Abstract
The acquired preparedness (AP) model of eating disorder (ED) risk suggests transaction between impulsive traits and eating expectancies, though there remains a lack of research investigating distinct facets of impulsivity within this framework. This study examined how different facets of impulsivity moderate associations between eating expectancies and binge-eating severity in daily life. Women with binge-eating symptoms (N = 40) completed surveys followed by 10 days of ecological momentary assessment (EMA). Generalized estimating equations examined the independent and interactive effects of impulsivity facets and eating expectancies on EMA-measured binge-eating severity. Significant interactions were found between eating expectancies and emotional and behavioral impulsivity, but not a cognitive facet. Results suggest that among women high in emotional impulsivity, those with greater eating expectancies report higher binge-eating severity. Conversely, among those with lower behavioral impulsivity, those with lower eating expectancies report lower binge-eating severity. Future prospective work is needed with non-clinical samples.
Keywords: impulsivity, eating expectancies, binge eating, women’s health
Risk for binge eating is multi-faceted, though both dispositional characteristics (e.g., impulsivity) and learned expectancies that eating will reduce aversive emotional states (i.e., negative affect eating expectancies; Combs, Smith, Flory, Simmons, & Hill, 2010) are consistent predisposing factors that have emerged across the literature (Culbert, Racine, & Klump, 2015; Pearson, Wonderlich, & Smith, 2015). While these factors are implicated in the acquired preparedness (AP) model of eating disorder (ED) risk (Combs et al., 2010), there remains limited research assessing the relevance of particular facets of impulsive traits. The AP model of ED risk denotes the theory that individuals are differentially at risk to acquire various eating expectancies given predisposing trait level differences; this theory notably differs from other models, such as affect regulation models, given its focus on both disposition and psychosocial learning (Combs et al., 2010). In the application of the AP model to ED risk, researchers have largely focused on transactions between the high-risk dispositional trait of negative urgency and the expectation that eating will alleviate negative affect (e.g., Combs & Smith, 2009; Pearson, Combs, Zapolski, & Smith, 2012; Racine & Martin, 2017).
As such, eating expectancies are an important construct in the AP model of ED risk, which refer to anticipated outcomes related to the consumption of food based on past reinforcement from eating (Hohlstein, Smith, & Atlas, 1998). By reducing negative affect in the short-term, binge eating becomes negatively reinforced, and thus individuals learn to expect that binge eating can regulate emotion (i.e., negative affect eating expectancy). Expectancies subsequently inform future behaviors, such that individuals are likely to engage in behaviors (e.g., binge eating) associated with rewarding outcomes (e.g., reduction in negative affect; Hohlstein et al., 1998). Although the AP model is traditionally a mediational model, studies have also considered whether learned disorder-specific risk factors contribute to different symptom presentation in individuals with high negative urgency using a moderation framework. Racine and Martin (2016) found that ED-specific risk factors moderated associations between negative urgency and dysregulated eating while an earlier study by Fischer, Anderson, and Smith (2004) similarly found that eating expectancies moderated an association between negative urgency and binge eating. Within cross-sectional models, the AP model may imply that individuals with both impulsivity and negative affect eating expectancies are at greatest risk for disordered eating symptoms at a given time point.
As demonstrated by Fischer and collegaues (2004), dispositional characteristics, particularly impulsivity, interact with eating expectancies. Various studies highlight that the construct of impulsivity is multidimensional in nature (e.g., Smith et al., 2007; Whiteside & Lynam, 2001), and a recent study found that different facets of impulsivity evidenced differential associations with eating pathology (Schaumberg et al., 2020). Despite this growing knowledge, the majority of research on the AP model has focused on emotional impulsivity (negative urgency -- i.e., the tendency to act rashly in response to negative emotions), with less attention to paid to other facets of impulsivity, such as one’s ability to focus attention and inhibit inappropriate behavior, irrespective of emotional states (i.e., effortful control; Evans & Rothbart, 2007). Although not assessed via its interaction with eating expectancies, lower levels of effortful control have been associated with binge eating behavior in a clinical sample (Claes, Robinson, Muehlenkamp, Vandereycken, & Bijttebier, 2010).
