Page M.J., Elbers R.G., Blencowe N.S., Boutron I., Cates C.J., Cheng H.-.Y., Corbett M.S., Eldridge S.M., Hernán M.A., Hopewell S., Hróbjartsson A., Junqueira D.R., Jüni P., Kirkham J.J., Lasserson T., Li T., McAleenan A., Reeves B.C., Shepperd S., Shrier I., Stewart L.A., Tilling K., White I.R., Whiting P.F., Higgins J.P.T. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- Sterne J.A., Hernan M.A., Reeves B.C., Savovic J., Berkman N.D., Viswanathan M., et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stubbs B., Vancampfort D., De Hert M., Mitchell A.J. The prevalence and predictors of type two diabetes mellitus in people with schizophrenia: a systematic review and comparative meta-analysis. Acta Psychiatr. Scand. 2015;132(2):144–157. doi: 10.1111/acps.12439. [DOI] [PubMed] [Google Scholar]
- Suvisaari J., Loo B.M., Saarni S.E., Haukka J., Perälä J., Saarni S.I., Viertiö S., Partti K., Lönnqvist J., Jula A. Inflammation in psychotic disorders: a population-based study. Psychiatry Res. 2011;189(2):305–311. doi: 10.1016/j.psychres.2011.07.006. [DOI] [PubMed] [Google Scholar]
- Taylor D.J., Kelly K., Kohut M.L., Song K.S. Is Insomnia a risk factor for decreased influenza vaccine response? Behav. Sleep Med. 2017;15(4):270–287. doi: 10.1080/15402002.2015.1126596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trzonkowski P., Myśliwska J., Godlewska B., Szmit E., Łukaszuk K., Wieckiewicz J., Brydak L., Machała M., Landowski J., Myśliwski A. Immune consequences of the spontaneous pro-inflammatory status in depressed elderly patients. Brain Behav. Immun. 2004;18(2):135–148. doi: 10.1016/S0889-1591(03)00111-9. [DOI] [PubMed] [Google Scholar]
- Van Praag H.M. Can stress cause depression? World J. Biol. Psychiatry. 2005;6:5–22. doi: 10.1080/15622970510030018. [DOI] [PubMed] [Google Scholar]
- Vancampfort D., Mitchell A.J., De Hert M., Sienaert P., Probst M., Buys R., Stubbs B. Prevalence and predictors of type 2 diabetes mellitus in people with bipolar disorder: a systematic review and meta-analysis. J. Clin. Psychiatry. 2015;76(11):1490–1499. doi: 10.4088/JCP.14r09635. [DOI] [PubMed] [Google Scholar]
- Vaughan W.T., Sullivan J.C., Elmadjian F. Immunity and schizophrenia; a survey of the ability of schizophrenic patients to develop an active immunity following the injection of pertussis vaccine. Psychosom. Med. 1949;11(6):327–333. doi: 10.1097/00006842-194911000-00001. [DOI] [PubMed] [Google Scholar]
- Vedhara K., Cox N.K., Wilcock G.K., Perks P., Hunt M., Anderson S., Lightman S.L., Shanks N.M. Chronic stress in elderly carers of dementia patients and antibody response to influenza vaccination. Lancet. 1999;353(9153):627–631. doi: 10.1016/S0140-6736(98)06098-X. [DOI] [PubMed] [Google Scholar]
- Wang Y., Yu L., Zhou H., Zhou Z., Zhu H., Li Y., Zheng Z., Li X., Dong C. Serologic and molecular characteristics of hepatitis B virus infection in vaccinated schizophrenia patients in China. J. Infect. Dev. Ctries. 2016;10(4):427–431. doi: 10.3855/jidc.7377. [DOI] [PubMed] [Google Scholar]
- Wong S.Y., Wong C.K., Chan F.W., Chan P.K., Ngai K., Mercer S., Woo J. Chronic psychosocial stress: does it modulate immunity to the influenza vaccine in Hong Kong Chinese elderly caregivers? Age (Dordr) 2013;35(4):1479–1493. doi: 10.1007/s11357-012-9449-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, n.d. 2022 International statistical classification of diseases and related health problems (ICD). https://www.who.int/standards/classifications/classification-of-diseases (Accessed Aug 8, 2021).
- Xiong J., Lipsitz O., Nasri F., Lui L., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zastrow A., Schnitzler P., Eckerle I., Herzog W., Friederich H.C. Immunogenicity and safety of H1N1 vaccination in anorexia nervosa–results from a pilot study. Int. J. Eat. Disord. 2012;45(1):146–149. doi: 10.1002/eat.20908. [DOI] [PubMed] [Google Scholar]
- Zhu H., Liu X., Xue Y., Shen C., Li Y., Wang A., Ding Y., Zheng Z., Dong C. Seroepidemiology of hepatitis B virus infection among Chinese schizophrenia patients. J. Infect. Dev. Ctries. 2015;9(5):512–518. doi: 10.3855/jidc.5416. [DOI] [PubMed] [Google Scholar]
- Zimmermann P., Curtis N. Factors that influence the immune response to vaccination. Clin. Microbiol. Rev. 2019;32(2):e00084. doi: 10.1128/CMR.00084-18. -18. [DOI] [PMC free article] [PubMed] [Google Scholar]