To address this gap, the current study investigated how facets of impulsivity interact with negative affect eating expectancies to predict momentary binge-eating severity in daily life. Exploring interactions between distinct components of impulsivity and eating expectancies will lend more nuanced understanding to the AP model and the specific dispositions that confer increased risk for severity of binge-eating symptoms in daily life. It was generally expected that eating expectancies would interact with impulsivity to predict binge-eating severity, such that the relationship between eating expectancies and binge-eating severity would be stronger among individuals higher in various facets of impulsivity. Whether this pattern of results holds for all facets of impulsivity is exploratory in nature.
Materials and Methods
Participants
Participants were women who engaged in recurrent binge eating that were recruited from clinical and community settings. Initial screening data indicated that over the prior 6 months, 62.5% of participants attended individual psychotherapy, 12.5% had attended group psychotherapy, and 10.0% had attended community support groups. In addition, 40.0% reported taking medication for eating, mood, or weight. Study eligibility included endorsement of regular binge eating (i.e., ≥once/week over the past three months) as determined by the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, 5th Edition, Research Version (SCID-5-RV; First, 2015), self-identification as female, and being 18–65 years old. The final sample (N=40; 87.5% non-Hispanic White) included 29 women with binge-eating disorder, 9 with bulimia nervosa, 1 with anorexia nervosa binge-purge subtype, and 1 with subthreshold binge-eating disorder.
Procedure
Participants were recruited from clinical and community settings, and completed a phone screen to confirm initial eligibility. Detailed descriptions of sampling procedures have been documented in previous studies using the same sample (Smith et al., 2020; Smith et al., 2020; Smith et al., 2020). Participants first completed a study visit followed by an 11-day EMA protocol on smart tablets using the Momentary Assessment Tool (Dvorak, 2018); the first day was a practice day and not included in analyses. During EMA, participants received five signal-contingent prompts between 8:30 a.m. and 9:00 p.m. Participants were also instructed to complete event-contingent recordings after eating episodes. After the EMA protocol, participants returned the tablet and received payment for participation. The study received IRB approval and participants provided written informed consent.
Measures
Baseline measures.
The following between-subjects measures were assessed at baseline.
Difficulties in Emotion Regulation-Short Form (DERS-SF; Kaufman et al., 2016).
The DERS-SF is an 18-item measure that assesses emotion regulation dimensions, with higher scores reflecting greater emotion dysregulation. The present study used the difficulties in engaging in goal directed behavior (DERS-SF-G; α=.94) and impulse control difficulties (DERS-SF-IMP; α=.94) subscales as measures of emotion-related impulsivity to assess problems accomplishing tasks when distressed and difficulties controlling behaviors when distressed, respectively.
UPPS-P Negative Urgency Scale (UPPS-P-NU; Whiteside & Lynam, 2001).
The UPPS-P-NU is a 4-item subscale of the UPPS-P that was used as another measure of emotion-related impulsivity. The UPPS-P-NU assesses the tendency to act rashly in response to negative emotions. Higher total scores reflect greater negative urgency (α=.80).
Effortful Control Scale (ECS; Evans & Rothbart, 2007).
The ECS is a 19-item measure that assesses components of effortful control that are linked to executive functioning irrespective of emotional context. Higher total scores indicating better effortful control. The present study used the attentional control (ECS-ATT; α=.78) and inhibitory control subscales (ECS-INH; α=.70), which measure abilities to focus attention (i.e., cognitive impulsivity) and inhibit inappropriate behavior (i.e., behavioral impulsivity), respectively.
Eating Expectancies Inventory (EEI; Hohlstein et al., 1998).
The EEI is a 34-item self-report measure that assesses participants’ cognitive expectancies for reinforcement from eating. The EEI is composed of five subscales. In the present study, participants completed the Eating Helps Manage Negative Affect (EEI-NA) subscale of the EEI that measures the degree to which individuals believe that eating will alleviate negative affect. Higher scores indicating greater negative affect eating expectancies (α=.89).
EMA measure.
The following measure was assessed via within-subjects momentary EMA signals.
Binge Eating.
EMA-reported eating episodes were assessed with questions assessing loss of control eating (While you were eating, to what extent did you: feel a sense of loss of control?; feel that you could not stop eating once you started?; feel disconnected [e.g., numb, zoned out, on auto-pilot]?) and overeating (To what extent do you: feel that you overate?; think that others would consider what you ate to be an usual or excessive amount of food?). Items were rated on a 5-point scale (not at all to extremely). Loss of control and overeating ratings were averaged to create a composite score of binge-eating severity at each eating episode (α=.94).
Statistical Analyses
To determine whether the DERS-SF-G, DERS-SF-IMP, and UPPS-NU reflected a single construct of emotional impulsivity, factor analytic strategies were used. A latent emotional impulsivity factor was first derived using total scores, which were moderately correlated (rs=.28-.58). A factor score was calculated for each participant using principal component analysis, which extracted one component with an Eigenvalue > 1. The three component loadings ranged between 0.74 and 0.89, and the variance accounted for by the extracted component was 64.68%. In subsequent analyses, the derived factor scores for each participant were used to reflect the latent variable of emotional impulsivity.
Generalized estimating equations (GEEs) examined the independent and interactive effects of impulsivity facets (emotional impulsivity factor score, ECS-ATT, ECS-INH) and EEI-NA (standardized z-scores) on EMA-measured binge-eating severity ratings. GEEs used an AR1 serial autocorrelation and gamma link functions given that each participant had multiple ratings of binge-eating symptoms. Age, BMI, and presence of regular compensatory behaviors were included as covariates. Presence of compensatory behaviors was coded as a dichotomous variable based on ED diagnosis (i.e., BED/subclinical BED vs. BN/AN-BP).
Results
A total of 1,399 eating episodes were reported via EMA, with 90.3% compliance to random prompts. GEE results are shown in Table 1. Across models, there were no significant main effects of the EEI-NA or impulsivity facets predicting EMA-measured binge-eating severity. However, there were significant interactions between EEI-NA and emotional impulsivity (p=.017), and between EEI-NA and ECS-INH (p=.016). As shown in Figure 1, women who reported greater emotional impulsivity and endorsed higher eating expectancies reported greater binge-eating severity across EMA relative to those with greater emotional impulsivity and lower eating expectancies. At 1 SD below the emotional impulsivity mean, β = −0.05, p = .413. At 1 SD above the emotional impulsivity mean, β = 0.15, p = .014. At low levels of emotional impulsivity, binge-eating severity did not differ based on eating expectancies. Those who reported higher inhibitory control on the ECS-INH and endorsed lower eating expectancies reported the lowest binge-eating severity across EMA (Figure 2). At 1 SD below the ECS-INH mean, β = 0.01 and p < .001. At 1 SD above the ECS-INH mean, β = 0.15 and p = .017. No interactive effects were found between EEI-NA and scores on the ECS-ATT.
Table 1.
Generalized estimating equation results predicting EMA-measured binge eating severity
| β | SE | Lower CI | Upper CI | Wald χ2 | p | |
|---|---|---|---|---|---|---|
|
| ||||||
| Intercept | 0.73 | 0.09 | 0.56 | 0.90 | 68.26 | <0.001 |
| Compensatory behavior | −0.12 | 0.11 | −0.34 | 0.10 | 1.08 | 0.300 |
| Age | <−0.01 | <0.01 | −0.01 | <0.01 | 0.37 | 0.543 |
| BMI | <−0.01 | 0.01 | −0.02 | 0.01 | 0.85 | 0.356 |
| EEI-NA | 0.05 | 0.04 | −0.02 | 0.13 | 1.87 | 0.172 |
| Emotional impulsivity | −0.01 | 0.05 | −0.11 | 0.08 | 0.09 | 0.765 |
| EEI-NA x emotional impulsivity | 0.11 | 0.05 | 0.02 | 0.20 | 5.65 | 0.017 |
| Intercept | 0.82 | 0.09 | 0.64 | 1.00 | 77.08 | <0.001 |
| Compensatory behavior | −0.21 | 0.12 | −0.44 | 0.02 | 3.28 | 0.070 |
| Age | <−0.01 | <0.01 | −0.01 | <0.01 | 0.46 | 0.496 |
| BMI | −0.01 | 0.01 | −0.02 | <0.01 | 1.63 | 0.202 |
| EEI-NA | 0.03 | 0.05 | −0.06 | 0.13 | 0.51 | 0.476 |
| ECS-ATT | −0.04 | 0.04 | −0.12 | 0.05 | 0.69 | 0.406 |
| EEI-NA x ECS-ATT | −0.06 | 0.04 | −0.13 | 0.01 | 2.58 | 0.108 |
| Intercept | 0.76 | 0.07 | 0.62 | 0.89 | 115.81 | <0.001 |
| Compensatory behavior | −0.12 | 0.09 | −0.30 | 0.06 | 1.59 | 0.207 |
| Age | <−0.01 | <0.01 | −0.01 | <0.01 | 0.50 | 0.480 |
| BMI | −0.01 | <0.01 | −0.02 | <0.01 | 2.30 | 0.129 |
| EEI-NA | 0.08 | 0.04 | −0.01 | 0.17 | 3.15 | 0.076 |
| ECS-INH | −0.06 | 0.05 | −0.15 | 0.03 | 1.56 | 0.212 |
| EEI-NA x ECS-INH | 0.07 | 0.03 | 0.01 | 0.13 | 5.80 | 0.016 |
Note. CI=95% confidence interval; BMI=body mass index; EMA=ecological momentary assessment; EEI-NA= Eating Expectancies Inventory Eating Helps Manage Negative Affect scale; emotional impulsivity=latent factor derived from UPPS-P negative urgency subscale and Difficulties in Emotion Regulation-Short Form difficulties engaging in goal directed and impulse control difficulties subscales; ECS-INH=Effortful Control Scale inhibitory control subscale; ECS-ATT=ECS attentional control subscale. Compensatory behavior was coded such that participants with compensatory behaviors were the reference group.
Figure 1.
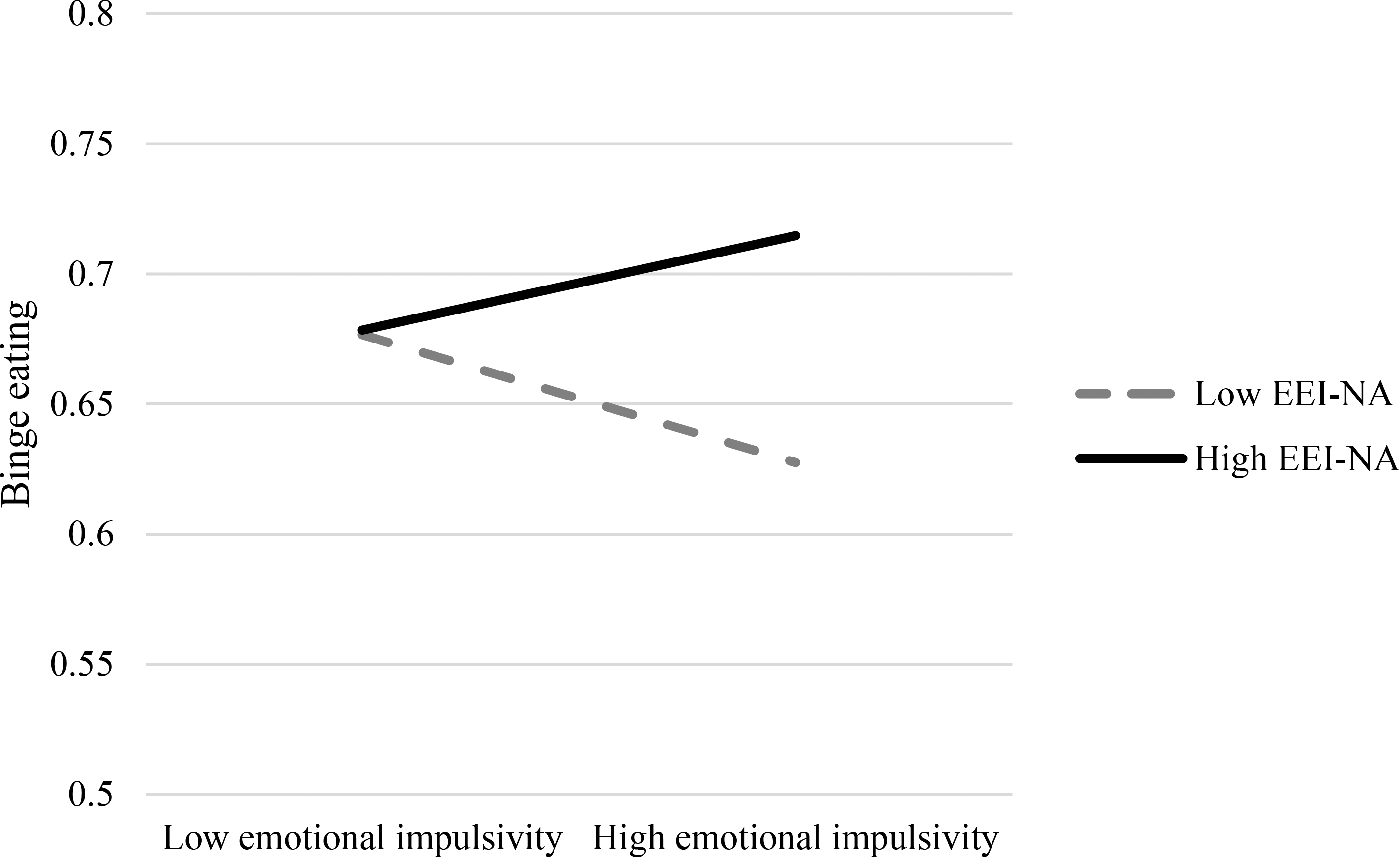
Interactions of emotional impulsivity (latent variable derived from DERS-SF-G, DERS-SF-IMP, and UPPS scores) and eating expectancies (EEI-NA) predicting EMA-measured binge eating severity. High and low values reflect 1 SD above and below sample means, respectively.
Figure 2.
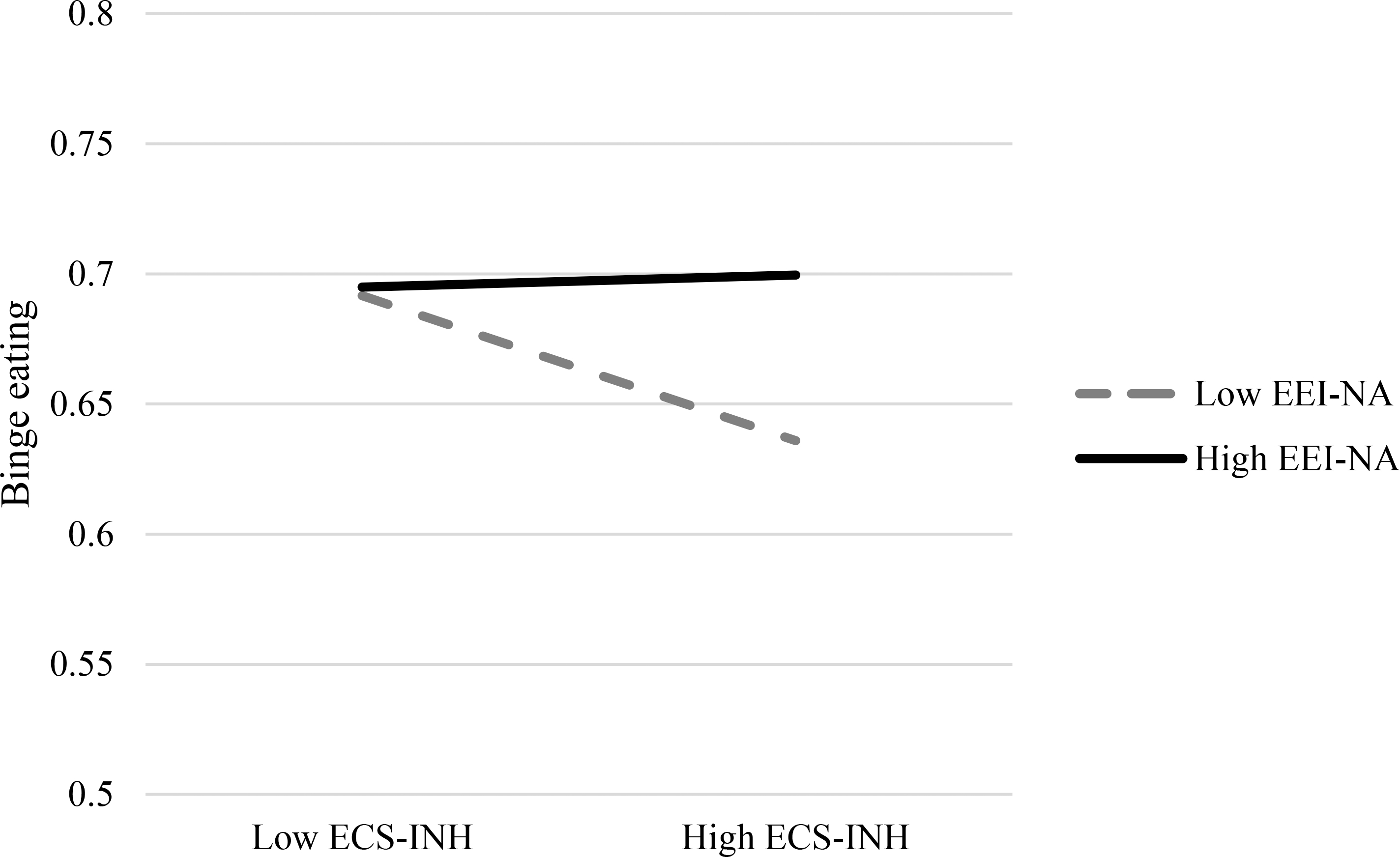
Interactions of behavioral impulsivity (ECS-INH) and eating expectancies (EEI-NA) predicting EMA-measured binge eating severity. High and low values reflect 1 SD above and below sample means, respectively.
Discussion
The present study evaluated how facets of impulsivity moderated associations between negative affect eating expectancies and binge-eating severity. Past studies have largely focused on the impact of emotional impulsivity on binge-eating severity within the context of the AP model (e.g., Pearson et al., 2012); this study extends previous research by investigating how other facets of impulsivity interact with negative affect eating expectancies to predict momentary binge-eating severity in daily life using an EMA design. Interactions were found between expectancies and two of the three facets of impulsivity (emotional impulsivity and ECS-INH), but not attentional control (ECS-ATT). Results suggest that among women who have greater negative affect eating expectancies, those with more impulsive tendencies when distressed (measured by the emotional impulsivity factor), report higher momentary binge-eating severity. Conversely, among women who endorse lower eating expectancies, those with lower overall behavioral impulsivity (measured by the ECS-INH) report the lowest severity of binge eating in daily life.
The interactive effects at high levels of emotional impulsivity align with tenets of the AP model that there is a transactional relationship between dispositional characteristics and learned expectancies (Combs et al., 2010). With respect to emotion-related impulsivity, women who have difficulties engaging in goal-directed behavior and controlling impulses when distressed may resort to immediately reinforcing behaviors (e.g., binge eating) to cope with negative affect, and for those who have developed high-risk eating expectancies this could potentiate future binge eating severity (Brockmeyer et al., 2014), thus creating an interactive effect between the two. Furthermore, lower behavioral impulsivity not intrinsically linked to emotion (i.e., higher ECS-INH scores) was associated with lower binge-eating severity at lower levels of eating expectancies. Thus, among individuals with a less developed expectancy that binge eating will serve to regulate emotions, an ability to inhibit inappropriate behavior may buffer against binge eating severity. The combination of low eating expectancies and high inhibitory control may buffer risk for binge eating severity. Given that directionality cannot be inferred from the current results, these facets of impulsivity should be examined in future longitudinal studies of the AP model using non-clinical samples.
It is important to note the lack of effects for attentional control (ECS-ATT). While attentional biases have been linked to binge eating severity (Stojek et al., 2018), cognitive dimensions of impulsivity may have a less direct effect on behavioral outcomes and/or may depend on one’s ability to inhibit behavioral responses. Much of the research in binge eating has focused on attentional biases to disorder-relevant stimuli (Stojek et al., 2018), and thus general attentional control may be less salient in predicting binge-eating severity.
This study used a sample of primarily Caucasian adult women and therefore these effects may not generalize to other demographic groups. In addition, the majority of participants in this study met criteria for an ED, and, because of this, variation related to impulsivity and expectancies may be limited, future research with non-clinical samples is warranted. The sample size was also modest, which may have limited ability to detect effects, and could explain the lack of significant main effects. Despite these limitations, the present study provides preliminary evidence of important interactions between emotional and attentional impulsivity and eating expectancies that lend nuance to the AP model of ED risk.
Future research should explore the impact of other facets of eating expectancies and impulsivity, such as eating to alleviate boredom and sensation seeking (Hohlstein et al., 1998; Whiteside & Lynam, 2001). Given the use of a clinical sample, this research may lend credence to a maintenance model of binge eating behavior as opposed to traditional mediational designs that focus on the development of ED risk. By extending the present findings, therapeutic interventions for binge eating should address both dispositional and learning factors, which could prove useful for comprehensive binge eating intervention efforts. These intervention efforts might focus more on affective and behavioral as opposed to cognitive facets of impulsivity when treating individuals with binge eating.
Footnotes
Declaration of interest statement: The authors declare that they have no conflict of interest.
References
- Brockmeyer T, Skunde M, Wu M, Bresslein E, Rudofsky G, Herzog W, & Frederich HC (2014). Difficulties in emotion regulation across the spectrum of eating disorders. Comprehensive Psychiatry, 55, 565–571. [DOI] [PubMed] [Google Scholar]
- Claes L, Robinson MD, Muehlenkamp JJ, Vandererycken W, & Bijttebier P (2010). Differentiating bingeing/purging and restrictive eating disorder subtypes: The roles of temperament, effortful control, and cognitive control. Personality and Individual Differences, 48, 166–170. [Google Scholar]
- Combs JL & Smith GT (2009). The acquired preparedness model of risk for binge eating disorder: Integrating non-specific and specific risk processes. In Chambers N (Ed.), Binge Eating: Psychological factors, symptoms, and treatment (pp. 55–86). Nova Science: New York. [Google Scholar]
- Combs JL, Smith GT, Flory K, Simmons JR, & Hill KK (2010). The acquired preparedness model of risk for bulimic symptom development. Psychology of Addictive Behaviors, 24, 475–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culbert KM, Racine SE, & Klump KL (2015). Research Review: What we have learned about the causes of eating disorders–a synthesis of sociocultural, psychological, and biological research. Journal of Child Psychology and Psychiatry, 56, 1141–1164. [DOI] [PubMed] [Google Scholar]
- Dvorak RD (2018). Momentary Assessment Tool (MAT): An integrated mobile platform for ecological assessment and intervention [computer software]. Orlando, FL: The University of Central Florida. [Google Scholar]
- Evans DE, & Rothbart MK (2007). Developing a model for adult temperament. Journal of Research in Personality, 41(4), 868–888. [Google Scholar]
- First MB (2015, January 23). Structured Clinical Interview for the DSM (SCID). Retrieved from https://onlinelibrary.wiley.com/
- Fischer S, Anderson KG, & Smith GT (2004). Coping with distress by eating or drinking: role of trait urgency and expectancies. Psychology of Addictive Behaviors, 18, 269–274. [DOI] [PubMed] [Google Scholar]
- Hohlstein LA, Smith GT, & Atlas JG (1998). An application of expectancy theory to eating disorders: Development and validation of measures of eating and dieting expectancies. Psychological Assessment, 10, 49–58. [Google Scholar]
- Kaufman EA, Xia M, Fosco G, Yaptangco M, Skidmore CR, & Crowell SE (2016). The Difficulties in Emotion Regulation Scale Short Form (DERS-SF): Validation and replication in adolescent and adult samples. Journal of Psychopathology and Behavioral Assessment, 38(3), 443–455. [Google Scholar]
- Pearson CM, Combs JL, Zapolski TC, & Smith GT (2012) A longitudinal transactional risk model for early eating disorder onset. Journal of Abnormal Psychology, 3, 707–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson CM, Wonderlich SA, & Smith GT (2015). A risk and maintenance model for bulimia nervosa: From impulsive action to compulsive behavior. Psychological Review, 122, 516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine SE & Martin SJ (2016). Exploring divergent trajectories: Disorder-specific moderators of the association between negative urgency and dysregulated eating. Appetite, 103, 45–53. [DOI] [PubMed] [Google Scholar]
- Racine SE & Martin SJ (2017). Integrating eating disorder-specific risk factors into the acquired preparedness model of dysregulated eating: A moderated mediation analysis. Eating Behaviors, 24, 54–60. [DOI] [PubMed] [Google Scholar]
- Schaumberg K, Wonderlich S, Crosby R, Peterson C, LeGrange D, Mitchell JE …Bardone-Cone AM (2020). Impulsivity and anxiety-related dimensions in adults with bulimic-spectrum disorders differentially relate to eating disordered behaviors. Eating Behaviors, 37, 101382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith GT, Fischer S, Cyders MA, Annus AM, Spillane NS, & McCarthy DM (2007). On the validity and utility of discriminating among impulsivity-like traits. Assessment, 14, 155–170. [DOI] [PubMed] [Google Scholar]
- Smith KE, Schaumberg K, Reilly EE, Anderson LM, Schaefer LM, Dvorak R, Crosby RD, & Wonderlich SA (2020). Examining the ecological validity of trait-level rumination measures among women with binge eating symptoms. Eating and Weight Disorders. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith KE, Mason TB, Juarascio A, Weinbach N, Dvorak R, Crosby RD, & Wonderlich SA (2020). The momentary interplay of affect, attention bias, and expectancies as predictors of binge eating in the natural environment. International Journal of Eating Disorders, 53, 586–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith KE, Mason TB, Schaefer LM, Juarascio A, Dvorak R, Weinbach N, Crosby RD, & Wonderlich SA (2020). Examining intra-individual variability in food-related inhibitory control and negative affect as predictors of binge eating using ecological momentary assessment. Journal of Psychiatric Research, 120, 137–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stojek M, Shank LM, Vannucci A, Bongiorno DM, Nelson EE, Waters AJ, ... & Tanofsky-Kraff M (2018). A systematic review of attentional biases in disorders involving binge eating. Appetite, 123, 367–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteside SP, & Lynam DR (2001). The Five Factor Model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences, 30(4), 669–689. [Google Scholar]


